Abstract
Introduction
Patients in the intensive care unit (ICU) are highly heterogeneous in characteristics, their clinical course, and outcomes. Genetic variability may partly explain the variability and similarity in disease courses observed among critically ill patients and may identify clusters of subgroups. The aim of this study is to conduct a systematic review of all genetic association studies of critically ill patients with their outcomes.
Methods and analysis
This systematic review will be conducted and reported according to the HuGE Review Handbook V1.0. We will search PubMed, Embase, and the Cochrane Library for relevant studies. All types of genetic association studies that included acutely admitted medical and surgical adult ICU patients will be considered for this review. All studies will be selected according to predefined selection criteria, evaluated and assessed for risk of bias independently by two reviewers. Risk of bias will be assessed according to the HuGE Review Handbook V1.0 with some modifications reflecting recent insights. We will provide an overview of all included studies by reporting the characteristics of the study designs, the patients included in the studies, the genetic variables, and the outcomes evaluated.
Ethics and dissemination
We will use data from peer-reviewed published articles, and hence, there is no requirement for ethics approval. The results of this systematic review will be disseminated through publication in a peer-reviewed scientific journal.
Systematic review registration
PROSPERO CRD42021209744.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-023-02401-3.
Keywords: Genetics, Critically ill patients, Intensive care unit, Genome-wide association study, Candidate gene study
Background
Patients with (multiple) organ failure in the hospital are admitted to the intensive care unit (ICU) [1]. These critically ill patients suffer high rates of adverse outcomes resulting in death or, when they survive, often a reduced quality of life [2–4]. The worldwide burden of critical illness is high and is expected to increase with aging populations [4]. Patients admitted to the ICU may have a wide variety of primary diagnoses for which they were initially admitted to the ICU. As a result, the patients in the ICU are highly heterogeneous. In addition, their critical illness may have an unpredictable course with divergent outcomes even when the initial diagnosis is the same. They can either show a quick recovery or they deteriorate with progressive multi-organ failure. Also, patterns of critical illness and (multi)organ failure may show remarkably similar patterns in disease courses, irrespective of the primary underlying disease [5].
In 2001, a draft sequence of the Human Genome became available which resulted in an explosion of studies that identified genetic determinants of diseases [6, 7]. Single-nucleotide polymorphisms (SNPs) are the most commonly occurring type of variant in the genome and also the most frequently studied variants in genetic association studies. The development of a haplotype map based on common genetic variants (i.e., SNPs) in the HapMap project has contributed to the understanding of the patterns of diversity across the human genome [8–10]. It has been shown that genetic variability is able to identify clusters of subgroups among heterogeneous patient groups [11]. Similarly, we hypothesize that genetic variability may partly explain the variability of disease courses observed among critically ill patients. Only observational studies of genetic associations can address this hypothesis.
Genetic association studies fall into two broad categories: candidate gene studies and genome-wide association studies (GWASs) [12]. Candidate gene studies are hypothesis based; genes are selected either by their location in a region of linkage or on the basis of other evidence [12]. While such studies did propose many associations, these were usually not successfully validated in independent cohorts, likely due to small and heterogeneous study samples, random error in exploration studies [13], or insufficient power to detect associations with polymorphisms [14]. The introduction of GWASs facilitated an unbiased survey of common SNPs and hypothesis-free discovery analyses [13]. Although GWASs also have limitations, they represent an important advance for discovery of genetic variants influencing diseases [15].
The discovery of novel genetic loci using hypothesis-free GWAS approaches may help to identify their underlying biology and improve our understanding of common causal pathways in critical illness and (multi)organ failure. However, most genetic association studies and reviews have focused on the evaluation of risk factors within single specific diseases or syndromes in critical care, such as sepsis or acute kidney injury [16–18]. In addition, an overview of all available existing evidence on genetics and a wide range of diseases and/or outcomes that are common in the ICU, such as (multiple) organ failure, sepsis, septic shock, multiple lung diseases, and mortality, is lacking. Therefore, the aim of this study is to conduct a systematic review of all genetic association studies in critically ill patients.
Methods
This systematic review referred to the HuGE Review Handbook V1.0 (guidelines for systematic review and meta-analysis of gene disease association studies) and its updated version that included GWAS to create a quality assessment tool [19, 20]. Several new domains were included in the tool to cover GWAS-related content, bringing it more in line with current insight in genetic research. The protocol will adhere to the PRISMA-P checklist [21].
Selection criteria
Types of studies
All types of genetic association studies will be included. We will include candidate gene studies and GWASs. Articles will be excluded if they do not report original data (e.g., review studies); if they are conference abstracts, case reports/series, and editorials; or if they are not conducted in humans. Association studies of (genome-wide) methylation or gene expression will also be excluded.
Only studies which included adult (≥ 18 years old) critically ill patients admitted to an ICU will be included in this review. Studies that include patients who developed multiple organ failure, heart failure, liver failure, acute kidney injury, renal insufficiency, sepsis, septic shock, acute respiratory distress syndrome, pulmonary edema, acute lung injury, and COVID-19 will all be included. Studies including patients with other diseases than mentioned above (e.g., neurological diseases such as stroke or subarachnoid hemorrhage) will be excluded as the majority of these patients will typically not be admitted to the ICU. Studies in cohorts of patients admitted to the ICU after planned surgery will also be excluded, while studies including patients after acute surgery will be considered for this review.
We will include genetic studies that evaluate the association with mortality, following the definition according to the original authors’ terminology. We will also include the genetic association study if any other patient-relevant outcome measure was reported for the primary analysis in the original study. Genetic studies that evaluate associations with surrogate outcomes or laboratory values, e.g., leucocytes, proteins, or cytokines, will be excluded for evaluation in this review.
Identifying studies
PubMed, Embase, and the Cochrane Library will be searched for relevant studies. The search strategies are listed in Supplementary material 1. All identified publications will be imported into EndNote, and duplicates will be removed. Two reviewers will independently evaluate the titles and abstracts of all the studies generated by the search strategies for eligibility according to predefined selection criteria. At least two reviewers will assess the full-text articles of the preliminary selected publications to see if they meet all inclusion criteria and to extract data. The reference lists of the articles selected will be scrutinized for additional studies. Any disagreements will be resolved through discussion, and if consensus cannot be reached, a third reviewer will be consulted. A database will be created for screening of eligible articles. The number of hits screened, the number of full-text studies retrieved, and the number of excluded studies will be reported using the PRISMA flow chart.
Data collection and analysis
The data of included articles will be extracted and registered in a database in Excel. We will extract the following data from each report: first author, year of publication, country of study, title, study design (candidate gene study/GWAS), type of genetic marker, genotyping method, sample size, gender, age, ethnicity, definition of the disease, and effect sizes such as odds ratios (ORs) [20]. After extraction, the data will be checked by a second reviewer to minimize the risk of transcription errors.
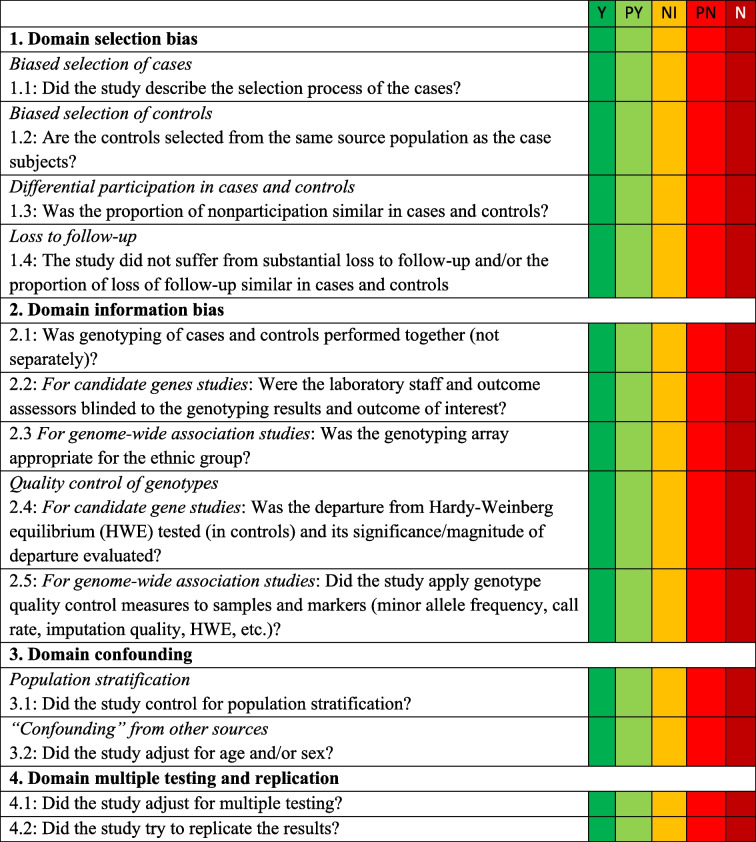
A quality assessment tool based on the HuGE Review Handbook V1.0 and its updated version with GWAS content will be used for assessment of the quality of individual studies [20, 21]. The risk of bias of each study will be assessed by 12 questions representing the following domains: selection bias, information bias, confounding, multiple testing and replication, and Hardy–Weinberg equilibrium. Details of the quality assessment tool are shown in Table 1. Two reviewers will assess the risk of bias of all included papers, independently. Any disagreements will be resolved through discussion, if necessary, including other reviewers. We will consider studies that are classified as low risk of bias in all domains as being at “overall low risk of bias.” Studies with one or more of these domains assessed as “some concerns” or “high risk of bias” will be judged as overall “high risk of bias.”
Table 1.
Risk-of-bias assessment for genetic association studies based on the HuGE Review Handbook V1.0*
Abbreviations: Y yes, PY probably yes, NI no information, PN probably no, N no
*Each domain has signaling questions. Only if answers to all signaling questions within a domain are “yes” or “probably yes,” then the domain will be assessed as “low risk of bias.” If the answers to any of the signaling questions within a domain are “no information,” then the domain will be assessed as “some concerns.” If one or more of the answers to signaling questions within a domain are “probably no” or “no,” then the domain will be assessed as “high risk of bias.” We will consider studies that are assessed as having “low risk of bias” in all domains as being at “overall low risk of bias.” Studies with one or more of these domains assessed as “some concerns” or “high risk of bias” will be judged as being at “overall high risk of bias”
Data synthesis and statistical analysis
A descriptive synthesis will be carried out including the major findings of each study. We will describe the characteristics of the studies designs and the patients included in the studies. Further, we will report the genes observed to be associated with the outcomes, classified according to the study design (candidate gene study or GWAS). We will present a systematic overview of the evidence and interpret and discuss the observations of the included studies.
Discussion
Critical illness leads to a major burden of disease for patients and relatives and generates high costs for hospitals. Such burden of critical illness is higher than generally appreciated and will continue to increase in the future [22]. Critical illness in itself is difficult to define but is characterized by ICU admission due to some degree of organ failure. ICU patients are very heterogeneous reflected by differences in ICU admittance diagnoses, differences in disease courses, and variations in outcomes. Previous genetic studies and reviews in the field of ICU medicine have focused on genetic associations within single specific diseases or syndromes.
In contrast with the wide variation in types of ICU patients, there are remarkable similar patterns of organ failure during critical illness, also across different admitting diagnoses, irrespective of the primary underlying disease. We hypothesize that there may be shared genetic variation associated with the occurrence and severity of organ failure. The present systematic review will be able to give an overview of genetic loci which are associated with some degree of organ failure and will enable easier access to published results by the public and researchers alike. Such results might encourage external validation of earlier findings. These results will help direct choice of genes of interest for future genetic studies on organ failure and/or critically ill patients.
An important potential limitation may be that this systematic review evaluates organ failure in a wide selection of heterogenous critically ill patients with varying admitting diagnoses, which contrasts with typical genetic reviews into genetic loci associated with one specific disease. Due to the large number of outcomes, the results may, therefore, end up in a large list of potential candidate genes and loci each with limited evidence and based on small samples of patients.
A newly developed quality assessment tool will be used to report the risk of bias of the included studies. This tool was based on the HuGE Review Handbook V1.0 with some modifications reflecting recent insights related to GWAS. While meant to improve the assessment of the risk of bias of the included studies, our modified instrument has not been applied previously and may not cover all possible sources of bias.
The quantitative results observed in different studies may be difficult to compare. A formal meta-analysis will likely not be feasible due to the heterogeneity of the study populations and outcomes and the variety in the candidate genes studied. Therefore, this study will likely present a systematic narrative overview of the evidence. If feasible, we will report the results of any meta-analysis only as a hypothesis generating explorative finding.
Supplementary Information
Additional file 1. Search strategy: Pubmed Search Strategy. Embase Search Strategy. Cochrane Library Search Strategy.
Acknowledgements
Not applicable.
Abbreviations
- ICU
Intensive care unit
- SNP
Single-nucleotide polymorphism
- GWAS
Genome-Wide Association Study
- OR
Odds ratio
Authors’ contributions
EC and WZ drafted the manuscript. HS and FK created the idea of the study, wrote significant parts of the manuscript, and contributed substantially to the final version. PV and GL critically reviewed the manuscript. All authors read and approved the final version of this manuscript.
Funding
W. Zhang was financially supported by a grant from the China Scholarship Council (file No. 202006210041). The other researchers received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
The study will use secondary data from peer-reviewed published articles, and hence, there is no requirement for ethics approval. The results of this systematic review will be disseminated through publication in a peer-reviewed scientific journal.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Eline G. M. Cox and Wenbo Zhang contributed equally to this work.
References
- 1.Zador Z, Landry A, Cusimano MD, Geifman N. Multimorbidity states associated with higher mortality rates in organ dysfunction and sepsis: a data-driven analysis in critical care. Crit Care. 2019;23:247. doi: 10.1186/s13054-019-2486-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lone NI, Walsh TS. Impact of intensive care unit organ failures on mortality during the five years after a critical illness. Am J Respir Crit Care Med. 2012;186:640–647. doi: 10.1164/rccm.201201-0059OC. [DOI] [PubMed] [Google Scholar]
- 3.Dinglas VD, Faraone LN, Needham DM. Understanding patient-important outcomes after critical illness: a synthesis of recent qualitative, empirical, and consensus-related studies. Curr Opin Crit Care. 2018;24:401–409. doi: 10.1097/MCC.0000000000000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vincent J-L, Marshall JC, Ñamendys-Silva SA, François B, Martin-Loeches I, Lipman J, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2:380–386. doi: 10.1016/S2213-2600(14)70061-X. [DOI] [PubMed] [Google Scholar]
- 5.Sakr Y, Lobo SM, Moreno RP, Gerlach H, Ranieri VM, Michalopoulos A, et al. Patterns and early evolution of organ failure in the intensive care unit and their relation to outcome. Crit Care. 2012;16:R222. doi: 10.1186/cc11868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lander S, Linton LM, Birren B, Nusbaum C, Zody MC, Baldwin J, et al. Initial sequencing and analysis of the human genome. Nature. 2001;409:860–921. doi: 10.1038/35057062. [DOI] [PubMed] [Google Scholar]
- 7.Lander ES. Initial impact of the sequencing of the human genome. Nature. 2011;470:187–197. doi: 10.1038/nature09792. [DOI] [PubMed] [Google Scholar]
- 8.Risch N, Merikangas K. The future of genetic studies of complex human diseases. Science. 1996;273:1516–1517. doi: 10.1126/science.273.5281.1516. [DOI] [PubMed] [Google Scholar]
- 9.Neale BM, Sham PC. The future of association studies: gene-based analysis and replication. Am J Hum Genet. 2004;75:353–362. doi: 10.1086/423901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Belmont JW, Boudreau A, Leal SM, Hardenbol P, Pasternak S, Wheeler DA, et al. A haplotype map of the human genome. Nature. 2005;437:1299–1320. doi: 10.1038/nature04226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiersema R, Jukarainen S, Vaara ST, Poukkanen M, Lakkisto P, Wong H, et al. Two subphenotypes of septic acute kidney injury are associated with different 90-day mortality and renal recovery. Crit Care. 2020;24:1–10. doi: 10.1186/s13054-020-02866-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hirschhorn JN, Daly MJ. Genome-wide association studies for common diseases and complex traits. Nat Rev Genet. 2005;6:95–108. doi: 10.1038/nrg1521. [DOI] [PubMed] [Google Scholar]
- 13.Ahasic A, Christiani D. Personalized critical care medicine: how far away are we? Semin Respir Crit Care Med. 2015;36:809–822. doi: 10.1055/s-0035-1564852. [DOI] [PubMed] [Google Scholar]
- 14.Clark MF, Baudouin SV. A systematic review of the quality of genetic association studies in human sepsis. Intensive Care Med. 2006;32:1706–1712. doi: 10.1007/s00134-006-0327-y. [DOI] [PubMed] [Google Scholar]
- 15.Pearson TA, Manolio TA. How to interpret a genome-wide association study. JAMA. 2008;299:1335–1344. doi: 10.1001/jama.299.11.1335. [DOI] [PubMed] [Google Scholar]
- 16.Lin MT, Albertson TE. Genomic polymorphisms in sepsis. Crit Care Med. 2004;32:569–579. doi: 10.1097/01.CCM.0000110878.49476.42. [DOI] [PubMed] [Google Scholar]
- 17.Lu JCT, Coca SG, Patel UD, Cantley L, Parikh CR. Searching for genes that matter in acute kidney injury: a systematic review. Clin J Am Soc Nephrol. 2009;4:1020–1031. doi: 10.2215/CJN.05411008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vilander LM, Kaunisto MA, Pettilä V. Genetic predisposition to acute kidney injury – a systematic review. BMC Nephrol. 2015;16:197. doi: 10.1186/s12882-015-0190-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647–g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 20.Sagoo GS, Little J, Higgins JPT. Systematic reviews of genetic association studies. PLoS Med. 2009;6:0239–245. doi: 10.1371/journal.pmed.1000028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Little J, Higgins J, Bray M, Ioannidis J, Khoury M, Manolio T, et al. The HuGENetTM HuGE Review Handbook, version 1.0. Guidelines for systematic review and meta-analysis of gene disease association studies | The EQUATOR Network. https://www.equator-network.org/reporting-guidelines/the-hugenet-huge-review-handbook-version-1-0-guidelines-for-systematic-review-and-meta-analysis-of-gene-disease-association-studies/. Accessed 15 Dec 2020.
- 22.Vincent JL, Marshall JC, Ñamendys-Silva SA, François B, Martin-Loeches I, Lipman J, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014 doi: 10.1016/S2213-2600(14)70061-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy: Pubmed Search Strategy. Embase Search Strategy. Cochrane Library Search Strategy.
Data Availability Statement
Not applicable.