Abstract
Purpose
This international study aimed to compare healthcare professionals’ perspectives on the unmet needs of their cancer patients with those of family caregivers and to investigate the degree to which patients’ age group moderates the associations.
Methods
Healthcare professionals involved in the care for cancer patients and their family caregivers were invited to participate in the International Psycho-Oncology Society (IPOS) Survivorship Online Survey. A total of 397 healthcare professionals from 34 countries provided valid study data. The participants evaluated whether the unmet need was the same for all age groups of patients and the degree of their patients’ needs not being met per patients’ age group. They evaluated the same questions for family caregivers.
Results
Patients’ unmet needs in medical care were evaluated as greater than those of caregivers across all age groups. On the other hand, pediatric patients’ unmet needs for spiritual concerns, sexuality/intimacy, and insomnia/fatigue were evaluated as greater than those of caregivers, whereas adolescent and young adult patients’ unmet needs for symptom management were greater than those of caregivers. Patients’ other unmet needs were evaluated as comparable with those of caregivers regardless of age groups.
Conclusion
The findings provide insights how best healthcare providers stratify resources to address the unmet needs of patients and caregivers by the patients’ age. Development of systematic assessment of unmet needs and provision of interventions tailored for patients’ lifespan to address the unmet needs of cancer patients, and caregivers are warranted.
Keywords: Unmet needs, Cancer patients, Family caregivers, Healthcare professionals’ perspectives, Pediatric cancer, Adolescent and young adult cancer, Global oncology
Cancer is a global burden as over 19.3 million new cancers are diagnosed in a year and approximately one-sixth of deaths (10 million deaths) are caused by cancer worldwide [1]. Cancer patients face physical, psychological, family, and social challenges related to the disease and treatment, which have a lasting impact on their daily function and reduced quality of life [2]. Family caregivers also encounter similar, if not more, challenges [3, 4]. Unresolved and inadequately managed distress impedes optimal self-care of the patients and caregivers’ support for their patients [5, 6]. Thus, identifying and addressing the unmet needs of the large and growing population of cancer patients and their family caregivers are urgent global health issues.
Several reviews have reported that up to 93% of cancer patients had unmet needs, and unmet needs in the psychological, information, daily activities, and physical domains are most commonly endorsed [7–9]. Reviews also noted that the unmet needs in other domains, such as spirituality, communication, and sexuality remain understudied [8], although the empirical evidence is cumulating in recent years. Similar patterns and additional unmet needs of providing quality support to the patient and self-care have also been found in studies with family caregivers of adult cancer patients [10–12].
Only a few studies to date, however, have examined the unmet needs of both patients and caregivers. For example, the overall amount of patients’ unmet needs was positively correlated with that of their caregivers’, suggesting concordance in unmet needs between patients and their caregivers [13]. A review of 50 studies with advanced cancer patients and caregivers reported that patients identify more diverse types of unmet needs than their caregivers (12 vs 7) [12]. On the other hand, patients underestimated their needs when compared with caregivers’ perceptions of the patients’ unmet needs [14, 15]. Although these studies attempted to understand the unmet needs of patients and their caregivers simultaneously, no direct comparison was made on the differential degree of discrete unmet needs between patients and caregivers. Such knowledge would be a first step toward developing and revising existing programs and services to effectively mitigate the unmet needs targeting specific subgroups.
Health care professionals (HCPs) play an essential role throughout the cancer treatment phase and beyond, providing various types of care support and critical information for effective cancer management. HCPs can offer a broad perspective on unmet needs of their patients and family caregivers, which views can shed light on developing a holistic model of care [16]. Despite increasing evidence of the unmet needs in cancer patients, limited research has systematically assessed the levels of unmet needs of patients and caregivers from HCPs’ perspectives [17], which is a critical step for healthcare institutions to provide quality care to them. Thus, the present study aimed to compare HCPs’ perspectives on the unmet needs of their cancer patients with those of family caregivers (aim 1).
A critical issue for cancer adaptation and survivorship involves patient’s developmental life stage [18], as problems and life disruptions caused by cancer are likely to be unique to their developmental milestones. Age is found to be the predictor of unmet needs in cancer patients, and younger patients tend to have greater unmet needs than the older patients across all domains [19–21]. Existing studies, however, have focused on specific age groups (e.g., young adults or older adults) and mainly with English-speaking participants, which precludes the possibility of systematic understanding of unmet needs across different lifespans globally. Thus, this study took a developmental framework to investigate the degree to which differences and similarities in the unmet needs between patients and caregivers differ across four major age groups (aim 2) around the globe.
Methods
Participants
Participants were sub-group of the International Psycho-Oncology Society (IPOS) Survivorship Online Survey study (see Kim et al. [22], for the overview of the parent study) that was available in 15 different languages. The International IPOS Survivorship Online Survey was distributed to HCPs who were involved in clinical services or research with cancer patients/survivors and their family caregivers worldwide. Individuals with a membership of the IPOS or the psycho-oncology society of their nation were encouraged to distribute the online survey invitation to their own regional psycho-oncology members and colleagues who were involved in work that directly pertain to cancer patients/survivors and their family members. There were no exclusion criteria based on discipline, experience, or types of patient groups. Participation in this cross-sectional study was voluntary, and no reimbursement was given.
The survey content and procedure were reviewed and approved by the Institutional Review Board of the University of Miami, FL, USA (IRB ID:20151140) and the IPOS research committee.
Procedure
Participants were invited to complete the survey on the web-based REDCap application that is HIPAA compliant and allows responders to skip irrelevant Sects. [23]. The first page of the survey presented the consent, which was required to proceed to complete the survey. The survey was distributed to over 50 psycho-oncology societies and their networking platforms as well as social media platforms, and to authors who have published in psycho-oncology journals globally.
The survey was developed in English by Kim et al. [22] and translated into 14 other languages. The translation-backtranslation method was employed by translators and back-translators with psycho-oncology expertise and who were fluent in both English and the corresponding language. Detailed translation procedure was reported in Kim et al. [22].
The IPOS survey consists of four sections (the full survey can be found in the parent study [22] or survey link: https://ipos-society.org/ipos-survivorship-online-survey/). The study presented here used the data majorly from the “Methods” section, which consists of a series of questions regarding the healthcare professionals’ perception of their patients’ unmet needs to address the unmet needs in their institution, and the “Results” section, which consists of a series of questions regarding the healthcare professionals’ perception of family caregivers’ unmet needs to address family caregivers’ unmet needs in their institution.
Measures
Unmet needs
To measure unmet needs the survey asked the healthcare professionals’ perspective of unmet needs in patients and caregivers of patients in different age groups (pediatric, adolescent and young adult, middle-aged adult, older adult). Participants evaluated the extent to which they perceived the 13 different types of needs being met by their cancer patients/survivors and their family caregivers. The types of unmet needs include emotional distress, finding meaning and spiritual concerns, family relationships, sexuality and intimacy, social relationships and isolation, medical care related to cancer, cancer-related symptom management, physical functioning decline, cognitive functioning decline, insomnia/sleep-difficulties and fatigue, financial concern related to cancer care, personal care, and balancing other social roles with new role as either a patient or a family member. The unmet needs domains were developed and validated in the previous study [10].
Participants evaluated their perception of the needs of the patients and their family members being met by first indicated whether the need is the same for all age groups of patients/survivors. For those who answer “proportion is the same for all age groups” the degree of the need being met using a scale from 0 (the concern is completely unaddressed; the need is not being met at all) to 100 (the concern is completely addressed; the need is fully being met) were asked. For those who answer “proportion differs depending on the age group” the degree of the need being met using a scale from 0 to 100 was asked per patients’ age group they were involved (see below). The online survey allows participants to skip irrelevant questions because not all participants work with cancer patients across all age groups. In this case, participants can skip any questions unrelated to their work. The values of need being met were reversed (100-value) to present a higher score for greater unmet needs.
Patients’ age groups
Cancer patients’ age was grouped in four: pediatric (0–14 or 15 years old), adolescents-and-young adults (15 or 16–39 years old), middle-aged (40–65 years old), and older adults (older than 66 years old). Participants evaluated their perception of the needs of the patients and their family members not being met per age group.
Demographic information
In the Sect. 1 and 4 of the IPOS survey, participants self-reported gender, age, country, discipline, job types, and time of involvement they work with different age groups of patients.
Statistical analysis
The degree to which HCPs evaluated the unmet needs of their patients differ from those of the family caregivers was compared using t-tests (aim 1). Two-way Analyses of Variances (ANOVAs) were used to examine whether difference in unmet needs between patients and family caregivers varied as a function of age group (aim 2). Significant interactions were followed up with simple effects tests to examine the difference in unmet needs between patients and caregivers across age groups. Statistical analysis was performed using SPSS version 27 (IBM). Statistical significance was set at a 2-tailed p-value < 0.05.
Results
Sample characteristics
Participants from 34 countries participated in the IPOS Survivorship Online Survey between February 2018 and February 2019. A total of 1472 participants at least partially completed the IPOS survey, among which 397 participants responded to the unmet need evaluations consist of variables of interest for this study. Those 397 participants completed the survey in one of the 15 languages and identified themselves working in 34 different countries. Supplementary material shows the country and language information.
As shown in Table 1, participants were primarily involved in clinical work, being on the job for 2–10 years, involved in the work for middle-aged patients and their family caregivers, middle-aged, and female. The majority were counselors or psychologists.
Table 1.
Sample descriptives
| N% (0 ~ 100%) | |||||
|---|---|---|---|---|---|
|
| |||||
| Job types | 397 | ||||
| Administration | 18.3% | ||||
| Clinical work | 43.2% | ||||
| Research | 19.3% | ||||
| Teaching, supervision, training | 15.9% | ||||
| Othera | 4.0% | ||||
| Duration in the jobb | < 2 yrs | 2–10 yrs | 11–20 yrs | > 20 yrs | |
| Administration | 305 | 23.0% | 44.6% | 19.3% | 13.1% |
| Clinical work | 335 | 13.4% | 38.5% | 27.2% | 20.9% |
| Research | 313 | 14.1% | 45.7% | 22.4% | 17.9% |
| Teaching, supervision, training | 335 | 21.8% | 37.0% | 22.7% | 18.5% |
| Other | 119 | 37.0% | 35.3% | 11.8% | 16.0% |
| Involved patients | 397 | ||||
| 0–14 years old | 10.25% | ||||
| 15–39 years old | 22.40% | ||||
| 40–65 years old | 38.66% | ||||
| > 66 years old | 26.92% | ||||
| Age | 227 | ||||
| 21–30 | 16.7% | ||||
| 31–40 | 30.0% | ||||
| 41–50 | 26.9% | ||||
| 51–60 | 18.9% | ||||
| 61 and above | 7.0% | ||||
| Gender | 227 | ||||
| Female | 80.2% | ||||
| Male | 17.2% | ||||
| Prefer not to answer | 2.6% | ||||
| Disciplines | 397 | ||||
| Counselor/psychologist | 46% | ||||
| Medical professional | 31% | ||||
| Other | 23% | ||||
Fundraising, program development, program evaluation, managing website, writing, public relations/ engagement/liaison, organizing department meetings.
The percentage of time and effort participants typically spent for administration, clinical work, research, teaching, and other; the duration on the job engaging in each of the activities (less than 2 years, 2–10 years, 11–20 years, and over 20 years) were asked
Evaluation of unmet needs of patients and caregivers
As shown in Table 2 (“All” columns), HCPs indicated that substantial proportions of cancer patients, and their caregivers are living with high levels of unmet needs across the range of domains examined. Among the 13 different types of needs assessed, 11 areas of needs were evaluated as not being met among greater than 40% of their patients and caregivers. HCPs identified needs for spiritual concerns and sexuality/intimacy most likely not being met and needs for medical care and symptom managements most likely being met, for both patients and caregivers. Furthermore, HCPs evaluated the needs for medical care were more likely unmet by their patients than by the caregivers, whereas HCPs evaluated all other needs were likely unmet at a comparable degree between patients and caregivers.
Table 2.
Means (SDs) of 13 types of unmet needs by patients’ age groups
| Unmet needs types | All |
0–14/15 |
15/16–39 |
40–65 |
> 66 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PT | CG | t | PT | CG | PT | CG | PT | CG | PT | CG | F | |
|
| ||||||||||||
| Emotional distress | 40.71 (27.01) | 41.00 (28.69) | − 0.08 | 54.32 (35.19) | 50.64 (32.93) | 41.60 (32.38) | 45.02 (28.45) | 39.48 (26.86) | 40.42 (25.41) | 45.06 (29.62) | 44.40 (29.77) | 0.77 |
| Spiritual concerns | 65.53 (26.82) | 61.58 (30.64) | 0.73 | 73.29a (26.84) | 62.33b (35.12) | 55.35 (27.43) | 52.98 (31.64) | 49.00 (26.68) | 48.02 (29.35) | 46.74 (30.43) | 51.57 (32.06) | 7.85*** |
| Family relationships | 49.31 (29.54) | 44.31 (29.30) | 1.31 | 57.30 (33.96) | 48.67 (35.73) | 48.27 (30.56) | 46.13 (26.68) | 38.84 (23.75) | 42.07 (23.92) | 52.08 (29.87) | 47.44 (27.62) | 1.15 |
| Sexuality/intimacy | 66.25 (32.13) | 65.00 (35.61) | 0.35 | 81.90a (27.13) | 65.24b (34.84) | 53.66 (30.16) | 54.64 (32.85) | 50.93 (26.98) | 54.07 (31.04) | 64.51 (27.52) | 60.53 (33.09) | 3.79* |
| Social relationships | 48.85 (29.71) | 47.50 (29.37) | 0.35 | 59.74 (34.78) | 59.15 (33.46) | 50.17 (30.78) | 46.60 (28.71) | 48.30 (27.87) | 46.05 (26.34) | 53.91 (28.38) | 49.86 (30.39) | 0.98 |
| Medical care | 32.14 (26.69) | 23.29 (17.36) | 2.25* | 62.30 (34.88) | 55.15 (36.02) | 49.22 (28.63) | 46.05 (31.31) | 46.73 (24.84) | 43.71 (29.15) | 49.92 (27.14) | 43.92 (31.51) | 0.63 |
| Symptom management | 34.03 (27.97) | 26.41 (20.71) | 1.58 | 53.87 (33.52) | 46.04 (35.40) | 49.05a (29.90) | 41.34b (29.54) | 45.48 (26.80) | 42.62 (27.37) | 47.9 (27.87) | 41.79 (29.75) | 3.02* |
| Physical functioning | 51.59 (30.02) | 40.91 (22.13) | 1.93† | 57.35 (35.41) | 54.50 (34.87) | 53.92 (31.38) | 50.83 (29.54) | 49.36 (26.46) | 44.98 (26.84) | 44.17 (28.54) | 44.04 (30.20) | 1.32 |
| Cognitive functioning | 58.33 (25.52) | 54.17 (29.68) | 0.77 | 62.64 (31.01) | 63.00 (34.04) | 53.67 (29.34) | 55.18 (31.24) | 50.60 (25.32) | 47.95 (28.81) | 47.56 (27.55) | 48.46 (31.71) | 0.25 |
| Insomnia | 40.36 (28.83) | 40.89 (27.39) | − 0.10 | 63.21a (29.89) | 58.68b (30.46) | 50.34 (27.70) | 51.48 (29.78) | 47.23 (25.33) | 45.46 (28.21) | 46.87 (26.28) | 47.11 (29.89) | 3.02* |
| Financial concerns | 57.38 (33.34) | 44.52 (32.32) | 1.91† | 67.68a (31.38) | 53.45b (33.27) | 57.06 (24.91) | 58.80 (30.20) | 49.85 (22.97) | 52.38 (27.08) | 54.62 (26.03) | 53.77 (31.86) | 1.90 |
| Personal care | 48.06 (26.47) | 43.89 (26.65) | 0.75 | 59.76 (33.81) | 55.88 (35.75) | 52.47 (25.60) | 49.31 (29.58) | 49.56 (23.00) | 47.26 (28.57) | 50.90 (26.62) | 46.65 (30.88) | 0.66 |
| Balancing roles | 60.00 (27.58) | 56.46 (24.82) | 1.04 | 67.93 (28.63) | 63.46 (32.43) | 53.90 (28.35) | 52.35 (29.31) | 49.81 (26.91) | 49.32 (27.34) | 56.98 (27.71) | 57.46 (30.74) | 0.84 |
PT=cancer patients or survivors; CG=caregivers of cancer patients or survivors. Scores for unmet needs ranged from 0 to 100, the higher the greater level of unmet needs. “All” column represents the levels of unmet need for all age groups, followed by columns presenting the levels of unmet need for cancer patients’ age group in four categories: pediatric (0–14 or15 years old), adolescents-and-young adults (15 or 16–39 years old), middle-age (40–65 years old), and older adults (older than 66 years old). Different subscripts indicate significant differences between patients and caregivers within the corresponding age group
p < .10
p < .05
p < .01
p < .001
Patients’ age effects on differential unmet needs between patients and caregivers
As shown in Table 2 across the four age groups, four interaction effects of patients vs caregivers by four age groups were significant (Fig. 1). Unmet needs in spiritual concerns, sexuality/intimacy, and insomnia were evaluated as significantly differ between patients and caregivers only among pediatric patients (0–14/15 years old). HCPs evaluated pediatric patients were more likely having their needs for managing spiritual concerns, sexuality, and intimacy, as well as insomnia and fatigue not being met than family caregivers of pediatric patients were. In addition, difference in unmet needs for symptom management between patients and caregivers was significant but this time only for adolescent and young adult patients (AYA; 15/16–39 years old) group. HCPs evaluated AYA patients’ needs for managing symptom were more likely unmet than family caregivers of AYA patients were. The interaction effects of patients vs caregivers by four age groups in the remaining nine unmet needs were not significant.
Fig. 1.
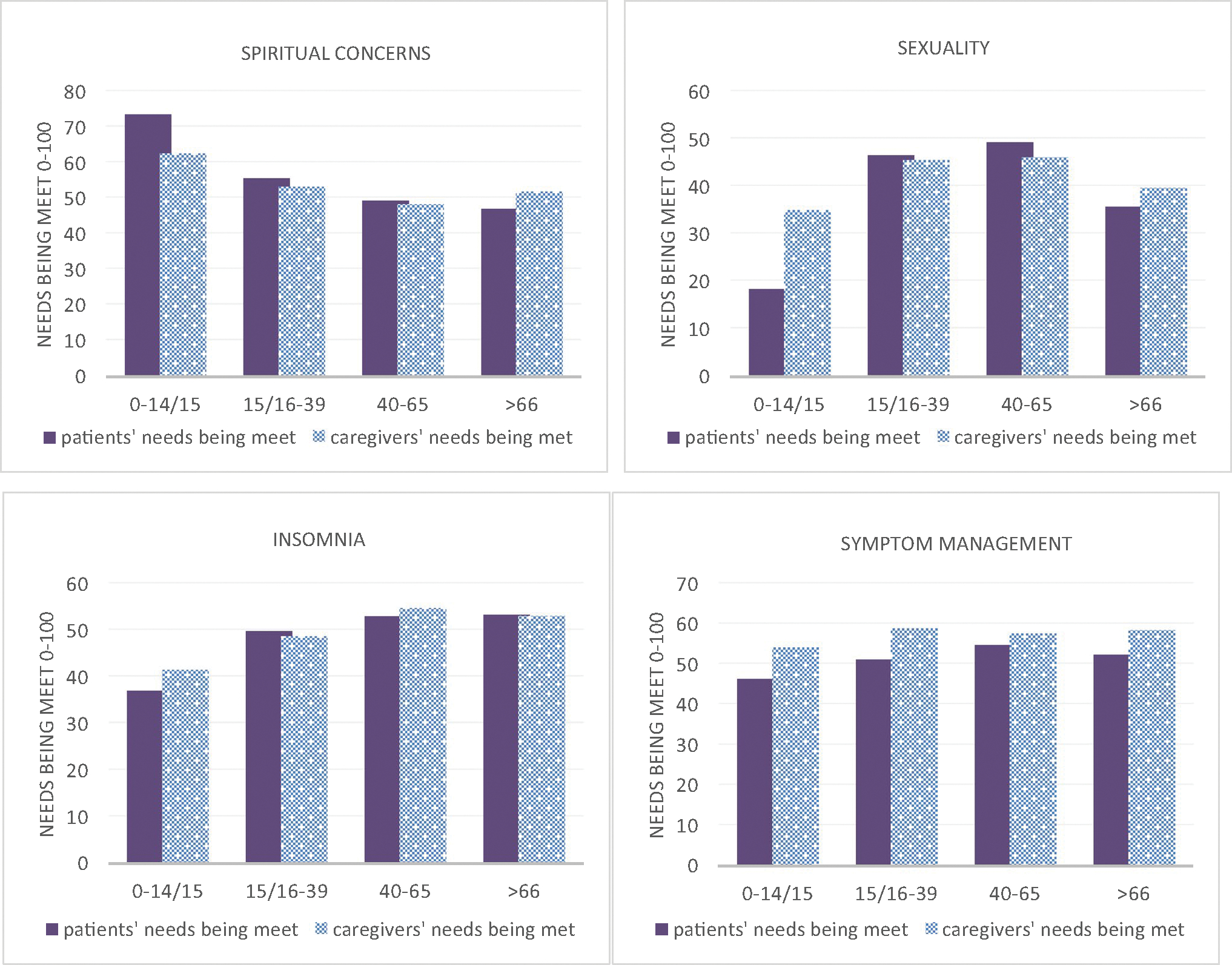
Unmet needs comparison between patients and caregivers by four age groups
Discussion
Healthcare professionals (HCPs) evaluated a substantial proportion of their patients’ and caregivers’ needs not being met, which also varied by patients’ age. Specifically, HCPs evaluated more than one-third of their patients and caregivers would concern that their various kinds of needs are not met. Overall, HCPs evaluated the degree to which their patients’ needs not being met was comparable to that of caregivers, except the needs for medical care for which patients’ unmet needs were greater than caregivers’.
Although the medical care need was evaluated as most addressed, HCPs perceived cancer patients’ needs for medical care and for managing concerns related to physical functioning (marginally significant though) are greater than their caregivers’ corresponding needs for the patient. Findings suggest the concerns related to manage cancer treatment and its physical consequences are critical for patients. Furthermore, the financial toxicity attributable in part to not being able to return to work due to the treatments and the side effects [24] may have a larger impact on patients than caregivers. These differences in unmet needs between patients and caregivers were evaluated as the case across different age groups, pinpointing that the resources for delivering optimal medical care and managing physical and financial sequelae of cancer should be prioritized to be given to patients in all ages.
Findings also pinpoint differential degrees of unmet needs between patients and caregivers depending on the patients’ age. For example, pediatric patients’ unmet needs for spiritual concerns, sexuality/intimacy, and insomnia/fatigue were evaluated as greater than those of caregivers, whereas adolescent and young adult patients’ unmet needs for symptom management were greater than those of caregivers. The findings suggest that younger patients, especially pediatric patients, should be classified as a vulnerable group in need of more psychosocial support. Our findings suggest that resources to address concerns related to spirituality, sexuality and intimacy, and managing cancer-related physical and psychosocial symptoms must be provided differentially by the patients’ age, reflecting typical developmental tasks.
Cancer can cause patients to question fundamental assumptions about the meaning of their lives, the phenomena were widely addressed but the majority focused on adult patients [25]. As only 1% of cancer occurs in children [1], HCPs may evaluate the existential issues related to forming self-identity and meaning of life raised by the pediatric cancer diagnosis as larger to the patients than patients of other ages and to their caregivers. As part of the initiative for pediatric palliative care [26], spiritual concerns are far less met for children with cancer than their caregivers. The unmet spiritual need may be attributed to the cognitive maturity of the patients [26] or HCPs’ ability to communicate these needs with patients in cognitive developmental age. The way to help patients find a positive meaning from cancer experience and search for answers to existential questions depends on the developmental stage [26]. HCPs with related training can promote a deep discussion about this topic with their patients. In addition, these issues occur after treatment completion and when patients return to their lives [25]. To facilitate spiritual aspects of care, HCPs should consider spiritual need as an issue beyond active treatment phase, and continually emphasize sense of peace and hope in their pediatric patients.
Similarly, the concern of the pediatric cancer and its treatment impair future fertility [27] may stand out to HCPs as far more crucial for pediatric patients than any patients in other age groups and the caregivers of pediatric patients, yet not consistently discussed with pediatric patients. Our finding is consistent with existing studies documenting that HCPs rarely discuss such issues with their patients [28], HCPs’ likelihood of discussing fertility preservation that is critical to long-term quality of life has been impeded by perceived risks, such as upsetting patients, the belief that erotic materials during semen collection should not be given for patients under 18, and difficulty locating facilities for fertility preservation [27].
Patient sexuality is not limited to fertility, it’s an experience affecting the sense of self, body image, and most importantly, ability to intimately connect with others [28]. HCPs’ capability to address these issues has been limited by time, experience, and embarrassment to discuss sexual matters [28]. Therefore, assessing barriers impeding HCPs’ capacity and skills to provide practical information and emotional support to assist pediatric patients to adapt to sexual and intimate changes after cancer is imperative.
Another critical need evaluated to be unlikely met among pediatric patients is disturbed sleep and fatigue, which was more so than among patients in other age groups and their caregivers. Accumulating evidence suggests that sleep problem is a significant concern in children with cancer due in part to cancer and treatment-related factors as well as the psychological stress. Along with other complications of cancer, sleep disturbances and fatigue, are concerted effects of medical and psychological complications and adversely impact patients’ quality of life and predispose them to worse medical outcomes [29]. Oncology HCPs are encouraged to form a multidisciplinary team to provide adequate care including cognitive-behavioral intervention for managing sleep problems of pediatric patients.
Difference in unmet needs for symptom management was found in adolescent and young adult (AYA) patients vs their caregivers, implying that HCPs recognized their capacity to address symptom management needs were limited for AYA compared with for their caregivers. Literature has documented that AYA cancer patients report substantial symptomatology in physical and cognitive function impairment, as a result of their disease and persist after completion of cancer therapy [30, 31]. Managing the symptoms can be a heavy burden for AYA patients while they are struggling with developmental priority regarding educational/work attainment and social/romantic relationships. They may be a vulnerable group who needs more helps in managing therapy-related sequelae, and healthcare providers should anticipate this need to provide timely interventions to ameliorate symptoms.
Besides the above-mentioned unmet needs, this study found that HCPs perceived most unmet needs between patients and caregivers were at comparable levels, regardless of patients’ age group. These findings were consistent with previous studies indicating cancer patients and the caregivers identified comparable unmet needs in commonly reported areas [11, 12]. On the other hand, we did not find any differences between patients and caregivers on patients’ age group of middle-aged and older adults.
The current study focuses on unmet needs of cancer patients globally, and the sample consists of more than half (59%) of HCPs from low-to-middle-income countries (LMICs). Cancer has received considerable public and research attention in high-income countries (HICs), with little research conducted in LMICs [32]. Although the overall incidence of cancer is lower in developing countries compared with developed countries, total cancer-related mortality is significantly higher in developing countries because investments in cancer diagnosis and treatment vary depending on the resources available in the country [32]. The rising care cancer burden in developing countries stresses already weak health infrastructures and poses health care challenges to these countries. The high cost of many cancer interventions makes whole-person cancer care less feasible and implementable in LMICs. It is imperative to address the global cancer unmet needs beyond the focus of HICs. As we know that management of the cancer burden in LMICs requires global partnerships between cancer-care mentors from HICs and local HCPs familiar with the specific culture, this study presents an initial step toward understanding the global cancer care burden. The inequities of cancer care around the world have prompted integrated global cancer initiatives implemented by more than 200 partners around the world. Knowledge about cancer care needs globally is imperative. Focusing on the unmet needs of cancer patients from LMICs merit future research attention. Especially countries experiencing geopolitical conflicts, domestic political turmoil, or war today are underrepresented in this study. Such neglect calls for future attention to the area with social instability and insecurity, which cause greater cancer burdens and unmet needs.
We are also aware that the perception of unmet needs is influenced by tradition, culture, and societal values. For example, truth-telling is not well executed in more conservative societies, resulting in difficult medical decision-making and doctor-patient communication [33]. Cultural misperceptions about cancer also prevailed among many countries. Cancer fatalism, a belief that everything in the course of cancer and cancer outcome is “God’s will or fate”, is prevailing in Asia, Middle Eastern, and Hispanic groups [34]. Irrational fatalism may reduce participation in health care interventions. In addition, a diagnosis of cancer is still mixed with social stigma in some countries such as India and the greater Middle East [34]. It is important to recognize the influence of culture and health practice belief systems on the reporting of certain unmet needs and accessibility of available resources. This is not to presume that there are no unmet psychological needs in more open western societies. Similar problems exist in rural underserved areas and ethnic minorities. Future studies are needed to fully elucidate the cultural issues of cancer unmet needs.
While the current study focuses on unmet needs of cancer patients globally, we should aware that these needs were influenced by sociodemographic factors such as age, gender, and income level; and clinical factors such as cancer stage, type of cancer, and treatment modules. Moreover, health care systems are highly dependent on resources, infrastructure, and cultural values, these contextual factors may vary widely between countries. Due to the sample size, none of the countries have sufficient samples to make meaningful comparisons at the country level. Exploring the interplay between countries and cultures on the unmet needs is a critical future direction. As we found that age is a significant moderator, future studies should compare the unmet needs by countries among different patient age groups.
The results of this study should be interpreted with additional caution. First, the unmet needs were based on perspectives of HCPs’ reports, thus the concordance between HCPs’ report of unmet needs and patients’ and caregivers’ reports is unknown. However, HCPs’ perspectives have their own values. HCPs’ reports of unmet needs reflect that they consider those needs to be important but also recognize deficiencies in means to help fulfilling these needs of their patients and caregivers. Systematic evaluation at the institutional level to identify resources and modification of existing services to reduce the gap is warranted.
Second, as our online survey allowed participants to skip irrelevant questions and sections, less than 30% fully completed the survey, particularly the section on family caregivers’ unmet needs, which reduces the statistical power for this study. The small sample size also did not allow sub-group analyses with regard to participants’ countries, dripline, or job duration. In addition, the needs of patients and caregivers may change over time. Investigation of the degree to which unmet needs change along the cancer illness trajectory is warranted.
We aimed to develop a holistic picture of the health professionals’ perspectives from a multidisciplinary panel of experts and the majority of participants had experience working with cancer patients or their caregivers for more than 2 years to represent rather broad perspectives. However, almost half of the participants were counselors or psychologists. The key findings may reflect priority areas from the lens of psychological or counseling discipline.
Clinical implications
Despite these limitations, this study is novel as it systematically assesses on HCPs’ perspectives about the unmet needs vary by patients’ age cohorts and differ between patients and caregivers. The survey sheds light on international collaboration in psycho-oncology research to inform clinical practice and policies aiming to address the unmet needs of cancer patients and their family caregivers. Thus, the study provides information that may be valuable in identifying areas of unmet needs where screening and interventions could be developed, especially for pediatric and AYA cancer patients.
The current study highlights the need to address concerns in spiritual concerns, sexuality, and insomnia facing pediatric cancer patients. Whether the significant disparities in these unmet needs by age group are a result of barriers in accessibility to, availability of, or capacity of corresponding services should be assessed. The results have shown that HCPs recognize themselves play a key role in facilitating appropriate intervention. Guidelines should be established to address these needs and trainings for HCPs to communicate and support their pediatric patients with these needs are imperative. Implementing such guidelines can increase awareness of those needs and enhance services targeting those needs. A published guideline, such as The Children’s Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood [35], is encouraged broaden the application of the guideline to include sexual, spiritual, and sleep concerns as late effects of pediatric cancer treatment and include them in patient education materials.
Conclusions
Exploring HCPs’ perspectives is a critical step to understand their opportunities and challenges of supporting their patients in achieving their developmental milestones and caregivers in their institutions. With the increasing awareness of treating the whole cancer patient, significant challenges remain in addressing pediatric and AYA unmet needs. The discovered unmet needs are central to the development and provision of effective targeted services.
Supplementary Material
Funding
The writing of this manuscript was supported by the National Institute of Nursing Research (R01NR016838) to YK.
Footnotes
Competing interests The authors declare no competing interests.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s00520-022-07478-5.
Ethics approval and consent to participate This is a non-human subject study as we did not collect any personal identifiable information. IRB Exempt approval is attached.
Consent for publication Not applicable’ for that section.
References
- 1.Sung H, Ferlay J, Siegel RL et al. (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin 71(3):209–249 [DOI] [PubMed] [Google Scholar]
- 2.Hansen DG, Larsen PV, Holm LV, Rottmann N, Bergholdt SH, Søndergaard J (2013) Association between unmet needs and quality of life of cancer patients: a population-based study. Acta Oncol 52(2):391–399 [DOI] [PubMed] [Google Scholar]
- 3.De Padova S, Grassi L, Vagheggini A et al. (2021) Post-traumatic stress symptoms in long-term disease-free cancer survivors and their family caregivers. Cancer Med 10(12):3974–3985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P (2013) Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol 14(8):721–732 [DOI] [PubMed] [Google Scholar]
- 5.Holland JC, Andersen B, Breitbart WS et al. (2013) Distress management. J Natl Compr Canc Netw 11(2):190–209 [DOI] [PubMed] [Google Scholar]
- 6.Kent EE, Rowland JH, Northouse L et al. (2016) Caring for caregivers and patients: research and clinical priorities for informal cancer caregiving. Cancer 122(13):1987–1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puts M, Papoutsis A, Springall E, Tourangeau A (2012) A systematic review of unmet needs of newly diagnosed older cancer patients undergoing active cancer treatment. Support Care Cancer 20(7):1377–1394 [DOI] [PubMed] [Google Scholar]
- 8.Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ (2009) What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer 17(8):1117–1128 [DOI] [PubMed] [Google Scholar]
- 9.Lisy K, Langdon L, Piper A, Jefford M (2019) Identifying the most prevalent unmet needs of cancer survivors in Australia: a systematic review. Asia Pac J Clin Oncol 15(5):e68–e78 [DOI] [PubMed] [Google Scholar]
- 10.Kim Y, Kashy DA, Spillers RL, Evans TV (2010) Needs assessment of family caregivers of cancer survivors: three cohorts comparison. Psycho-Oncol: Journal of the Psychological, Social and Behavioral Dimensions of Cancer 19(6):573–582 [DOI] [PubMed] [Google Scholar]
- 11.Lambert SD, Harrison JD, Smith E et al. (2012) The unmet needs of partners and caregivers of adults diagnosed with cancer: a systematic review. BMJ Support Palliat Care 2(3):224–230 [DOI] [PubMed] [Google Scholar]
- 12.Wang T, Molassiotis A, Chung BPM, Tan J-Y (2018) Unmet care needs of advanced cancer patients and their informal caregivers: a systematic review. BMC Palliat Care 17(1):1–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sklenarova H, Krümpelmann A, Haun MW et al. (2015) When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer 121(9):1513–1519 [DOI] [PubMed] [Google Scholar]
- 14.Kim Y, Carver CS, Ting A, Cannady RS (2020) Passages of cancer caregivers’ unmet needs across 8 years. Cancer 126(20):4593–4601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharpe L, Butow P, Smith C, McConnell D, Clarke S (2005) The relationship between available support, unmet needs and caregiver burden in patients with advanced cancer and their carers. Psycho-Oncol: Journal of the Psychological, Social and Behavioral Dimensions of Cancer 14(2):102–114 [DOI] [PubMed] [Google Scholar]
- 16.Philip J, Collins A, Brand CA et al. (2015) Health care professionals’ perspectives of living and dying with primary malignant glioma: implications for a unique cancer trajectory. Palliat Support Care 13(6):1519–1527 [DOI] [PubMed] [Google Scholar]
- 17.Franklin M, Patterson P, Allison KR, Rosso-Buckton A, Walczak A (2018) An invisible patient: Healthcare professionals’ perspectives on caring for adolescents and young adults who have a sibling with cancer. Eur J Cancer Care 27(6):e12970. [DOI] [PubMed] [Google Scholar]
- 18.Holland JC, Rowland JH (1989) Handbook of psychooncology: psychological care of the patient with cancer. Oxford University Press [Google Scholar]
- 19.Schmid-Büchi S, Halfens RJ, Müller M, Dassen T, van den Borne B (2013) Factors associated with supportive care needs of patients under treatment for breast cancer. Eur J Oncol Nurs 17(1):22–29 [DOI] [PubMed] [Google Scholar]
- 20.Griesser AC, Vlastos G, Morel L, Beaume C, Sappino AP, Haller G (2011) Socio-demographic predictors of high support needs in newly diagnosed breast cancer patients. Eur J Cancer Care 20(4):466–474 [DOI] [PubMed] [Google Scholar]
- 21.Abdollahzadeh F, Moradi N, Pakpour V et al. (2014) Un-met supportive care needs of Iranian breast cancer patients. Asian Pac J Cancer Prev 15(9):3933–3938 [DOI] [PubMed] [Google Scholar]
- 22.Kim Y, Ting A, Carver CS, et al. (2022) International collaboration for assessing unmet needs of cancer survivors and family caregivers: lens of healthcare professionals. Psycho-Oncol [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Capture RED. https://projectredcap.org/software/ [Google Scholar]
- 24.Gordon LG, Merollini K, Lowe A, Chan RJ (2017) A systematic review of financial toxicity among cancer survivors: we can’t pay the co-pay. Patient-Patient-Centered Outcomes Res 10(3):295–309 [DOI] [PubMed] [Google Scholar]
- 25.Barata A, Wood WA, Choi SW, Jim HS (2016) Unmet needs for psychosocial care in hematologic malignancies and hematopoietic cell transplant. Curr Hematol Malig Rep 11(4):280–287 [DOI] [PubMed] [Google Scholar]
- 26.Meireles CB, Maia LC, Miná VAL, et al. (2015) Influence of spirituality in pediatric cancer management: a systematic review. Int Arch Med 8(35) [Google Scholar]
- 27.Vadaparampil S, Quinn G, King L, Wilson C, Nieder M (2008) Barriers to fertility preservation among pediatric oncologists. Patient Educ Couns 72(3):402–410 [DOI] [PubMed] [Google Scholar]
- 28.Hordern AJ, Street AF (2007) Communicating about patient sexuality and intimacy after cancer: mismatched expectations and unmet needs. Med J Aust 186(5):224–227 [DOI] [PubMed] [Google Scholar]
- 29.Kaleyias J, Manley P, Kothare SV (2012) Sleep disorders in children with cancer. Semin Pediatr Neurol 19(1):25–34 [DOI] [PubMed] [Google Scholar]
- 30.Geue K, Sender A, Schmidt R et al. (2014) Gender-specific quality of life after cancer in young adulthood: a comparison with the general population. Qual Life Res 23(4):1377–1386 [DOI] [PubMed] [Google Scholar]
- 31.Prasad PK, Hardy KK, Zhang N et al. (2015) Psychosocial and neurocognitive outcomes in adult survivors of adolescent and early young adult cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol 33(23):2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shah SC, Kayamba V, Peek RM Jr, Heimburger D (2019) Cancer control in low-and middle-income countries: is it time to consider screening? J Global Oncol 5:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baider L, Goldzweig G (2016) The magic of dreams: conflicts and quandaries within multicultural societies in transition. In: Cancer care in countries and societies in transition. Springer; 47–64 [Google Scholar]
- 34.Ashraf MS, Jamil A (2016) Cancer care in Pakistan. In: Cancer Care in Countries and Societies in Transition. Springer; 231–245 [Google Scholar]
- 35.Landier W, Bhatia S, Eshelman DA et al. (2004) Development of risk-based guidelines for pediatric cancer survivors: the children’s oncology group long-term follow-up guidelines from the children’s oncology group late effects committee and nursing discipline. J Clin Oncol 22(24):4979–4990 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


