see also p 239
Summary points
Depression may occur in Asian American children and adolescents and canbe associated with significant morbidity and mortality
Asian American families may experience cultural, linguistic, andeconomic barriers to accessing mental health care for depression
Primary care clinicians who see Asian American children for“routine” or school physical examinations play a crucial role inrecognizing and treating depression
The clinician's role includes screening for warning signs of depressionand suicidal risk, providing supportive initial management and follow-up,educating children and parents about depression, and determining whetherspecialist referral is indicated
Referral to specialists should be considered when symptoms are severe orwhen mild symptoms do not remit after a brief course of supportivemanagement
Danny is an 11-year-old Chinese boy with a long history of behavioralproblems and academic delay. School officials referred him to the emergencydepartment of a local hospital after he ran to a fifth floor window ledge andthreatened to jump, Immediately before this episode occurred, Danny hadresponded to a question from the teacher in his English class by stating,“I don't know, I guess I just must be stupid.”
Danny's parents are separated, and he sees his father only once every fewmonths. When his mother, who speaks only Chinese, arrives in the emergencydepartment, she appears tired and tearful as she struggles to hold Danny's2-year-old sister in one arm while trying to make sure that his 5-year-oldbrother does not wander out of her sight. Because no Chinese-speakinginterpreters are available, Danny acts as the interpreter for his mother. Whenasked what might have happened if he had actually jumped from the window atschool, he replies, “What difference does it make?”
One of the major advances of modern day psychiatry has been the recognitionthat children and adolescents may develop depression and other mood disorderswith constellations of symptoms similar to those found inadults.1,2,3,4Little is available in the literature to guide parents, primary careclinicians, educators, or mental health providers on features that may bespecific to the diagnosis and treatment of mood disorders in Asian Americanyouth.
Available evidence suggests the following:
Asian Americans are less likely than whites to use mental healthservices5
Suicide rates in Asian American adolescents and young adults are higherthan in white youth and youngadults6
The prevalence rate of depressive diagnoses in adolescence is different inAsian Americans from that in whites. This diagnosis is less likely in AsianAmerican boys than in white boys, whereas depression is more prevalent inAsian American girls than in whitegirls7
Asian Americans are vulnerable to posttraumatic stress disorders anddepression associated with adverse experiences in their country oforigin8,9
BARRIERS TO CARE
Problems experienced by Asian Americans in accessing health care,especially mental health services, include cultural and linguistic barriers,stigma associated with psychiatric disorders, availability of appropriatestaff, and lack of adequate insurancecoverage.10 Primarycare clinicians to whom Asian American parents bring their children for“routine” or school-related check-ups may provide the onlyopportunity to identify debilitating depressive symptoms.
The crucial roles of such clinicians include overcoming barriers torecognition of depression (box1), assessing the presence and severity of depressive symptoms andsuicidal risk, determining when referral for psychiatric evaluation isindicated, and collaborating with psychiatrists and other mental healthproviders in effective management strategies.
Box 1.
How to overcome barriers to recognizing depression
|
DEPRESSIVE DISORDERS IN CHILDREN
Depression refers to transitory or persistent disturbances of mood that mayoccur from childhood through old age. Depressive disorders are specificconstellations of emotional, cognitive, and behavioral symptoms that also mayoccur across the age spectrum. Depression may be found in association with avariety of other psychiatric and medicaldisorders.11
A description of these disorders in adults begins on p239.12 Thediagnostic criteria for depressive disorders in children have modificationsthat allow for developmental variations inpresentation,1,2,3,4but not for variations related to ethnicity. These modifications permit thesubstitution of irritability for depressed mood, duration of 1 year instead of2 years for dysthymic disorder, and failure to make expected gains in weightor academic performance rather than decline from previouslevels.4
The estimated prevalence of depressive disorders is 2% in children and 5%inadolescents.1,2,3This rate may be considerably higher in pediatric patients with medical orneurologicillnesses.13,14Depressive disorders are associated with major impairments in social,academic, and emotional functioning that may persist after the resolution ofthe depressiveepisode.15 They arealso associated with an increased risk ofsuicide15,16and self-injurious behaviors that may result in chronic physical disability.Children and adolescents who experience depressive disorders are atsignificantly increased risk forrecurrence.15,17,18
ASSESSMENT AND EVALUATION
In view of the substantial morbidity and potential mortality associatedwith depressive disorders, screening for warning signs suggestive ofdepression (box 2) should beconsidered as part of the general pediatric evaluation of every child from age5 or 6 years. It may readily be incorporated into the history, review ofsystems, and physicalexamination.11
Box 2.
Warning signs of depression
|
Parents and children may differ significantly in their reports of emotionaland behavioral problems. Children tend to provide more reliable informationabout their emotional states than about their behavior. Parents on the otherhand give more reliable information about their children's behavioral ratherthan emotionalproblems.19Therefore, it is important to ask children or adolescents directly about theiremotional state. Such inquiries (box3) should be made with special attention to the age, developmentalstate, and cultural and linguistic background of thechild.19
Box 3.
Questions to ask children to assess their mood
|
Careful and direct inquiry is especially critical for Asian immigrantchildren who may be the only English-speaking member of the family. The roleof children and adolescents as “cultural brokers” for immigrant orless acculturated families is a major factor resulting in psychologicalstress. Asian boys and girls are often asked to interpret the concerns ofadult family members to outside authority figures, such as teachers, doctors,and government officials. This burden confers responsibility for many youthsbefore they are able to navigate their own pressures of “fittingin,” adopting Western values while retaining Asian ones at the urging ofparents, and maintaining high academic or work standards, including workingoutside and inside the home.
In the case example, Danny must provide information about his own problemswhile taking the “responsible” role of navigating his family'sneeds. The stresses involved in this double role may be contributing factorsto his depression. The availability of trained interpreters to assist inseparate interviews with monolingual parents can help to alleviate this burdenon the child and allows parent and child the opportunity to speak more freelyabout their concerns without the other being present.
Children and adolescents who are reported to have made suicidal statements,have engaged in potentially self-injurious behaviors, or exhibit other warningsigns of depression should be asked specifically about suicidal ideation andintent.16
When screening elicits findings suggestive of a depressive disorder, it isimportant to educate pediatric and adolescent patients and their parents aboutthe short- and long-term suffering and impairment in functioning associatedwith such disorders, the risk of suicide and other self-injurious behaviors,and the availability of effective treatment options.
Primary care clinicians should also maintain a high index of suspicion foranxiety disorders and other emotional and behavioral problems, the reportedprevalence of which is high in depressed children andadolescents.20,21Assessment should include inquiries about the family's previous efforts tomanage emotional and behavioral problems in the child or adolescent, includingpossible use of herbal remedies or other nonprescription medications.
REFERRAL TO A MENTAL HEALTH SPECIALIST
The primary care clinician who observes signs and symptoms suggestive ofdepression in a child or adolescent must make two immediate managementdecisions. The first is whether the patient's symptoms and behaviorsconstitute an acutely life-threatening crisis that requires emergencypsychiatric evaluation and possible psychiatric hospitalization(box 4). The second decision iswhether an initial course of supportive medical management is adequate toaddress the patient's depressive symptoms or is referral for timely but notemergent psychiatric evaluation indicated(box 5).
Box 4.
Indications for emergency psychiatric referral
|
Box 5.
Indications for timely (but not emergency) psychiatricreferral
|
Close and ongoing collaboration with the patients' parents or legalguardians is integral to choosing the best course of action. In thiscollaboration, the primary care practitioners should emphasize that the bestoutcomes can only be achieved with the active involvement of parents andsignificant loved ones. Particularly with Asian parents who place a high valueon education, stressing the effect that depression may have on academicachievement encourages parental acceptance of psychiatric referral andtreatment.
MANAGEMENT
Effective management of depression requires a comprehensive approach tounderlying environmental, psychological, and biologic factors; clearformulation of goals (box 6);and knowledge of recommended treatment guidelines for depression in childrenand adolescents.3Supportive management, including relief of minor medical conditions; reductionof environmental stressors; and offering the child and family the opportunityto express their concerns, may be sufficient to alleviate mild and transitorydepressive symptoms. More specific psychological and pharmacologic treatmentsshould be considered for serious and persistent depressive symptoms that areassociated with impairments in social and academic functioning.
Box 6.
Depression in children: management goals
|
Current evidence and clinical experience suggest that many children andadolescents with depressive disorders respond favorably to specific types ofpsychotherapeutic interventions, such as cognitive-behavioral therapy,interpersonal psychotherapy, and antidepressantmedication.3Unfortunately, the knowledge base about the safety and effectiveness ofpharmacologic treatments of depression in children and adolescents is limited.In addition, the potential for interactions between antidepressants and otherprescribed medications and nonprescription remedies must be considered. Givenall of these limitations, together with the absence of systematic data on thetreatment of depression in Asian American children, primary care cliniciansare advised to seek psychiatric consultation for a depressed child oradolescent before selecting a particular form of treatment.
Warning signs of depression include Danny's sadness, irritability, negativeself-image, and suicidal threats and behaviors. Environmental stressorsinclude his problems at school, the fragmentation and economic disadvantage ofhis family, and his mother's possible depressive disorder. Barriers to careinclude the absence of linguistically competent staff to assist ininterviewing his mother and helping her to cope effectively in an unfamiliarsetting.
Emergency psychiatric referral is indicated to assess the following:suicidal risk, severity of depressive symptoms, possibility of other emotionaland psychiatric disorders, need for psychiatric hospitalization, andindications for specific psychological or pharmacologic interventions.Referral for social service evaluation for Danny's mother is indicated. Thisreferral would allow professional assessment of the availability of family,friends, and public resources to help alleviate the stress she is experiencingin caring for her children and the potential benefit of psychiatric orpsychosocial intervention for her own depressive symptoms. Gaining collateralinformation from Danny's school is indicated to determine the need for apsychoeducational evaluation to assess for learning disorders and to develop aplan to help him with his academic difficulties.
Current experience suggests that Danny's depressive symptoms may respondfavorably to available treatments but that Danny is at risk for recurrenceafter remission of the present episode.
Danny's case illustrates common themes that may occur in the presentationof children with depressive symptoms. It also illustrates cultural andlinguistic barriers that may affect the evaluation and treatment of childrenfrom Asian American and other non-English-speaking backgrounds. As for otherconditions that may remit and relapse in childhood, adolescence, and intoadulthood, the role of the primary care clinician encompasses not only initialrecognition and specialist referral but also periodic monitoring to provideearly identification and intervention in case of recurrence. This role takeson special importance in the care of children from Asian American families.These families may be wary of psychiatrists and other mental healthprofessionals but are more accepting of the need for occasional medical visitsfor somatic complaints or annual physical examinations required byschools.
Box 7.
Suggestions for further reading
|
Figure 1.
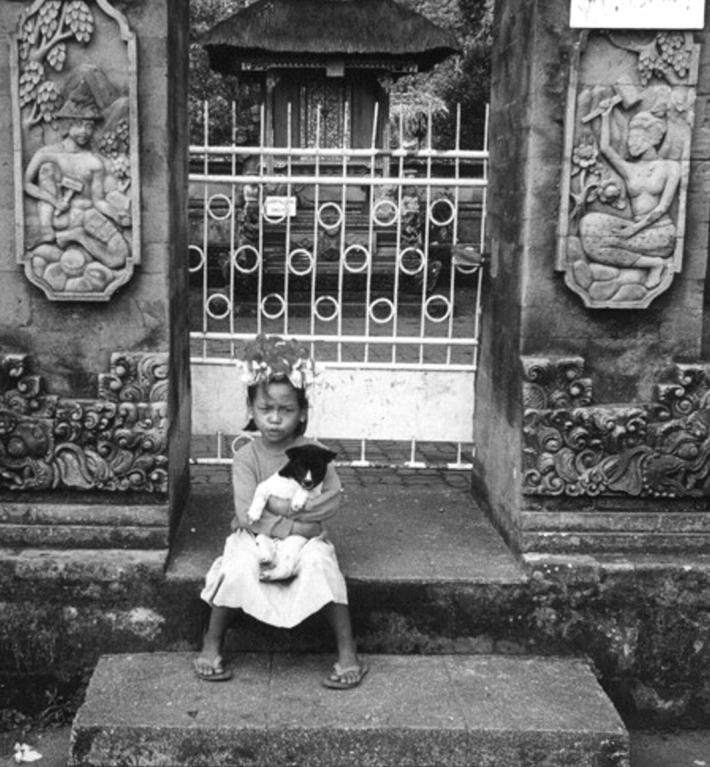
Matt Bridger/DHD Photo Gallery
Asking children about their mood must account for their cultural andlinguistic background
Competing interests: H Chung is Medical Director, Depression andAnxiety Management Team, Pfizer, Inc.
References
- 1.Weller EB, Weller RA. Mood disorders in prepubertal children. In:Wiener JM, ed. Textbook of Child and AdolescentPsychiatry. 2nd ed. Washington, DC: American Psychiatric Press;1997: 333-342.
- 2.Kashani JA, McNaul JP. Mood disorders in adolescents. In: WienerJM, ed. Textbook of Child and Adolescent Psychiatry.2nd ed. Washington, DC: American Psychiatric Press; 1997:343-385.
- 3.Birmaher B, Brent D, Benson RS. Summary of practice parameters forthe assessment and treatment of children and adolescents with depressivedisorders. J Am Acad Child Adolesc Psychiatry 1998;37:1234-1238 [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic andStatistical Manual of Mental Disorders, 4th ed. Washington, DC:American Psychiatric Association; 1994.
- 5.Durvasula R, Sue S. Severity of disturbance among Asian Americanoutpatients. Cult Divers Ment Health 1996;2:43-51. [PubMed] [Google Scholar]
- 6.Lorenzo MK, Pakiz B, Reinherz HZ, et al. Emotional and behavioralproblems of Asian American adolescents: a comparative study. ChildAdolesc Soc Work J 1995;12:197-212. [Google Scholar]
- 7.Kim LS, Chun CA. Ethnic differences in psychiatric diagnoses amongAsian American adolescents. J Nerv Ment Dis 1993;181:612-617. [DOI] [PubMed] [Google Scholar]
- 8.Sack WH, Clarke GN, Seeley J. Multiple forms of stress in Cambodianrefugees. Child Dev 1996;67:107-116. [PubMed] [Google Scholar]
- 9.Sack WH, Clarke G, Him C, et al. A 6-year follow-up study ofCambodian refugee adolescents traumatized as children. J Am AcadChild Adolesc Psychiatry [DOI] [PubMed]
- 10.The Coalition for Asian American Children and Families. Half-fullor half-empty? Health care, child care, and youth programs forAsian American children in New York City. April1999.
- 11.Tompson MC, McNeil FM, Rea MM, Asarnow JR. Identifying and treatingadolescent depression. West J Med 2000;172:172-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen JP, Chen H, Chung H. Depressive disorders in Asian Americanadults. West J Med 2002;176:239-244. [PMC free article] [PubMed] [Google Scholar]
- 13.Son SE, Kirchner JT. Depression in children and adolescents.Am Fam Physician 2000;62:2297-2308, 2311-2312. [PubMed] [Google Scholar]
- 14.Angold A. Childhood and adolescent depression. II: Research inclinical populations. Br J Psychiatry 1988;153:476-492. [DOI] [PubMed] [Google Scholar]
- 15.Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescentsgrown up. JAMA 1999;281:1707-1713. [DOI] [PubMed] [Google Scholar]
- 16.Practice parameter for the assessment and treatment of children andadolescents with suicidal behavior. J Am Acad Child AdolescPsychiatry 2001;40:495-499. [DOI] [PubMed] [Google Scholar]
- 17.Kovacs M, Feinberg TL, Crouse-Novak MA, Paulauskas SL, FinkelsteinR. Depressive disorders in childhood. I: A longitudinal prospective study ofcharacteristics and recovery. Arch Gen Psychiatry 1984;41:229-237. [DOI] [PubMed] [Google Scholar]
- 18.Lewinsohn PM, Rohde P, Klein DN, Seeley JR. Natural course ofadolescent major depressive disorder. I: Continuity into young adulthood.J Am Acad Child Adolesc Psychiatry 1999:38:56-63. [DOI] [PubMed] [Google Scholar]
- 19.King RA. Practice parameters for the psychiatric assessment ofchildren and adolescents. American Academy of Child and Adolescent Psychiatry.J Am Acad Child Adolesc Psychiatry 1997;36(10 Suppl):S4-S20. [DOI] [PubMed] [Google Scholar]
- 20.Kovacs M, Gatsonis C, Paulauskas SL, Richards C. Depressivedisorders in childhood. IV: A longitudinal study of comorbidity with and riskfor anxiety disorders. Arch Gen Psychiatry 1989;46:776-782. [DOI] [PubMed] [Google Scholar]
- 21.Angold A, Costello EJ. Depressive comorbity in children andadolescents: empirical, theoretical, and methodological issues. AmJ Psychiatry 1993;150:1779-1791. [DOI] [PubMed] [Google Scholar]


