Abstract
South Asians (SAs, individuals with ancestry from Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka) are among the fastest growing ethnic subgroups in the United States. SAs typically experience a high prevalence of diabetes, abdominal obesity, and hypertension, among other cardiovascular disease risk factors, which are often under recognized and undermanaged. The excess coronary heart disease risk in this growing population must be critically assessed and managed with culturally appropriate preventive services. Accordingly, this scientific document prepared by a multidisciplinary group of clinicians and investigators in cardiology, internal medicine, pharmacy, and SA-centric researchers describes key characteristics of traditional and nontraditional cardiovascular disease risk factors, compares and contrasts available risk assessment tools, discusses the role of blood-based biomarkers and coronary artery calcium to enhance risk assessment and prevention strategies, and provides evidenced-based approaches and interventions that may reduce coronary heart disease disparities in this higher-risk population.
Key words: diabetes, ethnic, lipid, prevention, risk, South Asian
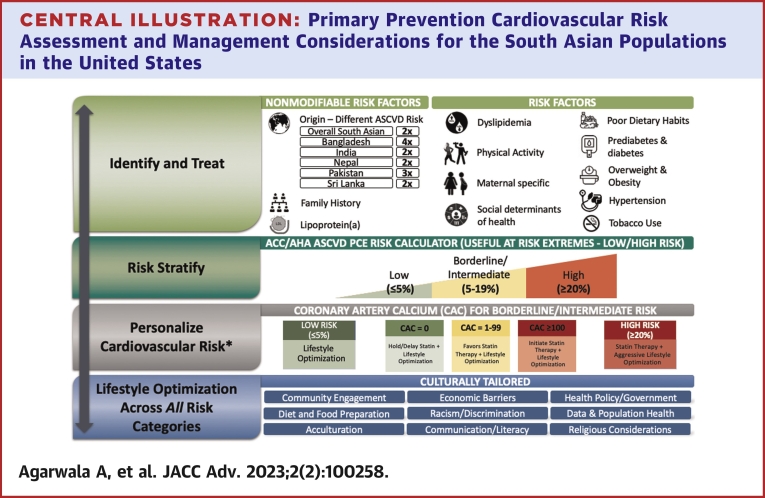
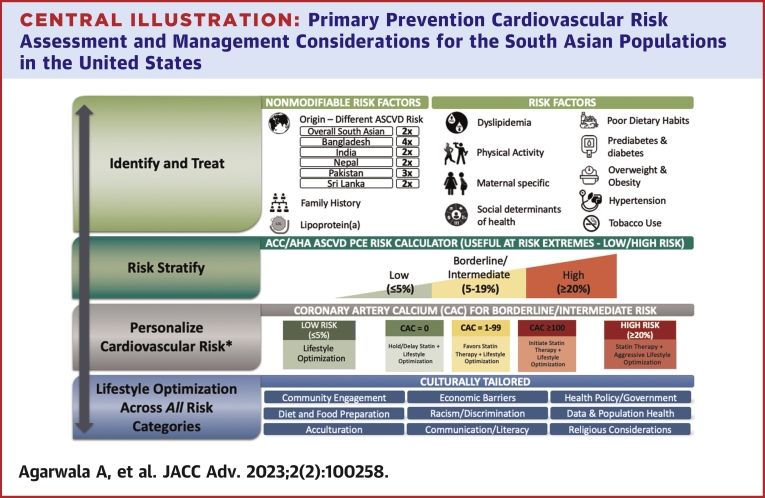
Central Illustration
Highlights
-
•
South Asians experience a higher burden of CHD compared with adults of other racial/ethnic groups.
-
•
Culturally adapted assessment and management of traditional and nontraditional risk factors is essential.
-
•
Available population ASCVD risk assessment tools may be unreliable, particularly for those at borderline and intermediate risk; CAC testing may help refine risk and personalize care.
-
•
Evaluation of South Asian subpopulations will help characterize the contribution of social determinants, environmental influences, and genetic susceptibility on heterogenous cardiovascular disease burden.
Cardiovascular disease (CVD) is the leading cause of noncommunicable disease burden globally and in the United States, contributing significantly to subsequent disability and rising health care costs.1 While successful primary and secondary CVD prevention campaigns have slowed the rate of CVD-related mortality, smaller decreases in heart disease death have been seen in some minority populations in the United States, including South Asians (SAs).2, 3, 4
South Asians (individuals who trace their ancestry from Bangladesh, Bhutan, India, the Maldives, Nepal, Pakistan, and Sri Lanka) are diverse with regard to region of origin, cultural identity, religious practices, cuisine, and language use. Accordingly, while the atherosclerotic cardiovascular disease (ASCVD) risk for SA adults is roughly double that of White adults,5, 6, 7 the risk of coronary heart disease (CHD) differs across SA subpopulations.5 Several cross-sectional studies have also reported a higher prevalence of prediabetes, type 2 diabetes (T2D), abdominal obesity, and hypertension, with lower levels of physical activity among SA adults compared to other racial/ethnic groups.8, 9, 10, 11, 12 The clinical presentation of ASCVD among SAs generally occurs earlier in life (mean age 53 years), with a higher burden of atherosclerosis, even in the absence of symptoms or clinical findings.9,13, 14, 15 Despite recognition of elevated ASCVD risk16 recommendations for risk, assessment, and stratification (a fundamental concept for the prevention of ASCVD), and subsequent management are not sufficiently tailored to the high ASCVD risk experienced by SA adults, largely because population-specific risk calculators inadequately estimate risk in this population, particularly for those at borderline or intermediate risk (≥5%-<20% by the pooled cohort equations [PCE]).5,17
Herein, we aim to address the roles of traditional and nontraditional risk factors, and review emerging strategies for risk assessment and reclassification, such as blood-based biomarkers and coronary artery calcium (CAC), that may better inform primary prevention of premature ASCVD in SAs who reside in the United States.
South Asians are a heterogenous population
In the United States, understanding the health and disease patterns in specific Asian subpopulations has been challenging largely because Asian subgroups have frequently been aggregated into a single “Asian” category. The earliest SA immigrants (namely, from India and Pakistan) were regarded as ‘other’ when reporting US census data until 1920, followed by ‘Hindu.’18 The Luce–Celler Act of 1946 granted naturalization rights and extended immigration quotas allowing 100 people each from India and Pakistan to immigrate to the United States per year; these quotas were lifted in 1965, encouraging an influx of skilled professionals from all SA countries.19 Family reunification in the mid-1980s allowed further diversification of the SA population. Accordingly, the SA diaspora has spread across the United States with heavily concentrated pockets in California, the District of Columbia, Illinois, New Jersey, New York, Texas, and Virginia.20 The category ‘Asian Indian’ was the only SA subgroup identification available for immigrants on the US census card until 2010, after which ‘other Asian’ was introduced as an additional write-in category to encompass people from the remaining SA countries.21,22
In addition to more detailed U.S. Census and vital statistics race and ethnicity reporting, recent (Supplemental Table 1) and emerging (Supplemental Table 2a and 2b) research have focused specifically on SA health data. For example, CHD mortality rates are higher among SAs living in their native countries compared to those living in Western countries.23,24 Similarly, immigrant SAs in Europe have higher CHD rates compared to local populations.78 U.S. Asian Indian men and women have persistently higher age-standardized mortality rates from ischemic heart disease and heart failure when compared to non-Hispanic White (NHW) individuals.3,6,25 Compared to other SA subpopulations, however, the highest risk of CHD is seen among those of Bangladeshi origin, followed by Pakistani, then Indian adults: HR 3.66 (95% CI: 2.38-5.61), HR 2.45 (95% CI: 2.06-2.91), HR 1.83 (95% CI: 1.64-2.04), respectively.5,26 Other studies have demonstrated that Bangladeshi adults have the highest burden of diabetes, hyperlipidemia, and CHD among SA subpopulations.27, 28, 29
Traditional risk factors
Traditional risk factors explain a large proportion of ASCVD risk in SA adults.5,8,9,30,31 The timing for screening among SAs compared to other ethnicities is less clear. ASCVD risk assessment guidelines in New Zealand suggest traditional risk factor (TRF) assessment in SA at age 30 years for men and 40 years for women, considering higher rates of CHD in immigrant SA living there.30 The US Preventive Service Task Force recommends lipid screening for men aged 20 to 35 and women 20 to 45, if they are at an increased risk of CHD (defined as: diabetes, history of previous CHD or atherosclerosis, family history of CVD, tobacco use, hypertension, and obesity (body mass index [BMI] ≥30 kg/m2)); however, they do not specify ethnicity/race.32
Type 2 diabetes
Compared to other racial/ethnic groups, SAs living in America have a high prevalence of T2D, albeit high variability exists by US state. The prevalence of T2D in SA according to the US National Health and Nutrition Examination Survey (2011-2016) was estimated at 22.4% compared to 12.1% in NHW, 20.4% in Black, and 22.1% in Hispanic adults, respectively.33 SA in the MASALA (Mediators of Atherosclerosis in South Asians Living in America) study (San Francisco and Chicago) showed a higher age-adjusted prevalence of diabetes compared to other adults in MESA (23% vs 6% in Whites, 18% in Blacks, 17% in Hispanic, and 13% in Chinese Americans).11 The age-adjusted prevalence of T2D using electronic health records (EHRs) for SA living in Northern California, New York City, and Atlanta were 29.1%, 10.7%, and 6.7%, respectively.34,35 The prevalence of T2D also varies among US and non-US community-dwelling SA subpopulations36: Bangladesh (10.4%-25%), Pakistani (11.6%-22.6%), Sri Lankan (7.8%-26.8%), Indian (7.1%-18.3%), Maldivian (7.6%), Bhutanese (4.9%), and Nepalese (3.0%-16.5%).28,29,36, 37, 38, 39 Once diagnosed, residual poor glycemic control is more likely encountered compared to NHW, related to lack of culturally appropriate education, social stigmatization, beliefs about the need for diabetes medications, and uptake of traditional remedies, for example.40, 41, 42, 43
National Health Interview Survey data suggest that Asian Indian adults were diagnosed with T2D 5 years younger (46 years old; 95% CI: 43.9-48.5 years), P < 0.001) than NHW (51 years old; 95% CI: 50.4-51.9 years), P < 0.001).44 Regional data using the California Health Interview Survey revealed that SAs were diagnosed with T2D 10.2 years earlier compared to NHW (mean age 44.9 vs 55.4, respectively).45
The high prevalence of diabetes is complex and multifactorial and is attributed to a combination of factors including excess visceral and intramyocellular adiposity and low lean muscle mass, obesity, metabolic syndrome, diet (traditionally vegetarian-but not all, high in fried carbohydrates, trans fat, and saturated fat), low rates of physical activity, high prevalence of low birth weight, pathophysiologic pathways including impaired insulin secretion and insulin resistance, and lifestyle and culture.46, 47, 48, 49, 50 Other metabolic abnormalities include higher plasma insulin levels, insulin-like growth factor–binding protein, and plasma leptin, and lower levels of adiponectin and resistin.10,51,52
South Asians are at high risk of T2D at a lower BMI compared to other ethnicities, even when accounting for other traditional risk factors.40 This is referred to as the ‘thin-fat’ or ‘South Asian’ phenotype of elevated fasting glucose, low high-density lipoprotein cholesterol (HDL-C), high triglycerides, and lower lean mass at normal ranges of BMI.36,53
Early and repeated screening for glucose intolerance and T2D may help identify at risk individuals. Indeed, there was a high incidence rate of glycemic progression in the MASALA study, where 32% (95% CI: 27.6-35.9) of participants progressed either from normal glucose tolerance to prediabetes or T2D, or from prediabetes to T2D over 5 years of follow-up.36 Recommendations from the American Diabetes Association (ADA), World Health Organization (WHO), National Institute for Health and Care Excellence (United Kingdom), and South Asian Health Foundation suggest that a BMI of ≥23 kg/m2 should trigger screening for diabetes in SA.54, 55, 56, 57, 58
Hypertension
In the United States, the age-adjusted prevalence of hypertension is 20 to 43% among studies of community-dwelling SA.35,59, 60, 61 These findings are consistent with the reported prevalence of 27% in a 2014 meta-analysis of observational studies from South Asian Association for Regional Cooperation member countries.62 Factors such as length of U.S. residency and poor dietary habits influence the development of hypertension.49,63
Hypertension is a well-established independent risk factor for myocardial infarction (MI), stroke, and chronic kidney disease.8,64, 65, 66 Compared to other racial groups/ethnicities, SAs have a higher rate of hypertension awareness, no difference in the rate of hypertension treatment, and lower rates of antihypertensive therapy adherence.67,68 Although outcomes data on ideal blood pressure (BP) goals, optimal medication regimen, and medication adherence are lacking, the guideline-recommended approach to aggressively treat BP is likely applicable. The most recent American College of Cardiology/American Heart Association (ACC/AHA) guidelines for the management of hypertension established new BP categories with lower treatment thresholds and BP goals.69 Indeed, 17% SA adults were recommended antihypertensive pharmacotherapy by the 2017 ACC/AHA hypertension guideline compared to 8% by Joint National Committee-7.70 The Blood Pressure Association UK Charity/South Asian Health Foundation has provided recommendations for managing hypertension in SA aimed at defining BP cutoff values, understanding the interplay of hypertension with other TRF, suggesting dietary and lifestyle enhancement, and explaining the value of pharmaceutical therapy if indicated.71 A summary of these recommendations is provided in Table 1.
Table 1.
Primary Prevention Management Considerations for Individuals of South Asian Ancestry72
| Step 1 | Inquire about country of origin (ASCVD risk is highest among those from Bangladesh and Pakistan) and length of residency in America, if applicable. | |
| Step 2 | Assess key risk factors. | |
| Risk factor | Screening/Testing, if applicable. | |
| Prediabetes and type 2 diabetes | ||
| Hypertension |
|
|
| Dyslipidemia Common patterns: 1) ‘Atherogenic dyslipidemia,’ characterized by: ↓ HDL-C, ↑ triglycerides, and ↑ total cholesterol; 2) ‘HDL paradox’ defined as dysfunctional HDL-C, even at higher values. |
|
|
| Tobacco use |
|
|
| Overweight and obesity | ||
| Physical activity |
|
|
| Family history of coronary artery disease (premature or any first-degree relative) |
|
|
| Diet and nutrition |
|
|
| Women’s reproductive health | ||
| Step 3 | Offer languages concordant with the patient’s ethnicity (eg, translator service), provide educational material written and translated into languages native to South Asian countries, provide and encourage education on cultural beliefs and practices for all team members of the healthcare team. | |
| Step 4 | Risk assess: Calculate cardiovascular risk using the 2013 PCE; ‘South Asian’ ethnicity is a risk-enhancing factor for those at borderline and intermediate risk by the PCE. | |
| Step 5 | Risk stratify: Consider use of CAC scoring to further stratify risk, particularly for those at borderline or intermediate risk (≥5%-<20% by the PCE), or those who are low risk by the PCE (<5%) with a family history of coronary heart disease.82,88,93,a | |
| Step 6 | If available, refer to a South Asian cardiovascular and metabolic specialty program.94 | |
ASCVD = atherosclerotic cardiovascular disease; BMI = body mass index; CAC = coronary artery calcium; HbA1c = hemoglobin A1c; HDL-C = high-density lipoprotein cholesterol; PCE = pooled cohort equations.
Particularly for Asian Indian adults based on available data.
Dyslipidemia
Atherogenic dyslipidemia among SAs is characterized by higher levels of triglycerides and total cholesterol, lower/similar low-density lipoprotein-cholesterol (LDL-C), and lower levels of HDL-C compared to NHW.95, 96, 97 Compared to other racial/ethnic groups, SAs also may have higher levels of apolipoprotein (Apo)-B100 and non-HDL-C, lipoprotein(a) [Lp(a)], and low levels of Apo-A1, although more data are required.9,98, 99, 100 For example, in the INTERHEART study, Asian Indians had the lowest HDL-C, the highest ratios for total cholesterol/HDL-C and Apo-B/Apo-A1, respectively, across all LDL-C categories compared to other ancestral groups. Importantly, all of these parameters predicted future coronary artery disease, respectively.23
The prevalence of HDL-C <40 mg/dL in males and <50 mg/dL in females has been reported as high as 52% and 54% of Asian Indian men and women using EHR data in Northern California, respectively.101 The cardioprotective effect of HDL-C may be blunted in SAs compared to other East Asian subgroups: the OR for 1 SD increase in HDL-C among SAs was 0.87 (95% CI: 0.72-1.06), vs 0.77 (95% CI: 0.70-0.85) in other East Asians at the time of the first MI.31 This may be explained by a higher concentration of smaller HDL-C particles that contribute proinflammatory and prooxidant effects and are unable to participate in effective reverse cholesterol transport.102,103 Higher Apo-A1 (principal structural and functional protein component of HDL-C) levels in SAs are associated with a lower risk of MI.31
Lp(a) is genetically determined and highly atherogenic. Lp(a) is estimated to be elevated (>50 mg/dL or >125 nmol/L) in 25% of SA globally.104,105 The population attributable risk of MI was highest for SA when Lp(a) was >50 mg/dL.106 Compared to other racial/ethnic groups, the association of Lp(a) concentrations and MI in a case-control study was highest in SA (OR: 2.14, 95% CI: 1.59-2.89, P < 0.001).106 Prospective data suggest an association between elevated Lp(a) and ASCVD (HR: 1.31, 95% CI: 1.04-1.64, P = 0.023).5 Lp(a) levels were not associated with CAC prevalence (P = 0.98), common carotid atherosclerosis (P = 0.97), or aortic valve calcification (P = 0.64) in the MASALA study.107,108 SAs tend to have lower Lp(a) levels than Black adults, which may signal the need for ethnic specific Lp(a) thresholds to select truly higher risk individuals.105,107
South Asian men and women have similar or lower LDL-C levels compared to other racial/ethnic groups.96,109 Among SA subgroups, Pakistani adults had higher mean LDL-C values compared to North Indian (120 mg/dL vs 109 mg/dL, respectively; P = 0.02), although no difference was found between North and South Indian (P = 0.49) or between South Indian and Pakistani adults (P = 0.06).110 Importantly, at first time MI in the INTERHERT study, SAs has lower mean LDL-C compared to all other Southeast Asian subgroups (mean LDL-C 125.2 mg/dL vs 150.4 mg/dL, respectively). Compared to other Asian ethnicities, SAs have smaller, less dense LDL-C particles with a higher concentration of ApoB.31 This indicates a larger atherogenic particle load that may account for the elevated risk of ASCVD, even at lower LDL-C concentrations.31,111
In the absence of randomized controlled or prospective data, the National Lipid Association has provided expert opinion recommendations regarding the optimal primary prevention targets for lipid profiles in SAs, based on risk profile (high = PCE 10 years 20%-29%, very high = PCE 10 years 30%-39%, and extreme = PCE >40%).88 For example, LDL-C (mg/dL) goals for the 3 risk categories are <70, <50, and <30, respectively. The ideal triglycerides target is <150 mg/dL, and HDL-C (mg/dL) is suggested to be >40 in men and >50 in women.
Overweight and obesity status
Body composition and fat distribution are important determinants of CVD risk in SAs who tend to have a higher percentage of body, liver, and visceral fat compared to other ancestral groups.10,112 Hence, BMI calculations in SAs may be unreliable considering this body fat distribution. As such, the ADA and WHO recommended lowering BMI cut points to encourage public health action, with a focus on weight reduction and increased physical activity.10,55,56 Accordingly, the prevalence of obesity in SAs varies between studies. For example, in SA, the prevalence of obesity (defined as BMI ≥27.5 kg/m2) was 39.3% in men and 36.8% in women in a Northern California EHR cohort.34 National survey data indicated the overall prevalence of obesity may be higher at 77.6% (defined as BMI ≥23 kg/m2 in this study).63 National data also suggest that compared to other Asian subgroups, SAs have the one of the highest prevalence of overweight/obesity status.113,114
Compared with European Whites, SAs have a relatively greater amount of abdominal adipose tissue.115 Central adiposity is associated with insulin resistance and metabolic syndrome, contributes to hypertension, high cholesterol, lower HDL-C, and independently predicts acute ischemic heart disease in Asian Indians.64
Clinicians should be aware of cultural beliefs regarding body habitus considering self-perceived underestimates of weight status and the effect of weight on the risk for chronic diseases.116,117 Age at immigration and duration of residence in the United States are also correlated with a higher prevalence of overweight/obese status.118,119 SA infants have higher visceral and subcutaneous adipose tissue deposits compared to NHW, falsely capturing a healthy weight status even in the setting of higher metabolic risk.120 Primordial prevention efforts including a greater emphasis on maternal health during pregnancy may be necessary, considering SA children (ages 5-7) are more likely to be overweight/obese compared to children of other race/ethnicities.121
The ADA Diabetes Guidelines suggest annual BMI screening with a cut point value of ≥23 kg/m2 in SAs to define overweight status.57 In addition to encouraging a “healthy meal plan” and increased physical activity, obesity guidelines from the American College of Endocrinology also suggest annual screening (same BMI cut point as ADA) and define abdominal obesity in SA as a waist circumferences of ≥85 cm in men and ≥74 cm in women57,78; this is lower than SA waist circumference recommendations by the International Diabetes Federation Epidemiology Task Force Consensus Group (≥90 cm in men; ≥80 cm in women).122 The large-scale utility of other measurements such as adiposity (eg, bioelectric impedance, magnetic resonance imaging, and air/water displacement plethysmography) is limited considering the lack of outcome data.78
Diet
As a result of urbanization, mechanization and increased availability of processed foods, SA countries and those who inhabit the diaspora have transitioned from diets rich in whole grains and complex carbohydrates to those that are higher in saturated fats and refined carbohydrates.49,123, 124, 125 In SA, a longer residence in the United States is directly associated with higher intake of saturated and trans fats, dietary cholesterol, and alcohol, for example (P < 0.05).126 This is consistent with the dietary habits of SAs after migration to European countries.127 Examples of deleterious cooking and dietary habits include: 1) high heat cooking and deep frying; 2) using reheated oil high in trans fats and advanced glycosylation end product; 3) using oils with high saturated fats (partially hydrogenated vegetable oil, palmolein oil); 4) lower quantity and quality of protein intake; and 5) high intake of sugar and refined carbohydrates.128,129
Alternatively, a diet higher in fruit, vegetables, nuts, and legumes is associated with a lower prevalence of hypertension and metabolic syndrome.49 A healthy plant-based diet was associated with a lower incidence of T2D, lower odds of fatty liver, and a better metabolic risk factor profile in MASALA.85 Additionally, a Mediterranean-type diet that incorporates traditional SA food is associated with a lower likelihood of obesity, fatty liver, and T2D.85 Higher attainment of cardiovascular health metrics (inclusive of a healthy diet) is associated with a lower prevalence of subclinical atherosclerosis as measured by CAC and carotid intima media thickness.126
Providing dietary recommendations requires a focus on providing culturally sensitive nutritional advice. For example, a relatively high proportion of Asian Indians follow a vegetarian diet, owing to religious beliefs or cultural reasons.130,131 Considerations must also be given to religious obligations such as Ramadan fasting, while encouraging balanced-meals (whole grains, fruits and vegetables, adequate hydration) during non-fasting hours.132, 133, 134 Dietary patterns vary among different SA communities. For example, a study of dishes from different parts of India showed a significant variation in fat and energy content.135 A South Asian food-specific carbohydrate counting tool has been developed to assist patients and providers understand the carbohydrate content of commonly consumed food products.136 The Canadian Heart and Stroke Foundation and National Lipid Association have also developed evidence-based dietary recommendations focused on portion control and informed choices, and are summarized in Table 1.83,84
Physical activity
When compared to other racial/ethnic groups living in North America, the prevalence of regular moderate physical activity is generally lowest in SA adults.10,137 A low-level of physical activity is independently associated with prediabetes and T2DM, obesity, and increased rate of death from CHD.138, 139, 140 Expectedly, regular moderate- or high-intensity exercise was protective for SAs in the setting of a first time acute MI in the INTERHEART study.8
Barriers to physical activity are variable and may be particular to a religion, gender, or generation. Low awareness of the benefits of physical activity, cultural gender norms (eg, modesty, healthy body weight perceptions), language barriers (poor English fluency), structural barriers (gender-segregation), perceived harm thresholds, career commitments, racial discrimination (institutional and personal), low levels of acculturation, communication gaps with health care professionals, and low self-efficacy have been cited as reasons for lower physical activity rates among SAs.141, 142, 143, 144 Women are more likely to be sedentary compared to men, attributed to cultural expectations (restricted participation in some religious and ethnic groups; household responsibilities, child care, and supporting extended family members, for example).145
For all American adults, a minimum of 150 minutes of moderate-intensity exercise per week is recommended.79 Concerted efforts are needed to raise awareness of the benefits of physical activity and encourage culturally sensitive interventions via social networks and cultural/religious organizations.80,146,147 Interventions aimed at increasing neighborhood social cohesion, engaging community leaders, using community-based participation tailored to beliefs and norms, gender-specific measures and programs, encouraging youth sports participation, and culturally specific activities (Bollywood dancing and Bhangra, for example), may be effective measures to influence physical activity in immigrants and subsequent generations of SAs.98,148, 149, 150, 151, 152, 153 Other specific cultural considerations for lifestyle modification are currently being explored; the SAHELI (South Asian Healthy Lifestyle Initiative) is a culturally targeted, community-based intervention designed to test the impact of lifestyle intervention to reduce the risk of CHD and T2D in SAs.154,155
Tobacco
The prevalence of tobacco use among American SAs is lower compared with other racial/ethnic groups, including other Asian ethnic groups.156,157 For example, the prevalence of current smoking was 12.4% among Filipinos, 5.9% among Chinese, and 18.5% among NHW compared with 5.1% among Asian Indians.59,158 In the MASALA study (with majority first-generation immigrants), 5% of men and 1% of women were current smokers. Commonly used questionnaires used to assess tobacco use typically do not capture cultural forms of tobacco, and therefore the prevalence of regular use of these products among SAs is not well understood and may be underestimated.159
In addition to combustible cigarette use, there are other forms of tobacco use specific to SA culture including smokeless (gutkha, naswar, paan, paan masala, zarda) and smoked products (bidi, hookah, shisha, chilam).160,161 Asking product-specific questions revealed high rates of alternative tobacco use in a New York City study among Bangladeshi and Gujurati adults.162 Tobacco use patterns may differ by gender as men were more likely to smoke while women were more likely to chew tobacco.163 SAs place emphasis on using culturally specific tobacco products during celebrations and social functions as a tribute to their heritage and a means of hospitality.161,164 There may also be inaccuracies in perceptions of the health effects and potential harms of tobacco products, which can further complicate their use.164
The prevalence of tobacco use may also differ among first generation compared with later generations. For example, among SA immigrants in the Northeast U.S., nearly half of female cigarette smokers were first-generation immigrants.165 Clinicians and public health officials should address the use and cardiovascular effects of these products using cultural-specific messaging. Available Center for Disease Control Asian-centric resources for smoking cessation are offered in non-South Asian languages.166 This is similar to other national anti-tobacco organizations.167 Pharmacotherapy and behavioral interventions to aid tobacco cessation should be offered to help curb use of these products, in line with national consensus recommendations.75
Nontraditional risk factors
Family history
Family history of premature ASCVD (FamHx) (traditionally defined as age <55 for men and <65 for women) is a non-modifiable, established risk factor, that carries a temporal relationship for the development of future ASCVD (larger influence of shared, genetic component for premature events, and a more balanced contribution of environmental and acquired CVD risk factors for later onset events).168 Observational data suggest that the prevalence of FamHx in SAs ranges between 40% to 60%.5,169, 170, 171 The presence of a FamHx is associated with CHD, OR ranging from 1.45 (95% CI: 1.30-1.60) to 1.71 (95% CI: 1.21-2.42), depending on the study population and self-reported definition used.5,170,172 However, this is similar to other racial/ethnic groups.169 A one-time screening Lp(a) value in the presence of a FamHx may be useful to help further stratify ASCVD risk.88,173 A positive FamHx should promote a screening lipid panel for familial lipid disorders in adults older than age 20.82
Markers of inflammation
Inflammation is an important pathophysiological mechanism responsible for the initiation and progression of atherothrombosis.174 C-reactive protein is a marker of systemic inflammation that is typically elevated in Asian Indians compared with Whites and is associated with traditional risk factors and prevalent CVD.175,176 Other inflammatory biomarkers and adipocytokines of potential significance include homocysteine, tumor necrosis factor-α, leptin, and adiponectin. Plasma homocysteine levels are elevated among Asian Indians as compared with Whites and are associated with increased ASCVD risk.177 Dietary cobalamin deficiency is a plausible mechanism underlying homocysteinemia in this population although supplementation with vitamins B12, B6, and folic acid did not decrease the risk of CVD in the HOPE (Heart Outcomes Prevention Evaluation) 2 trial.178,179
The association of tumor necrosis factor-α, leptin, and adiponectin with cardiovascular risk among SAs remains to be studied. Alternatively, high-sensitivity C-reactive protein, tumor necrosis factor-α, leptin, and adiponectin were not associated with subclinical atherosclerosis as measured by CAC score in small studies highlighting a potential divergence in the pathophysiological role of inflammation and subclinical coronary atherosclerosis among SAs.180 Studies directly comparing risk estimation of markers of inflammation and CAC scoring in other racial/ethnic groups have reported the superiority of CAC in estimating future coronary disease events.181, 182, 183
Maternal risk factors
Adverse pregnancy outcomes are related to an increased risk for ASCVD. Gestational diabetes mellitus (GDM) is a particularly important risk factor for ASCVD among SA American adults.184 Compared with NHW, non-Hispanic Black, Hispanic, and other Asian groups, nulliparous SA (Asian Indian) American women at first live birth experienced the highest rate of GDM in 2019 (129.1 per 1,000 live births), with a significant 4.4% per year increase in GDM rates between 2011 and 2019.185 Between 2014 and 2019, GDM rates were higher among Asian Indian women born outside the United States (122.7 per 1,000 live births) compared with those born in the United States (75.5 per 1,000 live births).186 SA American women in the MASALA study who reported a history of GDM had 3.2 times higher odds of having T2D, compared with women without GDM.187 Given the disproportionate burden of GDM experienced in SA American women, the American College of Obstetrics and Gynecology recommends screening for GDM early in pregnancy for SA (and other Asian American) women.90 GDM is known to have consequences for both the mother and offspring, although the available data are generally not from South Asian populations. GDM increases the risk of subsequent ASCVD in midlife188 and also increases the risk for premature ASCVD in the offspring.189 Confirming these findings and quantifying the magnitude of risk conferred among SA women remains to be evaluated.
Hypertensive disorders of pregnancy (HDP), which include pregnancy-induced hypertension and preeclampsia, are another important adverse pregnancy outcome that increases risk for ASCVD. In 2019, HDP rates among nulliparous Asian Indian women at first live birth were 54.1 per 1,000 live births, and HDP rates increased on average 9.0% per year between 2011 and 2019.190 HDP rates were higher among Asian Indian women born inside the United States (64.4 per 1,000 live births), compared with Asian Indian women born outside the United States (52.9 per 1,000 live births).186
While HDP is associated with a higher risk of subsequent premature mortality among other populations in the United States,191 the role of HDP and several other adverse pregnancy outcomes on the risk for ASCVD in SA American adults remains to be characterized. Differences in adverse pregnancy outcomes including GDM and HDP in subgroups of SA Americans (eg, Pakistani, Bangladeshi) have not been evaluated to date.
Barriers to accessing health care
As the SA population in the United States grows, public health strategies must adapt to meet their needs.192 Identifying a racial group as “high risk” may serve to improve and/or provide health care resources to vulnerable populations, but also has the potential to thwart health-seeking behavior, engagement in care, and adherence to therapy.193 Furthermore, it does not account for disparities in care provision and process, socioeconomic position, neighborhood environment, sociocultural factors, and racial discrimination.2,194 Specific health challenges that impact cardiovascular health in SA and proposed opportunities to overcome these barriers are listed in Table 2.
Table 2.
Barriers and Opportunities to Improve Cardiovascular Health in South Asian Adults
| Barriers | Comments |
|---|---|
| Racial and cultural discrimination195,196 | |
| Existing cultural attitudes regarding health care | |
| Acculturation |
|
| Socioeconomic status |
|
| Health literacy | |
| Geography - distance from healthcare center, extended wait times, child care responsibilities, and lack of access to transportation |
|
| Language207,208 |
|
| Health care practices do not align with modern Western or allopathic medicine |
|
| Opportunities | Comments |
|---|---|
| Culturally sensitive educational materials |
|
| Language/Health literacy |
|
| Engagement of cultural/religious organizations and social networks. | |
| Cultural competency |
|
| Disaggregation of health data |
|
MASALA = Mediators of Atherosclerosis in South Asians Living in America; SA = South Asians.
ASCVD risk management considerations for South Asians are depicted in the Central Illustration and described in Table 1.
Central Illustration.
Primary Prevention Cardiovascular Risk Assessment and Management Considerations for the South Asian Populations in the United States
∗Data available mostly for Asian Indian adults.
Risk assessment
Risk assessment is fundamental for ASCVD risk reduction counseling. However, risk prediction, discrimination, and calibration in SA adults remain challenging for the following reasons: 1) available guidelines recommended risk algorithms have not been derived from or prospectively validated in SA adults; 2) limited considerations have been given for native vs migrant populations; and 3) there is paucity of disaggregated data, which masks meaningful ASCVD health differences in SA subgroups. As such, available population-specific risk assessment tools unreliably estimate risk in SA at large and among subgroups5,17,27,214, 215, 216, 217, 218, 219, 220, 221 (Table 3).
Table 3.
Select Risk Assessment Calculators and Guideline Considerations Specific to South Asian Adults
| Risk Calculator | Population, Country | Number of South Asians in Derivation Cohort (%) | Guideline | Guideline Commentsa |
|---|---|---|---|---|
| Pooled cohort equations (PCE)222 | Pooled dataset of cohort studies, USA | 0% |
|
|
| Systematic COronary Risk Evaluation (SCORE)224 | Pooled dataset of cohort studies, Europe | 0% |
|
|
| Framingham Risk Score (FRS)227 | Population cohort, USA | 0% |
|
|
| Modified FRS230 | Population cohort, USA | 0% |
|
|
| QRISK231 | Electronic medical database, UK | 0% |
|
|
| QRISK Lifetime/3rd Joint British Societies’ (JBS3) Risk Calculator27,232 | Electronic medical database, UK | 2.3% 0.3% Bangladeshi; 1.0% Indian; 0.5% Pakistani; 0.5% Other Asian |
|
|
| QRISK2233 | Electronic medical database, UK | 1.11% 0.16% Bangladeshi (0.26% Women, 0.17% Men); 0.48% Indian (0.47% Women, 0.48% Men); 0.26% Pakistani (0.26% Women, 0.27% Men); 0.21% Other Asian (0.16% Women, 0.19% Men) |
|
|
| QRISK3234 | Electronic medical database, UK | 5.25% 0.9% Bangladeshi (0.8% Women, 1.1% Men); 2.0% Indian (1.9% Women, 2.1% Men); 1.1% Pakistani (1.0% Women, 1.2% Men); 1.25% Other Asian (1.3% Women, 1.2% Men) |
|
|
| PREDICT30 | Electronic medical database, New Zealand | “Indian”: 9% (5% Women, 4% Men) |
|
|
| INTERHEART Modifiable Risk Score236 | Cases of MI, age (±5 y), and sex-matched control, 52 countries | 14% |
|
|
| NORRISK2237 | Population-based survey cohort, Norway | 0% |
|
|
| NORRISK2-SADia238 | Updated NORRISK2; Population-based survey cohort, Norway. | 12% South Asian (5% Women, 7% Men) |
|
|
| ETHRISK239 | Recalibrated FRS, using 2 community-based surveys, UK. | 46% 11% Bangladeshi; 20% Indian; 15% Pakistani |
|
|
| UK Prospective Diabetes Study (UKPDS)240 | Population Cohort, UK | “Asian-Indian”: 10% (3% Women, 7% Men) |
|
|
ACC = American College of Cardiology; AHA = American Heart Association; CVD = cardiovascular disease; EAS = European Atherosclerosis Society; ESC = European Society of Cardiology; FRS = Framingham Risk Score; MI = myocardial infarction; N/A = not applicable; NICE = National for Health and Clinical Excellence; UK = United Kingdom; USA = United States of America; WHO = World Health Organization.
If applicable.
For example, the National Institute for Health and Care Excellence (NICE) guidelines recommended a crude adjustment factor to the Framingham Risk Score (FRS) for SAs (FRS multiplied by 1.4 for men; no recommendation for women).241 The FRS and UK Prospective Diabetes Study underestimates risk in SAs compared to a White European population.240 QRISK2 underestimates risk in SA women.233 The 3rd Joint British Societies' CVD risk calculator accounts for SA ethnicity; however, underestimates risk considering the small proportion (2.3%) of SA adults included in the cohort.232
QRISK3 (5.25% SAs), ETHRISK (46% SAs), NORRISK-2 SADia (12% SAs) are not yet incorporated into any national guidelines.238,239 The 2019 WHO risk charts (estimates risk in Bangladesh, Bhutan, India, Nepal, and Pakistan) misclassify higher-risk SAs to low-risk categories.242 The INTERHEART Modifiable Risk-Score has been internally and externally validated for the prediction of future ASCVD risk in SAs; however, its application is limited considering case-control data used to develop the risk calculator.236
The 2013 AHA/ACC PCE recommend using “White” race for SA adults, resulting in risk underestimation.17,222 The 2016 European Prevention guidelines and 2018 American Blood Cholesterol guidelines introduced SA ethnicity as an ‘ASCVD risk-enhancer’ when considering the initiation of statin therapy.82,243 However, substantial variability exists in the CVD prevalence, incidence, risk, and health-seeking behavior among SA subgroups.6,25,29,244, 245, 246 Studies conducted among SAs in Europe highlight an overall increased CVD risk among SAs, but also demonstrate heterogeneity of risk by country of origin, generation of immigration, and acculturation.98 While European observations appear to mirror those observed in SAs residing within the United States, additional studies are imperative to filling in knowledge gaps that exist within this group.
Coronary artery calcium
Considering unreliable ASCVD-risk estimation methods and the absence of a validated SA-specific risk calculator, the use of CAC may be a useful test to improve risk stratification and guide primary preventive efforts.17 CAC testing is a cost-effective, highly reproducible, and specific marker of subclinical atherosclerosis.247
SA men and women with a 10-year predicted risk of >7.5% by the PCE were found to have a high CAC burden.59 Although formal validation is required, the PCE may adequately predict risk among SAs at low risk and high risk (<5% and >20%).248 However, the extent of ASCVD-risk overestimation using the PCE was greater among SA adults considered at low- and intermediate-risk compared to among NHWs.17 For example, intermediate-risk SA have a 73% higher odds of CAC = 0 (low short-term risk strata) compared to NHWs (95% CI: 1.00, 2.99). When considering SA ethnicity as a ‘risk-enhancing factor’ according to the 2018 AHA/ACC Blood Cholesterol Guidelines (ie, systemic statin pharmacotherapy considerations for borderline and intermediate risk SA adults), an absence of CAC (CAC = 0) was found in 54% and 30% of participants at borderline risk and intermediate risk, respectively.82,248
Advanced coronary artery calcium measures: beyond the Agatston score
Advanced CAC measures such as vessel involvement, density, and volume in SAs are summarized in Table 4.169,170,248, 249, 250, 251, 252, 253 Overall, ASCVD event data are required to confirm the importance of these findings.254, 255, 256, 257, 258
Table 4.
Summary of Advanced Measures of CAC in South Asian Adults
| Author | Study | Main Finding(s) |
|---|---|---|
| Kanaya et al109 | MASALA, MESA |
|
| Al Rifai et al254 | MASALA, MESA |
|
| Roos et al250 | Observational Cohort |
|
| Al Rifai et al249 | MASALA |
|
| Kanaya et al264 | MASALA, MESA |
|
| Bhatia et al255 | MASALA |
|
| Patel et al169 | MASALA, MESA |
|
| Wang et al170 | SABRE |
|
CAC = coronary artery calcium; CI = confidence interval; FamHx = family history of CHD; HOMA-IR = homeostatic model assessment for insulin resistance; MASALA = Mediators of Atherosclerosis in South Asians Living in America;NHW = non-Hispanic White; OR = odds ratio; PCE = pooled cohort equations; SABRE = South Hall and Brent Revisited study; T2D = type 2 diabetes.
Coronary artery calcium for personalizing preventive therapies
Coronary artery calcium (CAC) scoring may also guide safe allocation of other preventive pharmacotherapies. Considering the 2017 ACC/AHA Blood Pressure guideline, CAC scoring may help identify those SA adults who would best qualify for aggressive lifestyle optimization and antihypertensive pharmacotherapy.69,70 For example, the proportion of SA participants that would qualify for antihypertensive pharmacotherapy per the ACC/AHA, but not by JNC7 guidelines, was higher among those with CAC >100.70 In other racial/ethnic groups, CAC imaging has demonstrated the potential to inform the intensification of blood pressure management.259, 260, 261 Considering a high prevalence of prediabetes (not an indication for statin therapy) in SA adults, the presence of CAC may also influence statin initiation; alternatively if CAC = 0, statin therapy may be deferred/avoided in lieu of ongoing prudent lifestyle interventions.88,248,262
Considering the interplay of TRF and CAC and risk of early ASCVD events, an emphasis on the simultaneous appraisal of TRF and CAC in SA may be of clinical importance.263 In adults ≤45 years old of other racial/ethnic groups, the presence of CAC increases with the number of TRF, OR: 4.5 (95% CI: 2.7-7.3), in patients with >3 vs 0 TRF.253 Notably, SAs and NHW men have similar CAC burden (men age 58 ± 9 years vs 63 ± 10 years) but higher CAC burden compared to other racial/ethnic groups (mean age 62 ± 10).109 SA men have similar rates of CAC progression to NHW (interscan time 4.8 ± 0.8 years).264 These data are consistent with other studies showing similar prevalence and severity of CAC between Asian Indians and Whites.265, 266, 267
Among those with CAC = 0 at baseline, the timing of repeat CAC scanning has not yet been defined specifically for SAs; however, a 3- to 5-year interval has been suggested for those at borderline or intermediate risk by the PCE, and 3 years for those with diabetes.268 Notably, among SA adults with no CAC at baseline in the MASALA study, the age-adjusted CAC incidence was 8.8% (95% CI, 6.8%-10.8%) in men and 3.6% (95% CI, 2.5%-4.8%) in women on repeat CAC measurement after 4.8 ± 0.8 years.264 Despite favorable outcome data in the absence of CAC,247 a potential limitation of the CAC score lies in its inability to detect the entire spectrum of plaque morphology and burden.269 Coronary computed tomography angiography (CCTA) can evaluate coronary anatomy, stenosis, and characterize atherosclerotic plaques beyond the ability of CAC. Among multiethnic, asymptomatic populations that did not include SA, the prevalence of noncalcified plaque by CCTA ranges between 5.5% and 16% in patients with no CAC (% participants CAC = 0, 23%-59%)269, 270, 271, 272 (NCT03920176). Although long-term outcome data are expected to confirm the clinical significance of these findings, a clinical practice statement from the American Society for Preventive Cardiology suggests judicious use of CCTA as an alternative to CAC in asymptomatic high-risk populations (eg, family history of premature ASCVD, familial hypercholesterolemia, diabetes, and those of SA descent with strong family history among others).273 Other major scientific societies have not embraced CCTA for ASCVD risk assessment in asymptomatic patients, highlighting the role of early and aggressive risk factor identification and management as a reasonable approach. This may be particularly applicable to those at the highest ASCVD risk, such as low-income, low-education, low rates of acculturation, and those with poor access to health care, for example.
In many of the aforementioned studies of CAC, the majority of SAs were Asian Indian (a lower-risk SA subgroup compared to other SA subpopulations such as Pakistani and Bangladesh, particularly those living in the United States), yielding caution to the widespread use of CAC for risk stratification until clinical outcome data are available.5 However, in other racial/ethnic groups, CAC is proven to improve ASCVD risk assessment, thereby serving as a guide for initiating or deferring preventive therapies.247 CAC scoring has shown promise with respect to further ASCVD risk refinement in SA adults as suggested by available consensus recommendations, particularly for Asian Indian adults.88,180,262
Conclusions
ASCVD risk among South Asian adults in North America is heterogeneous and must be individualized. Awareness and management of traditional risk factors remain essential. Available risk stratification tools have their limitations, however the use of clinical tools, including blood biomarkers and CAC, may help transcend these limitations and personalize care. The difference in risk factor profiles and CVD phenotypes, and contribution of genetic susceptibility, environmental influences, and health-related behavior to this observed heterogeneity will be available as the MASALA, MASALA-2G, and OurHealth studies advance.152,274,275 Further characterization of national and cultural heterogeneity, the effect of immigrant duration, ASCVD risk in second- and third-generation SA subgroups, the effect of ethnically mixed families on cardiovascular risk profiles, and coronary vasculature characteristics (ie, vessel dimensions and subclinical atherosclerosis assessment), for example, represent remaining knowledge gaps for immigrant SAs living in European countries that are equally applicable to North American SAs.79 Education for patients and the healthcare team at large on navigating cultural, religious, social, geographic, and economic barriers is essential to delivering high-quality care.72 From a health policy perspective,276 it is imperative that the health needs of this group are addressed to ensure culturally appropriate medical and health services as a means of mitigating cardiovascular risk in this higher risk population.
Funding support and author disclosures
Dr. Natarajan has received investigator-initiated grants from Amgen, Apple, AstraZeneca, Boston Scientific, and Novartis; personal fees from Apple, AstraZeneca, Blackstone Life Sciences, Foresite Labs, Novartis, Roche/Genentech; is a co-founder of TenSixteen Bio; is a scientific advisor board member of Esperion Therapeutics, geneXwell, and TenSixteen Bio; spousal employment at Vertex, all unrelated to the present work; and is supported by grants from NHLBI/NIH (R01HL142711, R01HL127564). Dr Shah is supported by grants from NHLBI (K23HL157766). Dr Kanaya is supported by grants from NHLBI/NIH (2K24HL112827, P30DK092924, 5P30DK098722). All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
Hicham Skali, MD, served as Guest Associate Editor for this paper. Michael Landzberg, MD, served as Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental tables, please see the online version of this paper.
Supplementary data
References
- 1.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mital R., Bayne J., Rodriguez F., Ovbiagele B., Bhatt D.L., Albert M.A. Race and ethnicity considerations in patients with coronary artery disease and stroke: JACC focus seminar 3/9. J Am Coll Cardiol. 2021;78(24):2483–2492. doi: 10.1016/j.jacc.2021.05.051. [DOI] [PubMed] [Google Scholar]
- 3.Shah N.S., Xi K., Kapphahn K.I., et al. Cardiovascular and cerebrovascular disease mortality in Asian American subgroups. Circ Cardiovasc Qual Outcomes. 2022;15(5):e008651. doi: 10.1161/CIRCOUTCOMES.121.008651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention . 2019. Health, United States Spotlight – Racial and Ethnic Disparities in Heart Disease. https://www.cdc.gov/nchs/hus/spotlight/HeartDiseaseSpotlight_2019_0404.pdf. [Google Scholar]
- 5.Patel A.P., Wang M., Kartoun U., Ng K., Khera A.V. Quantifying and understanding the higher risk of atherosclerotic cardiovascular disease among South Asian individuals: results from the UK Biobank prospective cohort study. Circulation. 2021;144(6):410–422. doi: 10.1161/CIRCULATIONAHA.120.052430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jose P.O., Frank A.T., Kapphahn K.I., et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64(23):2486–2494. doi: 10.1016/j.jacc.2014.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pursnani S., Merchant M. South Asian ethnicity as a risk factor for coronary heart disease. Atherosclerosis. 2020;315:126–130. doi: 10.1016/j.atherosclerosis.2020.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Joshi P., Islam S., Pais P., et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297(3):286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 9.Anand S.S., Yusuf S., Vuksan V., et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the study of health assessment and risk in ethnic groups (SHARE) Lancet. 2000;356(9226):279–284. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 10.Shah A.D., Kandula N.R., Lin F., et al. Less favorable body composition and adipokines in South Asians compared with other US ethnic groups: results from the MASALA and MESA studies. Int J Obes (Lond) 2016;40(4):639–645. doi: 10.1038/ijo.2015.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanaya A.M., Herrington D., Vittinghoff E., et al. Understanding the high prevalence of diabetes in U.S. South Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes Care. 2014;37(6):1621–1628. doi: 10.2337/dc13-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hastings K.G., Jose P.O., Kapphahn K.I., et al. Leading causes of death among Asian American subgroups (2003-2011) PLoS One. 2015;10(4):e0124341. doi: 10.1371/journal.pone.0124341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yusuf S., Reddy S., Ounpuu S., Anand S. Global burden of cardiovascular diseases: part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104(23):2855–2864. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 14.Kianoush S., Rifai M.A., Jain V., et al. Prevalence and predictors of premature coronary heart disease among Asians in the United States: a national health interview survey study. Curr Probl Cardiol. 2022:101152. doi: 10.1016/j.cpcardiol.2022.101152. [DOI] [PubMed] [Google Scholar]
- 15.Murray C.J.L., Lopez A.D. Harvard School of Public Health; 1996. Global Health Statistics, Global Burden of Disease and Injury Series. [Google Scholar]
- 16.Gany F., Palaniappan L., Prasad L., Acharya S., Leng J. South Asian health. From research to practice and policy: an overview. J Immigr Minor Health. 2019;21(Suppl 1):3–6. doi: 10.1007/s10903-017-0552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al Rifai M., Cainzos-Achirica M., Kanaya A.M., et al. Discordance between 10-year cardiovascular risk estimates using the ACC/AHA 2013 estimator and coronary artery calcium in individuals from 5 racial/ethnic groups: comparing MASALA and MESA. Atherosclerosis. 2018;279:122–129. doi: 10.1016/j.atherosclerosis.2018.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.United States Census Bureau. Measuring Race and Ethnicity Across the Decades: 1790–2010. https://www.census.gov/data-tools/demo/race/MREAD_1790_2010.html
- 19.Kennedy E. The immigration act of 1965. Ann Am Acad Polit Soc Sci. 1966;367:137–149. [Google Scholar]
- 20.Budiman A., Ruiz N.G. Pew Research Center; 2021. Key Facts about Asian Origin Groups in the U.S. [Google Scholar]
- 21.United States Census Bureau . 2022. National Population by Characteristics: 2010-2019. https://www.census.gov/data/tables/time-series/demo/popest/2010s-national-detail.html. [Google Scholar]
- 22.Marks R., Jones N. United States Census Bureau; 2020. Collecting and Tabulating Ethnicity and Race Responses in the 2020 Census. [Google Scholar]
- 23.Yusuf S., Hawken S., Ounpuu S., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 24.Yusuf S., Rangarajan S., Teo K., et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371(9):818–827. doi: 10.1056/NEJMoa1311890. [DOI] [PubMed] [Google Scholar]
- 25.Koirala B., Turkson-Ocran R.A., Baptiste D., et al. Heterogeneity of cardiovascular disease risk factors among Asian immigrants: insights from the 2010 to 2018 national health interview survey. J Am Heart Assoc. 2021;10(13):e020408. doi: 10.1161/JAHA.120.020408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tu J.V., Chu A., Rezai M.R., et al. The incidence of major cardiovascular events in immigrants to Ontario, Canada: the CANHEART immigrant study. Circulation. 2015;132(16):1549–1559. doi: 10.1161/CIRCULATIONAHA.115.015345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hippisley-Cox J., Coupland C., Robson J., Brindle P. Derivation, validation, and evaluation of a new QRISK model to estimate lifetime risk of cardiovascular disease: cohort study using QResearch database. BMJ. 2010;341:c6624. doi: 10.1136/bmj.c6624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhopal R., Unwin N., White M., et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ. 1999;319(7204):215–220. doi: 10.1136/bmj.319.7204.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Satish P., Vela E., Bilal U., et al. Burden of cardiovascular risk factors and disease in five Asian groups in Catalonia: a disaggregated, population-based analysis of 121 000 first-generation Asian immigrants. Eur J Prev Cardiol. 2022;29(6):916–924. doi: 10.1093/eurjpc/zwab074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pylypchuk R., Wells S., Kerr A., et al. Cardiovascular disease risk prediction equations in 400 000 primary care patients in New Zealand: a derivation and validation study. Lancet. 2018;391(10133):1897–1907. doi: 10.1016/S0140-6736(18)30664-0. [DOI] [PubMed] [Google Scholar]
- 31.Karthikeyan G., Teo K.K., Islam S., et al. Lipid profile, plasma apolipoproteins, and risk of a first myocardial infarction among Asians: an analysis from the INTERHEART study. J Am Coll Cardiol. 2009;53(3):244–253. doi: 10.1016/j.jacc.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 32.U.S. Preventive Services Task Force . 2013. Lipid Disorders in Adults (Cholesterol, Dyslipidemia): Screening. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening-2008. [Google Scholar]
- 33.Cheng Y.J., Kanaya A.M., Araneta M.R.G., et al. Prevalence of diabetes by race and ethnicity in the United States, 2011-2016. JAMA. 2019;322(24):2389–2398. doi: 10.1001/jama.2019.19365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gordon N.P., Lin T.Y., Rau J., Lo J.C. Aggregation of Asian-American subgroups masks meaningful differences in health and health risks among Asian ethnicities: an electronic health record based cohort study. BMC Public Health. 2019;19(1):1551. doi: 10.1186/s12889-019-7683-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beasley J.M., Ho J.C., Conderino S., et al. Diabetes and hypertension among South Asians in New York and Atlanta leveraging hospital electronic health records. Diabetol Metab Syndr. 2021;13(1):146. doi: 10.1186/s13098-021-00766-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gujral U.P., Pradeepa R., Weber M.B., Narayan K.M., Mohan V. Type 2 diabetes in South Asians: similarities and differences with white Caucasian and other populations. Ann N Y Acad Sci. 2013;1281:51–63. doi: 10.1111/j.1749-6632.2012.06838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zaninotto P., Mindell J., Hirani V. Prevalence of cardiovascular risk factors among ethnic groups: results from the health surveys for England. Atherosclerosis. 2007;195(1):e48–e57. doi: 10.1016/j.atherosclerosis.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 38.Shah N.S., Luncheon C., Kandula N.R., Cho P., Loustalot F., Fang J. Self-reported diabetes prevalence in Asian American subgroups: behavioral risk factor surveillance system, 2013-2019. J Gen Intern Med. 2022;37(8):1902–1909. doi: 10.1007/s11606-021-06909-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banerjee A.T., Shah B. One size does not fit all: diabetes prevalence among immigrants of the South Asian diaspora. J Immigr Minor Health. 2021;23(4):653–658. doi: 10.1007/s10903-020-01093-4. [DOI] [PubMed] [Google Scholar]
- 40.Xiao M., O'Neill C. Detection and management of diabetes in England: results from the health survey for England. Diabetes Ther. 2017;8(5):1163–1174. doi: 10.1007/s13300-017-0300-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krishnakumar A., Verma R., Chawla R., et al. Evaluating glycemic control in patients of South Asian origin with type 2 diabetes using a digital therapeutic platform: analysis of real-world data. J Med Internet Res. 2021;23(3):e17908. doi: 10.2196/17908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singh H., Cinnirella M., Bradley C. Support systems for and barriers to diabetes management in South Asians and Whites in the UK: qualitative study of patients' perspectives. BMJ Open. 2012;2(6):1–7. doi: 10.1136/bmjopen-2012-001459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kumar K., Greenfield S., Raza K., Gill P., Stack R. Understanding adherence-related beliefs about medicine amongst patients of South Asian origin with diabetes and cardiovascular disease patients: a qualitative synthesis. BMC Endocr Disord. 2016;16(1):24. doi: 10.1186/s12902-016-0103-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhatt R.H., Ingle S.M., Sackpraseuth A.J., et al. Differences in the age of diagnosis of diabetes in Asian American ethnic groups: the national health interview survey (NHIS) 2006-2018. J Asian Health. 2021;9 [Google Scholar]
- 45.Becerra M.B., Becerra B.J. Disparities in age at diabetes diagnosis among Asian Americans: implications for early preventive measures. Prev Chronic Dis. 2015;12:E146. doi: 10.5888/pcd12.150006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anand S.S., Tarnopolsky M.A., Rashid S., et al. Adipocyte hypertrophy, fatty liver and metabolic risk factors in South Asians: the molecular study of health and risk in ethnic groups (mol-SHARE) PLoS One. 2011;6(7):e22112. doi: 10.1371/journal.pone.0022112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Narayan K.M.V., Kanaya A.M. Why are South Asians prone to type 2 diabetes? A hypothesis based on underexplored pathways. Diabetologia. 2020;63(6):1103–1109. doi: 10.1007/s00125-020-05132-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jepson R., Harris F.M., Bowes A., Robertson R., Avan G., Sheikh A. Physical activity in South Asians: an in-depth qualitative study to explore motivations and facilitators. PLoS One. 2012;7(10):e45333. doi: 10.1371/journal.pone.0045333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gadgil M.D., Anderson C.A., Kandula N.R., Kanaya A.M. Dietary patterns are associated with metabolic risk factors in South Asians living in the United States. J Nutr. 2015;145(6):1211–1217. doi: 10.3945/jn.114.207753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thomas N., Grunnet L.G., Poulsen P., et al. Born with low birth weight in rural Southern India: what are the metabolic consequences 20 years later? Eur J Endocrinol. 2012;166(4):647–655. doi: 10.1530/EJE-11-0870. [DOI] [PubMed] [Google Scholar]
- 51.Kalhan R., Puthawala K., Agarwal S., Amini S.B., Kalhan S.C. Altered lipid profile, leptin, insulin, and anthropometry in offspring of South Asian immigrants in the United States. Metabolism. 2001;50(10):1197–1202. doi: 10.1053/meta.2001.26704. [DOI] [PubMed] [Google Scholar]
- 52.Martin M., Palaniappan L.P., Kwan A.C., Reaven G.M., Reaven P.D. Ethnic differences in the relationship between adiponectin and insulin sensitivity in South Asian and Caucasian women. Diabetes Care. 2008;31(4):798–801. doi: 10.2337/dc07-1781. [DOI] [PubMed] [Google Scholar]
- 53.Patel S.A., Shivashankar R., Ali M.K., et al. Is the “South Asian phenotype” unique to South Asians?: comparing cardiometabolic risk factors in the CARRS and NHANES studies. Glob Heart. 2016;11(1):89–96.e83. doi: 10.1016/j.gheart.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hanif W., Ali S.N., Bellary S., et al. Pharmacological management of South Asians with type 2 diabetes: consensus recommendations from the South Asian Health Foundation. Diabet Med. 2021;38(4):e14497. doi: 10.1111/dme.14497. [DOI] [PubMed] [Google Scholar]
- 55.Misra A. Ethnic-specific criteria for classification of body mass index: a perspective for Asian Indians and American Diabetes Association position statement. Diabetes Technol Ther. 2015;17(9):667–671. doi: 10.1089/dia.2015.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Consultation W.E. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 57.Committee ADAPP 3. Prevention or delay of type 2 diabetes and associated comorbidities: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S39–S45. doi: 10.2337/dc22-S003. [DOI] [PubMed] [Google Scholar]
- 58.National Institute for Health and Care Excellence (NICE) Citation: Surveillance report 2018 - Obesity: identification, assessment and management (2014) NICE guideline CG189 and BMI: preventing ill health and premature death in black, Asian and other minority ethnic groups (2013) NICE guideline PH46 [Internet] National Institute for Health and Care Excellence (NICE); London: 2018 May 24. https://www.ncbi.nlm.nih.gov/books/NBK550939/ [PubMed] [Google Scholar]
- 59.Kandula N.R., Kanaya A.M., Liu K., et al. Association of 10-year and lifetime predicted cardiovascular disease risk with subclinical atherosclerosis in South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Am Heart Assoc. 2014;3(5):e001117. doi: 10.1161/JAHA.114.001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yi S.S., Thorpe L.E., Zanowiak J.M., Trinh-Shevrin C., Islam N.S. Clinical characteristics and lifestyle behaviors in a population-based sample of Chinese and South Asian immigrants with hypertension. Am J Hypertens. 2016;29(8):941–947. doi: 10.1093/ajh/hpw014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fei K., Rodriguez-Lopez J.S., Ramos M., et al. Racial and ethnic subgroup disparities in hypertension prevalence, New York city health and nutrition examination survey, 2013-2014. Prev Chronic Dis. 2017;14:E33. doi: 10.5888/pcd14.160478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Neupane D., McLachlan C.S., Sharma R., et al. Prevalence of hypertension in member countries of South Asian Association for Regional Cooperation (SAARC): systematic review and meta-analysis. Medicine (Baltimore) 2014;93(13):e74. doi: 10.1097/MD.0000000000000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Commodore-Mensah Y., Selvin E., Aboagye J., et al. Hypertension, overweight/obesity, and diabetes among immigrants in the United States: an analysis of the 2010-2016 national health interview survey. BMC Public Health. 2018;18(1):773. doi: 10.1186/s12889-018-5683-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pais P., Pogue J., Gerstein H., et al. Risk factors for acute myocardial infarction in Indians: a case-control study. Lancet. 1996;348(9024):358–363. doi: 10.1016/s0140-6736(96)02507-x. [DOI] [PubMed] [Google Scholar]
- 65.Eastwood S.V., Tillin T., Chaturvedi N., Hughes A.D. Ethnic differences in associations between blood pressure and stroke in South Asian and European men. Hypertension. 2015;66(3):481–488. doi: 10.1161/HYPERTENSIONAHA.115.05672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Major R.W., Davies M.J., Crasto W., Gray L.J., Webb D.R., Khunti K. Association between undiagnosed hypertension and microalbuminuria in South Asians without known diabetes. J Hum Hypertens. 2015;29(3):185–189. doi: 10.1038/jhh.2014.62. [DOI] [PubMed] [Google Scholar]
- 67.van der Linden E.L., Couwenhoven B.N., Beune E.J.A.J., Daams J.G., van den Born B.H., Agyemang C. Hypertension awareness, treatment and control among ethnic minority populations in Europe: a systematic review and meta-analysis. J Hypertens. 2021;39(2):202–213. doi: 10.1097/HJH.0000000000002651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu Q., Quan H., Chen G., Qian H., Khan N. Antihypertensive medication adherence and mortality according to ethnicity: a cohort study. Can J Cardiol. 2014;30(8):925–931. doi: 10.1016/j.cjca.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 69.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 70.Patel J., Mehta A., Rifai M.A., et al. Hypertension guidelines and coronary artery calcification among South Asians: results from MASALA and MESA. Am J Prev Cardiol. 2021;6:100158. doi: 10.1016/j.ajpc.2021.100158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Blood Pressure Association . 2009. Love Your Heart - A South Asian Guide to Controlling Your Blood Pressure. https://www.bloodpressureuk.org/media/bpuk/docs/SouthAsian-(1).pdf. [Google Scholar]
- 72.American College of Cardiology . 2022. New ACC Health Equity Series Kicks Off With South Asian Cardiovascular Health Discussion. [Google Scholar]
- 73.Gujral U.P., Prabhakaran D., Pradeepa R., et al. Isolated HbA1c identifies a different subgroup of individuals with type 2 diabetes compared to fasting or post-challenge glucose in Asian Indians: the CARRS and MASALA studies. Diabetes Res Clin Pract. 2019;153:93–102. doi: 10.1016/j.diabres.2019.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gujral U.P., Vittinghoff E., Mongraw-Chaffin M., et al. Cardiometabolic abnormalities among normal-weight persons from five racial/ethnic groups in the united states: a cross-sectional analysis of two cohort studies. Ann Intern Med. 2017;166(9):628–636. doi: 10.7326/M16-1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Barua R.S., Rigotti N.A., Benowitz N.L., et al. 2018 ACC expert consensus decision pathway on tobacco cessation treatment: a report of the American College of Cardiology Task Force on clinical expert consensus documents. J Am Coll Cardiol. 2018;72(25):3332–3365. doi: 10.1016/j.jacc.2018.10.027. [DOI] [PubMed] [Google Scholar]
- 76.Centers for Disease Control and Prevention . 2021. Clinical Cessation Tools. [Google Scholar]
- 77.American Diabetes Association Professional Practice Committee 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17–S38. doi: 10.2337/dc22-S002. [DOI] [PubMed] [Google Scholar]
- 78.Garvey W.T., Mechanick J.I., Brett E.M., et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22 Suppl 3:1–203. doi: 10.4158/EP161365.GL. [DOI] [PubMed] [Google Scholar]
- 79.Piercy K.L., Troiano R.P. Physical activity guidelines for Americans from the US Department of Health and Human Services. Circ Cardiovasc Qual Outcomes. 2018;11(11):e005263. doi: 10.1161/CIRCOUTCOMES.118.005263. [DOI] [PubMed] [Google Scholar]
- 80.Thanawala M.S., Siddique J., Schneider J.A., et al. Association of social networks and physical activity in South Asians: the Mediators of Atherosclerosis in South Asians Living in America Cohort study. J Phys Act Health. 2020;17(2):149–155. doi: 10.1123/jpah.2019-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Paluch A.E., Gabriel K.P., Fulton J.E., et al. Steps per day and all-cause mortality in middle-aged adults in the coronary artery risk development in young adults study. JAMA Netw Open. 2021;4(9):e2124516. doi: 10.1001/jamanetworkopen.2021.24516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grundy S.M., Stone N.J., Bailey A.L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2019;73(24):e285–e350. doi: 10.1016/j.jacc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 83.National Lipid Association. Heart-Healthy Eating South Asian/Indian Style. May 2021. https://www.lipid.org/sites/default/files/heart-healthy_eating_south_asian.pdf
- 84.Heart and Stroke Foundation. Healthy Eating for South Asians. https://www.heartandstroke.ca/-/media/pdf-files/canada/south-asian-resources/366_southasianheathyeating_single.ashx
- 85.Bhupathiraju S.N., Sawicki C.M., Goon S., et al. A healthy plant-based diet is favorably associated with cardiometabolic risk factors among participants of South Asian ancestry. Am J Clin Nutr. 2022;116(4):1078–1090. doi: 10.1093/ajcn/nqac174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Heart UK The Cholestrol Charity. South Asian Diets and Cholesterol.
- 87.Abdool M., Khunti K., Seidu S. Healthy eating resources for South Asians. Diabetes Prim Care. 2018;20:139–141. [Google Scholar]
- 88.Kalra D., Vijayaraghavan K., Sikand G., et al. Prevention of atherosclerotic cardiovascular disease in South Asians in the US: a clinical perspective from the National Lipid Association. J Clin Lipidol. 2021;15(3):402–422. doi: 10.1016/j.jacl.2021.03.007. [DOI] [PubMed] [Google Scholar]
- 89.Jacobson T.A., Maki K.C., Orringer C.E., et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9(6 Suppl):S1–S122.e1. doi: 10.1016/j.jacl.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 90.ACOG Practice Bulletin No. 190: gestational diabetes mellitus. Obstet Gynecol. 2018;131(2):e49–e64. doi: 10.1097/AOG.0000000000002501. [DOI] [PubMed] [Google Scholar]
- 91.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):2199–2269. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 92.National Institute for Health and Care Excellence . 2015. Diabetes in Pregnancy: Management From Preconception to the Postnatal Period. [PubMed] [Google Scholar]
- 93.Hecht H., Blaha M.J., Berman D.S., et al. Clinical indications for coronary artery calcium scoring in asymptomatic patients: expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2017;11(2):157–168. doi: 10.1016/j.jcct.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 94.Kulkarni A., John Mancini G.B., Deedwania P.C., Patel J. 2021. South Asian Cardiovascular Health: Lessons Learned From the National Lipid Association Scientific Statement. https://www.acc.org/latest-in-cardiology/articles/2021/08/02/14/16/south-asian-cardiovascular-health. [Google Scholar]
- 95.Bilen O., Kamal A., Virani S.S. Lipoprotein abnormalities in South Asians and its association with cardiovascular disease: current state and future directions. World J Cardiol. 2016;8(3):247–257. doi: 10.4330/wjc.v8.i3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Enas E.A., Garg A., Davidson M.A., Nair V.M., Huet B.A., Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J. 1996;48(4):343–353. [PubMed] [Google Scholar]
- 97.Bhalodkar N.C., Blum S., Rana T., et al. Comparison of levels of large and small high-density lipoprotein cholesterol in Asian Indian men compared with Caucasian men in the Framingham Offspring Study. Am J Cardiol. 2004;94(12):1561–1563. doi: 10.1016/j.amjcard.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 98.Cainzos-Achirica M., Fedeli U., Sattar N., et al. Epidemiology, risk factors, and opportunities for prevention of cardiovascular disease in individuals of South Asian ethnicity living in Europe. Atherosclerosis. 2019;286:105–113. doi: 10.1016/j.atherosclerosis.2019.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Menon A.S., Kotwal N., Singh Y., Girish R. Statins: cholesterol guidelines and Indian perspective. Indian J Endocrinol Metab. 2015;19(5):546–553. doi: 10.4103/2230-8210.163105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Smith J., Cianflone K., Al-Amri M., Sniderman A. Body composition and the apoB/apoA-I ratio in migrant Asian Indians and White Caucasians in Canada. Clin Sci (Lond) 2006;111(3):201–207. doi: 10.1042/CS20060045. [DOI] [PubMed] [Google Scholar]
- 101.Frank A.T., Zhao B., Jose P.O., Azar K.M., Fortmann S.P., Palaniappan L.P. Racial/ethnic differences in dyslipidemia patterns. Circulation. 2014;129(5):570–579. doi: 10.1161/CIRCULATIONAHA.113.005757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bakker L.E., Boon M.R., Annema W., et al. HDL functionality in South Asians as compared to White Caucasians. Nutr Metab Cardiovasc Dis. 2016;26(8):697–705. doi: 10.1016/j.numecd.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 103.Dodani S., Dong L., Guirgis F.W., Reddy S.T. Carotid intima media thickness and low high-density lipoprotein (HDL) in South Asian immigrants: could dysfunctional HDL be the missing link? Arch Med Sci. 2014;10(5):870–879. doi: 10.5114/aoms.2014.46208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tsimikas S., Fazio S., Ferdinand K.C., et al. NHLBI Working Group recommendations to reduce lipoprotein(a)-mediated risk of cardiovascular disease and aortic stenosis. J Am Coll Cardiol. 2018;71(2):177–192. doi: 10.1016/j.jacc.2017.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mehta A., Jain V., Saeed A., et al. Lipoprotein(a) and ethnicities. Atherosclerosis. 2022;349:42–52. doi: 10.1016/j.atherosclerosis.2022.04.005. [DOI] [PubMed] [Google Scholar]
- 106.Paré G., Çaku A., McQueen M., et al. Lipoprotein(a) levels and the risk of myocardial infarction among 7 ethnic groups. Circulation. 2019;139(12):1472–1482. doi: 10.1161/CIRCULATIONAHA.118.034311. [DOI] [PubMed] [Google Scholar]
- 107.Huffman M.D., Kandula N.R., Baldridge A.S., Tsai M.Y., Prabhakaran D., Kanaya A.M. Evaluating the potential association between lipoprotein(a) and atherosclerosis (from the Mediators of Atherosclerosis among South Asians Living in America Cohort) Am J Cardiol. 2019;123(6):919–921. doi: 10.1016/j.amjcard.2018.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Makshood M., Joshi P.H., Kanaya A.M., et al. Lipoprotein (a) and aortic valve calcium in South Asians compared to other race/ethnic groups. Atherosclerosis. 2020;313:14–19. doi: 10.1016/j.atherosclerosis.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kanaya A.M., Kandula N.R., Ewing S.K., et al. Comparing coronary artery calcium among U.S. South Asians with four racial/ethnic groups: the MASALA and MESA studies. Atherosclerosis. 2014;234(1):102–107. doi: 10.1016/j.atherosclerosis.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Reddy N.K., Kaushal V., Kanaya A.M., Kandula N.R., Gujral U.P., Shah N.S. Cardiovascular risk factor profiles in North and South Indian and Pakistani Americans: the MASALA study. Am Heart J. 2022;244:14–18. doi: 10.1016/j.ahj.2021.10.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kulkarni K.R., Markovitz J.H., Nanda N.C., Segrest J.P. Increased prevalence of smaller and denser LDL particles in Asian Indians. Arterioscler Thromb Vasc Biol. 1999;19(11):2749–2755. doi: 10.1161/01.atv.19.11.2749. [DOI] [PubMed] [Google Scholar]
- 112.Wolf R.M., Nagpal M., Magge S.N. Diabetes and cardiometabolic risk in South Asian youth: a review. Pediatr Diabetes. 2021;22(1):52–66. doi: 10.1111/pedi.13078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lauderdale D.S., Rathouz P.J. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int J Obes Relat Metab Disord. 2000;24(9):1188–1194. doi: 10.1038/sj.ijo.0801365. [DOI] [PubMed] [Google Scholar]
- 114.Ye J.R.G., Baltrus P., Daniels E. Cardiovascular risk factors among Asian Americans: results from a national health survey. Ann Epidemiol. 2009;19(10):718–723. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lear S.A., Humphries K.H., Kohli S., Chockalingam A., Frohlich J.J., Birmingham C.L. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT) Am J Clin Nutr. 2007;86(2):353–359. doi: 10.1093/ajcn/86.2.353. [DOI] [PubMed] [Google Scholar]
- 116.Patel S., Bhopal R., Unwin N., White M., Alberti K.G., Yallop J. Mismatch between perceived and actual overweight in diabetic and non-diabetic populations: a comparative study of South Asian and European women. J Epidemiol Community Health. 2001;55(5):332–333. doi: 10.1136/jech.55.5.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tang J.W., Mason M., Kushner R.F., Tirodkar M.A., Khurana N., Kandula N.R. South Asian American perspectives on overweight, obesity, and the relationship between weight and health. Prev Chronic Dis. 2012;9:E107. doi: 10.5888/pcd9.110284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Roshania R., Narayan K.M., Oza-Frank R. Age at arrival and risk of obesity among US immigrants. Obesity (Silver Spring) 2008;16(12):2669–2675. doi: 10.1038/oby.2008.425. [DOI] [PubMed] [Google Scholar]
- 119.Bharmal N., Kaplan R.M., Shapiro M.F., et al. The association of duration of residence in the United States with cardiovascular disease risk factors among South Asian immigrants. J Immigr Minor Health. 2015;17(3):781–790. doi: 10.1007/s10903-013-9973-7. [DOI] [PubMed] [Google Scholar]
- 120.Sivasubramanian R., Malhotra S., Fitch A.K., Singhal V. Obesity and metabolic care of children of South Asian ethnicity in Western Society. Children (Basel) 2021;8(6):447. doi: 10.3390/children8060447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Balakrishnan R., Webster P., Sinclair D. Trends in overweight and obesity among 5-7-year-old White and South Asian children born between 1991 and 1999. J Public Health (Oxf) 2008;30(2):139–144. doi: 10.1093/pubmed/fdn013. [DOI] [PubMed] [Google Scholar]
- 122.Alberti K.G., Zimmet P., Shaw J., Group IETFC The metabolic syndrome–a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 123.Kalra D.K., Sikand G., Vijayaraghavan K., Guyton J.R. JCL roundtable: South Asian atherosclerotic risk. J Clin Lipidol. 2020;14(2):161–169. doi: 10.1016/j.jacl.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 124.LeCroy M.N., Stevens J. Dietary intake and habits of South Asian immigrants living in Western countries. Nutr Rev. 2017;75(6):391–404. doi: 10.1093/nutrit/nux023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gulati S., Misra A. Abdominal obesity and type 2 diabetes in Asian Indians: dietary strategies including edible oils, cooking practices and sugar intake. Eur J Clin Nutr. 2017;71(7):850–857. doi: 10.1038/ejcn.2017.92. [DOI] [PubMed] [Google Scholar]
- 126.Talegawkar S.A., Kandula N.R., Gadgil M.D., Desai D., Kanaya A.M. Dietary intakes among South Asian adults differ by length of residence in the USA. Public Health Nutr. 2016;19(2):348–355. doi: 10.1017/S1368980015001512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Holmboe-Ottesen G., Wandel M. Changes in dietary habits after migration and consequences for health: a focus on South Asians in Europe. Food Nutr Res. 2012;56:1–12. doi: 10.3402/fnr.v56i0.18891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kakde S., Bhopal R.S., Bhardwaj S., Misra A. Urbanized South Asians' susceptibility to coronary heart disease: the high-heat food preparation hypothesis. Nutrition. 2017;33:216–224. doi: 10.1016/j.nut.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 129.Gupta N., Shah P., Goel K., et al. Imbalanced dietary profile, anthropometry, and lipids in urban Asian Indian adolescents and young adults. J Am Coll Nutr. 2010;29(2):81–91. doi: 10.1080/07315724.2010.10719820. [DOI] [PubMed] [Google Scholar]
- 130.Singh P.N., Arthur K.N., Orlich M.J., et al. Global epidemiology of obesity, vegetarian dietary patterns, and noncommunicable disease in Asian Indians. Am J Clin Nutr. 2014;100 Suppl 1:359S–364S. doi: 10.3945/ajcn.113.071571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Jin Y., Kanaya A.M., Kandula N.R., Rodriguez L.A., Talegawkar S.A. Vegetarian diets are associated with selected cardiometabolic risk factors among middle-older aged South Asians in the United States. J Nutr. 2018;148(12):1954–1960. doi: 10.1093/jn/nxy217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Akhtar A.M., Ghouri N., Chahal C.A.A., et al. Ramadan fasting: recommendations for patients with cardiovascular disease. Heart. 2022;108(4):258–265. doi: 10.1136/heartjnl-2021-319273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Alper A.T., Akboğa M.K., Özcan K.S., et al. Recommendations for Ramadan fasting to patients with cardiovascular diseases; Turkish Society of Cardiology consensus report. Anatol J Cardiol. 2021;25(5):284–293. doi: 10.5152/AnatolJCardiol.2021.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mahmood A., Dar S., Dabhad A., Aksi B., Chowdhury T.A. Advising patients with existing conditions about fasting during Ramadan. BMJ. 2022;376:e063613. doi: 10.1136/bmj-2020-063613. [DOI] [PubMed] [Google Scholar]
- 135.Kassam-Khamis T., Judd P.A., Thomas J.E. Frequency of consumption and nutrient composition of composite dishes commonly consumed in the UK by South Asian Muslims originating from Bangladesh, Pakistan and East Africa (Ismailis) J Hum Nutr Diet. 2000;13(3):185–196. doi: 10.1046/j.1365-277x.2000.00230.x. [DOI] [PubMed] [Google Scholar]
- 136.Wagle A. 2014. Carbohydrate Counting for Traditional South Asian Foods. http://www.wsmclinic.com/formpdf/South-Asian-Carb-Counting-tool.pdf. [Google Scholar]
- 137.Bryan S.N., Tremblay M.S., Pérez C.E., Ardern C.I., Katzmarzyk P.T. Physical activity and ethnicity: evidence from the Canadian community health survey. Can J Public Health. 2006;97(4):271–276. doi: 10.1007/BF03405602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Shah A.D., Vittinghoff E., Kandula N.R., Srivastava S., Kanaya A.M. Correlates of prediabetes and type II diabetes in US South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Ann Epidemiol. 2015;25(2):77–83. doi: 10.1016/j.annepidem.2014.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hayes L., White M., Unwin N., et al. Patterns of physical activity and relationship with risk markers for cardiovascular disease and diabetes in Indian, Pakistani, Bangladeshi and European adults in a UK population. J Public Health Med. 2002;24(3):170–178. doi: 10.1093/pubmed/24.3.170. [DOI] [PubMed] [Google Scholar]
- 140.Chopra S.M., Misra A., Gulati S., Gupta R. Overweight, obesity and related non-communicable diseases in Asian Indian girls and women. Eur J Clin Nutr. 2013;67(7):688–696. doi: 10.1038/ejcn.2013.70. [DOI] [PubMed] [Google Scholar]
- 141.Daniel M., Wilbur J., Fogg L.F., Miller A.M. Correlates of lifestyle: physical activity among South Asian Indian immigrants. J Community Health Nurs. 2013;30(4):185–200. doi: 10.1080/07370016.2013.838482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kandula N.R., Tirodkar M.A., Lauderdale D.S., Khurana N.R., Makoul G., Baker D.W. Knowledge gaps and misconceptions about coronary heart disease among U.S. South Asians. Am J Prev Med. 2010;38(4):439–442. doi: 10.1016/j.amepre.2009.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Horne M., Skelton D., Speed S., Todd C. The influence of primary health care professionals in encouraging exercise and physical activity uptake among White and South Asian older adults: experiences of young older adults. Patient Educ Couns. 2010;78(1):97–103. doi: 10.1016/j.pec.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 144.Patel N., Ferrer H.B., Tyrer F., et al. Barriers and facilitators to healthy lifestyle changes in minority ethnic populations in the UK: a narrative review. J Racial Ethn Health Disparities. 2017;4(6):1107–1119. doi: 10.1007/s40615-016-0316-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ranasinghe C.D., Ranasinghe P., Jayawardena R., Misra A. Physical activity patterns among South-Asian adults: a systematic review. Int J Behav Nutr Phys Act. 2013;10:116. doi: 10.1186/1479-5868-10-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bharmal N.H., McCarthy W.J., Gadgil M.D., Kandula N.R., Kanaya A.M. The association of religious affiliation with overweight/obesity among South Asians: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Relig Health. 2018;57(1):33–46. doi: 10.1007/s10943-016-0290-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Sriskantharajah J., Kai J. Promoting physical activity among South Asian women with coronary heart disease and diabetes: what might help? Fam Pract. 2007;24(1):71–76. doi: 10.1093/fampra/cml066. [DOI] [PubMed] [Google Scholar]
- 148.Yi S.S., Kanaya A.M., Wen M., Russo R., Kandula N. Associations of neighborhood factors and activity behaviors: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Immigr Minor Health. 2021;23(1):54–61. doi: 10.1007/s10903-020-01021-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Cross-Bardell L., George T., Bhoday M., Tuomainen H., Qureshi N., Kai J. Perspectives on enhancing physical activity and diet for health promotion among at-risk urban UK South Asian communities: a qualitative study. BMJ Open. 2015;5(2):e007317. doi: 10.1136/bmjopen-2014-007317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Vahabi M., Damba C. A feasibility study of a culturally and gender-specific dance to promote physical activity for South Asian immigrant women in the greater Toronto area. Womens Health Issues. 2015;25(1):79–87. doi: 10.1016/j.whi.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 151.Banga Y., Azhar A., Sandhu H., Tang T.S. Dance dance “cultural” revolution: tailoring a physical activity intervention for South Asian children. J Immigr Minor Health. 2020;22(2):291–299. doi: 10.1007/s10903-019-00921-6. [DOI] [PubMed] [Google Scholar]
- 152.Shah N.S., Siddique J., Huffman M.D., Kanaya A.M., Kandula N.R. Cardiovascular health and subclinical atherosclerosis in second generation South Asian Americans: the MASALA study. Indian Heart J. 2021;73(5):629–632. doi: 10.1016/j.ihj.2021.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Natesan A., Nimbal V.C., Ivey S.L., Wang E.J., Madsen K.A., Palaniappan L.P. Engaging South Asian women with type 2 diabetes in a culturally relevant exercise intervention: a randomized controlled trial. BMJ Open Diabetes Res Care. 2015;3(1):e000126. doi: 10.1136/bmjdrc-2015-000126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kandula N.R., Patel Y., Dave S., et al. The South Asian Heart Lifestyle Intervention (SAHELI) study to improve cardiovascular risk factors in a community setting: design and methods. Contemp Clin Trials. 2013;36(2):479–487. doi: 10.1016/j.cct.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Kandula N.R., Dave S., De Chavez P.J., et al. Translating a heart disease lifestyle intervention into the community: the South Asian Heart Lifestyle Intervention (SAHELI) study; a randomized control trial. BMC Public Health. 2015;15:1064. doi: 10.1186/s12889-015-2401-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Rao M., Bar L., Yu Y., et al. Disaggregating Asian American cigarette and alternative tobacco product use: results from the national health interview survey (NHIS) 2006-2018. J Racial Ethn Health Disparities. 2022;9(3):856–864. doi: 10.1007/s40615-021-01024-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Centers for Disease Control and Prevention . 2022. Burden of Cigarette Use in the U.S. [Google Scholar]
- 158.Centers for Disease Control and Prevention . 2022. Asian, Native Hawaiian and Pacific Islander People and Commercial Tobacco: Health Disparities and Ways to Advance Health Equity. [Google Scholar]
- 159.Manderski M.T., Steinberg M.B., Rahi K.N., Banerjee S.C., Delnevo C.D. Surveillance of tobacco use among South Asians in the US: are we underestimating prevalence? J Community Health. 2016;41(6):1140–1145. doi: 10.1007/s10900-016-0226-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Han B.H., Wyatt L.C., Sherman S.E., Islam N.S., Trinh-Shevrin C., Kwon S.C. Prevalence and correlates of cultural smokeless tobacco products among South Asian Americans in New York city. J Community Health. 2019;44(3):479–486. doi: 10.1007/s10900-019-00649-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mukherjea A., Morgan P.A., Snowden L.R., Ling P.M., Ivey S.L. Social and cultural influences on tobacco-related health disparities among South Asians in the USA. Tob Control. 2012;21(4):422–428. doi: 10.1136/tc.2010.042309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Changrani J., Gany F.M., Cruz G., Kerr R., Katz R. Paan and Gutka use in the United States: a pilot study in Bangladeshi and Indian-Gujarati immigrants in New York city. J Immigr Refug Stud. 2006;4(1):99–110. doi: 10.300/J500v04n01_07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Gupta P.C. Survey of sociodemographic characteristics of tobacco use among 99,598 individuals in Bombay, India using handheld computers. Tob Control. 1996;5(2):114–120. doi: 10.1136/tc.5.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hrywna M., Jane Lewis M., Mukherjea A., Banerjee S.C., Steinberg M.B., Delnevo C.D. Awareness and use of South Asian tobacco products among South Asians in New Jersey. J Community Health. 2016;41(6):1122–1129. doi: 10.1007/s10900-016-0208-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Delnevo C.D., Steinberg M.B., Hudson S.V., Ulpe R., Dipaola R.S. Epidemiology of cigarette and smokeless tobacco use among South Asian immigrants in the Northeastern United States. J Oncol. 2011;2011:252675. doi: 10.1155/2011/252675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Centers for Disease Control and Prevention . 2022. Asian Americans. [Google Scholar]
- 167.American Lung Association. Quit Smoking. https://www.lung.org/quit-smoking
- 168.Patel J., Al Rifai M., Scheuner M.T., et al. Basic vs more complex definitions of family history in the prediction of coronary heart disease: the multi-ethnic study of atherosclerosis. Mayo Clin Proc. 2018;93(9):1213–1223. doi: 10.1016/j.mayocp.2018.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Patel J., Al Rifai M., Cainzos-Achirica M., et al. Family history of CHD is associated with severe CAC in South Asians: comparing the MASALA and MESA studies. J Am Coll Cardiol Img. 2017;10(8):958–960. doi: 10.1016/j.jcmg.2017.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wang J., Tillin T., Hughes A.D., Chaturvedi N. Associations between family history and coronary artery calcium and coronary heart disease in British Europeans and South Asians. Int J Cardiol. 2020;300:39–42. doi: 10.1016/j.ijcard.2019.07.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Brister S.J., Hamdulay Z., Verma S., Maganti M., Buchanan M.R. Ethnic diversity: South Asian ethnicity is associated with increased coronary artery bypass grafting mortality. J Thorac Cardiovasc Surg. 2007;133(1):150–154. doi: 10.1016/j.jtcvs.2006.05.068. [DOI] [PubMed] [Google Scholar]
- 172.Chow C.K., Islam S., Bautista L., et al. Parental history and myocardial infarction risk across the world: the INTERHEART study. J Am Coll Cardiol. 2011;57(5):619–627. doi: 10.1016/j.jacc.2010.07.054. [DOI] [PubMed] [Google Scholar]
- 173.Trinder M., Uddin M.M., Finneran P., Aragam K.G., Natarajan P. Clinical utility of lipoprotein(a) and LPA genetic risk score in risk prediction of incident atherosclerotic cardiovascular disease. JAMA Cardiol. 2020;6(3):1–9. doi: 10.1001/jamacardio.2020.5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Bäck M., Yurdagul A., Tabas I., Öörni K., Kovanen P.T. Inflammation and its resolution in atherosclerosis: mediators and therapeutic opportunities. Nat Rev Cardiol. 2019;16(7):389–406. doi: 10.1038/s41569-019-0169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Chambers J.C., Eda S., Bassett P., et al. C-reactive protein, insulin resistance, central obesity, and coronary heart disease risk in Indian Asians from the United Kingdom compared with European Whites. Circulation. 2001;104(2):145–150. doi: 10.1161/01.cir.104.2.145. [DOI] [PubMed] [Google Scholar]
- 176.Anand S.S., Razak F., Yi Q., et al. C-reactive protein as a screening test for cardiovascular risk in a multiethnic population. Arterioscler Thromb Vasc Biol. 2004;24(8):1509–1515. doi: 10.1161/01.ATV.0000135845.95890.4e. [DOI] [PubMed] [Google Scholar]
- 177.Chambers J.C., Ireland H., Thompson E., et al. Methylenetetrahydrofolate reductase 677 C-->T mutation and coronary heart disease risk in UK Indian Asians. Arterioscler Thromb Vasc Biol. 2000;20(11):2448–2452. doi: 10.1161/01.atv.20.11.2448. [DOI] [PubMed] [Google Scholar]
- 178.Refsum H., Yajnik C.S., Gadkari M., et al. Hyperhomocysteinemia and elevated methylmalonic acid indicate a high prevalence of cobalamin deficiency in Asian Indians. Am J Clin Nutr. 2001;74(2):233–241. doi: 10.1093/ajcn/74.2.233. [DOI] [PubMed] [Google Scholar]
- 179.Lonn E., Yusuf S., Arnold M.J., et al. Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med. 2006;354(15):1567–1577. doi: 10.1056/NEJMoa060900. [DOI] [PubMed] [Google Scholar]
- 180.Mehta A., Patel J., Al Rifai M., et al. Inflammation and coronary artery calcification in South Asians: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis. 2018;270:49–56. doi: 10.1016/j.atherosclerosis.2018.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Blaha M.J., Budoff M.J., DeFilippis A.P., et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. 2011;378(9792):684–692. doi: 10.1016/S0140-6736(11)60784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Möhlenkamp S., Lehmann N., Moebus S., et al. Quantification of coronary atherosclerosis and inflammation to predict coronary events and all-cause mortality. J Am Coll Cardiol. 2011;57(13):1455–1464. doi: 10.1016/j.jacc.2010.10.043. [DOI] [PubMed] [Google Scholar]
- 183.Patel J., Pallazola V.A., Dudum R., et al. Assessment of coronary artery calcium scoring to guide statin therapy allocation according to risk-enhancing factors: the multi-ethnic study of atherosclerosis. JAMA Cardiol. 2021;6(10):1161–1170. doi: 10.1001/jamacardio.2021.2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kramer C.K., Campbell S., Retnakaran R. Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Diabetologia. 2019;62(6):905–914. doi: 10.1007/s00125-019-4840-2. [DOI] [PubMed] [Google Scholar]
- 185.Shah N.S., Wang M.C., Freaney P.M., et al. Trends in gestational diabetes at first live birth by race and ethnicity in the US, 2011-2019. JAMA. 2021;326(7):660–669. doi: 10.1001/jama.2021.7217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Shah N.S., Wang M.C., Kandula N.R., et al. Gestational diabetes and hypertensive disorders of pregnancy by maternal birthplace. Am J Prev Med. 2022;62(4):e223–e231. doi: 10.1016/j.amepre.2021.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Gadgil M.D., Oza-Frank R., Kandula N.R., Kanaya A.M. Type 2 diabetes after gestational diabetes mellitus in South Asian women in the United States. Diabetes Metab Res Rev. 2017;33(5):1–11. doi: 10.1002/dmrr.2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Gunderson E.P., Sun B., Catov J.M., et al. Gestational diabetes history and glucose tolerance after pregnancy associated with coronary artery calcium in women during midlife: the CARDIA study. Circulation. 2021;143(10):974–987. doi: 10.1161/CIRCULATIONAHA.120.047320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Yu Y., Arah O.A., Liew Z., et al. Maternal diabetes during pregnancy and early onset of cardiovascular disease in offspring: population based cohort study with 40 years of follow-up. BMJ. 2019;367:l6398. doi: 10.1136/bmj.l6398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Shah N.S., Harrington K.A., Huang X., Cameron N.A., Yee L.M., Khan S.S. Trends in de novo hypertensive disorders of pregnancy among Asian and Hispanic population subgroups in the United States, 2011 to 2019. JAMA Cardiol. 2022;7(7):742–746. doi: 10.1001/jamacardio.2022.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Wang Y.X., Arvizu M., Rich-Edwards J.W., et al. Hypertensive disorders of pregnancy and subsequent risk of premature mortality. J Am Coll Cardiol. 2021;77(10):1302–1312. doi: 10.1016/j.jacc.2021.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.The Lancet Racism in the USA: ensuring Asian American health equity. Lancet. 2021;397(10281):1237. doi: 10.1016/S0140-6736(21)00769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Stangl A.L., Earnshaw V.A., Logie C.H., et al. The Health Stigma and Discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31. doi: 10.1186/s12916-019-1271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Kianoush S., Al-Rifai M., Kalra A., et al. Use of preventive cardiovascular health care among Asian American individuals: a national health interview survey study. Curr Probl Cardiol. 2022:101241. doi: 10.1016/j.cpcardiol.2022.101241. [DOI] [PubMed] [Google Scholar]
- 195.Hussain-Gambles M., Atkin K., Leese B. Why ethnic minority groups are under-represented in clinical trials: a review of the literature. Health Soc Care Community. 2004;12(5):382–388. doi: 10.1111/j.1365-2524.2004.00507.x. [DOI] [PubMed] [Google Scholar]
- 196.Hilton B.A., Grewal S., Popatia N., et al. The desi ways: traditional health practices of South Asian women in Canada. Health Care Women Int. 2001;22(6):553–567. doi: 10.1080/07399330127195. [DOI] [PubMed] [Google Scholar]
- 197.Misra R., Hunte H. Perceived discrimination and health outcomes among Asian Indians in the United States. BMC Health Serv Res. 2016;16(1):567. doi: 10.1186/s12913-016-1821-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Gee G.C., Ponce N. Associations between racial discrimination, limited English proficiency, and health-related quality of life among 6 Asian ethnic groups in California. Am J Public Health. 2010;100(5):888–895. doi: 10.2105/AJPH.2009.178012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Lucas A., Murray E., Kinra S. Heath beliefs of UK South Asians related to lifestyle diseases: a review of qualitative literature. J Obes. 2013;2013:827674. doi: 10.1155/2013/827674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Patel N.R., Chew-Graham C., Bundy C., Kennedy A., Blickem C., Reeves D. Illness beliefs and the sociocultural context of diabetes self-management in British South Asians: a mixed methods study. BMC Fam Pract. 2015;16:58. doi: 10.1186/s12875-015-0269-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Needham B.L., Mukherjee B., Bagchi P., et al. Acculturation strategies among South Asian immigrants: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Immigr Minor Health. 2017;19(2):373–380. doi: 10.1007/s10903-016-0372-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Al-Sofiani M.E., Langan S., Kanaya A.M., et al. The relationship of acculturation to cardiovascular disease risk factors among U.S. South Asians: findings from the MASALA study. Diabetes Res Clin Pract. 2020;161:108052. doi: 10.1016/j.diabres.2020.108052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Lommel L.L., Chen J.L. The relationship between self-rated health and acculturation in Hispanic and Asian adult immigrants: a systematic review. J Immigr Minor Health. 2016;18(2):468–478. doi: 10.1007/s10903-015-0208-y. [DOI] [PubMed] [Google Scholar]
- 204.Asanin J., Wilson K. “I spent nine years looking for a doctor”: exploring access to health care among immigrants in Mississauga, Ontario, Canada. Soc Sci Med. 2008;66(6):1271–1283. doi: 10.1016/j.socscimed.2007.11.043. [DOI] [PubMed] [Google Scholar]
- 205.Lee H.Y., Rhee T.G., Kim N.K., Ahluwalia J.S. Health literacy as a social determinant of health in Asian American immigrants: findings from a population-based survey in California. J Gen Intern Med. 2015;30(8):1118–1124. doi: 10.1007/s11606-015-3217-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Vida Estacio E., McKinley R.K., Saidy-Khan S., Karic T., Clark L., Kurth J. Health literacy: why it matters to South Asian men with diabetes. Prim Health Care Res Dev. 2015;16(2):214–218. doi: 10.1017/S1463423614000152. [DOI] [PubMed] [Google Scholar]
- 207.Lee S., Martinez G., Ma G.X., et al. Barriers to health care access in 13 Asian American communities. Am J Health Behav. 2010;34(1):21–30. doi: 10.5993/ajhb.34.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Ahmed F., Abel G.A., Lloyd C.E., Burt J., Roland M. Does the availability of a South Asian language in practices improve reports of doctor-patient communication from South Asian patients? Cross sectional analysis of a national patient survey in English general practices. BMC Fam Pract. 2015;16:55. doi: 10.1186/s12875-015-0270-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Ko A., Turner J. Culturally sensitive care for Asian immigrants: home healthcare perspectives. Home Healthc Now. 2017;35(9):507–513. doi: 10.1097/NHH.0000000000000608. [DOI] [PubMed] [Google Scholar]
- 210.Torsch V.L., Ma G.X. Cross-cultural comparison of health perceptions, concerns, and coping strategies among Asian and Pacific Islander American elders. Qual Health Res. 2000;10(4):471–489. doi: 10.1177/104973200129118589. [DOI] [PubMed] [Google Scholar]
- 211.Gumber A., Gumber L. Improving prevention, monitoring and management of diabetes among ethnic minorities: contextualizing the six G's approach. BMC Res Notes. 2017;10(1):774. doi: 10.1186/s13104-017-3104-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Vu M., Muhammad H., Peek M.E., Padela A.I. Muslim women's perspectives on designing mosque-based women's health interventions-an exploratory qualitative study. Women Health. 2018;58(3):334–346. doi: 10.1080/03630242.2017.1292344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Magnani J.W., Mujahid M.S., Aronow H.D., et al. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation. 2018;138(2):e48–e74. doi: 10.1161/CIR.0000000000000579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Bhopal R., Fischbacher C., Vartiainen E., Unwin N., White M., Alberti G. Predicted and observed cardiovascular disease in South Asians: application of FINRISK, Framingham and SCORE models to Newcastle heart project data. J Public Health (Oxf) 2005;27(1):93–100. doi: 10.1093/pubmed/fdh202. [DOI] [PubMed] [Google Scholar]
- 215.Thulani U.B., Mettananda K.C.D., Warnakulasuriya D.T.D., et al. Validation of the World Health Organization/International Society of Hypertension (WHO/ISH) cardiovascular risk predictions in Sri Lankans based on findings from a prospective cohort study. PLoS One. 2021;16(6):e0252267. doi: 10.1371/journal.pone.0252267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Aarabi M., Jackson P.R. Predicting coronary risk in UK South Asians: an adjustment method for Framingham-based tools. Eur J Cardiovasc Prev Rehabil. 2005;12(1):46–51. [PubMed] [Google Scholar]
- 217.Rana J.S., Tabada G.H., Solomon M.D., et al. Accuracy of the atherosclerotic cardiovascular risk equation in a large contemporary, multiethnic population. J Am Coll Cardiol. 2016;67(18):2118–2130. doi: 10.1016/j.jacc.2016.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Gopal D.P., Usher-Smith J.A. Cardiovascular risk models for South Asian populations: a systematic review. Int J Public Health. 2016;61(5):525–534. doi: 10.1007/s00038-015-0733-4. [DOI] [PubMed] [Google Scholar]
- 219.Bellary S., O'Hare J.P., Raymond N.T., et al. Premature cardiovascular events and mortality in south Asians with type 2 diabetes in the United Kingdom Asian Diabetes Study - effect of ethnicity on risk. Curr Med Res Opin. 2010;26(8):1873–1879. doi: 10.1185/03007995.2010.490468. [DOI] [PubMed] [Google Scholar]
- 220.Tillin T., Hughes A.D., Mayet J., et al. The relationship between metabolic risk factors and incident cardiovascular disease in Europeans, South Asians, and African Caribbeans: SABRE (Southall and Brent Revisited) – a prospective population-based study. J Am Coll Cardiol. 2013;61(17):1777–1786. doi: 10.1016/j.jacc.2012.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Rodriguez F., Chung S., Blum M.R., Coulet A., Basu S., Palaniappan L.P. Atherosclerotic cardiovascular disease risk prediction in disaggregated Asian and Hispanic subgroups using electronic health records. J Am Heart Assoc. 2019;8(14):e011874. doi: 10.1161/JAHA.118.011874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Goff D.C., Lloyd-Jones D.M., Bennett G., et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2014;129(25 Suppl 2):S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 223.Arnett D.K., Blumenthal R.S., Albert M.A., et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2019;140(11):e563–e595. doi: 10.1161/CIR.0000000000000677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Conroy R.M., Pyörälä K., Fitzgerald A.P., et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24(11):987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 225.Mach F., Baigent C., Catapano A.L., et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–188. doi: 10.1093/eurheartj/ehz455. [DOI] [PubMed] [Google Scholar]
- 226.Visseren F.L.J., Mach F., Smulders Y.M., et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Cardiol. 2022;29(1):5–115. doi: 10.1093/eurjpc/zwab154. [DOI] [PubMed] [Google Scholar]
- 227.Kannel W.B., McGee D., Gordon T. A general cardiovascular risk profile: the Framingham Study. Am J Cardiol. 1976;38(1):46–51. doi: 10.1016/0002-9149(76)90061-8. [DOI] [PubMed] [Google Scholar]
- 228.Calabria B., Korda R.J., Lovett R.W., et al. Absolute cardiovascular disease risk and lipid-lowering therapy among Aboriginal and Torres Strait Islander Australians. Med J Aust. 2018;209(1):35–41. doi: 10.5694/mja17.00897. [DOI] [PubMed] [Google Scholar]
- 229.Pearson G.J., Thanassoulis G., Anderson T.J., et al. 2021 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in adults. Can J Cardiol. 2021;37(8):1129–1150. doi: 10.1016/j.cjca.2021.03.016. [DOI] [PubMed] [Google Scholar]
- 230.National Collaborating Centre for Primary Care (UK) 2008. Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. [DOI] [PubMed] [Google Scholar]
- 231.Hippisley-Cox J., Coupland C., Vinogradova Y., Robson J., May M., Brindle P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ. 2007;335(7611):136. doi: 10.1136/bmj.39261.471806.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Board J. Joint British Societies' consensus recommendations for the prevention of cardiovascular disease (JBS3) Heart. 2014;100 Suppl 2:ii1–ii67. doi: 10.1136/heartjnl-2014-305693. [DOI] [PubMed] [Google Scholar]
- 233.Hippisley-Cox J., Coupland C., Vinogradova Y., et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336(7659):1475–1482. doi: 10.1136/bmj.39609.449676.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Hippisley-Cox J., Coupland C., Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ. 2017;357:j2099. doi: 10.1136/bmj.j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ministry of Health . Ministry of Health; 2018. Cardiovascular Disease Risk Assessment and Management for Primary Care. [Google Scholar]
- 236.McGorrian C., Yusuf S., Islam S., et al. Estimating modifiable coronary heart disease risk in multiple regions of the world: the INTERHEART modifiable risk score. Eur Heart J. 2011;32(5):581–589. doi: 10.1093/eurheartj/ehq448. [DOI] [PubMed] [Google Scholar]
- 237.Selmer R., Igland J., Ariansen I., et al. NORRISK 2: a Norwegian risk model for acute cerebral stroke and myocardial infarction. Eur J Prev Cardiol. 2017;24(7):773–782. doi: 10.1177/2047487317693949. [DOI] [PubMed] [Google Scholar]
- 238.Rabanal K.S., Igland J., Tell G.S., et al. Validation of the cardiovascular risk model NORRISK 2 in South Asians and people with diabetes. Scand Cardiovasc J. 2021;55(1):56–62. doi: 10.1080/14017431.2020.1821909. [DOI] [PubMed] [Google Scholar]
- 239.Brindle P., May M., Gill P., et al. Primary prevention of cardiovascular disease: a web-based risk score for seven British Black and minority ethnic groups. Heart. 2006;92(11):1595–1602. doi: 10.1136/hrt.2006.092346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Stevens R.J., Kothari V., Adler A.I., Stratton I.M., United Kingdom Prospective Diabetes Study (UKPDS) Group The UKPDS risk engine: a model for the risk of coronary heart disease in type II diabetes (UKPDS 56) Clin Sci (Lond) 2001;101(6):671–679. [PubMed] [Google Scholar]
- 241.National Clinical Guideline Centre (UK) 2014. Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. [PubMed] [Google Scholar]
- 242.WHO CVD Risk Chart Working Group World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–e1345. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Piepoli M.F., Hoes A.W., Agewall S., et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and other Societies on Cardiovascular Disease Prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2016;37(29):2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Palaniappan L.P., Araneta M.R., Assimes T.L., et al. Call to action: cardiovascular disease in Asian Americans: a science advisory from the American Heart Association. Circulation. 2010;122(12):1242–1252. doi: 10.1161/CIR.0b013e3181f22af4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Holland A.T., Wong E.C., Lauderdale D.S., Palaniappan L.P. Spectrum of cardiovascular diseases inAsian-American racial/ethnic subgroups. Ann Epidemiol. 2011;21(8):608–614. doi: 10.1016/j.annepidem.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Satish P., Sadaf M.I., Valero-Elizondo J., et al. Heterogeneity in cardio-metabolic risk factors and atherosclerotic cardiovascular disease among Asian groups in the United States. Am J Prev Cardiol. 2021;7:100219. doi: 10.1016/j.ajpc.2021.100219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Greenland P., Blaha M.J., Budoff M.J., Erbel R., Watson K.E. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol. 2018;72(4):434–447. doi: 10.1016/j.jacc.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Haque W., Grandhi G.R., Kanaya A.M., et al. Implications of the 2019 American College of Cardiology/American Heart Association primary prevention guidelines and potential value of the coronary artery calcium score among South Asians in the US: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis. 2021;334:48–56. doi: 10.1016/j.atherosclerosis.2021.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Al Rifai M., Kanaya A.M., Kandula N.R., et al. Association of coronary artery calcium density and volume with predicted atherosclerotic cardiovascular disease risk and cardiometabolic risk factors in South Asians: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Curr Probl Cardiol. 2022:101105. doi: 10.1016/j.cpcardiol.2022.101105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Roos C.J., Kharagjitsingh A.V., Jukema J.W., Bax J.J., Scholte A.J. Comparison by computed tomographic angiography-the presence and extent of coronary arterial atherosclerosis in South Asians versus Caucasians with diabetes mellitus. Am J Cardiol. 2014;113(11):1782–1787. doi: 10.1016/j.amjcard.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 251.Criqui M.H., Denenberg J.O., Ix J.H., et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311(3):271–278. doi: 10.1001/jama.2013.282535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Williams M., Shaw L.J., Raggi P., et al. Prognostic value of number and site of calcified coronary lesions compared with the total score. J Am Coll Cardiol Img. 2008;1(1):61–69. doi: 10.1016/j.jcmg.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 253.Mortensen M.B., Dzaye O., Bødtker H., et al. Interplay of risk factors and coronary artery calcium for CHD risk in young patients. J Am Coll Cardiol Img. 2021;14(12):2387–2396. doi: 10.1016/j.jcmg.2021.05.003. [DOI] [PubMed] [Google Scholar]
- 254.Al Rifai M., Kanaya A.M., Kandula N.R., et al. Distribution of calcium volume, density, number, and type of coronary vessel with calcified plaque in South Asians in the US and other race/ethnic groups: the MASALA and MESA studies. Atherosclerosis. 2021;317:16–21. doi: 10.1016/j.atherosclerosis.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Bhatia H.S., Lin F., Thomas I.C., et al. Coronary artery calcium incidence and changes using direct plaque measurements: the MASALA study. Atherosclerosis. 2022;353:41–46. doi: 10.1016/j.atherosclerosis.2022.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Blaha M.J., Budoff M.J., Tota-Maharaj R., et al. Improving the CAC score by addition of regional measures of calcium distribution: multi-ethnic study of atherosclerosis. J Am Coll Cardiol Img. 2016;9(12):1407–1416. doi: 10.1016/j.jcmg.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Tota-Maharaj R., Joshi P.H., Budoff M.J., et al. Usefulness of regional distribution of coronary artery calcium to improve the prediction of all-cause mortality. Am J Cardiol. 2015;115(9):1229–1234. doi: 10.1016/j.amjcard.2015.01.555. [DOI] [PubMed] [Google Scholar]
- 258.Dzaye O., Dudum R., Mirbolouk M., et al. Validation of the coronary artery calcium data and reporting system (CAC-DRS): dual importance of CAC score and CAC distribution from the Coronary Artery Calcium (CAC) consortium. J Cardiovasc Comput Tomogr. 2020;14(1):12–17. doi: 10.1016/j.jcct.2019.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Uddin S.M.I., Mirbolouk M., Kianoush S., et al. Role of coronary artery calcium for stratifying cardiovascular risk in adults with hypertension. Hypertension. 2019;73(5):983–989. doi: 10.1161/HYPERTENSIONAHA.118.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Erbel R., Lehmann N., Möhlenkamp S., et al. Subclinical coronary atherosclerosis predicts cardiovascular risk in different stages of hypertension: result of the Heinz Nixdorf Recall Study. Hypertension. 2012;59(1):44–53. doi: 10.1161/HYPERTENSIONAHA.111.180489. [DOI] [PubMed] [Google Scholar]
- 261.McEvoy J.W., Martin S.S., Dardari Z.A., et al. Coronary artery calcium to guide a personalized risk-based approach to initiation and intensification of antihypertensive therapy. Circulation. 2017;135(2):153–165. doi: 10.1161/CIRCULATIONAHA.116.025471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Blaha M.J., Cainzos-Achirica M., Greenland P., et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the multi-ethnic study of atherosclerosis (MESA) Circulation. 2016;133(9):849–858. doi: 10.1161/CIRCULATIONAHA.115.018524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Stone N.J., Smith S.C., Orringer C.E., et al. Managing atherosclerotic cardiovascular risk in young adults: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79(8):819–836. doi: 10.1016/j.jacc.2021.12.016. [DOI] [PubMed] [Google Scholar]
- 264.Kanaya A.M., Vittinghoff E., Lin F., et al. Incidence and progression of coronary artery calcium in South Asians compared with 4 race/ethnic groups. J Am Heart Assoc. 2019;8(2):e011053. doi: 10.1161/JAHA.118.011053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Hatwalkar A., Agrawal N., Reiss D.S., Budoff M.J. Comparison of prevalence and severity of coronary calcium determined by electron beam tomography among various ethnic groups. Am J Cardiol. 2003;91(10):1225–1227. doi: 10.1016/s0002-9149(03)00268-6. [DOI] [PubMed] [Google Scholar]
- 266.Wasnik A., Raut A., Morani A. Coronary calcium scoring in asymptomatic Indian population: correlation with age, gender and risk factors–a prospective study on 500 subjects. Indian Heart J. 2007;59(3):232–238. [PubMed] [Google Scholar]
- 267.Jain P., Kooner J.S., Raval U., Lahiri A. Prevalence of coronary artery calcium scores and silent myocardial ischaemia was similar in Indian Asians and European Whites in a cross-sectional study of asymptomatic subjects from a U.K. population (LOLIPOP-IPC) J Nucl Cardiol. 2011;18(3):435–442. doi: 10.1007/s12350-011-9371-2. [DOI] [PubMed] [Google Scholar]
- 268.Dzaye O., Dardari Z.A., Cainzos-Achirica M., et al. Warranty period of a calcium score of zero: comprehensive analysis from MESA. J Am Coll Cardiol Img. 2021;14(5):990–1002. doi: 10.1016/j.jcmg.2020.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Iwasaki K., Matsumoto T., Aono H., Furukawa H., Samukawa M. Prevalence of non-calcified coronary plaque on 64-slice computed tomography in asymptomatic patients with zero and low coronary artery calcium. Can J Cardiol. 2010;26(7):377–380. doi: 10.1016/s0828-282x(10)70419-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Nasir K., Cainzos-Achirica M., Valero-Elizondo J., et al. Coronary atherosclerosis in an asymptomatic U.S. population: Miami heart study at Baptist Health South Florida. J Am Coll Cardiol Img. 2022;15(9):1604–1618. doi: 10.1016/j.jcmg.2022.03.010. [DOI] [PubMed] [Google Scholar]
- 271.Bergstrom G., Persson M., Adiels M., et al. Prevalence of subclinical coronary artery atherosclerosis in the general population. Circulation. 2021;144(12):916–929. doi: 10.1161/CIRCULATIONAHA.121.055340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Villines T.C., Hulten E.A., Shaw L.J., et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: an International Multicenter) registry. J Am Coll Cardiol. 2011;58(24):2533–2540. doi: 10.1016/j.jacc.2011.10.851. [DOI] [PubMed] [Google Scholar]
- 273.Budoff M.J., Lakshmanan S., Toth P.P., et al. Cardiac CT angiography in current practice: an American Society for preventive cardiology clinical practice statement. Am J Prev Cardiol. 2022;9:100318. doi: 10.1016/j.ajpc.2022.100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Kanaya A.M., Kandula N., Herrington D., et al. Mediators of Atherosclerosis in South Asians Living in America (MASALA) study: objectives, methods, and cohort description. Clin Cardiol. 2013;36(12):713–720. doi: 10.1002/clc.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Our Health. Help us Understand and Improve Cardiovascular Disease Risk Among South Asian Populations. https://ourhealthstudy.org
- 276.Shams P., Hussain M., Karani S., et al. Can sound public health policies stem the tide of burgeoning epidemic of cardiovascular disease in South Asians? Curr Cardiol Rep. 2021;23(12):181. doi: 10.1007/s11886-021-01612-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.