Abstract
We investigated the effects of menstrual cycle phase on thermal sensation, thermal pleasantness, and autonomic thermoregulatory responses during mild cold exposure. Eight healthy young women participated. Experiments were conducted in the follicular and luteal phases: 120 min exposure at 23.5 °C after 40-min at a baseline temperature of 29 °C. Body core temperature was higher (P = 0.01) in the luteal phase than in the follicular phase. Thermal sensation of the whole body (P = 0.59), hands (P = 0.46), and toes (P = 0.94), and thermal pleasantness of the whole body (P = 0.79) were no different between phases. In both phases, mean skin temperature decreased (P = 0.00) in the same manner without any change in metabolic rate (P = 0.90). These results suggest the change of body core temperature in the menstrual cycle phases has no effect on thermal perception of cold or on autonomic cold-defense response.
Keywords: Thermal sensation, Thermal pleasantness, Thermoregulation, Cold exposure, Estradiol, Progesterone
Introduction
Fluctuations of body temperature linked with the phases of the menstrual cycle are observed for women of reproductive age. Body temperature is higher in the luteal phase (L phase) than in the follicular phase (F phase) [1–8]. Thus, higher levels of plasma reproductive hormones, for example estradiol and progesterone, may be involved in the increase of body temperature, although the mechanism remains unclear. The purpose of this study was to determine whether the change of body temperature affects thermal perception and autonomic thermoregulation during the menstrual phases.
Homeothermic animals have both cold and heat-defense effectors, and body temperature is usually maintained at a level where each effector works a little (i.e., at a balance point, formally called a set point) [9]. When body temperature exceeds or falls below the balance point, heat and cold-defense effectors are activated. Thus, there are two possible mechanisms of the increase of body temperature in the L phase:
the balance point shifts to a higher body core temperature; and
the balance point remains unchanged, but body temperature increases.
Previous studies have shown that the threshold body temperature for initiation of shivering, sweating, and skin vasodilation is higher in the L phase than in the F phase [1, 5]. These results suggest that the increase of body temperature in the L phase results from an upward shift of the balance point. Therefore, the same change of body temperature from the balance point may induce similar autonomic responses in both phases.
Thermal perception can be divided into two categories: thermal sensation and pleasantness [10]. Thermal sensation is information about the thermal condition of external objects or the environment, and thermal pleasantness is an emotional experience. Thermal pleasantness is affected by body temperature [11]. For example, when body temperature becomes higher, the unpleasant nature of cold is attenuated or diminished. Cunningham and Cabanac [12] compared thermal pleasantness of the hand for women in the F and L phases. The hand temperature at which the women felt pleasant was higher in the L phase than in the F phase. Kim and Tokura [13] assessed cold-unpleasantness of the whole body by estimating the dressing behavior of women in the cold, which was augmented in the L phase. However, because dressing per se modulates thermal perception, we could not quantitatively estimate whether whole-body thermal perception changes during the menstrual cycle. Moreover, it remains unclear whether the change in body temperature during the phases of the menstrual cycle affects thermal perception.
In this study, women were exposed to a gradually cooled environment, in which gradual changes in autonomic cold-defense responses and thermal perception were observed without change in body core temperature [14]. We hypothesized that autonomic cold-defense responses and thermal perception of cold are similar in the L and F phases. We also hypothesized that the difference between body temperature in the two phases would be maintained during cold exposure.
Methods
Subjects
Female subjects (n = 8; age, 22.0 ± 1.4 years; body weight, 53.9 ± 2.9 kg; and height, 159.1 ± 3.9 cm (mean ± SD)) participated in this study. They were healthy, on the basis of a medical check, were all non-smokers, had a regular menstrual cycle, and took no oral contraception. In addition, to minimize the effect of climatic change on thermal perception and thermoregulation (for example acclimation) during the experiment, subjects who spent most of the day in a room were selected. For over 2 months they were asked to measure sublingual temperature every morning in bed (basal body temperature) by use of a digital thermometer (MC-100L; Omron, Kyoto, Japan). The measurement was to verify regular fluctuation of their basal body temperature with an amplitude of >0.5 °C, and to predict upcoming phases. Each subject gave informed consent to the experimental protocol, which was approved by the Human Research Ethics Committee of the Faculty of Human Sciences of Waseda University. The experiments were conducted in accordance with the Declaration of Helsinki.
Experimental procedure
Experiments were conducted from July to December of the same year. The experiments were repeated twice on separate days: once during the L phase and once during the F phase. The order of the two trials was balanced among all subjects. Each subject finished the two trials within 3 months. The experiment in the L phase was conducted 4–10 days after elevation of the basal body temperature; in the F phase experiments were conducted 6–11 days after the onset of menstrual flow. Subjects finished dinner before 2000 h on the day before the experiment. They arrived at the laboratory at 0900 h on the day of the experiment, and were asked to eat a provided breakfast and to drink 500 mL water. Dressed in a T-shirt and shorts, they entered a climatic chamber maintained at an ambient temperature (T a) of 29 °C with a relative humidity of 30 %. Subjects rested in a sitting position for 1.5 h, while all measuring devices were applied. They rested for another 40 min to enable baseline data to be obtained, and T a was then reduced to 23.5 °C within 40 min and kept at this level for 80 min (Fig. 1a). The starting point at which T a was reduced was defined as time 0. The cooling procedure induced gradual changes of autonomic cold-defense responses and thermal perception in the young women [14]. No changes in body core temperature or shivering were reported.
Fig. 1.
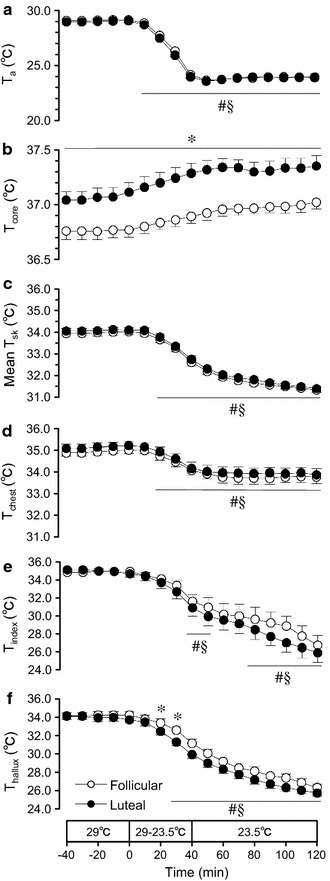
Ambient temperature (T a, a), body core temperature (T core, b), mean skin temperature (mean T sk, c), and skin temperatures of the chest (T chest, d), index finger (T index, e), and hallux (T hallux, f) in the follicular and luteal phases. Values are mean ± SE (n = 8). *P < 0.05, significant differences between the follicular and luteal phases; #P < 0.05, significant differences from the baseline value at 0 min in the follicular phase; §P < 0.05, significant differences from the baseline value at 0 min in the luteal phase
Measurements
T a was continuously monitored with a copper–constantan thermocouple. Subjects were asked to swallow a transmitter pill (length 2 cm, diameter 1.2 cm; CorTemp®2000; HQ, Palmetto, FL, USA) for measurement of body temperature. We started measurement 90 min later when the pill had reached the intestinal cavity (in accordance with the manufacturer's recommendation).The intestinal temperature was used as an index of body core temperature (T core).Data were collected at 20-s intervals by use of a receiver attached to the subject’s waist. Skin surface temperature (T sk) was measured with copper–constantan thermocouples, at 10-s intervals, at seven sites: forehead (T sk1), chest (T sk2), forearm (T sk3), hand (T sk4), thigh (T sk5), lower leg (T sk6), and foot (T sk7). Calculation of mean skin temperature (mean T sk) as 0.07T sk1 + 0.35T sk2 + 0.14T sk3 + 0.05T sk4 + 0.19T sk5 + 0.13T sk6 + 0.07T sk7 was based on the formula of Hardy and DuBois [15]. Temperature at the tip of the left index finger (T index) and hallux (T hallux) were also measured.
Heart rates (HR) were obtained from continuous electrocardiogram measurements (Life Scope BSM-2401; Nihon Kohden, Tokyo, Japan). Blood pressure was measured at the level of the left humeral artery by sonometric pickup every 10 min (STBP-780; Colin, Komaki, Japan), and mean arterial pressure (MAP) was calculated as (systolic pressure − diastolic pressure)/3 + diastolic pressure.
Cutaneous blood flow at the tip of the right index finger and chest were determined by laser Doppler flowmetry (LDFindex and LDFchest, respectively; ALF 21; Advance, Tokyo, Japan) at 1-s intervals and averaged every 10 min. Cutaneous vascular conductance on the index finger (CVCindex) and on the chest (CVCchest) was calculated as LDF/MAP. Changes in LDF and CVC were expressed as percentage changes from the average values at −10 to 0 min (defined as 100 %).
Metabolic rate was determined by indirect calorimetry (ML206 Gas Analyzer; AD Instrument, Bella Vista, Australia). A facial mask (Hans Rudolph, Shawnee, OK, USA) was attached to subjects. Expired gas was collected, and O2 and CO2 concentrations and flow rate of expired gas were analyzed at 20-s intervals. Metabolic rate was calculated from values for non-protein respiration quotient and oxygen consumption rate, and expressed as kilojoules (kJ) per body surface area (m2) per hour.
Thermal sensation and pleasantness of the whole body were assessed every 10 min. We instructed subjects to carefully separate thermal sensation from thermal pleasantness. Thermal sensation of the hands and toes were also assessed every 10 min. Subjects were asked to show their sensation by marking on a 15-cm line rating scale which was labeled “neutral” 2.5 cm from the right end and “cold” or “unpleasant” 2.5 cm from the left end [16]. Before each experiment, they were instructed in the procedure, and that the meanings of the points “cold” and “unpleasant” were “maximum cold” and “maximum unpleasant”, respectively. We expressed thermal perception by measuring the length from the neutral point to the marked point.
A 20-mL blood sample was taken from the antecubital vein at the 40th min in the baseline period. Serum samples were stored at −80 °C until assay. Levels of estradiol, progesterone, testosterone, thyroid-stimulating hormone (TSH), free triiodothyronine (FT3), and free thyroxine (FT4) were measured by a clinical laboratory testing service (BML, Tokyo, Japan). All measurements were conducted by chemiluminescence immunoassay.
Statistical analysis
Differences between mean values of T a, T core, mean T sk, T chest, T index, T hallux, HR, MAP, LDFindex, % LDFindex, LDFchest, % LDFchest, % CVCindex, %CVCchest, metabolic rate, and ratings of thermal perception were analyzed by two-way analysis of variance with repeated measures (phase and time as main effects). Post-hoc testing was conducted by use of the Bonferroni method. Differences between plasma levels of the hormones and integrated values of the metabolic rate in the F and L phases were assessed by use of paired t tests. Correlations between skin temperature and thermal perception in each phase for individual subjects were estimated by use of Pearson’s correlation coefficients. Linear regression analysis was conducted by the least-squares method. Regression slopes and intercepts were averaged, and differences between slopes and intercepts of the regression lines in the L and F phases were assessed by use of the paired t test. All values except ratings, MAP, and hormone levels were averaged every 10 min. Data are presented as means with standard errors (SE) except for those indicated as standard deviation (SD). A null hypothesis was rejected at the level of P < 0.05.
Results
Serum levels of estradiol and progesterone were more than 4 and 25 times greater, respectively, in the L phase than in the F phase (P = 0.01 and 0.04, respectively; Table 1). Levels of testosterone (P = 0.18), thyroid stimulating hormone (TSH, P = 0.59), free triiodothyronine (FT3, P = 0.80), and free thyroxine (FT4, P = 0.32) were no different in the two phases (Table 1).
Table 1.
Serum estradiol, progesterone, testosterone, TSH, FT3, and FT4 at baseline
| Follicular phase | Luteal phase | |
|---|---|---|
| Estradiol (pg/ml) | 32.4 ± 6.8 | 130.4 ± 32.8* |
| Progesterone (ng/ml) | 0.2 ± 0.02 | 5.1 ± 2.00* |
| Testosterone (ng/dl) | 51.1 ± 6.1 | 57.2 ± 7.2 |
| TSH (μIU/ml) | 1.1 ± 0.1 | 1.2 ± 0.1 |
| FT3 (pg/ml) | 3.0 ± 0.1 | 3.0 ± 0.1 |
| FT4 (ng/dl) | 1.3 ± 0.1 | 1.3 ± 0.1 |
Values are mean ± SE (n = 8)
TSH thyroid stimulating hormone, FT 3 free triiodothyronine, FT 4 free thyroxine
* P < 0.05, vs. follicular phase
T core was higher (P = 0.01) in the L phase than in the F phase throughout the experiments (Fig. 1b). Although a significant main effect of time was observed (P = 0.00), there were no significant changes in T core from the value at 0 min in both phases. Mean T sk and skin temperature of the chest (T chest) decreased (P = 0.00) by 20–120 min from the value at 0 min; however, there were no differences between the values for the two phases (P = 0.25 and 0.23, respectively; Fig. 1c, d). T index decreased (P = 0.00) by 40–50 and 80–120 min from the value at 0 min without significant difference between the values for the two phases (P = 0.42, Fig. 1e). T hallux decreased (P = 0.00) by 30–120 min from the value at 0 min, and was lower in the L phase than in the F phase at 20–30 min (P = 0.02, Fig. 1f).
HR was higher (P = 0.00) in the L phase than in the F phase throughout the experiments (Fig. 2a). Although a significant main effect of time was observed (P = 0.00), HR remained unchanged from the value at 0 min during cold exposure in both phases. MAP increased (P = 0.00) by 70–120 min from the value at 0 min; however, there were no differences between the values for the two phases (P = 0.59, Fig. 2b).
Fig. 2.
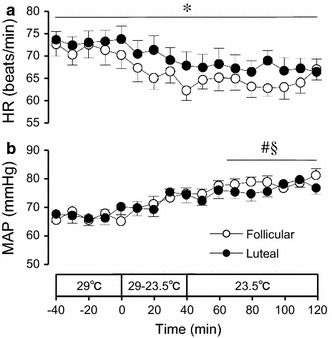
Heart rates (HR, a) and mean arterial pressure (MAP, b) in the follicular and luteal phases. Values are mean ± SE (n = 8). *P < 0.05, significant differences between the follicular and luteal phases; #P < 0.05, significant differences from the baseline value at 0 min in the follicular phase; §P < 0.05, significant differences from the baseline value at 0 min in the luteal phase
It is not appropriate to use absolute values of LDF collected on different days, because the values are affected by adhesive force and the position of the probe. However, to represent percentage changes in LDF, the absolute values of LDF are shown (Fig. 3a, d). LDFindex, % LDFindex, and % CVCindex decreased (P = 0.00) during exposure at 23.5 °C compared with the value at 0 min in both phases (Fig. 3a, b, and c, respectively). Although the values of LDFindex, % LDFindex, and % CVCindex during exposure at 23.5 °C seems to be different in the L and F phases, the differences were not statistically significant (P = 0.27, 0.08, and 0.51, respectively). LDFchest was higher (P = 0.00) in the L phase than in the F phase throughout the experiments. Although a significant main effect for time was observed (P = 0.00), no significant change from the 0-min value was found for either phase (Fig. 3d). Percentage LDFchest and CVCchest decreased (P = 0.00) by 60–120 min from the value at 0 min without any differences between the two phases (P = 0.71 and P = 0.21, respectively, Fig. 3e, f).
Fig. 3.
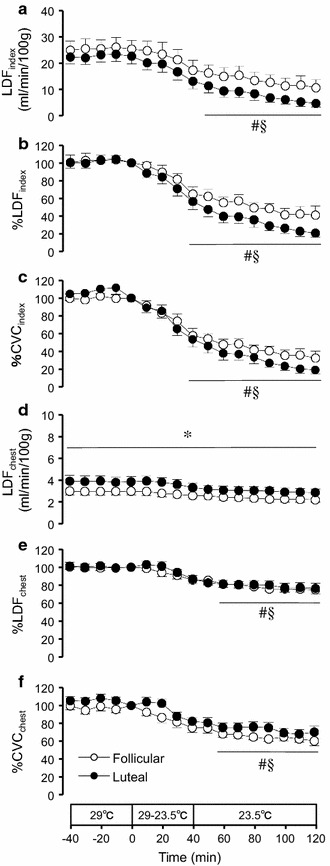
Laser Doppler flow (LDF) for the index finger (LDFindex, a), percentage change in the LDF for the index finger (%LDFindex, b), percentage change in cutaneous vascular conductance (CVC) for the index finger (%CVCindex, c), LDF for the chest (LDFchest, d), percentage change in LDF for the chest (%LDFchest, e), and percentage change in CVC for the chest (%CVCchest, f) in the follicular and luteal phases. One-hundred percent for LDF and CVC denote average values during the last 10 min of the baseline period. Values are mean ± SE (n = 8). *Significant difference between the follicular and luteal phases, P < 0.05. #P < 0.05, significant differences from the baseline value at 0 min in the follicular phase; §P < 0.05, significant differences from the baseline value at 0 min in the luteal phase
Although the metabolic rate during exposure at 23.5 °C tended to be higher in the L phase than in the F phase, no statistically significant difference was observed (P = 0.23, Fig. 4). In addition, the integrated value (i.e., metabolic rate × hour) during cold exposure periods (40–120 min) was not different (325.6 ± 27.7 and 358.2 ± 19.8 kJ/m2 in the F and L phases, respectively, P = 0.32). No increase during cold exposure was found in either phase (P = 0.09).
Fig. 4.
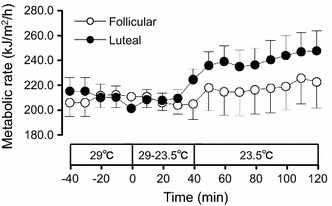
Metabolic rate estimated by indirect calorimetry in the follicular and luteal phases. Values are mean ± SE (n = 8)
Rating scores for thermal sensation and pleasantness for the whole body and thermal sensation for the hands and toes are shown in Fig. 5a, b. The ratings for “cold” and “unpleasant” are expressed as negative values. Thermal sensation for the whole body was reduced (P = 0.00) by 40–120 min from the value at 0 min in the F and L phases; however, there were no differences between the phases (P = 0.59, Fig. 5a). Thermal pleasantness for the whole body also decreased (P = 0.00) in the cold at 90–120 min in the two phases, and no differences between the F and L phases were found (P = 0.79, Fig. 5b). Although a significant (P = 0.00) main effect of time was observed for thermal sensation of the hand and toes, there were no statistically significant changes from the 0-min values, and no differences between the phases were found (P = 0.46 and 0.94, respectively, Fig. 5c, d).
Fig. 5.
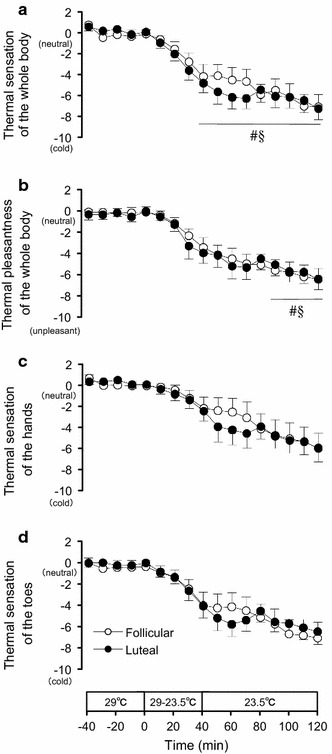
Thermal sensation (a, n = 8) and pleasantness (b, n = 8) for the whole body, and thermal sensation for the hands (c, n = 7) and toes (d, n = 7) in the follicular and luteal phases. Values are mean ± SE. #P < 0.05, significant differences from the baseline value at 0 min in the follicular phase; §P < 0.05, significant differences from the baseline value at 0 min in the luteal phase
Figure 6 shows the linear regression line between mean T sk and thermal sensation for the whole body (Fig. 6a) and between mean T sk and thermal pleasantness for the whole body (Fig. 6b) at 0–120 min. There were significant linear correlations for each relationship (P = 0.00–0.04). The average regression slopes, which were estimated for all the subjects, were no different in the F and L phases (Fig. 6a, 2.17 ± 0.29 and 2.21 ± 0.38, respectively, P = 0.92; Fig. 6b, 2.11 ± 0.21 and 1.95 ± 0.32, respectively, P = 0.60). In addition, the average regression intercepts were no different in the F and L phases (Fig. 6a, −74.57 ± 9.90 and −76.26 ± 12.83, respectively, P = 0.87; Fig. 6b, −72.03 ± 7.11 and −67.22 ± 10.83, respectively, P = 0.62).
Fig. 6.
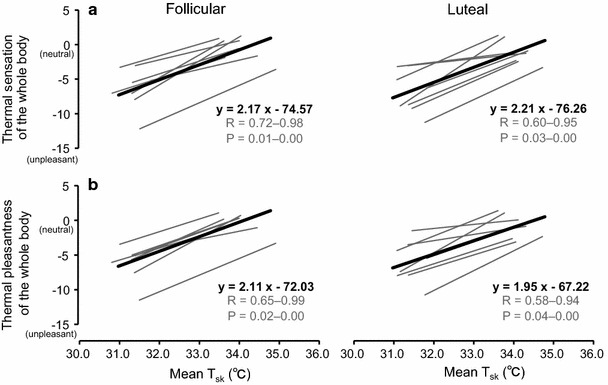
Linear regression line between mean skin temperature (mean T sk) and thermal sensation for the whole body (a: left follicular phase, right luteal phase, n = 8), and mean T sk and thermal pleasantness for the whole body (b: left follicular phase, right luteal phase, n = 8) at 0–120 min. The gray lines represent the linear regressions for each subject. The bold black lines and equations were based on average slope and intercept of the regression lines, which were estimated from results for all the subjects. Correlation coefficients (R) and probability values (P) are the maximum and minimum values for all the subjects
The linear regression lines for local skin temperature and thermal sensation of the hands and toes at 0–120 min are shown in Fig. 7. Significant linear correlations (P = 0.00–0.04) were obtained for each individual relationship except for one subject for the relationship between T index and thermal sensation of the hands. Hence, one subject was excluded from regression analysis (Fig. 7a). The average regression slopes, which were estimated from results for six (Fig. 7a) or seven (Fig. 7b) subjects, were no different between the F and L phases (Fig. 7a, 0.78 ± 0.11 and 0.71 ± 0.10, respectively, P = 0.64; Fig. 7b, 0.81 ± 0.13 and 0.80 ± 0.18, respectively, P = 0.97). In addition, average regression intercepts were no different in the F and L phases (Fig. 7a, −27.04 ± 3.88 and −24.72 ± 3.73, respectively, P = 0.64; Fig. 7b, −28.22 ± 3.97 and −27.58 ± 5.62, respectively, P = 0.90).
Fig. 7.
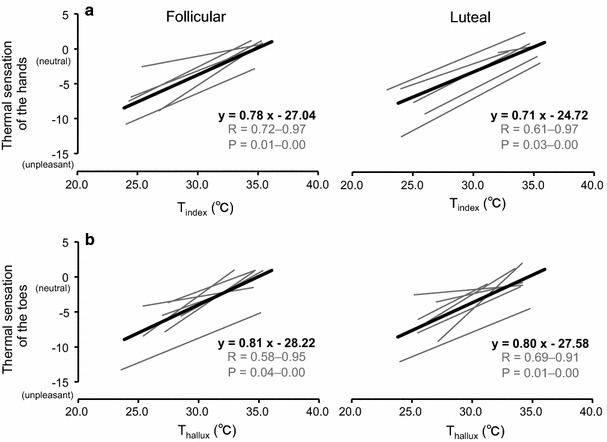
Linear regression line between temperature of the index finger (T index) and thermal sensation of the hands (a: left follicular phase, right luteal phase, n = 6), and temperature of the hallux (T hallux) and thermal sensation of the toes (b: left: follicular phase, right luteal phase, n = 7) at 0–120 min. The gray lines represent the linear regressions for each subject. The bold black lines and equations were based on the average slope and intercept of the regression lines, which were estimated from results for six (a) or seven (b) subjects. Correlation coefficients (R) and probability values (P) represent the maximum and minimum values for the subjects
Discussion
The purpose of this study was to determine whether the change of body temperature with menstrual cycle affects autonomic thermoregulatory responses and thermal perception in a cold environment. The difference between T core in the L and F phases was maintained during cold exposure. However, there were no differences between autonomic cold-defense responses and thermal perception in the two phases.
Autonomic thermoregulatory responses
Percentage changes in LDFchest and % CVCchest were no different between the L and F phases (Fig. 3e, f), which may indicate that relative change of heat-loss response of the torso was similar during the cold exposure in both phases. LDFchest at 29 °C and during cold exposure was greater in the L phase than in the F phase, which might reflect greater skin blood flow. However, the value was much smaller than that for the index finger, and skin temperature was no different between the two phases (Fig. 1d). Mean T sk reflects skin blood flow and ambient temperature, which was no different between the two phases. Therefore, we propose that heat loss from the whole body is no different between the L and F phases at T a of 29 °C and during cold exposure.
T hallux in the L phase became lower than in the F phase only when T a decreased from 29 to 23.5 °C (Fig. 1f), although T index, LDFindex, and % LDFindex were no different. The peripheral skin area has numerous arteriovenous anastomoses, which largely contribute to heat loss response [17]. Although transient response to cold might be different in the L and F phases, the effect of the peripheral skin as the cold-defense effector was similar. Rossi et al. [18] also reported that forearm blood flow is no different in the L and F phases at a steady T a of 22–24 °C.
The metabolic rate was no different between the L and F phases at a T a of 29 °C and during cold exposure (Fig. 4). Similar findings have been reported elsewhere [3, 5–8].These results suggest that, under these environmental conditions, only the response attenuating autonomic heat-loss mechanisms worked in the same manner in both the L and F phases. Moreover, the balance point of body temperature for thermoregulation shifts to a higher level in the L phase.
The preoptic area of the hypothalamus (POA) is the center of autonomic thermoregulation [19]. Deactivation of the warm-sensitive neurons in the area elicits autonomic responses to cold. Progesterone suppresses activity of the warm-sensitive neurons in the POA [20, 21]. Therefore, a higher level of progesterone in the L phase may have suppressed the effect of a higher T core.
Stephenson and Kolka reported that plasma volume is lower in the L phase than in the F phase [22]. In our study, without any difference in MAP, HR was higher in the L phase than in the F phase at the baseline T a of 29 °C and during cold exposure (Fig. 2). In the L phase, venous return to the heart may decrease, because of smaller plasma volume. To maintain cardiac output, heart rate may have increased via baroreflex control.
Thermal sensation and pleasantness
Frank et al. [11] demonstrated that, in humans, thermal information from both body core and skin surface generates the thermal perception of the whole body. In our study, mean T sk was no different between the two phases at T a of 29 °C or during cold exposure (Fig. 1c), and T core remained higher in the L phase than in the F phase (Fig. 1b). However, the thermal perception of the whole body and periphery was no different between the L and F phases (Fig. 5a, b, c, and d).
Because the difference in T core was maintained between the two phases, we were able to estimate the effect of the difference on thermal perception of skin temperature. If the relationship between T core and skin temperature is different between the phases, the results indicate interaction with T core. Regression analysis for skin temperature and thermal perception of the whole body or for local skin temperature and thermal sensation of the hands and toes indicated the relationships were similar for the L and F phases (Fig. 6). These results indicate that the different T core had no effect on thermal perception.
In a normal environment, body temperature is maintained so that autonomic cold and heat-defense effectors are both used a little (the balance point) [9]. This thermal condition induces thermal pleasantness [23], although the link between the autonomic control and thermal pleasantness has not been examined well. Thermal pleasantness is related to positive anticipation of the current thermal environment. In other words, thermal unpleasantness (i.e., negative anticipation) drives a human being to counteract the thermal environment accordingly. Therefore, similar thermal perceptions in the L and F phases suggest that the balance point of body temperature for initiating cold and warm-seeking (negative-anticipation) behavior shifts to a higher level in the L phase.
Recent studies of humans by use of positron emission tomography and functional magnetic resonance imaging have shown that the insular cortex is related to thermal sensation [24, 25], and the amygdala, orbitofrontal cortex, cingulate cortex, associative cortices, and ventral striatum are related to thermal pleasantness [26–28]. Progesterone receptors are widely expressed in the brain, including the hypothalamus, amygdala, and frontal cortex [29]. Therefore, progesterone may modulate thermal sensation and/or thermal pleasantness by affecting the brain regions involved in thermal perception.
Conclusions
This study showed that the different body core temperature in the L and F phases was maintained during cold exposure in the range 29–23.5 °C. Attenuation of heat loss caused by skin vasoconstriction occurred in both phases. Thermal perception of the whole body and periphery was not affected by the menstrual cycle. The change in body core temperature with the menstruation cycle has no effect on either autonomic thermoregulation or thermal perception under these experimental conditions. We speculate that the balance point (formally called the set point) for body temperature for initiation of autonomic and behavioral cold and heat-defense effectors shifts to a higher level in the L phase.
Acknowledgments
This study was supported by a Grant-in-Aid for Scientific Research (B), no. 20390066, from the Ministry of Education, Culture, Sports, Science, and Technology of Japan.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Hessemer V, Brück K. Influence of menstrual cycle on shivering, skin blood flow, and sweating responses measured at night. J Appl Physiol. 1985;59:1902–1910. doi: 10.1152/jappl.1985.59.6.1902. [DOI] [PubMed] [Google Scholar]
- 2.Webb P. 24-hour energy expenditure and the menstrual cycle. Am J Clin Nutr. 1986;44:614–619. doi: 10.1093/ajcn/44.5.614. [DOI] [PubMed] [Google Scholar]
- 3.Hayashi K, Kawashima T, Suzuki Y. Effect of menstrual cycle phase on the ventilatory response to rising body temperature during exercise. J Appl Physiol. 2012;113:237–245. doi: 10.1152/japplphysiol.01199.2011. [DOI] [PubMed] [Google Scholar]
- 4.Hessemer V, Brück K. Influence of menstrual cycle on thermoregulatory, metabolic, and heart rate responses to exercise at night. J Appl Physiol. 1985;59:1911–1917. doi: 10.1152/jappl.1985.59.6.1911. [DOI] [PubMed] [Google Scholar]
- 5.Kolka MA, Stephenson LA. Control of sweating during the human menstrual cycle. Eur J Appl Physiol Occup Physiol. 1989;58:890–895. doi: 10.1007/BF02332224. [DOI] [PubMed] [Google Scholar]
- 6.Hirata K, Nagasaka T, Hirai A, et al. Effects of human menstrual cycle on thermoregulatory vasodilation during exercise. Eur J Appl Physiol Occup Physiol. 1986;54:559–565. doi: 10.1007/BF00943341. [DOI] [PubMed] [Google Scholar]
- 7.Frascarolo P, Schutz Y, Jéquier E. Decreased thermal conductance during the luteal phase of the menstrual cycle in women. J Appl Physiol. 1990;69:2029–2033. doi: 10.1152/jappl.1990.69.6.2029. [DOI] [PubMed] [Google Scholar]
- 8.Stephenson LA, Kolka MA, Wilkerson JE. Metabolic and thermoregulatory responses to exercise during the human menstrual cycle. Med Sci Sports Exerc. 1982;14:270–275. doi: 10.1249/00005768-198204000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Romanovsky AA. Do fever and anapyrexia exist? Analysis of set point-based definitions. Am J Physiol Regul Integr Comp Physiol. 2004;287:R992–R995. doi: 10.1152/ajpregu.00068.2004. [DOI] [PubMed] [Google Scholar]
- 10.Hensel H. Thermoreception and temperature regulation. London: Academic Press; 1981. [PubMed] [Google Scholar]
- 11.Frank SM, Raja SN, Bulcao CF, Goldstein DS. Relative contribution of core and cutaneous temperatures to thermal comfort and autonomic responses in humans. J Appl Physiol. 1999;86:1588–1593. doi: 10.1152/jappl.1999.86.5.1588. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham DJ, Cabanac M. Evidence form behavioral thermoregulatory responses of a shift in setpoint temperature related to the menstrual cycle. J Physiol (Paris) 1971;63:236–238. [PubMed] [Google Scholar]
- 13.Kim HE, Tokura H. Effects of the menstrual cycle on dressing behavior in the cold. Physiol Behav. 1995;58:699–703. doi: 10.1016/0031-9384(95)00118-3. [DOI] [PubMed] [Google Scholar]
- 14.Nagashima K, Yoda T, Yagishita T, et al. Thermal regulation and comfort during a mild-cold exposure in young Japanese women complaining of unusual coldness. J Appl Physiol. 2002;92:1029–1035. doi: 10.1152/japplphysiol.00399.2001. [DOI] [PubMed] [Google Scholar]
- 15.Hardy JD, DuBois EF. The technic of measuring radiation and convection. J Nutr. 1938;15:461–475. [Google Scholar]
- 16.Marks LE, Stevens JC, Bartoshuk LM, et al. Magnitude-matching: the measurement of taste and smell. Chem Senses. 1988;13:63–87. doi: 10.1093/chemse/13.1.63. [DOI] [Google Scholar]
- 17.Romanovsky AA. Skin temperature: its role in thermoregulation. Acta Physiol (Oxf) 2014;210:498–507. doi: 10.1111/apha.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rossi M, Di Maria C, Erba P, et al. Study of skin vasomotion during phollicular and luteal phase in young healthy women. Clin Hemorheol Microcirc. 2009;42:107–115. doi: 10.3233/CH-2009-1189. [DOI] [PubMed] [Google Scholar]
- 19.Nagashima K. Central mechanisms for thermoregulation in a hot environment. Ind Health. 2006;44:359–367. doi: 10.2486/indhealth.44.359. [DOI] [PubMed] [Google Scholar]
- 20.Tsai CL, Matsumura K, Nakayama T. Effects of progesterone on thermosensitive neurons in preoptic slice preparations. Neurosci Lett. 1988;86:56–60. doi: 10.1016/0304-3940(88)90182-6. [DOI] [PubMed] [Google Scholar]
- 21.Nakayama T, Suzuki M, Ishizuka N. Action of progesterone on preoptic thermosensitive neurones. Nature. 1975;258:80. doi: 10.1038/258080a0. [DOI] [PubMed] [Google Scholar]
- 22.Stephenson LA, Kolka MA. Plasma volume during heat stress and exercise in women. Eur J Appl Physiol Occup Physiol. 1988;57:373–381. doi: 10.1007/BF00417979. [DOI] [PubMed] [Google Scholar]
- 23.Kingma BR, Frijns AJ, Schellen L, van Marken Lichtenbelt WD. Beyond the classic thermoneutral zone. Temperature. 2014;1:142–149. doi: 10.4161/temp.29702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craig AD, Chen K, Bandy D, Reiman EM. Thermosensory activation of insular cortex. Nat Neurosci. 2000;3:184–190. doi: 10.1038/72131. [DOI] [PubMed] [Google Scholar]
- 25.Hua LH, Strigo IA, Baxter LC, et al. Anteroposterior somatotopy of innocuous cooling activation focus in human dorsal posterior insular cortex. Am J Physiol Regul Integr Comp Physiol. 2005;289:319–325. doi: 10.1152/ajpregu.00123.2005. [DOI] [PubMed] [Google Scholar]
- 26.Kanosue K, Sadato N, Okada T, et al. Brain activation during whole body cooling in humans studied with functional magnetic resonance imaging. Neurosci Lett. 2002;329:157–160. doi: 10.1016/S0304-3940(02)00621-3. [DOI] [PubMed] [Google Scholar]
- 27.Rolls ET, Grabenhorst F, Parris BA. Warm pleasant feelings in the brain. Neuroimage. 2008;41:1504–1513. doi: 10.1016/j.neuroimage.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 28.Farrell MJ, Johnson J, McAllen R, et al. Brain activation associated with ratings of the hedonic component of thermal sensation during whole-body warming and cooling. J Therm Biol. 2011;36:57–63. doi: 10.1016/j.jtherbio.2010.11.003. [DOI] [Google Scholar]
- 29.Brinton RD, Thompson RF, Foy MR, et al. Progesterone receptors: form and function in brain. Front Neuroendocrinol. 2008;29:313–339. doi: 10.1016/j.yfrne.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


