Abstract
Functional dyspepsia (FD) is a common and frequently occurring disease in clinic. With the influence of environmental factors, social factors and dietary factors, the incidence rate of FD in the general population is yearly increasing. Traditional Chinese medicine has a long history and far-reaching influence in the treatment of FD. It can prevent and treat FD in the form of multiple-components, targets and channels, with obvious effect and prominent advantages. This article starts with the common syndrome types of FD, and discusses the research progress of single Chinese medicine, effective ingredients and the mechanism of traditional Chinese medicines in treating FD, in order to provide a theoretical basis for the treatment of FD with traditional Chinese medicines.
Keywords: action mechanisms, Banxia Xiexin Decoction, Chaihu Shugan Powder, functional dyspepsia, traditional Chinese medicines, Zhizhu Pills
1. Introduction
Functional dyspepsia (FD) is a digestive system disease without obvious organic lesion, which refers to a group of clinical syndromes caused by gastric and duodenal dysfunction (Colak et al., 2022, Vanner et al., 2016). The prevalence of FD in Asia is as high as 8%–23% (Ghoshal et al., 2011). The central symptoms of FD now contain not only epigastric pain and burning, but also postprandial fullness, and early satiation at above the “bothersome” level (Suzuki, 2020). At present, there are many theories about the pathogenesis of FD. It is generally believed that the formation of FD may be related to the increase of gastric emptying time to food, the uncoordinated movement of stomach and duodenum, the decrease of gastric sensory capacity, Helicobacter pylori infection, and the decrease of gastric fundus's receptivity to food under the influence of various factors. Its pathological characteristics are mainly reflected in the abnormal sensory signal of gastrointestinal tract (Christine, 2016), the interaction disorder of brain gut axis (Yang et al., 2021), and the abnormal regulation of anterior cingulate cortex response area (Lee et al., 2022, Liu et al., 2018). There is no specific name for FD in the ancient books of Chinese medicine. According to the clinical manifestations of FD, it can be classified as “fullness”, “stomachache”, “abdominal distension” and other diseases (Li, Chen, & Li, 2017). It is believed that FD is closely related to the liver, spleen and stomach (Xiao, Wu, Wang, Li, & Fang, 2015), and water drinking, phlegm dampness and blood stasis are the main pathological factors (Jin & Liu, 2019).
Currently, the commonly used therapeutic drugs for FD include antacids, gastrointestinal motility promoting drugs, antidepressants and so on (Madisch et al., 2018). However, with the long-term use of large quantities of drugs, there are still many problems such as monotonous treatment plan and poor treatment effect (Wang, Herndon, & Lu, 2020). Therefore, the use of chemical medicine alone in the treatment of FD has certain limitations. Traditional Chinese medicine (TCM) has a long history and far-reaching influence in treating FD. Some studies have shown that TCMs can play a therapeutic role by regulating cell apoptosis, inhibiting inflammatory reaction, regulating hormone level, maintaining intestinal flora diversity, improving visceral sensitivity and other ways, with definite efficacy, fewer adverse reactions and low recurrence rate (Lin et al., 2012, Wang et al., 2021). In recent years, TCM has played an important role in the treatment of FD.
According to the clinical and basic research of many scholars in recent years, the treatment of FD with TCMs can be summarized into five syndrome types (Table 1): liver-stomach disharmony, spleen deficiency with qi stagnation, syndrome of intermingled heat and cold, dampness-heat of spleen and stomach, and deficiency-cold of spleen and stomach (Li, Chen, & Li, 2017). According to these five syndrome types, we have achieved satisfactory results in clinical and experimental research through syndrome differentiation and treatment with TCMs. This article starts with these five syndrome types, and discusses the research progress of the mechanism of action of single Chinese medicine, effective ingredients and responsible compounds in treating FD related to these five syndrome types, in order to provide a theoretical basis for the treatment of FD with Chinese medicine.
Table 1.
Cardinal symptoms and secondary symptoms in five syndrome types.
| Five syndrome types | Cardinal symptoms | Secondary symptoms |
|---|---|---|
| Liver-stomach disharmony | Gasteremphraxis, hypochondriasis | Xerostomia, bitterness, irritability, etc |
| Spleen deficiency with qi stagnation | Abdominal distension, anorexia | Weakness, nausea, vomiting, etc |
| Syndrome of intermingled heat and cold | Gasteremphraxis, coldness in the stomach | Xerostomia, bitterness, diarrhoea, etc |
| Dampness-heat of spleen and stomach | Abdominal distension, anorexia | Dizzy, discomforting evacuation, etc |
| Deficiency-cold of spleen and stomach | Stomachache, coldness in the stomach | Weakness, diarrhoea, etc |
2. Etiology and pathogenesis of FD in TCM
2.1. Liver-stomach disharmony
TCM believes that the liver is the source of relieving the internal organs and promoting the smooth flow of qi. If the liver qi is not smooth, the qi mechanism will be stagnant. If the wood is flourishing, the disease will occur. In clinical practice, many experts regard disharmony between liver and stomach as the main pathogenesis of FD. Song et al. showed that disharmony between liver and stomach is the most important syndrome type of FD by using prospective and multicenter research methods (Song et al., 2020). Also, through many years of clinical experience, Professor Wei Wei concluded that stagnation of liver qi is the key to the onset of FD, which damages the stomach, leading to disharmony between liver and stomach (Luo et al., 2021).
2.2. Spleen deficiency with qi stagnation
The spleen and stomach are the hub for the movement of qi in and out of the human body. The deficiency of spleen qi leads to the biochemical disorder of qi and blood. If there is no source of biochemistry, the movement of qi and stomach will be lost, leading to qi stagnation, phlegm, water dampness and many other pathological products. Professor Chun Gan believes that the pathogenesis of FD is essentially weakness of the spleen and stomach (Yan & Gan, 2021). At the same time, qi stagnates in the middle energizer, and qi is not smooth. The basic pathogenesis of spleen deficiency and qi stagnation runs through FD all the time. Yang et al also believed that the weakness of the spleen and stomach was the cause of many diseases. On the basis of the weakness of the spleen and stomach, phlegm, blood stasis and fluid intake were important factors that led to the onset and progression of FD (Yang & Li, 2019).
2.3. Syndrome of intermingled heat and cold
The spleen and stomach are the acquired foundation of the human body. When the spleen rises, the stomach falls. Eating raw cold wantonly will hurt the function of the spleen and stomach, produce wet turbidity, and then transform into heat, resulting in mixed cold and heat. Syndrome of intermingled heat and cold is also an important pathogenesis of FD. Li et al. believed that the main pathogenesis of FD was the mixture of cold and heat (Li, Wei, & Yang, 2015). This disease was caused by the interaction of spleen cold and stomach heat, which blocked the middle energizer (Shi & Chang, 2016). Li et al. also believed that the onset of FD was mostly cold and warm, which hurt the spleen and stomach, causing stagnation of qi and difficulty in running qi and blood, thus producing many pathological products (Li, Wei, & Yang, 2015).
2.4. Dampness-heat in spleen and stomach
Dampness and heat are inherent in the spleen and stomach, and the qi mechanism is unfavorable. The clear qi does not rise, the turbid qi does not fall, and the damp and turbid qi turn into heat. Therefore, we can see the symptoms related to FD, such as abdominal fullness and discomfort, and sticky discomfort in the mouth. According to modern epidemiological research, it is found that dampness-heat is the most common physical type of FD patients, and it is the most significant in the spleen and stomach (Li, 2017). At the same time, Xu et al. also believed that dampness heat in the spleen and stomach was the key to the onset of FD (Xu et al., 2013). Patients who ate fat, sweet and thick tasting food indiscriminately would suffer from this disease if the dampness was turbid and the spleen was trapped.
2.5. Deficiency-cold of spleen and stomach
This syndrome is often caused by overeating cold food, which damages the yang qi of the spleen and stomach, so it causes many symptoms such as stupidity, vomiting, loose discharge, etc. In clinic, the patients with FD are mainly of insufficiency-cold in spleen and stomach, which is also an important pathogenesis in the development of FD. Liu (2021) believes that spleen stomach deficiency cold is an important pathogenesis of FD, and on the basis of deficiency cold, it also has many pathological products such as phlegm dampness and water drinking. In addition, some scholars discussed the main characteristics of FD patients, which showed that the pathogenesis of FD patients was deficiency-cold of spleen and stomach (Junghyo, Yochan, Dongsoo, & Changgue, 2013).
3. Therapeutic effect of TCM on FD and its related mechanisms
3.1. Treatment for smoothing liver and regulating stomach
3.1.1. Single herb and effective ingredients
Hordei Fructus Germinatus (Maiya in Chinese) is the mature fruits of Hordeum vulgare L., which has been germinated and dried. It can soothe the liver and stomach, strengthen the spleen and broaden the body. Through clinical observation and research, Tian et al. found that stir-fried Hordei Fructus Germinatus can increase gastric juice secretion, regulate gastrointestinal function, and play a significant role in improving the symptoms of FD patients (Tian, Liu, & Chen, 2017). Wu et al. further clarified the material basis of Hordei Fructus Germinatus for anti-functional dyspepsia (Wu et al., 2020). Through relevant experimental studies, they confirmed that its main effective substances are Maillard reaction products (MRPs). The role of MRPs in regulating brain gut peptides and intestinal flora can achieve the prevention and treatment of FD, which provides the corresponding theoretical basis for the treatment of FD with Hordei Fructus Germinatus.
Aucklandiae Radix (Muxiang in Chinese) can soothe the liver, regulate qi, and relieve stomach pain. Some scholars have verified through experiments that Aucklandiae Radix can regulate gastric acid secretion, accelerate gastric emptying rate, accelerate motilin release, and regulate gastrointestinal movement of FD mice (Chen et al., 1994, Ma, 2021). Lignanolide, a ingredient from Aucklandiae Radix, which can also relax gastrointestinal smooth muscle, relieve spasm, relieve pain, and treat gallbladder, so as to improve the related symptoms of FD patients (Wang, Wang, Mao, Zhang, & Huang, 2001).
3.1.2. Representative prescriptions
Chaihu Shugan Powder is composed of seven traditional Chinese medicines, including Citri Reticulatae Pericarpium (Chenpi in Chinese), Bupleuri Radix (Chaihu in Chinese), Chuanxiong Rhizoma (Chuanxiong in Chinese), Paeoniae Radix Alba (Baishao in Chinese), Cyperi Rhizoma (Xiangfu in Chinese), Aurantii Fructus (Zhiqiao in Chinese), Glycyrrhizae Radix et Rhizoma (Gancao in Chinese). Modern pharmacology believes that Chaihu Shugan Powder has many functions such as promoting gastric emptying, regulating gastrointestinal motility, improving depression and reducing inflammation, and it has a good effect on relieving clinical symptoms of FD (Wang et al., 2021). Li et al. observed the effect of Chaihu Shugan Powder on gastric motility, gastric tissue mitochondrial function and mitophagy in FD model rats (Li, Jia, Wang, Wang, & Ling, 2021). Finally, it was found that the mechanism of Chaihu Shugan Powder in preventing and treating FD may be related to the improvement of mitochondrial function in gastric tissue and the inhibition of mitophagy. Luo et al. observed the response of different concentrations of Chaihu Shugan Powder to FD rats, and finally concluded that the mechanism of Chaihu Shugan Powder in the treatment of FD may be related to its ability to regulate the endoplasmic reticulum stress molecule glucose-regulated protein (GRP78), and c-Jun amino-terminal kinase (c-JNK) is closely related (Luo & Ling, 2019). In addition, some studies have shown that Chaihu Shugan Powder can also inhibit the excessive autophagy of Cajal interstitial cells in the gastric antrum muscle (Zeng et al., 2017), inhibit gastric smooth muscle injury caused by abnormal activation of NF-κB apoptosis signaling pathway (Shangguan, 2017), and it also can inhibit the expression of endoplasmic reticulum stress molecules inositol-requiring enzyme 1 (IRE1) and tumor necrosis factor receptor-associated factor 2 (TRAF2) (Xu et al., 2018), so as to achieve the prevention and treatment of FD.
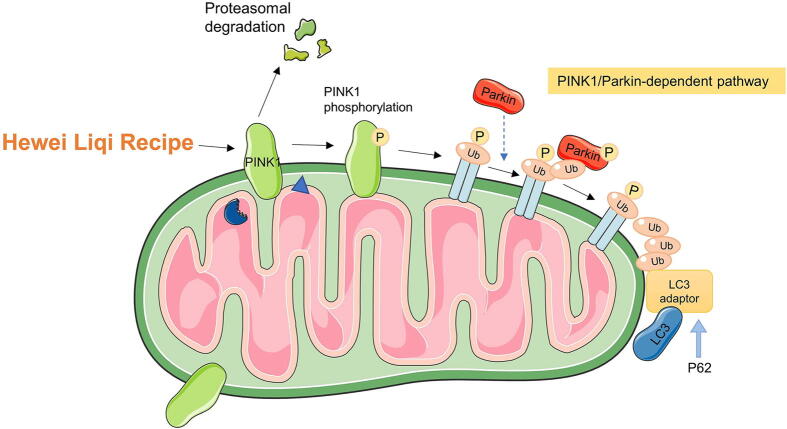
Hewei Liqi Recipe is composed of Bupleuri Radix (Chaihu in Chinese), Codonopsis Radix (Dangshen in Chinese), Aurantii Fructus Immaturus (Zhishi in Chinese), Aucklandiae Radix (Muxiang in Chinese), Magnoliae Officinalis Cortex (Houpo in Chinese), Citri Reticulatae Pericarpium (Chenpi in Chinese), Amomi Fructus Rotundus (Doukou in Chinese), and Glycyrrhizae Radix et Rhizoma (Gancao in Chinese). It is used to soothe the liver and stomach, and regulate qi. Bai (2021) observed the effect of Hewei Liqi Recipe on FD rats from the perspective of mitochondrial autophagy. The results showed that Hewei Liqi Recipe improved the activation of AMPK pathway by downregulating the expression of mitochondrial autophagy related pathway proteins PINK1, Parkin, P62, LC3, AMPK, ACC, S6K, and confirmed that AMPK and its downstream target substances participated in mitochondrial autophagy induced by PINK1/Parkin pathway. Hewei Liqi Recipe can regulate the expression of AMPK and its downstream target substances, thereby regulating PINK1/Parkin pathway to reduce mitochondrial autophagy and alleviate the symptoms of functional dyspepsia in rats (Fig. 1).
Fig. 1.
Mechanism of Hewei Liqi Recipe on PINK1/Parkin pathway in treating FD.
3.1.3. Clinical application
Wang et al. used the method of systematic evaluation to compare the effect of liver and stomach soothing TCMs and motivators in the treatment of FD (Wang et al., 2012). The final results showed that the effective rate of TCMs was significantly higher than that of western medicine group. Wei et al. observed the effect of Chaizhi Pinggan Decoction on patients with FD. The results showed that Chaizhi Pinggan Decoction could regulate the levels of gastrointestinal hormones and serum neuropeptide S-receptor-1 in patients with FD, and improve the clinical efficacy (Wei, Wei, & Yuan, 2021). Yang et al. observed that Chaihu Shugan Powder was used to treat patients with functional FD (disharmony between liver and stomach), and the results showed that the Chinese medicine group could significantly improve the clinical symptoms of FD patients, and the effective rate was higher than that of the western medicine group, with no adverse reactions and high safety (Yang et al., 2013).
3.2. Treatment for strengthening spleen and promoting qi stagnation
3.2.1. Single herb and effective ingredients
Aurantii Fructus Immaturus is from cultivars of Citrus aurantium L. or the dry young fruits of Citrus sinensis Osbecks, which was first found in Shennong’s Classic of Materia Medica. It has the effect of invigorating the spleen, promoting qi and resolving phlegm, and is often used to treat FD, gastroptosis, constipation and other diseases. Some studies have shown that Aurantii Fructus Immaturus can play a role in the treatment of FD by regulating cell apoptosis, inhibiting inflammatory response, regulating gastrointestinal activity and emotional state (Wang et al., 2022). Through experimental studies, Deng et al. found that Aurantii Fructus Immaturus can enhance the expression of c-Kit and serum stem cell factor (SCF), activate the SCF/c-Kit signaling pathway, and then promote the proliferation of Cajal interstitial cells, thereby improving gastrointestinal motility disorders of FD rats (Deng et al., 2018). At the same time, it can also strengthen spleen and promote qi stagnation, relieve constipation, abdominal distension, nausea and other symptoms. In addition, Wang et al. found that Aurantii Fructus Immaturus can effectively regulate the intestinal flora of FD rats, correct its disordered state, and at the same time support the growth of beneficial intestinal bacteria and inhibit the reproduction of harmful bacteria, which can play a therapeutic role (Wang et al., 2021). In addition to the above mechanisms of action, Aurantii Fructus Immaturus can also increase the secretion of motilin, gastrin (GAS), and vasoactive peptide substances, thereby reducing somatostatin, thereby relieving gastrointestinal motility disorders and improving FD-related clinical symptoms (Lin et al., 2012, Zhang and Li, 2018). Li et al. studied the effect of Aurantii Fructus Immaturus on FD rats, and found that it can improve the visceral hypersensitivity of FD model rats, and the mechanism of action may be related to the regulation of 5-hydroxytryptamine (5-HT) and c-fos expression (Li et al., 2016). Wu et al. also confirmed that Aurantii Fructus Immaturus has a certain regulatory effect on the adaptability of the proximal stomach of FD rats (Wu et al., 2016). When the concentration reached 6 mg/mL or 10 mg/mL, the longitudinal smooth muscle tension of proximal gastric corpus decreased with the increase of Aurantii Fructus Immaturus. The mechanism may be related to reducing the smooth muscle tone of the proximal gastric corpus. In addition, Huang et al. also confirmed that Aurantii Fructus Immaturus can improve gastric emptying and intestinal propulsion in FD rats, and increase the release of MTL (Huang, Chi, Zeng, & Lu, 2012). The above studies confirmed that Aurantii Fructus immaturus and its effective components can prevent and control FD through various ways.
Arecae Semen (Binlang in Chinese) is a dry ripe seed. And it also known as big belly and belongs to the stomach and large intestine meridians. It has the effect of promoting qi, strengthening spleen and treating malaria. Arecae Semen in the treatment of FD mainly works by enhancing gastrointestinal motility and regulating gastrointestinal hormones. For example, Zou et al. studied the effects of Arecae Semen extract on gastrointestinal motility and gastrointestinal motility in FD rats, and the results showed that Arecae Semen could enhance gastric motility and smooth muscle contraction in FD rats, thereby achieving the effect of treating FD (Zou, Dong, Wei, & Wei, 2007). At the same time, Arecae Semen can regulate the secretion of gastrointestinal peptide hormones in FD rats, which can significantly increase motilin (MTL) and significantly decrease vasoactive intestinal peptide (VIP), which can significantly promote the gastrointestinal activity of FD rats (Zou, Wei, & Yuan, 2004).
Galli Gigerii Endothelium Corneum (Jineijin in Chinese) is the dry gizzard intine of Gallus gallus domesticus Brisson. It was first recorded in the Shennong’s Classic of Materia Medica, and it was listed as the top grade. And it has the functions of strengthening the stomach and eliminating food, astringent essence and stopping constipation, and clearing fossils. It is used for indigestion, vomiting, diarrhea, enuresis, nocturnal emission, gallstones and many other diseases. The treatment of FD by Galli Gigerii Endothelium Corneum mainly works by improving gastrointestinal motility, improving intestinal propulsion, and regulating the expression of pepsin. Li et al. explored the effect of Galli Gigerii Endothelium Corneum extract on the activity of pepsin and gastric juice secretion in rats, and the results showed that the gastric juice volume of Jineijin group and blank was significantly improved, and there was a significant difference, so it is speculated that the Galli Gigerii Endothelium Corneum can play a therapeutic effect on FD by increasing the secretion of gastric juice and improving the activity of pepsin (Li, Li, Li, Peng, & Li, 2008). In addition, Galli Gigerii Endothelium Corneum can also enhance gastric emptying and small intestinal propulsion rate, increase GAS and motilin, and up-regulate the protein expression of aquaporin 4 (AQP4) in gastric tissue in FD model rats. Also it can reduce the expression level of constitutive nitric oxide synthase (cNOS) in gastric tissue, thereby improving gastrointestinal function in FD model rats (Shen, Huang, & Yuan, 2019).
3.2.2. Representative prescriptions
Simo Decoction is composed of four traditional Chinese medicines: Ginseng Radix et Rhizoma (Renshen in Chinese), Arecae Semen, Aquilariae Lignum Resinatum (Chenxiang in Chinese), and Linderae Radix (Wuyao in Chinese). The main function is to promote qi and reduce inversion, widen the chest and disperse knots. Clinical studies have shown that Simo Decoction can significantly improve the postprandial fullness, hiccups and other clinical symptoms of FD patients, with fewer adverse reactions and higher safety (Deng et al., 2022). Zhang et al. used network pharmacology and molecular docking to explore the mechanism of action of Simo Decoction in the treatment of FD (Zhang, Zhong, Ao, & Chen, 2020). Qiu et al. established a rat model of FD by gavage of iodoacetamide, solitary rearing and sleep deprivation by platform standing, and observed the relationship between Simo Decoction and RhoA and ROCK in gastric tissue of FD rats, and finally found that Simo Decoction can regulate RhoA and the expression of ROCK to achieve the therapeutic effect on FD (Qiu et al., 2022). In addition, Simo Decoction can also adjust the content of NO, AchE, CCK and SP substances in serum, fundus, gastric antrum and duodenum to achieve the effect of treating FD (Zhou, Cai, & Wang, 2015).
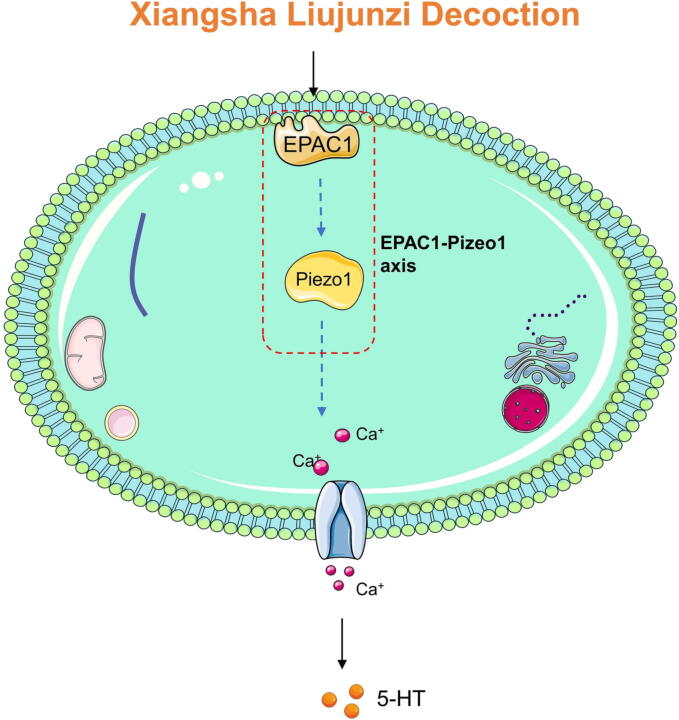
Xiangsha Liujunzi Decoction is composed of six herbs including Aucklandiae Radix, Amomi Fructus (Sharen in Chinese), Ginseng Radix et Rhizoma, Atractylodis Macrocephalae Rhizoma (Baizhu in Chinese), Poria (Fuling in Chinese) and Glycyrrhizae Radix et Rhizoma. It has the effect of invigorating qi and spleen, promoting qi and resolving phlegm. Clinical studies have shown that Xiangsha Liujunzi Decoction can significantly improve the clinical symptoms and quality of life of patients with FD, with high safety and fewer adverse reactions (Luv et al., 2017). Liu et al. evaluated the effect of Xiangsha Liujunzi Decoction on FD through food intake, sucrose preference test and electromyography (Liu et al., 2015). The results showed that the prescription could alleviate the symptoms of FD by increasing the production of ghrelin, CCK and VIP and by increasing the levels of these neuropeptides in the circulation. Shi (2019) established a rat model of FD by gavage with iodoacetamide, and observed the effect of Xiangsha Liujunzi Decoction on FD rats. The results found that Xiangsha Liujunzi Decoction could interfere with EC cells through the EPAC1-PIEZO2 axis. The release of 5-HT, thereby reducing the degree of visceral hypersensitivity, indicates that it has a better preventive and therapeutic effect on FD (Fig. 2). In addition, Xiangsha Liujunzi Decoction can also rebuild the mitochondrial quality control system by inhibiting PINK1/Parkin mediated mitochondrial self-discipline and division, and improve gastrointestinal motility disorder in FD patients (Zhang, Wang, Wang, & Tang, 2022).
Fig. 2.
Mechanism of Xiangsha Liujunzi Decoction in preventing FD from acting on EPAC1-PIEZO2 Axis.
Zhizhu Pills recorded in Treatise on the Spleen and Stomach, which is composed of Aurantii Fructus Immaturus and Atractylodis Macrocephalae Rhizoma. It is widely used in clinical practice and has good curative effect on digestive system diseases such as functional dyspepsia, gastroesophageal reflux disease and functional constipation (Wang et al., 2018). Modern pharmacology believes that Zhizhu Pills is mainly involved in the negative regulation of apoptosis, epithelial cell proliferation, amino acid response, estradiol response, nitric oxide synthesis and other biological processes to exert its therapeutic effect on FD (Wang et al., 2018). Through experimental studies, Shan et al. found that Zhizhu Pills can improve the function of the “brain-gut” axis by regulating the levels of CORT, NO, CCK and CGRP, thus playing a therapeutic role in FD (Shan, Zhao, Zang, Zheng, & Jia, 2022). Another study found that Zhizhu Pills can up-regulate the expression of growth hormone secretagogue receptor (GHSR) protein, increase the levels of ghrelin and 5-HT, and reduce the level of CGRP, thereby improving gastrointestinal motility and gastric emptying speed, and has a good relieving effect on the clinical symptoms of FD (Li et al., 2016).
3.2.3. Clinical application
Hu et al. conducted a systematic evaluation and eta-analysis on the treatment of FD with Simo Decoction oral liquid by using a randomized controlled trial (RCT) (Hu et al., 2017). The results showed that Simo Decoction oral liquid can effectively improve the clinical symptoms of FD patients, and improve the gastric emptying function of FD patients. Researchers used a randomized, double-blind, placebo-controlled trial to observe the treatment of FD patients with spleen deficiency and qi stagnation by adding and subtracting Liujunzi Decoction, and finally found that the traditional Chinese medicines group could significantly alleviate the symptoms of FD patients and improve the gastric emptying of patients (Zhang et al., 2013).
3.3. Treatment for acrid dispersing and bitter descending
3.3.1. Single herb and effective ingredients
Zingiberis Rhizoma (Ganjiang in Chinese) has the effect of warming the stomach and dispelling cold. Coptidis Rhizoma (Huanglian in Chinese) can clear away heat and dry dampness. The two drugs work together to regulate the rise and fall of spleen and stomach qi. Some scholars explored the effect of different compatibility ratios of Coptidis Rhizoma and Zingiberis Rhizoma on gastric emptying and intestinal propulsion percentage of FD rats through experimental studies, and further detected the content of gas in the serum of FD rats after administration. The results showed that Coptidis Rhizoma had a significant inhibitory effect on gastric emptying, but had a significant role in promoting intestinal propulsion; Different polar parts of Zingiberis Rhizoma significantly promoted gastric emptying and intestinal propulsion. The drugs with different proportion of Coptidis Rhizoma and Zingiberis Rhizoma can significantly promote the intestinal propulsion (Shi et al., 2011).
3.3.2. Representative prescriptions
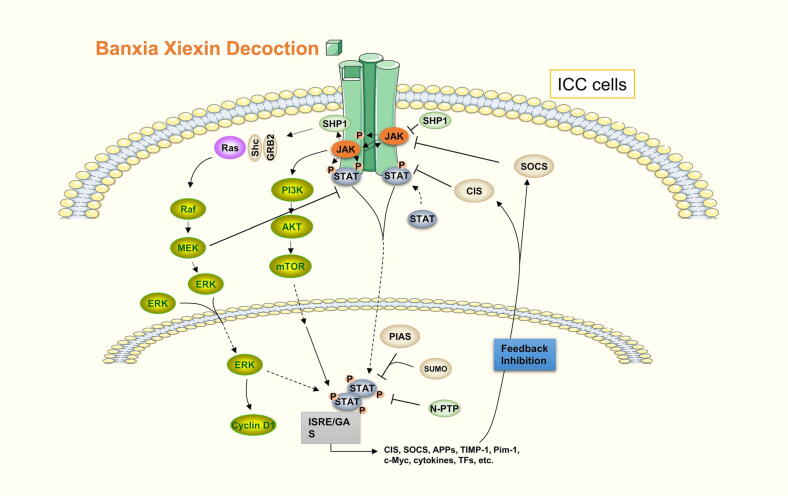
Banxia Xiexin Decoction is a famous prescription in treatise on FD. This recipe consists of Pinelliae Rhizoma (Banxia in Chinese), Coptidis Rhizoma, Scutellariae Radix (Huangqin in Chinese), Zingiberis Rhizoma, Glycyrrhizae Radix et Rhizoma, Ginseng Radix et Rhizoma, and Jujubae Fructus (Dazao in Chinese). It has the effects of reconciling the liver and spleen, calming cold and heat, dispelling sputum and dispersing knots, and has good clinical curative effect on various digestive system diseases such as functional dyspepsia, gastric ulcer and duodenal ulcer (Lee, Ahn, & Yang, 2022). Some studies have shown that Banxia Xiexin Decoction regulates Cajal interstitial cells of FD patients, increases the expression of c-kit and stem cell factors, and has achieved good results in the prevention and treatment of FD (Joung, Choi, & Son, 2021). According to the research of network pharmacology, the mechanism of Banxia Xiexin Decoction in the treatment of FD mainly involves various pathways such as regulation of inflammatory response, regulation of gastric motility, gastrointestinal hypersensitivity and estrogen content (Zhou, Wang, Cao, & Wang, 2021). Wang (2021) explored the cellular and molecular mechanism of Banxia Xiexin Decoction in the treatment of FD from the perspective of miRNA, and found that Banxia Xiexin Decoction could inhibit the apoptosis of interstitial cell of Cajal (ICC) by up-regulating the expression of miR-451-5p, and promote the apoptosis of ICC proliferation. And it can activate the JAK1/STAT3/ERK signaling pathway, increase the expression of Cyclin D1 protein, drive the process of ICC from G1 phase to S phase, and then play a therapeutic role in FD (Fig. 3). In addition, Banxia Xiexin Decoction can also improve the symptoms of FD by regulating brain-gut peptide (Ren, Ren, Lei, & Chen, 2019), and promoting gastric emptying and increasing the level of ghrelin in gastric antrum tissuerelin (Wu, Zhang, & Shen, 2014), and then it can play a role in alleviating nausea, vomiting, abdominal distension, constipation and other symptoms in FD patients.
Fig. 3.
Mechanism of Banxia Xiexin Decoction in treating FD through JAK1/STAT3/ERK signal pathway.
3.3.3. Clinical application
Yuan et al. used the method of Meta-analysis to evaluate the efficiency and safety of Banxia Xiexin Decoction in treating FD (Yuan, Li, & Jia, 2020). Compared with western medicines, the results showed that Banxia Xiexin Decoction has higher clinical efficacy in treating FD patients and lower incidence of adverse reactions, which can significantly relieve the symptoms of FD. Zhao et al. evaluated the effectiveness and safety of Banxia Xiexin Decoction in treating FD with mixed cold and heat through a randomized controlled experiment (Zhao et al., 2013). The results showed that Banxia Xiexin Decoction could effectively improve the total dyspepsia symptom score and the single dyspepsia symptom score of FD patients, without adverse reactions. Chang et al. used Weikangning Capsule to treat patients with FD (Chang et al., 2017). The results showed that Weikangning Capsule can significantly improve the clinical symptoms of patients with FD compared with western medicines, and can improve the mood of patients to a certain extent, alleviate anxiety and depression psychological disorders, and improve the quality of life. They also discussed that the mechanism of its treatment of FD is related to the protective effect of Nrf2.
3.4. Treatment for eliminating heat and removing dampness
3.4.1. Single herb and effective ingredients
Hyperici Perforati Herba (Guanyejinsitao in Chinese) is a kind of TCMs that can clear away heat and dampness, soothe the liver and relieve depression. Hyperici Perforati Herba, is also widely used in the treatment of nervous system diseases and digestive system diseases (Erdal & Nur, 2021). Some studies have shown that Hyperici Perforati Herba can increase the expression of PGP9.5 mRNA and abnormally downregulated in the gastric antrum and duodenum of FD rats. At the same time, it can reduce the expression of GFAP mRNA, so that the damaged ENS of FD rats can be restored, thereby improving the gastrointestinal motility of FD rats (Zhang, 2021).
Swertiae Herba (Dangyao in Chinese) is a traditional Chinese medicine with high therapeutic and medicinal value. It has the effects of clearing away heat and dampness, and strengthening the stomach. It is widely used in many diseases of the digestive system. Some scholars observed the effects of the extracts of the local medicine of different concentrations on the gastrointestinal hormone levels of FD rats, and finally found that the extracts of the local medicine can significantly increase the plasma motilin and gastrin levels of FD rats, reduce the serum somatostatin, thereby improving the symptoms of FD and playing an important role in the treatment of FD (Zhang, Wang, Wei, Wang, & Han, 2016).
3.4.2. Representative prescriptions
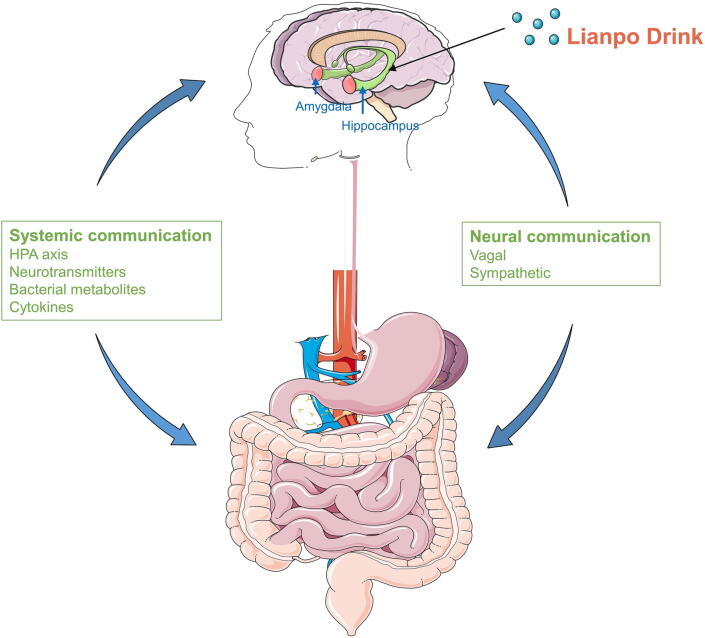
Lianpo Drink, composed of Magnoliae Officinalis Cortex (Houpo in Chinese), Coptidis Rhizoma, Acori Tatarinowii Rhizoma (Shichangpu in Chinese), Pinelliae Rhizoma, Sojae Semen Praeparatum (Dandouchi in Chinese), Phragmitis Rhizoma (Lugen in Chinese) and Gardeniae Fructus (Zhizi in Chinese), which has the effect of clearing away heat and dampness, regulating qi and harmonizing, and is a commonly used prescription for treating FD. Some studies have shown that Lianpo Drink can improve the responsiveness of antral smooth muscle of FD rats to acetylcholine and 5-HT, strengthen gastrointestinal contraction, and play a role in promoting gastric motility, thus relieving the symptoms of FD rats (Xu et al., 2022). At the same time, some studies have also confirmed that Lianpo Drink can participate in regulating the “brain gut” interaction disorder by up regulating the levels of monoamine transmitters 5-HT and noradrenaline in the hippocampus of FD rats, and play a therapeutic effect on functional dyspepsia by using the “brain-gut” axis approach (Xu, 2020) (Fig. 4). Sanren Decoction is also a common prescription for treating FD. Dong confirmed that Sanren Decoction can improve the level of motilin and gastrin in patients with FD and improve the clinical symptoms of abdominal distension, dyspepsia and other symptoms of FD patients by clinical and experimental studies, with significant efficacy and no adverse reactions (Dong, 2018).
Fig. 4.
“Brain-gut” axis mechanism of Lianpo Drink in treating FD.
3.4.3. Clinical application
Zhang (2020) used Chaihu Dayuan Drink to treat FD patients. Through clinical observation, it can effectively improve the clinical symptoms of FD patients and regulate the secretion of gastrointestinal hormones. Compared with Mosapride citrate tablets, it has more advantages in improving the clinical symptoms, and is safer without adverse reactions. Yin (2021) observed the patients with FD by clearing away heat and removing dampness. Compared with western medicine, the results showed that TCMs can effectively improve the Nepean dyspepsia symptom index (NDSI) score and Nepean Dyspepsia Life Quality Index (NDLQI) score, improve clinical symptoms and enhance the quality of life of patients.
3.5. Treatment for warming stomach and invigorating spleen
3.5.1. Single herb and effective ingredients
Amomi Fructus has the effect of warming the spleen, regulating qi and calming the fetus. It is used for vomiting, diarrhea, indigestion and other diseases. Amomi Fructus mainly plays a role in treating FD by regulating gastrointestinal function and strengthening gastric motility. Zhu et al. used 25% Amomi Fructus extract to observe the condition of FD rats for four weeks (Zhu, Zhang, Zhang, & Wang, 2006). The results showed that Amomi Fructus extract could significantly increase the levels of substance P (SP) and motilin (MTL) in the gastric antrum tissue of FD rats, thereby playing a therapeutic role in FD. In addition, Zhang (2014) observed 40 patients with FD for four weeks by using Amomi Fructus volatile oil (3 times/d). The results showed that Amomi Fructus could significantly relieve the clinical symptoms of FD patients, such as belching, nausea, vomiting, abdominal distension, and promote the secretion and release of SP and MTL in the body. It was an effective method to treat FD.
3.5.2. Representative prescriptions
Huangqi Jianzhong Decoction is composed of seven TCMs: Astragali Radix, Cinnamomi ramulus (Guizhi in Chinese), Paeoniae Radix Alba (Baishao in Chinese), Glycyrrhizae Radix et Rhizoma Praeparata Cum Melle (Zhigancao in Chinese), Zingiberis Rhizoma Recens (Shengjiang in Chinese), Jujubae Fructus and maltose. This prescription is a representative prescription for the treatment of FD. Some studies have shown that Huangqi Jianzhong Decoction can play a therapeutic role by promoting gastric emptying and increasing the gastrointestinal hormone substance SP in gastric antrum (Qiu & Xu, 2008). In addition, some scholars used Liangfu Pills to explore the mechanism of action on FD rats of deficiency-cold of spleen and stomach. Studies showed that Liangfu Pills mainly involved in biological processes such as drug reaction, negative transcriptional regulation, positive regulation of apoptosis process, and cell surface receptor signal pathway. At the same time, experimental research showed that Liangfu Pills could significantly increase the expression of 5-HT and down regulate the expression of TRPV1 to alleviate the symptoms of FD rats (He et al., 2022).
3.5.3. Clinical application
Researchers evaluated the effectiveness and safety of Weiyan No.1 Formula in treating FD with deficient cold of spleen and stomach, and found that TCMs can effectively improve the clinical symptoms, without adverse reactions, and with high safety (Zhang et al., 2013). Li et al. evaluated the clinical therapeutic effect of FD with Wenwei Jianzhong Decoction, and the results showed that it can effectively improve the clinical symptoms of FD patients such as epigastric pain, epigastric distension, and regulate the secretion of MTL and GAS (Li, Sun, & Li, 2021).
3.6. Other thoughts on FD treatment
Under the influence of the above pathogenesis, FD will also produce many pathological products in the pathogenesis. If the liver depression and qi stagnation persist for a long time, and the qi mechanism is not good for relieving, it is easy to turn heat into poison; Spleen deficiency and qi stagnation result in poor spleen transport and turbidity; The spleen and stomach are deficient in cold, the spleen’s yang-qi are insufficient, and the yang-qi is unable to promote the blood circulation, which results in blood stasis. Therefore, heat toxin, dampness and blood stasis are important pathological products in the pathogenesis of FD. According to its pathological products, many scholars have applied the methods of clearing away heat and toxin, removing dampness and turbidity, promoting blood circulation and removing blood stasis to the treatment of FD. For example, Professor Baogui Chen emphasized that gastrointestinal diseases are easy to produce dampness and blood stasis after a long time, so on the basis of syndrome differentiation and treatment, corresponding drugs should be added according to its pathological products to improve the clinical symptoms (Tang et al., 2018). Professor Delu Tian also stressed the need to eliminate heat toxin, blood stasis and other pathological products, so as to trace the origin and treat according to syndrome differentiation (Li & Tian, 2013).
4. Discussion
The above content starts with the common syndrome types of FD and explores the research progress in the single ingredient and effective ingredients of traditional Chinese medicine, as well as the mechanism of action of TCM in treating FD.
In terms of mechanism of action, TCM can prevent and treat FD by regulating brain gut peptides, regulating gastrointestinal hormone content, improving gastric motility, regulating immune function, regulating intestinal microbiota, and regulating inflammatory response. In terms of clinical efficacy, TCM treatment can alleviate patients' clinical symptoms and alleviate the side effects of Western medicine treatment.
According to the above discussion, the single herb, effective ingredients, and prescriptions of TCMs have played an important therapeutic role in the treatment of FD (Table 2), with significant effects in clinical applications (Table 3).
Table 2.
Representative prescriptions in five syndrome types.
| Five syndrome types | Representative prescriptions |
|---|---|
| Liver-stomach disharmony | Chaihu Shugan Powder (Citri Reticulatae Pericarpium, Bupleuri Radix, Chuanxiong Rhizoma, Cyperi Rhizoma, Paeoniae Radix Alba, Aurantii Fructus, Glycyrrhizae Radix et Rhizoma) |
| Hewei Liqi Formula (Bupleuri Radix, Codonopsis Radix, Aurantii Fructus Immaturus, Aucklandiae Radix, Magnoliae Officinalis Cortex, Citri Reticulatae Pericarpium, Amomi Fructus Rotundus, Glycyrrhizae Radix et Rhizoma) | |
| Spleen deficiency with qi stagnation | Simo Decoction (Ginseng Radix et Rhizoma, Arecae Semen, Aquilariae Lignum Resinatum, Linderae Radix) |
| Xiangsha Liujunzi Decoction (Aucklandiae Radix, Amomi Fructus, Ginseng Radix et Rhizoma, Atractylodis Macrocephalae Rhizoma, Poria, Glycyrrhizae Radix) | |
| Zhizhu Pills (Aurantii Fructus Immaturus, Atractylodis Macrocephalae Rhizoma) | |
| Syndrome of intermingled heat and cold | Banxia Xiexin Decoction (Pinelliae Rhizoma, Coptidis Rhizoma Scutellariae Radix, Zingiberis Rhizoma, Glycyrrhizae Radix et Rhizoma, Ginseng Radix et Rhizoma, Jujubae Fructus) |
| Dampness-heat of spleen and stomach | Lianpo Drink (Magnoliae Officinalis Cortex, Coptidis Rhizoma, Acori Tatarinowii Rhizoma, Pinelliae Rhizoma, Sojae Semen Praeparatum, Phragmitis Rhizoma, Gardeniae Fructus) |
| Sanren Decoction (Armeniacae Semen Amarum, Amomi Fructus Rotundus, Coicis Semen, Pinelliae Rhizoma, Magnoliae Officinalis Cortex, Tetrapanacis Medulla, Talcum, Lophatheri Herba) | |
| Deficiency-cold of spleen and stomach | Huangqi Jianzhong Decoction (Astragali Radix, Cinnamomi ramulus, Paeoniae Radix Alba, Glycyrrhizae Radix et Rhizoma Praeparata Cum Melle, Zingiberis Rhizoma Recens, Jujubae Fructus, Maltose) |
Table 3.
Clinical application of Traditional Chinese Medicines in the treatment of FD.
| Prescriptions | Herbs | Effect evaluation methods | Experimental design | Cases | Effectiveness | Security |
|---|---|---|---|---|---|---|
| Chaizhi Pinggan Decoction | Aurantii Fructus, Bupleuri Radix, Paeoniae Radix Rubra, etc | Standard for TCM diseases and syndromes therapeutic results | Before-after study | 76 | 97.37 % | High |
| Chaihu Shugan Powder | Citri Reticulatae Pericarpium, Bupleuri Radix, Chuanxiong Rhizoma, Cyperi Rhizoma, etc | Meta-analysis | Random controlled trials | 1939 | RR = 1.20, 95 %, CI 1.14 to 1.27 | None |
| Simo Decoction | Ginseng Radix et Rhizoma, Arecae Semen, Aquilariae Lignum Resinatum, etc | Systematic review, Meta-analysis | Random controlled trials | 2713 | RR = 1.14; 95 % CI 1.09, 1.20; P < 0.00001 | High |
| Xiangsha Liujunzi Decoction | Aucklandiae Radix, Amomi Fructus, Ginseng Radix et Rhizoma, Atractylodis Macrocephalae Rhizoma, etc | Total dyspepsia symptoms scale, single dyspepsia symptom scale | Randomized, double-blind, placebo-controlled trial | 54 | Effective | High |
| Banxia Xiexin Decoction | Pinelliae Rhizoma, Coptidis Rhizoma, Scutellariae Radix, Zingiberis Rhizoma, etc | Total dyspepsia symptoms scale, single dyspepsia symptom scale | Random controlled trials | 101 | Effective | High |
| Weikangning Capsule | Scutellariae Radix, Rhizoma Zingiberis, Ginseng Radix et Rhizoma, etc | Establishment of the lentivirus-mediated nuclear factor erythroid 2 like 2 (Nrf2) gene-knockdown stable strain of GES-1 cells | Random controlled trials | 10 | Effective | None |
| Chaihu Dayuan Drink | Citri Reticulatae Pericarpium, Scutellariae Radix, Coptidis Rhizoma, etc | The standard for TCM diseases and syndromes therapeutic results | Random controlled trials | 72 | 83.33 % | None |
| Huanglian Wendan Decoction | Coptidis Rhizoma, Bambusae Caulisin Taenias, Glycyrrhizae Radix et Rhizoma, etc | Scoring of Nipin dyspepsia symptom Index (NDSI), Nipin dyspepsia quality of life index (NDLQI), The standard for TCM diseases and syndromes therapeutic results | Random controlled trials | 72 | Effective | High |
| Weiyan No.1 Formula | Zingiberis Rhizoma, Cyperi Rhizoma, Atractylodis Macrocephalae Rhizoma, etc | Total dyspepsia symptoms scale, single dyspepsia symptom scale, the standard for TCM diseases and syndromes therapeutic results | Random controlled trials | 162 | Effective | High |
| Wenwei Jianzhong Decoction | Astragali Radix, Poria, Atractylodis Macrocephalae Rhizoma, etc | Gastrointestinal symptom rating scale, the standard for TCM diseases and syndromes therapeutic results | Random controlled trials | 38 | Effective | High |
5. Conclusion and outlook
FD is a common and frequently occurring disease in the digestive system, and its incidence has a high trend in recent years. TCM is a treasure of Chinese civilization. Its simple and inexpensive characteristics have always played an indelible role in the history of the struggle between human beings and diseases. Its overall concept and the characteristics of syndrome differentiation make TCM play a role in the treatment of diseases in the form of multi-component, multi-target, and multi-channel. TCM has accumulated a lot of rich experience in the treatment of FD since ancient times. Compared with the simple use of western medicine, TCM have many advantages in the prevention and treatment of FD, such as high safety, less adverse reactions, and low recurrence rate.
Based on the several guidelines or consensus focused on TCMs in treating FD in recent years, this paper reviewed the common etiology and pathogenesis of FD, demonstrated the mechanism of action of TCMs in the treatment of FD, and highlighted the strong advantages and broad application prospects of TCMs in the treatment of FD. It can be seen that the holistic concept of TCM and the holistic thinking of syndrome differentiation and treatment have unique advantages in the treatment of FD, and TCM has significant therapeutic effects in the treatment of FD. However, there are still many problems in the research on the prevention and treatment of FD with TCM. First of all, due to the diversity and complexity of the components of TCM s, the interaction between the effective components is still unclear, so it is necessary to combine with other disciplines and constantly update the experimental technology to clarify its mechanism; Moreover, many studies remain in the research stage of cell experiment or animal experiment, and the results of their experiments have not been verified in clinical practice. In the future, the research works need to be combined with clinical practice to promote the use of TCMs for FD in clinical practice. With the integration of multiple disciplines and the continuous updating of experimental technology, the mechanism of TCMs in treatment of FD will be more clear, and better progress will be made in future research.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Zixiang Kou, Email: kouzixiang181818@126.com.
Baogui Chen, Email: baogui16388@vip.163.com.
References
- Bai L. Experimental study on the effect of Hewei Liqi prescription in regulating mitochondrial autophagy on functional dyspepsia. Liaoning University of Traditional Chiinese Medicine. 2021;3:14–16. [Google Scholar]
- Chang Y., Wei W., Tong L., Liu Y., Zhou A., Chen J.…Su X. Weikangning therapy in functional dyspepsia and the protective role of Nrf2. Experimental and Therapeutic Medicine. 2017;14(4):2885–2894. doi: 10.3892/etm.2017.4892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christine F. Upper gastrointestinal sensitivity to meal-related signals in adult humans - relevance to appetite regulation and gut symptoms in health, obesity and functional dyspepsia. Physiology & Behavior. 2016;162:69–82. doi: 10.1016/j.physbeh.2016.03.021. [DOI] [PubMed] [Google Scholar]
- Chen S.F., Li Y.Q., He F.Y., Pan L.L. Effects of Aucklandia odora on gastric acid secretion, gastric emptying and gastrin, somatostatin and motilin levels. Chinese Journal of Integrated Traditional and Western Medicine. 1994;7:406–408. [Google Scholar]
- Colak H., Gunes F.E., Ozen A.Y., Karakoyun B. Investigation of eating habits in patients with functional dyspepsia. Turkish Journal of Gastroenterology. 2022;33(8):673–681. doi: 10.5152/tjg.2022.21502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng L., Zhou X., Lan Z., Tang K., Zhu X., Mo X.…Wu M. Simotang alleviates the gastrointestinal side effects of chemotherapy by altering gut microbiota. Journal of Microbiology and Biotechnology. 2022;32(4):405–418. doi: 10.4014/jmb.2110.10018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J., Ling J.H., Shangguan X.C., Che Y., Wang Y.J., Zhang Y.Q., Xie T.Y. Research progress of Chinese herbal compound Citrusaurantium for functional dyspepsia treatment. Genomics and Applied Biology. 2018;37(4):1656–1660. [Google Scholar]
- Dong J.T. Clinical curative effect of Sanren decoction in the treatment of damp-heat type functional dyspepsia and its mechanism. Yunnan Journal of Traditional Chinese Medicine and Materia Medica. 2018;39(4):55–57. [Google Scholar]
- Erdal E., Nur G.S. A unique phenolic extraction method from olive oil macerate of Hypericum perforatum using DMSO: Assessment of in vitro anticancer activity, LCMS/MS profile, total phenolic content and antioxidant capacity. South African Journal of Botany. 2021;139(4):6–11. [Google Scholar]
- Ghoshal U.C., Singh R., Chang F.Y., Hou X., Wong B.C., Kachintorn U. Epidemiology of uninvestigated and functional dyspepsia in Asia: Facts and fiction. Journal of Neurogastroenterology and Motility. 2011;17(3):235–244. doi: 10.5056/jnm.2011.17.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J.Y., Gui B., Chen Y.F., Yin Y.Q., Tao S.H., Shen Z.B.…Wei L. Mechanism of Liangfu Pills in treatment of functional dyspepsia: Based on network pharmacology and experimental verification. China Journal of Chinese Materia Medica. 2022;47(14):3853–3862. doi: 10.19540/j.cnki.cjcmm.20211230.705. [DOI] [PubMed] [Google Scholar]
- Hu Y., Bai Y., Hua Z., Yang J., Yang H., Chen W.…Zhao Z. Effect of Chinese patent medicine Si-Mo-Tang oral liquid for functional dyspepsia: A systematic review and meta-analysis of randomized controlled trials. PLoS One1. 2017;12(2):1–15. doi: 10.1371/journal.pone.0171878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang A.F., Chi Y.G., Zeng Y.E., Lu L.P. Influence of Fructus Aurantii Immaturus flavonoids on gastrointestinal motility in rats with functional dyspepsia. Traditional Chinese Drug Research and Clinical Pharmacology. 2012;23(6):612–615. [Google Scholar]
- Jin T.Y., Liu W. Professor Liu Wen's experience in treating functional dyspepsia by differentiating qi from phlegm. Chinese Journal of Integrated Traditional and Western Medicine on Digestion. 2019;27(12):945–947. [Google Scholar]
- Joung J.Y., Choi S.H., Son C.G. Interstitial cells of cajal: Potential targets for functional dyspepsia treatment using medicinal natural products. Evidence-based Complementary and Alternative Medicine. 2021;9:4–6. doi: 10.1155/2021/9952691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junghyo C., Yochan A., Dongsoo L., Changgue S. Distributions of sasang constitutions and six syndromes in patients with functional dyspepsia and healthy subjects. Journal of Traditional Chinese Medicine. 2013;33(5):626–629. doi: 10.1016/s0254-6272(14)60032-7. [DOI] [PubMed] [Google Scholar]
- Lee B., Ahn E.K., Yang C. Herbal medicine prescriptions for functional dyspepsia: A nationwide population-based study in Korea. Evidence-based Complementary and Alternative Medicine. 2022;10:3–8. doi: 10.1155/2022/3306420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X.L., Zhang S.S., Yang C., Wang Z.F., Wu Z.Y., Yu Q., Chang J. Effect of Zhizhu Pill on gastric smooth muscle contractile response and protein expression of growth hormone secretagogue receptor in functional dyspepsia rats. Chinese Journal of Integrated Traditional and Western Medicine. 2016;36(2):210–215. [PubMed] [Google Scholar]
- Liu J., Li F., Tang X.D., Ma J., Ma X., Ge D.Y.…Wang Y. Xiangsha Liujunzi decoction alleviates the symptoms of functional dyspepsia by regulating brain-gut axis and production of neuropeptides. BMC Complementary and Alternative Medicine. 2015;15:387–389. doi: 10.1186/s12906-015-0913-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu P., Fan Y., Wei Y., Zeng F., Li R., Fei N., Qin W. Altered structural and functional connectivity of the insula in functional dyspepsia. Neurogastroenterology and Motility. 2018;30(9):133–145. doi: 10.1111/nmo.13345. [DOI] [PubMed] [Google Scholar]
- Li H., Sun H.T., Li P.R. Clinical observation on Wenwei Jianzhong decoction in the treatment of functional dyspepsia of deficiency cold of spleen and stomach type. Chinese Medicine Modern Distance Education of China. 2021;19(16):99–101. [Google Scholar]
- Li J.X., Chen J., Li Y. Consensus on diagnosis and treatment of functional dyspepsia with integrated traditional and western medicine. Chinese Journal of Integrated Traditional and Western Medicine on Digestion. 2017;25(12):889–894. [Google Scholar]
- Li L., Jia Q.L., Wang Y.J., Wang X.X., Ling J.H. Effect of Chaihu Shugansan on mitochondrial function and mitophagy in gastric tissue of rats with functional dyspepsia. China Journal of Experimental Traditional Medical Formulae. 2021;27(23):26–34. [Google Scholar]
- Li S.G. Beijing University of Traditional Chinese Medicine; 2017. Comparative study on TCM constitution types and their correlations of Chinese and Korean patients with functional dyspepsia. Thesis of Master Degree. [Google Scholar]
- Li W.X., Li F.Y., Li D., Peng X.Z., Li H. Comparative study on gastrointestinal motility of mice treated with aqueous extracts of chicken trollium. Hunan Journal of Traditional Chinese Medicine. 2008;24:100–101. [Google Scholar]
- Li Y.J., Wei W., Yang J.Q. Experience in the treatment of functional dyspepsia with Xinkai Kujiang method. World Journal of Integrated Traditional and Western Medicine. 2015;10(8):1152–1154. [Google Scholar]
- Li Z.H., Tian D.L. The experience of treating functional dyspepsia with Professor Tian Delu's theory of “clearing and descending”. Journal of Beijing University of Traditional Chinese Medicine. 2013;20(2):45–46. [Google Scholar]
- Lin G.M., Zhang X., Yin L.B., Hou Y., Yang J.X., Jia T.Z. Effect of raw and stir-frying with bran Fructus Aurantii Immaturus on gut hormone of spleen deficiency rats induced by reserpine guiding. Journal of Traditional Chinese Medicine and Pharmacy. 2012;18(12):11–12. [Google Scholar]
- Liu, W. J. (2021). Research on the distribution characteristics of TCM syndrome types of functional dyspepsia and Professor Liu Huayi's experience in syndrome differentiation and treatment. Tianjin University of Traditional Chinese Medicine. Thesis of Master Degree.
- Luv L., Wang F.Y., Ma X.X., Li Z.H., Huang S.P., Shi Z.H., Ji H.J., Bian L.Q., Zhang B.H., Chen T., Yin X.L., Tang X.D. Efficacy and safety of Xiangsha Liujunzi granules for functional dyspepsia: A multi-center randomized double-blind placebo-controlled clinical study. World Journal of Gastroenterology. 2017;23(30):5589–5601. doi: 10.3748/wjg.v23.i30.5589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo G.B., Ling J.H. Influences of Chaihu Shugan powder on expressions of GRP78 and c-JNK in gastric antrum tissue of rats with functional dyspepsia. Shanxi Journal of Traditional Chinese Medicine. 2019;35(5):56–58. [Google Scholar]
- Luo M.X., Mao X.Y., Su X.L., Yang Y., Pan Y.Y., Wei W. Professor Wei wei's experience in treating functional dyspepsia by referring to deficiency, depression, blood stasis and stagnation. Jilin Journal of Chinese Medicine. 2021;41(11):1442–1445. [Google Scholar]
- Madisch A., Andresen V., Enck P., Labenz J., Frieling T., Schemann M. The diagnosis and treatment of functional dyspepsia. Deutsches Arzteblatt International. 2018;115(13):222–232. doi: 10.3238/arztebl.2018.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y.N. Jiangxi University of Traditional Chinese Medicine; 2021. Study on the changes of components of Aucklandiae Radix before and after processing and its effects on gastrointestinal in mice. Thesis of Master Degree. [Google Scholar]
- Qiu J.J., Li Y.C., Qiu Y., Guo L., Liu Y.J., Wan J.J.…Guo H.S. Study on the relationship between Simo decoction and the expression of gastric RhoA and ROCK in rats with functional dyspepsia. Jilin Journal of Chinese Medicine. 2022;42(1):58–61. [Google Scholar]
- Qiu X.Y., Xu S. Experimental study on the effect of Huangqi Jianzhong decoction on gastrointestinal motility in rats with functional dyspepsia. Chinese Journal of Traditional Medical Science and Technology. 2008;15(3):176–177. [Google Scholar]
- Ren X.J., Ren H.H., Lei M.H., Chen Y. Study on the mechanism of Banxia Xiexin decoction in treating functional dyspepsia based on brain-gut axis theory. Journal of Jiangxi College of Traditional Chinese Medicine. 2019;31(3):119–121. [Google Scholar]
- Shan G.S., Zhao Q.M., Zang B.R., Zheng W., Jia T.Z. Study of Zhizhu pill preparation by raw and processed Baizhu (Atractylodes macrocephala) on functional dyspepsia rats of brain-gut axis. Chinese Archives of Traditional Chinese Medicine. 2022;40(3):44–47. [Google Scholar]
- Shangguan X.C. Guangxi Medical University; 2017. Effect of Chaihu Shugansan on apoptosis of gastric smooth muscle cell and expression of NF-ΚB protein in rats with funtional dyspepsia. Thesis of Master Degree. [Google Scholar]
- Shen M., Huang X.Q., Yuan M.J. Improvement of gastrointestinal function in rats with functional dyspepsia. Fujian Journal of Traditional Chinese Medicine. 2019;50(4):35–37. [Google Scholar]
- Shi X.S. Beijing University of Traditional Chinese Medicine; 2019. Study on the role of EC in visceral hypersensitivity of FD based on EPAC1-PIEZO2 axis and the intervention of Xiangsha Liujunzi decoction. Thesis of Master Degree. [Google Scholar]
- Shi Y., Chang J.S. Li Qiugui's clinical experience in applying Banxia Xiexin decoction. Global Traditional Chinese Medicine. 2016;9(7):822–824. [Google Scholar]
- Shi Q.R., Yu S.Y., Sun X.R., Yan H., Sun S.G., Xie Y.P., Zhang J. Effects of the drug pair of Coptidis Rhizoma and Zingiberis Rhizomaon gastric emptying and serum gastrinin rats with functional dyspepsia. Chinese Pharmaceutical Journal. 2011;46(13):988–992. [Google Scholar]
- Song J., Yang L., Su S., Piao M.Y., Li B.L., Yu Y.…Hou X.H. Agreement of gastroenterologists in traditional Chinese medical differential diagnosis of functional dyspepsia compared with traditional Chinese medical practitioners: A prospective, multicenter study. Journal of Digestive Diseases. 2020;21(7):399–405. doi: 10.1111/1751-2980.12873. [DOI] [PubMed] [Google Scholar]
- Suzuki H. Recent advances in the definition and management of functional dyspepsia. The Keio Journal of Medicine. 2020;70(1):7–18. doi: 10.2302/kjm.2020-0006-OA. [DOI] [PubMed] [Google Scholar]
- Tang L., Lin X.L., Zhang M.Y., Wang L.P., Zhang M.Y., Chen B.G. Analysis on prescription rules of Chen Baogui's prescriptions for treating epigastric fullness based on data mining. China Journal of Chinese Materia Medica. 2018;43(20):4163–4168. doi: 10.19540/j.cnki.cjcmm.20180611.011. [DOI] [PubMed] [Google Scholar]
- Tian Z.Y., Liu S.X., Chen C.Q. Research progress on Chinese materia medica in treatment of pediatric functional dyspepsia. Chinese Traditional and Herbal Drugs. 2017;48(4):803–807. [Google Scholar]
- Vanner S., Greenwood-Van M.B., Mawe G., Shea-Donohue T., Verdu E.F., Wood J., Grundy D. Fundamentals of neurogastroenterology: Basic science. Gastroenterology. 2016;18(16):2–18. doi: 10.1053/j.gastro.2016.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Herndon C.C., Lu C. Non-pharmacological approach in the management of functional dyspepsia. Journal of Neurogastroenterology and Motility. 2020;26(1):6–15. doi: 10.5056/jnm19005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M.W. Beijing University of Traditional Chinese Medicine; 2021. Molecular mechanism of Banxia Xiexin decoction in treating functional dyspepsia. Thesis of Master Degree. [Google Scholar]
- Wang W.F., Liu F.L., Xia X.T., Wang W.S., Tu Q.R., Wang T., Teng G.F. Analysis on the addition and subtraction of Zhizhu pill and its clinical application. Guiding Journal of Traditional Chinese Medicine and Pharmacology. 2018;24(15):100–102. [Google Scholar]
- Wang Y.B., Wang Q., Mao F.L., Zhang Y.F., Huang F. Pharmacological study on Radix Aucklandiae. Journal of China Pharmaceutical University. 2001;32(2):66–68. [Google Scholar]
- Wang Y.J., Jia Q.L., Guo L.K., Gu C.L., Li L., Wang X.X., Ling J.H. Network pharmacological analysis of the mechanism of action of Fructus Aurantii Immaturus in the treatment of functional dyspepsia. Traditional Chinese Drug Research and Clinical Pharmacology. 2022;33(5):666–673. [Google Scholar]
- Wang Z.H., Zhao A.L., Zhang Y.Y., Zhao S.X., Zhuo A.X., Zhou C. Mechanism of Chaihu Shugan powder in treatment of functional dyspepsia based on network pharmacology and molecular docking. Drugs & Clinic. 2021;36(9):1794–1806. [Google Scholar]
- Wei W., Wei J.J., Yuan H.X. Observation of the effects of Chaizhi Pinggan decoction on the levels of gastrointestinal hormones and NPSR1 in functional dyspepsia patients with disharmony between liver and stomach. Chinese Journal of Surgery of Integrated Traditional and Western Medicine. 2021;27(6):869–871. [Google Scholar]
- Wu L., Lai Y., Wang Y., Tan L., Wen L., Yang H. Maillard reaction products of stir Fried Hordei Fructus Germinatus are important for its efficacy in treating functional dyspepsia. Journal of Medicinal Food. 2020;23(6):420–431. doi: 10.1089/jmf.2019.4430. [DOI] [PubMed] [Google Scholar]
- Wu J., Zhang X.X., Shen H. Effect of Banxia Xiexin decoction on gastric emptying and ghrelin in gastric antrum tissue with functional dyspepsia. Journal of Sichuan of Traditional Chinese Medicine. 2014;32(1):70–72. [Google Scholar]
- Wu Z.Y., Zhang S.S., Lu X.F., Li P.C., Wang J.J., Zhang H.Y.…Li X.L. Effect of Aurantii Fructus Immaturus of flavonoidon on the proximal gastric accommodation of functional dyspepsia rats. Chinese Journal of Integrated Traditional and Western Medicine on Digestion. 2016;24(3):188–193. [Google Scholar]
- Xiao H.L., Wu Y.J., Wang X., Li Y.F., Fang Z.Q. Medication rule for treatment of functional dyspepsia: An analysis of traditional Chinese medicine literature based on China national knowledge Internet. China Journal of Chinese Materia Medica. 2015;40(19):3866–3869. [PubMed] [Google Scholar]
- Xu J. Study on the mechanism of Lianpu Yin in treatment of functional dyspepsia by brain-gut co-regulated pathways. Hubei University of Traditional Chinese Medicine. 2020;4:57–59. [Google Scholar]
- Xu J., Zhang L., Hou X.H., Li T.W., Gao Q.H., Zhang S.N., Lyu W.L. Effects of Lianpo Drink on gastric motility of functional dyspepsia rats. China Journal of Traditional Chinese Medicine and Pharmacy. 2022;37(2):1018–1021. [Google Scholar]
- Xu K., Ling J.H., Zhou Z., Zhang L.M., Zhang Y.Q., Xie T.Y., Wang Y.J. Effect of Chaihushugansan decoction on expression of endoplasmic reticulum stress-related molecules IRE1 and TRAF2 in functional dyspepsia rats. Acta Universitatis Medicinalis Anhui. 2018;53(4):516–520. [Google Scholar]
- Xu W.F., Yao S.K., Li N.Q., Zhang Y.L., Ke M.Y., Wang X.Y. Study of TCM differentiating treatment on patients with functional dyspepsia. Chinese Journal of Integrated Traditional and Western Medicine on Digestion. 2013;21(5):225–228. [Google Scholar]
- Yan X., Gan C. Gan Chun's experience in the diagnosis and treatment of functional dyspepsia with syndrome of spleen deficiency and qi stagnation. Journal of Jiangxi College of Traditional Chinese Medicine. 2021;33(2):15–17. [Google Scholar]
- Yang N., Jiang X., Qiu X., Hu Z., Wang L., Song M. Modified chaihu shugan powder for functional dyspepsia: Meta-analysis for randomized controlled trial. Evidence-based Complementary and Alternative Medicine. 2013;10:5–9. doi: 10.1155/2013/791724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang N.N., Tan C.X., Lin L.L., Su X.T., Li Y.J., Qi L.Y.…Liu C.Z. Potential mechanisms of acupuncture for functional dyspepsia based on pathophysiology. Frontiers in Neuroscience. 2021;15:1–14. doi: 10.3389/fnins.2021.781215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Li H.Z. Clinical experience of Xiaoyao powder in the treatment of functional dyspepsia. Chinese Medicine Modern Distance Education of China. 2019;17(8):78–79. [Google Scholar]
- Yin Q. Jiangxi University of Traditional Chinese Medicine; Thesis of Master Degree: 2021. Clinical observation of modified Huanglian Wendan decoction in the treatment of functional dyspepsia postprandial disorder ayndrome (apleen-stomach damp-heat type) clinical observation of modified Huanglian Wendan decoction. [Google Scholar]
- Yuan T., Li P., Jia B. A meta-analysis of Xin kai bitter method in the treatment of functional dyspepsia. Annals of Palliative Medicine. 2020;9(3):993–1003. doi: 10.21037/apm-20-860. [DOI] [PubMed] [Google Scholar]
- Zeng L.J., Ling J.H., Deng J., Wang Y.J., Zhang Z., Lei Z.J. Effect of Chaihu Shugan powder on autophagy of cajal interstitial cells in gastric antrum muscles of rats with functional dyspepsia. Lishizhen Medicine and Materia Medica Research. 2017;28(5):1041–1044. [Google Scholar]
- Zou B.C., Dong L., Wei M.X., Wei L.F. Effects of areca nut on gastric motility and gastrointestinal hormones. Shaanxi Journal of Traditional Chinese Medicine. 2007;28(3):370–372. [Google Scholar]
- Zou B.C., Wei M.X., Yuan J.L. Effect of Areca nut on gastrointestinal of normal peptide and its function of improving the gastrointestinal motility. Study Journal of Traditional Chinese Medicine. 2004;22(6):1040–1041. [Google Scholar]
- Zhao L., Zhang S., Wang Z., Wang C., Huang S., Shen H.…Wu B. Efficacy of modified ban xia xie xin decoction on functional dyspepsia of cold and heat in complexity syndrome: A randomized controlled trial. Evidence-based Complementary and Alternative Medicine. 2013;56(4):1–8. doi: 10.1155/2013/812143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Wang X., Wang F., Tang X. Xiangsha Liujunzi decoction improves gastrointestinal motility in functional dyspepsia with spleen deficiency syndrome by restoring mitochondrial quality control homeostasis. Phytomedicine. 2022;105:1–10. doi: 10.1016/j.phymed.2022.154374. [DOI] [PubMed] [Google Scholar]
- Zhang S., Zhao L., Wang H., Wu B., Wang C., Huang S.…Lai Y. Efficacy of gastrosis No.1 compound on functional dyspepsia of spleen and stomach deficiency-cold syndrome: A multi-center, double-blind, placebo-controlled clinical trial. Chinese Journal of Integrative Medicine. 2013;19(7):498–504. doi: 10.1007/s11655-013-1503-x. [DOI] [PubMed] [Google Scholar]
- Zhang F.Y. Clinical value of Amomum Villosum in the treatment of functional dyspepsia. Journal of Clinical Rational Drug Use. 2014;7(12):124–125. [Google Scholar]
- Zhang N. Inner Mongolia Medical University; Thesis of Master Degree: 2021. Effect of hypericum perforatum on gastrointestinal motility and ENS in rats with functional dyspepsia. [Google Scholar]
- Zhang X.Q., Wang F., Wei H.L., Wang C.L., Han X.D. Effect of Swertia Herba on the expression of gastrointestinal hormones in functional dyspepsia of wistar rats. Chinese Journal of Basic Medicine In Traditional Chinese Medicine. 2016;22(7):912–914. [Google Scholar]
- Zhang Y. Chaihu Dayuan decoction in the treatment of functional dyspepsia with pattern of dampnessheat in stomach and spleen. Jilin Journal of Chinese Medicine. 2020;40:1034–1037. [Google Scholar]
- Zhang Z.X., Li X. The study of Fructus aurantii immaturus consolidating the mechanism of improving gastric dysmotillity in functional dyspepsia rats. Shaanxi Journal of Traditional Chinese Medicine. 2018;39(8):998–1000. [Google Scholar]
- Zhou J.P., Wang X.P., Cao Z.Q., Wang Y.F. Internet pharmacology study of Banxia Xiexin decoction in the treatment of functional dyspepsia. World Chinese Medicine. 2021;16(17):2576–2581. [Google Scholar]
- Zhou S.N., Cai G.X., Wang S. Effect of Simo decoction on functional dyspepsia with qi staganacy of both liver and spleen and on nitrie oxide, acetylcholinesterase, cholecystokinin and substance P in serum, the bottom of stomach, the gastric antrum and the duodenum. Chinese Journal of Integrated Traditional and Western Medicine on Digestion. 2015;23(1):17–20. [Google Scholar]
- Zhu J.Z., Zhang J., Zhang Z.J., Wang W. Effects of Amomum villosum on functional digestion disorder in rats. West China Journal of Pharmaceutical Sciences. 2006;21(1):58–60. [Google Scholar]