Abstract
We report a case of cardiac beriberi in a 76-year-old man who was hospitalized with a congestive condition of subacute onset, diagnosed as high-output heart failure associated with severe tricuspid regurgitation and indication for caval valve implantation, which, after thiamine replacement, resulted in improvement of all conditions. (Level of Difficulty: Beginner.)
Key Words: beriberi, heart failure, thiamine deficiency, tricuspid valve insufficiency
Central Illustration
Thiamine (vitamin B1) is a water-soluble vitamin available in fruits, vegetables, meat, and grains, and it is essential for cell metabolism. Chronic alcoholism and inadequate diet are the main risk factors for vitamin B1 deficiency worldwide. Its deficiency can affect the cardiovascular system in a manifestation also called wet beriberi.1,2
Learning Objectives
-
•
To explain that thiamine deficiency is a reversible cause of heart failure.
-
•
To identify that pulmonary hypertension can be caused by thiamine deficiency.
Cardiac beriberi, a rare cause of thiamine deficiency, occurs because of decreased cardiac function at the expense of impaired cellular metabolism, where a state of high compensatory output is initiated owing to reduced systemic vascular resistance.3
Not only is thiamine deficiency a reversible cause of heart failure (HF), but patients with HF can also experience such a deficiency. The main mechanisms are the use of diuretics, advanced age, and metabolism alteration.1,4
History of Presentation
A 76-year-old man was referred to our hospital with dyspnea and generalized edema that began 20 days before admission. He presented with no signs of hemodynamic instability, and his heart hate was 72 beats/min in sinus rhythm. On physical examination, he was well perfused and had jugular venous distention. Lung auscultation revealed bilateral crackles and a systolic murmur on tricuspid focus. His abdomen had voluminous ascites, and he had important peripheral edema. He was overweight, with a body mass index of 27.8 kg/m2 (height 1.76 m; weight 86 kg).
on, admission transthoracic echocardiography (TTE) revealed a right ventricle with compromised systolic function, fractional area change of 33%, and tricuspid regurgitation (TR) with vena contracta of 14 mm, preserved left ventricular function, and a normal functioning aortic bioprosthesis. His cardiac index was calculated through TTE with a value of 8.0 L/min/m2, suggesting hyperdynamic circulation.
A previous TTE 9 months before admission had shown normal right and left ventricular function and no tricuspid valve disfunction.
Medical History
The patient had hypertension, hypothyroidism, and a history of poor intake of meat for the past 6 months, with loss of weight and a history of chronic alcoholism. In addition, he had undergone implantation of an aortic bioprosthesis and myocardial revascularization in 2019.
The Committee of Ethics in Research at Hospital de Urgências de Goiás, linked to the Plataforma Brasil, approved this study under number CAAE: 85497418.2.0000.0033.
Differential Diagnoses
The differential diagnoses included acute pulmonary embolism, chronic thromboembolic pulmonary hypertension, myocarditis, ischemic cardiomyopathy, and carcinoid syndrome.
Investigations
After the initial screening, a new 3D TEE was performed for better evaluation of both ventricles and investigation of carcinoid syndrome. This examination confirmed a serious TR with effective regurgitant orifice area of 0.94 cm2, regurgitant volume of 59 mL, dilation of the tricuspid annulus (44 mm) secondary to right atrial dilatation, and hepatic vein flow (Figures 1, 2, 3, 4, and 5, Videos 1, 2, 3, and 4).
Figure 1.
2-Dimensional Transthoracic Echocardiography
Parasternal right ventricle inflow view with color showing coaptation failure of tricuspid valve before treatment. RA = right atrium.
Figure 2.
2-Dimensional Transthoracic Echocardiography
4-chamber apical view with color showing coaptation failure of tricuspid valve before treatment. RA = right atrium; RV = right ventricle; TR = tricuspid regurgitation.
Figure 3.
2-Dimensional Transthoracic Echocardiography
4-chamber apical view without color showing coaptation failure of tricuspid valve before treatment. Abbreviations as in Figure 2.
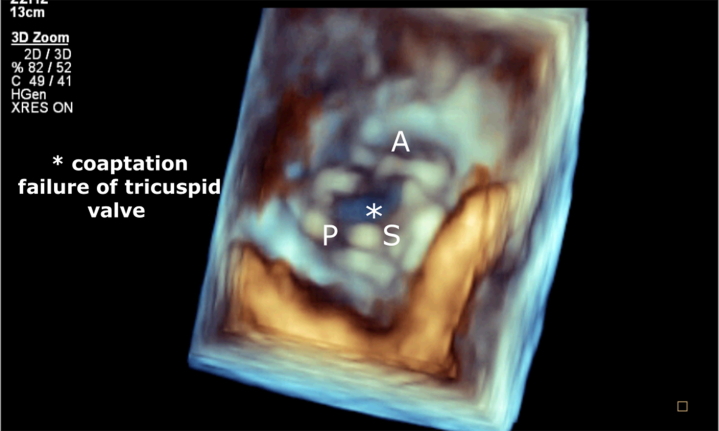
Figure 4.
3-Dimensional Transthoracic Echocardiography
Coaptation failure of tricuspid valve before treatment. A = anterior; P = posterior; S = septal.
Figure 5.
2-Dimensional Transthoracic Echocardiography
(A) Hepatic vein flow. (B) Right ventricle inflow view. Effective regurgitant orifice area 0.94 cm2 and regurgitant volume 59 mL.
During hospitalization, pulmonary scintigraphy was performed to exclude acute embolism and chronic thromboembolic pulmonary hypertension, as is recommended by the European Society of Cardiology guidelines; myocarditis and myocardial ischemia were excluded by cardiac magnetic resonance, which revealed an unspecific myocardial delayed enhancement nonischemic pattern. Right and left cardiac catheterization was performed and showed a dominant right coronary artery and left main occluded on their origin, both irrigated by 2 aortocoronary saphenous vein graft anastomosis to the right coronary artery and left anterior descending, with normal flow and no obstructive lesions. The pulmonary artery pressure was 55/13 mm Hg, and the mean pulmonary artery pressure was 27 mm Hg, with pulmonary artery wedge pressure of 13 mm Hg; unfortunately, the invasive measurements of cardiac output and hemodynamic calculation of resistances were not taken at that moment. Laboratory test results were as follows: acute kidney injury Kidney Disease Improving Global Outcomes2 (KDIGO2), lactic acid 1.0 mmol/L, normal thyroid function, thiamine serum levels 34.2 μg/L (reference: 32-82 μg/L), and paracentesis with analysis of serum ascites albumen gradient ≥1.1.5
Management
During hospitalization, the patient showed partial clinical improvement after triple diuretic therapy with furosemide, spironolactone, and hydrochlorothiazide in high doses but maintained monthly repeated hospitalizations because of ascites and congestion, in NYHA functional class III. The heart team discussed the diagnostic hypotheses when faced with secondary TR of undefined cause and without clinical improvement, and caval valve implantation (CAVI) was then indicated.
As reported, we were faced with a case of HF with TTE and clinical evidence of high-output hemodynamic states of an undefined cause. Several causes may lead to HF, including cardiac beriberi. Therefore, on an outpatient basis, empirical oral thiamine replacement at a dose of 300 mg per day was started.
After approximately 60 days, waiting for the CAVI reimbursement issues, the patient returned to the outpatient consultation, with significant clinical improvement, in NYHA functional class I, without ascites or edema during this period, and after the initial treatment he did not need further hospitalization for clinical compensation.
A new TEE was then performed as an immediate preprocedure index and showed complete improvement in the TR, as seen in Figure 6 and Video 5, and tricuspid annulus measuring 33 mm, right chambers with normal diameters as seen in the parallel comparisons between before and after treatment in Figure 7, preserved RV function (fractional area change 41%) with pulmonary artery systolic pressure 36 mm Hg. The CAVI implantation was cancelled, thiamine replacement was maintained at a dose of 100 mg, and diuretic doses were reduced.
Figure 6.
2-Dimensional Transthoracic Echocardiography
4-chamber apical court showing mild tricuspid regurgitation after treatment. LA = left atrium; LV = left ventricle; other abbreviations as in Figure 2.
Figure 7.
2-Dimensional Transthoracic Echocardiography
Comparison of the end-systolic area. (A) Area measure of 13.7 cm2 before thiamine treatment. (B) Area measure of 8.48 cm2 after thiamine treatment. EDA = end diastolic area; ESA = end systolic area; FAC = fractional area change; RV = right ventricle.
Discussion
The present case highlights a picture of HF and pulmonary arterial hypertension (PAH) secondary to thiamine deficiency, which after its replacement resulted in improvement of HF symptoms, echocardiographic findings of TR, and dilation of the right heart chambers.
The pathophysiological basis involved in this process is still unclear. The work of both ventricles is increased in thiamine deficiency, and this can be explained by the increase in blood volume, which may imply an increase in pulmonary artery pressure due to increased pulmonary blood flow, causing (PAH).6
Similar cases have been reported, and as described in those reports, the hyperdynamic state was the key point for suspecting cardiac beriberi.3,7,8 Our patient had an echocardiographic estimated cardiac index of 8.0 L/min/m2, and after the exclusion of other causes, this was one of the main data for initiating empirical treatment with thiamine replacement. By contrast, Asakura et al6 described a case of PAH associated with right heart failure and TR responsive to empirical treatment with thiamine without signs of high output, concluding that cardiac beriberi does not necessarily occur to the detriment of a hyperdynamic circulation.6
The laboratory measurement of thiamine deficiency has its limitations because of the short half-life in the blood. In our case report, the serum levels of thiamine collected 7 days after admission were 34.2 μg/L (reference value 32-82 μg/L), which could invalidate the hypothesis of deficiency. Otherwise, inasmuch as the nutritional oral adjustment had already been initiated and the plasma concentration was directly related to the individual's caloric intake on the last few days, the laboratory measurement may have detected the recent thiamine intake rather than the actual corporal thiamine status.4,9
The confirmatory laboratory test for thiamine deficiency is performed through the activity of erythrocytic transketolase; however, it is an expensive test and is not available in most services. For this reason, the therapeutic test is performed to confirm suspected cases.10
The diagnosis of cardiac beriberi in this case was made through a therapeutic trial with the administration of thiamine. The patient had determined risk factors for vitamin B1 deficiency, such as previous alcoholism and low thiamine food intake. Moreover, prevalent differential diagnosis was excluded.
Follow-Up
After 120 days, the patient’s condition was reassessed, and he remaining in a clinically stable status.
Conclusions
Cardiac beriberi is a rare form of potentially reversible HF, of which the diagnosis can be made by excluding the most prevalent other causes and applying this inexpensive and trivial therapeutic testing, considering dosage limitations and no collateral effects as described in this case report.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
2-Dimensional Transthoracic Echocardiography
Parasternal right ventricle inflow view with color showing coaptation failure of tricuspid valve before treatment.
2-Dimensional Transthoracic Echocardiography
4-chamber apical view without color showing coaptation failure of tricuspid valve before treatment.
2-Dimensional Transthoracic Echocardiography
4-chamber apical view with color showing coaptation failure of tricuspid valve before treatment.
3-Dimensional Transthoracic Echocardiography
Coaptation failure of tricuspid valve before treatment.
2-Dimensional Transthoracic Echocardiography
4-chamber apical view with color showing mild tricuspid regurgitation after treatment
References
- 1.Sliwa K., Viljoen C.A., Hasan B., Ntusi N.A.B. Nutritional heart disease and cardiomyopathies: JACC focus seminar 4/4. J Am Coll Cardiol. 2023;81(2):187–202. doi: 10.1016/j.jacc.2022.08.812. [DOI] [PubMed] [Google Scholar]
- 2.Attaluri P., Castillo A., Edriss H., Nugent K. Thiamine deficiency: an important consideration in critically ill patients. Am J Med Sci. 2018;356(4):382–390. doi: 10.1016/j.amjms.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 3.Park J.H., Lee J.H., Jeong J.O., Seong I.W., Choi S.W. Thiamine deficiency as a rare cause of reversible severe pulmonary hypertension. Int J Cardiol. 2007;121(1):e1–e3. doi: 10.1016/j.ijcard.2006.08.054. [DOI] [PubMed] [Google Scholar]
- 4.Eshak E.S., Arafa A.E. Thiamine deficiency and cardiovascular disorders. Nutr Metab Cardiovasc Dis. 2018;28(10):965–972. doi: 10.1016/j.numecd.2018.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Humbert M., Kovacs G., Hoeper M.M., et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618–3731. doi: 10.1093/eurheartj/ehac237. [DOI] [PubMed] [Google Scholar]
- 6.Asakura T., Kodera S., Kanda J., Ikeda M. Thiamine-responsive pulmonary hypertension. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2012-007938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamasaki H., Tada H., Kawano S., Aonuma K. Reversible pulmonary hypertension, lactic acidosis, and rapidly evolving multiple organ failure as manifestations of Shoshin beriberi. Circ J. 2010;74(9):1983–1985. doi: 10.1253/circj.cj-10-0202. [DOI] [PubMed] [Google Scholar]
- 8.Coelho L.S., Hueb J.C., Minicucci M.F., Azevedo P.S., Paiva S.A., Zornoff L.A. Thiamin deficiency as a cause of reversible cor pulmonale. Arq Bras Cardiol. 2008;91(1):e7–e9. doi: 10.1590/s0066-782x2008001300013. [DOI] [PubMed] [Google Scholar]
- 9.Helali J., Park S., Ziaeian B., Han J.K., Lankarani-Fard A. Thiamine and heart failure: challenging cases of modern-day cardiac beriberi. Mayo Clin Proc Innov Qual Outcomes. 2019;3(2):221–225. doi: 10.1016/j.mayocpiqo.2019.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gabrielli A., Caruso L., Stacpoole P.W. Early recognition of acute cardiovascular beriberi by interpretation of hemodynamics. J Clin Anesth. 2001;13(3):230–238. doi: 10.1016/s0952-8180(01)00246-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
2-Dimensional Transthoracic Echocardiography
Parasternal right ventricle inflow view with color showing coaptation failure of tricuspid valve before treatment.
2-Dimensional Transthoracic Echocardiography
4-chamber apical view without color showing coaptation failure of tricuspid valve before treatment.
2-Dimensional Transthoracic Echocardiography
4-chamber apical view with color showing coaptation failure of tricuspid valve before treatment.
3-Dimensional Transthoracic Echocardiography
Coaptation failure of tricuspid valve before treatment.
2-Dimensional Transthoracic Echocardiography
4-chamber apical view with color showing mild tricuspid regurgitation after treatment