Abstract
The objective of this study was to investigate whether exertional dyspnea correlates with exercise responses, especially arterial blood pH and plasma norepinephrine (NE) changes, in patients with sequelae of tuberculosis (TBsq). Cardiopulmonary exercise testings were performed in 49 TBsq patients and 9 controls. Each group had a break point in the dyspnea, plasma lactate, and plasma NE changes during exercise, all of which occurred at a similar exercise point. In TBsq patients in both exercise phases before and after the dyspnea break point, the dyspnea-slope (∆Borg scale/∆minute ventilation) correlated with the pH-slope (∆pH/∆oxygen uptake) (r = −0.616, p < 0.0001; r = −0.629, p < 0.0001, respectively, before and after the break point) and with the NE-slope (∆NE/∆oxygen uptake) (r = 0.443, p = 0.0012; r = 0.643, p < 0.0001, respectively, before and after the break point). In TBsq patients during exercise, increases in circulating NE levels and exertional acidosis were correlated with exertional dyspnea.
Keywords: Acidosis, Dyspnea, Exercise, Norepinephrine, Sequelae of pulmonary tuberculosis
Introduction
In 2005, an estimated 8.8 million people were infected with tuberculosis and 1.6 million people died of tuberculosis worldwide [1]. In Japan, tuberculosis was one of the most contagious diseases before World War II; after that, the mortality of tuberculosis decreased rapidly over a 2-decade period [2]. During the time when no effective anti-tuberculosis drugs were available, surgical therapy, such as thoracoplasty, was the most effective therapy, and in Japan, 1 million patients with pulmonary tuberculosis underwent chest surgery [3, 4]. Advanced pulmonary tuberculosis, due to delays in its diagnosis and treatment, continues to be a disease that causes a major health burden that can result in residual anatomic and cardiopulmonary changes [4–7], despite developments in anti-tuberculosis therapy [8–12]. In Japan, the sequelae of pulmonary tuberculosis (TBsq) due to complicated TB and/or surgical therapy are related to the cardiopulmonary disorder that frequently occurs and still limits patients’ activities of daily living because of exertional dyspnea. Though there are currently no recommendations for evaluation of cardiopulmonary impairment in TBsq patients [9, 10], a better understanding of the mechanisms and the assessment of dyspnea would help improve our ability to treat and care for TBsq patients.
We have performed cardiopulmonary exercise testing (CPET) on patients with symptoms of dyspnea, including TBsq patients, in our department since 1989 to assess the pathophysiological mechanisms of exertional dyspnea. Although the mechanisms for exertional dyspnea are considered to be multifactorial in respiratory disease patients [13, 14], we previously reported that, in idiopathic pulmonary fibrosis (IPF) patients during exercise, increases in circulating norepinephrine and exercise-induced acidosis due to pulmonary vascular and ventilatory disorders were associated with the intensity of exertional dyspnea [15]. In TBsq patients, however, little is known about the relationships among these parameters.
This study was undertaken to investigate how the intensity of exertional dyspnea contributes to the cardiopulmonary response in TBsq patients, and to test the hypothesis that the intensity of exertional dyspnea may correlate with the change in arterial blood pH and catecholamine levels during exercise in such patients.
Materials and methods
Study subjects
The exercise pathophysiology of 49 patients with TBsq who were referred for evaluation of exertional dyspnea to our department from July 1989 to December 2008 and of 9 healthy volunteers with a similar distribution of age, gender, and anthropometric measurements, was retrospectively investigated (Table 1). The institutional ethics committee approved the study, and, before each CPET session, all patients and control subjects gave written informed consent allowing their CPET data to be used for clinical studies. The inclusion criteria for the study were:
a post-tuberculosis lung disorder (the presence of both a history of pulmonary tuberculosis and a reduced lung volume defined as a vital capacity of 80% of predicted value);
a clinically stable condition (no respiratory infection for at least 4 weeks prior to CPET);
able to tolerate CPET for at least 4 min (i.e., 4 or more measurement points) to ensure adequate evaluation, and exercise limitation caused primarily by exertional dyspnea on CPET, that is, breathing discomfort either alone or in conjunction with leg discomfort at the same level was the primary reason for stopping (see section “Cardiopulmonary exercise testing”); and
absence of any other significant diseases, including neuromuscular diseases, malignancies, cardiac diseases, anemia, and/or peripheral vascular diseases.
Table 1.
Subjects’ baseline characteristics
| Control subjects (n = 9) | TBsq patients (n = 49) | p value | |
|---|---|---|---|
| Gender ratio, M:F | 7:2 | 36:13 | NS |
| Age, years | 67.0 ± 3.4 (52–84) | 67.0 ± 1.4 (30–80) | NS |
| Smoking history, smoker:never | 5:4 | 30:19 | NS |
| BMI, kg m−2 | 20.6 ± 1.0 (16.1–25.7) | 19.2 ± 0.5 (13.1–27.8) | NS |
| Pulmonary function | |||
| VC, L | 3.3 ± 0.3 (1.8–5.0) | 1.7 ± 0.1 (0.7–2.8) | <0.0001 |
| %VC, % | 104.9 ± 6.9 (83.9–142.3) | 54.3 ± 1.9 (29.4–79.2) | <0.0001 |
| FEV1, L | 2.5 ± 0.2 (1.5–3.3) | 1.1 ± 0.1 (0.5–2.1) | <0.0001 |
| FEV1/FVC, % | 81.2 ± 2.6 (71.5–91.7) | 70.7 ± 3.1 (29.4–100.0) | NS |
Values are mean ± standard error of the mean with the range shown in parentheses unless otherwise stated
TBsq sequelae of pulmonary tuberculosis, M male, F female, BMI body mass index, VC vital capacity, FEV1 forced expiratory volume in one-second, FVC forced vital capacity, NS not significant
Twenty-five patients had undergone previously thoracoplasty (10 patients), lobectomy (5 patients), pneumonectomy (5 patients), or artificial pneumothorax (5 patients). The remaining 24 patients had only a severe lung disorder due to a past history of large lung involvement and/or pleuritis. At the time of CPET, no patients were receiving beta blockers, long-term oxygen therapy, or therapy with non-invasive ventilation; 7 patients were receiving digitalis, 2 patients were receiving diuretics, 1 patient was receiving calcium antagonists, and 5 patients were receiving inhaled anticholinergic agents daily. All control subjects were healthy volunteers who were enrolled in another study [15].
Study design
Pulmonary function testing
Pulmonary function testing was done as previously described [16] at the same time as CPET. The results are expressed as percentages of reference values [16].
Cardiopulmonary exercise testing
CPET was performed as previously described [15]. Briefly, while breathing room air with a mask, the patients and the subjects exercised on a treadmill using the Sheffield [17] or one of two modified Sheffield protocols [15]. The protocol was selected after considering the intensity of the subjects’ daily activities and their pulmonary function. CPET was performed until patient exhaustion or the presence of signs indicating that exercise should stop. Expired gas data were collected breath-by-breath using a Vmax 229 (Sensor Medics Corporation, Yorba Linda, CA, USA) and were recorded at 30-s intervals during each stage. Systemic arterial blood samples were drawn through an indwelling radial artery cannula. Pre-exercise resting measurements were done during the steady-state period after at least 3 min of breathing using a mask while sitting. Dyspnea intensity (Borg scale) and arterial blood gases were measured at rest and during the last 15-s at 1 min, at each exercise stage, and at end exercise. Soon after obtaining a sample for arterial blood gas analysis, blood samples for plasma norepinephrine (NE) and plasma lactate (LT) levels were collected and measured as described previously [15]. In addition, the subjects were asked to express their predominant reason for stopping exercise at exhaustion: breathing discomfort, leg discomfort, both, or other reasons.
Data and statistical analysis
Break point
By plotting individual dyspnea- , LT-
, LT- , and NE-
, and NE- curves during exercise, a break point was determined for each subject using the intersection of two lines [15, 18]. To illustrate the relationship between the cardiorespiratory parameters and each percentage of Δoxygen uptake (
curves during exercise, a break point was determined for each subject using the intersection of two lines [15, 18]. To illustrate the relationship between the cardiorespiratory parameters and each percentage of Δoxygen uptake ( ) (=peak
) (=peak  − resting
− resting  ) that occurs during exercise, the values of the parameters at each percentage of
) that occurs during exercise, the values of the parameters at each percentage of  were calculated for each subject by linear interpolation between adjacent measurement points, as previously described [15].
were calculated for each subject by linear interpolation between adjacent measurement points, as previously described [15].
Exercise-response slopes
The exercise-response slopes were calculated as previously described [15]. Briefly, using linear interpolation between adjacent measurement points for each subject, the point corresponding to the dyspnea break point was calculated at which the exercise parameter value, for example the Borg scale or the minute ventilation ( ), corresponded to the
), corresponded to the  value at the dyspnea break point. Next, the dyspnea-slope was calculated for each subject as the ratio of ΔBorg scale to
value at the dyspnea break point. Next, the dyspnea-slope was calculated for each subject as the ratio of ΔBorg scale to  during the early exercise phase (from resting to the point corresponding to the dyspnea break point), or during the late exercise phase (from the point corresponding to the dyspnea break point to the peak exercise point). The other exercise–response slopes (such as the NE-slope), except for the dyspnea-slope, were calculated for each subject as the ratio of Δ exercise parameter (such as NE level) to
during the early exercise phase (from resting to the point corresponding to the dyspnea break point), or during the late exercise phase (from the point corresponding to the dyspnea break point to the peak exercise point). The other exercise–response slopes (such as the NE-slope), except for the dyspnea-slope, were calculated for each subject as the ratio of Δ exercise parameter (such as NE level) to  during the early exercise phase or during the late exercise phase.
during the early exercise phase or during the late exercise phase.
Sample size calculation
The effect size was estimated to be approximately 0.6 by the correlation coefficient values between the dyspnea-slope and other exercise response-slopes during the late exercise phase, which was previously reported for an IPF population [15] but not for TBsq patients. With α = 0.05, β = 0.20, and a two-tailed test of statistical significance, a sample size of at least 19 TBsq patients was calculated on the basis of the effect size for this study [19].
The data are expressed as mean ± SE. Categorical variables were analyzed using Fisher’s exact probability test, and continuous variables were analyzed using the Mann–Whitney test and the Tukey–Kramer test. The statistical significance of the differences due to the interaction of exercise phase and group were determined using repeated-measures ANOVA. Pearson’s correlation coefficients were used to assess the relationships between variables. All analyses were conducted using Statview 5.0 (Abacus Concepts, Berkeley, CA, USA); p values of 0.05 were regarded as significant.
Results
Exercise response
The CPET results are presented in Table 2. The peak oxygen uptake and the peak tidal volume were significantly lower, and the peak physiologic dead space/tidal volume (V D/V T)-ratio and the peak PaCO2 were significantly higher in TBsq patients than in controls. These findings suggest that the TBsq patients had a significantly reduced exercise tolerance with a ventilatory impairment.
Table 2.
Subjects’ exercise responses
| Control subjects (n = 9) | TBsq patients (n = 49) | |||
|---|---|---|---|---|
| Rest | Peak | Rest | Peak | |
 (mL kg−1 min−1) (mL kg−1 min−1) |
4.1 ± 0.3 | 28.2 ± 1.5 | 5.0 ± 0.2* | 16.1 ± 0.7§ |
 (% predicted) (% predicted) |
104.4 ± 7.7 | 58.3 ± 2.2§ | ||
| Dyspnea (borg scale) | 0.1 ± 0.1 | 7.8 ± 0.3 | 0.1 ± 0.1 | 8.5 ± 0.2 |
| HR (beats min−1) | 81 ± 3 | 144 ± 5 | 92 ± 2* | 128 ± 3* |
 /HR (mL beats−1) /HR (mL beats−1) |
2.7 ± 0.2 | 10.4 ± 0.6 | 2.8 ± 0.1 | 6.4 ± 0.3‡ |
| f (beats min−1) | 22 ± 2 | 34 ± 2 | 27 ± 1 | 39 ± 1 |
| VT (mL) | 577 ± 60 | 1611 ± 160 | 517 ± 16 | 829 ± 37§ |
 (L min−1) (L min−1) |
12.2 ± 0.7 | 54.3 ± 4.6 | 13.2 ± 0.4 | 31.3 ± 1.4§ |
| VD/VT-ratio | 0.40 ± 0.03 | 0.22 ± 0.01 | 0.39 ± 0.01 | 0.32 ± 0.01‡ |
| pH | 7.420 ± 0.005 | 7.358 ± 0.009 | 7.407 ± 0.004 | 7.335 ± 0.006 |
| PaO2 (mmHg) | 97.4 ± 3.1 | 84.3 ± 2.7 | 84.4 ± 1.7† | 58.6 ± 1.5§ |
| PaCO2 (mmHg) | 36.5 ± 0.8 | 38.1 ± 0.9 | 43.2 ± 0.9‡ | 49.8 ± 1.1§ |
| LT (mg dl−1) | 10.1 ± 1.3 | 43.8 ± 5.5 | 10.7 ± 0.6 | 25.9 ± 1.5† |
| NE (ng mL−1) | 0.4 ± 0.0 | 2.3 ± 0.5 | 0.9 ± 0.1‡ | 3.5 ± 0.3* |
Values are mean ± standard error of the mean
TBsq sequelae of pulmonary tuberculosis,  oxygen uptake, HR heart rate, f breathing frequency,VT tidal volume,
oxygen uptake, HR heart rate, f breathing frequency,VT tidal volume,  minute ventilation, VD/VT physiologic dead space/tidal volume ratio, PaO2 arterial oxygen tension, PaCO2 arterial carbon dioxide tension, LT plasma lactate level, NE plasma norepinephrine level
minute ventilation, VD/VT physiologic dead space/tidal volume ratio, PaO2 arterial oxygen tension, PaCO2 arterial carbon dioxide tension, LT plasma lactate level, NE plasma norepinephrine level
* p < 0.05, † p < 0.01, ‡ p < 0.001, § p < 0.0001 versus control subjects during each exercise phase
Correlates of exertional dyspnea
First, the changes in the cardiopulmonary parameters were examined in both TBsq patients and controls (Fig. 1). In both groups, there was a break point in the dyspnea-percentage of the  curve with the current exercise protocols (Fig. 1a). In each group, there was a break point in the NE-percentage or the LT-percentage of the
curve with the current exercise protocols (Fig. 1a). In each group, there was a break point in the NE-percentage or the LT-percentage of the  curve during exercise, and these break points occurred at a similar exercise point as the dyspnea break point (Fig. 1a, c, e). There were no differences in the changes in exertional dyspnea, pH, and plasma NE in both groups (Fig. 1a, b, c), although the TBsq patients’ performance was significantly reduced (Table 2).
curve during exercise, and these break points occurred at a similar exercise point as the dyspnea break point (Fig. 1a, c, e). There were no differences in the changes in exertional dyspnea, pH, and plasma NE in both groups (Fig. 1a, b, c), although the TBsq patients’ performance was significantly reduced (Table 2).
Fig. 1.
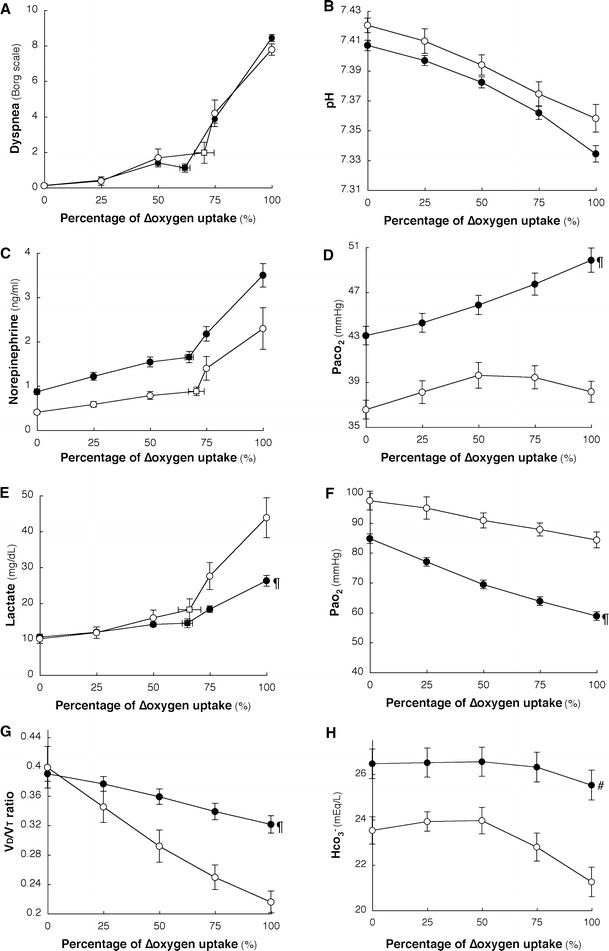
Cardiopulmonary parameter-percentages of the  curve of controls and TBsq patients. Cardiopulmonary responses in control subjects and TBsq patients are shown plotted against the percentage of
curve of controls and TBsq patients. Cardiopulmonary responses in control subjects and TBsq patients are shown plotted against the percentage of  that occurs during exercise.
that occurs during exercise.  , the increment in
, the increment in  between resting and peak exercise; open symbols, control subjects; solid symbols, TBsq patients, V
D/V
T
-ratio physiologic dead space/tidal volume-ratio. Square symbols show the dyspnea, lactate, or norepinephrine-break point, with error bars. In all subjects, both the dyspnea and norepinephrine-break points were determined, but in 9 TBsq patients, it was too difficult to determine the lactate break points reliably. Data are mean ± standard error of the mean. #
p < 0.001, ¶
p < 0.0001; differences due to the interaction of exercise phase and group on repeated-measures ANOVA
between resting and peak exercise; open symbols, control subjects; solid symbols, TBsq patients, V
D/V
T
-ratio physiologic dead space/tidal volume-ratio. Square symbols show the dyspnea, lactate, or norepinephrine-break point, with error bars. In all subjects, both the dyspnea and norepinephrine-break points were determined, but in 9 TBsq patients, it was too difficult to determine the lactate break points reliably. Data are mean ± standard error of the mean. #
p < 0.001, ¶
p < 0.0001; differences due to the interaction of exercise phase and group on repeated-measures ANOVA
Second, the slope of each cardiopulmonary parameter in response to exercise during the early and late exercise phases, and the correlates of the dyspnea-slope in both exercise phases were examined (Table 3). In controls, the NE-slope and the PaCO2-slope were correlated with the dyspnea-slope in the late exercise phase. In TBsq patients, of the cardiopulmonary exercise-response slopes, the pH-slope, the NE-slope, and the PaCO2-slope were well correlated with the dyspnea-slope in both exercise phases; however, the PaO2-slope was not as strongly correlated with the dyspnea-slope as the above parameters. On repeated-measures ANOVA, the PaCO2, the HCO3 −, and the V D/V T-ratio were significantly higher, and the plasma LT level was significantly lower in TBsq patients than in controls during exercise (Fig. 1d, h, g, e). Furthermore, there was no difference in peak pH between the two groups (Table 2). These findings suggest that TBsq patients stopped primarily because of metabolic acidosis followed by a respiratory acidosis caused by pulmonary ventilatory disorders, during which an increasing plasma NE level was detected.
Table 3.
Correlations between the dyspnea-slope before and after the break point in the dyspnea- relationship during exercise
relationship during exercise
| Control subjects (n = 9) | TBsq patients (n = 49) | |||||||
|---|---|---|---|---|---|---|---|---|
| Before the break point | After the break point | Before the break point | After the break point | |||||
| r | p value | r | p value | r | p value | r | p value | |
| pH-slope | 0.528 | NS | −0.095 | NS | −0.616 | <0.0001 | −0.629 | <0.0001 |
| PaO2-slope | 0.093 | NS | −0.025 | NS | −0.328 | 0.0209 | −0.359 | 0.0108 |
| PaCO2-slope | −0.145 | NS | −0.701 | 0.0330 | 0.513 | 0.0001 | 0.583 | <0.0001 |
| LT-slope | −0.479 | NS | 0.270 | NS | 0.542 | <0.0001 | 0.498 | 0.0002 |
| NE-slope | −0.305 | NS | 0.689 | 0.0393 | 0.443 | 0.0012 | 0.643 | <0.0001 |
| HR-slope | −0.090 | NS | −0.177 | NS | 0.363 | 0.0098 | 0.325 | 0.0224 |
| f-slope | 0.014 | NS | −0.129 | NS | 0.188 | NS | 0.099 | NS |
| VT-slope | 0.059 | NS | 0.088 | NS | −0.160 | NS | −0.142 | NS |
The exercise-response slopes were calculated when the parameters were plotted against  from rest to the break point, or from the break point to the peak exercise point using linear regression analysis for each subject
from rest to the break point, or from the break point to the peak exercise point using linear regression analysis for each subject
TBsq, sequelae of pulmonary tuberculosis;  oxygen uptake; the break point, the dyspnea-
oxygen uptake; the break point, the dyspnea- break point determined by each subject; PaO2, arterial oxygen tension; PaCO2, arterial carbon dioxide tension; LT, plasma lactate level; NE, plasma norepinephrine level
break point determined by each subject; PaO2, arterial oxygen tension; PaCO2, arterial carbon dioxide tension; LT, plasma lactate level; NE, plasma norepinephrine level
Dyspnea-slope (∆Borg scale/ ) is expressed as L−1 min, pH-slope (∆pH/
) is expressed as L−1 min, pH-slope (∆pH/ ) as L−1 min, PaO2-slope (∆PaO2/
) as L−1 min, PaO2-slope (∆PaO2/ ) as mmHg L−1 min, PaCO2-slope (∆PaCO2/
) as mmHg L−1 min, PaCO2-slope (∆PaCO2/ ) as mmHg L−1 min, LT-slope (∆LT/
) as mmHg L−1 min, LT-slope (∆LT/ ) as mg dL−1 L−1 min, NE-slope (∆NE/
) as mg dL−1 L−1 min, NE-slope (∆NE/ ) as ng mL−1 L−1 min, HR-slope (∆Heart rate/
) as ng mL−1 L−1 min, HR-slope (∆Heart rate/ ) as beats L−1, f-slope (∆breathing frequency/
) as beats L−1, f-slope (∆breathing frequency/ ) as breaths L−1, V
T-slope (∆tidal volume/
) as breaths L−1, V
T-slope (∆tidal volume/ ) as mL L−1 min
) as mL L−1 min
NS not significant
Discussion
This study demonstrated that, in TBsq patients:
there were break points in the dyspnea, NE, and LT-percentage of the
 curves during exercise, and these break points occurred at a similar exercise point; and
curves during exercise, and these break points occurred at a similar exercise point; andin both exercise phases before and after the dyspnea break point, the dyspnea-slope correlated well with the pH-slope, the NE-slope, and the PaCO2-slope of the cardiopulmonary exercise response-slopes.
These findings suggest that, during exercise, acidosis and the increased plasma NE level were associated with dyspnea in TBsq patients.
In TBsq patients, one of the important systemic respiratory functions during exercise may be to control the exertional acidosis. In this study, compared with controls, TBsq patients during both exercise phases showed higher PaCO2, HCO3 −, and V D/V T-ratio values (Fig. 1d, h, g), and a lower lactate value (Fig. 1e), which suggests that the TBsq patients had a more severe ventilatory impairment than controls. Of note, there was no difference in pH at peak exercise between controls and TBsq patients. Furthermore, during both exercise phases, the pH-slope and the PaCO2-slope were significantly correlated with the dyspnea-slope in TBsq patients, but the PaO2-slope showed a weak relationship with the dyspnea-slope (Table 3). The results of this study are supported by those of a study dealing with the exercise pathophysiology of TBsq patients using non-invasive ventilation and supplemental oxygen during testing; they found that:
O2 alone did not significantly improve exercise tolerance, with only a small reduction in exertional dyspnea compared with the non-invasive ventilation test; and
at peak exercise, higher serum lactate levels, lower PaCO2 levels, and the same pH were found during the non-invasive ventilation test compared with the breathing room air test [20].
These findings suggest that TBsq patients may be unable to compensate for exertional acidosis, which consists of exertional lactic acidosis followed by respiratory acidosis because of their insufficient ventilatory capacities, resulting in stopping exercise to reach a certain pH, though there is variation during exercise in both lactate and PaCO2 levels. This phenomenon of regulating the exertional acidosis may be associated with increasing subjective exertional dyspnea. Similarly, these exercise patterns were observed in IPF patients also [15].
Circulating NE likely plays an important role in the regulation of the cardiorespiratory system in normal subjects [21–25]. Although few studies have examined the effect of the sympathetic nerve response on exertional dyspnea in respiratory disease patients, in normal subjects exposure to hypoxemia [26] and/or hypercapnia [26, 27] during exercise increased sympathetic activity and changed the peripheral chemoreceptor sensitivity, the response of which was linked to an increase in the ventilatory drive [28]. In our study, circulating NE in the TBsq patients had a break point during exercise at a similar exercise point as the dyspnea break point that corresponded to a lactate threshold point, which in turn correlated with the dyspnea-slope. These findings suggest that exertional dyspnea-related circulating NE levels may sensitively identify a significant exertional acidosis in TBsq patients and in IPF patients [15]. We believe that, even if the subjects vary in their diagnoses or ventilatory capacities, there may be common phenomena related to exertional dyspnea. Identification of the phenomena that can explain the mechanism for exertional dyspnea among TBsq patients, IPF patients [15], and controls is of great interest, and the following two points require consideration:
they were similarly unable to regulate the exertional acidosis to stop their exercise through raising the plasma NE level, although there was variation during exercise in both lactate and PaCO2 levels for a given level of mechanical disturbance in the lungs; and
both sympathetic and dyspnea-break points occurred at a lactate threshold point, which may be important in determining the exercise phase.
This study had some limitations. First, the number of subjects was small, especially for control subjects. Therefore, it is difficult to establish a firm conclusion and generalize the findings. Second, the diagnosis of TBsq was not always associated with the same pathophysiological state. Resolution of TBsq results in varying degrees of fibrosis, emphysema, bronchiectasis, and/or thoracic deformity because of chest surgery or pleural changes. Furthermore, pulmonary function tests in this study showed a restrictive pattern or the coexistence of restrictive and obstructive patterns. These findings are currently incompletely characterized. Thus, it is unclear whether our results are related to the variety of structural changes that occur in TBsq patients. Third, our population did not include patients with very severe TBsq who can exercise for only a short period, because we were not able to obtain a sufficient evaluation of their cardiopulmonary function. Thus, it remains unknown whether these results are applicable to very severe cases.
In conclusion, in TBsq patients, assessments of changes in circulating NE levels and in acidosis during exercise may provide important clues to the exercise pathophysiology of exertional dyspnea, and may have clinical implications as an objective marker.
Acknowledgments
The authors would like to thank Mr Minoru Hotta for his help in obtaining the CPET measurements.
Conflict of interest statement
None of the authors have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.World Health Organization (2009) http://www.who.int/mediacentre/factsheets/fs104/en/index.html. Accessed 7 Apr. 2009
- 2.Koizumi K. The revolution of thoracotomy for lung cancer surgery. Ann Thorac Cardiovasc Surg. 2007;13:228–235. [PubMed] [Google Scholar]
- 3.Mori M. Tuberculosis sequelae in Japan. Kekkaku. 1999;74:1–4. [PubMed] [Google Scholar]
- 4.Shneerson JM. Respiratory failure in tuberculosis: a modern perspective. Clin Med. 2004;4:72–76. doi: 10.7861/clinmedicine.4-1-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim MA, Kim SH, Zo JH, Hwangbo B, Lee JH, Chung HS. Right heart dysfunction in post-tuberculosis emphysema. Int J Tuberc Lung Dis. 2004;8:1120–1126. [PubMed] [Google Scholar]
- 6.Pasipanodya JG, Miller TL, Vecino M, Munguia G, Garmon R, Bae S, Drewyer G, Weis SE. Pulmonary impairment after tuberculosis. Chest. 2007;131:1817–1824. doi: 10.1378/chest.06-2949. [DOI] [PubMed] [Google Scholar]
- 7.Phillips MS, Kinnear WJ, Shneerson JM. Late sequelae of pulmonary tuberculosis treated by thoracoplasty. Thorax. 1987;42:445–451. doi: 10.1136/thx.42.6.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jager L, Franklin KA, Midgren B, Lofdahl K, Strom K. Increased survival with mechanical ventilation in posttuberculosis patients with the combination of respiratory failure and chest wall deformity. Chest. 2008;133:156–160. doi: 10.1378/chest.07-1522. [DOI] [PubMed] [Google Scholar]
- 9.(2003) Treatment of tuberculosis. MMWR Recomm Rep 52:1–77 [PubMed]
- 10.Taylor Z, Nolan CM, Blumberg HM. Controlling tuberculosis in the United States. Recommendations from the American Thoracic Society, CDC, and the Infectious Diseases Society of America. MMWR Recomm Rep. 2005;54:1–81. [PubMed] [Google Scholar]
- 11.Leger P, Bedicam JM, Cornette A, Reybet-Degat O, Langevin B, Polu JM, Jeannin L, Robert D. Nasal intermittent positive pressure ventilation. Long-term follow-up in patients with severe chronic respiratory insufficiency. Chest. 1994;105:100–105. doi: 10.1378/chest.105.1.100. [DOI] [PubMed] [Google Scholar]
- 12.Chan ED, Iseman MD. Current medical treatment for tuberculosis. Br Med J. 2002;325:1282–1286. doi: 10.1136/bmj.325.7375.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.(1999) Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Respir Crit Care Med 159:321–340 [DOI] [PubMed]
- 14.Manning HL, Schwartzstein RM. Pathophysiology of dyspnea. N Engl J Med. 1995;333:1547–1553. doi: 10.1056/NEJM199512073332307. [DOI] [PubMed] [Google Scholar]
- 15.Miki K, Maekura R, Hiraga T, Hashimoto H, Kitada S, Miki M, Yoshimura K, Tateishi Y, Fushitani K, Motone M. Acidosis and raised norepinephrine levels are associated with exercise dyspnoea in idiopathic pulmonary fibrosis. Respirology. 2009;14:1020–1026. doi: 10.1111/j.1440-1843.2009.01607.x. [DOI] [PubMed] [Google Scholar]
- 16.Hiraga T, Maekura R, Okuda Y, Okamoto T, Hirotani A, Kitada S, Yoshimura K, Yokota S, Ito M, Ogura T. Prognostic predictors for survival in patients with COPD using cardiopulmonary exercise testing. Clin Physiol Funct Imaging. 2003;23:324–331. doi: 10.1046/j.1475-0961.2003.00514.x. [DOI] [PubMed] [Google Scholar]
- 17.Sheffield LT. Graded exercise test (GRX) for ischemic heart disease. In: AHA Committee on Exercise, editor. A handbook for physicians. Dallas: Am Heart Association; 1972. pp. 35–38. [Google Scholar]
- 18.O’Donnell DE, Hamilton AL, Webb KA. Sensory-mechanical relationships during high-intensity, constant-work-rate exercise in COPD. J Appl Physiol. 2006;101:1025–1035. doi: 10.1152/japplphysiol.01470.2005. [DOI] [PubMed] [Google Scholar]
- 19.Machin D, Campbell MJ, Tan SB, SH T. Sample size tables for clinical studies. 3. UK: Wiley-Blackwell; 2008. [Google Scholar]
- 20.Tsuboi T, Ohi M, Chin K, Hirata H, Otsuka N, Kita H, Kuno K. Ventilatory support during exercise in patients with pulmonary tuberculosis sequelae. Chest. 1997;112:1000–1007. doi: 10.1378/chest.112.4.1000. [DOI] [PubMed] [Google Scholar]
- 21.Ekblom B, Goldbarg AN, Kilbom A, Astrand PO. Effects of atropine and propranolol on the oxygen transport system during exercise in man. Scand J Clin Lab Invest. 1972;30:35–42. doi: 10.3109/00365517209081087. [DOI] [PubMed] [Google Scholar]
- 22.Heistad DD, Wheeler RC, Mark AL, Schmid PG, Abboud FM. Effects of adrenergic stimulation on ventilation in man. J Clin Invest. 1972;51:1469–1475. doi: 10.1172/JCI106943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Butland RJ, Pang JA, Geddes DM. The selectivity of the beta-adrenoceptor for ventilation in man. Br J Clin Pharmacol. 1982;14:707–711. doi: 10.1111/j.1365-2125.1982.tb04961.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rowell LB, O’Leary DS. Reflex control of the circulation during exercise: chemoreflexes and mechanoreflexes. J Appl Physiol. 1990;69:407–418. doi: 10.1152/jappl.1990.69.2.407. [DOI] [PubMed] [Google Scholar]
- 25.Clark AL, Galloway S, MacFarlane N, Henderson E, Aitchison T, McMurray JJ. Catecholamines contribute to exertional dyspnoea and to the ventilatory response to exercise in normal humans. Eur Heart J. 1997;18:1829–1833. doi: 10.1093/oxfordjournals.eurheartj.a015179. [DOI] [PubMed] [Google Scholar]
- 26.Somers VK, Mark AL, Zavala DC, Abboud FM. Influence of ventilation and hypocapnia on sympathetic nerve responses to hypoxia in normal humans. J Appl Physiol. 1989;67:2095–2100. doi: 10.1152/jappl.1989.67.5.2095. [DOI] [PubMed] [Google Scholar]
- 27.Ehrsam RE, Heigenhauser GJ, Jones NL. Effect of respiratory acidosis on metabolism in exercise. J Appl Physiol. 1982;53:63–69. doi: 10.1152/jappl.1982.53.1.63. [DOI] [PubMed] [Google Scholar]
- 28.Weil JV, Byrne-Quinn E, Sodal IE, Kline JS, McCullough RE, Filley GF. Augmentation of chemosensitivity during mild exercise in normal man. J Appl Physiol. 1972;33:813–819. doi: 10.1152/jappl.1972.33.6.813. [DOI] [PubMed] [Google Scholar]


