Abstract
Previous studies have shown that electroacupuncture (EA) can induce cardioprotection against ischemia–reperfusion (IR) injury, but its mechanisms are incompletely understood. We have previously shown that several other forms of remote preconditioning of the heart work, at least in part, via the release of circulating cardioprotective factors into the bloodstream, that can be dialyzed and subsequently shown to reduce IR injury in isolated hearts. We used the same methods to assess whether EA leads to similar humoral cardioprotection. EA rabbits were subjected to 60 min of bilateral stimulation at the Neiguan point, following which their blood was drawn, dialyzed, and used to perfuse hearts in Langendorff preparation and subsequently subjected to 60 min of global ischemia and 120 min of reperfusion. Compared to controls, dialysate from EA animals led to significant reduction in infarct size and improved functional recovery. The degree of cardioprotection was no different to that seen in animals randomized to receive remote preconditioning using transient limb ischemia (4 cycles of 5 min ischemia/5 min reperfusion). These results suggest that EA recapitulates the cardioprotection achieved by remote preconditioning, by similarly leading to release of circulating cardioprotective factors.
Keywords: Remote preconditioning, Electroacupuncture, Cardioprotection
Introduction
Remote ischemic preconditioning (rIPC) resulting from brief episodes of ischemia followed by reperfusion of an organ [1] or limb [2, 3] has been shown to exert a powerful cardioprotective effect against damage resulting from a prolonged ischemic insult, in both animal models and human clinical trials [4]. We have previously shown that rIPC induced by transient limb ischemia and reperfusion releases a dialyzable factor into the blood that provides potent cardioprotection in isolated heart preparations [5]. We have recently demonstrated that several other modes of inducing remote cardioprotection are also mediated, at least in part, by dialyzable circulating humoral factors, including intra-arterial adenosine, direct peripheral nerve stimulation, and topical capsaicin [6, 7].
Interestingly, cardioprotection has also been demonstrated in experimental models following treatment by electroacupuncture. Gao et al. [8] used electroacupuncture at the Neiguan point, located on the medial surface of the forelimb between the radius and ulnar, which is said to be cardiospecific. Electroacupuncture was applied daily for 3 days and resulted in reduction in infarct size compared to controls, in rats subsequently subjected to 30 min LAD occlusion. Their treatment protocol at a non-cardiac acupoint failed to have an effect in their study. In a second study from this group [9], a role for beta receptor stimulation as an underlying mechanism was suggested, as the cardioprotection of EA was abolished by pretreatment with propranolol. Subsequently, Zhang and colleagues [10] used electroacupuncture as a ‘postconditioning’ stimulus in rabbits, starting the intervention during the early reperfusion phase, following 30 min of LAD ischemia. Stimulation at the cardiospecific Neiguan point, but not the ‘non-cardiac’ Lieque point, located beside the stylus process of the radius, markedly decreased the number of apoptotic cells, reduced the content of malondialdehyde, and inhibited Bax protein expression while enhancing Bcl-2 expression and glutathione peroxidase activity in the ischemic zone. Most recently, Zhou et al. [11] have suggested a role for cardiac sympathetic nerves and opiate receptor stimulation. The cardioprotective effects of EA were partially blocked by pretreatment with naloxone or chelerythrine alone and completely blocked by pretreatment with both naloxone and chelerythrine. We have previously shown that the cardioprotective effect of dialysate obtained from animal preconditioned with limb ischemia is also abrogated by pretreatment with naloxone [5]. Thus, while there is increasing evidence to suggest that electroacupuncture has cardioprotective effects, not all studies have been positive [12], and the mechanism of its effect is not fully understood. In particular, the possibility that it works via the release of circulating cardioprotective factors has not been tested. We therefore used our established model in a proof-of-principle study to assess whether electroacupuncture induces cardioprotection via humoral mechanisms in a similar way to other modes of remote conditioning stimuli.
Methods
All animal protocols were approved by the Animal Care and Use Committee of the Hospital for Sick Children in Toronto and conformed to the Guide for the Care and Use of Laboratory Animals, published by the National Institutes of Health (NIH Publication No. 85-23, Revised 1996).
Our experimental method has been described in detail elsewhere [5]. Briefly, all animals were anesthetized (Akmezine 0.25 mg/kg and pentobarbital sodium 30 mg/kg) and ventilated, and instrumented with a large-bore cannula in the carotid artery for rapid blood sampling after study intervention. Rabbits were divided into three groups: group 1 (sham), animals were anesthetized for 40 min, but no other intervention was performed prior to blood-draw; group 2 (rIPC), remote ischemic preconditioning was induced through four cycles of 5 min of hindlimb ischemia (via a tourniquet), followed by 5 min of reperfusion as previously described [2]; and group 3, electroacupuncture (EA) was applied bilaterally with one needle at the P6 Neiguan point (located on the medial forelimb 1/6 the length of the line from the wrist to the elbow between the radius and ulna) and the other needle at P5 (Jianshi point). We used the stimulation protocol previously shown to be cardioprotective by Zhang et al. [10]. Disperse-dense waves of alternating frequencies of 2 and 15 Hz were applied at an intensity of 1–2 mA, to maintain a slight twitch of the limb for 60 min (KWD-808 I Multi-Purpose Health Device; Changzhou, China) (Fig. 1). At the end of the study intervention, 80 ml of blood was rapidly drawn from each animal, and the animal was then euthanized. Dialysate (12–14-kDa cutoff membrane, SpectraPor; Spectrum Laboratories, Rancho Dominguez, CA, USA) of the blood plasma was then prepared using our previously reported protocol [5], and used to perfuse untreated rabbit hearts mounted in Langendorff preparation. Following a period of stabilization of 20 min, each heart was perfused for approximately 20 min with control, rIPC, or EA dialysate, and then subjected to 30 min of global ischemia, followed by 2 h of reperfusion. Hemodynamic responses were measured throughout the protocol using a balloon-tipped catheter placed in the left ventricle (PowerLab data acquisition system; ADInstruments, Colorado Springs, CO, USA). At the end of the study, the heart was removed from the Langendorff apparatus, and the LV was excised and frozen at −80 °C. The frozen heart was cut transversely into 2-mm-thick slices using a rabbit Heart Slicer Matrix (Zivic Instruments, Pittsburgh, PA, USA) and stained with 1.25 % triphenyltetrazolium chloride (Sigma) in 200 mM Tris (pH 7.4) for 20 min in a water bath at 37 °C. After fixation for 2 h in 10 % neutral-buffered formaldehyde, each slice was photographed by electronic scanning (CanoScan 4400F). The viable myocardium stained brick red, and infarct tissues appeared pale. The infarct and LV areas were measured via automated planimetry using Adobe Photoshop CS2 software, with infarct size expressed as a percentage of the total LV area.
Fig. 1.
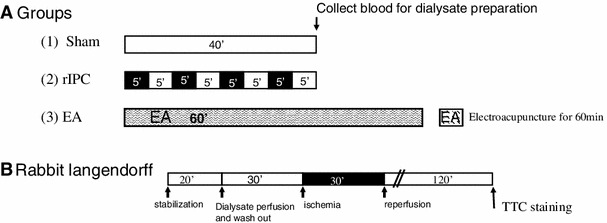
Schematic showing study protocol. a (1) Sham animals were anesthetized for 40 min prior to blood draw. (2) Remote ischemic preconditioning (rIPC) (four cycles of transient limb ischemia, black boxes, 5 min; and reperfusion white boxes, 5 min) was performed prior to blood draw. (3) Electroacupuncture (EA) was applied bilaterally at the Neiguan point for 60 min prior to blood draw. b Overview of the Langendorff protocol. After stabilization, each heart randomized to be perfused with previously prepared dialysate from one of the groups described above, followed by 30 min of global ischemia and 120 min of reperfusion. At the end of the protocol the heart was assessed for infarct size by TTC staining (see text for details)
Data are reported as mean ± standard error (SE). For each individual outcome, a linear regression model, with maximum likelihood algorithm for parameter determination, was created (PROC GENMOD with the SAS system, using standard settings, normal distribution, and identity link function). To eliminate the issue of multiple comparisons, binary dummy variables were created for each study groups (mutually exclusive binary strings with 7 values each representing each study group), and all 7 dummy variables were included in the same regression model (using the sham group as the reference category, against which all other groups were compared). This allowed between-group comparisons from the regression model parameter estimates without performing multiple statistical tests. Statistical significance of each between-group comparison was based on the likelihood ratio test, based on the ratio between the difference in parameter estimate of the experimental group versus the reference group and the standard error of that difference. This single-model approach allowed for better handling of the small sample sizes than a standard ANOVA, and eliminated the need for post hoc testing. Level of statistical significance was set as p < 0.05 for all analyses. All statistical analyses were performed using SAS v.9.2 (SAS Institute; Cary, NC, USA).
Results
In total, 23 donor rabbits were used. The data from 5 hearts were excluded at the time of Langendorff preparation due to ventilation failure during procedure in 1 animal, due to VF during stabilization in 2 hearts, and due to VF during reperfusion in 2 hearts. There were no differences in the number of hearts excluded between the groups. Therefore, data from 18 animals were analyzed in this study; 6 in each of the 3 groups, sham, rIPC and EA. The data for each of the groups are detailed in Table 1.
Table 1.
Haemodynamic data
| Group | n | HR, beats/min | LVDP, mmHg (baseline) or % (120 min after reperfusion) | +dP/dt, mmHg/s (baseline) or % (120 min after reperfusion) | −dP/dt, mmHg/s (baseline) or % (120 min after reperfusion) | LVEDP, mmHg | CFR, ml/min |
|---|---|---|---|---|---|---|---|
| Baseline | |||||||
| Sham | 6 | 180 ± 8 | 133 ± 5.6 | 2,086 ± 192 | −1,498 ± 89 | 7.3 ± 0.6 | 64.4 ± 2.1 |
| rIPC | 6 | 165 ± 2 | 110 ± 4.6 | 1,880 ± 132 | −1,301 ± 42 | 5.9 ± 0.2 | 54.4 ± 1.7 |
| EA at Neiguan point | 7 | 170 ± 7 | 88 ± 3.9 | 2,159 ± 331 | −1,336 ± 64 | 6.7 ± 0.3 | 53.1 ± 5.3 |
| 120 min after reperfusion | |||||||
| Sham | 6 | 155 ± 12 | 31.7 ± 3.5 | 34.5 ± 12.6 | −34.2 ± 4.6 | 37.4 ± 6.8 | 28.1 ± 2.5 |
| rIPC | 6 | 146 ± 7 | 43.2 ± 2.5* | 48.9 ± 4.9 | −45.6 ± 2.2 | 24.9 ± 4.4* | 26.7 ± 2.0 |
| EA at Neiguan point | 7 | 135 ± 6 | 41.6 ± 6.2* | 35.4 ± 9.8 | −39.3 ± 7.8 | 12.3 ± 3.4** | 25.3 ± 3.1 |
Values are mean ± SE
n Number of rabbits in each group, HR heart rate, LVDP left ventricular developed pressure, +dP/dt maximum rates or contraction, −dP/dt maximum rates of relaxation, % percentage of baseline (pre-ischemia), LVEDP left ventricular end-diastolic pressure, CFR coronary rate flow, rIPC remote ischemic preconditioning, EA electroacupuncture at the Neiguan point
** p < 0.01 vs. sham, * p < 0.05 vs. Sham
Infarct size
As expected, perfusion with rIPC dialysate significantly attenuated the infarct size when compared with sham dialysate (28.1 ± 5.3 % in rIPC vs. 45.4 ± 3.4 % in sham, p < 0.01). Dialysate from the EA group also significantly decreased the infarct size in comparison to the sham dialysate (29.4 ± 5.3 % in EA vs. 45.4 ± 3.4 % in sham, EST −16.073 (6.685), p < 0.05) (Fig. 2). There was no difference between rIPC and EA (p = ns).
Fig. 2.
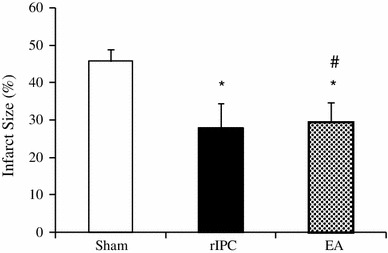
The infarct size (as a percentage of total myocardium) in the Sham, rIPC, and EA groups. *p < 0.05 compared with sham, # p = non-significant when compared with rIPC
Functional haemodynamic data
Post-ischemic cardiac performance was significantly improved with perfusion with rIPC dialysate in isolated perfused hearts at 120 min of reperfusion. The recovery of LV developed pressure (LVDP) was significantly greater in hearts perfused with rIPC dialysate than that of hearts perfused with the sham dialysate (p < 0.05). Both +dP/dt and −dP/dt trended towards being improved with rIPC compared to sham (p < 0.07 and 0.11, respectively). Furthermore, there was a trend towards rIPC improving the diastolic recovery, with the LVEDP lower compared to the sham group (24.9 ± 4.4 % in rIPC vs. 37.4 ± 6.8 % in sham, p < 0.05). Perfusion with EA dialysate also significantly improved the post-ischemic cardiac performance. Recovery of LVDP was greater in hearts perfused with EA dialysate (41.6 ± 6.2 % of pre-ischemic value) compared to sham dialysate (31.7 ± 3.5 % of pre-ischemic value, p < 0.05). However, neither +dP/dt nor −dP/dt were improved with EA compared to sham (+dP/dt, 35.4 ± 9.8 % in EA vs. 34.5 ± 4.6 % in sham, p = ns; and −dP/dt, −39.3 ± 7.8 % in EA vs. −34.2 ± 4.6 % in sham, p = ns). Nonetheless, EA improved diastolic recovery, with the LVEDP being significantly lower compared to the sham-operated hearts (15.3 ± 3.4 % in EA vs. 37.4 ± 6.8 % in sham, p = 0.0008).
Discussion
We have demonstrated that electroacupuncture provokes the release of a dialyzable factor(s) into the bloodstream of animals, which has a cardioprotective effect leading to decreased infarct size and enhanced functional recovery after prolonged global ischemia. As such, it recapitulates the effects of rIPC induced by transient ischemia and reperfusion of the limb.
The exact mechanisms of the various effects of acupuncture and electroacupuncture largely remain incompletely understood. However, we were intrigued by the potential similarities between the cardioprotection induced by electroacupuncture reported by others [9, 10], and rIPC induced by transient limb ischemia and other stimuli. Our data suggest that the mechanism of EA appears to be similar to that of the other modes of rIPC, inducing the release of bloodborne humoral factors, which have similar cardioprotective efficacy. Our proof-of-principle study was not designed to elucidate further details of the signal transduction of electroacupuncture, but is likely that it stimulates local nerve tracts, or peripheral sensory nerves, much in the same way as direct femoral nerve stimulation and topical capsaicin was shown to induce release of cardioprotective factors in our previous study [7]. Indeed, the apparent site-specificity of EA-induced cardioprotection shown in previous studies [10] suggests that this is a local effect rather than a generic effect of the stimulus itself. Furthermore, the observations of Tsou and coworkers [13] showing that the cardioprotective effects of EA are abrogated by local median nerve transection and intravenous naloxone are entirely compatible with our previous observations showing femoral nerve transection blocks release of humoral cardioprotection in limb-ischemia rIPC [7], and our findings that naloxone blocked the cardioprotective effect of rIPC dialysate in an isolated cardiomyocyte model [5]. It should be noted, however, that not all studies of EA have shown cardioprotection. In a recent study, Dow et al. [12] failed to demonstrate cardioprotection in a rat model of EA, attributing the lack of difference compared to control to a lack of hemodynamic effect of the EA protocol. While this is plausible, and we did not measure such responses, it should be noted that the stimulus used was somewhat different to that used in the current study, and the anesthesia used in their model was ketamine, which itself can act variably as a preconditioning agent [14], or blocker of preconditioning [15], depending on the model.
Nonetheless, the protocol used by us and others has been shown to be cardioprotective, and, consequently, this study adds another stimulus to the portfolio of remote stimuli that induce the humoral release of cardioprotective substance. It remains to be demonstrated whether one method is superior to another, but much of the available clinical data have been obtained using transient limb ischemia, using a blood pressure cuff [4, 16]. While a readily available and facile technique, EA represents another method that may be used in the clinical setting, although clearly more studies are required to demonstrate its optimal delivery, dose–response, and clinical effectiveness.
In summary, electroacupuncture at the Neiguan point, previously shown to induce cardioprotection in vivo, leads to release of blood-borne cardioprotective factors that reduce myocardial damage and enhance functional recovery in response to prolonged myocardial ischemia in isolated hearts.
Acknowledgments
This work was supported by Grants from the Canadian Institutes of Health Research, and a Transatlantic Network of Research Excellence grant from the Leducq Foundation.
Conflict of interest
None.
References
- 1.Przyklenk K, Bauer B, Ovize M, Kloner RA, Whittaker P. Regional ischemic ‘preconditioning’ protects remote virgin myocardium from subsequent sustained coronary occlusion. Circulation. 1993;87:893. doi: 10.1161/01.CIR.87.3.893. [DOI] [PubMed] [Google Scholar]
- 2.Kharbanda RK, Mortensen UM, White PA, Kristiansen SB, Schmidt MR, Hoschtitzky JA, Vogel M, Sorensen K, Redington AN, MacAllister R. Transient limb ischemia induces remote ischemic preconditioning in vivo. Circulation. 2002;106:2881–2883. doi: 10.1161/01.CIR.0000043806.51912.9B. [DOI] [PubMed] [Google Scholar]
- 3.Tapuria N, Kumar Y, Habib MM, Abu Amara M, Seifalian AM, Davidson BR. Remote ischemic preconditioning: a novel protective method from ischemia reperfusion injury—a review. J Surg Res. 2008;150:304–330. doi: 10.1016/j.jss.2007.12.747. [DOI] [PubMed] [Google Scholar]
- 4.Cheung MM, Kharbanda RK, Jonstantinov IE, Shimizu M, Frndova H, Li J, Holtby HM, Cox PN, Smallhorn JF, Van Arsdell GS, Redington AN. Randomised controlled trial of the effects of remote ischemic preconditioning on children undergoing cardiac surgery first clinical application in humans. J Am Coll Cardiol. 2006;47:2277–2282. doi: 10.1016/j.jacc.2006.01.066. [DOI] [PubMed] [Google Scholar]
- 5.Shimizu M, Tropak M, Diaz RJ, Suto F, Surendra H, Kuzmin E, Li J, Gross G, Wilson GJ, Callaham J, Redington AN. Transient limb ischemia remotely preconditions through a humoral mechanism acting directly on the myocardium evidence suggesting cross-species protection. Clin Sci. 2009;117:191–200. doi: 10.1042/CS20080523. [DOI] [PubMed] [Google Scholar]
- 6.Steensrud T, Li J, Dai X, Manlhiot C, Kharbanda RK, Tropak M, Redington A. Pretreatment with nitric oxide donor SNAP or nerve transection blocks humoral preconditioning by remote limb ischemia or intra-arterial adenosine. Am J Physiol Heart Circ Physiol. 2010;299(5):298–603. doi: 10.1152/ajpheart.00396.2010. [DOI] [PubMed] [Google Scholar]
- 7.Redington KL, Disenhouse T, Strantzas SC, Gladstone R, Wei C, Tropack MB, Dai X, Manlhiot C, Li J, Redington AN. Remote cardioprotection by direct peripheral nerve stimulation and topical capsaicin is mediated by circulating humoral factors. Basic Res Cardiol. 2012;107(2):241. doi: 10.1007/s00395-011-0241-5. [DOI] [PubMed] [Google Scholar]
- 8.Gao J, Fu W, Jin Z, Yu X. A preliminary study on the cardioprotection of acupuncture pretreatment in rats with ischemia and reperfusion: involvement of cardiac beta-adrenoceptors. J Physiol Sci. 2006;56(4):275–279. doi: 10.2170/physiolsci.RP006606. [DOI] [PubMed] [Google Scholar]
- 9.Gao J, Fu W, Jin Z, Yu X. Acupuncture pretreatment protects heart from injury in rats with myocardial ischemia and reperfusion via inhibition of the beta(1)-adrenoceptor signaling pathway. Life Sci. 2007;80(16):1484–1489. doi: 10.1016/j.lfs.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 10.Zhang H, Liu L, Huang G, Zhou L, Wu W, Zhang T, Huang H. Protective effect of electroacupuncture at the Neiguan point in a rabbit model of myocardial ischemia–reperfusion injury. Can J Cardiol. 2009;25(6):35–363. doi: 10.1016/S0828-282X(09)70095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou W, Ko Y, Benharash P, Yamakawa K, Patel S, Ajijola OA, Mahajan A. Cardioprotection of electroacupuncture against myocardial ischemia–reperfusion injury by modulation of cardiac norepinephrine release. Am J Physiol Heart Circ Physiol. 2012;302(9):H1818–H1825. doi: 10.1152/ajpheart.00030.2012. [DOI] [PubMed] [Google Scholar]
- 12.Dow J, Painovich J, Hale SL, Tjen-A-Looi S, Longhurst JC, Kloner RA. Absence of actions of commonly used Chinese herbal medicines and electroacupuncture on myocardial infarct size. J Cardiovasc Pharmacol Ther. 2012;17(4):403–411. doi: 10.1177/1074248412443310. [DOI] [PubMed] [Google Scholar]
- 13.Tsou MT, Huang CH, Chiu JH. Electroacupuncture on PC6 (Neiguan) attenuates ischemia/reperfusion injury in rat hearts. Am J Chin Med. 2004;32(6):951–965. doi: 10.1142/S0192415X04002557. [DOI] [PubMed] [Google Scholar]
- 14.Hanouz JL, Zhu L, Persehaye E, Massetti M, Babatasi G, Khayat A, Ducouret P, Plaud B, Gérard JL. Ketamine preconditions isolated human right atrial myocardium: roles of adenosine triphosphate-sensitive potassium channels and adrenoceptors. Anesthesiology. 2005;102(6):1190–1196. doi: 10.1097/00000542-200506000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Han J, Kim N, Joo H, Kim E. Ketamine abolishes ischemic preconditioning through inhibition of K(ATP) channels in rabbit hearts. Am J Physiol Heart Circ Physiol. 2002;283(1):H13–H21. doi: 10.1152/ajpheart.01064.2001. [DOI] [PubMed] [Google Scholar]
- 16.Hausenloy DJ, Mwamure PK, Venugopal V, Harris J, Barnard M, Grundy E, Ashley E, Vichare S, Di Salvo C, Kolvekar S, Hayward M, Keogh B, MacAllister RJ, Yellon DM. Effect of remote ischemic preconditioning on myocardial injury in patients undergoing coronary artery bypass graft surgery: a randomised controlled trial. Lancet. 2007;370(9587):575–579. doi: 10.1016/S0140-6736(07)61296-3. [DOI] [PubMed] [Google Scholar]


