Abstract
Skipping breakfast is one of the most prevalent irregular eating habits. Several pieces of evidence have reported the association between breakfast omission and a higher risk of cardiovascular diseases. Numerous publications have focused on the impact of skipping breakfast on various cardiovascular risk factors. Therefore, the current systematic review and meta-analysis aimed to assess this impact, especially with regard to anthropometric measurements, serum lipid profiles, blood pressure, and glycemic control indicators. A comprehensive search was performed in PubMed, Web of Science, Embase, Scopus, and the Cochrane Central Register of Controlled Trials up to 1 April 2023. A total of 11 eligible trials were identified to evaluate the combined effects of skipping breakfast. Final integrated results demonstrated that breakfast omission significantly decreased the body weight (mean difference = −0.66, 95% CI: −1.09 to −0.24, p = 0.002, I2 = 0.0) and increased the level of serum low-density lipoprotein cholesterol (LDL-C) (mean difference = 9.89, 95% CI: 5.14 to 14.63, p = 0.000, I2 = 17.3). Subgroup analysis also revealed potential factors that may affect the outcomes, for example, the physiological condition of participants, duration, gender, and type of breakfast. In conclusion, skipping breakfast may reduce body weight while increasing the level of serum LDL-C at the same time. In view of the limited trials, further studies are needed to expound the role of breakfast omission in cardiovascular diseases.
Keywords: anthropometrics, blood pressure, cardiovascular risk factors, glycemic control, lipid profiles, meta-analysis, skipping breakfast, systematic review
1. Introduction
Breakfast is generally considered as the first meal before ten o’clock in the morning. Skipping breakfast is defined as the omission of any food except water (1). For a long time, it has been widely accepted that breakfast holds significant importance as the first meal of the day, playing a crucial role in health behaviors, although its exact mechanism remains unclear (2). Human diets have changed drastically over the past few decades due to the transformation of lifestyles. According to a nationally representative survey in Canada, 11% of adults never took breakfast (3). Similarly, data from National Health and Nutrition Examination Survey (NHANES) 1999–2014 reported that more than one in five US adults skipped breakfast. The consumption of breakfast had a dismal situation (4–6).
According to the data from the American Heart Association (AHA), more than 26 million adults in the United States suffer from cardiovascular diseases (CVDs), excluding hypertension (7). In 2018, cardiovascular disease accounted for approximately one-third of all U.S. deaths, becoming a huge burden on human health and society (8, 9). These situations are not just confined to the US as cardiovascular diseases have long been a leading cause of death globally (10). Predictions for 2025 and 2060 suggest a substantial increase in the prevalence of cardiovascular diseases (11). It was reported that a potential risk factor for cardiovascular disease is irregular or inconsistent diet, for example, skipping breakfast. Results from a British birth cohort indicated that irregular diet positively associated with cardiometabolic risk (12). A national representative prospective cohort study demonstrated a significant increase in the risk of mortality from cardiovascular disease associated with skipping breakfast (13). Several studies have reached the same conclusion (14–17). However, skipping breakfast was also considered as an intermittent fasting strategy that may benefit the development of cardiovascular disease in specific situations. When considering the chrononutrition nutritional physiology, taking breakfast was related to the endocrine pancreatic clock and insulin secretion, which ultimately enhance the metabolic pathways related to cardiovascular diseases (18). In addition, many disease states including obesity, raised blood cholesterol, and raised blood pressure are regarded as risk factors for cardiovascular diseases. Nevertheless, few studies have elaborated on the effect of skipping breakfast on them, making it necessary to conduct this systematic review and meta-analysis to clarify it.
2. Method
2.1. Search strategy and eligibility criteria
A comprehensive systematic search was conducted in PubMed, Web of Science, Embase, Scopus, and the Cochrane Central Register of Controlled Trials from database inception to 1 April 2023. Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) Guideline was followed to evaluate the effect of skipping breakfast on cardiovascular risk factors (19). The method of subject words combined with free words was adopted to perform a retrieval scheme. These search terms were used to identify the relevant literature: (“breakfast” OR “morning meal” OR “skip breakfast” OR “skipping breakfast” OR “breakfast omission” OR “omit breakfast” OR “fasting”) AND (“cardiovascular disease” OR “cardiovascular disease risk factors” OR “weight” OR “body mass index (BMI)” OR “waist circumference” OR “waist-to-hip ratio (waist:hip ratio)” OR “lipid profiles” OR “high-density lipoprotein cholesterol (HDL-C)” OR “low-density lipoprotein cholesterol (LDL-C)” OR “total cholesterol (TC)” OR “total triglyceride (TG)” OR “diastolic blood pressure (DBP)” OR “systolic blood pressure (SBP)” OR “glucose” OR “blood glucose” OR “blood sugar” OR “fasting blood sugar (FBS)” OR “fasting plasma glucose (FPG)” OR “fasting blood glucose (FBG)” OR “glycated hemoglobin (HbA1c)” OR “insulin resistance index (HOMA-IR)”). Overall, these indicators can be divided into four classes: anthropometrics, serum lipid profiles, blood pressure, and glycemic control indicator. No limitations were set for the limited relevant trials. Literature would be included if they fulfill the following inclusion criteria (1): Randomized controlled trials or prospective cohort studies (2). Trials aiming to probe the effect of skipping breakfast on the factors mentioned above (3). Participants of the intervention group must finish breakfast before 10:00, without limitations on the type or the features of breakfast (4). Participants of the control group consume nothing but water. The exclusion criteria were as follows (1): Case reports, observational studies, and retrospective studies (2). Participants with special pathological conditions (for example, fasting because of surgery) (3). Trials including pharmacological or dietary supplement interventions. Literature search was performed by two reviewers (J.Y. and J.X.) independently. To ensure the rigor of the retrieval strategy, we also hand-searched and checked the reference lists of included articles and relevant reviews. Any disagreement in this progress has been discussed and resolved.
2.2. Data extraction and quality assessment
Two authors (J.Y. and Y.L.) collected the characteristics of 11 included trials independently including (a) name of the first author, year of publication, and study region; (b) sample size, number of male and female participants, mean age of participants, study design, and duration; and (c) health status of participants, intervention details, and outcomes of interest. A third reviewer (D.X. or Y.W.) checked the extracted data in case of any errors. Cochrane Risk of Bias 2.0 tool (RoB2) was conducted to assess the risk of bias in RCTs including four domains: bias due to the randomization process, deviations from intended interventions, missing outcome data, and selection of the reported results (20). Meanwhile, GRADE was adopted to evaluate the evidence level of RCTs while the Newcastle–Ottawa Scale (NOS) was used for cohort studies. Quality was rated as high, medium, low, and very low according to the risk of bias, inconsistency, indirectness, imprecision, and publication bias (21). Publication bias was assessed via Egger’s tests and funnel plots, and trim and fill methods for any asymmetry if it exists (22). If there existed multiple intervention groups in the trials, the breakfast and no-breakfast groups were combined to explore the effect of skipping breakfast on the indicators mentioned above.
2.3. Data integration and quantitative analysis
The data of interest were presented in the form of mean and standard error or 95% confidence intervals (CIs). For data only in graphs or figures, we contacted the original authors if possible. For parallel-controlled trials, mean difference (MD) was calculated by the change from baseline in both control and intervention groups. Moreover, the value of the last endpoint was selected to analyze if there was more than one endpoint while the final level of cardiovascular risk factors was extracted to compute the MD in crossover trials. The following formula was used if the net change of SD is not provided:
based on a correlation coefficient R = 0.5 (23). Units of the following indicators were harmonized as mg/dL including serum lipid profiles and fasting glucose. I2 and chi-squared statistics were adopted as a measure of heterogeneity, only I2< 50% and p-value > 0.05 were considered as no statistical heterogeneity. Based on the heterogeneity test, either a random‐ or fixed‐effect model was chosen for pooled results. The method of leave-one-out sensitivity analysis was used to identify the heterogeneity, and so was subgroup analysis. Leave-one-out sensitivity analysis performs multiple meta-analyses by excluding one study at each analysis to determine the impact and effect of individual studies or data in the context of overall data (24). All of the statistical analyses above were conducted via Stata version 15 software (STATA Corp, College Station, TX, USA).
3. Results
3.1. Literature search
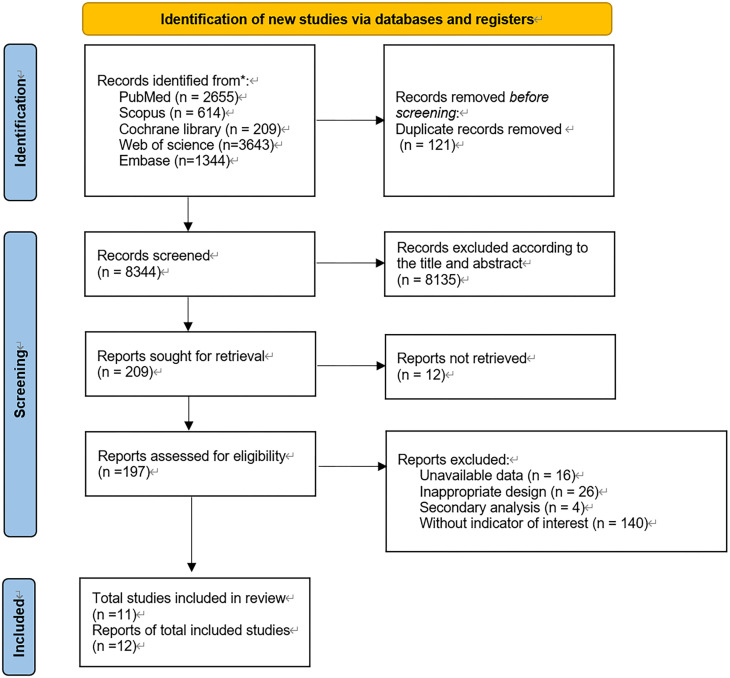
The detailed screening methodology is presented in Figure 1. A total of 8,465 pieces of literature were identified initially by the search strategy. Duplicate records were removed, resulting in 8,344 remaining articles. After browsing the title and abstract, 209 articles were selected for further intensive reading. Final screening led to 11 pieces of literature included in the current systematic review and meta-analysis.
Figure 1.
Flowchart.
3.2. Characteristics of the trials
The 11 studies evaluating the effect of skipping breakfast on cardiovascular risk factors were included in this systematic review, namely, 9 RCTs, 1 randomized crossover trial, and 1 cohort study (25–35). The publication year of trials ranged from 1992 to 2019. In total, 1,118 participants aged from 11 to 55 were allocated to the breakfast group or breakfast skipping group. Most of the participants were healthy individuals, and only 4 trials were conducted among patients with overweight, obesity, or metabolic syndrome. Study duration ranged from 2 days to 10 years, and the majority of the trials (n = 10) had an intervention duration of more than 4 weeks. The detailed summary is shown in Table 1.
Table 1.
Characteristics of included studies.
| Author, year | Country | Size, n | Male/female, n | Mean age (years) | Ault or minor | Study design | Duration | Health status of participants | Intervention group | Control group | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Geliebter 2014 | USA | 36 | 18/18 | 33.4 ± 6.5 | Adult | Randomized, controlled parallel-arm | 1 month | Healthy | Consumption of oat porridge, frosted cornflakes within 15 min at 8:30 | Breakfast skipping | Weight; waist; waist:hip ratio; SBP; DBP; HDL-C; LDL-C; TC; TG; fasting glucose; HOMA-IR |
| Neumann 2016 | USA | 24 | 0/24 | 24.1 ± 2 | Adult | Randomized, controlled | 8 days | Healthy | Consumption of protein-based breakfast or carbohydrate-based breakfast | Breakfast skipping | Weight; BMI |
| Goff 2019 | UK | 665 | 329/336 | 22.7 | Minor and adult | Cohort | 10 years | Healthy | Consumption of regular breakfast | Breakfast skipping | BMI; waist:hip ratio; SBP; HDL-C; TC; HbA1c |
| Kobayashi 2013 | Japan | 8 | 8/0 | 25.3 ± 1.2 | Adult | Randomized, crossover | 2 days | Healthy | Consumption of meals at predetermined time: breakfast (8:00), lunch (12:00), and supper (19:00) | Breakfast skipping, lunch (12:00), and supper (19:00) | Fasting glucose |
| Zhang 2017 | USA | 178 | 48/130 | 52.2 | Adult | Randomized, controlled | 1 year | Metabolic syndrome | Consumption of regular breakfast | Breakfast skipping | Weight; BMI; waist; SBP; DBP; HDL-C; LDL-C; TC; TG; HbA1c; fasting glucose; HOMA-IR |
| Schlundt 1992 | USA | 38 | 0/38 | 18–55 | Adult | Randomized | 3 months | Obesity | Consumption of breakfast (1,672 kJ), lunch (1,254 kJ), and supper (2,090 kJ) | Consumption of lunch (1,254 kJ) and supper (2,090 kJ) without breakfast | Weight |
| Leidy 2015 | USA | 54 | 22/32 | 19 ± 1 | Adult | Randomized, controlled | 3 months | Overweight, obesity | Consumption of 1,464 kJ breakfast (13 g protein) or a high-protein breakfast (35 g protein) | Breakfast skipping | Weight, BMI |
| LeCheminant 2016 | USA | 49 | 0/49 | 23.7 ± 6.8 | Adult | Randomized, controlled | 1 month | Healthy | Consumption of at least 15% of daily energy requirement before 8:30 | Without consuming any energy until 11:30 | Weight, BMI |
| Chowdhury 2016 | UK | 23 | 8/15 | 44 ± 10 | Adult | Randomized, controlled | 6 weeks | Obesity | Consumption of daily breakfast (at least 700 kcal) | Extended fasting (0 kcal until 12:00) | Weight; BMI; waist; waist:hip ratio; HDL-C; LDL-C; TC; TG; fasting glucose; HOMA-IR |
| Betts 2014 | UK | 33 | 12/21 | 36 ± 11 | Adult | Randomized, controlled | 6 weeks | Healthy | Consumption of daily breakfast (at least 700 kcal) | Extended fasting (0 kcal until 12:00) | Weight; BMI; waist; waist:hip ratio; SBP; DBP; HDL-C; LDL-C; TC; TG; fasting glucose; HOMA-IR |
| Farshchi 2005 | UK | 10 | 0/10 | 25.5 ± 5.7 | Adult | Randomized, crossover | 1 month | Healthy | Consumption breakfast cereal with 2% fat milk before 8:00 | Breakfast skipping | Weight; BMI; waist; waist:hip ratio; HDL-C; LDL-C; TC; TG; fasting glucose |
3.3. Risk of bias and grading of the evidence
Full details of the risk of bias and grading of the evidence are shown in Supplementary Appendix. Among 11 trials included in this systematic review, five RCTs were rated for high risk of the lack of blinding in the randomization process, deviations from the intended interventions, and missing outcome data. Meanwhile, due to the inconsistency and imprecision of the outcome variables, most of the evidence was graded as low or moderate. Publication bias was also presented in Supplementary Appendix.
3.4. Effect of skipping breakfast on cardiovascular risk factors
3.4.1. Anthropometrics
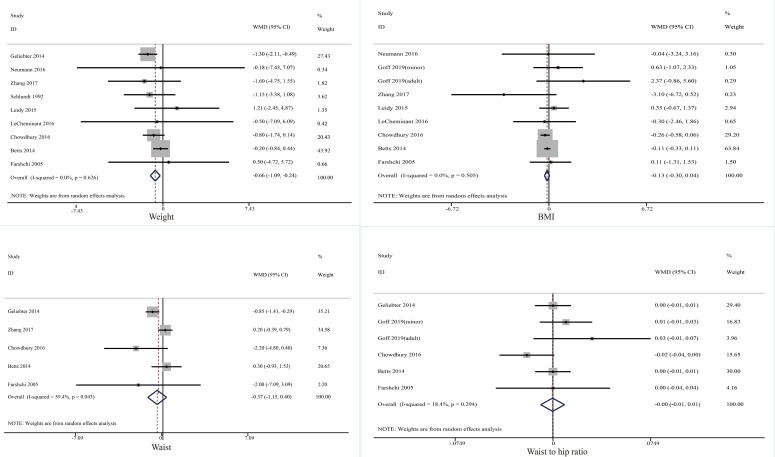
Ten trials investigated the effect of skipping breakfast on anthropometrics (Figure 2). Compared to taking breakfast, skipping breakfast could reduce weight significantly (mean difference = −0.66, 95% CI: −1.09 to −0.24, p = 0.002, I2 = 0.0). No significant changes were observed in other indicators: BMI: mean difference = −0.13, 95% CI: −0.30 to 0.04, p = 0.144, I2 = 0.0; Waist circumference: mean difference = −0.37, 95% CI: −1.15 to 0.40, p = 0.344, I2 = 59.4; waist-to-hip ratio: mean difference = 0.00, 95% CI: −0.01 to 0.01, p = 0.344, I2 = 59.4.
Figure 2.
Effect of skipping breakfast on anthropometrics.
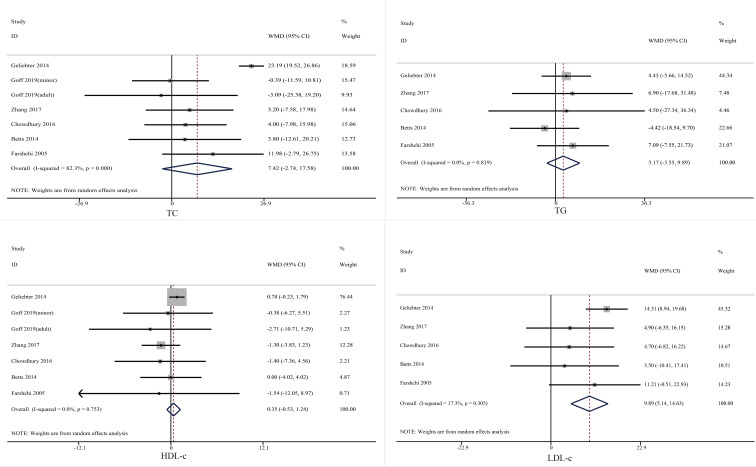
3.4.2. Serum lipid profiles
Six trials probed the effect of skipping breakfast on serum lipid profiles (Figure 3). The merged data indicated that skipping breakfast did cause a significant increase in serum LDL-C (mean difference = 9.89, 95% CI: 5.14 to 14.63, p = 0.000, I2 = 17.3). No statistical significance was observed in the remaining indicators: serum TC: mean difference = 7.42, 95% CI: −2.74 to 17.58, p = 0.152, I2 = 41.0; serum TG: mean difference = 3.17, 95% CI: −3.55 to 9.89, p = 0.355, I2 = 0.0; serum HDL-C: mean difference = 0.35, 95% CI: −0.53 to 1.24, p = 0.435, I2 = 0.0.
Figure 3.
Effect of skipping breakfast on serum lipid profiles.
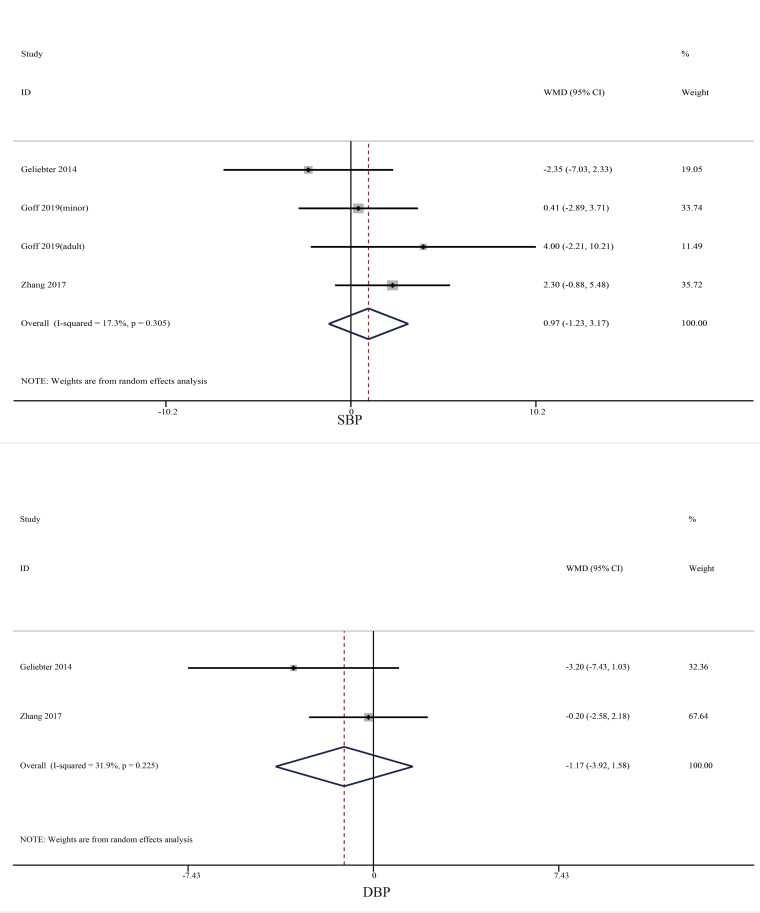
3.4.2.1. Blood pressure
Four studies focused on the effect of skipping breakfast on blood pressure (Figure 4). No significant changes were reported either among SBP (mean difference = 0.97, 95% CI: −1.23 to 3.17, p = 0.386, I2 = 17.3) or DBP (mean difference = −1.17, 95% CI: −3.92 to 1.58, p = 0.404, I2 = 31.9).
Figure 4.
Effect of skipping breakfast on blood pressure.
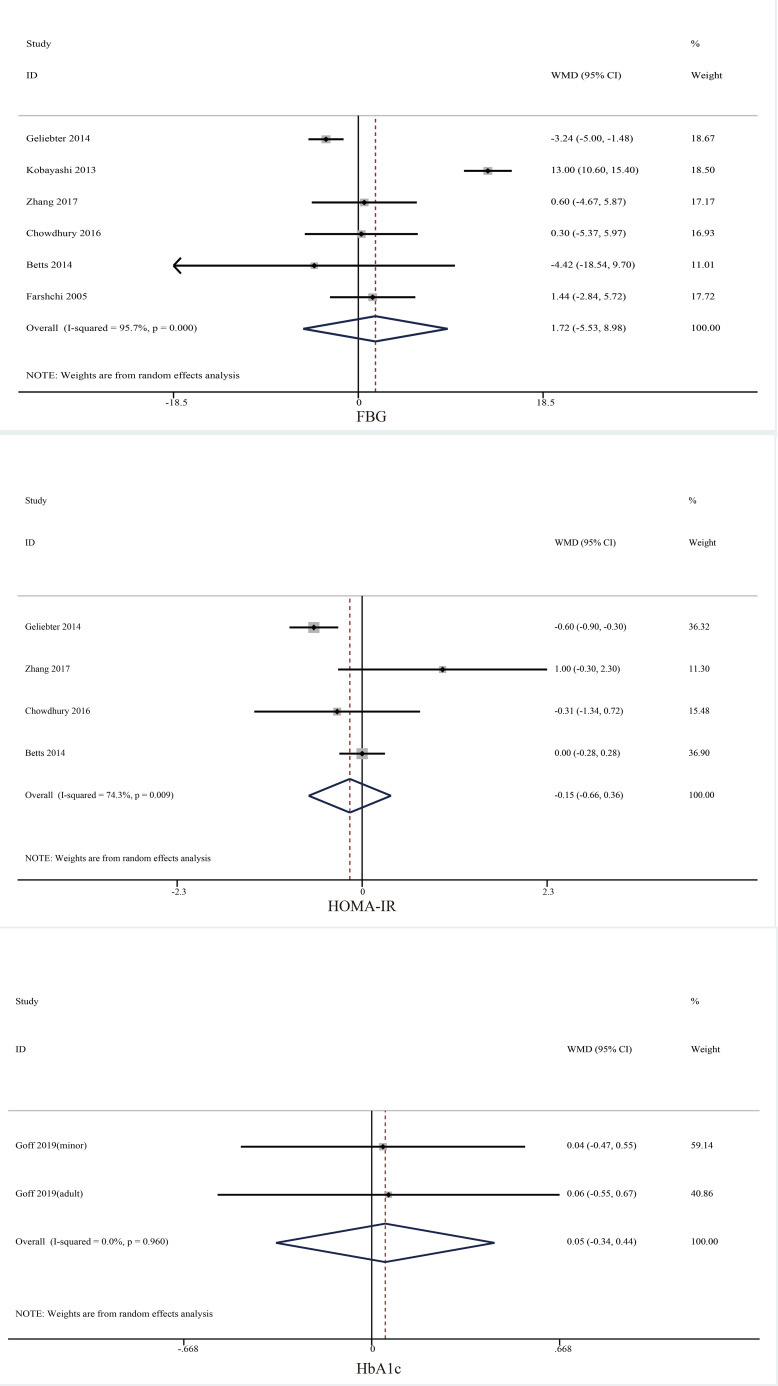
3.4.2.2. Glycemic control indicators
Seven trials reported the effect of skipping breakfast on glycemic control indicators (Figure 5). However, no significant changes were found in FBG (mean difference = 0.00, 95% CI: −0.05 to 0.05, p = 0.642, I2 = 97.2), HbA1c (mean difference = 0.05, 95% CI: −0.34 to 0.44, p = 0.808, I2 = 96.0), and HOMA-IR (mean difference = −0.15, 95% CI: −0.66 to 0.36, p = 0.558, I2 = 74.3).
Figure 5.
Effect of skipping breakfast on glycemic control indicators.
3.4.2.3. Subgroup analysis
Subgroup analysis was performed based on the physiological condition of the participants, duration of the trials, gender, intervention of the control groups, and the design of the studies. Very little literatures focusing on DBP and HbA1c led to the failure of their subgroup analysis. A series of subgroup analyses elucidated that participants with overweight/obesity or metabolic syndrome (mean difference = −0.80, 95% CI: −1.62 to −0.24, p = 0.054, I2 = 0.0) tend to lose more weight compared with healthy individuals (mean difference = −0.64, 95% CI: −1.26 to −0.03, p = 0.410, I2 = 11.9). Moreover, the level of serum LDL-C among healthy people (mean difference = 12.50, 95% CI: 7.63 to 17.73, p = 0.000, I2 = 4.2) was higher than that of other participants (mean difference = 4.80, 95% CI: −3.24 to 12.85, p = 0.242, I2 = 0.0). Outcome measures, especially weight, waist circumference, serum LDL-C, and TC, were affected by the treatment duration (weight: ≤4 weeks, mean difference = −1.23, 95% CI: −2.02 to −0.44, p = 0.002, I2 = 0.0; >4 weeks, mean difference = −0.43, 95% CI: −0.93 to 0.07, p = 0.094, I2 = 0.0; waist circumference: ≤4 weeks, mean difference = −0.86, 95% CI: −1.42 to 0.37, p = 0.258, I2 = 34.3; >4 weeks, mean difference = 0.00, 95% CI: −0.87 to 0.87, p = 0.995, I2 = 37.6; serum LDL-C: ≤4 weeks, mean difference = 13.77, 95% CI: 8.89 to 18.66, p = 0.000, I2 = 0.0; >4 weeks, mean difference = 4.48, 95% CI: −2.49 to 11.44, p = 0.208, I2 = 0.0; serum TC: ≤4 weeks, mean difference = 19.96, 95% CI: 10.01 to 29.91, p = 0.000, I2 = 52.0; >4 weeks, mean difference = 2.41, 95% CI: −3.70 to 8.52, p = 0.440, I2 = 0.0). Gender and type of breakfast also had their role in subgroup analysis. More details of subgroup analysis are presented in Supplementary Appendix.
4. Discussion
This meta-analysis, involving 11 trials, summarized the effects of skipping breakfast on cardiovascular risk factors, including anthropometrics, serum lipid profiles, blood pressure, and glycemic control indicators. It conclusively demonstrated that skipping breakfast can lead to weight reduction and elevated levels of serum LDL-C. However, there was no conclusive evidence to certify the relationship between breakfast skipping and other cardiovascular risk factors. Breakfast skippers tend to lose 0.66 kg weight than those who took breakfast. Compared to having breakfast, breakfast skipping reduced the level of serum LDL-C by 9.89 mg/dL. The overall results of this meta-analysis were similar to previous articles (17, 36). Subgroup analysis based on literature characteristics provided more findings.
Several meta-analyses, focusing on RCTs and cohort studies, have consistently reached the conclusion that skipping breakfast may lead to weight reduction in both adults and minors (37, 38). Moreover, observational studies have reported that breakfast acts as a protective factor against overweight or obesity, and this effect is particularly pronounced among male participants (39). The primary mechanism behind this effect is believed to involve hormones that regulate appetite and energy balance, specifically leptin and ghrelin (40). Chowdhury and Betts et al. (26, 27) reported that skipping breakfast may decrease the level of leptin while another trial only observed a decreasing tendency of leptin in the fasting group than those who took breakfast. Fasting, especially short-term fasting, was reported to have the capacity to reduce the level of leptin (41, 42). Notably, a low level of leptin was associated with weight loss, which may partly explain the effect of skipping breakfast in reducing body mass (43, 44). Similar to leptin, ghrelin also has its role in controlling weight. Both leptin and ghrelin engage in energy balance through the hypothalamus and finally contribute to weight loss and leptin has a stronger effect (45–47). Furthermore, leptin is involved in the regulation of signal pathways related to obesity, for example, inflammation and endoplasmic reticulum stress (48–50). Ghrelin also joins the feeding behavior by regulating the responsiveness over satiety signals (51). Although breakfast omission may decrease satiety and result in a daily reduction in energy intake, this effect is prone to be transient. The debate regarding whether energy intake or energy expenditure takes precedence in weight regulation when skipping breakfast remains controversial (52, 53). It should be noted that hormones mentioned above refer to serum leptin and serum ghrelin rather than circulating leptin and ghrelin.
Interestingly, both the duration and the health states of participants revealed different effects on the final pooled results. A recent meta-analysis specifically considered trials lasting more than 4 weeks for data analysis, as there might be a positive correlation between significant weight loss in 1 month and greater weight loss over the long term (17, 54, 55). We acknowledged and considered diverse perspectives on this matter. Our subgroup analysis suggested that skipping breakfast within 1 month may cause more weight loss. Most of the literature focusing on breakfast or skipping breakfast has explored the short-term effects, typically with a duration of less than 4 weeks (56–59). The distinction between short- and long-term effects is not clearly defined. As discussed above, skipping breakfast can lead to short-term weight loss due to hormonal effects, and the majority of trials were conducted within 24 hours, 3 days, or 1 week. It is plausible that short-term omission of breakfast has a stronger impact on weight loss.
Reeves et al. (60) reported that healthy and overweight participants tend to differ in their patterns of energy intake consumption. The breakfast group showed a higher energy intake compared to the no-breakfast group. Notably, participants in the breakfast-skipping group consumed more energy in the afternoon than those who had breakfast, suggesting variable effects among individuals with different BMIs (normal weight, overweight, and obesity). Upon dividing all participants into two groups, we observed that individuals with a healthy weight lost less weight than those classified as having an unhealthy weight. The study demonstrated that neither prolonged morning fasting nor increased afternoon appetite was associated with compensatory intake during ad libitum lunch in obese adults. Interestingly, it appeared that obese individuals were suppressed by ghrelin, regardless of the duration of the overnight fast, which was contrary to common expectations (56). Breakfast skipping did not seem to significantly affect appetite, implying no extra energy intake due to the absence of breakfast. Consequently, the daily energy intake and meal frequency of the breakfast-skipping group were less than those of the breakfast group. Paoli et al. (61) categorized breakfast omission as a form of fasting, potentially explaining the results mentioned earlier. The most recent review indicated that fasting had different effects on weight loss among normal-weight, overweight, and obese individuals, although those of normal weight lost a higher percentage of weight. This may be attributable to the large weight base of the obese since this is a simple mathematical phenomenon of absolute value and percentage. We reached this possible reason with trepidation because of few relevant literature. Whether male or female participants have a better weight loss effect is still unclear because of inconsistent conclusions (62–64). We tried to stratify the analysis by gender but failed, and most of the studies were conducted in both male and female participants. Gender difference is open to debate.
LDL-C is widely considered a significant risk and predictive factor for cardiovascular diseases (65, 66). The pooled results demonstrated that skipping breakfast could lead to elevated levels of serum LDL-C, aligning with findings from several previous studies (28, 67, 68). Physical inactivity and an inadequate diet have been associated with increased components of metabolic syndrome. Unhealthy practices like skipping breakfast are linked to a rise in serum LDL-C levels (69). Both short- and long-term studies have shown that omitting breakfast is associated with increased serum LDL-C levels (28, 70). Moreover, when considering duration (4 weeks) as a stratification factor, the results suggested a more pronounced tendency of elevated serum LDL-C levels when breakfast was omitted within 4 weeks compared to durations exceeding 4 weeks. Although subgroup analysis for durations exceeding 4 weeks showed no significance, observational studies reported opposing results, which warrant further investigation (25, 71).
Several publications have explored the relationship between skipping breakfast and serum TC, primarily focusing on adolescents (72–74). However, only one study from Korea reported a significantly higher level of serum TC in adults who skipped breakfast (75). It appears that the short-term effect of breakfast on serum TC may not be strongly supported due to a lack of sufficient research literature. Shifting the focus to blood pressure, cross-sectional observational studies have indicated elevated blood pressure among female breakfast skippers, attributed to glucocorticoids and cortisol rhythm (76). As for adolescents, skipping breakfast may be a predictive factor for elevated blood pressure (77).
In addition, the absence of daily breakfast was associated with potential glycemic disorders, which resulted in elevated HbA1c and higher fasting plasma glucose from observational studies (78). Abnormal blood glucose rhythms and energy metabolism were also caused by this, including diurnal variation in blood glucose. In the potential sequence caused by skipping breakfast, glucose homeostasis may occur before energy balance (29, 79). Glucose status was improved if breakfast was added among those who habitually skip breakfast, including FBG and HOMA-IR (80, 81).
We sought to discover the effect of skipping breakfast on other cardiovascular risk factors (for example, LDL-C) with this meta-analysis, although the results were not statistically different. From an eating time perspective, breakfast skipping is similar to the strategy of delayed time-restricted feeding (dTRE). Compared to simply skipping breakfast, dTRE restricts feeding to at least after 10 a.m. until 8 a.m. the next day without energy restriction; in other words, this strategy skips breakfast (82). The latest meta-analysis indicated the benefits of dTRE on metabolic health since it increases the insulin sensitivity, lowers blood pressure, and reduces oxidative stress (83). Low-energy and high-energy dTRE reported different effects on lipid metabolism, glucose metabolism, and chronobiology, which involves hormone, gene, and protein expression levels (18). Considering that the included literature more closely resembles a regular diet that omits breakfast, maybe changes in energy are more likely to cause statistically significant changes in other cardiovascular risk factors (84–86). Due to the lack of direct evidence, this conjecture was derived indirectly.
In general, the contemporary dietary pattern is becoming increasingly diverse, emphasizing the need for vigilance regarding unhealthy eating behaviors or habits, such as skipping breakfast. Recent research has revealed a multitude of health outcomes and effects associated with breakfast consumption or omission. Furthermore, scholarly attention has been drawn to determining the healthier and more balanced breakfast options, highlighting the significance of considering aspects like the proportion of carbohydrates and proteins, as well as their respective sources (58, 87–92).
This current systematic review has several strengths and limitations. This is a comprehensive meta-analysis focusing on the effect of skipping breakfast on cardiovascular risk factors. For the first time, we noticed that gender differences, health status, and duration may affect the pooled results. Possible causes and mechanisms of pooled results were presented. Subject to the number of relevant literature and low to moderate level of evidence, more high-quality and large-sample studies are needed to verify or expand our findings.
5. Conclusion
Skipping breakfast may lead to weight loss and elevated levels of serum LDL-C. While it might be an alternative way to lose weight, it is a bad idea because of its negative effects on some cardiovascular risk factors.
Author contributions
GS: Funding acquisition, Supervision, Validation, Writing – review & editing. JY: Conceptualization, Data curation, Formal Analysis, Methodology, Writing – original draft. JX: Conceptualization, Data curation, Writing – review & editing. DX: Investigation, Methodology, Software, Supervision, Writing – review & editing. YW: Formal Analysis, Project administration, Writing – review & editing. SY: Data curation, Formal Analysis, Resources, Investigation, Software, Writing – review & editing. YL: Project administration, Supervision, Validation, Conceptualization, Investigation, Writing – review & editing. HX: Visualization, Writing – review & editing. SW: Methodology, Project administration, Resources, Visualization, Writing – review & editing.
Acknowledgments
The authors sincerely thank all the contributions to this article.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2023.1256899/full#supplementary-material
References
- 1. Leidy HJ, Gwin JA, Roenfeldt CA, Zino AZ, Shafer RS. Evaluating the intervention-based evidence surrounding the causal role of breakfast on markers of weight management, with specific focus on breakfast composition and size. Adv Nutr (2016) 7(3):563S–75S. doi: 10.3945/an.115.010223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gibney MJ, Barr SI, Bellisle F, Drewnowski A, Fagt S, Livingstone B, et al. Breakfast in human nutrition: the international breakfast research initiative. Nutrients (2018) 10(5):559. doi: 10.3390/nu10050559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barr SI, DiFrancesco L, Fulgoni VL, 3rd. Association of breakfast consumption with body mass index and prevalence of overweight/obesity in a nationally-representative survey of canadian adults. Nutr J (2016) 15:33. doi: 10.1186/s12937-016-0151-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lu Z, Sun Z, Wu R, Du W, Zhang H, Zhang N, et al. Breakfast prevalence of medical students is higher than students from nonmedical faculties in inner Mongolia medical university. Eur J Clin Nutr (2020) 74(10):1442–7. doi: 10.1038/s41430-020-0569-8 [DOI] [PubMed] [Google Scholar]
- 5. Yokoro M, Wakimoto K, Otaki N, Fukuo K. Increased prevalence of breakfast skipping in female college students in covid-19. Asia Pac J Public Health (2021) 33(4):438–40. doi: 10.1177/1010539521998861 [DOI] [PubMed] [Google Scholar]
- 6. Heo J, Choi WJ, Ham S, Kang SK, Lee W. Association between breakfast skipping and metabolic outcomes by sex, age, and work status stratification. Nutr Metab (Lond) (2021) 18(1):8. doi: 10.1186/s12986-020-00526-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: A report from the american heart association. Circulation (2021) 143(8):e254–743. doi: 10.1161/CIR.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 8. Kaminsky LA, German C, Imboden M, Ozemek C, Peterman JE, Brubaker PH. The importance of healthy lifestyle behaviors in the prevention of cardiovascular disease. Prog Cardiovasc Dis (2022) 70:8–15. doi: 10.1016/j.pcad.2021.12.001 [DOI] [PubMed] [Google Scholar]
- 9. Little MP, Azizova TV, Richardson DB, Tapio S, Bernier MO, Kreuzer M, et al. Ionising radiation and cardiovascular disease: systematic review and meta-analysis. BMJ (2023) 380:e072924. doi: 10.1136/bmj-2022-072924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the gbd 2019 study. J Am Coll Cardiol (2020) 76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mohebi R, Chen C, Ibrahim NE, McCarthy CP, Gaggin HK, Singer DE, et al. Cardiovascular disease projections in the United States based on the 2020 census estimates. J Am Coll Cardiol (2022) 80(6):565–78. doi: 10.1016/j.jacc.2022.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pot GK, Hardy R, Stephen AM. Irregular consumption of energy intake in meals is associated with a higher cardiometabolic risk in adults of a british birth cohort. Int J Obes (2014) 38(12):1518–24. doi: 10.1038/ijo.2014.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sila S, Ilic A, Misigoj-Durakovic M, Soric M, Radman I, Satalic Z. Obesity in adolescents who skip breakfast is not associated with physical activity. Nutrients (2019) 11(10):2511. doi: 10.3390/nu11102511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen H, Zhang B, Ge Y, Shi H, Song S, Xue W, et al. Association between skipping breakfast and risk of cardiovascular disease and all cause mortality: A meta-analysis. Clin Nutr (2020) 39(10):2982–8. doi: 10.1016/j.clnu.2020.02.004 [DOI] [PubMed] [Google Scholar]
- 15. Li ZH, Xu L, Dai R, Li LJ, Wang HJ. Effects of regular breakfast habits on metabolic and cardiovascular diseases a protocol for systematic review and meta-analysis. Medicine (2021) 100(44):e27629. doi: 10.1097/md.0000000000027629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, et al. Meal timing and frequency: implications for cardiovascular disease prevention: A scientific statement from the american heart association. Circulation (2017) 135(9):E96–E121. doi: 10.1161/cir.0000000000000476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bonnet JP, Cardel MI, Cellini J, Hu FB, Guasch-Ferre M. Breakfast skipping, body composition, and cardiometabolic risk: A systematic review and meta-analysis of randomized trials. Obes (Silver Spring) (2020) 28(6):1098–109. doi: 10.1002/oby.22791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Santos HO, Genario R, Tinsley GM, Ribeiro P, Carteri RB, CdF C-R, et al. A scoping review of intermittent fasting, chronobiology, and metabolism. Am J Clin Nutr (2022) 115(4):991–1004. doi: 10.1093/ajcn/nqab433 [DOI] [PubMed] [Google Scholar]
- 19. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. BMJ (2021) 372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: A revised tool for assessing risk of bias in randomised trials. BMJ (2019) 366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 21. Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. Grade guidelines: 3. Rating the quality of evidence. J Clin Epidemiol (2011) 64(4):401–6. doi: 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 22. Duval S TR. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics (2000) 56(2):455–63. doi: 10.1111/j.0006-341x.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 23. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ (2011) 343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Willis BH, Riley RD. Measuring the statistical validity of summary meta-analysis and meta-regression results for use in clinical practice. Stat Med (2017) 36(21):3283–301. doi: 10.1002/sim.7372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Goff LM, Huang PY, Silva MJ, Bordoli C, Enayat EZ, Molaodi OR, et al. Associations of dietary intake with cardiometabolic risk in a multi-ethnic cohort: A longitudinal analysis of the determinants of adolescence, now young adults, social well-being and health (Dash) study. Br J Nutr (2019) 121(9):1069–79. doi: 10.1017/s0007114519000291 [DOI] [PubMed] [Google Scholar]
- 26. Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: A randomized controlled trial in lean adults. Am J Clin Nutr (2014) 100(2):539–47. doi: 10.3945/ajcn.114.083402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chowdhury EA, Richardson JD, Holman GD, Tsintzas K, Thompson D, Betts JA. The causal role of breakfast in energy balance and health: A randomized controlled trial in obese adults. Am J Clin Nutr (2016) 103(3):747–56. doi: 10.3945/ajcn.115.122044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr (2005) 81(2):388–96. doi: 10.1093/ajcn.81.2.388 [DOI] [PubMed] [Google Scholar]
- 29. Kobayashi F, Ogata H, Omi N, Nagasaka S, Yamaguchi S, Hibi M, et al. Effect of breakfast skipping on diurnal variation of energy metabolism and blood glucose. Obes Res Clin Pract (2014) 8(3):e201–98. doi: 10.1016/j.orcp.2013.01.001 [DOI] [PubMed] [Google Scholar]
- 30. LeCheminant GM, LeCheminant JD, Tucker LA, Bailey BW. A randomized controlled trial to study the effects of breakfast on energy intake, physical activity, and body fat in women who are nonhabitual breakfast eaters. Appetite (2017) 112:44–51. doi: 10.1016/j.appet.2016.12.041 [DOI] [PubMed] [Google Scholar]
- 31. Leidy HJ, Hoertel HA, Douglas SM, Higgins KA, Shafer RS. A high-protein breakfast prevents body fat gain, through reductions in daily intake and hunger, in “Breakfast skipping” Adolescents. Obesity (2015) 23(9):1761–4. doi: 10.1002/oby.21185 [DOI] [PubMed] [Google Scholar]
- 32. Neumann BL, Dunn A, Johnson D, Adams JD, Baum JI. Breakfast macronutrient composition influences thermic effect of feeding and fat oxidation in young women who habitually skip breakfast. Nutrients (2016) 8(8):490. doi: 10.3390/nu8080490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Geliebter A, Astbury NM, Aviram-Friedman R, Yahav E, Hashim S. Skipping breakfast leads to weight loss but also elevated cholesterol compared with consuming daily breakfasts of oat porridge or frosted cornflakes in overweight individuals: A randomised controlled trial. J Nutr Sci (2014) 3:e56. doi: 10.1017/jns.2014.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schlundt DG HJ, Sbrocco T, Pope-Cordle J, Sharp T. The role of breakfast in the treatment of obesity: A randomized clinical trial. Am J Clin Nutr (1992) 55(3):645–51. doi: 10.1093/ajcn/55.3.645 [DOI] [PubMed] [Google Scholar]
- 35. Zhang L CL, Liu J, Ma Y. The association between breakfast skipping and body weight, nutrient intake, and metabolic measures among participants with metabolic syndrome. Nutrients (2017) 9(4):384. doi: 10.3390/nu9040384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sievert K, Hussain SM, Page MJ, Wang Y, Hughes HJ, Malek M, et al. Effect of breakfast on weight and energy intake: systematic review and meta-analysis of randomised controlled trials. BMJ (2019) 364:l42. doi: 10.1136/bmj.l42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ma X, Chen Q, Pu Y, Guo M, Jiang Z, Huang W, et al. Skipping breakfast is associated with overweight and obesity: A systematic review and meta-analysis. Obes Res Clin Pract (2020) 14(1):1–8. doi: 10.1016/j.orcp.2019.12.002 [DOI] [PubMed] [Google Scholar]
- 38. Yamamoto R, Tomi R, Shinzawa M, Yoshimura R, Ozaki S, Nakanishi K, et al. Associations of skipping breakfast, lunch, and dinner with weight gain and overweight/obesity in university students: A retrospective cohort study. Nutrients (2021) 13(1):271. doi: 10.3390/nu13010271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Szajewska H, Ruszczynski M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in europe. Crit Rev In Food Sci And Nutr (2010) 50(2):113–9. doi: 10.1080/10408390903467514 [DOI] [PubMed] [Google Scholar]
- 40. Espinoza García AS, Martínez Moreno AG, Reyes Castillo Z. The role of ghrelin and leptin in feeding behavior: genetic and molecular evidence. Endocrinología Diabetes y Nutrición (English ed) (2021) 68(9):654–63. doi: 10.1016/j.endien.2020.10.009 [DOI] [PubMed] [Google Scholar]
- 41. Hollstein T, Basolo A, Unlu Y, Ando T, Walter M, Krakoff J, et al. Effects of short-term fasting on ghrelin/gh/igf-1 axis in healthy humans: the role of ghrelin in the thrifty phenotype. J Clin Endocrinol Metab (2022) 107(9):e3769–e80. doi: 10.1210/clinem/dgac353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Nunez-Salces M, Li H, Feinle-Bisset C, Young RL, Page AJ. The regulation of gastric ghrelin secretion. Acta Physiol (Oxf) (2021) 231(3):e:13588. doi: 10.1111/apha.13588 [DOI] [PubMed] [Google Scholar]
- 43. Obradovic M, Sudar-Milovanovic E, Soskic S, Essack M, Arya S, Stewart AJ, et al. Leptin and obesity: role and clinical implication. Front Endocrinol (Lausanne) (2021) 12:585887. doi: 10.3389/fendo.2021.585887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mendoza-Herrera K, Florio AA, Moore M, Marrero A, Tamez M, Bhupathiraju SN, et al. The leptin system and diet: A mini review of the current evidence. Front Endocrinol (Lausanne) (2021) 12:749050. doi: 10.3389/fendo.2021.749050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Freire RH, Alvarez-Leite JI. Appetite control: hormones or diet strategies? Curr Opin Clin Nutr Metab Care (2020) 23(5):328–35. doi: 10.1097/MCO.0000000000000675 [DOI] [PubMed] [Google Scholar]
- 46. Tucker JAL, Bornath DPD, McCarthy SF, Hazell TJ. Leptin and energy balance: exploring leptin’s role in the regulation of energy intake and energy expenditure. Nutr Neurosci (2022), 1–9. doi: 10.1080/1028415X.2022.2161135 [DOI] [PubMed] [Google Scholar]
- 47. Flanagan A, Bechtold DA, Pot GK, Johnston JD. Chrono-nutrition: from molecular and neuronal mechanisms to human epidemiology and timed feeding patterns. J Neurochem (2021) 157(1):53–72. doi: 10.1111/jnc.15246 [DOI] [PubMed] [Google Scholar]
- 48. Mori H, Hanada R, Hanada T, Aki D, Mashima R, Nishinakamura H, et al. Socs3 deficiency in the brain elevates leptin sensitivity and confers resistance to diet-induced obesity. Nat Med (2004) 10(7):739–43. doi: 10.1038/nm1071 [DOI] [PubMed] [Google Scholar]
- 49. Tirosh A, Tuncman G, Calay ES, Rathaus M, Ron I, Tirosh A, et al. Intercellular transmission of hepatic er stress in obesity disrupts systemic metabolism. Cell Metab (2021) 33(2):319–33.e6. doi: 10.1016/j.cmet.2020.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. De Souza CT, Araujo EP, Bordin S, Ashimine R, Zollner RL, Boschero AC, et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology (2005) 146(10):4192–9. doi: 10.1210/en.2004-1520 [DOI] [PubMed] [Google Scholar]
- 51. Shan X, Yeo GS. Central leptin and ghrelin signalling: comparing and contrasting their mechanisms of action in the brain. Rev Endocr Metab Disord (2011) 12(3):197–209. doi: 10.1007/s11154-011-9171-7 [DOI] [PubMed] [Google Scholar]
- 52. Clayton DJ, James LJ. The effect of breakfast on appetite regulation, energy balance and exercise performance. Proc Nutr Soc (2016) 75(3):319–27. doi: 10.1017/S0029665115004243 [DOI] [PubMed] [Google Scholar]
- 53. Clayton DJ, Stensel DJ, James LJ. Effect of breakfast omission on subjective appetite, metabolism, acylated ghrelin and glp-17-36 during rest and exercise. Nutrition (2016) 32(2):179–85. doi: 10.1016/j.nut.2015.06.013 [DOI] [PubMed] [Google Scholar]
- 54. Nackers LM, Ross KM, Perri MG. The association between rate of initial weight loss and long-term success in obesity treatment: does slow and steady win the race? Int J Behav Med (2010) 17(3):161–7. doi: 10.1007/s12529-010-9092-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wadden TA FG, Wang J, Pierson RN, Yang MU, Moreland K, Stunkard AJ, et al. Clinical correlates of short- and long-term weight loss. Am J Clin Nutr (1992) 56):1. doi: 10.1093/ajcn/56.1.271S [DOI] [PubMed] [Google Scholar]
- 56. Chowdhury EA, Richardson JD, Tsintzas K, Thompson D, Betts JA. Effect of extended morning fasting upon ad libitum lunch intake and associated metabolic and hormonal responses in obese adults. Int J Obes (Lond) (2016) 40(2):305–11. doi: 10.1038/ijo.2015.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Jakubowicz D, Barnea M, Wainstein J, Froy O. High caloric intake at breakfast vs. Dinner differentially influences weight loss of overweight and obese women. Obes (Silver Spring) (2013) 21(12):2504–12. doi: 10.1002/oby.20460 [DOI] [PubMed] [Google Scholar]
- 58. Jakubowicz D, Wainstein J, Tsameret S, Landau Z. Role of high energy breakfast “Big breakfast diet” in clock gene regulation of postprandial hyperglycemia and weight loss in type 2 diabetes. Nutrients (2021) 13(5):1558. doi: 10.3390/nu13051558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ruddick-Collins LC, Morgan PJ, Fyfe CL, Filipe JAN, Horgan GW, Westerterp KR, et al. Timing of daily calorie loading affects appetite and hunger responses without changes in energy metabolism in healthy subjects with obesity. Cell Metab (2022) 34(10):1472–85 e6. doi: 10.1016/j.cmet.2022.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Reeves S, Huber JW, Halsey LG, Horabady-Farahani Y, Ijadi M, Smith T. Experimental manipulation of breakfast in normal and overweight/obese participants is associated with changes to nutrient and energy intake consumption patterns. Physiol Behav (2014) 133:130–5. doi: 10.1016/j.physbeh.2014.05.015 [DOI] [PubMed] [Google Scholar]
- 61. Magkos F. Is calorie restriction beneficial for normal-weight individuals? A narrative review of the effects of weight loss in the presence and absence of obesity. Nutr Rev (2022) 80(7):1811–25. doi: 10.1093/nutrit/nuac006 [DOI] [PubMed] [Google Scholar]
- 62. Brikou D, Zannidi D, Karfopoulou E, Anastasiou CA, Yannakoulia M. Breakfast consumption and weight-loss maintenance: results from the medweight study. Br J Nutr (2016) 115(12):2246–51. doi: 10.1017/S0007114516001550 [DOI] [PubMed] [Google Scholar]
- 63. Dashti HS, Gomez-Abellan P, Qian J, Esteban A, Morales E, Scheer F, et al. Late eating is associated with cardiometabolic risk traits, obesogenic behaviors, and impaired weight loss. Am J Clin Nutr (2021) 113(1):154–61. doi: 10.1093/ajcn/nqaa264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Scott HA, Marcinow M, Hicks R, Buchholz AC. Breakfast cereal consumption moderates the association between body composition and body esteem in young women but not in young men. Can J Diet Pract Res (2014) 75(4):214–7. doi: 10.3148/cjdpr-2014-012 [DOI] [PubMed] [Google Scholar]
- 65. Mattiuzzi C, Sanchis-Gomar F, Lippi G. Worldwide burden of ldl cholesterol: implications in cardiovascular disease. Nutr Metab Cardiovasc Dis (2020) 30(2):241–4. doi: 10.1016/j.numecd.2019.09.008 [DOI] [PubMed] [Google Scholar]
- 66. Hilvo M, Dhar I, Laaperi M, Lysne V, Sulo G, Tell GS, et al. Primary cardiovascular risk prediction by ldl-cholesterol in caucasian middle-aged and older adults: A joint analysis of three cohorts. Eur J Prev Cardiol (2022) 29(3):e128–e37. doi: 10.1093/eurjpc/zwab075 [DOI] [PubMed] [Google Scholar]
- 67. Arimoto M, Yamamoto Y, Imaoka W, Kuroshima T, Toragai R, Nakamura M, et al. Small dense low-density lipoprotein cholesterol levels in breakfast skippers and staple foods skippers. J Atheroscler Thromb (2023) 30(10):1376–88. doi: 10.5551/jat.64024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lee DW, Choi DW, Ju YJ, Lee SA, Park EC. The association between low frequency of having breakfast and dyslipidemia in South Korean men and women. Eur J Clin Nutr (2019) 73(6):896–904. doi: 10.1038/s41430-018-0289-5 [DOI] [PubMed] [Google Scholar]
- 69. Sierra-Johnson J, Unden AL, Linestrand M, Rosell M, Sjogren P, Kolak M, et al. Eating meals irregularly: A novel environmental risk factor for the metabolic syndrome. Obes (Silver Spring) (2008) 16(6):1302–7. doi: 10.1038/oby.2008.203 [DOI] [PubMed] [Google Scholar]
- 70. Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ. Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the childhood determinants of adult health study. Am J Clin Nutr (2010) 92(6):1316–25. doi: 10.3945/ajcn.2010.30101 [DOI] [PubMed] [Google Scholar]
- 71. Souza MR, Neves MEA, Gorgulho BM, Souza AM, Nogueira PS, Ferreira MG, et al. Breakfast skipping and cardiometabolic risk factors in adolescents: systematic review. Rev Saude Publica (2021) 55:107. doi: 10.11606/s1518-8787.2021055003077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. The Relationship between Breakfast Habits KR. and plasma cholesterol levels in schoolchildren. J Sch Health (1991) 61(2):81–5. doi: 10.1111/j.1746-1561.1991.tb03242.x [DOI] [PubMed] [Google Scholar]
- 73. Shang X, Li Y, Xu H, Zhang Q, Hu X, Liu A, et al. Healthy breakfast habits and changes in obesity-related cardiometabolic markers in children: A longitudinal analysis. Eur J Clin Nutr (2020) 74(12):1685–97. doi: 10.1038/s41430-020-0614-7 [DOI] [PubMed] [Google Scholar]
- 74. Yoon SR, Fogleman SK, Kim H, Lee KE, Kim OY. Breakfast intake effect on the association between fast-food consumption and the risk of obesity and dyslipidemia in korean adults aged 20-39 years based on the korea national health and nutrition examination survey iv 2013-2014. Clin Nutr Res (2020) 9(2):107–21. doi: 10.7762/cnr.2020.9.2.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. de Souza MR, Neves MEA, Souza AM, Muraro AP, Pereira RA, Ferreira MG, et al. Skipping breakfast is associated with the presence of cardiometabolic risk factors in adolescents: study of cardiovascular risks in adolescents - erica. Br J Nutr (2021) 126(2):276–84. doi: 10.1017/S0007114520003992 [DOI] [PubMed] [Google Scholar]
- 76. Witbracht M, Keim NL, Forester S, Widaman A, Laugero K. Female breakfast skippers display a disrupted cortisol rhythm and elevated blood pressure. Physiol Behav (2015) 140:215–21. doi: 10.1016/j.physbeh.2014.12.044 [DOI] [PubMed] [Google Scholar]
- 77. Aparicio-Cercos C, Alacreu M, Salar L, Moreno Royo L. Waist-to-height ratio and skipping breakfast are predictive factors for high blood pressure in adolescents. Sci Rep (2020) 10(1):16704. doi: 10.1038/s41598-020-73355-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bi H, Gan Y, Yang C, Chen Y, Tong X, Lu Z. Breakfast skipping and the risk of type 2 diabetes: A meta-analysis of observational studies. Public Health Nutr (2015) 18(16):3013–9. doi: 10.1017/S1368980015000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Nas A, Mirza N, Hagele F, Kahlhofer J, Keller J, Rising R, et al. Impact of breakfast skipping compared with dinner skipping on regulation of energy balance and metabolic risk. Am J Of Clin Nutr (2017) 105(6):1351–61. doi: 10.3945/ajcn.116.151332 [DOI] [PubMed] [Google Scholar]
- 80. Jeans MR, Vandyousefi S, Landry MJ, Leidy HJ, Gray MJ, Bray MS, et al. Breakfast consumption may improve fasting insulin, homa-ir, and hba1c levels in predominately low-income, hispanic children 7-12 years of age. Nutrients (2022) 14(11):2320. doi: 10.3390/nu14112320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Kim HS, Jung SJ, Jang S, Kim MJ, Cha YS. Rice-based breakfast improves fasting glucose and homa-ir in korean adolescents who skip breakfast, but breakfast skipping increases aromatic amino acids associated with diabetes prediction in korean adolescents who skip breakfast: A randomized, parallel-group, controlled trial. Nutr Res Pract (2022) 16(4):450–63. doi: 10.4162/nrp.2022.16.4.450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Heilbronn LK, Regmi P. Will delaying breakfast mitigate the metabolic health benefits of time-restricted eating? Obes (Silver Spring) (2020) 28 Suppl 1:S6–7. doi: 10.1002/oby.22776 [DOI] [PubMed] [Google Scholar]
- 83. Xie Z, He Z, Ye Y, Mao Y. Effects of time-restricted feeding with different feeding windows on metabolic health: A systematic review of human studies. Nutrition (2022) 102:111764. doi: 10.1016/j.nut.2022.111764 [DOI] [PubMed] [Google Scholar]
- 84. Li Z, Huang L, Luo Y, Yu B, Tian G. Effects and possible mechanisms of intermittent fasting on health and disease: A narrative review. Nutr Rev (2023) 81(12):1626–35. doi: 10.1093/nutrit/nuad026 [DOI] [PubMed] [Google Scholar]
- 85. Stockman MC, Thomas D, Burke J, Apovian CM. Intermittent fasting: is the wait worth the weight? Curr Obes Rep (2018) 7(2):172–85. doi: 10.1007/s13679-018-0308-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Santos HO, Tinsley GM. Is breakfast consumption detrimental, unnecessary, or an opportunity for health promotion? A review of cardiometabolic outcomes and functional food choices. Diabetes Metab Res Rev (2023):e3684. doi: 10.1002/dmrr.3684 [DOI] [PubMed] [Google Scholar]
- 87. Tang J, Dong JY, Eshak ES, Cui R, Shirai K, Liu K, et al. Breakfast type and cardiovascular mortality: the Japan collaborative cohort study. J Atheroscler Thromb (2022) 30(9):1255–64. doi: 10.5551/jat.63564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Carew AS, Mekary RA, Kirkland S, Theou O, Siddiqi F, Urquhart R, et al. Prospective study of breakfast frequency and timing and the risk of incident type 2 diabetes in community-dwelling older adults: the cardiovascular health study. Am J Clin Nutr (2022) 116(2):325–34. doi: 10.1093/ajcn/nqac087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Zhu S, Cui L, Zhang X, Shu R, VanEvery H, Tucker KL, et al. Habitually skipping breakfast is associated with chronic inflammation: A cross-sectional study. Public Health Nutr (2021) 24(10):2936–43. doi: 10.1017/S1368980020001214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Gwin JA, Leidy HJ. A review of the evidence surrounding the effects of breakfast consumption on mechanisms of weight management. Adv Nutr (2018) 9(6):717–25. doi: 10.1093/advances/nmy047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Sun Y, Rong S, Liu B, Du Y, Wu Y, Chen L, et al. Meal skipping and shorter meal intervals are associated with increased risk of all-cause and cardiovascular disease mortality among us adults. J Acad Nutr Diet (2023) 123(3):417–26 e3. doi: 10.1016/j.jand.2022.08.119 [DOI] [PubMed] [Google Scholar]
- 92. Paoli A, Tinsley G, Bianco A, Moro T. The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients (2019) 11(4):719. doi: 10.3390/nu11040719 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.