Abstract
Background
Symptomatic COVID-19 and Long COVID, also referred to as post-acute sequelae of SARS-CoV-2 (PASC) or post-COVID conditions, have been widely reported in young, healthy people, but their prevalence has not yet been determined in student athletes. We sought to estimate the prevalence of reported COVID-19, symptomatic COVID-19, and Long COVID in college athletes in the United States attending 18 schools from spring 2020 to fall 2021.
Methods
We developed an online survey to measure the prevalence of student athletes who tested positive for COVID-19, developed Long COVID, and did not return to their sport during the relevant time period. We surveyed a convenience sample of 18 collegiate school administrators, representing about 7,000 student athletes. Of those schools surveyed, 16 responded regarding the spring 2020 semester, and 18 responded regarding the full academic year of fall 2020 to spring 2021 (both semesters).
Results
According to the survey responses, there were 9.8% of student athletes who tested positive for COVID-19 in spring 2020 and 25.4% who tested positive in the academic year of fall 2020 to spring 2021. About 4% of student athletes who tested positive from spring 2020 to spring 2021 developed Long COVID, defined as new, recurring, or ongoing physical or mental health consequences occurring 4 or more weeks after SARS-CoV-2 infection.
Conclusions
This study highlights that Long COVID occurs among young, healthy athletes and is a real consequence of COVID-19. Understanding the prevalence of Long COVID in this population requires longer follow-up and further study.
Keywords: Long COVID, College, Athletes, Young, Healthy, SARS-CoV-2, COVID-19, Sports
Background
The longer-term effects of SARS-CoV-2, the virus that causes COVID-19, are only beginning to be explored and understood, but evidence suggests the effects could be substantial. Long COVID, also referred to as post-acute sequelae of SARS-CoV-2 (PASC), or post-COVID conditions, is defined as new, recurring, or ongoing physical or mental health consequences occurring 4 or more weeks after SARS-CoV-2 infection [1]. Prevalence of Long COVID based on self-report of symptoms estimates range from 2 to 16% [2–5]. Long COVID affects all ages and has been reported among persons with severe or mild symptoms from COVID-19 [6]. There are fewer estimates of Long COVID among young, healthy adults, but estimates of prevalence of symptomatic infection and Long COVID among the young adult population are lower than in the general population [7–9]. Student athletes are a unique group of young, physically active people who can provide insight on the impact of SARS-CoV-2 infection and occurrence of Long COVID. Throughout the pandemic, college athletic departments monitored their athletes closely for both COVID-19 and Long COVID, including whether or not athletes were able to return to their sport [10]. Recent data have examined the effect of Long COVID on athletes, particularly regarding cardiac outcomes, and some studies have found that Long COVID cardiac symptoms among athletes can resemble orthostatic intolerance in athletes and low cardiorespiratory fitness [11, 12]. However, previous studies have not yet determined the prevalence of symptomatic infection and Long COVID in general among young athletes.
This report estimates the prevalence of reported COVID-19, symptomatic COVID-19, and Long COVID in college athletes in the United States attending 18 schools from the spring 2020 academic semester through the fall 2021 academic semester.
Methods
We recruited a convenience sample of 18 schools. We shared an online survey with healthcare administrators at all 1,121 schools in the National Collegiate Athletic Association (NCAA), National Junior College Athletic Association (NJCA), and National Association of Intercollegiate Athletics (NAIA). Of 1,121, healthcare administrators contacted via email, 18 responded to the initial survey. The initial survey pertained to the 2020 spring semester and to the entire academic year (both semesters) of fall 2020 to spring 2021 (2020–2021). Two of the 18 schools shared results for the 2020–2021 academic year only, due to students not participating in sports in the spring 2020 semester. Four of the original 18 schools responded to an additional follow-up survey regarding the fall 2021 semester.
We developed an online survey to measure the prevalence of student athletes who tested positive for COVID-19, developed Long COVID, and did not return to their sport during the period. The three leagues, which include 1,121 member schools combined, shared contact information for member schools’ healthcare administrators with the research team. The research team distributed an online consent form and survey to healthcare administrators on October 12, 2021.
The survey collected the number of student athletes, COVID-19 cases, cases with Long COVID, and students who had to stop participating in sport for the duration of the relevant time period (spring 2020, 2020–2021, or fall 2021). The survey asked participants to report only cases with a positive COVID-19 test result. We defined Long COVID in accordance with the Centers for Disease Control and Prevention (CDC), which defines Long COVID as new, recurring, or ongoing physical or mental health symptoms that continue for longer than 4 weeks after infection [1]. We defined infection after vaccination, in accordance with the CDC, as a case of COVID-19 that occurs after someone has been fully vaccinated (14 days after receipt of a second dose of a mRNA vaccine or receipt of 1 dose of a single-dose vector vaccine) [13].
A follow-up survey was sent to the initial respondents on January 18, 2022, to solicit data from the fall 2021 semester (August 1 to December 30, 2021). Responses were reported in aggregate for each school and no individual student information was provided. This study received exemption from the Yale University Institutional Review Board. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.1
Outcomes were reported by school semester or academic year, including spring 2020 semester, 2020–2021 academic year, and fall 2021 semester.
Results
The median number of student athletes per school was 442.5 [95% confidence interval (347.7, 537.3)] in spring 2020 and 454.5 (374.2, 534.8) in 2020–2021. Four of the 18 school administrators shared the number of total student athletes by gender. At these four schools during spring 2020, 55.1% were male, 44.9% were female, and 0% were other gender (Table 1). During 2020–2021, 52.4% were male, 47.6% were female, and 0% were other gender. During fall 2021, 50.8% were male, 49.2% were female, and 0% were other gender. All schools that responded to both surveys were members of the NCAA league. All three NCAA Divisions were represented in the study during spring 2020 and 2020–2021 and, across all time periods, most schools competed in Division I.
Table 1.
Description and characteristics of participating colleges
| 2020 Spring Semester | 2020–2021 Academic Year (Fall 2020 to Spring 2021) | 2021 Fall Semester | |
|---|---|---|---|
| Overall number of participating schools (N = 1,121) | 16 | 18 | 4 |
| Overall number of eligible student athletes in sample | 6,923 | 7,651 | 1,776 |
| Schools by Division | |||
| Division I | 12 | 13 | 3 |
| Division II | 1 | 1 | 0 |
| Division III | 3 | 4 | 1 |
| Schools by Region | |||
| Northeast | 4 | 5 | 0 |
| Southeast | 6 | 7 | 3 |
| Midwest | 1 | 1 | 0 |
| Southwest | 4 | 4 | 1 |
| Northwest | 1 | 1 | 0 |
| Schools by Size of Student Athlete Population | |||
| Median number of students | 442.5 (95% CI 347.7, 537.3) | 454.5 (95% CI 374.2, 534.8) | NA |
| Number of students in 1st quartile (smallest programs) | 678 | 1,000 | NA |
| Number of students in 2nd quartile | 1,571 | 1,598 | NA |
| Number of students in 3rd quartile | 1,998 | 1,957 | NA |
| Number of students in 4th quartile (largest programs) | 2,676 | 3,096 | NA |
| Gender of students (from schools that reported gender among total students) | |||
| Total number of schools that reported gender | 4 | 4 | 4 |
| Total number of students with gender reported | 2,060 | 2,145 | 1,776 |
| Male | 1,135 (55.1%) | 1,124 (52.4%) | 902 (50.8%) |
| Female | 925 (44.9%) | 1,021 (47.6%) | 874 (49.2%) |
| Other | 0 | 0 | 0 |
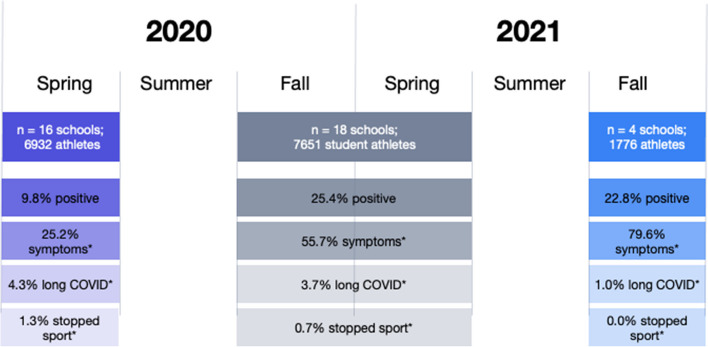
The survey reports represented 6,923 total student athletes in spring 2020 and 7,651 student athletes in 2020–2021. The number of student athletes who tested positive for COVID-19 was 678 (9.8%) in spring 2020 and 1,943 (25.4%) in 2020–2021 (Fig. 1). Of the student athletes who tested positive, the number of those who were symptomatic was 171 (25.2%) in spring 2020 and 1,082 (55.7%) in 2020–2021. Of the student athletes who tested positive, the number of those who had Long COVID was 29 (4.3%) in spring 2020 and 71 (3.7%) in 2020–2021. Finally, of the student athletes who tested positive, 9 (1.3%) stopped participating in their sport (training or competition) for the rest of the spring 2020 semester and 14 (0.7%) stopped participating in their sport for the rest of the 2020–2021 academic year.
Fig. 1.
Key findings on the prevalence rate of Long COVID** among COVID-positive student athletes in the NCAA. *Rate among those student athletes who tested positive. **Long COVID is defined as new, recurring, or on-going physical or mental health consequences occurring 4 or more weeks after SARS-CoV-2 infection
Four schools that had participated in the initial survey also participated in a follow-up survey regarding the fall 2021 semester and representing 1,776 student athletes. For these schools that reported cases from fall 2021, we also compared the percent testing positive, symptomatic, and with Long COVID to rates during the earlier time periods at only these 4 schools. Of the student athletes at these 4 schools, 103 (6.2%) tested positive for COVID-19 in spring 2020, 480 (27.9%) tested positive during 2020–2021, and 406 (22.8%) tested positive in fall 2021. Of the student athletes who tested positive at these schools, 45 (43.7%) were symptomatic in spring 2020, 292 (60.8%) were symptomatic in 2020–2021, and 323 (79.6%) were symptomatic in fall 2021; 4 (3.9%) developed Long COVID in spring 2020, 8 (1.7%) developed Long COVID in 2020–2021, and 4 (1.0%) developed Long COVID in fall 2021; 0 (0.0%) stopped participating in their sport for the rest of the semester or year in each time period (spring 2020, 2020–2021, and fall 2021).
During 2020–2021, 106 (5.4%) of the 1,943 student athletes who tested positive for COVID-19 had been fully vaccinated against COVID-19 (infection after vaccination), and there was no report of Long COVID among this group.
Discussion
Our study adds to the understanding of the longer-term effects of COVID-19 in a relatively young, healthy adult population. Our findings indicate that in a young sample population that is especially fit, a significant number of COVID-19 infections can be symptomatic (we found 25.2% to 79.6%, depending on time period) and some people (we found 1.0% to 4.3%, depending on time period) will still experience Long COVID, or symptoms lasting longer than one month. Further study is needed to confirm these estimates of the prevalence of COVID-19, symptomatic COVID-19, and Long COVID among physically active young adults. Given the heterogeneity of Long COVID experiences, determining the prevalence of severe Long COVID among a young, healthy population is necessary to target treatment and to educate young people on the risks of COVID-19 [14].
Previous research of young adult populations has indicated that symptomatic infection and Long COVID are less common among the younger adult population [7–9]. Our results are similar to previous reports. The rate of Long COVID among people ages 18–24 years has been estimated to be 2.2% of people living in private households in the UK, compared with 2.4% of people all ages [9]. Regarding athletes, a previous study indicated that test positivity of student athletes in the NCAA was comparable to test positivity of non-athlete students; however the study did not determine the prevalence of COVID-19 or Long COVID within the population [10]. One study of athletes ages 18–35 years indicated that about half of athletes with COVID-19 were symptomatic 30 days after the initial COVID-19 infection, with 1.2% having moderate or severe symptoms [15]. Previous research on athletes has shown that Long COVID, in particular cardiac symptoms, can occur and that the physiological impact of COVID-19, including on heart rate, lasts 2–3 months on average [16–18].
There are several limitations to this study. First, we have a convenience sample of 18 schools that responded to our survey out of 1,121 and only 4 that also responded regarding the fall 2021 follow-up survey. However, these schools are diverse and represent thousands of students, and the survey included all student athletes from each school, which should reduce bias. Although thousands of students were represented, some students may have left during the school semester and thus would have been counted in the total number of students, but would not have been captured in the study results. However, only two schools reported sending students home or canceling competition during spring 2020, so study results would be biased only by the number of students at the remaining 16 schools who left mid-semester of their own accord. Additionally, Long COVID symptoms are often ill-defined and underreported, especially during our study period, which could have led to an underreporting of those students who had symptoms more than 4 weeks after initial infection. We were unable to confirm that symptoms reported as Long COVID were not due to some other cause, as we asked health administrators at schools for each given time period, “How many student athletes who tested positive for COVID-19 had COVID-19 symptoms for longer than 1 month?” We were also unable to determine the rate of Long COVID among those students who were fully vaccinated and tested positive for COVID-19 due to uneven reporting. Testing and treatment protocols varied between schools and may have affected these comparisons. Finally, characteristics of students, including gender, were not uniformly reported, and were thus excluded from analyses.
Conclusion
Long COVID occurs among young, healthy athletes and is a real consequence of COVID-19. Understanding the prevalence of Long COVID in young, previously healthy populations requires longer follow-up and further study.
Acknowledgements
Not applicable.
Abbreviations
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- PASC
Post-acute sequelae SARS-CoV-2 infection
- COVID-19
Coronavirus disease 2019
- Long COVID
Symptoms that continue for longer than 4 weeks after SARS-CoV-2 infection
- NCAA
National Collegiate Athletic Association
- NJCA
National Junior College Athletic Association
- NAIA
National Association of Intercollegiate Athletics
- CDC
Centers for Disease Control and Prevention
Authors’ contributions
D.M., S.S., B.A., A.L., D.A., E.B., R.S., H.K. contributed to study design. D.M., S.S., B.A., A.L. E.B., R.S., H.K. contributed to manuscript drafting and editing. D.M. conducted analysis.
Funding
This work did not receive any funding. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Availability of data and materials
All datasets are available from the corresponding author upon reasonable request. These datasets will be shared with results by conference only, as school identifiers must be excluded consistent with the consent obtained.
Declarations
Ethics approval and consent to participate
This study received exemption from the Yale University Institutional Review Board. This activity was reviewed by the Centers for Disease Control and Prevention (CDC) and was conducted consistent with applicable federal law and CDC policy.1 Informed consent was obtained via an online consent form that the research team distributed with the study survey to healthcare administrators on October 12, 2021.
Consent for publication
Not applicable.
Competing interests
In the past three years, Harlan Krumholz received expenses and/or personal fees from Element Science, Eyedentify, and F-Prime. He is a co-founder of HugoHealth, Refactor Health, and Ensight-AI. He is the co-editor of Journal Watch: Cardiology of the Massachusetts Medical Society and is a section editor of UpToDate. He is associated with contracts, through Yale New Haven Hospital, from the Centers for Medicare & Medicaid Services and, through Yale University, from Janssen, Johnson & Johnson Consumer, and Pfizer. The other authors report no potential conflicting interests.
Footnotes
See e.g., 45 C.F.R. part 46. 102(I)(2), 21 C.F.R. part 56; 42 U.S.C. § 241 (d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.CDC. Your Health: Post-COVID Conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html. Published 2021. Updated September 16, 2021. Accessed 3 Apr 2022.
- 2.Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 3.Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nature Medicine. 2021;27(4):626–31. [DOI] [PMC free article] [PubMed]
- 4.Huang Y, Pinto MD, Borelli JL, Asgari Mehrabadi M, Abrahim HL, Dutt N, Lambert N, Nurmi EL, Chakraborty R, Rahmani AM, Downs CA. COVID Symptoms, Symptom Clusters, and Predictors for Becoming a Long-Hauler Looking for Clarity in the Haze of the Pandemic. Clin Nurs Res. 2022;31(8):1390–8. 10.1177/10547738221125632. [DOI] [PMC free article] [PubMed]
- 5.Caspersen IH, Magnus P, Trogstad L. Excess risk and clusters of symptoms after COVID-19 in a large Norwegian cohort. Eur J Epidemiol. 2022;37(5):539–48. [DOI] [PMC free article] [PubMed]
- 6.Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taquet M, Dercon Q, Luciano S, Geddes JR, Husain M, Harrison PJ. Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021;18(9):e1003773. doi: 10.1371/journal.pmed.1003773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wanga V, Chevinsky JR, Dimitrov LV, et al. Long-term symptoms among adults tested for SARS-CoV-2 - United States, January 2020-April 2021. MMWR Morb Mortal Wkly Rep. 2021;70(36):1235–1241. doi: 10.15585/mmwr.mm7036a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK. Office for National Statistics UK; 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/latest. Accessed 11 Mar 2022.
- 10.Schultz EA, Kussman A, Jerome A, Abrams GD, Hwang CE. Comparison of SARS-CoV-2 test positivity in NCAA division I student athletes vs nonathletes at 12 institutions. JAMA Netw Open. 2022;5(2):e2147805–e2147805. doi: 10.1001/jamanetworkopen.2021.47805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao P, Peritz DC, Systrom D, Lewine K, Cornwell WK, 3rd, Hsu JJ. Orthostatic and exercise intolerance in recreational and competitive athletes with long COVID. JACC Case Rep. 2022;4(17):1119–1123. doi: 10.1016/j.jaccas.2022.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwendinger F, Knaier R, Radtke T, Schmidt-Trucksäss A. Low cardiorespiratory fitness post-COVID-19: a narrative review. Sports Med. 2023;53(1):51–74. doi: 10.1007/s40279-022-01751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC. The Possibility of COVID-19 after Vaccination: Breakthrough Infections. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/effectiveness/why-measure-effectiveness/breakthrough-cases.html. Published 2021. Updated December 17, 2021. Accessed 3 Apr 2022.
- 14.Groff D, Sun A, Ssentongo AE, et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review. JAMA Netw Open. 2021;4(10):e2128568–e2128568. doi: 10.1001/jamanetworkopen.2021.28568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Casasco M, Iellamo F, Scorcu M, et al. Return to play after SARS-CoV-2 infection in competitive athletes of distinct sport disciplines in Italy: a FMSI (Italian Federation of Sports Medicine) study. J Cardiovasc Dev Dis. 2022;9(2):59. [DOI] [PMC free article] [PubMed]
- 16.Guevarra CC, Murray N, Cipriani D, et al. Cardiovascular involvement among collegiate athletes following COVID-19 infection. J Clin Transl Res. 2022;8(1):1–5. [PMC free article] [PubMed] [Google Scholar]
- 17.Lakatos BK, Tokodi M, Fábián A, et al. Frequent constriction-like echocardiographic findings in elite athletes following mild COVID-19: a propensity score-matched analysis. Front Cardiovasc Med. 2021;8:760651. doi: 10.3389/fcvm.2021.760651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radin JM, Quer G, Ramos E, et al. Assessment of prolonged physiological and behavioral changes associated with COVID-19 infection. JAMA Netw Open. 2021;4(7):e2115959. doi: 10.1001/jamanetworkopen.2021.15959. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All datasets are available from the corresponding author upon reasonable request. These datasets will be shared with results by conference only, as school identifiers must be excluded consistent with the consent obtained.