Abstract
Cannabinoids have recently gained a renewed interest due to their potential applicability to various medical conditions, specifically the management of chronic pain conditions. Unlike many other medications, medical cannabis is not associated with serious adverse events, and no overdose deaths have been reported. However, both safety and efficacy data for medical cannabis treatment of chronic, nonmalignant pain conditions are lacking. Therefore, representatives from the American Society of Pain and Neuroscience summarize the evidence, according to level and grade, for medical cannabis treatment of several different pain conditions. Treatment of cancer-related pain has prospective evidentiary support for the use of medical cannabis. Although 3 large and well-designed randomized controlled trials investigated cannabis treatment of cancer-related pain, the evidence yielded only a grade D recommendation. Neuropathic pain has been investigated in prospective studies, but a lack of high-quality evidence renders cannabis treatment for this indication a grade C recommendation. Both safety and efficacy data are lacking for use of medical cannabis to treat chronic nonmalignant pain conditions.
Keywords: analgesia, chronic pain, marijuana treatment, neuralgia, postoperative pain
Introduction
To reduce pain in the perioperative setting, multimodal analgesia, including opioids and peripheral nerve blocks, is often used;1,2 however, treatment is ineffective for approximately 1 of 4 patients.3 This can be problematic because poorly managed and uncontrolled acute pain may increase the risk of complications, prolong hospital stays, reduce quality of life, and lead to development of chronic pain conditions.4,5
Cannabinoids have recently gained a renewed interest due to their potential applicability to many medical conditions, especially chronic pain conditions. Endogenous cannabinoids, such as anandamide and 2-arachidonoylglycerol, are secreted in times of stress and are known to have many different downstream effects, which include regulation of mood, appetite, and nociception.6 Similarly, the key chemical components of cannabis, namely tetrahydrocannabinol (THC) and cannabidiol (CBD), act on the cannabinoid 1 and 2 receptors to produce antinociceptive effects.6–8
Historically, cannabis-based products (CBPs) were considered effective for pain relief, but their use was limited because of a lack of clinical evidence.9,10 However, evidence documenting modest improvement with use for certain conditions, such as chronic pain and rheumatoid arthritis, has rapidly increased,11–13 but clinical evidence regarding its analgesic efficacy for various pain conditions remains conflicting.10,14 Because new treatment strategies for acute and chronic pain conditions are needed and the efficacy of CBPs for pain management is uncertain, we sought to evaluate the analgesic outcomes of patients with various chronic pain conditions. As a leader in the field of pain medicine, the American Society of Pain and Neuroscience performed a comprehensive review with the aim of developing recommendations for clinicians who consider prescribing cannabis or CBPs for the treatment of pain conditions and identifying knowledge gaps and potential areas of future studies on this topic.
Medical Cannabis Laws
Federal Regulations
In 1970, the Controlled Substances Act (CSA) consolidated all prior federal laws related to potential substances for abuse. These substances are classified by the CSA in 5 schedules according to their potential for abuse and medical efficacy (Table 1).15,16 The CSA has classified cannabis, CBPs, and THC as Schedule I drugs, which is currently a source of conflict between federal and state cannabis regulations.
Table 1.
Scheduled Classes of Controlled Substances by the Controlled Substances Act of 1970
| Schedule | Description | Example Substances |
|---|---|---|
| I | High abuse potential No accepted medical use |
Heroin, LSD, MDMA, mescaline, psilocybin, marijuana/cannabis, cannabinoids, and peyote |
| II | High abuse potential Accepted medical use |
Amphetamine, barbiturates, cocaine, fentanyl, methadone, and morphine |
| III | Medium abuse potential Accepted medical use |
Ketamine, anabolic steroids, and buprenorphine |
| IV | Moderate abuse potential Accepted medical use |
Benzodiazepines, tramadol, and carisoprodol |
| V | Lowest abuse potential Accepted medical use |
Pregabalin, lacosamide, cannabis-derived pharmaceutical formulation (ie, Epidiolex)a |
Notes: aOther cannabidiol formulations remain Schedule I except for those derived from hemp, which were unscheduled after passage of the Agricultural Improvement Act of 2018 but are still regulated by the US Food and Drug Administration.
Abbreviations: LSD, lysergic acid diethylamide; MDMA, methylenedioxymethamphetamine.
Schedule I is the most restrictive classification and includes substances with no accepted medical use and the highest potential for abuse. Safety data on use of these substances under medical supervision are lacking. Some other substances classified as Schedule I include mescaline, psilocybin, heroin, methylenedioxymethamphetamine, and lysergic acid diethylamide.
Because cannabis and cannabinoids are classified as Schedule I drugs, the ability to perform clinical trials with cannabis is considerably hindered. This classification also affects the ability of clinicians to prescribe cannabis and CBPs to their patients. Substances classified as Schedule I under the CSA can be legally possessed and/or dispensed only as part of federally approved research grants or programs. All involved manufacturers and distributors are required to obtain Schedule I drug-specific registration before initiating such research. Moreover, cannabis for research must be obtained through a facility that is contracted with the National Institute on Drug Abuse. Currently, the only facility approved to provide cannabis for research purposes is the University of Mississippi.
Because cannabis and its derivatives are classified as Schedule I drugs, physicians cannot formally prescribe these substances and may only recommend medical cannabis for their patients.15,17 According to a 2002 9th Circuit Court of Appeals decision in Conant v Walters, physicians are protected against federal prosecution for communicating about medical cannabis use with their patients by the First Amendment of the US Constitution.18,19 The court also ruled that physicians should not be held liable for a patient’s actions. Various state laws have permitted the distribution of cannabis through dispensaries, which conflicts with the CSA.
The Agricultural Improvement Act of 2018 (ie, the Farm Bill), signed into law by President Trump on December 20, 2018, legalized hemp at the federal level. Hemp is a type of cannabis plant that contains low levels of THC—the psychoactive compound that produces the high associated with cannabis. Specifically, the Farm Bill defines hemp as the Cannabis sativa L plant with a Δ9-THC concentration of 0.3% or less.20
The Farm Bill’s legalization of hemp has had a notable effect on the CBD industry. CBD is a compound in hemp that has many potential health benefits. Before the Farm Bill was passed, CBD was classified as a Schedule I controlled substance and was thereby illegal to possess or sell. However, the Farm Bill’s legalization of hemp has made it legal to manufacture and sell CBD products that are derived from hemp.
The Farm Bill has had mixed reactions. Some have welcomed the change, arguing that it will provide consumers with access to a safe and effective natural remedy. Others have expressed concern about the potential for CBD to be abused or misused. The US Food and Drug Administration (FDA) has not yet issued any regulations governing the sale of CBD products. Consequently, the CBD market is currently unregulated, which has led to concern about the quality and safety of some CBD products. The FDA is currently working to develop regulations for the sale of CBD products, and these regulations are expected to be finalized soon.20
State Regulations
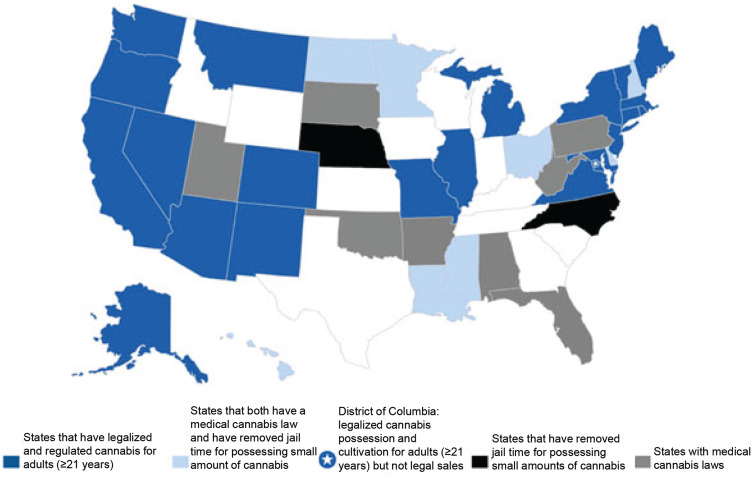
Medicinal use of cannabis was decriminalized for the first time by the state of California in 1996. The Compassionate Use Act of 1996 allowed patients and caregivers in California to cultivate and possess cannabis for medicinal use.15 State-regulated medical cannabis programs have since flourished due to limited interference by the federal government. Currently, 33 states and the District of Columbia have approved medicinal use of cannabis (Figure 1). A recent amendment to the US Consolidated Appropriations Act of 2018 restricts appropriation of federal funds to interfere with state-regulated implementation of medical cannabis laws.16
Figure 1.
Current Cannabis Regulations Among All US States. Modified from Marijuana Policy Project. https://www.mpp.org/states/; used with permission.
Policy Reform
Additional clinical and political evidence is clearly needed to guide future medical cannabis policies. In a 2017 report, the National Academies of Sciences, Engineering, and Medicine outlined that further evidence is required for US policymakers to make sound decisions regarding the use of cannabis.21 Some proposals to this end include price and tax structural reforms, increased cannabis research for remedicalization, and bridging the lack of political evidence.22–24
Safety
In contrast with many other medications, medical cannabis has not been reported to cause serious adverse events; no deaths due to overdose have been reported. Drugs that cannot be used with cannabis are not reported, although potential drug–drug interactions with some medications may negatively affect patients.25 Cotreatment with high-dose CBD and clobazam results in increased plasma levels of N-desmethylclobazam (a clobazam metabolite with sedative properties) and thereby requires a dose reduction of clobazam.26 Therefore, clinicians should be cautious when starting patients on medical cannabis and should be aware of treatments with a small therapeutic margin. Dizziness is the most common nonserious adverse event reported. However, tolerance to the psychoactive effects of cannabis can develop in a few days without loss of the medicinal benefits, unlike that of opioids; thus, long-term cannabis efficacy can be achieved with a consistent daily dose for several years.27–29
The liver is the primary site of metabolism of cannabis compounds, and approximately one-third of metabolites are eliminated in the urine. Metabolism of cannabis compounds may be altered in patients with kidney or liver impairment, and serum metabolite levels may be increased in patients taking metabolic enzyme inhibitors or decreased in those taking enzyme inducers. Some evidence suggests that cannabis may potentiate the antinociceptive effects of opioids, which permits lower and presumably safer opioid dosing to achieve comparable levels of analgesia.30,31
Cannabis use either alone or in combination with opioids has been reported to increase risk of opioid misuse, especially by patients with substance use disorders.29,31,32
Evidence for Medical Use
Headache
A small randomized controlled trial33 and several observational studies34–42 reported limited evidence for the efficacy of cannabis treatment of headache. All other evidence stems from case reports and clinical experience, which highlights the need for additional studies on this topic.43 The occurrence of nausea, vomiting, anxiety, and pain during acute migraine may be alleviated by administration of cannabis products.43 In general, inhaled cannabis may be more effective as an abortive treatment for acute headache, whereas oral formulations are more useful as a preventive treatment.34,43
Pini et al33 compared the efficacy of nabilone (a synthetic cannabinoid and dibenzopyran derivative)43 vs ibuprofen for the treatment of long-standing, intractable medication overuse headache in a randomized controlled trial. The 26 patients who completed that pragmatic crossover trial reported lower pain intensity and lower daily analgesic intake when taking nabilone than when taking ibuprofen. Furthermore, nabilone treatment resulted in a lower level of medication dependence and higher quality of life than did ibuprofen treatment. However, an observational study40 reported that medication overuse headache occurred in 81% of cannabis users vs 41% of noncannabis users. The authors of that study40 concluded that cannabis use was significantly associated with medication overuse headache (odds ratio, 6.3; 95% CI, 3.6–11.1; P<0.001) and that patients should be advised to reduce cannabis use to treat medication overuse headache effectively. Of note, cannabis discontinuation or withdrawal has also been reported to induce headache in patients.43
Cannabis use may provide relief for patients with migraine, although the level of evidence is poor and primarily reported by retrospective observational studies. A large retrospective study34 analyzing 12,293 cannabis treatment sessions for headache and 7441 sessions for migraine reported a nearly 50% decrease in headache and migraine severity ratings after cannabis use. The authors also reported that tolerance to cannabis efficacy for headache and migraine occurs with subsequent uses; therefore, tolerance is a risk factor for cannabis use for this indication. Another retrospective analysis35 performed at 2 clinics in Colorado with 121 adult patients with migraine reported that abortive or preventive treatment with cannabis was associated with a reduced migraine frequency from 10.4 to 4.6 migraines per month. The patients in that study most commonly used inhaled forms of cannabis for acute migraine treatment. The efficacy of cannabis treatment of migraine is further substantiated by a cross-sectional study of 145 patients,38 of whom 61% reported at least a 50% decrease in monthly migraine frequency after initiating cannabis treatment. These patients also reported lower migraine disability, opioid use, and triptan consumption. Furthermore, another cross-sectional study42 reported that patients with migraine had better relief of migraine symptoms with cannabis than with noncannabis products, even after statistically controlling for migraine severity.
Patients with migraine reportedly prefer hybrid strains of cannabis, such as OG Shark, which has a high level of Δ9-THC and low level of CBD.39 OG Shark was also noted to be the most preferred cannabis strain for relief of migraine and headache symptoms.39 This may reflect the potent analgesic, anti-inflammatory, and antiemetic properties of THC for migraine and chronic pain treatment.39 This finding was further supported by a mixed-effect regression model reported in an observational study41 that showed that CBPs with THC levels of 10% or higher are the strongest predictor of symptom relief for migraine. However, THC doses are often limited because of dose-dependent adverse effects of psychosis and psychotropic effects.44
In addition to migraine and medication overuse headache, other types of headache may also benefit from cannabis treatment. A study of 139 patients with cluster headache at 2 headache centers reported a history of cannabis use by 45.3% of patients.36 In that study, cannabis use was associated with younger age, male sex, and tobacco smoking. Only 25.9% of cannabis users reported some efficacy for cluster headache symptoms, whereas 51.8% reported variable or uncertain effects. Similarly, in a cohort of patients with multiple sclerosis–associated trigeminal neuralgia,37 more than 70% of patients reported relief with inhaled cannabis. Because of the limitations in currently reported studies, the role of cannabis in dependence, withdrawal, and rebound headaches is unclear.
Musculoskeletal Pain
Noncancer-related chronic pain affects approximately 30% of the US population, and musculoskeletal pain, such as back, arthritis, and myofascial pain, accounts for a large proportion of chronic pain globally.45 Use of medical cannabis for treating chronic musculoskeletal pain remains divisive. The primary limitation of medical cannabis treatment of musculoskeletal pain is that most relevant studies are focused on spinal cord injury, multiple sclerosis, and fibromyalgia.12 Although many clinical trials of medical cannabis treatment of noncancer-related chronic pain have been performed, a systematic review showed that only 4 of 79 of those trials had a low risk of bias.12 Additionally, the evidence for cannabis efficacy for musculoskeletal pain is limited because of small sample sizes, limited duration, unclear dosages (reporting maximum dose vs actual dose), and pain intensity changes as secondary outcomes in many studies.46 Despite these biases and limitations, moderate quality evidence suggests that medical cannabis is effective for the treatment of noncancer-related chronic musculoskeletal pain.12
Although a systematic review reported no differences in musculoskeletal pain relief according to the type of cannabinoid tested,12 a subsequent systematic review46 reported that the highest quality evidence indicated that nabiximols was superior to other cannabinoids. Nabiximols contains an approximate 1:1 THC/CBD ratio and was approved for treatment of intractable spasticity related to multiple sclerosis in humans in several European countries and Canada.47 Although some evidence supports the use of medical cannabis for rheumatoid arthritis pain13 and orofacial pain,48 no randomized trials have been performed with patients who have osteoarthritis or myofascial pain.
Common adverse effects of medical cannabis treatment of musculoskeletal pain include fatigue, dizziness, and mild to moderate cognitive disturbances.49 Because data to determine appropriate dosages and detect potential adverse effects associated with long-term usage are lacking, the use of medical cannabis for treating musculoskeletal pain is controversial. Although evidence to recommend its routine use is deficient, the safety profile of medical cannabis is reassuring. Nevertheless, medical cannabis should be used only after discussion with a clinician regarding its uncertainties and when standard therapies are ineffective.
Cancer-Related Pain
Chronic pain adversely affects the quality of life for patients with all stages of cancer.50,51 Although cancer-related pain is often the largest contributor to poor quality of life, patients with cancer are also commonly affected by anorexia and nausea, especially when undergoing chemotherapy treatment. Consequently, CBPs have long been heralded as appropriate for oncology patients because of their purported benefits for providing analgesia, stimulating appetite, and reducing emesis.52,53 Although the FDA has approved the use of certain CBPs for the treatment of nausea and vomiting, anorexia, and weight loss, no CBPs are approved for the treatment of cancer-related pain.54 Increasingly liberalized jurisdictions and legal standings have resulted in off-label use of CBPs during the past several years.55 Some recent studies reported that up to 40% of patients with cancer in the US used cannabis for symptom management.56,57 Current National Comprehensive Cancer Network guidelines thereby advocate for clinicians to assess CBP use and provide education about regional legalities.58
Although cancer-related pain is typically treated with opioid-based therapies, many patients have pain that is either refractory to opioids or limited by opioid-specific adverse effects.59,60 Therefore, alternative treatment strategies, including use of CBPs, are often sought, especially for patients with advanced cancer.52–54 Despite moderate to extensive preclinical evidence for the analgesic benefits of cannabis, a similar depth of clinical evidence for cannabis use in humans is lacking. Consequently, no national recommendations supporting the use of CBPs for the treatment of cancer-related pain are available, and most oncologists report feeling unequipped to make discrete supportive recommendations for cannabis use.61 The European Society for Medical Oncology 2018 guidelines state that supporting evidence for CBP treatment of cancer-related pain is largely lacking and provided a grade D recommendation (ie, conclusions are limited or not possible because of unavailable, poor quality, or contradictory evidence) for its use.62
The most robust supporting evidence for treatment of cancer-related pain with CBPs is derived from 2 large randomized controlled trials that reported superiority of nabiximols vs placebo for treating cancer pain that is refractory to opioid therapy.63,64 An oromucosal sublingual spray containing nabiximols is the most studied CBP for cancer-related pain.64 However, a recent randomized controlled trial by Lynch et al65 reported that nabiximols treatment was equivalent to placebo for patients with chemotherapy-induced peripheral neuropathy. Despite this finding, nabiximols was approved for treatment of cancer-related pain in Canada and several parts of Europe. In 2017, Aviram et al66 reported a benefit from all CBPs tested for the treatment of cancer-related pain in a meta-analysis of 10 studies. Most of those studies used THC formulations, and an aggregate 0.76 pain score reduction vs that of placebo was reported.66
Evidence and Grading (Level II, Grade D)
The evidence for cannabis and CBP treatment of cancer-related pain is considered level II because of 3 well-designed, large randomized controlled trials. However, this evidence yields only a grade D recommendation because of the lack of supportive evidence for CBPs reported by more robust clinical trials and across all cancer contexts.
Chronic Postoperative Pain
Persistent postsurgical pain (PPSP) is a well-recognized phenomenon that occurs in 10% to 20% of patients and typically lasts 3 to 6 months after a procedure.5,67 The precise cause is procedure-specific and can be predominantly neuropathic or nociceptive, mixed neuropathic-nociceptive, or even partly nociplastic.5,67–69 Targeted treatment strategies are dependent on the implicated underlying cause of the pain. Moreover, robust treatment of acute postoperative pain is also suggested to prevent the development of PPSP. Although various neuromodulators, anti-inflammatory drugs, and opioids are recommended for treatment of acute postoperative pain and/or PPSP, treatment with cannabis or CBPs is not supported by any recommendations from major organizations or high-level evidence.5,67,70,71
Use of cannabis or CBPs for the treatment of postoperative pain is not described by either the 2016 clinical practice guideline for the management of postoperative pain authored by the American Pain Society, American Society of Regional Anesthesia and Pain Medicine, and American Society of Anesthesiologists or the 2020 fact sheet published by the International Association of the Study of Pain.70,71 Moreover, low-level evidence in this context is also largely lacking. An ongoing clinical trial (NCT03825965) sponsored by McMaster University seeks to compare the efficacy of cannabinoids vs placebo for the treatment of PPSP after total knee arthroplasty.72 However, results from this study are forthcoming and have not been published.
Evidence and Grading (Level IV-V, Grade F)
The evidence for cannabis and CBP use for treating PPSP is level IV to V. However, this evidence yields only a grade F recommendation because of the lack and clarity of supportive evidence and absence of recognition or recommendations from multiple national organizations.
Fibromyalgia
Fibromyalgia is a pain syndrome consisting of chronic widespread pain. Additionally, fibromyalgia has a range of associated symptoms, such as fatigue, sleep disturbances, and depression/anxiety.73 In the general population, the estimated global prevalence is 2.7%, and most affected patients are female.74 Fibromyalgia is the third most common musculoskeletal pain condition after lumbar pain and osteoarthritis.75
Numerous guidelines have been published for the appropriate diagnosis of fibromyalgia. The 2016 guidelines by the American College of Rheumatology state that pain must be present in at least 4 of 5 regions (ie, left upper, right upper, left lower, right lower, and axial regions), in addition to a Widespread Pain Index score of at least 7, presence of generalized pain, and symptoms lasting more than 3 months.76 Guidelines by the American Pain Society Pain Taxonomy state that a multisite pain score of at least 6, moderate to severe sleep problems or fatigue, and symptoms lasting more than 3 months are required for fibromyalgia diagnosis.77
Various studies have investigated the use of medical cannabis for the treatment of fibromyalgia symptoms, such as pain, sleep disturbances, and fatigue.78–81 Ware et al78 performed a randomized, double-blind, controlled study comparing nabilone to amitriptyline treatment of insomnia for patients with fibromyalgia. For the 29 patients who completed the trial, improved sleep quality (measured with the Insomnia Severity Index and Leeds Sleep Evaluation Questionnaire) was greater with nabilone than with amitriptyline.78 Skrabek et al79 conducted a randomized, double-blind, placebo-controlled trial of the efficacy of nabilone for pain and quality of life improvement in 40 patients with fibromyalgia. Nabilone dosage was titrated from 0.5 mg at bedtime to 1 mg twice a day during a 4-week treatment period. After 4 weeks, visual analog scale, Fibromyalgia Impact Questionnaire, and anxiety scores were improved, but several adverse effects were reported, which included dizziness, nausea, and dry mouth. These adverse effects are commonly reported for nabilone and other synthetic THC compounds.79
Some observational studies have also investigated the use of medical cannabis for the treatment of fibromyalgia symptoms.80,81 A pilot study by Schley et al80 assessed the use of medical cannabis in 9 patients with fibromyalgia. Although the study did not include a control group, dronabinol doses of 10 mg to 15 mg significantly reduced pain levels recorded by the patients. Weber et al81 performed a retrospective, multicenter, telephone interview survey study of patients with fibromyalgia who were treated with an average of 7.5 mg of THC (dronabinol) during a 7-month period. Dronabinol treatment decreased visual analog scale pain scores from 7.9 to 4.4 for those patients.
Evidence and Grading (Level II, Grade C)
Because several randomized, multicenter, placebo-controlled trials have assessed the use of medical cannabis for fibromyalgia, the evidence level is II. However, this evidence yields only a grade C recommendation because of the lack of supportive evidence from numerous clinical trials and the need for more randomized placebo-controlled trials with larger sample sizes.
Neuropathic Pain
Neuropathic pain is defined as pain secondary to a lesion or disease of the somatosensory system.82 It can result from various conditions, such as metabolic conditions (eg, diabetic neuropathy), autoimmune conditions, trauma, infection, or exposure to toxins.82 The worldwide prevalence for neuropathic pain is estimated to be between 7% and 10% of the general population.83 Neuropathic pain can be further subdivided into central neuropathic pain and peripheral neuropathic pain.83 The causes of central neuropathic pain include pain secondary to brain injury, spinal cord injury, stroke, and multiple sclerosis.83 The causes of peripheral neuropathic pain include trigeminal neuralgia, peripheral nerve injury, postherpetic neuralgia, and many radiculopathies.83
The first-line treatment of neuropathic pain generally consists of gabapentinoids, tricyclic antidepressants, or selective serotonin-norepinephrine reuptake inhibitors, which is outlined by the Neuropathic Pain Special Interest Group of the International Association for the Study of Pain.84 Second-line treatments of neuropathic pain include lidocaine, capsaicin, and tramadol, and third-line treatments consist of opioids such as morphine and oxycodone.84 Despite the lack of widespread use of cannabis or CBPs for neuropathic pain, research has indicated that cannabinoids targeting the endocannabinoid system may be beneficial.85
Several studies have assessed the use of medical cannabis for neuropathic pain conditions. In a randomized, placebo-controlled trial by Abrams et al,86 50 patients with HIV-associated peripheral neuropathy were randomly assigned to smoke cannabis (3.56% THC) or placebo cigarettes 3 times a day for 5 days. Overall, 52% of patients in the cannabis group reported a greater than 30% reduction in pain, whereas 24% of those in the placebo group had a greater than 30% pain reduction. Additionally, the first treatment dose reduced pain by a median of 72% in the cannabis group. In a similar study by Ellis et al,87 28 patients with HIV-associated peripheral neuropathy received treatment with cannabis 4 times daily for 5 days or a placebo treatment. Patients in the cannabis group had significantly greater pain relief than did those in the placebo group.
Additional studies have observed the use of cannabis for pain symptoms associated with diabetic neuropathy. In a study by Wallace et al,88 16 participants with diabetic neuropathy received treatment with cannabis to assess short-term efficacy and tolerability. Each patient underwent treatment with various dosing sessions, which included placebo, low THC (1%), medium THC (4%), and high THC (7%). Cannabis treatment resulted in a significant dose-dependent reduction in diabetic neuropathy–associated pain for patients in whom first-line medications failed. In a study by Wilsey et al,89 38 patients with diabetic neuropathy had a similar dose-dependent reduction in pain. Both of these studies highlight the potential efficacy of inhaled cannabis for the treatment of central and peripheral neuropathic pain and its potential for dose-dependent reductions in pain.
Evidence and Grading (Level I, Grade C)
Despite increasing evidence of the efficacy of inhaled cannabis and cannabis extracts on treating neuropathic pain, additional randomized controlled trials with large sample sizes are needed to further assess the efficacy of medical cannabis for neuropathic pain. Level I evidence from several randomized controlled trials supports the use of cannabis for neuropathic pain. However, because of a lack of additional large-scale randomized controlled trials, the use of cannabis for the treatment of neuropathic pain yields a grade C recommendation at this time.
Conclusions
Cancer-related pain is a pain condition that appears to have some prospective evidentiary support for the use of medical cannabis. Although 3 large and well-designed randomized controlled trials have investigated cannabis treatment of cancer-related pain, the evidence yields only a grade D recommendation. Neuropathic pain is another pain condition that has been investigated in prospective studies, but a lack of high-quality evidence renders cannabis treatment for this indication a grade C recommendation.
Currently, both safety and efficacy data are lacking for the use of medical cannabis to treat chronic nonmalignant pain conditions. Transformational policy reform is needed to facilitate continued research and obtain data on medicinal use of cannabis through large randomized controlled trials. Such policy reforms will ostensibly lead to state and federal regulatory congruences, increased transparency, and consideration of stakeholder concerns to effectively adapt to increasingly societal acceptance of medical cannabis and its use among patients.
Acknowledgment
Nisha Badders, PhD, ELS, Mayo Clinic, substantively edited the manuscript. The Scientific Publications staff at Mayo Clinic provided proofreading and administrative and clerical support.
Funding Statement
There is no funding to report.
Abbreviations
CBD, cannabidiol; CBP, cannabis-based product; CSA, Controlled Substances Act; FDA, US Food and Drug Administration; PPSP, persistent postsurgical pain; THC, tetrahydrocannabinol.
Data Sharing Statement
All relevant data supporting the findings of this study are reported in the article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Dr Jackie Weisbein reports consulting, advisory board, and/or research for Abbott, Saluda, Biotronik, SI Bone, Vertos, and Medtronic, outside the submitted work. Dr Jason E Pope reports research, consultant for, and/or stock from Abbott, Saluda, Biotronik, SPR Therapeutics, Thermaquil, Spark, Painteq, Vertos, Aurora, WISE, and Boston Scientific, outside the submitted work; In addition, Dr Jason E Pope has a patent DRG Neuromonitoring licensed to NIS. Dr Dawood Sayed reports personal fees from Nevro, Saluda, and Vertos; stocks from Painteq, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists task force on acute pain management. Anesthesiology. 2012;116(2):248–273. doi: 10.1097/ALN.0b013e31823c1030 [DOI] [PubMed] [Google Scholar]
- 2.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227–233. doi: 10.2106/JBJS.J.00739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu CL, Raja SN. Treatment of acute postoperative pain. Lancet. 2011;377(9784):2215–2225. doi: 10.1016/S0140-6736(11)60245-6 [DOI] [PubMed] [Google Scholar]
- 4.Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001;87(1):62–72. doi: 10.1093/bja/87.1.62 [DOI] [PubMed] [Google Scholar]
- 5.Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618–1625. doi: 10.1016/S0140-6736(06)68700-X [DOI] [PubMed] [Google Scholar]
- 6.Borgelt LM, Franson KL, Nussbaum AM, Wang GS. The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy. 2013;33(2):195–209. doi: 10.1002/phar.1187 [DOI] [PubMed] [Google Scholar]
- 7.Klein TW. Cannabinoid-based drugs as anti-inflammatory therapeutics. Nat Rev Immunol. 2005;5(5):400–411. doi: 10.1038/nri1602 [DOI] [PubMed] [Google Scholar]
- 8.Martin BR, Wiley JL. Mechanism of action of cannabinoids: how it may lead to treatment of cachexia, emesis, and pain. J Support Oncol. 2004;2(4):305–314. [PubMed] [Google Scholar]
- 9.Aggarwal SK. Cannabinergic pain medicine: a concise clinical primer and survey of randomized-controlled trial results. Clin J Pain. 2013;29(2):162–171. doi: 10.1097/AJP.0b013e31824c5e4c [DOI] [PubMed] [Google Scholar]
- 10.Abdallah FW, Hussain N, Weaver T, Brull R. Analgesic efficacy of cannabinoids for acute pain management after surgery: a systematic review and meta-analysis. Reg Anesth Pain Med. 2020;45(7):509–519. doi: 10.1136/rapm-2020-101340 [DOI] [PubMed] [Google Scholar]
- 11.Madden K, van der Hoek N, Chona S, et al. Cannabinoids in the management of musculoskeletal pain: a critical review of the evidence. JBJS Rev. 2018;6(5):e7. doi: 10.2106/JBJS.RVW.17.00153 [DOI] [PubMed] [Google Scholar]
- 12.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456–2473. doi: 10.1001/jama.2015.6358 [DOI] [PubMed] [Google Scholar]
- 13.Richards BL, Whittle SL, Buchbinder R. Neuromodulators for pain management in rheumatoid arthritis. Cochrane Database Syst Rev. 2012;1(1):CD008921. doi: 10.1002/14651858.CD008921.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stevens AJ, Higgins MD. A systematic review of the analgesic efficacy of cannabinoid medications in the management of acute pain. Acta Anaesthesiol Scand. 2017;61(3):268–280. doi: 10.1111/aas.12851 [DOI] [PubMed] [Google Scholar]
- 15.Mead A. Legal and regulatory issues governing cannabis and cannabis-derived products in the United States. Front Plant Sci. 2019;10:697. doi: 10.3389/fpls.2019.00697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mead A. The legal status of cannabis (marijuana) and cannabidiol (CBD) under U.S. law. Epilepsy Behav. 2017;70(Pt B):288–291. doi: 10.1016/j.yebeh.2016.11.021 [DOI] [PubMed] [Google Scholar]
- 17.Hoffmann DE, Weber E. Medical marijuana and the law. N Engl J Med. 2010;362(16):1453–1457. doi: 10.1056/NEJMp1000695 [DOI] [PubMed] [Google Scholar]
- 18.Annas GJ. Medical marijuana, physicians, and state law. N Engl J Med. 2014;371(11):983–985. doi: 10.1056/NEJMp1408965 [DOI] [PubMed] [Google Scholar]
- 19.Conant v Walters, 309 F3d 629 (9th Cir 2002); 2002.
- 20.Testimony of Amy Abernethy, MD, PhD. Hemp production and the 2018 farm bill: hearing before, senate committee on agriculture, nutrition, and forestry; 2019. Available from: https://www.fda.gov/news-events/congressional-testimony/hemp-production-and-2018-farm-bill-07252019. Accessed November 30, 2023.
- 21.The National Academies Collection: Reports funded by National Institutes of Health. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. The National Academies Collection: Reports funded by National Institutes of Health; 2017. [PubMed] [Google Scholar]
- 22.Grbic J, Goddard P, Ryder D. Observations of the role of science in the United States medical cannabis state policies: lessons learnt. Int J Drug Policy. 2017;42:109–114. doi: 10.1016/j.drugpo.2016.12.019 [DOI] [PubMed] [Google Scholar]
- 23.Taylor SL. Evidence-based policy? The re-medicalization of cannabis and the role of expert committees in the UK, 1972-1982. Int J Drug Policy. 2016;37:129–135. doi: 10.1016/j.drugpo.2016.04.014 [DOI] [PubMed] [Google Scholar]
- 24.Pardo B. Cannabis policy reforms in the Americas: a comparative analysis of Colorado, Washington, and Uruguay. Int J Drug Policy. 2014;25(4):727–735. doi: 10.1016/j.drugpo.2014.05.010 [DOI] [PubMed] [Google Scholar]
- 25.Herkenham M, Lynn AB, Little MD, et al. Cannabinoid receptor localization in brain. Proc Natl Acad Sci U S A. 1990;87(5):1932–1936. doi: 10.1073/pnas.87.5.1932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Devinsky O, Cross JH, Laux L, et al. Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl J Med. 2017;376(21):2011–2020. doi: 10.1056/NEJMoa1611618 [DOI] [PubMed] [Google Scholar]
- 27.Ware MA, Wang T, Shapiro S, et al. Cannabis for the Management of Pain: assessment of Safety Study (COMPASS). J Pain. 2015;16(12):1233–1242. doi: 10.1016/j.jpain.2015.07.014 [DOI] [PubMed] [Google Scholar]
- 28.Johnson JR, Lossignol D, Burnell-Nugent M, Fallon MT. An open-label extension study to investigate the long-term safety and tolerability of THC/CBD oromucosal spray and oromucosal THC spray in patients with terminal cancer-related pain refractory to strong opioid analgesics. J Pain Symptom Manage. 2013;46(2):207–218. doi: 10.1016/j.jpainsymman.2012.07.014 [DOI] [PubMed] [Google Scholar]
- 29.Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474–2483. doi: 10.1001/jama.2015.6199 [DOI] [PubMed] [Google Scholar]
- 30.Millar SA, Stone NL, Yates AS, O’Sullivan SE. A systematic review on the pharmacokinetics of cannabidiol in humans. Front Pharmacol. 2018;9:1365. doi: 10.3389/fphar.2018.01365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ujvary I, Hanus L. Human metabolites of cannabidiol: a review on their formation, biological activity, and relevance in therapy. Cannabis Cannabinoid Res. 2016;1(1):90–101. doi: 10.1089/can.2015.0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cooper ZD, Bedi G, Ramesh D, Balter R, Comer SD, Haney M. Impact of co-administration of oxycodone and smoked cannabis on analgesia and abuse liability. Neuropsychopharmacology. 2018;43(10):2046–2055. doi: 10.1038/s41386-018-0011-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pini LA, Guerzoni S, Cainazzo MM, et al. Nabilone for the treatment of medication overuse headache: results of a preliminary double-blind, active-controlled, randomized trial. J Headache Pain. 2012;13(8):677–684. doi: 10.1007/s10194-012-0490-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cuttler C, Spradlin A, Cleveland MJ, Craft RM. Short- and long-term effects of cannabis on headache and migraine. J Pain. 2020;21(5–6):722–730. doi: 10.1016/j.jpain.2019.11.001 [DOI] [PubMed] [Google Scholar]
- 35.Rhyne DN, Anderson SL, Gedde M, Borgelt LM. Effects of medical marijuana on migraine headache frequency in an adult population. Pharmacotherapy. 2016;36(5):505–510. doi: 10.1002/phar.1673 [DOI] [PubMed] [Google Scholar]
- 36.Leroux E, Taifas I, Valade D, Donnet A, Chagnon M, Ducros A. Use of cannabis among 139 cluster headache sufferers. Cephalalgia. 2013;33(3):208–213. doi: 10.1177/0333102412468669 [DOI] [PubMed] [Google Scholar]
- 37.Consroe P, Musty R, Rein J, Tillery W, Pertwee R. The perceived effects of smoked cannabis on patients with multiple sclerosis. Eur Neurol. 1997;38(1):44–48. doi: 10.1159/000112901 [DOI] [PubMed] [Google Scholar]
- 38.Aviram J, Vysotski Y, Berman P, Lewitus GM, Eisenberg E, Meiri D. Migraine frequency decrease following prolonged medical cannabis treatment: a cross-sectional study. Brain Sci. 2020;10(6):360. doi: 10.3390/brainsci10060360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baron EP, Lucas P, Eades J, Hogue O. Patterns of medicinal cannabis use, strain analysis, and substitution effect among patients with migraine, headache, arthritis, and chronic pain in a medicinal cannabis cohort. J Headache Pain. 2018;19(1):37. doi: 10.1186/s10194-018-0862-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang N, Woldeamanuel YW. Medication overuse headache in patients with chronic migraine using cannabis: a case-referent study. Headache. 2021;61(8):1234–1244. doi: 10.1111/head.14195 [DOI] [PubMed] [Google Scholar]
- 41.Stith SS, Diviant JP, Brockelman F, et al. Alleviative effects of Cannabis flower on migraine and headache. J Integr Med. 2020;18(5):416–424. doi: 10.1016/j.joim.2020.07.004 [DOI] [PubMed] [Google Scholar]
- 42.Gibson LP, Hitchcock LN, Bryan AD, Bidwell LC. Experience of migraine, its severity, and perceived efficacy of treatments among cannabis users. Complement Ther Med. 2021;56:102619. doi: 10.1016/j.ctim.2020.102619 [DOI] [PubMed] [Google Scholar]
- 43.Duarte RA, Dahmer S, Sanguinetti SY, Forde G, Duarte DP, Kobak LF. Medical cannabis for headache pain: a primer for clinicians. Curr Pain Headache Rep. 2021;25(10):64. doi: 10.1007/s11916-021-00974-z [DOI] [PubMed] [Google Scholar]
- 44.Bagshaw SM, Hagen NA. Medical efficacy of cannabinoids and marijuana: a comprehensive review of the literature. J Palliat Care. 2002;18(2):111–122. doi: 10.1177/082585970201800207 [DOI] [PubMed] [Google Scholar]
- 45.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11(11):1230–1239. doi: 10.1016/j.jpain.2010.07.002 [DOI] [PubMed] [Google Scholar]
- 46.Stockings E, Campbell G, Hall WD, et al. Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions: a systematic review and meta-analysis of controlled and observational studies. Pain. 2018;159(10):1932–1954. doi: 10.1097/j.pain.0000000000001293 [DOI] [PubMed] [Google Scholar]
- 47.Patti F, Chisari CG, Fernandez O, et al. A real-world evidence study of nabiximols in multiple sclerosis patients with resistant spasticity: analysis in relation to the newly described ‘spasticity-plus syndrome’. Eur J Neurol. 2022;29(9):2744–2753. doi: 10.1111/ene.15412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grossman S, Tan H, Gadiwalla Y. Cannabis and orofacial pain: a systematic review. Br J Oral Maxillofac Surg. 2022;60(5):e677–e690. doi: 10.1016/j.bjoms.2021.06.005 [DOI] [PubMed] [Google Scholar]
- 49.Lynch ME, Ware MA. Cannabinoids for the treatment of chronic non-cancer pain: an updated systematic review of randomized controlled trials. J Neuroimmune Pharmacol. 2015;10(2):293–301. doi: 10.1007/s11481-015-9600-6 [DOI] [PubMed] [Google Scholar]
- 50.Bruera E, Kim HN. Cancer pain. JAMA. 2003;290(18):2476–2479. doi: 10.1001/jama.290.18.2476 [DOI] [PubMed] [Google Scholar]
- 51.Portenoy RK. Treatment of cancer pain. Lancet. 2011;377(9784):2236–2247. doi: 10.1016/S0140-6736(11)60236-5 [DOI] [PubMed] [Google Scholar]
- 52.Kramer JL. Medical marijuana for cancer. CA Cancer J Clin. 2015;65(2):109–122. doi: 10.3322/caac.21260 [DOI] [PubMed] [Google Scholar]
- 53.Pawasarat IM, Schultz EM, Frisby JC, et al. The efficacy of medical marijuana in the treatment of cancer-related pain. J Palliat Med. 2020;23(6):809–816. doi: 10.1089/jpm.2019.0374 [DOI] [PubMed] [Google Scholar]
- 54.National Center for Complementary and Integrative Health. Cannabis (Marijuana) and cannabinoids: what you need to know. Available from: https://www.nccih.nih.gov/health/cannabis-marijuana-and-cannabinoids-what-you-need-to-know. Accessed May 30, 2023.
- 55.Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manage. 2015;34(1):7–31. doi: 10.1002/pam.21804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pergam SA, Woodfield MC, Lee CM, et al. Cannabis use among patients at a comprehensive cancer center in a state with legalized medicinal and recreational use. Cancer. 2017;123(22):4488–4497. doi: 10.1002/cncr.30879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tringale KR, Huynh-Le MP, Salans M, Marshall DC, Shi Y, Hattangadi-Gluth JA. The role of cancer in marijuana and prescription opioid use in the United States: a population-based analysis from 2005 to 2014. Cancer. 2019;125(13):2242–2251. doi: 10.1002/cncr.32059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Swarm RA, Paice JA, Anghelescu DL, et al. Adult cancer pain, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(8):977–1007. doi: 10.6004/jnccn.2019.0038 [DOI] [PubMed] [Google Scholar]
- 59.Portenoy RK, Ahmed E. Principles of opioid use in cancer pain. J Clin Oncol. 2014;32(16):1662–1670. doi: 10.1200/JCO.2013.52.5188 [DOI] [PubMed] [Google Scholar]
- 60.Koyyalagunta D, Bruera E, Solanki DR, et al. A systematic review of randomized trials on the effectiveness of opioids for cancer pain. Pain Physician. 2012;15(3 Suppl):1. [PubMed] [Google Scholar]
- 61.Braun IM, Wright A, Peteet J, et al. Medical oncologists’ beliefs, practices, and knowledge regarding marijuana used therapeutically: a nationally representative survey study. J Clin Oncol. 2018;36(19):1957–1962. doi: 10.1200/JCO.2017.76.1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fallon M, Giusti R, Aielli F, et al. Management of cancer pain in adult patients: ESMO clinical practice guidelines. Ann Oncol. 2018;29(Suppl 4):iv166–iv191. doi: 10.1093/annonc/mdy152 [DOI] [PubMed] [Google Scholar]
- 63.Johnson JR, Burnell-Nugent M, Lossignol D, Ganae-Motan ED, Potts R, Fallon MT. Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC: CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manage. 2010;39(2):167–179. doi: 10.1016/j.jpainsymman.2009.06.008 [DOI] [PubMed] [Google Scholar]
- 64.Portenoy RK, Ganae-Motan ED, Allende S, et al. Nabiximols for opioid-treated cancer patients with poorly-controlled chronic pain: a randomized, placebo-controlled, graded-dose trial. J Pain. 2012;13(5):438–449. doi: 10.1016/j.jpain.2012.01.003 [DOI] [PubMed] [Google Scholar]
- 65.Lynch ME, Cesar-Rittenberg P, Hohmann AG. A double-blind, placebo-controlled, crossover pilot trial with extension using an oral mucosal cannabinoid extract for treatment of chemotherapy-induced neuropathic pain. J Pain Symptom Manage. 2014;47(1):166–173. doi: 10.1016/j.jpainsymman.2013.02.018 [DOI] [PubMed] [Google Scholar]
- 66.Aviram J, Samuelly-Leichtag G. Efficacy of cannabis-based medicines for pain management: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2017;20:6. [PubMed] [Google Scholar]
- 67.Richebe P, Capdevila X, Rivat C. Persistent postsurgical pain: pathophysiology and preventative pharmacologic considerations. Anesthesiology. 2018;129(3):590–607. doi: 10.1097/ALN.0000000000002238 [DOI] [PubMed] [Google Scholar]
- 68.Haroutiunian S, Nikolajsen L, Finnerup NB, Jensen TS. The neuropathic component in persistent postsurgical pain: a systematic literature review. Pain. 2013;154(1):95–102. doi: 10.1016/j.pain.2012.09.010 [DOI] [PubMed] [Google Scholar]
- 69.Niraj G, Rowbotham DJ. Persistent postoperative pain: where are we now? Br J Anaesth. 2011;107(1):25–29. doi: 10.1093/bja/aer116 [DOI] [PubMed] [Google Scholar]
- 70.Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of regional anesthesia and pain medicine, and the American society of anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016;17(2):131–157. doi: 10.1016/j.jpain.2015.12.008 [DOI] [PubMed] [Google Scholar]
- 71.Pogatzki-Zahn E, Lavandhomme P. Prevention of Chronic Post-Surgical Pain. International Association for the Study of Pain. Available from: https://www.iasp-pain.org/resources/fact-sheets/prevention-of-chronic-post-surgical-pain/. Accessed May 30, 2023.
- 72.Adili A, Madden K. Cannabinoids vs. Placebo on persistent post-surgical pain following TKA: a Pilot RCT. ClinicalTrials.gov. Available from: https://clinicaltrials.gov/ct2/show/study/NCT03825965. Accessed November 30, 2023.
- 73.Sarzi-Puttini P, Giorgi V, Marotto D, Atzeni F. Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment. Nat Rev Rheumatol. 2020;16(11):645–660. doi: 10.1038/s41584-020-00506-w [DOI] [PubMed] [Google Scholar]
- 74.Queiroz LP. Worldwide epidemiology of fibromyalgia. Curr Pain Headache Rep. 2013;17(8):356. doi: 10.1007/s11916-013-0356-5 [DOI] [PubMed] [Google Scholar]
- 75.Spaeth M. Epidemiology, costs, and the economic burden of fibromyalgia. Arthritis Res Ther. 2009;11(3):117. doi: 10.1186/ar2715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wolfe F, Clauw DJ, Fitzcharles MA, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3):319–329. doi: 10.1016/j.semarthrit.2016.08.012 [DOI] [PubMed] [Google Scholar]
- 77.Arnold LM, Bennett RM, Crofford LJ, et al. AAPT diagnostic criteria for fibromyalgia. J Pain. 2019;20(6):611–628. doi: 10.1016/j.jpain.2018.10.008 [DOI] [PubMed] [Google Scholar]
- 78.Ware MA, Fitzcharles MA, Joseph L, Shir Y. The effects of nabilone on sleep in fibromyalgia: results of a randomized controlled trial. Anesth Analg. 2010;110(2):604–610. doi: 10.1213/ANE.0b013e3181c76f70 [DOI] [PubMed] [Google Scholar]
- 79.Skrabek RQ, Galimova L, Ethans K, Perry D. Nabilone for the treatment of pain in fibromyalgia. J Pain. 2008;9(2):164–173. doi: 10.1016/j.jpain.2007.09.002 [DOI] [PubMed] [Google Scholar]
- 80.Schley M, Legler A, Skopp G, Schmelz M, Konrad C, Rukwied R. Delta-9-THC based monotherapy in fibromyalgia patients on experimentally induced pain, axon reflex flare, and pain relief. Curr Med Res Opin. 2006;22(7):1269–1276. doi: 10.1185/030079906x112651 [DOI] [PubMed] [Google Scholar]
- 81.Weber J, Schley M, Casutt M, et al. Tetrahydrocannabinol (Delta 9-THC) treatment in chronic central neuropathic pain and fibromyalgia patients: results of a multicenter survey. Anesthesiol Res Pract. 2009;2009. doi: 10.1155/2009/827290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Haanpää M, Treede R-D. Diagnosis and classification of neuropathic pain. Pain Clin Updates. 2010;18(7):1–6. [Google Scholar]
- 83.van Hecke O, Austin SK, Khan RA, Smith BH, Torrance N. Neuropathic pain in the general population: a systematic review of epidemiological studies. Pain. 2014;155(4):654–662. doi: 10.1016/j.pain.2013.11.013 [DOI] [PubMed] [Google Scholar]
- 84.Cavalli E, Mammana S, Nicoletti F, Bramanti P, Mazzon E. The neuropathic pain: an overview of the current treatment and future therapeutic approaches. Int J Immunopathol Pharmacol. 2019;33:2058738419838383. doi: 10.1177/2058738419838383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Maldonado R, Banos JE, Cabanero D. The endocannabinoid system and neuropathic pain. Pain. 2016;157. doi: 10.1097/j.pain.0000000000000428 [DOI] [PubMed] [Google Scholar]
- 86.Abrams DI, Jay CA, Shade SB, et al. Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial. Neurology. 2007;68(7):515–521. doi: 10.1212/01.wnl.0000253187.66183.9c [DOI] [PubMed] [Google Scholar]
- 87.Ellis RJ, Toperoff W, Vaida F, et al. Smoked medicinal cannabis for neuropathic pain in HIV: a randomized, crossover clinical trial. Neuropsychopharmacology. 2009;34(3):672–680. doi: 10.1038/npp.2008.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wallace MS, Marcotte TD, Umlauf A, et al. Efficacy of inhaled cannabis on painful diabetic neuropathy. J Pain. 2015;16(7):616–627. doi: 10.1016/j.jpain.2015.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wilsey B, Marcotte T, Tsodikov A, et al. A randomized, placebo-controlled, crossover trial of cannabis cigarettes in neuropathic pain. J Pain. 2008;9(6):506–521. doi: 10.1016/j.jpain.2007.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]