Abstract
Background
The prevalence of metabolic dysfunction-associated fatty liver disease (MAFLD) has been rising rapidly in western China. Diet acts as an effective therapy for MAFLD. However, there has been scarce research on the association between a posteriori diet patterns (DPs) and MAFLD in this region.
Method
We identified three a posteriori DPs which were “Sichuan Basin pattern” characterized by a high intake of fish/seafood, poultry, fresh fruit and vegetables, indicating a balanced and modern DP; the “Yunnan–Guizhou Plateau dietary pattern” characterized mainly by a high intake of animal oil and salt, indicating an agricultural and poor DP; and the “Qinghai–Tibet Plateau dietary pattern” characterized by a high intake of coarse grains, wheat products, tubers and tea, respectively, indicating a high-altitude DP. Then, we performed marginal structural models that combined logistic regression and inverse probability exposure weighting (IPEW) to examine the associations between MAFLD and these a posteriori DPs.
Result
We found the “Yunnan–Guizhou Plateau dietary pattern” revealed stronger positive association (OR = 1.50, 95% CI 1.40–1.60) with MAFLD than that of the “Qinghai–Tibet Plateau dietary pattern” (OR = 1.21, 95% CI 1.14–1.30). In contrast, the “Sichuan Basin dietary pattern” showed no significant association with MAFLD. In the further stratified analysis, we found those above associations were stronger in ethnic minorities and rural residents than their counterparts.
Conclusion
Our study implied the unfavourable effects of “Yunnan–Guizhou Plateau dietary pattern” on MAFLD and provided evidence that reducing the intake of oil and sodium may be optimal for MAFLD control in the multi-ethnic region in western China.
Supplementary Information
The online version contains supplementary material available at 10.1186/s41043-023-00485-0.
Keywords: MAFLD, Dietary pattern, Multi-ethnic, West China, Metabolic dysfunction
Introduction
Metabolic dysfunction-associated fatty liver disease (MAFLD), formerly named non-alcoholic fatty liver disease (NAFLD), has emerged as the most common cause of chronic liver disease, affecting over one quarter of the population worldwide [1, 2]. In China, the prevalence of MAFLD is reported to be 29.2% [3], mainly due to sharp changes in lifestyle and diet [4]. In western China, where the majority of ethnic minorities live, the prevalence of MAFLD ranges from 21.8 to 26.1% [5, 6]. Of note, during the last decade, the prevalence of MAFLD in this region has doubled according to previous studies [6, 7].
Despite the alarming data, currently there is no pharmacotherapy available for MAFLD. Diet is the main driver of hepatic triglyceride accumulation [8] and thus may act as an effective therapy for MAFLD prevention and treatment [9, 10]. Considerable research has placed interest on the relationship between diet and MAFLD, but most of these studies have focused on either nutrients or some a priori dietary patterns [11, 12]. Single food or nutrient studies were not able to take complex combinations of foods into account [13]. While a priori dietary patterns, such as the Mediterranean diet (MED), Healthy Eating Index (HEI) and Dietary Approaches to Stop Hypertension (DASH) [14–17], have all been developed based on Western-like diets from developed countries, they may be not suitable for the multi-ethnic region in western China. A posteriori dietary patterns can represent the actual dietary habits of different regions, which could better provide insights into optimal dietary advices [18]. However, the effects of a posteriori dietary patterns on MAFLD in the multi-ethnic region in western China remains unclear.
To the best of our knowledge, there are no available evidence on the association between a posteriori dietary patterns and MAFLD in western China, although clear knowledge of this is critical for policy-making regarding MAFLD prevention [19]. The China Multi-Ethnic Cohort (CMEC) is a large-scale epidemiological study which has recruited nearly 0.1 million participants in western China with huge diversity in socioeconomic status, ethnicity, etc. [20]. In this context, the CMEC study provides a unique opportunity to shed light on the above research gap. Therefore, in this present work we aimed to examine the associations between a posteriori DPs and MAFLD in the multi-ethnic region in western China.
Materials and methods
Study population
The present work is based on the baseline data of the China Multi-Ethnic Cohort (CMEC) study, and detailed information about the CMEC has been described elsewhere [20]. Briefly, a total of 99,556 participants were recruited from May 2018 to September 2019 in the multi-ethnic region in western China. For every participant, data on demographics, behaviours and diet were recorded face-to-face by trained staff via an electronic questionnaire. Blood, urine and X-ray tests were also conducted. This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the local ethics committee and the Sichuan University Medical Ethical Review Board [ID: K2016038] and all participants provided informed consent.
For the current analysis, we focused on participants between the ages of 30–79 years. We excluded participants whose total energy intake was extreme (N = 2433) (for males: < 800 or > 4200 kcal/day; for females: < 600 or > 3500 kcal/day), as well as those with an implausible body mass index (BMI)(N = 172) (< 14 or > 45 kg/m2). Participants with no available information on diet or outcome were also excluded (N = 4656). Furthermore, to capture a more reasonable causal effect and eliminate potential reverse causality, participants with self-reported chronic hepatitis/cirrhosis, coronary heart disease, stroke, hypertension, hyperlipidaemia, diabetes or cancer diagnosed by physicians were excluded as well. The final study sample consisted of 66,377 participants. Details are provided in Additional file 1: Figure 1.
Assessment of dietary intake and dietary patterns
Dietary intake information was assessed via a validated quantitative food frequency questionnaire (FFQ) [21]. The FFQ mainly includes 13 food groups (include rice, wheat products, coarse grain, tubers, red and processed meats, poultry, fish/seafood, eggs, fresh vegetables, soybean products, preserved vegetables, fresh fruits and dairy products). Participants were interviewed to recall the quantity (average number of grams per meal) and frequency (how many times per day, week, year) of each food group during the last 12 months. Information about alcohol, tea and soft drink consumption was also collected. The validity and reproducibility were accessed by performing 24-h dietary recall (1113 participants) and repeated FFQ (7516 participants), respectively. We used intraclass correlation coefficients to access the reproducibility, which ranged from 0.15 for fresh vegetables to 0.67 for alcohol. We used de-attenuated Spearman rank correlation coefficients to assess the validity, which ranged from 0.10 for soybean products to 0.66 for rice. More details could be found in our previous work [21].
A posteriori dietary patterns were identified by performing principal component factor analysis (PCFA) via varimax rotation [22]. In consideration of eigenvalues, variance explained, scree plot and interpretability, three patterns were finally obtained. Food groups with absolute factor loadings ≥ 0.35 were considered to contribute to the corresponding factor. For each dietary pattern, factor scores were assigned to participants by summing the standardized intake of each food group weighed by factor loadings. A higher score means a higher adherence to the corresponding dietary pattern.
Assessment of outcome
We used the criteria for MAFLD that were recently proposed by a panel of international experts from 22 countries [1]. The criteria were based on hepatic steatosis detected by either imaging, biomarkers or liver histology plus one of the following three conditions: overweight/obesity, type 2 diabetes mellitus or the presence of metabolic dysregulation. Overweight/obesity was defined as BMI ≥ 23 kg/m2 (criterion for Asians). Metabolic dysregulation was defined as the presence of at least two of the following conditions: (1) waist circumference ≥ 90/80 cm in men/women; (2) blood pressure ≥ 130/85 mmHg; (3) plasma triglycerides (TG) ≥ 1.7 mmol/L; (4) plasma high-density lipoprotein cholesterol (HDL-C) < 1.0/1.3 mmol/L for men/women; and (5) prediabetes (fasting plasma glucose within 5.6–6.9 mmol/L or haemoglobin A1c within 5.7–6.4%). Notably, in this analysis, we removed the insulinemia test and the high-sensitivity C-reactive protein (hs-CRP) test from the original criteria, because they were not collected in our baseline survey.
Assessment of covariates
To obtain potential confounders, a directed acyclic graph was constructed according to the protocol of “Evidence Synthesis for Constructing Directed Acyclic Graphs” (ESC-DAGs) [23]. Guided by the DAG, we adjusted for the following covariates in our final models, including gender, age, ethnicity, urbanicity, marital status, education level, income, occupation, smoking status, alcohol use, physical activity (metabolic equivalent tasks), total energy intake (kcal/day), menopause status, family history of cardiovascular diseases (CVD) and insomnia status. See more details in Additional file 1: Figure 2.
Statistical analysis
The baseline characteristics of participants were presented according to MAFLD status (with/without), as well as according to quintiles of each DP. (Quintile 1 represents lowest adherence, and quintile 5 represents highest adherence.) Continuous variables were presented as mean and standard deviation. Categorical variables were presented as number and percentages. Analysis of variance (ANOVA) was used to describe mean difference for continuous variables, and Chi-squared test was used to examine proportion difference for categorical variables.
To examine the associations of DPs and MAFLD, marginal structural models that combined logistic regression and inverse probability exposure weighting (IPEW) were used [24]. The entropy balancing weighting method was adopted due to the preferable performance of covariate balances [25] (see Additional file 1: Figure 3). The DP scores were modelled as categorical variables with five levels, with the lowest level (first quantile) as the reference group. Multiple imputation was conducted for missing food group values (with 5 imputations).
Furthermore, we conducted stratification analyses to detect potential effect modifiers among subgroups, including age, gender, urbanicity, ethnicity and income level. Sensitivity analyses were conducted to assess the robustness of our findings. First, we repeated our analyses with traditional logistic regression adjusting for the same covariates. Second, we redefined the outcome based on the NAFLD criteria. Third, participants with self-reported chronic hepatitis/cirrhosis, coronary heart disease, stroke, hypertension, hyperlipidaemia, diabetes or cancer diagnosed by physicians were included in the analysis. Fourth, we conducted an analysis based on complete cases instead of the imputation data.
All analyses were performed with R Project for Statistical Computing version 4.1.1.
Results
Characteristics of dietary patterns
Three a posteriori dietary patterns were identified using PCFA, and detailed information is presented in Table 1. Overall, these three DPs were highly geography-related. The first DP, named “Sichuan Basin dietary pattern”, was predominant among participants in the Sichuan Basin and was characterized by a high intake of fish/seafood, poultry, fresh fruits and vegetables, eggs, dairy products and vegetable oil with relative low intake of animal oil, salt indicating a more balanced DP. The second DP, named “Yunnan–Guizhou Plateau dietary pattern”, was predominant among participants in the Yunnan–Guizhou Plateau and was characterized mainly by a high intake of animal oil, rice, salt, preserved vegetables and alcohol, with low intake of dairy products, coarse grains, vegetable oil, fresh fruit and eggs. The third DP, named “Qinghai–Tibet Plateau dietary pattern”, was predominant among participants in the Qinghai–Tibet Plateau and was mainly representative of a high intake of coarse grains, wheat products, tubers, tea, potatoes and legumes with low intake of animal oil, salt, fresh vegetables and fish/sea food. In total, these three a posteriori DPs explained 28.5% of the variance in dietary intake.
Table 1.
Rotated factor-loading matrix for the three dietary patterns
| Food groups | Dietary pattern | ||
|---|---|---|---|
| Sichuan Basin | Yunnan–Guizhou Plateau | Qinghai–Tibet Plateau | |
| Animal oil | − 0.24 | 0.61 | − 0.12 |
| Rice | 0.07 | 0.53 | 0.00 |
| Salt | − 0.03 | 0.35 | − 0.13 |
| Preserved vegetables | 0.07 | 0.35 | 0.22 |
| Alcohol | 0.11 | 0.30 | 0.11 |
| Legumes | 0.23 | 0.26 | 0.23 |
| Fresh vegetables | 0.43 | 0.25 | − 0.06 |
| Fish/seafood | 0.60 | 0.19 | − 0.03 |
| Red meat (includes processed) | 0.24 | 0.18 | 0.22 |
| Potatoes | 0.13 | 0.17 | 0.54 |
| Poultry | 0.56 | 0.16 | 0.08 |
| Tea | − 0.06 | 0.01 | 0.52 |
| Wheat products | − 0.05 | − 0.03 | 0.64 |
| Fresh fruits | 0.49 | − 0.07 | 0.02 |
| Eggs | 0.52 | − 0.07 | 0.08 |
| Vegetable oil | 0.36 | − 0.10 | − 0.04 |
| Coarse grains | 0.02 | − 0.29 | 0.65 |
| Dairy products | 0.50 | − 0.44 | 0.07 |
| Variance explained (%) | 10.9 | 9.0 | 8.6 |
Characteristics of study population
Overall, there were 10,706 participants with MAFLD out of the 66,377 total participants, and the prevalence in our study population was 16.13%. The demographic, anthropometric characteristics of the participants with and without MAFLD are presented in Table 2. Generally, there were significant difference in gender, ethnicity, region, physical activity, obesity, alcohol intake, smoking status, education level and annual income between subjects with and without MAFLD. Subjects with MAFLD were more likely to be female and Han majority, majority of subjects live in rural area, and they tended to have lower physical activity levels and higher WC as well as BMI; furthermore, they also tend to have higher alcohol consumption.
Table 2.
Comparison of the characteristics of participants with and without MAFLD
| Variables | Without MAFLD n = 5 5613 |
With MAFLD n = 10 706 |
P value |
|---|---|---|---|
| Age (years) | 49.45 (11.11) | 49.59 (10.23) | 0.215 |
| Gender (%) | < 0.001 | ||
| Male | 19 728 (35.5) | 5145 (48.1) | |
| Female | 35 885 (64.5) | 5561 (51.9) | |
| Ethnicity (%) | < 0.001 | ||
| Han majority | 31 836 (57.2) | 6535 (61.0) | |
| Ethnic minority | 23 777 (42.8) | 4171 (39.0) | |
| Region (%) | < 0.001 | ||
| Urban | 18 288 (32.9) | 4781 (44.7) | |
| Rural | 37 325 (67.1) | 5925 (55.3) | |
| Physical activity (METs-h/day)a | 27.90 (18.44) | 24.92 (17.36) | < 0.001 |
| Central obesityb (%) | < 0.001 | ||
| Yes | 11,831 (21.3) | 6969 (65.2) | |
| No | 43,645 (78.7) | 3721 (34.8) | |
| BMI (kg/m2) | 23.17 (3.02) | 27.13 (3.08) | < 0.001 |
| Alcohol intakec (%) | < 0.001 | ||
| Heavy | 3357 (6.0) | 806 (7.5) | |
| Light | 52,256 (94.0) | 9900 (92.5) | |
| Education level (%) | < 0.001 | ||
| No formal school | 14 120 (25.4) | 2488 (23.2) | |
| Primary school | 13 835 (24.9) | 2641 (24.7) | |
| Middle and high school | 21 061 (37.9) | 4180 (39.0) | |
| College or university | 6596 (11.9) | 1397 (13.0) | |
| Annual income (%) | < 0.001 | ||
| < ¥12,000 | 9230 (16.6) | 1537 (14.4) | |
| ¥12,000–19999 | 10 178 (18.3) | 1839 (17.2) | |
| ¥20,000–59999 | 20 606 (37.1) | 3851 (36.0) | |
| ¥60,000–99999 | 8061 (14.5) | 1706 (15.9) | |
| ¥100,000–199,999 | 5979 (10.8) | 1386 (13.0) | |
| > ¥200,000 | 1486 (2.7) | 377 (3.5) | |
| Smoking status (%) | < 0.001 | ||
| Never | 42 999 (77.3) | 7666 (71.6) | |
| Previous | 10 554 (19.0) | 2471 (23.1) | |
| Current | 2060 (3.7) | 569 (5.3) |
BMI body mass index
aMETs-h/day: hours of metabolic equivalent tasks per day
bCentral obesity was defined as waist circumference ≥ 90 cm in men or ≥ 80 cm in women
cHeavy alcohol intake was defined as ≥ 140 g/week for men and ≥ 70 g/week for women
The characteristics of participants across quintiles of each DP score are shown in Table 3. Overall, participants in the highest quantile of the Sichuan Basin dietary pattern were more likely to be female, younger, Han majority, urban residents and non-smoker, they also tend to have higher education level and income level, and they were less likely to have central obesity. Contrast to participants in the bottom quantile, participants in the highest quantile of the Yunnan–Guizhou dietary pattern were more likely to be male, older, ethnic minority, rural residents, they tend to have lower education level and income level, most of them are married and have a habit of heavy drink, and they also are less likely to have central obesity and to be a smoker. Characteristics of participants in highest quantile of Qinghai–Tibet Plateau dietary pattern are similar as those in highest quantile of Yunnan–Kweichow Plateau pattern, they were more likely to be male, older, ethnic minority, rural residents, they tend to have lower education level and income level, and they also tend to have lower education level and income level.
Table 3.
Characteristic of participants across quintiles of dietary pattern scores
| Sichuan Basin | * | Yunnan–Kweichow Plateau | * | Qinghai–Tibet Plateau | * | ||||
|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q5 | Q1 | Q5 | Q1 | Q5 | ||||
| Age | 51.67 (11.08) | 47.69 (10.73) | 47.55 (11.44) | 51.40 (10.11) | 49.54 (10.86) | 50.13 (10.98) | |||
| Male sex (%) | 4470 (33.7) | 5662 (42.6) | 3279 (24.7) | 7022 (52.9) | 3316 (25.0) | 6611 (49.8) | |||
| Han majority (%) | 3763 (28.3) | 11,311 (85.2) | 8627 (65.0) | 7347 (55.3) | 6362 (47.9) | 6766 (51.0) | |||
| Rural residents (%) | 11,572 (87.2) | 5295 (39.9) | 6332 (47.7) | 10,605 (79.9) | 9221 (69.5) | 9399 (70.8) | |||
| Physical activity (METs-h/day)a | 29.56 (20.03) | 24.43 (15.74) | 21.24 (14.84) | 30.18 (19.01) | 28.41 (18.43) | 26.51 (18.55) | |||
| With central obesityb (%) | 4198 (31.7) | 3413 (25.8) | 3905 (29.5) | 3378 (25.5) | 3331 (25.1) | 4857 (36.7) | |||
| Education level | |||||||||
| No formal school | 6050 (45.6) | 1131 (8.5) | 3124 (23.5) | 3583 (27.0) | 3990 (30.1) | 4154 (31.3) | |||
| Primary school | 4059 (30.6) | 2301 (17.3) | 2083 (15.7) | 4619 (34.8) | 3227 (24.3) | 3661 (27.6) | |||
| Middle and high school | 2776 (20.9) | 7010 (52.8) | 5130 (38.6) | 4582 (34.5) | 4597 (34.6) | 4296 (32.4) | |||
| University | 390 (2.9) | 2834 (21.3) | 2939 (22.1) | 492 (3.7) | 1462 (11.0) | 1165 (8.8) | |||
| Annual income (%) | |||||||||
| < ¥12,000 | 3722 (28.1) | 1043 (7.9) | 1391 (10.5) | 2876 (21.7) | 2860 (21.6) | 2013 (15.2) | |||
| ¥12,000–19999 | 3253 (24.5) | 1508 (11.4) | 2039 (15.4) | 2783 (21.0) | 2573 (19.4) | 2721 (20.5) | |||
| ¥20,000–59999 | 4718 (35.6) | 4570 (34.5) | 4585 (34.6) | 5290 (39.9) | 4566 (34.4) | 5145 (38.8) | |||
| ¥60,000–99999 | 1018 (7.7) | 2857 (21.6) | 2447 (18.5) | 1339 (10.1) | 1732 (13.1) | 1767 (13.3) | |||
| ¥100,000–199999 | 454 (3.4) | 2475 (18.7) | 2110 (15.9) | 790 (6.0) | 1281 (9.7) | 1233 (9.3) | |||
| > ¥200,000 | 99 (0.7) | 801 (6.0) | 683 (5.2) | 179 (1.4) | 246 (1.9) | 383 (2.9) | |||
| Occupation (%) | |||||||||
| Primary industry | 7280 (54.9) | 2014 (15.2) | 2411 (18.2) | 7471 (56.3) | 5177 (39.0) | 5016 (37.8) | |||
| Secondary industry | 659 (5.0) | 1310 (9.9) | 774 (5.8) | 1145 (8.6) | 1075 (8.1) | 796 (6.0) | |||
| Tertiary industry | 3818 (28.8) | 6407 (48.3) | 6722 (50.7) | 3099 (23.3) | 5099 (38.4) | 4662 (35.1) | |||
| Unemployed | 1508 (11.4) | 3534 (26.6) | 3359 (25.3) | 1557 (11.7) | 1912 (14.4) | 2794 (21.1) | |||
| Smoking status (%) | |||||||||
| Never | 10,623 (80.0) | 9638 (72.6) | 11,617 (87.5) | 8248 (62.1) | 11,301 (85.1) | 9018 (67.9) | |||
| Previous | 2268 (17.1) | 2946 (22.2) | 1292 (9.7) | 4337 (32.7) | 1651 (12.4) | 3526 (26.6) | |||
| Current | 385 (2.9) | 692 (5.2) | 367 (2.8) | 691 (5.2) | 324 (2.4) | 732 (5.5) | |||
| Without family history of CVDc (%) | 10,486 (79.0) | 7975 (60.1) | 8576 (64.6) | 9668 (72.8) | 9395 (70.8) | 9459 (71.2) | |||
| Menopaused (%) | |||||||||
| Premenopause | 3814 (28.7) | 4667 (35.2) | 5992 (45.1) | 2906 (21.9) | 5077 (38.2) | 3506 (26.4) | |||
| Perimenopause | 602 (4.5) | 537 (4.0) | 647 (4.9) | 465 (3.5) | 734 (5.5) | 432 (3.3) | |||
| Post-menopause | 4389 (33.1) | 2410 (18.2) | 3357 (25.3) | 2883 (21.7) | 4149 (31.3) | 2726 (20.5) | |||
| Without insomnia | 7238 (54.7) | 7917 (59.9) | 7988 (60.4) | 7641 (58.0) | 7234 (54.7) | 7938 (60.1) | |||
| Energy intake (Kcal/day) | 10,775.52 (3,871.93) | 15,921.89 (4,445.82) | 11,860.37 (4,085.58) | 16,475.08 (4,451.20) | 10,953.17 (3,762.20) | 16,410.08 (4,613.38) | |||
| Heavy alcohol intake e (%) | 489 (3.7) | 1250 (9.4) | 98 (0.7) | 2397 (18.1) | 248 (1.9) | 1333 (10.0) | |||
| Married or cohabit (%) | 11,676 (87.9) | 11,962 (90.1) | 11,755 (88.5) | 11,998 (90.4) | 11,672 (87.9) | 12,091 (91.1) | |||
CVD cardiovascular disease
Q: represent the quintile of dietary pattern score
*All p values are < 0.05
aMETs-h/day: hours of metabolic equivalent tasks per day
Dietary pattern and MAFLD
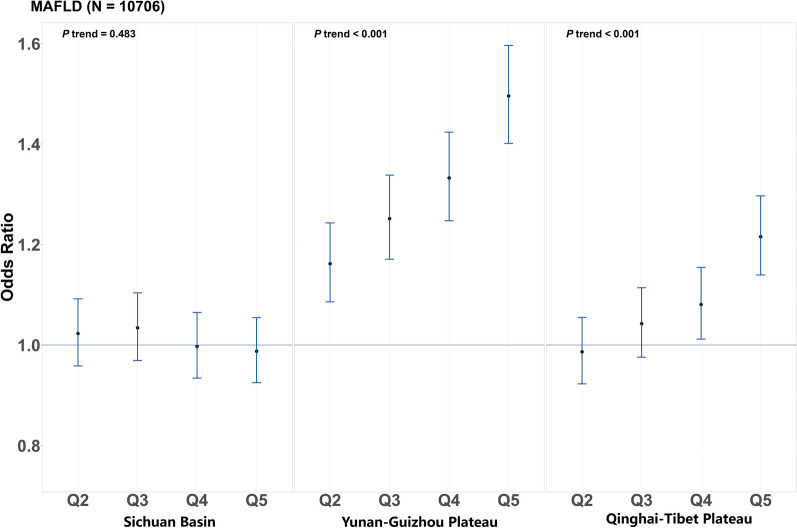
Figure 1 presents the associations between a posteriori DPs and MAFLD after adjusting for potential confounders. Overall, we found that the association between these three a posteriori DPs and MAFLD varied. More specifically, the Yunnan–Guizhou Plateau dietary pattern was positively associated with MAFLD, participants in the highest quantile of this pattern had a 50% greater risk of developing MAFLD (OR = 1.50, 95% CI 1.40–1.60, p for trend < 0.001) than those in the bottom category. The Qinghai–Tibet Plateau dietary pattern is also positively associated with MAFLD (OR = 1.21, 95% CI 1.14–1.30, p for trend < 0.0001), participants in the highest quantile had a 21% greater risk of developing MAFLD. However, the Sichuan Basin dietary pattern did not show significant association with MAFLD in this study.
Fig. 1.
Estimated association between dietary patterns and MAFLD. Estimated association between dietary patterns and MAFLD according to quintiles of dietary pattern scores, with the lowest quintile as reference group. N in the brackets represent the number of MAFLD. Q2–Q5 represent the second to fifth quintiles of dietary pattern scores. The filled dots represent adjusted odds ratios, and the vertical blue lines represent 95% CIs
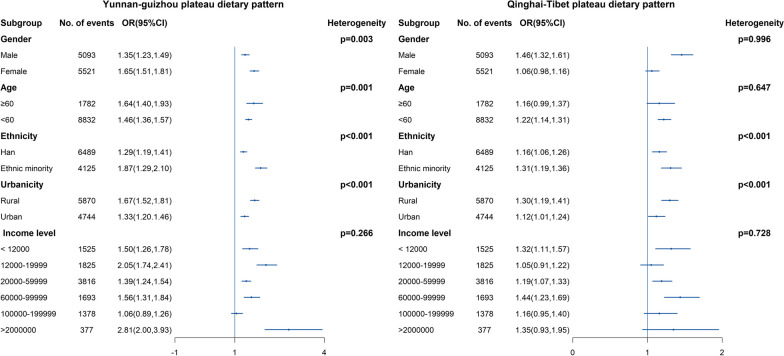
Figure 2 shows the results of the stratification analyses result for the Yunnan–Guizhou Plateau dietary pattern and the Qinghai–Tibet Plateau dietary pattern. The result of Sichuan Basin Dietary Pattern was not presented due to it is not significant associated with MAFLD. For both a posterior DPs, we observed a stronger positive association. For Yunnan–Guizhou Plateau pattern, we found the association in rural residents (OR = 1.67, CI 1.52–1.81) is greater than in urban residents (OR = 1.33, CI 1.20–1.46), and the association in ethnicity minority (OR = 1.87, CI 1.29–2.10) is also greater than in Han majority (OR = 1.29, CI 1.19–1.41). Similarly, for Qinghai–Tibet Plateau pattern, we found the association in rural residents (OR = 1.30, CI 1.19–1.41) is greater than in urban residents (OR = 1.12, CI 1.01–1.24), and the association in ethnicity minority (OR = 1.31, CI 1.19–1.36) is also greater than in Han majority (OR = 1.16, CI 1.06–1.26). Both P values were less than 0.05. We did not observe this difference in gender subgroup.
Fig. 2.
Stratified analysis of estimated association between dietary patterns and MAFLD. Stratified analysis of estimated associations between the Sichuan Basin dietary pattern or the Yunnan–Guizhou Plateau dietary pattern and MAFLD according to gender, age, ethnicity, region and household income, by comparing the highest with the lowest quintiles. Chi-squared tests were performed to examine heterogeneity among different subgroups. The filled blue dots represent adjusted odds ratios, and the vertical blue lines represent 95% CIs
The results of the sensitivity analyses are provided in Additional file 1: Figures 4–7, which were roughly the same as the main analyses, indicating that our findings were robust.
Discussion
In this study, we found that the Yunnan–Guizhou Plateau dietary pattern and the Qinghai–Tibet Plateau dietary pattern were positively associated with MAFLD, while the Sichuan Basin dietary pattern was not significantly associated with MAFLD. And we also found that this positive association was greater in rural residents and ethnicity minority.
In the present study, we found that the prevalence of MAFLD was 16.13%, which was relatively low. In a previous study conducted in east China, the prevalence was 26.1% [26], and another meta-analysis [27] showed a prevalence of 29.1% in China. The reason why the prevalence was low in this population may as follows. Many risk factors have been identified in previous study [28, 29], which including age, obesity, genetic background, socioeconomic status, complications and lifestyle such as diet and physical activity. It has been well recognized that obesity is a vital contributor to MAFLD, several researches have studied the relationship between obesity and MAFLD [30, 31], and most studies concluded that obesity was positively associated with MAFLD. For our study population, the mean BMI was 23.81 and the ratio of have central obesity was 28.4% indicating a relative thin population which may contribute to the low prevalence of MAFLD. Genetic background is another well-studied risk factor for MAFLD [32–34], and it has been showed that the Uygur and Hui ethnic groups have higher rates of NAFLD than the other groups [27, 32]. Our study population consist 9 different ethnicity groups and there may be huge diversity in every aspect of these ethnicity such as genetic background, socioeconomic level, culture including lifestyle, dietary patterns, which could result in dramatic differences in the prevalence of NAFLD.
Our results showed the unfavourable role of the Yunnan–Guizhou Plateau dietary pattern which is characterized by high intake of animal oil, rice and salt. Our previous work has also revealed a strong positive association between this dietary pattern and MetS, a risk factor for MAFLD [21]. Our results were consistent with a body of published works. Animal oil is rich in saturated fatty acid (SFA), and it has proved that SFA was positively associated with MAFLD [35, 36]. In a study conducted in Chinese population, researchers found that high intake of SUA was positively associated with MAFLD (OR = 7.56. CI 3.55–15.88) [37]. Another study has also come into same conclusion by replacing SFA with unsaturated fatty acid (USFA) [38]. In a study enrolled in 28,438 participants from Korea, researchers found that high adherence to carbohydrate/rice-rich diet had a 1.63 to 1.88 times stronger association with MAFLD [39]. Another study that focuses on middle-aged Japanese has also found that high intake of rice was positively associated with MAFLD [40]. The undesirable role of salt for MAFLD has been recognized well [41]. A previous study based on Korea National Health and Nutrition Examination Survey concluded that high salt intake was related to high prevalence of MAFLD (OR = 1.49, CI 1.28–1.73). Similarly, a recent study involved in 23,867 Chinese participants has also come into the conclusion that salt intake was associated with increased NAFLD (OR = 1.60, CI 1.46–1.75) [42]. As for the Qinghai–Tibet Plateau dietary pattern, it is a bit more complex, the negative role of this dietary pattern was only observed in the highest two quintiles. This may due to the interaction between its mixed components. This dietary pattern was dominated by high intake of coarse grains, wheat products, tea and potatoes, and the characteristic of this pattern was that it was rich in both high carbohydrates and dietary fibre. According to previous studies, high intake of dietary fibre and tea may be benefit for MAFLD prevention [43–45], while the intake of high carbohydrates may be related to higher risk of MAFLD [39].
In our study, we also observed a stronger positive association between both Yunnan–Guizhou Plateau dietary pattern and Qinghai–Tibet Plateau dietary pattern with MAFLD in rural and ethnic minority populations. A few of studies have examined the heterogeneity of the association between dietary patterns and MAFLD [46], and they did not find heterogeneity across subgroups. Researches have confirmed that higher-quality food could reduce the risk of MAFLD [47, 48]. For the rural residents and ethnic minorities, most of them lived in plateau area with relatively low-level income, which can substantially restrict the affordability and availability of high-quality food [49]. In this distinct living environment, some featured foods were consumed much more such as potato, rice, as well as red meat and animal oil. Previous researches have indicated that high intake of foods list above was positively associated with MAFLD [50–52]. It has been proved that the dietary culture may differ in ethnicity and socioeconomic status [53], and this might also give rising to this heterogeneity of effect. In the rural and ethnic minority region, the cooking style, way of storage and the taste of food may differ from those of their counterparts. These might also explain the heterogeneity in associations to some extent.
This was the first and largest study to examine the associations between a posteriori DPs and MAFLD in the multi-ethnic region in western China. Our study sample consisted of multi-ethnic participants, which provided a unique opportunity to exclusively detect the relationship between dietary patterns and MAFLD in China’s multi-ethnic region. Besides, we performed the statistical analyses under the guide of the framework of causal inference, which could transparent confounder selection and effect estimation. However, there are limitations in our work. First, it was a cross-sectional study, so the association may not be causal. Second, in the assessment of MAFLD, objective indicators, including insulin and hs-CRP, were not collected for the sake of data availability, which may undermine the number of MAFLD patients. Third, the FFQ used in our study only included 13 crude food groups for feasibility. In this study, many participants were illiterate; often, they spoke different local languages and consumed distinct foods, so it is not be feasible to conduct a more detailed FFQ. Fourth, although we identified potential confounders using a DAG, residual confounders may remain.
Conclusion
In conclusion, in this study we found that both the Yunnan–Guizhou Plateau dietary pattern which is characterized by a higher intake of animal oil, rice and salt and the Qinghai–Tibet Plateau dietary pattern which is characterized by high intake of coarse grain, wheat products, potatoes and tea were positively associated with MAFLD. This may suggest the unpreferable role of salt, animal oil and high carbohydrates in the progress of MAFLD, thereby providing insights into the future dietary intervention in the multi-ethnic regions in western China.
Supplementary Information
Acknowledgements
We thank all the team members and participants involved in the China Multi-Ethnic Cohort (CMEC). We are grateful to Prof. Xiaosong Li at Sichuan University for his leadership and fundamental contribution to the establishment of the CMEC. Prof. Li was the former principal investigator of the CMEC study who passed away in 2019 and will remain in our hearts forever.
Abbreviations
- MAFLD
Metabolic dysfunction-associated fatty liver disease
- SES
Socioeconomic status
- DASH
Dietary Approaches to Stop Hypertension
- BMI
Body mass index
- WC
Waist circumference
- CMEC
The China Multi-Ethnic Cohort Study
- MED
Mediterranean diet
- HEI
Healthy Eating Index
- NAFLD
Non-alcoholic fatty liver disease
- FFQ
Food frequency questionnaire
- DAG
Directed acyclic graph
- OR
Odds ratio
- CI
Confidence interval
Author contributions
XZ and NQ proposed the study concept and design; acquired, analysed and interpreted the data; and drafted the manuscript. QM, LC, XJ, DZ and XZ acquired the data and critically revised the manuscript. NZ, DT and YH carried out statistical analysis. QZ and XX proposed the study concept and design; acquired the data; critically revised the manuscript for important intellectual content; and approved the final article.
Funding
This study was primarily supported by the National Natural Science Foundation of China (Grant Nos. 82273740). The views expressed are those of the author(s) and not necessarily those of the funders. The funders had no role in the design of the study, the collection, analysis and interpretation of the data or the writing of the manuscript.
Data availability
Data described in the manuscript, codebook and analytic code will be made available from the corresponding author (Xiong Xiao, Ph.D., email: xiaoxiong.scu@scu.edu.cn) upon reasonable request, with approval by the principal investigators of the China Multi-Ethnic Cohort study.
Declarations
Ethical approval
This study was performed in accordance with the Declaration of Helsinki. All procedures involving research study participants were approved by the Sichuan University Medical Ethical Review Board [ID: K2016038]. All participants provided written informed consent before data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xingren Zhu and Nimaqucuo have contributed equally as first co-authors.
Qibing Zeng and Xiong Xiao: Joint corresponding authors.
Contributor Information
Qibing Zeng, Email: 178945324@qq.com.
Xiong Xiao, Email: xiaoxiong.scu@scu.edu.cn.
References
- 1.Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 2.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 3.Li J, Zou B, Yeo YH, Feng Y, Xie X, Lee DH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–398. doi: 10.1016/S2468-1253(19)30039-1. [DOI] [PubMed] [Google Scholar]
- 4.Du SF, Wang HJ, Zhang B, Zhai FY, Popkin BM. China in the period of transition from scarcity and extensive undernutrition to emerging nutrition-related non-communicable diseases, 1949–1992. Obes Rev. 2014;15(Suppl 1):8–15. doi: 10.1111/obr.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu K, Guo YS, Zhao CH, Kang SX, Li JL, Wang JX, et al. Etiology exploration of non-alcoholic fatty liver disease from traditional Chinese medicine constitution perspective: a cross-sectional study. Front Public Health. 2021;9:635818. doi: 10.3389/fpubh.2021.635818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen YL, Li H, Li S, Xu Z, Tian S, Wu J, et al. Prevalence of and risk factors for metabolic associated fatty liver disease in an urban population in China: a cross-sectional comparative study. BMC Gastroenterol. 2021;21:1–12. doi: 10.1186/s12876-021-01782-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li H, Wang YJ, Tan K, Zeng L, Liu L, Liu FJ, et al. Prevalence and risk factors of fatty liver disease in Chengdu, Southwest China. Hepatobiliary Pancreat Dis Int. 2009;8:377–382. [PubMed] [Google Scholar]
- 8.Mazidi M, Ofori-Asenso R, Kengne AP. Dietary patterns are associated with likelihood of hepatic steatosis among US adults. J Gastroenterol Hepatol. 2020;35:1916–1922. doi: 10.1111/jgh.15076. [DOI] [PubMed] [Google Scholar]
- 9.El-Agroudy NN, Kurzbach A, Rodionov RN, O'Sullivan J, Roden M, Birkenfeld AL, et al. Are lifestyle therapies effective for NAFLD treatment? Trends Endocrinol Metab. 2019;30:701–709. doi: 10.1016/j.tem.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 10.Mirizzi A, Franco I, Leone CM, Bonfiglio C, Cozzolongo R, Notarnicola M, et al. Effects of some food components on non-alcoholic fatty liver disease severity: results from a cross-sectional study. Nutrients. 2019;11:13. doi: 10.3390/nu11112744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zadeh SH, Mansoori A, Hosseinzadeh M. Relationship between dietary patterns and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2021;36:1470–1478. doi: 10.1111/jgh.15363. [DOI] [PubMed] [Google Scholar]
- 12.Koch M, Nothlings U, Lieb W. Dietary patterns and fatty liver disease. Curr Opin Lipidol. 2015;26:35–41. doi: 10.1097/MOL.0000000000000141. [DOI] [PubMed] [Google Scholar]
- 13.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Properzi C, O'Sullivan TA, Sherriff JL, Ching HL, Jeffrey GP, Buckley RF, et al. Ad libitum Mediterranean and low-fat diets both significantly reduce hepatic steatosis: a randomized controlled trial. Hepatology. 2018;68:1741–1754. doi: 10.1002/hep.30076. [DOI] [PubMed] [Google Scholar]
- 15.Ryan MC, Itsiopoulos C, Thodis T, Ward G, Trost N, Hofferberth S, et al. The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. J Hepatol. 2013;59:138–143. doi: 10.1016/j.jhep.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 16.Li W-Q, Park Y, McGlynn KA, Hollenbeck AR, Taylor PR, Goldstein AM, et al. Index-based dietary patterns and risk of incident hepatocellular carcinoma and mortality from chronic liver disease in a prospective study. Hepatology. 2014;60:588–597. doi: 10.1002/hep.27160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma Y, Yang W, Simon TG, Smith-Warner SA, Fung TT, Sui J, et al. Dietary patterns and risk of hepatocellular carcinoma among US men and women. Hepatology. 2019;70:577–586. doi: 10.1002/hep.30362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tucker KL. Dietary patterns, approaches, and multicultural perspective. Appl Physiol Nutr Metab. 2010;35:211–218. doi: 10.1139/H10-010. [DOI] [PubMed] [Google Scholar]
- 19.Adejumo AC, Samuel GO, Adegbala OM, Adejumo KL, Ojelabi O, Akanbi O, et al. Prevalence, trends, outcomes, and disparities in hospitalizations for nonalcoholic fatty liver disease in the United States. Ann Gastroenterol. 2019;32:504-+. doi: 10.20524/aog.2019.0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao X, Hong F, Yin JZ, Tang WE, Zhang G, Liang X, et al. Cohort profile: the china multi-ethnic cohort (CMEC) study. Int J Epidemiol. 2021;50:721-+. doi: 10.1093/ije/dyaa185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiao X, Qin ZX, Lv XY, Dai YX, Ciren ZG, Yangla Y, et al. Dietary patterns and cardiometabolic risks in diverse less-developed ethnic minority regions: results from the China Multi-Ethnic Cohort (CMEC) Study. Lancet Reg Health-W Pac. 2021;15:13. doi: 10.1016/j.lanwpc.2021.100252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edefonti V, Randi G, La Vecchia C, Ferraroni M, Decarli A. Dietary patterns and breast cancer: a review with focus on methodological issues. Nutr Rev. 2009;67:297–314. doi: 10.1111/j.1753-4887.2009.00203.x. [DOI] [PubMed] [Google Scholar]
- 23.Ferguson KD, McCann M, Katikireddi SV, Thomson H, Green MJ, Smith DJ, et al. Evidence synthesis for constructing directed acyclic graphs (ESC-DAGs): a novel and systematic method for building directed acyclic graphs. Int J Epidemiol. 2020;49:322–329. doi: 10.1093/ije/dyz150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ukoumunne OC, Williamson E, Forbes AB, Gulliford MC, Carlin JB. Confounder-adjusted estimates of the risk difference using propensity score-based weighting. Stat Med. 2010;29:3126–3136. doi: 10.1002/sim.3935. [DOI] [PubMed] [Google Scholar]
- 25.Hainmueller J. Entropy balancing for causal effects: a multivariate reweighting method to produce balanced samples in observational studies. Polit Anal. 2017;20:25–46. doi: 10.1093/pan/mpr025. [DOI] [Google Scholar]
- 26.Chen YL, Li H, Li S, Xu Z, Tian S, Wu J, et al. Prevalence of and risk factors for metabolic associated fatty liver disease in an urban population in China: a cross-sectional comparative study. BMC Gastroenterol. 2021;21:16–30. doi: 10.1186/s12876-021-01782-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou F, Zhou J, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: a systematic review and meta-analysis. Hepatology. 2019;70:1119–1133. doi: 10.1002/hep.30702. [DOI] [PubMed] [Google Scholar]
- 28.He SM, Bao WG, Shao MB, Wang W, Wang CY, Sun J, et al. Risk factors for non-alcoholic fatty liver disease in a Chinese population. Acta Gastro-Enterol Belg. 2011;74:503–508. [PubMed] [Google Scholar]
- 29.Li D, Zhang M, Wu S, Tan H, Li N. Risk factors and prediction model for nonalcoholic fatty liver disease in northwest China. Sci Rep. 2022;12:13877. doi: 10.1038/s41598-022-17511-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: from pathophysiology to therapeutics. Metab Clin Exp. 2019;92:82–97. doi: 10.1016/j.metabol.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 31.Godoy-Matos AF, Silva WS, Valerio CM. NAFLD as a continuum: from obesity to metabolic syndrome and diabetes. Diabetol Metab Syndr. 2020;12:1–10. doi: 10.1186/s13098-020-00570-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cai W, Song JM, Zhang B, Sun YP, Yao H, Zhang YX. The prevalence of nonalcoholic fatty liver disease and relationship with serum uric acid level in Uyghur population. Sci World J. 2014. [DOI] [PMC free article] [PubMed]
- 33.Han MAT, Yu Q, Tafesh Z, Pyrsopoulos N. Diversity in NAFLD: a review of manifestations of nonalcoholic fatty liver disease in different ethnicities globally. J Clin Transl Hepatol. 2021;9:71–80. doi: 10.14218/JCTH.2020.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kalia HS, Gaglio PJ. The prevalence and pathobiology of nonalcoholic fatty liver disease in patients of different races or ethnicities. Clin Liver Dis. 2016;20:215-+. doi: 10.1016/j.cld.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 35.He K, Li Y, Guo X, Zhong L, Tang S. Food groups and the likelihood of non-alcoholic fatty liver disease: a systematic review and meta-analysis. Br J Nutr. 2020;35:1–13. doi: 10.1017/S0007114520000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nakashita C, Xi L, Inoue Y, Kabura R, Masuda S, Yamano Y, et al. Impact of dietary compositions and patterns on the prevalence of nonalcoholic fatty liver disease in Japanese men: a cross-sectional study. BMC Gastroenterol. 2021;21:342. doi: 10.1186/s12876-021-01919-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jiang LP, Sun HZ. Long-chain saturated fatty acids and its interaction with insulin resistance and the risk of nonalcoholic fatty liver disease in type 2 diabetes in Chinese. Front Endocrinol. 2022;13:1051807. doi: 10.3389/fendo.2022.1051807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morrison MC, Mulder P, Stavro PM, Saurez M, Arola-Arnal A, van Duyvenvoorde W, et al. Replacement of dietary saturated fat by PUFA-rich pumpkin seed oil attenuates non-alcoholic fatty liver disease and atherosclerosis development, with additional health effects of virgin over refined oil. PLoS ONE. 2015;10:196. doi: 10.1371/journal.pone.0139196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Park S, Kang S. High carbohydrate and noodle/meat-rich dietary patterns interact with the minor haplotype in the 22q13 loci to increase its association with non-alcoholic fatty liver disease risk in Koreans. Nutr Res. 2020;82:88–98. doi: 10.1016/j.nutres.2020.08.011. [DOI] [PubMed] [Google Scholar]
- 40.Tajima R, Kimura T, Enomoto A, Yanoshita K, Saito A, Kobayashi S, et al. Association between rice, bread, and noodle intake and the prevalence of non-alcoholic fatty liver disease in Japanese middle-aged men and women. Clin Nutr. 2017;36:1601–1608. doi: 10.1016/j.clnu.2016.09.034. [DOI] [PubMed] [Google Scholar]
- 41.Shojaei-Zarghani S, Safarpour AR, Fattahi MR, Keshtkar A. Sodium in relation with nonalcoholic fatty liver disease: a systematic review and meta-analysis of observational studies. Food Sci Nutr. 2022;10:1579–1591. doi: 10.1002/fsn3.2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luo XF, Li Y, Zhou Y, Zhang C, Li LJ, Luo YT, et al. Association of non-alcoholic fatty liver disease with salt intake and dietary diversity in chinese medical examination adults aged 18–59 years: a cross-sectional study. Front Nutr. 2022;9:930316. doi: 10.3389/fnut.2022.930316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun TP, Deng Y, Geng XY, Fang Q, Li XQ, Chen LK, et al. Plasma alkylresorcinol metabolite, a biomarker for whole-grain intake, is inversely associated with risk of nonalcoholic fatty liver disease in a case-control study of Chinese adults. J Nutr. 2022;152:1052–1058. doi: 10.1093/jn/nxab404. [DOI] [PubMed] [Google Scholar]
- 44.Xia Y, Wang XN, Zhang SM, Zhang Q, Liu L, Meng G, et al. Daily tea drinking is not associated with newly diagnosed non-alcoholic fatty liver disease in Chinese adults: the Tianjin chronic low-grade systemic inflammation and health cohort study. Nutr J. 2019;18:1–18. doi: 10.1186/s12937-019-0502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alferink LJM, Erler NS, de Knegt RJ, Janssen HLA, Metselaar HJ, Murad SD, et al. Adherence to a plant-based, high-fibre dietary pattern is related to regression of non-alcoholic fatty liver disease in an elderly population. Eur J Epidemiol. 2020;35:1069–1085. doi: 10.1007/s10654-020-00627-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang W, Wang XY, Huang JL, Wang SY, Yao Q, Li HW. Healthy Eating Index-2015 in relation to risk of metabolic dysfunction-associated fatty liver disease among US population: National Health and Nutrition Examination Survey 2017–2018. Front Nutr. 2023;9:1043901. doi: 10.3389/fnut.2022.1043901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maskarinec G, Lim U, Jacobs S, Monroe KR, Ernst T, Buchthal SD, et al. Diet quality in midadulthood predicts visceral adiposity and liver fatness in older ages: the multiethnic cohort study. Obesity. 2017;25:1442–1450. doi: 10.1002/oby.21868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chan R, Wong VWS, Chu WCW, Wong GLH, Li LS, Leung J, et al. Diet-quality scores and prevalence of nonalcoholic fatty liver disease: a population study using proton-magnetic resonance spectroscopy. PLoS ONE. 2015;10:e0139310. doi: 10.1371/journal.pone.0139310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Q, Liu Z, Hu W, Chen X, Li J, Wan Q, et al. Social capital and dietary patterns in three ethnic minority groups native to Yunnan Province, Southwest China. PLoS ONE. 2021;16:e0256078. doi: 10.1371/journal.pone.0256078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Romero-Gomez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67:829–846. doi: 10.1016/j.jhep.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 51.Machado MV, Cortez-Pinto H. Diet, microbiota, obesity, and NAFLD: a dangerous quartet. Int J Mol Sci. 2016;17:481. doi: 10.3390/ijms17040481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moore MP, Cunningham RP, Dashek RJ, Mucinski JM, Rector RS. A fad too far? Dietary strategies for the prevention and treatment of NAFLD. Obesity (Silver Spring) 2020;28:1843–1852. doi: 10.1002/oby.22964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hiza HAB, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113:297–306. doi: 10.1016/j.jand.2012.08.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the manuscript, codebook and analytic code will be made available from the corresponding author (Xiong Xiao, Ph.D., email: xiaoxiong.scu@scu.edu.cn) upon reasonable request, with approval by the principal investigators of the China Multi-Ethnic Cohort study.