Abstract
To evaluate exercise preconditioning (EP)-induced cardioprotective effects against exercise-induced acute myocardial injury and investigate the alterations of C-type natriuretic peptide (CNP) and its specific receptor, natriuretic peptide receptor B (NPR-B), during EP-induced cardioprotection. Rats were subjected to treadmill exercise as an EP model (4 periods of 10 min each at 30 m/min with intervening periods of rest lasting 10 min). High-intensity exercise was performed 0.5 and 24 h after the EP. EP attenuated high-intensity exercise-induced myocardial injury in both the early and late phases. After EP and high-intensity exercise, CNP and NPR-B levels increased robustly, but no alterations in the plasma CNP were observed. The enhanced NPR-B, plasma and tissue CNP, and its mRNA levels after high-intensity exercise were significantly elevated by EP. These results suggest that cardiac CNP and NPR-B play an important role in EP-mediated cardioprotection against high-intensity exercise-induced myocardial injury in rats.
Keywords: Exercise preconditioning, Cardioprotection, C-type natriuretic peptide, Natriuretic peptide receptor B, Myocardial injury
Introduction
A single bout of internal exercise can enhance the tolerance of an ischemic heart to a subsequent ischemic insult. This effect is known as exercise preconditioning (EP) [1–3]. EP is associated with reduced myocardial infarction during subsequent ischemia reperfusion (I/R) injury, preventing myocardial stunning [4], and attenuating isoproterenol-induced myocardial injury [5]. EP consists of two chronologically distinct phases: an early phase, which occurs immediately after the exercise and is short-lived, and a late phase, which peaks at 24 h post-exercise and can last several days. We have already demonstrated that EP provides a cardioprotective effect against exhaustive exercise-induced myocardial injury, and the translocation and activation of protein kinase C (PKC) may play an important role in the cardioprotective mechanism afforded by EP. However, the mechanism underlying this cardioprotection has yet to be established.
C-type natriuretic peptide (CNP) is an endogenous active peptide that is found mainly in the central nervous system and endothelial cells, and it was recently detected in the myocardium [6]. Because it is cleared rapidly from the circulation and present at very low concentrations in plasma, CNP is thought to act locally [7]. It is well established that CNP causes vasodilation of the blood vessels and improves cardiac function [8]. It brings out cardiovascular roles through paracrine and autocrine means by the activation of NPR-B and natriuretic peptide receptor C (NPR-C). NPR-B is a guanylate cyclase (GC) linked receptor, which appears to be activated preferentially by CNP [9], whereas NPR-C acts mainly as a clearance receptor and also mediates CNP effects in several cell types [10]. Evidence shows that the promotion of hormones in the heart during the EP early and late phases provides a cardioprotective effect [11]. However, research about the alterations of CNP and NPR-B in cardioprotection during EP is still lacking. In the present study, we hypothesized that EP attenuates high-intensity exercise-induced myocardial injury and causes an increase in CNP expression, which probably brings out its cardioprotective effects through the up-regulation of NPR-B.
Materials and methods
Animals
One hundred and fifty adult (8-week-old) male Sprague–Dawley rats (Sippr BK, Shanghai, China) were randomly assigned to standard cages that were maintained at a constant temperature and humidity. During the experimental period, all of the animals were housed in a 12 h light: 12 h dark cycle and were provided with rat chow and water ad libitum. All of the animal care and experimental procedures were conducted in accordance with the Guide for the Care and Use of Laboratory Animals and approved by the Ethics Committee for Science Research of the Shanghai University of Sport.
Experimental protocol
All of the animals received a habituation period of 3 consecutive days of treadmill exercise at 10–20 min/day. The treadmill speed and grade were fixed at 15 m/min and 0 % grade. After the treadmill habituation, the animals received 1 day of rest. To normalize for handling stress, the rats in group C (control) were placed on nonmoving treadmills for a length of time equal to the exercise treatments. The other rats were randomized into the following treatment groups: Group HE (high-intensity exercise) was run 3 h on the treadmill at 35 m/min and 0 % grade; Group EEP (early exercise preconditioning) was subjected to a single bout of interval exercise for four periods of 10 min each at 30 m/min with 10-min intervening periods of rest at 0 % grade. To assess the cardiac effects of EP in late phase, Group LEP (late exercise preconditioning) exercised as group EEP, but rats were sacrificed at a different time; Group EEP+HE (early exercise preconditioning plus high-intensity exercise) exercised as Group EEP, but followed up with high-intensity exercise for 0.5 h after the EP; Group LEP+HE (late exercise preconditioning plus high-intensity exercise) exercised as group LEP, but followed up with high-intensity exercise 24 h after the EP. All of the exercise began with a 5-min warm-up and ended with a 5-min cool down period at 15 m/min and 0 % grade. All rats were sacrificed 0.5 h after the exercise, except rats in LEP which were sacrificed 24 h after the exercise.
The animals were anesthetized with trichloroacetaldehyde monohydrate (400 mg/kg, intraperitoneally), the abdominal cavity was quickly opened, and the blood was drawn from the inferior cava vein. The heart was exposed for perfusion fixation for histology analysis or rapidly excised for quantitative real-time polymerase chain reaction and western blot analysis.
Cardiac troponin I (cTnI) and CNP assay in plasma
The blood samples were centrifuged immediately after collection, and the plasma was separated. Plasma cTnI levels were measured by using automated immunochemiluminescence on an access 2 immunoassay system (Beckman Coulter, USA). This assay is based on a single step sandwich principle with paramagnetic particles coated as the solid phase and two monoclonal cTnI antibodies. The sensitivity threshold for cTnI was 0.01 μg/l.
By using a double-antibody sandwich enzyme-linked immunosorbent assay (ELISA), the plasma CNP levels were measured with a rat CNP ELISA kit (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s instructions.
Hematoxylin-basic fuchsin-picric acid (HBFP) staining
After the perfusion fixation, the samples were fixed in a 4 % paraformaldehyde solution for at least 4 h, and then were embedded in paraffin. Sections of 4 μm were dewaxed and rehydrated before all of the histological experiments.
For the hematoxylin-basic fuchsin-picric acid (HBFP) staining, the sections were stained in alum hematoxylin, differentiated in 1 % acid alcohol, stained in 0.1 % basic fuchsin, rinsed in absolute acetone, differentiated in 0.1 % picric acid in absolute acetone, and rinsed in absolute acetone again. Finally, the sections were cleared in xylene and covered with a coverslip. Five visual fields from each section, with five sections per group, totaling 25 visual fields were captured by the microscope (Olympus Tokyo Japan). The images were randomly taken for morphometric analysis by Image-Pro Plus 6.0 software (Media Cybernetics, Silver Spring, MD, USA) with positive events. The myocardial ischemia/hypoxia density was calculated to display the degree of positive events.
In situ hybridization
In situ hybridization was performed using RNA probes for the CNP gene with the CNP ISH assay kit (Boster Inc, Wuhan, China). The 3 mRNA-probes were:
5′-AATCT CAAGG GAGAC CGATC GCGAC TGCTT CGGGA-3′
5′-TGGGC TCGCC TTCTG CACGA GCACC CCAAC GCGCG-3′
5′-TGCTT TGGCC TCAAG CTGGA CCGGA TCGGC TCCAT-3′.
After deparaffinization and rehydration, the sections were immersed in 3 % hydrogen peroxide for 10 min and then digested with citric acid diluted pepsin for 5–7 min. Next, the sections were incubated with pre-hybridization solution at 42 °C for 3 h followed by digoxin-labeled oligonucleotide probe hybridization solution at 42 °C for 24 h. After the hybridization treatment, the sections were washed in SSC at 37 °C. The bound probe was detected using a streptavidin–biotin complex kit (Boster Inc, Wuhan, China) with diaminobenzidine/peroxidase substrate to produce a brown-colored signal. For the negative controls, the probe hybridization solution was replaced with PBS. The CNP in situ hybridization density was calculated in the same way as for the HBFP staining.
Quantitative real-time polymerase chain reaction
Total RNA from the left ventricular myocardium was extracted by Trizol and was treated with DNase. Then, 1.5 μg of the total RNA samples was reverse-transcribed with oligo primers and SuperaScriptTM III Reverse Transcriptase (Invitrogen, Carlsbad, CA, USA). A quantitative analysis of cardiac CNP mRNA expression was done by real-time polymerase chain reaction (RT-PCR), using a CNP-specific forward primer (5′-CTCTAAAG-GATGGTGGTGGGTA-3′) and reverse primer (5′-CACAGGGTGAGGGTAGGAACA-3′) to amplify the product. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was used for normalization, using the forward primer (5′-GGAAAGCTGTGGCGTGAT-3′) and the reverse primer (5′-AAGGTGGAAGAATGGGAGTT-3′). The thermal cycling conditions were as follows: an initial denaturation at 95 °C for 10 min, followed by 40 cycles of 10 s of denaturing at 95 °C, 60 s of annealing at 60 °C, and 20 s of extension at 72 °C. Real-time PCR was performed in a 384-well plate by the real-time PCR detection system (ABI 7900, USA). To determine relative mRNA expression, we used GAPDH as a control gene. Data were collected after each cycle and are displayed graphically.
Immunohistochemistry and immunofluorescence
Immunohistochemistry and immunofluorescence were performed to observe the CNP or NPR-B in rat myocardium. For immunohistochemistry, the sections were immersed in hydrogen peroxide for 10 min to block the endogenous peroxidase activity, washed 3 times with PBS, and then digested with pepsin for antigen retrieval. After the non-specific binding was blocked with serum, the sections were incubated overnight at 4 °C with primary antibodies specific to CNP (Santa Cruz Biotechnology, Santa Cruz, CA, USA) that were diluted at 1:200. The detection was performed using a streptavidin–biotin complex kit (Boster Inc, Wuhan, China) with a diaminobenzidine/peroxidase substrate to produce a brown color, and the sections were then counterstained with hematoxylin. For immunofluorescence, the sections were digested with pepsin for antigen retrieval and were then washed 3 times with PBS. After the non-specific binding was blocked with serum, the sections were incubated overnight at 4 °C with primary antibodies specific to NPR-B (Santa Cruz Biotechnology, Santa Cruz, CA, USA) that were diluted at 1:200, followed by incubation with Cy3-labeled second antibodies diluted at 1:500 for 30 min at room temperature. The nuclei were stained for 5 min with DAPI (10 μg/ml). Images were captured by the laser scanning confocal microscopy (Zeiss LSM 700, Carl Zeiss Jena, Germany). The positive CNP immunoreactive density and NPR-B immunofluorescence density was calculated in the same way as for the HBFP staining.
Western blotting
Left ventricular myocardium was homogenized in cold RIPA buffer (Beyotime Inc, Jiangsu, China) by an ultrasonic vibrator and a mechanical homogenizer. The protein content was determined according to the method of the bicinchoninic acid assay. Thirty micrograms of protein sample per lane was separated by SDS-PAGE and subsequently transferred to nitrocellulose membranes (Millipore Corp, Bedford, MA). After blocking, the immunoblots were incubated with primary antibody against CNP or NPR-B (Santa Cruz Biotechnology, CA, USA) or GAPDH at 4 °C overnight followed by incubation with a secondary horseradish peroxidase-conjugated IgG (Santa Cruz Biotechnology, CA, USA) for 1 h at room temperature. The results were visualized with the enhanced chemiluminescence method and were evaluated by Image J software (NIH, Bethesda, MD, USA).
Statistical analysis
All of the data are expressed as the mean ± SD and were analyzed by one-way ANOVA (SPSS 19.0; SPSS, Chicago, IL, USA). Correlation analysis was used to assess the relationships between the variables. A value of p < 0.05 was considered statistically significant.
Results
Early and late cardioprotective effect of EP against high-intensity exercise-induced myocardial injury
The HBFP-stained images and the image analysis showed that the hypoxic and ischemic cardiomyocytes stained a vivid crimson red color in contrast to the light brown color of the non-hypoxic and non-ischemic tissue (Fig. 1a). Large areas of ischemic tissue stained by a vivid crimson red color were seen in Group HE, while cardiomyocytes in Group C displayed a light brown color. In Group EEP and Group LEP, a red spot stain was only seen in a small fraction of cardiomyocytes, while in Group EEP+HE and Group LEP+HE, a red patchy stain was scattered across the cardiomyocytes. The image analysis revealed that compared with Group C, the myocardial ischemia/hypoxia density values in Group HE developed significantly (p < 0.05), but no differences in Group EEP and Group LEP (p = NS) were observed (Fig. 1b). The myocardial ischemia/hypoxia density values in Group EEP+HE and Group LEP+HE were significantly lower than those in Group HE (p < 0.05), and no significant differences were found between Group EEP+HE and Group LEP+HE (p = NS).
Fig. 1.
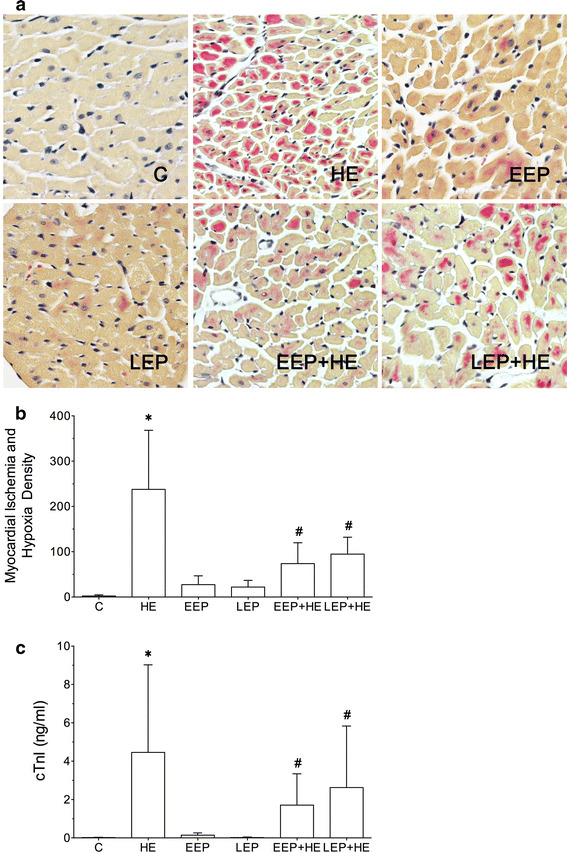
Cardioprotection of EP against high intensive exercise-induced myocardial injury. a Myocardial ischemia/hypoxia detected by HBFP staining. Hypoxic and ischemic cardiomyocytes stained a vivid crimson red color, while the light brown color showed the non-hypoxic and non-ischemic tissue (original magnification ×400). b Quantitative analysis of HBFP staining. The myocardial ischemia/hypoxia density values in Group HE were significantly higher than those in Group C (p < 0.05), while compared with Group HE, the myocardial ischemia/hypoxia density values in Group EEP+HE and Group LEP+HE decreased significantly (p < 0.05). c Alterations of plasma cTnI levels in cardioprotection of EP. The cTnI levels in Group HE were significantly higher than those in Group C (p < 0.05), while compared with Group HE, the cTnI levels in Group EEP+HE and Group LEP+HE decreased significantly (p < 0.05). The data are expressed as the mean ± SD. *p < 0.05 vs Group C, # p < 0.05 vs Group HE
Plasma cTnI levels, as measured by immunochemiluminescence, showed that compared with Group C, plasma cTnI levels in Group HE developed significantly (p < 0.05), while no differences in Group EEP and Group LEP (p = NS) were observed (Fig. 1c). Compared with Group HE, the plasma cTnI levels in Group EEP+HE and Group LEP+HE decreased significantly (p < 0.05). No significant differences were found between Group EEP+HE and Group LEP+HE (p = NS).
mRNA expression of CNP in the cardioprotective effect of EP
The CNP mRNA in situ hybridization signal demonstrated a brown granular pattern of distribution in the myocardial tissue (Fig. 2a). The CNP mRNA in situ hybridization density values were measured to determine the differences of CNP mRNA expression in each group (Fig. 2b). Compared with Group HE, the CNP mRNA in situ hybridization density values were significantly higher in Group EEP+HE and Group LEP+HE (p < 0.05), while no significant differences in in situ hybridization density values were found between Group EEP+HE and Group LEP+HE (p = NS). Moreover, the CNP quantitative PCR results showed the same trend of the CNP mRNA levels in Group EEP+HE and Group LEP+HE, which increased significantly compared to Group HE (Fig. 2c).
Fig. 2.
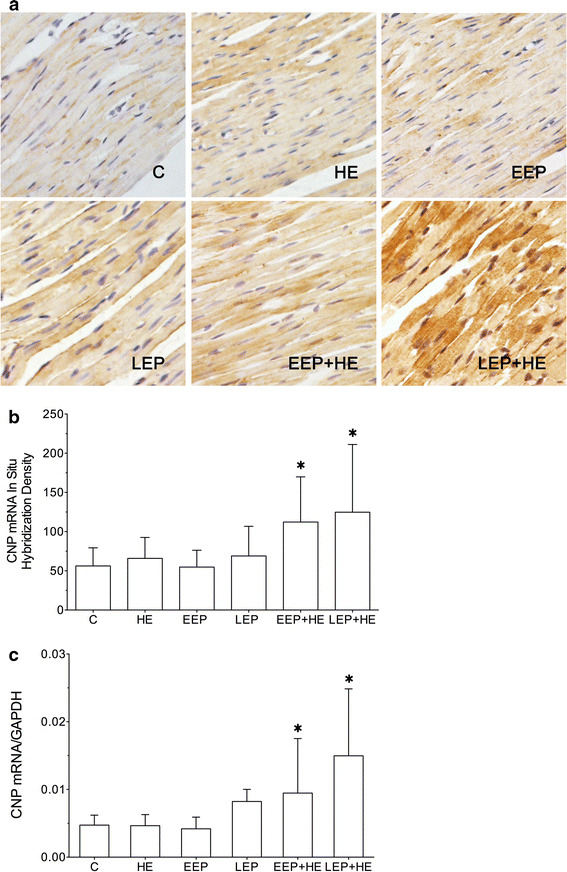
Expression of CNP mRNA in myocardial tissue. a The myocardial CNP mRNA was detected by in situ hybridization staining. The CNP mRNA in situ hybridization signal demonstrated a canary yellow granular pattern of distribution in Group C, Group HE and Group EEP, while a brown lump pattern of distribution was observed in Group EEP+HE and Group LEP+HE (original magnification ×400). b Quantitative analysis of CNP mRNA in situ hybridization staining. The in situ hybridization density values in Group EEP+HE and Group LEP+HE were significantly higher than those in Group HE (p < 0.05). c CNP mRNA levels determined by quantitative real-time polymerase chain reaction analysis. The CNP mRNA levels in Group EEP+HE and Group LEP+HE were significantly higher than those in Group HE (p < 0.05). The data are expressed as the mean ± SD. *p < 0.05 vs Group C
Expression of CNP in the cardioprotective effect of EP
The CNP immunohistochemistry results revealed that in Group C, CNP was localized and showed a cytosolic diffuse pattern (Fig. 3a). Compared with Group C, the pattern of CNP changed in the other groups. An immunoreaction image analysis of CNP revealed that in comparison with Group C, the CNP immunoreactive density values increased in Group HE, Group EEP and Group LEP (p < 0.05, Fig. 3b). Compared with Group HE, the CNP immunoreactive density values significantly increased in Group EEP+HE and Group LEP+HE (p < 0.05). No significant differences were found between Group EEP+HE and Group LEP+HE (p = NS). The same result was found by western blot, which showed that compared with Group C, CNP levels increased in Group HE, Group EEP and Group LEP (p < 0.05); compared with Group HE, the CNP levels increased significantly in Group EEP+HE and Group LEP+HE (p < 0.05, Fig. 3c). Additionally, no significant differences were found between Group EEP+HE and Group LEP+HE (p = NS). Plasma CNP levels measured by ELISA showed that compared with Group HE, the plasma CNP levels in Group EEP+HE and Group LEP+HE increased significantly (p < 0.05, Fig. 3d). No significant differences were found between Group EEP+HE and Group LEP+HE (p = NS).
Fig. 3.
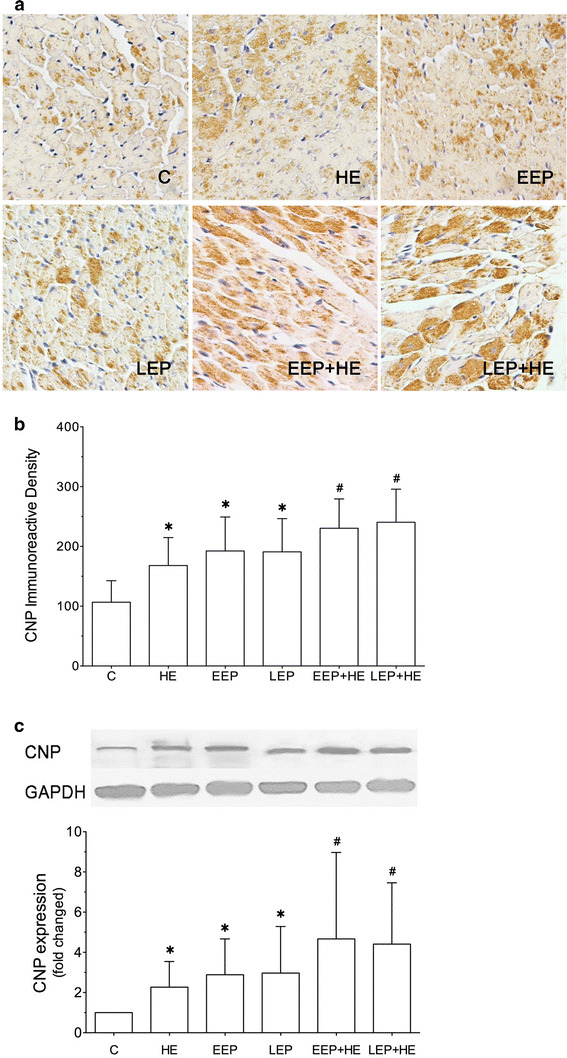

Expression of CNP in myocardial tissue. a Immunohistochemistry staining of CNP in cardiomyocytes. All of the groups with CNP immunostaining demonstrated a brown granular pattern of distribution (original magnification ×400). b Quantitative analysis of CNP immunostaining. The CNP immunoreactive density values in Group HE, Group EEP and Group LEP were significantly higher than those in Group C (p < 0.05); compared with Group HE, the CNP immunoreactive density values in Group EEP+HE and Group LEP+HE increased significantly (p < 0.05). c Myocardial CNP was determined by western blot analysis. The CNP levels in Group HE, Group EEP and Group LEP were significantly higher than those in Group C (p < 0.05); compared with Group HE, the CNP levels in Group EEP+HE and Group LEP+HE increased significantly (p < 0.05). d Plasma CNP levels were measured by an immunosorbent assay. The plasma CNP levels in Group EEP+HE and Group LEP+HE were significantly higher than those in Group C (p < 0.05). The data are presented as the mean ± SD. *p < 0.05 vs Group C, # p < 0.05 vs Group HE
Expression of NPR-B in the cardioprotective effect of EP
The NPR-B immunofluorescence results revealed that NPR-B appeared as a red granular pattern and was located at the cell periphery of the myocardium (Fig. 4a). An immunofluorescence image analysis of NPR-B revealed that in comparison with Group C, the NPR-B immunofluorescence density values increased in Group HE, Group EEP and Group LEP (p < 0.05, Fig. 4b). Compared with Group HE, the NPR-B immunofluorescence density values significantly increased in Group EEP+HE and Group LEP+HE (p < 0.05). No significant differences were found between Group EEP+HE and Group LEP+HE (p = NS). The NPR-B western blot results are presented in (Fig. 4c). Compared with Group C, the NPR-B levels increased in Group HE, Group EEP and Group LEP (p < 0.05). Compared with Group HE, NPR-B levels increased significantly in Group EEP+HE and Group LEP+HE (p < 0.05). Additionally, no significant differences were found between Group EEP+HE and Group LEP+HE (p = NS).
Fig. 4.

Expression of NPR-B in myocardial tissue. a Immunohistochemistry staining of NPR-B in cardiomyocytes. All of the groups of myocardial NPR-B demonstrated a red granular pattern and were located at the cell periphery of the myocardium (original magnification ×400). b Quantitative analysis of NPR-B immunofluorescence. The NPR-B immunofluorescence density values in Group HE, Group EEP, and Group LEP were significantly higher than those in Group C (p < 0.05); compared with Group HE, the NPR-B immunofluorescence density values in Group EEP+HE and Group LEP+HE increased significantly (p < 0.05). c Myocardial NPR-B was measured by western blot analysis. The NPR-B levels in Group HE, Group EEP and Group LEP were significantly higher than those in Group C (p < 0.05); compared with Group HE, the NPR-B levels in Group EEP+HE and Group LEP+HE increased significantly (p < 0.05). The data are presented as the mean ± SD. *p < 0.05 vs Group C, # p < 0.05 vs Group HE
Correlation analysis between HBFP and CNP or NPR-B in myocardium
The results of the correlation analysis showed that, in Group HE, myocardial ischemia/hypoxia density was positively correlated with CNP immunoreactive density (R = 0.762) and NPR-B immunofluorescence density (R = 0.789, Fig. 5a). The same trend was seen in Group EEP+HE that myocardial ischemia/hypoxia density was positively correlated with CNP immunoreactive density (R = 0.780) and NPR-B immunofluorescence density (R = 0.827, Fig. 5b). Meanwhile, in Group LEP + HE, myocardial ischemia/hypoxia density had a linear correlation with CNP immunoreactive density (R = 0.764) and NPR-B immunofluorescence density (R = 0.890, Fig. 5).
Fig. 5.

Correlation analysis between CNP or NPR-B in the myocardium. a Correlation in Group HE. Myocardial ischemia/hypoxia density was positively correlated with CNP immunoreactive density (R = 0.762, p < 0.05) and NPR-B immunofluorescence density (R = 0.789, p < 0.05) in Group HE. b Correlation in Group EEP+HE. Myocardial ischemia/hypoxia density was positively correlated with CNP immunoreactive density (R = 0.780, p < 0.05) and NPR-B immunofluorescence density (R = 0.827, p < 0.05) in Group EEP+HE. c Correlation in Group LEP+HE. Myocardial ischemia/hypoxia density was positively correlated with CNP immunoreactive density (R = 0.764, p < 0.05) and NPR-B immunofluorescence density (R = 0.890 p < 0.05) in Group LEP+HE
Discussion
Early and late cardioprotective effect of EP against high-intensity exercise-induced myocardial injury
“Exercise is medicine”, and research has shown that regular exercise, in addition to reducing cardiovascular risk factors, could protect hearts through modulating cardiac mast cell activation [12]. Even one bout of acute exercise has beneficial cardiac effects against isoproterenol-induced injury [13]. EP, a single bout of interval exercise, could enhance the tolerance of an ischemic heart to a subsequent ischemic insult [14]. EP contains an early and late cardioprotective phase, which may share cardioprotective effects via different mechanisms. Evidence showed that the cardioprotective effects induced by EP during the early phase are superior to that of the late phase [15]. This was well demonstrated in an animal model of myocardial infarction [1, 14, 16], in which the myocardial infarction size was reduced by 76 % in early exercise preconditioning and by 52 % in late exercise preconditioning. The same phenomenon was found in our previous studies by using an exercise-induced myocardial injury model [2, 3, 17], but a more severe myocardial ischemia/hypoxia was seen in the late phase of EP-induced cardioprotection. We hypothesized that exercise capacity improved during the late phase of EP, leading to an enhanced tolerance of the heart to ischemic insults. In addition, the severity of myocardial hypoxia and ischemia does not always match the severity of myocardial injury [2]. Accordingly, in the present experiment, we used 3 h of high-intensity exercise followed by EP to evaluate whether EP offers cardioprotective effects during the late phase. Since cTnI is an important part of myofibrils in the myocardium and may leak out of injured cells into the circulating blood, plasma cTnI serves as a myocardial infarction biomarker in a clinical setting, and is also used to evaluate exercise-induced myocardial injury [18, 19]. HBFP staining was implemented to analyze myocardial ischemia/hypoxia. In this study we used plasma cTnI and HBFP staining to comprehensively assess myocardial injury. The evaluations of cTnI and HBFP staining shared the same results and decreased significantly in Group EEP + HE and Group LEP + HE, confirming that EP reduces high-intensity exercise-induced myocardial injury during both the early and late phases.
Up-regulation of CNP induced by EP
The mechanisms behind the early and late cardioprotective effects of EP involve the secretion of myocardial endogenous substances such as adenosine and opioid peptide [20, 21]. CNP is an important endogenous peptide in our body that regulates cardiovascular homeostasis and has been recently found in the myocardium. Because it brings out a localized regulation through paracrine and autocrine means, alterations in tissues, such as mechanical stress [22], anoxia or ischemia [23], and hormone changes [24, 25] are important factors causing the tissue secretion of CNP. Sun et al. [23] found that the expression of CNP in lung tissue significantly increased after 14 days of hypoxia. Another study showed that pacing-induced heart failure causes a significant improvement of CNP levels in the myocardium of adult minipigs [26]. In the present study, the CNP levels in the myocardium improved significantly after EP and high-intensity exercise. It is reasonable to attribute the alterations of mechanical stress and ischemia induced by EP and high-intensity exercise, to an improvement of CNP levels in the myocardium. Since the expression of myocardial CNP showed a good correlation with the degree of myocardial ischemia/hypoxia in Group HE, Group EEP+HE and Group LEP+HE, our results support the hypothesis that ischemia/hypoxia might be a stimulus for the secretion of myocardial CNP in vivo. Furthermore, we discovered that the CNP mRNA levels in Group EEP+HE and Group LEP+HE presented a significant increase, but this was not observed in Group HE, Group EEP or Group LEP, suggesting that the transcription of CNP mRNA in the myocardium after high-intensity exercise was significantly elevated by EP. Other research found that CNP mRNA levels in the vascular tissue and cultured endothelial cells were up-regulated after undergoing long-term stimulation [22, 27], which indicated that the transcription of CNP mRNA in the cytoplasm would not change immediately after the alterations of mechanical tension in the tissues. In addition, the improvement of CNP mRNA in Group EEP + HE and Group LEP + HE might be a factor that promotes CNP synthesis in the myocardium.
EP-induced early and late phase cardioprotection is associated with CNP expression
CNP exerts direct cardiac effects where it acts as an inotropic and chronotropic agent, causing relaxation of the coronary artery and preventing cardiac hypertrophy. Evidence shows that exogenous CNP administered post-myocardial infarction attenuates cardiac fibrosis and left ventricular hypertrophy and increases survival [28]. Meanwhile, one single perfusion with CNP significantly relaxed the coronary artery through the hyperpolarization of smooth muscle [29], and caused an inotropic and chronotropic response in failing hearts [30–32]. Furthermore, endogenous CNP in the myocardium exerts cardiac effects as well. CNP overexpression is observed in heart failure cardiomyocytes and plays an important role in regulating cardiac hypertrophy and remodeling [33]. In our experiment, with the enhanced CNP level in the myocardium that is observed in Group EEP+HE and Group LEP+HE, the high-intensity exercise-induced myocardial injury is attenuated by the early and late phase of EP, suggesting that CNP improves myocardial ischemia through the relaxation of the coronary artery and causes negative inotropic and positive lusitropic responses in cardiomyocytes. This phenomenon was similar to other reports; Hobbs et al. discovered that administration with exogenous CNP reduced infarct size following I/R injury by regulating coronary blood flow and improving cardiac function in vitro [34], another study showed continuous perfusion with CNP improved left ventricle dysfunction and attenuated the development of cardiac remodeling after myocardial infarction [28]. Interestingly, exogenous CNP could even improve left ventricle performance during restoring exercise in heart failure dogs, which might be attributed to CNP-induced coronary vasodilatation [35]. The improvement of left ventricle function might be due to CNP-induced positive inotropic effects, which activate the NPR-B/cGMP pathway to inhibit phosphodiesterase 3 (PDE3) [30], but dominate negative inotropic and positive lusitropic responses will be followed by phosphorylation of phospholamban (PLB) and troponin I in cardiomyocytes mediated by NPR-B signaling [31, 36]. Meanwhile, we discovered that alterations of CNP in the plasma were consistent with that in the myocardium, which indicated that the overexpression of CNP in the myocardium led to a significant improvement in the plasma. The same phenomenon was observed in heart failure patients [37, 38], such that improvement of CNP in the coronary artery might elicit elevated plasma CNP levels. Therefore, CNP may exert its cardiovascular effect as an endogenous agent, but its mechanism and target organs still need further investigation.
Up-regulation of NPR-B in the EP-induced early and late phases of cardioprotection
The NPR-B receptor is a single transmembrane receptor, which is linked with GC on the cytoplasmic side. With the activation of guanylate cyclase, the level of intracellular cyclic guanosine monophosphate (cGMP) improves significantly. cGMP is an intracellular second messenger that causes vasodilation and regulates cardiac inotropic effects via the activation of downstream protein kinases and ion channels [9]. NPR-B is the specific receptor for CNP and is highly expressed in vascular tissue and hearts. Consequently, perfusion with CNP is often accompanied by increased intracellular cGMP levels, causing vasodilation and inotropic and lusitropic responses of cardiomyocytes [29–31]. In a heart failure model, impairment of myocardial function corresponds with the down-regulation NPR-B in the right ventricle myocardium [26]. These data indicate that NPR-B plays a very important role in regulating cardiac functions. In the present study, alterations of NPR-B in the myocardium match those of CNP, and are also positively correlated with the degree of myocardial ischemia/hypoxia in Group HE, Group EEP+HE, and Group LEP+HE. These results imply that CNP probably induces its cardiac effects by paracrine and autocrine ways through the activation of NPR-B. Moreover, we found that NPR-B levels in the myocardium are up-regulated greatly in Group EEP+HE and Group LEP+HE, while ischemic cardiomyocytes decreased significantly. Enhanced NPR-B might cause an improvement in intracellular cGMP in both vascular smooth muscle cells and cardiomyocytes, which activate the protein kinase G (PKG) pathway. The accumulation of cGMP in coronary smooth muscle cells might cause the opening of potassium channels and induce the relaxation of the coronary artery [29, 39], while in cardiomyocytes, enhanced cGMP might evoke phosphorylation of phospholamban and troponin I, leading to negative inotropic and positive lusitropic responses [31]. Consequently, the present study suggests that myocardial NPR-B plays an important role in the CNP-induced cardiac effects that occur during the EP-induced early and late phases of cardioprotection.
Conclusions
This work suggests that EP attenuates high-intensity exercise-induced myocardial injury in the early and late phases of cardioprotection. EP promotes the secretion of CNP and the up-regulation of NPR-B in the myocardium. EP elevates the levels of CNP in the myocardium during high-intensity exercise, which might cause an increase of CNP in plasma and evoke early and late cardioprotective effects against high-intensity exercise-induced myocardial injury, probably via the up-regulation of NPR-B.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Nos. 31071031, 31471136).
Abbreviations
- EP
Exercise preconditioning
- CNP
C-type natriuretic peptide
- NPR-B
Natriuretic peptide receptor B
- NPR-C
Natriuretic peptide receptor C
- PKC
Protein kinase C
- cTnI
Cardiac troponin I
- GC
Guanylate cyclase
- cGMP
Cyclic guanosine monophosphate
- PKG
Protein kinase G
- PLB
Phospholamban
- PDE3
Phosphodiesterase 3
Compliance with ethical standards
Conflict of interest
The authors declare no conflicts of interest.
References
- 1.Parra VM, Macho P, Sanchez G, Donoso P, Domenech RJ. Exercise preconditioning of myocardial infarct size in dogs is triggered by calcium. J Cardiovasc Pharmacol. 2015;65:276–281. doi: 10.1097/FJC.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 2.Hao Z, Pan SS, Shen YJ, Ge J. Exercise preconditioning-induced early and late phase of cardioprotection is associated with protein kinase C epsilon translocation. Circ J. 2014;78:1636–1645. doi: 10.1253/circj.CJ-13-1525. [DOI] [PubMed] [Google Scholar]
- 3.Hao Z, Pan SS, Shen YJ, Ge J. Exercise preconditioning-induced late phase of cardioprotection against exhaustive exercise: possible role of protein kinase C delta. J Physiol Sci. 2014;64:333–345. doi: 10.1007/s12576-014-0323-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lennon SL, Quindry JC, French JP, Kim S, Mehta JL, Powers SK. Exercise and myocardial tolerance to ischaemia-reperfusion. Acta Physiol Scand. 2004;182:161–169. doi: 10.1111/j.1365-201X.2004.01346.x. [DOI] [PubMed] [Google Scholar]
- 5.Shen YJ, Pan SS, Zhuang T, Wang FJ. Exercise preconditioning initiates late cardioprotection against isoproterenol-induced myocardial injury in rats independent of protein kinase C. J Physiol Sci. 2011;61:13–21. doi: 10.1007/s12576-010-0116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Del Ry S, Cabiati M, Vozzi F, Battolla B, Caselli C, Forini F, et al. Expression of C-type natriuretic peptide and its receptor NPR-B in cardiomyocytes. Peptides. 2011;32:1713–1718. doi: 10.1016/j.peptides.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 7.Del Ry S. C-type natriuretic peptide: a new cardiac mediator. Peptides. 2013;40:93–98. doi: 10.1016/j.peptides.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Lumsden NG, Khambata RS, Hobbs AJ. C-type natriuretic peptide (CNP): cardiovascular roles and potential as a therapeutic target. Curr Pharm Des. 2010;16:4080–4088. doi: 10.2174/138161210794519237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pagel-Langenickel I, Buttgereit J, Bader M, Langenickel TH. Natriuretic peptide receptor B signaling in the cardiovascular system: protection from cardiac hypertrophy. J Mol Med (Berl) 2007;85:797–810. doi: 10.1007/s00109-007-0183-4. [DOI] [PubMed] [Google Scholar]
- 10.Rose RA, Giles WR. Natriuretic peptide C receptor signalling in the heart and vasculature. J Physiol. 2008;586:353–366. doi: 10.1113/jphysiol.2007.144253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alleman RJ, Stewart LM, Tsang AM, Brown DA. Why does exercise “trigger” adaptive protective responses in the heart? Dose Response. 2015;13:1–19. doi: 10.2203/dose-response.14-023.Alleman. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phungphong S, Kijtawornrat A, Wattanapermpool J, Bupha-Intr T. Regular exercise modulates cardiac mast cell activation in ovariectomized rats. J Physiol Sci. 2016;66:165–173. doi: 10.1007/s12576-015-0409-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jimenez SK, Jassal DS, Kardami E, Cattini PA. A single bout of exercise promotes sustained left ventricular function improvement after isoproterenol-induced injury in mice. J Physiol Sci. 2011;61:331–336. doi: 10.1007/s12576-011-0147-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Domenech R, Macho P, Schwarze H, Sanchez G. Exercise induces early and late myocardial preconditioning in dogs. Cardiovasc Res. 2002;55:561–566. doi: 10.1016/S0008-6363(02)00334-6. [DOI] [PubMed] [Google Scholar]
- 15.Kavazis AN. Exercise preconditioning of the myocardium. Sports Med. 2009;39:923–935. doi: 10.2165/11317870-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 16.Parra VM, Macho P, Domenech RJ. Late cardiac preconditioning by exercise in dogs is mediated by mitochondrial potassium channels. J Cardiovasc Pharmacol. 2010;56:268–274. doi: 10.1097/FJC.0b013e3181eb3049. [DOI] [PubMed] [Google Scholar]
- 17.Shen YJ, Pan SS, Ge J, Hao Z. Exercise preconditioning provides early cardioprotection against exhaustive exercise in rats: potential involvement of protein kinase C delta translocation. Mol Cell Biochem. 2012;368:89–102. doi: 10.1007/s11010-012-1346-3. [DOI] [PubMed] [Google Scholar]
- 18.Kobirumaki-Shimozawa F, Inoue T, Shintani SA, Oyama K, Terui T, Minamisawa S, et al. Cardiac thin filament regulation and the Frank-Starling mechanism. J Physiol Sci. 2014;64:221–232. doi: 10.1007/s12576-014-0314-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shave R, Baggish A, George K, Wood M, Scharhag J, Whyte G, et al. Exercise-induced cardiac troponin elevation: evidence, mechanisms, and implications. J Am Coll Cardiol. 2010;56:169–176. doi: 10.1016/j.jacc.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 20.Dickson EW, Hogrefe CP, Ludwig PS, Ackermann LW, Stoll LL, Denning GM. Exercise enhances myocardial ischemic tolerance via an opioid receptor-dependent mechanism. Am J Physiol Heart Circ Physiol. 2008;294:H402–H408. doi: 10.1152/ajpheart.00280.2007. [DOI] [PubMed] [Google Scholar]
- 21.Husain K, Somani SM. Interaction of exercise and adenosine receptor agonist and antagonist on rat heart antioxidant defense system. Mol Cell Biochem. 2005;270:209–214. doi: 10.1007/s11010-005-5285-0. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Z, Xiao Z, Diamond SL. Shear stress induction of C-type natriuretic peptide (CNP) in endothelial cells is independent of NO autocrine signaling. Ann Biomed Eng. 1999;27:419–426. doi: 10.1114/1.203. [DOI] [PubMed] [Google Scholar]
- 23.Sun DJ, Yang JP, Sun YH. The expression and significance of urotensin II, nitric oxide, and C-type natriuretic peptide in hypoxia-induced pulmonary hypertension in rats. Zhonghua Jie He He Hu Xi Za Zhi. 2006;29:185–188. [PubMed] [Google Scholar]
- 24.Horio T, Tokudome T, Maki T, Yoshihara F, Suga S, Nishikimi T, et al. Gene expression, secretion, and autocrine action of C-type natriuretic peptide in cultured adult rat cardiac fibroblasts. Endocrinology. 2003;144:2279–2284. doi: 10.1210/en.2003-0128. [DOI] [PubMed] [Google Scholar]
- 25.Mendonca MC, Koles N, Doi SQ, Sellitti DF. Transforming growth factor-beta1 regulation of C-type natriuretic peptide expression in human vascular smooth muscle cells: dependence on TSC22D1. Am J Physiol Heart Circ Physiol. 2010;299:H2018–H2027. doi: 10.1152/ajpheart.00656.2010. [DOI] [PubMed] [Google Scholar]
- 26.Del Ry S, Cabiati M, Lionetti V, Emdin M, Recchia FA, Giannessi D. Expression of C-type natriuretic peptide and of its receptor NPR-B in normal and failing heart. Peptides. 2008;29:2208–2215. doi: 10.1016/j.peptides.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 27.Maeda S, Iemitsu M, Miyauchi T, Kuno S, Matsuda M, Tanaka H. Aortic stiffness and aerobic exercise: mechanistic insight from microarray analyses. Med Sci Sports Exerc. 2005;37:1710–1716. doi: 10.1249/01.mss.0000175052.37087.f8. [DOI] [PubMed] [Google Scholar]
- 28.Soeki T, Kishimoto I, Okumura H, Tokudome T, Horio T, Mori K, et al. C-type natriuretic peptide, a novel antifibrotic and antihypertrophic agent, prevents cardiac remodeling after myocardial infarction. J Am Coll Cardiol. 2005;45:608–616. doi: 10.1016/j.jacc.2004.10.067. [DOI] [PubMed] [Google Scholar]
- 29.Liang CF, Au AL, Leung SW, Ng KF, Feletou M, Kwan YW, et al. Endothelium-derived nitric oxide inhibits the relaxation of the porcine coronary artery to natriuretic peptides by desensitizing big conductance calcium-activated potassium channels of vascular smooth muscle. J Pharmacol Exp Ther. 2010;334:223–231. doi: 10.1124/jpet.110.166652. [DOI] [PubMed] [Google Scholar]
- 30.Qvigstad E, Moltzau LR, Aronsen JM, Nguyen CH, Hougen K, Sjaastad I, et al. Natriuretic peptides increase beta1-adrenoceptor signalling in failing hearts through phosphodiesterase 3 inhibition. Cardiovasc Res. 2010;85:763–772. doi: 10.1093/cvr/cvp364. [DOI] [PubMed] [Google Scholar]
- 31.Moltzau LR, Aronsen JM, Meier S, Nguyen CH, Hougen K, Orstavik O, et al. SERCA2 activity is involved in the CNP-mediated functional responses in failing rat myocardium. Br J Pharmacol. 2013;170:366–379. doi: 10.1111/bph.12282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Afzal F, Qvigstad E, Aronsen JM, Moltzau LR, Sjaastad I, Skomedal T, et al. Agents increasing cyclic GMP amplify 5-HT4-elicited positive inotropic response in failing rat cardiac ventricle. Naunyn Schmiedebergs Arch Pharmacol. 2011;384:543–553. doi: 10.1007/s00210-011-0670-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Y, de Waard MC, Sterner-Kock A, Stepan H, Schultheiss HP, Duncker DJ, et al. Cardiomyocyte-restricted over-expression of C-type natriuretic peptide prevents cardiac hypertrophy induced by myocardial infarction in mice. Eur J Heart Fail. 2007;9:548–557. doi: 10.1016/j.ejheart.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Hobbs A, Foster P, Prescott C, Scotland R, Ahluwalia A. Natriuretic peptide receptor-C regulates coronary blood flow and prevents myocardial ischemia/reperfusion injury: novel cardioprotective role for endothelium-derived C-type natriuretic peptide. Circulation. 2004;110:1231–1235. doi: 10.1161/01.CIR.0000141802.29945.34. [DOI] [PubMed] [Google Scholar]
- 35.Li T, Cheng HJ, Ohte N, Hasegawa H, Morimoto A, Herrington DM, et al. C-type natriuretic peptide improves left ventricular functional performance at rest and restores normal exercise responses after heart failure. J Pharmacol Exp Ther. 2016;357:545–553. doi: 10.1124/jpet.115.231696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pierkes M, Gambaryan S, Boknik P, Lohmann SM, Schmitz W, Potthast R, et al. Increased effects of C-type natriuretic peptide on cardiac ventricular contractility and relaxation in guanylyl cyclase A-deficient mice. Cardiovasc Res. 2002;53:852–861. doi: 10.1016/S0008-6363(01)00543-0. [DOI] [PubMed] [Google Scholar]
- 37.Kalra PR, Clague JR, Bolger AP, Anker SD, Poole-Wilson PA, Struthers AD, et al. Myocardial production of C-type natriuretic peptide in chronic heart failure. Circulation. 2003;107:571–573. doi: 10.1161/01.CIR.0000047280.15244.EB. [DOI] [PubMed] [Google Scholar]
- 38.Del Ry S, Cabiati M, Stefano T, Catapano G, Caselli C, Prescimone T, et al. Comparison of NT-proCNP and CNP plasma levels in heart failure, diabetes and cirrhosis patients. Regul Pept. 2011;166:15–20. doi: 10.1016/j.regpep.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 39.Barber DA, Burnett JC, Jr, Fitzpatrick LA, Sieck GC, Miller VM. Gender and relaxation to C-type natriuretic peptide in porcine coronary arteries. J Cardiovasc Pharmacol. 1998;32:5–11. doi: 10.1097/00005344-199807000-00002. [DOI] [PubMed] [Google Scholar]


