Abstract
Spontaneous coronary artery dissection is a rare but potentially life-threatening condition that predominantly affects women, particularly during pregnancy or postpartum period. We present a case of peripartum spontaneous coronary artery dissection in a 41-year-old African woman, highlighting the clinical presentation, diagnostic challenges, and management strategies.
Key Words: myocardial infarction, Peripartum, spontaneous coronary artery dissection, Sub-Saharan Africa
Central Illustration
Case Presentation
A 41-year-old Black female patient presented to the emergency department of Abidjan Heart Institute on March, 31, 2023, with acute chest pain and shortness of breath 1 week after her fourth uncomplicated spontaneous vaginal delivery of a healthy baby. She complained of 6 hours of crushing central chest pain with posterior radiation, 7 of 10 (visual analog scale). She had no significant past medical history or cardiovascular risk factors except for gestational hypertension. On exam, heart rate was 104 beats/min, blood pressure 165/100 mm Hg, and saturation 98% on room air. Pulmonary and cardiac auscultation was unremarkable. No pain or edema was found in her lower extremities.
Learning Objectives
-
•
To be able to make a differential diagnosis of chest pain syndromes during pregnancy and peripartum period.
-
•
To plan and decide on the management strategies for peripartum SCAD.
Question 1: What Is the Differential Diagnosis of an Acute Chest Pain in Peripartum?
-
•
Pulmonary embolism
-
•
Type 1 myocardial infarction
-
•
Spontaneous coronary artery dissection
-
•
Aortic dissection
-
•
Other
There is a wide range of chest pain syndromes during pregnancy or puerperium, including pulmonary embolism (PE), amniotic fluid embolism, acute myocardial infarction, and aortic dissection.1 Acute high-risk chest pain diseases are the leading causes of maternal death in developed countries.2 Thus, early recognition and management of these threatening conditions are essential for reducing mortality in pregnancy and puerperium. Recent comprehensive data from the Nationwide Inpatient Sample showed that the most frequent acute high-risk chest pain disease is PE (86.5%),3 which is significantly ahead of acute myocardial infarction (9.6%) and aortic dissection (3.3%). D-dimer testing to rule out PE during pregnancy and puerperium remains debated, because it is physiologically elevated in these situations. Identification of deep vein thrombosis of the lower limbs may be useful, with sensitivity >90% and specificity of ∼95% for proximal localization. Finally, definitive diagnosis of PE requires imaging, and, in our case, PE was excluded after computed tomography pulmonary angiography, as well as aortic dissection.
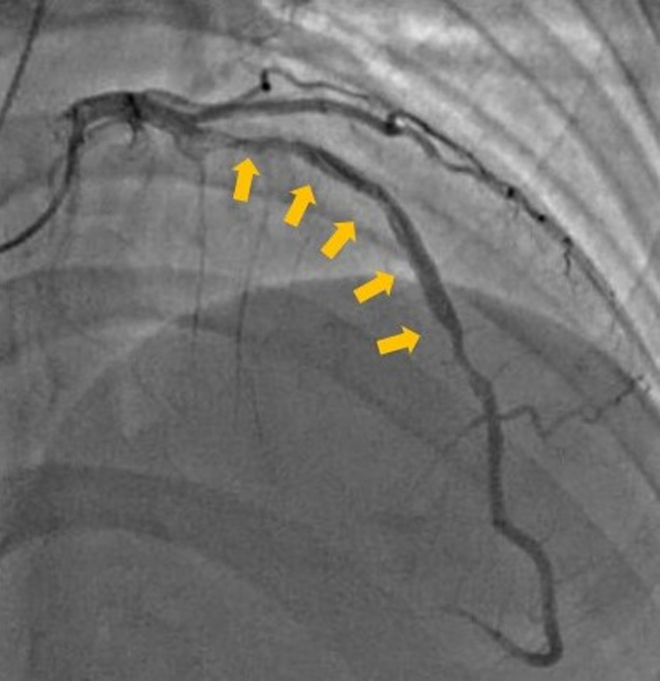
Peripartum spontaneous coronary artery dissection (SCAD) is an uncommon presentation of acute myocardial infarction and can be challenging to diagnose due to its overlapping clinical presentation with other cardiac conditions. In the presented case, electrocardiogram showed, and T-wave inversion in inferior and anterior leads, and slight ST-segment elevation in V2-V3 leads. Blood sampling showed high levels of troponin I (5,338 ng/L), creatine kinase (528 IU/L) and creatine kinase-myocardial band (48 IU). After loading doses of 300 mg aspirin and 300 mg clopidogrel, immediate coronary angiography revealed a type 1 SCAD with long dissection flap involving the proximal and mid segments of the left anterior descending artery, and TIMI flow grade 3 (Figure 1, Video 1). Intracoronary imaging with intravascular ultrasound or optical coherence tomography allows better identification of intimal tears and flap and confirmation of guidewire position in the true lumen during percutaneous coronary intervention (PCI) procedure. These advanced tools are not available in our practice.
Figure 1.
Coronary Angiography at Admission
Left coronary angiogram showing type 1 spontaneous coronary artery dissection of the left anterior descending artery. LAO 10°, CRA 40°. Yellow arrows indicate the intimal flap. CRA = cranial; LAO = left anterior oblique.
Question 2: What Are the Predisposing Factors for Peripartum SCAD?
The pathophysiology of peripartum SCAD is not fully understood, but hormonal and mechanical factors associated with pregnancy may be incriminated. Hormonal changes, such as increased levels of estrogen and progesterone and decreased collagen synthesis lead to weakening of the media.4 Additionally, some investigators suggested that hemodynamic changes that occur during pregnancy, including higher plasma volume and cardiac output, lead to increased shear forces on intima and may contribute to the development of dissections.
Fibromuscular dysplasia was the most commonly reported associated pathology. Fibromuscular dysplasia affects younger women and is currently underdiagnosed.5 Other patients with peripartum SCAD have inherited connective tissue disorders, such as Marfan, Ehlers-Danlos, and Loeys-Dietz syndromes, whose prevalence in peripartum SCAD patients is estimated to be <2.5% or pre-existing conditions that may predispose to peripartum SCAD including abnormalities of the coronary arteries, vasculitis such as Kawasaki disease, hypereosinophilic syndrome, ulcerative colitis, and systemic lupus erythematosus.5
In this case, the patient had no known pre-existing cardiovascular risk factors, apart from gestational hypertension, which further highlights the importance of considering peripartum SCAD in the differential diagnosis of chest pain in young individuals, even in the absence of traditional risk factors.
Question 3: How to Manage Peripartum Coronary Artery Dissection?
Clinical presentation, hemodynamic parameters, and angiographic and/or imaging features of the dissection are the main factors for the choice of the treatment, resulting in individualized management for each patient. A multidisciplinary team approach should be implemented involving at least a cardiologist, obstetrician, and anesthetist, as well as additional experts when needed.2 Currently, the treatment approach is largely conservative (>80%), as most segments involved in the dissection heal spontaneously.6 In clinically unstable patients (ongoing ischemia, cardiogenic shock, ventricular arrythmias) with persistent or recurrent dissection, PCI is preferred.6 Coronary artery bypass graft surgery artery revascularization procedure may be considered in some uncommon cases: left main/multivessel SCAD or PCI failure. In our case, the patient was managed medically with close observation, given she was asymptomatic without hemodynamic compromise and with single-epicardic vessel disease. She received dual antiplatelet therapy (aspirin 100 mg once daily, clopidogrel 75 mg once daily), beta blocker (bisoprolol 1.25 mg once daily), statin (atorvastatin 40 mg once daily), and angiotensin converting enzyme inhibitor (perindopril 5 mg once daily).
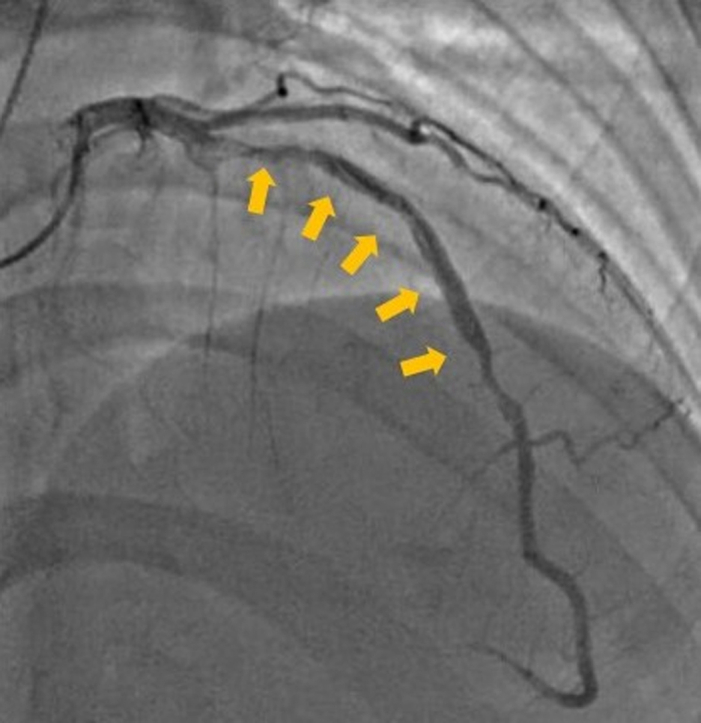
One day after, the patient's clinical course deteriorated, and she developed recurrent chest pain and electrocardiogram changes, probably as a result of extent of the coronary artery dissection. Subsequently, the decision was made to perform PCI on the left anterior descending artery. Two drug-eluting stents were successfully implanted in the left anterior descending coronary artery, resulting in rapid symptom relief (Figure 2, Video 2). It should be pointed out that PCI is sometimes a challenging task in daily clinical practice, with 20% to 60% of PCIs having complications, especially extension of the dissection.7
Figure 2.
Coronary Angiography of the Left Coronary Artery After Percutaneous Coronary Intervention
Favorable outcomes after percutaneous coronary intervention of the left anterior descending artery. LAO 10°, CRA 40°. CRA = cranial; LAO = left anterior oblique.
Question 4: What Are the Long-term Outcomes and/or Recurrent Peripartum?
Peripartum SCAD has a variable prognosis, with outcomes ranging from complete recovery to significant morbidity and mortality. In the case we describe, the patient responded well to PCI with favorable outcomes. Left ventricular ejection fraction was 60%, without regional wall motion abnormalities. However, long-term follow-up is crucial for reassessing cardiac function, identifying recurrent SCAD events and major adverse cardiac events, and managing potential cardiovascular risk factors. Recurrence rates range between 17% and 50%, being more frequent between 30 and 60 days after the first episode.7 In a recent study carried among 750 consecutive SCAD with long-term follow-up, peripartum SCAD was an independent predictor of a 3-year occurrence of major adverse cardiac events, as well as genetic disorders and extracoronary fibromuscular dysplasia.8 Patients who underwent PCI at index hospitalization had similar postdischarge major adverse cardiac events compared with no PCI.8 Collaboration between obstetric and cardiology teams can facilitate appropriate counseling and support for subsequent pregnancies, ensuring optimal outcomes for both mother and child.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Left Coronary Angiogram Showing Type 1 SCAD of the LAD (Note: Guidewire Crossing)
Post PCI Angiogram of the LAD
References
- 1.Sahni G. Chest pain syndromes in pregnancy. Cardiol Clin. 2012;30(3):343–367. doi: 10.1016/j.ccl.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 2.Mehta L.S., Warnes C.A., Bradley E., et al. Cardiovascular considerations in caring for pregnant patients: a scientific statement from the American Heart Association. Circulation. 2020;141(23) doi: 10.1161/CIR.0000000000000772. [DOI] [PubMed] [Google Scholar]
- 3.Wu S., Xu X., He Q., et al. Incidence and outcomes of acute high-risk chest pain diseases during pregnancy and puerperium. Front Cardiovasc Med. 2022;9 doi: 10.3389/fcvm.2022.968964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elkayam U., Jalnapurkar S., Barakkat M.N., et al. Pregnancy-associated acute myocardial infarction: a review of contemporary experience in 150 cases between 2006 and 2011. Circulation. 2014;129(16):1695–1702. doi: 10.1161/CIRCULATIONAHA.113.002054. [DOI] [PubMed] [Google Scholar]
- 5.Zeven K. Pregnancy-associated spontaneous coronary artery dissection in women: a literature review. Curr Ther Res. 2023;98 doi: 10.1016/j.curtheres.2023.100697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krittanawong C., Saw J., Olin J.W. Updates in spontaneous coronary artery dissection. Curr Cardiol Rep. 2020;22(10):123. doi: 10.1007/s11886-020-01378-y. [DOI] [PubMed] [Google Scholar]
- 7.Cano-Castellote M., Afanador-Restrepo D.F., González-Santamaría J., et al. Pathophysiology, diagnosis and treatment of spontaneous coronary artery dissection in peripartum women. J Clin Med. 2022;11(22):6657. doi: 10.3390/jcm11226657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saw J., Starovoytov A., Aymong E., et al. Canadian Spontaneous Coronary Artery Dissection cohort study: 3-year outcomes. J Am Coll Cardiol. 2022;80(17):1585–1597. doi: 10.1016/j.jacc.2022.08.759. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Left Coronary Angiogram Showing Type 1 SCAD of the LAD (Note: Guidewire Crossing)
Post PCI Angiogram of the LAD