Funding: The development of this material was supported in part through funding from the Genetics in Primary Care (GPC): A Faculty Development Initiative. The GPC is a contract (# 240-98-0020) funded by the Maternal and Child Health Bureau and Bureau of Health Professions, Health Resources and Services Administration, with co-funding from the National Human Genome Research Institute, National Institutes of Health, and the Agency for Healthcare Research and Quality.
Your patient, a 36-year-old woman, recently learned that her former college roommate was diagnosed with breast cancer. She wants to know if she should have the genetic test her friend mentioned to assess her risk. Her only family history is that her mother has breast cancer at age 72. She mentions that her roommate did not have a family history of breast cancer, “except on her father's side, and that doesn't count.”
Table 1.
| Nongenetic contributors to breast cancer risk |
|---|
|
PREVALENCE
The National Cancer Institute estimates that about 1 in 50 women will have breast cancer by age 50 years and that about 1 in 10 women in the United States will develop breast cancer by age 80 years.1 Excluding cancers of the skin, breast cancer is the most common cancer among women, accounting for 1 of 3 cancer diagnoses. Male breast cancer is rare. The ratio of male breast cancer to female breast cancer is 1:125.
Women commonly overestimate their lifetime risk of breast cancer to a substantial degree,2,3,4,5 and they overestimate the proportion of female deaths attributable to breast cancer.4, 6 In 1 survey, for example, women between ages 40 and 50 years overestimated their short-term risk of dying of breast cancer by 22-fold and their lifetime risk by 12-fold.4 Concerns about the appropriate use of genetic testing in general are amplified by the milieu of women's concerns about breast cancer. Studies have shown that women are receptive to BRCA1 and BRCA2 testing,7,8,9 despite the lack of a family history that might justify its use.
ETIOLOGY
Breast cancer is caused by both nongenetic (listed in the box) and genetic factors. Most of these risk factors, with the exception of atypical hyperplasia, produce less than a 2-fold increase in the risk of breast cancer and, thus, may contribute relatively little to risk in women from high-risk families. Other possible risk factors include a diet that is high in fat and low in fiber, fruits, and vegetables; lack of exercise; and induced abortion. The relationship between these risk factors and a genetic predisposition is not yet understood. Some hormonal risk factors such as age of menarche and of menopause could be influenced by polygenic inheritance. A family history of breast cancer is a rare but important contributor to breast cancer risk.
Women at high risk of inherited breast cancer typically have several relatives who had breast cancer diagnosed before age 45 to 50 years and 1 or more relatives affected with bilateral or multifocal breast cancer; they may also have a family history of ovarian cancer or male breast cancer.10
BRCA1 AND BRCA2
Mutations in the BRCA1 and BRCA2 genes have been identified as a cause of inherited susceptibility to breast and ovarian cancer. The estimated lifetime risk of breast cancer associated with BRCA1 and BRCA2 mutations ranges from 30% to 85%. Penetrance is probably determined in part by the nature of specific mutations and in part by environmental and genetic modifiers.11, 12 For women in an unselected population found to have a BRCA1 or BRCA2 mutation, the predictive value of the test would be less certain and probably at the lower end of the range.13,14,15,16
Out of 10,000 women, 1,000 will have a mother or sister who has had breast cancer, but only 15 have a BRCA1 or BRCA2 mutation that confers high risk. It is estimated that in a primary care practice of 1,000 patients, 1 case of breast cancer will be diagnosed every 1 to 2 years, but 1 case of inherited breast cancer due to BRCA1 or BRCA2 mutation will be diagnosed every 20 years.17
Table 2.
| Aspects of the family history useful in risk assessment for breast cancer |
|---|
|
Other genetic factors
Details of extremely rare genetic syndromes with a high breast cancer risk are given at www.geneclinics.org/profiles/brca/index.html. Current research also suggests a possible risk association between breast cancer and several common genetic variants. Common genetic variants are likely to be considerably more common than high-risk cancer-predisposing mutations and, as a result may have a larger effect on overall population risk. In addition, the effect of genetic variants of this kind is likely to vary with environmental exposures and other nongenetic risk factors.
RISK ASSESSMENT
The risk of breast cancer developing depends on a person's family history and nongenetic risk factors. When taking a family history to be used in estimating breast cancer risk, the physician should obtain a history of all cancers in biologic relatives, especially breast and ovarian cancers. The next box lists aspects of the family history that can be used to identify high-risk individuals.
GENERAL RISK FOR THE DEVELOPMENT OF BREAST CANCER BASED ON FAMILY HISTORY
Women can be stratified into high, moderate, and average risk by the family history.
High risk
Women at high risk typically have several relatives who had breast cancer diagnosed before age 45 to 50 years and 1 or more relatives affected with bilateral or multifocal breast cancer; they may also have a family history of ovarian cancer or male breast cancer.10
Moderate risk
Women with a single affected first-degree relative who has cancer or more distantly related family members who have breast cancer are usually at only moderately increased risk.
Average risk
Women with a first-degree relative who had cancer diagnosed after age 60 years or 2 second-degree relatives who had cancer diagnosed after age 50 years may have a risk indistinguishable from the average risk.18
INTERPRETING FAMILY HISTORY WHEN HIGH-RISK CRITERIA ARE NOT PRESENT
Two empiric models for predicting breast cancer risk are available: the Gail model,19 which is based on nongenetic factors and limited family history, and the Claus model,18 which is based solely on family history. Both have limitations, and the risk estimates derived from the 2 models may differ for an individual patient. Despite their limitations, they represent the best methods currently available for individual risk assessment. However, they do not provide information about the likelihood of having a BRCA1 or BRCA2 mutation.
Table 4.
| Inherited breast cancer risk |
|---|
| In evaluating the family history for inherited breast cancer risk, consider the following: |
|
The Gail model projects individualized probabilities of developing breast cancer based on the major predictors of risk: current age, age at menarche, age at first live birth, number of previous breast biopsies, presence of atypical hyperplasia, and number of first-degree relatives (mother or sister) with breast cancer. It provides a useful estimate of risk for women who do not have a family history of breast cancer. Because it does not consider second-degree relatives, paternal relatives, ethnicity, ages of diagnosis of breast cancer, or genetically related cancer other than breast cancer, the Gail model is not useful for assessing women whose risk primarily is inherited factors.20
The Claus model uses empiric data from the Cancer and Steroid Hormone Study.21 The risk estimate is based on a woman's current age and the number of first- and second-degree relatives with breast cancer and their age of diagnosis. It does not take into consideration any other factors known to increase breast cancer risk. It is not intended to be used in families with highly penetrant mutations in susceptibility genes such as BRCA1 or BRCA2 because it may underestimate risk if the patient does not have sisters, if the inheritance is paternal, or if the family history is of ovarian rather than breast cancer.20
The Claus risk model provides the best available estimate of risk based on family history of breast cancer that is not high risk and can be used to reassure most women whose inherited risk is low (table 1). Compared with the average woman's risk of 10% of having breast cancer by age 80 years, the risk is significantly higher only when a relative is affected before age 50 or when several relatives are affected. As a result, most women with a family history, such as the woman in the case example, can be reassured about their risk.
Table 1.
Estimated risk of breast cancer according to family history*
| Breast cancer in a mother or sister, by age when affected, yr | Risk of breast cancer by age 79, % | Breast cancer in a mother and sister, both affected at age, yr | Risk of breast cancer by age 79, % |
|---|---|---|---|
| 20-29 | 21 | 20-29 | 48 |
| 30-39 | 17 | 30-39 | 44 |
| 40-49 | 13 | 40-49 | 35 |
| 50-59 | 11 | 50-59 | 25 |
| 60-69 | 10 | 60-69 | 16 |
| 70-79 | 9 | 70-79 | 11 |
From Claus et al.18
INTERPRETING FAMILY HISTORY WHEN HIGH-RISK CRITERIA ARE PRESENT
There is no simple, well-defined threshold for high risk. In general, the more family history risk factors present, the greater the likelihood that an inherited risk is present. When obtaining a triaged family history (see Gene Scene, wjm July 2001;175:48-49), look for red flags that suggest that further evaluation of the patient's family history is indicated (see next box).
Studies indicate that a BRCA1 or BRCA2 cancer-predisposing mutation is more likely to be present if the family history includes Ashkenazi Jewish ancestry, breast cancer diagnosed before age 50 years, bilateral breast cancer, breast cancer in a male, ovarian cancer, or the occurrence of both breast cancer and ovarian cancer in the same person.22,23,24,25,26 (See www.geneclinics.org/profiles/brcal/index.html for more in-depth information.) Because these studies were based on referral populations, the quantitative estimates of mutation frequency cannot necessarily be generalized to patients seen in primary care settings.
A method of calculating the probability of the presence of a cancer-predisposing BRCA1 or BRCA2 mutation has been developed. This calculation is based on observations in referral populations in which most women tested were affected with cancer.26,27 CancerGene software includes these models and a tool for assessing the likelihood of a mutation (www.swmed.edu/home_pages/cancergene/).
GENETIC TESTING
Primary care physicians are faced with the question: To whom should DNA-based genetic testing be offered? The phrasing of the question as “offered” as opposed to “recommended” represents the 2 dynamics of the testing decision. First, is there a medical indication for the testing? and second, how do the benefits and risks of testing coincide with the patient's reasons for testing and management decisions she would make based on the results? (See www.geneclinics.org/profiles/brcal/index.html for a discussion of the efficacy of possible risk-reduction strategies.)
The offer of testing is actually to the patient's family because testing should be offered first to an affected family member. Once a cancer-predisposing mutation has been identified, testing is technically straightforward and can be done through a blood test. However, several factors complicate genetic testing for breast cancer risk. For example:
The cause of cancer predisposition has not yet been identified in some high-risk families, suggesting that additional genes and mutations have yet to be found. False-negative results are a significant problem.
Full-scale sequencing for BRCA1 and BRCA2 mutations can produce results of unknown clinical significance—such as when a previously undescribed sequence variant is found.
Full-scale sequencing for BRCA1 and BRCA2 mutations costs $2,600. (For women of Ashkenazi Jewish descent, a much less expensive test can be used that tests only for the 3 mutations that are common in this ethnic group.) Health insurance coverage varies.
Risk prediction for those carrying a mutation is imprecise.
In addition, the results of the test will affect other family members beyond your patient. The importance of providing education and obtaining informed consent before performing testing for cancer-predisposing gene mutations has been emphasized by several expert groups.28,29 Pretest counseling, often done by genetic counselors, addresses issues of the fees involved in testing and counseling; the meaning of positive and negative test results, including when the test is informative and when it is not; other options besides testing, including future discussion on the topic and/or DNA banking; medical interventions available for patients with high genetic risk; and possible psychological or economic effects of testing for individual and family members. Testing of at-risk asymptomatic relatives who are younger than 18 years is generally not recommended because of concerns about issues of informed consent among minors, the lack of proven surveillance or prevention strategies, and concerns about stigmatization and discrimination. The possible benefits and risks of testing as outlined in table 2 should be discussed so that the patient can make an informed decision on whether or not to pursue testing.
Table 2.
Arguments for and against BRCA1 and BRCA2 testing in women whose family history indicates high risk
| Arguments for testing | Arguments against testing |
|---|---|
| In a family with a known mutation (positive BRCA1 and BRCA2 test result in a family member with cancer), a negative test result in an at-risk family member means she has not inherited the mutation | In a family without a known mutation, a negative test result does not provide helpful information (noninformative test) |
| In a cancer patient: | In a cancer patient: |
| A positive test result could benefit relatives | Alternative approaches, such as DNA banking, might have less negative effect on labeling, psychological harms, etc |
| A positive test result might affect treatment or screening decisions | |
| Labeling: | Labeling: |
| Patients who have an identifiable mutation can be enrolled in research studies or registries and may be first in line for new therapies | A positive test result could have economic repercussions (insurance, employment discrimination) or lead to stigmatization—viewing oneself negatively or being treated differently by others |
| A positive test result may reduce feelings of self-blame and provide an explanation for disease | Patient's offspring and other relatives may also be affected by test results |
| Positive test results may increase patient's health efforts through: | Negative test results may decrease patient's health efforts through: |
| Clinical or breast self-examination, screening | False reassurance (reduced screening efforts, etc) |
| Lifestyle changes | Failure to relieve anxiety or provide explanation for cancer |
| Psychological benefits: | Psychological harms: |
| Increased sense of control | Alarm, confusion, anxiety, worry, depression, uncertainty, etc |
| Possible decreased anxiety | Concern about risk to offspring |
| Disruption of family relationships | |
| Possibility of improved certainty about the cancer risk in family members | Possibility of ambiguous or noninformative results |
Resources for primary care physicians and patients are listed in the next box.
If there is no other history of breast cancer and no history of ovarian cancer, your patient's risk of having breast cancer based on her family history is similar to that of an average-risk woman. There would be little justification for testing for the BRCA1 and BRCA2 genes in this patient, and testing could cause harm through false reassurance and its consequences. Your patient's likelihood of having a negative test result would be high, which could lead to a mistaken belief that her risk for breast cancer was lower than average because of the negative test result. In fact, her pretest risk estimate would not be changed by a negative test result because she is not expected to have a cancer-predisposing mutation. There has been little population-based testing of BRCA1 and BRCA2 (as opposed to testing in high-risk families in which the penetrance has been high). Thus, we could not provide her with accurate risk prediction information if her test results were positive. Therefore, the patient may benefit most from a discussion of risk that allows her to recognize her low short-term risk of breast cancer and a review of recommended breast cancer prevention strategies for the general population (mammography, breast self-examination, and clinician examination). Her lifetime risk of developing breast cancer remains at about 10%.
Your patient also has articulated a common misunderstanding—that a family history of a cancer that occurs predominantly in women is important only if the affected persons are related to the mother. In fact, cancer predisposition that is inherited in an autosomal dominant manner can be transmitted by either the father or the mother. The roommate had a paternal aunt with early-onset breast cancer and 2 paternal cousins with ovarian cancer. After individual and family genetic counseling, the roommate underwent BRCA1 and BRCA2 mutation analysis and was found to have a recognized cancer-predisposing mutation in BRCA1. The roommate's older brother had chosen to be tested to provide genetic counseling to his 2 daughters. The roommate's 50-year-old sister decided not to have testing because she did not have children, was getting routine mammograms, and was not interested in any other risk reduction interventions.
Table 6.
| Resources* |
|---|
|
Please see this article on our web site, www.ewjm.com, for a link to more contact information
Summary points
Women are concerned about breast cancer and often overestimate their risk; they may view themselves as candidates for molecular genetic testing even when their likelihood of having cancer is minimal
Mutations of the BRCA1 or BRCA2 genes are rare, and risk-reduction strategies are not well established by evidence-based medicine
Certain ethnic groups have a higher prevalence of clinically significant BRCA1 and BRCA2 gene mutations
Testing for BRCA1 and BRCA2 cancer-producing mutations is mentioned frequently in the medical and lay press; patients may ask about the availability of this testing
Molecular genetic testing of the BRCA1 and BRCA2 genes is being marketed to physicians
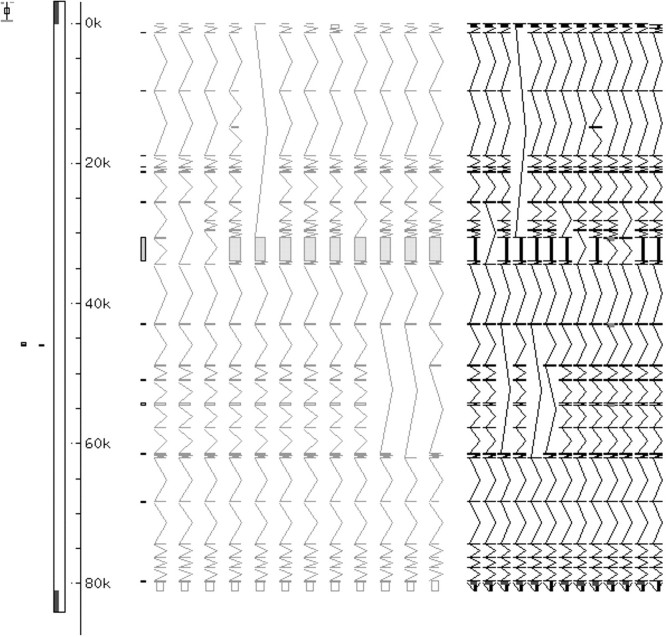
Figure 1.
BRCA1, human genome sequence
Acknowledgments
Information in this article was adapted from Culver JB, Hull J, Levy-Lahad E, Daly M, Burke W. Breast cancer genetics — an overview, and BRCA1 and BRCA2 hereditary breast/overian cancer (updated March 4, 2000). In: GeneClinics: Clinical Genetic Information Resource (database online]. Copyright, University of Washington, Seattle.
Competing interests: Dr Pinsky is affiliated with GeneClinics, an organization mentioned in this article.
References
- 1.Feuer EJ, Wun LM, Boring CC, Flanders WD, Timmel MJ, Tong T. The lifetime risk of developing breast cancer. J Natl Cancer Inst 1993;85: 892-897. [DOI] [PubMed] [Google Scholar]
- 2.McCaul KD, Branstetter AD, O'Donnell SM, Jacobson K, Quinlan KB. A descriptive study of breast cancer worry. J Behav Med 1998;21: 565-579. [DOI] [PubMed] [Google Scholar]
- 3.Alexander NE, Ross J, Sumner W, Nease RF Jr, Littenberg B. The effect of an educational intervention on the perceived risk of breast cancer. J Gen Intern Med 1996;11: 92-97. [DOI] [PubMed] [Google Scholar]
- 4.Black WC, Nease RF Jr, Tosteson AN. Perceptions of breast cancer risk and screening effectiveness in women younger than 50 years of age. J Natl Cancer Inst 1995;87: 720-731. [DOI] [PubMed] [Google Scholar]
- 5.Lavelle K, Charlton A. Women's perception of risk of cancer. BMJ 1998;317: 542-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gallup Survey 1995, cited in Mortality Vital Statistics Report. Med Tribune 1996;37: 17. [Google Scholar]
- 7.Chaliki H, Loader S, Levenkron JC, Logan-Young W, Hall WJ, Rowley PT. Women's receptivity to testing for a genetic susceptibility to breast cancer. Am J Public Health 1995;85: 1133-1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tambor ES, Rimer BK, Strigo TS. Genetic testing for breast cancer susceptibility: awareness and interest among women in the general population. Am J Med Genet 1997;68: 43-49. [PubMed] [Google Scholar]
- 9.Press NA, Yasui Y, Reynolds S, Durfy SJ, Burke W. Women's interest in genetic testing for breast cancer susceptibility may be based on unrealistic expectations. Am J Med Genet 2001;99: 99-110. [DOI] [PubMed] [Google Scholar]
- 10.Hoskins KF, Stopfer JE, Calzone KA, et al. Assessment and counseling for women with a family history of breast cancer: a guide for clinicians. JAMA 1995;273: 577-585. [PubMed] [Google Scholar]
- 11.Easton DF, Ford D, Bishop DT. Breast and ovarian cancer incidence in BRCA1-mutation carriers: Breast Cancer Linkage Consortium. Am J Hum Genet 1995;56: 265-271. [PMC free article] [PubMed] [Google Scholar]
- 12.Ford D, Easton DF, Stratton M, et al. Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families: The Breast Cancer Linkage Consortium. Am J Hum Genet 1998;62: 676-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thorlacius S, Struewing JP, Hartge P, et al. Population-based study of risk of breast cancer in carriers of BRCA2 mutation. Lancet 1998;352: 1337-1339. [DOI] [PubMed] [Google Scholar]
- 14.Struewing JP, Hartge P, Wacholder S, et al. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med 1997;336: 1401-1408. [DOI] [PubMed] [Google Scholar]
- 15.Fodor FH, Weston A, Bleiweiss IJ, et al. Frequency and carrier risk associated with common BRCA1 and BRCA2 mutations in Ashkenazi Jewish breast cancer patients. Am J Hum Genet 1998;63: 45-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burke W, Press N, Pinsky L. BRCA1 and BRCA2: a small part of the puzzle. J Natl Cancer Inst 1999;91: 904-905. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal TC, Puck SM. Screening for genetic risk of breast cancer. Am Fam Physician 1999;59: 99-104, 106. [PubMed] [Google Scholar]
- 18.Claus EB, Risch N, Thompson WD. Autosomal dominant inheritance of early-onset breast cancer: implications for risk prediction. Cancer 1994;73: 643-651. [DOI] [PubMed] [Google Scholar]
- 19.Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst 1989;81: 1879-1886. [DOI] [PubMed] [Google Scholar]
- 20.Garber J. A 40-year-old woman with a strong family history of breast cancer. JAMA 1999;282: 1953-1960. [DOI] [PubMed] [Google Scholar]
- 21.Claus EB, Risch N, Thompson WD. Genetic analysis of breast cancer in the Cancer and Steroid Hormone Study. Am J Hum Genet 1991;48: 232-242. [PMC free article] [PubMed] [Google Scholar]
- 22.Couch FJ, DeShano ML, Blackwood MA, et al. BRCA1 mutations in women attending clinics that evaluate the risk of breast cancer. N Engl J Med 1997;336: 1409-1415. [DOI] [PubMed] [Google Scholar]
- 23.Shattuck-Eidens D, Oliphant A, McClure M, et al. BRCA1 sequence analysis in women at high risk for susceptibility mutations: risk factor analysis and implications for genetic testing. JAMA 1997;278: 1242-1250. [PubMed] [Google Scholar]
- 24.Chang-Claude J, Dong J, Schmidt S, et al. Using gene carrier probability to select high-risk families for identifying germline mutations in breast cancer susceptibility genes. J Med Genet 1998;35: 116-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frank TS, Manley SA, Olopade OI, et al. Sequence analysis of BRCA1 and BRCA2: correlation of mutations with family history and ovarian cancer risk. J Clin Oncol 1998;16: 2417-2425. [DOI] [PubMed] [Google Scholar]
- 26.Parmigiani G, Berry D, Aguilar O. Determining carrier probabilities for breast cancer-susceptibility genes BRCA1 and BRCA2. Am J Hum Genet 1998;62: 145-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berry DA, Parmigiani G, Sanchez J, Schildkraut J, Winer E. Probability of carrying a mutation of breast-ovarian cancer gene BRCA1 based on family history. J Natl Cancer Inst 1997;89: 227-238. [DOI] [PubMed] [Google Scholar]
- 28.McKinnon WC, Baty BJ, Bennett RL, et al. Predisposition genetic testing for late-onset disorders in adults: a position paper of the National Society of Genetic Counselors. JAMA 1997;278: 1217-1220. [PubMed] [Google Scholar]
- 29.Geller G, Botkin JR, Green MJ, et al. Genetic testing for susceptibility to adult-onset cancer: the process and content of informed consent. JAMA 1997;277: 1467. [PubMed] [Google Scholar]