A 65-year-old man with a 70-pack-year smoking history presents to your office because he has had dyspnea for 2 years that has worsened in the past 1 to 2 months so that walking to the bathroom results in considerable distress. Despite the albuterol inhaler given to him in the past, he continues to complain that he is “suffocating.” The patient says he has not smoked in the past 5 years. Oxygen saturation with the patient breathing room air is 91%, and after the patient walks, it drops to 86%. On physical examination, he is thin and has difficulty speaking long sentences or laughing. His lungs are hyperresonant to percussion, and he has decreased breath sounds bilaterally. A chest film shows hyperexpanded lung fields, and spirometry shows a forced expiratory volume 1 second (FEV1) of 0.85 L/min (38% of predicted) with a ratio of FEV1 to forced vital capacity (FVC) of 51%. What therapeutic interventions are indicated for this patient to help manage his chronic obstructive pulmonary disease (COPD) and relieve his dyspnea?
SEARCHING AND APPRAISING THE LITERATURE
We searched MEDLINE from 1966 through December 2000, combining the key words obstructive lung disease with dyspnea. The search was limited to human studies and studies in the English language, and it identified 580 articles, which in review led to the identification of 30 more articles. We reviewed these 610 articles initially by title, followed by abstract to determine their relevance for inclusion. Fifty-four articles were used for therapy recommendations and consisted of 27 randomized, double-blind, placebo trials; 5 randomized, single-blind, placebo trials; 5 randomized, double-blind trials; 4 single- or double-blind, placebo trials; 8 randomized-only trials; 3 meta-analyses; 1 case series; and 1 consensus statement.
DYSPNEA, ITS PREVALENCE IN ADVANCED COPD, AND ITS RELATION TO FEV1
Dyspnea is defined as the unpleasant sensation associated with breathing that is commonly found in various disorders including advanced COPD. The mechanisms of dyspnea in COPD are beyond the scope of this review but are covered extensively elsewhere.1-3 The overriding complaint of the 416 dying COPD patients enrolled in the SUPPORT trial was dyspnea, which was twice as common as pain or confusion throughout the entire 6 months of their dying.4-6 A patient's baseline FEV1 has been shown to predict poorly the level of dyspnea.7 The loss of FEV1 does not correlate with changes in dyspnea, as shown in a cohort study of 34 patients with COPD observed for an average of 5 years.8 In addition, the improvement in dyspnea after bronchodilator treatment is not always associated with changes in FEV1.9
WHAT ARE THE PHARMACOLOGIC THERAPIES FOR DYSPNEA IN PATIENTS WITH ADVANCED COPD?
Oxygen
Oxygen therapy is clearly indicated for COPD patients with hypoxemia at rest or with exertion.10,11 Administering oxygen to patients with emphysema augments their exercise capacity and reduces their dyspnea.12 In a study of 9 COPD patients with exercise-induced hypoxemia, supplementary oxygen during exercise reduced dyspnea more than ventilatory requirements. This suggests that preventing hypoxemia plays a role in dyspnea that may go beyond reducing ventilatory requirements.13 The current indications for oxygen do not include dyspnea.14,15 However, dyspneic hospice patients may obtain oxygen therapy without meeting approved guidelines of the Health Care Financing Administration.16 Even in the absence of hypoxemia at rest and with only mild desaturation with exertion, oxygen administration during exercise may relieve dyspnea in patients with COPD.17 The route of administration, either transtracheal or with nasal prongs, may not have an effect on dyspnea, but higher flow rates may improve exercise tolerance.18 It is postulated that oxygen may eliminate signals from the carotid bodies, thereby reducing dyspnea and ventilatory demand. This mechanism would alter a patient' “set point” for the partial pressure of arterial carbon dioxide (PaCO2), which by the alveolar gas equation would result in a lower minute ventilation and work of breathing, thereby relieving dyspnea.
Bronchodilators
Inhaled β-agonist and anticholinergic agents have traditionally been used as bronchodilators in the treatment of dyspnea from COPD. A randomized placebo-controlled trial of the use of albuterol in 13 COPD patients found that this β2-agonist reduced exercise-induced dyspnea and dynamic hyperinflation without necessarily increasing the FEV1 or FVC.19 The authors postulated that the amelioration in dyspnea was due to decreased dynamic hyperinflation. Two other randomized studies looking at the β-agonists salmeterol xinafoate and salbutamol/clenbuterol have shown the efficacy of β-agonists on dyspnea relief in COPD.20,21
A trial of oxitropium bromide, an anticholinergic agent, in 32 patients with COPD showed that the use of this agent improved dyspnea at rest and after exercise, increased 6-minute walking distance, and increased the FEV1.22 Furthermore, the FEV1 changes with bronchodilation did not correlate with improvements in dyspnea or walking distance. The use of this bronchodilator also led to a decrease in dyspnea during exercise in a study of 19 patients with COPD.23 Tiotropium bromide is a newer, once-a-day, potent anticholinergic agent (soon to be available as dry-powder inhaler) recently shown in severely obstructed patients to decrease rescue inhaler requirements and significantly relieve dyspnea and wheezing, with a more than 10% improvement in vital capacity sustained over 3 months.24
Which bronchodilating agent, β-agonist or anticholinergic, is better?
In a randomized, double-blind trial of 261 COPD patients, those given the anticholinergic agent ipratropium bromide showed greater improvements in FEV1 and increased duration of action than those given the β-agonist metaproterenol sulfate.25 In a study of 223 COPD patients, anticholinergic therapy maintained bronchodilating action over 85 days, whereas the effects of the β-agonist diminished during this period.26 In addition, patients had a significantly greater reduction in dyspnea and other quality-of-life scores with the use of the anticholinergic agent. An analysis of data from 7 clinical trials comparing ipratropium with a β-agonist given for at least 90 days found a significantly greater increase in FEV1 with ipratropium; bronchodilation with ipratropium was sustained, whereas the β-agonist effect waned over time with prolonged use.27 A randomized, double-blind study of 534 COPD patients showed that combining an anticholinergic agent with a β-agonist significantly improved the FEV1 beyond that with either agent alone.28
Which delivery system, nebulizer or metered-dose inhaler, is better?
Nebulizers deliver more medicine to the lungs but in a less efficient manner—with a potentially worse side effect profile—than metered-dose inhalers (MDIs).29 The MDIs require less time for administration than nebulizers at a significantly reduced cost.30,31 Jenkins and associates compared inhaled with nebulized salbutamol in 19 out-patients with stable COPD and found no differences in dyspnea, bronchodilation, rescue inhaler use, or walking distance.32 Other investigations have failed to show any benefit of nebulizers over MDIs.33,34 Because of the reduced time and cost with MDIs and the lack of a clear therapeutic advantage with nebulizers, it is prudent to first use bronchodilators by MDIs if the patient's technique is adequate. Near the end of life and during acute exacerbations, patients with advanced disease will often be too weak to use an MDI effectively, in which case nebulized delivery becomes the better option.
Theophylline
Theophylline, a methylxanthine, is commonly prescribed for the treatment of COPD. Mahler and colleagues studied 12 patients with nonreversible COPD given sustained-release theophylline to keep its level between 10 and 20 μg/mL over 4 weeks.35 Theophylline use was associated with a significant improvement in dyspnea versus placebo, without a change in exercise tolerance, lung function, or arterial blood gas values. A dose-ranging study of 14 COPD patients compared 3 one-week periods of placebo versus low-dose theophylline (levels, 10-20 μg/mL) versus high-dose theophylline (levels, 18-20 μg/mL). There were improvements in FEV1 and FVC in the theophylline group compared with those receiving placebo.36 Self-assessment of dyspnea and exercise tolerance improved for both low and high doses of theophylline but did not reach significance. Four patients were unable to complete the high-dose theophylline phase because of side effects. Withdrawal of theophylline from stable COPD patients leads many patients to have a deterioration of symptoms and exercise endurance.37 Theophylline may provide symptomatic improvement for patients with severe COPD, and if used, it should be prescribed once a day to achieve levels of 10 to 12 μg/mL with avoidance of drug interactions.
Oral opioids
Woodcock and colleagues piqued interest in using opioids for the dyspnea of COPD by showing that a 1-time administration of 1 mg/kg of dihydrocodeine improved exercise tolerance and decreased exertional dyspnea.38 Administration of the drug led to reduced oxygen consumption at rest and during exercise, which the authors hypothesized to be the reason for the improvements. A follow-up study then assessed the use of dihydrocodeine, placebo, or alternating-day therapy, each for 1 week, with the same findings.39
Light and co-workers compared oral morphine sulfate, 0.8 mg/kg, versus placebo in 13 patients with COPD.40 Morphine use led to an increase in exercise tolerance. Despite the associated increase in ventilatory requirements with morphine, there was no increase in dyspnea.40 The authors thought the better exercise tolerance was from morphine blunting the central perception of dyspnea and lowering the ventilatory drive for a given PaCO2. This study showed a significant elevation in PaCO2, a fall in PaO2, and drowsiness with morphine. Poole and associates gave patients increasing doses of sustained-release morphine over 6 weeks, with a mean dose achieved of 25 mg per day.41 The intervention had no effect on quality of life, exercise tolerance, dyspnea, or oxygen saturations, with a trend (although not significant) toward more side effects during the morphine phase.
Other studies of the opioids diamorphine and dextromethorphan hydrobromide have failed to show significant benefits.42,43 Rice and colleagues compared codeine and promethazine hydrochloride in a randomized, double-blind, crossover trial.44 The use of codeine had no effect on dyspnea but caused significant elevations in PaCO2 levels.44
Given that opioids may cause serious side effects—such as retention of carbon dioxide, hypoxemia, drowsiness, and nausea—and that the clinical benefit remains unproved, their routine prescription for dyspnea in a patient with COPD cannot be recommended. However, severely dyspneic patients without significant hypoxemia or carbon dioxide retention may benefit from a careful trial of oral morphine or dihydrocodeine with close monitoring. For palliative care of end-stage COPD patients, opioids may be given without hesitancy or fear of legal reprise under the theory of double effect if the purpose is to relieve dyspnea and symptoms and not accelerate death.45
Inhaled opioids
Because of the side effects of systemically delivered opioids, inhaled morphine has been considered for treating dyspnea because opioid peptide activity has been found in bronchial mucosa.46 In a randomized, double-blind, crossover study of inhaled morphine, involving 9 patients with COPD and 2 with idiopathic pulmonary fibrosis, patients showed an improvement in their exercise endurance after morphine inhalation compared with placebo.47 In a subsequent study, increasing doses of aerosolized morphine were given to 8 patients with COPD, but the drug had no significant effect on dyspnea or exercise function compared with placebo.48 In a study of 12 COPD patients given as much as 25 mg of nebulized morphine, there was no improvement in dyspnea or exercise endurance.49 Two other studies also failed to demonstrate any advantage from inhaled morphine.50,51 There is currently no good evidence to support the use of inhaled opioids for relieving the dyspnea of COPD.
Anxiolytic agents and promethazine
Although early work suggested that benzodiazepines may be helpful in relieving the dyspnea of COPD,52 more recent evidence does not support this. Man and coworkers studied alprazolam in 24 patients; taking the drug did not lead to an improvement in baseline or exertional dyspnea, exercise tolerance, or sense of well-being.53 Subjects who took alprazolam had lower PaO2 and higher PaCO2. Woodcock and associates evaluated the use of diazepam (25 mg per day) or promethazine (125 mg per day) for 2 weeks each in a randomized, double-blind study.54 Diazepam caused substantial drowsiness, decreased exercise tolerance, increased PaO2, and no change in dyspnea versus placebo. Promethazine use, however, was associated with an increase in exercise tolerance and decreased dyspnea, and it had no notable side effects. But a follow-up study in which promethazine was given to COPD patients for 1 month found no significant changes from baseline, although only 7 of 11 patients completed the study.44 Based on the findings of these small investigations, benzodiazepines do not appear to have a role in treating dyspnea in COPD; however, promethazine may have a beneficial effect.
Buspirone hydrochloride is a nonsedating, nonaddictive anxiolytic agent that has received attention in dyspnea therapy for COPD. In a randomized trial of 16 patients, those taking buspirone, 20 mg a day for 15 days, showed an improvement in anxiety and depressive scores, exercise performance, and dyspnea during exercise without alterations in respiratory drive or arterial blood gas values.55 However, in another small randomized trial of 11 patients, treatment with buspirone at a dose of at least 30 mg per day for 6 weeks had no effect on anxiety scores, exercise tolerance, or dyspnea indices compared with placebo.56 The authors hypothesized that the lack of treatment response may have been due to participants having only mild anxiety scores at study entry and recommended a trial of buspirone in patients with moderate to severe anxiety and COPD.
Antidepressant drugs
Patients with COPD have a high prevalence of psychiatric illnesses—estimates are that about 58% of patients have a psychiatric problem, 16% have a depressive disorder, and 34% have an anxiety disorder.57 But few studies have investigated whether treatment of the psychiatric illnesses, with antidepressants or other psychotropic medications, affects the dyspnea. Studies to date have involved small numbers of patients, and they have had conflicting results.58-60
WHAT ABOUT NONPHARMACOLOGIC INTERVENTIONS?
Pulmonary rehabilitation and inspiratory muscle training
Ries and co-workers in a randomized controlled trial and a meta-analysis showed that pulmonary rehabilitation can lessen dyspnea.61,62 Pulmonary rehabilitation has been more recently confirmed to reduce dyspnea and COPD exacerbations, improve quality of life, and extend exercise capacity for patients with COPD.63,64 Programs that involve only education and not structured exercise training likely are not effective.65 Another study found that patients who have severe dyspnea may not profit from exercise training as much as those with moderate dyspnea.66 A limitation of this study, however, was that severely dyspneic patients received home training and possibly were less compliant than patients with moderate dyspnea who received rehabilitation in a hospital or outpatient setting. The addition of domiciliary noninvasive positive pressure ventilation to an exercise training program has been shown to improve exercise tolerance and quality of life over exercise training alone.67 Inspiratory muscle training may also lessen dyspnea. Harver and colleagues found that an inspiratory resistance breathing device used daily led to improved muscle strength and reduced dyspnea in patients with COPD.68
Weiner and co-workers further showed that inspiratory muscle training improved the perception of dyspnea.69 This is in contrast to a meta-analysis that concluded that respiratory muscle training did not benefit COPD patients.70 Berry and associates found no additional benefits from inspiratory muscle training over general exercise reconditioning alone.71 The benefits of inspiratory muscle training, therefore, remain controversial.
Lung-volume reduction surgery
Surgical approaches such as lung-volume reduction surgery may improve dyspnea in patients with COPD and should be considered in those who qualify based on current recommendations.72 However, it is still unclear if this invasive and highly costly procedure is effective long-term therapy, especially for patients with end-stage disease; as such, further judgment should be delayed until the results of the ongoing multicenter National Emphysema Therapy Trial become available.
After giving your patient the influenza and pneumococcal vaccinations, you arrange for home oxygen to be given (2 liters) for exertion and at night. You also decide to start a regimen of ipratropium bromide, 2 to 4 puffs 4 times a day, and albuterol inhaler, 2 to 4 puffs 4 times a day (combination therapy with Combivent would be another consideration). Salmeterol would be an important adjunctive therapy, either initially or in the near future, depending on the clinical course and other patient-specific factors. The patient does not meet criteria for depression, so prescribing an antidepressant drug is not indicated. However, on further discussion, he relates a significant anxiety component with possible panic attacks associated with his more severe dyspneic episodes. For this, you prescribe a starting dose of buspirone, 7.5 mg twice a day, to be titrated over the next several weeks to 30 mg a day. In addition, you refer the patient to a local pulmonary rehabilitation center for exercise training. You agree to give these initial therapies a trial before contemplating either theophylline and/or a careful trial of an oral opioid if his dyspnea becomes more severe and refractory to other interventions.
Table 1.
| Resources |
|---|
| • Breathe Easy: A Guide to Living With Lung Disease (www.lung.ca/copd/index2.html) |
| This guide from The Canadian Lung Association provides knowledge about how to help people living with chronic lung disease. It includes advice about sexuality, exercise, stress management, medications, and use of respiratory devices. |
| • Chronic Obstructive Pulmonary Disease (www.nhlbi.nih.gov/health/public/lung/other/copd) |
| This online publication from the National Institutes of Health includes diagrams of the airways with comprehensive descriptions of signs and symptoms of COPD, its detection, and its treatment. Special attention is given to ways patients and their families can cope with this illness and what clinical research efforts are under way to understand the causes of COPD, improve treatment, and manage the disease. |
| • American Lung Association Factsheet (www.lungusa.org/diseases/copd_factsheet.html) |
| A concise list of facts covering the epidemiology, pathogenesis, and treatment of COPD. |
| • Courage and Information for Life with Chronic Obstructive Pulmonary Disease: The handbook for patients, families, and care givers managing COPD (emphysema, asthmatic bronchitis, or chronic bronchitis). Carter R, Nicotra B, Tucker JV, eds. Onset, MA: New Technology Publishing Inc, October 1999. Extracts available at www.healthyresources.com/copd/courage. |
| This book was coauthored by a pulmonary physician, an exercise physiologist, and a patient with COPD. It is a practical, easy-to-read resource for patients and physicians. |
Summary points
Oxygen is indicated for all patients with chronic obstructive pulmonary disease (COPD) who have hypoxemia either at rest or during exercise. Hospice patients with dyspnea may receive oxygen without meeting criteria of the Health Care Financing Administration
Bronchodilators should be tried in all patients with COPD. Patients with profound dyspnea benefit greatly from anticholinergic inhalers (ipratropium bromide or tiotropium) and longer acting β-agonists (salmeterol xinofoate)
Theophylline as once-a-day therapy may be useful in a small percentage of patients
Oral opioids are not indicated for routine use in patients with COPD but have a role in severely dyspneic patients with advanced disease. The current literature suggests that inhaled opioids are not effective for COPD
Benzodiazepines are not effective in the relief of dyspnea in patients with COPD
Pulmonary rehabilitation has proven efficacy for dyspnea relief in COPD, although the role of lung-volume reduction surgery is highly patient-dependent and remains under investigation
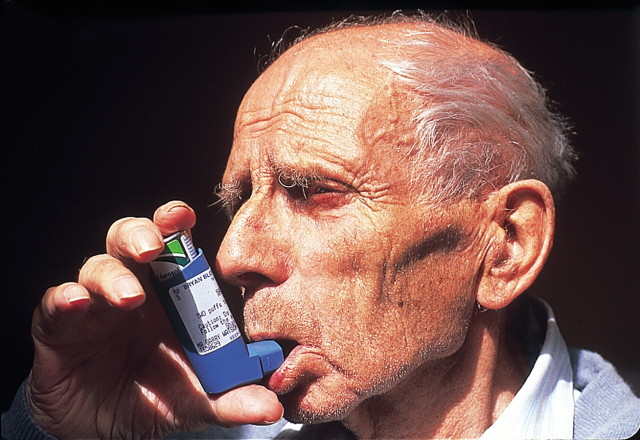
Figure 1.
Drug delivery through metered-dose inhalers can be effective if the patient's technique is adequate
Gary Watson/SPL
Funding: This work was supported in part by an AFAR Pharmacology in Aging grant and the Paul Beeson Faculty Scholar Award from the Alliance for Aging Research (Ely), grant AG01023-01A1 from the National Institutes of Health, Bethesda, MD (Ely); and by the Geriatric Research and Education Clinical Center (Ely)
Competing interests: None declared