Abstract
Humans are generally in standing or sitting positions on Earth during the day. The musculoskeletal system supports these positions and also allows motion. Gravity acting in the longitudinal direction of the body generates a hydrostatic pressure difference and induces footward fluid shift. The vestibular system senses the gravity of the body and reflexively controls the organs. During spaceflight or exposure to microgravity, the load on the musculoskeletal system and hydrostatic pressure difference is diminished. Thus, the skeletal muscle, particularly in the lower limbs, is atrophied, and bone minerals are lost via urinary excretion. In addition, the heart is atrophied, and the plasma volume is decreased, which may induce orthostatic intolerance. Vestibular-related control also declines; in particular, the otolith organs are more susceptible to exposure to microgravity than the semicircular canals. Using an advanced resistive exercise device with administration of bisphosphonate is an effective countermeasure against bone deconditioning. However, atrophy of skeletal muscle and the heart has not been completely prevented. Further ingenuity is needed in designing countermeasures for muscular, cardiovascular, and vestibular dysfunctions.
Keywords: Spaceflight, Gravity, Atrophy, Bone mineral density, Hydrostatic pressure, Orthostatic intolerance, Bisphosphonate
Introduction
Land-living vertebrates are believed to have evolved from fish [1]. During the process of evolution, the paired fins were modified into the limbs of early tetrapods or amphibia. The limbs came to be used to raise the animal body from the ground, and in combination with lateral trunk flexions, to propel the body forward. Reptiles are also descended from early tetrapods. When the mammals evolved, the trunk was also used to achieve an upright position. In humans, the trunk musculature has come to be used for balancing the body on the lower limbs and for movements of the head and trunk. In the lower limbs, the soleus is essential for bipedal standing and walking. In most mammals or quadrupeds, the center of gravity lies between the forelimbs and hind limbs, and the load on the hind limbs is thus smaller in quadrupeds than that on the lower limbs in humans. Thus, they do not require a large soleus mass. The soleus muscle, which acts on the ankle joint, is small in quadrupeds, but is relatively large in humans. In contrast, the gastrocnemius in the same triceps surae muscle is larger than the soleus in quadrupeds [2, 3]. The vestibular system senses the direction of gravity or posture and plays important roles in controlling posture via the motor neurons [4].
Standing, sitting, and walking exercise occupy about 16 h per day, and are the most common positions in the daily lives of humans. The gravity is loaded in the longitudinal direction of the body and has a major effect on the cardiovascular system [5, 6]. During recumbent posture, the body fluid, especially blood, is distributed uniformly along the body, and arterial pressure (AP) is uniform from head to foot because the gravitational force and gradient along the longitudinal direction of the body is almost zero. However, changes in posture to either sitting or standing result in generation of a hydrostatic pressure gradient due to the force of gravity. The hydrostatic pressure on the head is low, whereas that on the feet is high. The high hydrostatic pressure on the feet causes high arterial and venous pressure. With this high venous pressure, the veins in the lower body are dilated, since their walls are highly compliant or extremely soft. With this pooling, the venous return and cardiac output are decreased, and AP should be decreased because it is the product of cardiac output and total peripheral resistance of the blood vessels. During postural change or standing, baroreflex control is considered important [7, 8].
Recently, humans have begun expanding their habitat into space. During human spaceflight and exposure to a microgravity environment, the effects of gravity on the body are diminished. The body and tissue structures adapt to the new environment, but the adaptation makes daily living difficult following return to Earth or a 1-g environment. To prevent adverse effects or deconditioning, various techniques or countermeasures have been considered and adopted. Multiple studies using Earth-based analogs and simulation of microgravity have been successfully performed in humans and animals, and are significant for their contribution to the study of adaptation and deconditioning [9–11]; however, the results are sometimes intermixed with data from spaceflights. Thus, this paper focuses on and summarizes general changes and deconditioning in the musculoskeletal, cardiovascular, and vestibular systems during human spaceflight, as well as reviewing the effects of the countermeasures.
Adaptation to microgravity and deconditioning
Skeletal muscles
Based on the myosin heavy chain isoform pattern, the skeletal muscles of the adult mammalian limb generally contain one slow fiber (type I) and two types of fast fibers (type IIa and IIb) [12]. In the triceps surae of the lower limb, the soleus is the slow muscle and contains primarily the type I slow-twitch oxidative fibers. The gastrocnemius is the type II fast-twitch glycolytic muscle [13–17]. Postural or antigravity muscles possess many slow-twitch myofibers, whereas propulsive or locomotor muscles have numerous fast-twitch myofibers [18–23].
Muscles are needed for movement and to counteract gravity, and they must be used in order to maintain the structure and the function. During spaceflight or in a microgravity environment, humans do not need to support their bodies; thus the antigravity muscles become atrophied. The volume of quadriceps and triceps surae decreased by −6.0 and −6.3%, respectively, after 8 days, and −5.5 to −15.4 and −8.8 to −15.9%, respectively, after 9–16 days of spaceflight [24, 25]. Fitts et al. reported that the slow-twitch and antigravity soleus shows greater atrophy than the fast-twitch gastrocnemius [26]. However, after 17 days of spaceflight, the gastrocnemius (−12%) tended to atrophy more than the soleus (−10%). Over longer spaceflight durations of 112–196 days, crew members showed further decreases in gastrocnemius (−24%) and soleus (−20%) volume, and the decrease was smaller in the soleus [27] (Fig. 1). In any of these cases, type II fibers are more atrophied than the type I (Fig. 2). In the atrophied vastus lateralis of the quadriceps muscle, the decline of cross-sectional area in the type II and I fibers were −21 and −11%, respectively, after 5 days of spaceflight, and −21 to −36 and −16 to −17%, respectively, after 11 days of spaceflight [28]. In the soleus muscle, type IIa fibers declined by −26% and type I fibers declined by −15% after 17 days of spaceflight [29]. Type IIb fibers are the most susceptible to a microgravity environment and the most atrophied. However, type I fibers also exhibit atrophy, and the percentage distribution of type II fibers becomes larger in the atrophied muscle (Fig. 2). These observations are opposite to those in rats. Type I and type II fibers declined by −30 and −15%, respectively, after 14 days of spaceflight, and hind limb suspension [30]. Thus, consideration of species difference is also necessary for discussion of the muscle atrophy mechanism during spaceflight. In the hind limb unloading rat model, electromyography is diminished at the onset of unloading. The amplitude recovers within a week, but the atrophy progresses [31–33]. Thus, species difference should be considered, but muscle atrophy is not induced by unloading only. After landing, following a 9- to 16-day spaceflight, the atrophy of the plantar flexor progresses for 4 days [25]. Muscle damage with weight bearing after spaceflight may be induced [27, 34]. Along with atrophy of the lower leg muscle, maximal voluntary contraction of the calf during plantar flexion is also reduced from −0.1 to −37.6% during 1, 3, and 6 months of spaceflight [35]. No correlation was found between the decrease and flight duration. As observed in the decrease in muscle volume, peak force decreased by −21 and −25% for type I and type IIa fibers, respectively [29].
Fig. 1.
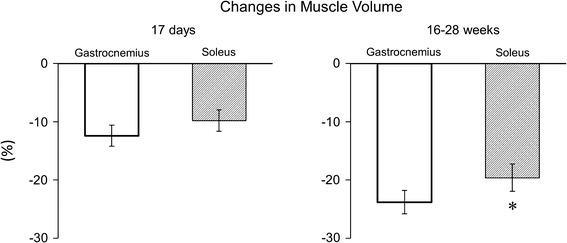
Changes in muscle volume of triceps surae in astronauts after short (17 days) and long (16–28 weeks) spaceflights (drawn from data in Ref. [27]). *p < 0.05 vs gastrocnemius
Fig. 2.
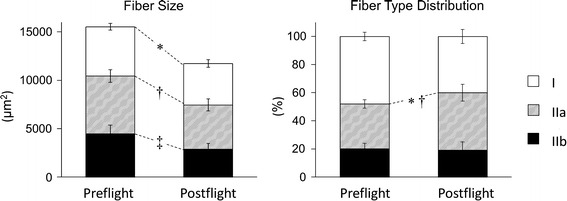
Changes in muscle fiber size (left panel) and fiber type distribution (right panel) of the vastus lateralis in astronauts after 11 days of spaceflight (drawn from data in Ref. [28]). *p < 0.05 vs type I of preflight, † p < 0.05 vs type IIa of preflight, ‡ p < 0.05 vs type IIb of preflight
Skeletal system
Bone has mainly two functions. One is a rigid structure to support and move the body on the ground, to protect organs. The other is a reservoir of calcium in the body [1]. In a microgravity environment, the function of support has less meaning, as in fish in water.
Unloading of the skeleton results in calcium leaving the bones. Within a few days of exposure to microgravity, urinary calcium excretion increases by 60–70% [36]. Densitometry of the calcaneus showed a tendency for increased bone mineral loss with longer spaceflight (−7.4% after 2 months of spaceflight, and −4.5 and −7.9% after 4 months of spaceflight) [37–39]. In the vertebral column, loss of bone mineral density (BMD) from −0.67 to 0.93% after 2–4 months, and −0.3 to −10.8% after 5–7 months of spaceflight were observed [36, 40]. The values are variable due to individual heterogeneity and variable methodology of measurements, but the decreases are twice those of bed rest, which is also unloading for the bones and a simulation of microgravity exposure [41, 42]. BMD decreases at weight-bearing points, such as the neck, spine, pelvis, and femur. In contrast, the upper extremities showed minimal or no decreases in BMD [43, 44] (Fig. 3). However, the skull exhibited increases in BMD [27, 45]. The trabecular zone is more susceptible to microgravity, and loss in BMD is larger than that in the cortical zone in the femur [40]. Thus, regional differences in BMD change are observed, and care should be taken in using metabolites as bone markers [46, 47].
Fig. 3.
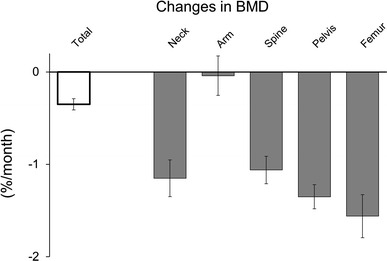
Changes in bone mineral density (BMD) of various portions of astronauts after 4–14.4 months of spaceflight (drawn from data in Ref. [44])
Cardiovascular system
Humans live in an upright position about 16 h per day on Earth. The difference in posture from that of quadrupeds also affects cardiovascular condition. When posture is changed from a supine or recumbent position to an upright position, a hydrostatic pressure difference is observed along the longitudinal direction of the body [5]. Venous vessels are highly compliant, and the increase in intravascular pressure induces vessel distention and footward fluid shift [6, 48–52]. This fluid redistribution or footward blood shift may decrease the stroke volume of the heart [53]. To maintain AP, particularly in the head, heart rate (HR) and total peripheral resistance are raised reflexively [54]. In a microgravity environment or during spaceflight, the hydrostatic pressure in the upper body is constantly as high as that during supine or recumbent posture. Thus, forehead thickness increases by 7% compared with that of preflight in a supine position [55], and intraocular pressure by 92% [56]. The heart size and stroke volume is increased temporally with the fluid shift [57–59]. In spite of the headward fluid shift, central venous pressure (CVP) decreases [58]. The change is opposite from that during simulated microgravity, such as head-down tilt and water immersion [60–62]. The decrease in CVP may be induced by change in the thoracic shape and reduction of intrathoracic pressure due to loss of gravitational compression for the thoracic cage and mediastinum [63–65]. Thus, the vena cava may be enlarged, and intravenous pressure is decreased, but the transmural pressure may be increased.
Apparent diuresis is not observed during spaceflight [66–68]; however, fluid intake is further decreased, and body fluid balance is negative. Eight and twelve days of flight decreased the plasma volume by −17%, probably due to the negative fluid balance and movement of the fluid to the extravascular space [69].
In a microgravity environment, large contractility of the heart is not required to send blood toward the head against gravity, and to maintain AP. Thus, the heart is atrophied by −8 to −10% after 10 days of spaceflight [70]. Figure 4 shows the relationship between averages of stroke volume and sympathetic nerve activity before and after spaceflight. They vary inversely, and a decrease in stroke volume induces an increase in sympathetic nerve activity. Stroke volume is largest and muscle sympathetic nerve activity is smallest during preflight supine position. With a change in position from supine to upright position, stroke volume decreased, and sympathetic nerve activity increased. Stroke volume significantly decreased, and sympathetic nerve activity increased after spaceflight even in the supine position. However, their relationship was maintained even after spaceflight [71] (Fig. 4). Even in the subjects who experienced presyncope during 10 min of standing test, the relationship was similar to that in non-presyncopal subjects after 4–215 days of spaceflight [72]. Stroke volume in pre-syncopal subjects at 6 min is 75% of that in non-presyncopal subjects, but HR is further increased. Thus, the relationship between stroke volume and HR is maintained even in presyncopal subjects (Fig. 5). As seen in these values, responses of sympathetic nerves or HR to changes in stroke volume, i.e., responses in the central arc of the baroreflex, are maintained at levels similar to those during preflight in spite of the decrease in cardiac size and blood volume control [71, 73–76]. Response in the peripheral arc of baroreflex control, i.e., decreased vascular contractility or responses in resistant vessels for sympathetic nerves, are also observed. Astronauts who could not complete 10 min of standing after 9–14 days of spaceflight revealed significantly reduced response of vasoconstriction [74]. The relationship between the low vasoconstrictive response and failure to complete stand tests was observed in an additional 87 astronauts after spaceflight [75, 77, 78]. However, the control of the AP may have been lost during the last minute of standing in those presyncopal subjects [72]. Thus, it is hard to determine whether the lowered vascular resistance is the reason or result of presyncope. Furthermore, vascular resistance is already elevated after spaceflight compared to that during preflight [71, 74, 75, 77, 78]. Since the capacity of vasoconstriction is finite, the elevated resting vasoconstriction associated with low circulating plasma volume and stroke volume may have represented a reduction in vasoconstrictive reserve. It is therefore unclear whether lower vascular contractility or simply lower vasoconstrictive reserve secondary to hypovolemia is being observed.
Fig. 4.
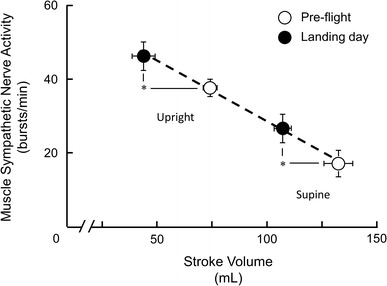
Muscle sympathetic nerve activity plotted as a function of left ventricular stroke volume before and on landing day after 16 days of spaceflight (mean ± SE). With a change in position from supine to upright, stroke volume decreased, and sympathetic nerve activity increased. Stroke volume significantly decreased, and sympathetic nerve activity increased after spaceflight in both supine and upright positions. However, a relationship was maintained similar to that before spaceflight. *p < 0.05 for comparison between pre- and postflight muscle sympathetic nerve activity and stroke volumes (redrawn from data in Ref. [71])
Fig. 5.
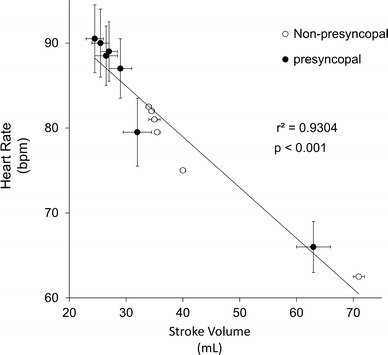
Heart rate plotted as a function of left ventricular stroke volume during tilt test before and after 4–215 days of spaceflight in astronauts who completed 10 min of tilt test (non-presyncopal) and those who could not stand for the entire 10 min (mean ± SE). Values are plotted regardless of flight duration, and values during 6 min after the onset of tilt are plotted (drawn from data in Ref. [72]). The relationship between stroke volume and HR in presyncopal subjects is maintained, similar to that in non-presyncopal subjects after spaceflight
After 9–14 days of spaceflight and returning to Earth, orthostatic intolerance or orthostatic hypotension, i.e., acute drop of systolic AP more than 20 mmHg, has been observed in 64% of astronauts [74]. As described above, the orthostatic hypotension is considered to be induced mostly by cardiac atrophy, decrease in blood volume, and possibly decrease in vascular contractility [74, 75, 77, 78]. AP control at the onset of standing is importantly controlled by the vestibular system, particularly the otolith organs [50, 51, 79]. The otolith function or otolith-related control is considered to be weakened after spaceflight, and orthostatic hypotension at the onset of postural change may be induced by otolith deconditioning, as described in the next section [80–83].
Vestibular system
The vestibular system contains semicircular canals and otolith organs. Semicircular canals sense angular acceleration, and the otolith organs sense linear acceleration [84]. This system is important for equilibrium; in particular, the otolith organs contribute to the determination of body orientation with respect to gravity. This system also plays important roles in controlling posture via the motor neurons [4]. On Earth, 1-g acts in a vertical direction during any posture, but the gravity is zero in any direction during spaceflight. This unloading changes the characteristics of the vestibular system and its related functions.
The caloric test, the test for semicircular canal function, was performed before and after a 10-day spaceflight. The intensity of the response was similar to that measured on Earth [85]. The vestibulo-ocular reflex is involved in both otolith and semicircular canals, but head yaw oscillation in the test is sensed by semicircular canals only. A week of spaceflight did not change in the gain or the responsiveness [86]. For otolith function, an ocular-counter rolling test using a short-arm centrifuge during spaceflight showed a 10% decrease in magnitude [87]. In an otolith tilt-translation test, the difference in angle between real vertical direction and subjective vertical is measured. No difference was observed between the real and subjective vertical direction before spaceflight, but a difference of 15° was found after a 16-day spaceflight [88]. Postural equilibrium control measured by oscillation in the center of gravity was seriously disrupted immediately following 4- to 16-day spaceflight in all subjects [89, 90]. Thus, the function of otolith organs is more susceptible to exposure to microgravity than that of semicircular canals. However, the results from the center of gravity test may be exaggerated by the muscle atrophy described above. In order to evaluate the changes to otolith organs more accurately, function tests using less affected muscles will need to be done.
Countermeasures
Lower body negative pressure
A lower body negative pressure (LBNP) device applies ambient pressure lower than the normal atmospheric pressure to the lower portion of the body to induce footward fluid shift. The chamber is sealed, and the seal is attached to the iliac crest of the subject. The chamber pressure of −40 to −60 mmHg, which is below the normal ambient pressure, generates a force or weight bearing against the foot and footward fluid shift similar to that on Earth [50, 74, 91, 92]. With the fluid shift during −40 mmHg, renin was released [93], but lower negative pressure, such as −10 to −20 mmHg, did not affect the renin release, and cardiovascular impact was relatively small [94].
The LBNP device in the Mir space station did not have a saddle to support the body. Thus, negative pressure made the feet press against the bottom of the chamber and induced muscle contraction in the lower legs [95]. The contraction avoided venous distension and blood pooling in the legs. Thus, the fluid shift is considered to be less than that using the LBNP device with a saddle used during Skylab and the Shuttle program. The increase in HR was higher with the saddle compared to that without the saddle [95, 96].
The LBNP is used as a countermeasure with saline ingestion. LBNP with saline ingestion (6–9 g NaCl in 900–1200 ml water) during the last 2–5 days before landing subjectively improved orthostatic tolerance [95, 97]. About 1 l of isotonic saline ingestion and −30 mmHg of LBNP exposure 4 h a day prior to landing showed less HR increase and less decrease in systolic blood pressure compared with astronauts without LBNP during the simulated orthostatic test [98]. Thus, the program is beneficial for preventing orthostatic tolerance following landing, but a 5-h treatment for each astronaut makes it impractical to use.
Combined with treadmill running, the countermeasure for the musculoskeletal system, LBNP is proposed as both musculoskeletal and cardiovascular countermeasure [99–107]. The body needs to pull toward the treadmill in a microgravity environment during exercise. Bungee cords are used to strap astronauts, but they exert forces against the feet of only 75 and 54% of the body weight during walking and running, respectively, compared with those on Earth [108]. Pumping effect with the muscle contraction further enhances headward fluid shift. As described above, LBNP can generate similar force or body weight against the feet, and similar footward body fluid shift, as observed on the Earth. However, running and walking causes central fluid shift, and use of a LBNP device with no exercise is required as a countermeasure for cardiovascular deconditioning [104, 109].
Exercise
On the Mir space station, Russian astronauts or cosmonauts performed exercise using the bungee cord and treadmill 2–3 h on 3 of 4 days. The countermeasure was not effective for bone loss [44]. In addition to the treadmill, a cycle ergometer was also used on the International Space Station (ISS). Little information is available about the level of the force, but BMD was decreased by 4% in the lumbar spine and by 10% in the femur during a 6-month spaceflight [40]. Maximal voluntary contraction revealed a significant decrease of 17% during a 3- to 6-month spaceflight [110]. Thus, the devices are not effective as a countermeasure for bone loss during long-duration spaceflights.
Astronauts on the ISS allotted 2.5 h per day, 6 days per week for exercise countermeasures during the mission. The time also includes equipment set-up, reconfiguration, and personal hygiene [111, 112]. In microgravity, high-intensity interval training is much more effective than aerobic training [113]. For the first long-duration spaceflight on the ISS in 2000, the treadmill and cycle ergometer were used for exercise. After 6 weeks, the interim resistive exercise device (iRED) was assembled [114, 115]. In 2008, the advanced resistive exercise device (ARED) was launched to the ISS. The iRED provided the ability to perform eight exercises, i.e., squats, single-leg squats, heel raises, single-leg heel raises, deadlifts, Romanian deadlifts, upright rows, and bent-over rows [112]. The ARED included these exercises and added nine more, i.e., back squat, sumo squat, sumo deadlift, shrugs, shoulder press, bench press, bicep curl, triceps extension, and single-arm row [112]. The iRED had a maximum load equivalent of 1337 N, and the eccentric force was 60–80% of the concentric force. On the other hand, ARED had a greater load of 2675 N, and the eccentric force was 90% of the concentric force. Thus, ARED had greater resistance capability [116]. The combination of treadmill, cycle ergometer, and iRED did not maintain the muscle volume and peak power. After 6 months of spaceflight, the gastrocnemius and soleus atrophied by −10 and −15%, respectively. Their peak power had declined by 32% after the spaceflight [117]. The calf muscle volume decreased; the isokinetic strength decreased −16 to −31%, and the isometric strength also decreased −2 to −35% in 4 astronauts after 6 months of spaceflight [118]. By using ARED, the isokinetic strength changes were relatively improved in the thigh muscles, i.e., −9 to −20% with iRED and −4 to −15% with ARED during an ISS expedition of 60–190 days, but did not reach statistical significance [119]. With iRED, the BMD and bone mineral content (BMC) were still decreased in the pelvis and hip by −6 to −12% during 4–5 months of spaceflight. By using ARED, these changes were diminished, and the BMD and BMC in the pelvis and hip after the spaceflight were not significantly different from those before the spaceflight [112, 120]. However, the BMC and BMD of the lumber vertebral column significantly decreased by −0.2 to −5% with the use of either equipment. The changes in the vertebrae were not significantly different between the types of equipment. ARED was used with nutritional and pharmaceutical countermeasures, i.e., oral bisphosphonates (alendrone), calcium, and vitamin D [121]. Bisphosphonates block osteoclast activation and thus slow bone resorption. Moreover, they slow bone loss, improve BMD, and reduce fracture rates [122–124]. Bisphosphonates were started 3 weeks before the flight and continued throughout the flight [121]. They were taken at a dose of 70 mg/week, which is a dose for osteoporosis treatment and twice the dose for preventing osteoporosis [125]. About 400–800 IU of vitamin D3 was taken daily, and 800 IU is a dose for postmenopausal women. More than 1000 mg of Ca was also taken daily, which is a similar dose to that given to postmenopausal women [121, 126]. Before the use of ARED and bisphosphonates, exercise with iRED decreased total hip BMD and BMC after spaceflight. However, the countermeasure using both ARED and bisphosphonates maintained BMD and BMC during 4.5–6.2 months of spaceflight (Fig. 6). Excessive load or training with squats, overuse injuries, and fatigue-related problems such as spine injuries still required attention [127], but the combination of nutritional and pharmaceutical countermeasures and ARED was effective in avoiding bone mineral loss for the lower extremities.
Fig. 6.
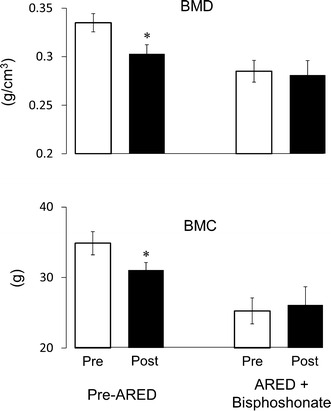
Bone mineral density (BMD) and bone mineral content (BMC) in the total hip of before (pre) and after (post) 4.5–6.2 months of spaceflight (mean ± SE). Values are from astronauts who flew before the advanced resistance exercise device (ARED) was employed as a countermeasure (pre-ARED) and those who used combined ARED and medicated bisphosphonate (ARED + bisphosphonate). Before the use of ARED and bisphosphonates, total hip BMD and BMC decreased after spaceflight. However, a countermeasure using both ARED and bisphosphonates maintained the BMD and BMC during 4.5–6.2 months of spaceflight. *p < 0.05 vs preflight (drawn from data in Ref. [121])
Future perspectives
Pharmaceutical countermeasures have been successful in preventing deconditioning of the skeletal system. However, exercise countermeasures as represented by ARED do not completely prevent muscle and cardiac deconditioning. Thus, atrophy of skeletal muscles and the heart is not induced by disuse only. Gravity-sensing or gravity-related mechanisms may be present, and the atrophy continues throughout the spaceflight [128]. Furthermore, the reflex via the gravity sensors, such as muscle contraction for postural control [129, 130] and vestibulo-cardiovascular control during microgravity [79, 131, 132], is considered to change and leads to atrophy of the myocardium and skeletal muscles for standing. Artificial gravity with resistance exercise would resolve the deconditioning and be an important countermeasure [133–136], but the ability to provide such a device on a spacecraft will be an engineering challenge. In preparation for a Mars exploration mission, it will be necessary to develop an integrated and compact countermeasure for mission success. Further research on a combination of electric activating devices, such as galvanic vestibular stimulation and electrical stimulation of antagonist muscles to resist volitional contraction of the agonist instead of gravity, is expected [83, 137].
Conclusion
In this manuscript, we have summarized changes in the musculoskeletal, cardiovascular, and vestibular systems with exposure to a microgravity environment, and their current countermeasures. Spaceflight or exposure to microgravity immediately induces bone loss with an increase in urinary calcium excretion and muscle atrophy. The heart is also atrophied, and plasma volume decreases. Thus, decrease in stroke volume is considered to result in orthostatic intolerance. The otolith-related function also declines. As a countermeasure, ARED and bisphosphonates are effective for maintaining BMD and BMC, as well as effectively avoiding the deconditioning of bones, but they are only partially effective for muscles. LBNP and fluid loading do not completely avoid cardiac atrophy. Further ingenuity is needed to design countermeasures capable of preventing muscle and cardiac atrophy, and for maintaining vestibular function in future spaceflights.
Compliance with ethical standard
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The article does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.Joseph J. Locomotor system. In: Hamilton WJ, editor. Textbook of human anatomy. London: The macmillan press; 1976. [Google Scholar]
- 2.Kumakura H, Inokuchi S. Lay-out of the human triceps surae muscle: with special concern for the origin of the human bipedal posture. Showa Univ J Med Sci. 1991;3:79–89. doi: 10.15369/sujms1989.3.79. [DOI] [Google Scholar]
- 3.Suzuki A, Hayama S. Individual variation in myofiber type composition in the triceps surae and flexor digitorum superficialis. Anthropol Sci. 1994;102(Suppl):127–138. doi: 10.1537/ase.102.Supplement_127. [DOI] [Google Scholar]
- 4.St George RJ, Fitzpatrick RC. The sense of self-motion, orientation and balance explored by vestibular stimulation. J Physiol. 2011;589:807–813. doi: 10.1113/jphysiol.2010.197665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watenpaugh DE, Hargens AR. The cardiovascular system in microgravity. In: Fregly MJ, Blatteis CM, editors. Handbook of physiology, the gravitational environment. Maryland: American Physiological Society; 1996. [Google Scholar]
- 6.Hargens AR, Watenpaugh DE. Cardiovascular adaptation to spaceflight. Med Sci Sports Exerc. 1996;28:977–982. doi: 10.1097/00005768-199608000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Dampney RA, Stella A, Golin R, Zanchetti A. Vagal and sinoaortic reflexes in postural control of circulation and renin release. Am J Physiol. 1979;237:H146–H152. doi: 10.1152/ajpheart.1979.237.2.H146. [DOI] [PubMed] [Google Scholar]
- 8.Sato T, Kawada T, Sugimachi M, Sunagawa K. Bionic technology revitalizes native baroreflex function in rats with baroreflex failure. Circulation. 2002;106:730–734. doi: 10.1161/01.CIR.0000024101.77521.4D. [DOI] [PubMed] [Google Scholar]
- 9.Watenpaugh DE (2016) Analogs of microgravity: head-down tilt and water immersion. J Appl Physiol (1985) 120: 904–914 [DOI] [PubMed]
- 10.Hargens AR, Vico L (2016) Long-duration bed rest as an analog to microgravity. J Appl Physiol (1985) 120: 891–903 [DOI] [PubMed]
- 11.Globus RK, Morey-Holton E (2016) Hindlimb unloading: rodent analog for microgravity. J Appl Physiol (1985) 120: 1196–1206 [DOI] [PubMed]
- 12.Fitts RH, Widrick JJ. Muscle mechanics: adaptations with exercise-training. Exerc Sport Sci Rev. 1996;24:427–473. doi: 10.1249/00003677-199600240-00016. [DOI] [PubMed] [Google Scholar]
- 13.Edgerton VR, Smith JL, Simpson DR. Muscle fibre type populations of human leg muscles. Histochem J. 1975;7:259–266. doi: 10.1007/BF01003594. [DOI] [PubMed] [Google Scholar]
- 14.Sickles DW, Pinkstaff CA. Comparative histochemical study of prosimian primate hind limb muscles. I. Muscle fiber types. Am J Anat. 1981;160:175–186. doi: 10.1002/aja.1001600204. [DOI] [PubMed] [Google Scholar]
- 15.Acosta L, Jr, Roy RR. Fiber-type composition of selected hind limb muscles of a primate (cynomolgus monkey) Anat Rec. 1987;218:136–141. doi: 10.1002/ar.1092180207. [DOI] [PubMed] [Google Scholar]
- 16.Suzuki A, Cassens RG. A histochemical study of myofiber types in the serratus ventralis thoracis muscle of sheep during growth. J Anim Sci. 1983;56:1447–1458. doi: 10.2527/jas1983.5661447x. [DOI] [PubMed] [Google Scholar]
- 17.Johnson MA, Polgar J, Weightman D, Appleton D. Data on the distribution of fibre types in thirty-six human muscles. An autopsy study. J Neurol Sci. 1973;18:111–129. doi: 10.1016/0022-510X(73)90023-3. [DOI] [PubMed] [Google Scholar]
- 18.Armstrong RB, Saubert CWt, Seeherman HJ, Taylor CR. Distribution of fiber types in locomotory muscles of dogs. Am J Anat. 1982;163:87–98. doi: 10.1002/aja.1001630107. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki A, Tamate H. Distribution of myofiber types in the hip and thigh musculature of sheep. Anat Rec. 1988;221:494–502. doi: 10.1002/ar.1092210106. [DOI] [PubMed] [Google Scholar]
- 20.Smith JL, Edgerton VR, Betts B, Collatos TC. EMG of slow and fast ankle extensors of cat during posture, locomotion, and jumping. J Neurophysiol. 1977;40:503–513. doi: 10.1152/jn.1977.40.3.503. [DOI] [PubMed] [Google Scholar]
- 21.Walmsley B, Hodgson JA, Burke RE. Forces produced by medial gastrocnemius and soleus muscles during locomotion in freely moving cats. J Neurophysiol. 1978;41:1203–1216. doi: 10.1152/jn.1978.41.5.1203. [DOI] [PubMed] [Google Scholar]
- 22.Burke RE. Motor units: anatomy, physiology, and functional organization. In: Brooks VB, editor. Handbook of physiology, the nerve system, vol II, motor control . Maryland: American Physiological Society; 1981. [Google Scholar]
- 23.Gollnick PD, Sjodin B, Karlsson J, Jansson E, Saltin B. Human soleus muscle: a comparison of fiber composition and enzyme activities with other leg muscles. Pflugers Arch. 1974;348:247–255. doi: 10.1007/BF00587415. [DOI] [PubMed] [Google Scholar]
- 24.LeBlanc A, Rowe R, Schneider V, Evans H, Hedrick T. Regional muscle loss after short duration spaceflight. Aviat Space Environ Med. 1995;66:1151–1154. [PubMed] [Google Scholar]
- 25.Akima H, Kawakami Y, Kubo K, Sekiguchi C, Ohshima H, Miyamoto A, Fukunaga T. Effect of short-duration spaceflight on thigh and leg muscle volume. Med Sci Sports Exerc. 2000;32:1743–1747. doi: 10.1097/00005768-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Fitts RH, Riley DR, Widrick JJ. Physiology of a microgravity environment invited review: microgravity and skeletal muscle. J Appl Physiol. 2000;89:823–839. doi: 10.1152/jappl.2000.89.2.823. [DOI] [PubMed] [Google Scholar]
- 27.LeBlanc A, Lin C, Shackelford L, Sinitsyn V, Evans H, Belichenko O, Schenkman B, Kozlovskaya I, Oganov V, Bakulin A, Hedrick T, Feeback D. Muscle volume, MRI relaxation times (T2), and body composition after spaceflight. J Appl Physiol. 2000;89:2158–2164. doi: 10.1152/jappl.2000.89.6.2158. [DOI] [PubMed] [Google Scholar]
- 28.Edgerton VR, Zhou MY, Ohira Y, Klitgaard H, Jiang B, Bell G, Harris B, Saltin B, Gollnick PD, Roy RR, et al. Human fiber size and enzymatic properties after 5 and 11 days of spaceflight. J Appl Physiol. 1995;78:1733–1739. doi: 10.1152/jappl.1995.78.5.1733. [DOI] [PubMed] [Google Scholar]
- 29.Widrick JJ, Knuth ST, Norenberg KM, Romatowski JG, Bain JL, Riley DA, Karhanek M, Trappe SW, Trappe TA, Costill DL, Fitts RH. Effect of a 17 day spaceflight on contractile properties of human soleus muscle fibres. J Physiol. 1999;516(Pt 3):915–930. doi: 10.1111/j.1469-7793.1999.0915u.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ohira Y, Jiang B, Roy RR, Oganov V, Ilyina-Kakueva E, Marini JF, Edgerton VR. Rat soleus muscle fiber responses to 14 days of spaceflight and hind limb suspension. J Appl Physiol. 1992;73:51S–57S. doi: 10.1152/jappl.1992.73.2.S51. [DOI] [PubMed] [Google Scholar]
- 31.Alford EK, Roy RR, Hodgson JA, Edgerton VR. Electromyography of rat soleus, medial gastrocnemius, and tibialis anterior during hind limb suspension. Exp Neurol. 1987;96:635–649. doi: 10.1016/0014-4886(87)90225-1. [DOI] [PubMed] [Google Scholar]
- 32.Winiarski AM, Roy RR, Alford EK, Chiang PC, Edgerton VR. Mechanical properties of rat skeletal muscle after hind limb suspension. Exp Neurol. 1987;96:650–660. doi: 10.1016/0014-4886(87)90226-3. [DOI] [PubMed] [Google Scholar]
- 33.Ohira T, Kawano F, Ohira T, Goto K, Ohira Y. Responses of skeletal muscles to gravitational unloading and/or reloading. J Physiol Sci. 2015;65:293–310. doi: 10.1007/s12576-015-0375-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Narici M, Kayser B, Barattini P, Cerretelli P. Effects of 17-day spaceflight on electrically evoked torque and cross-sectional area of the human triceps surae. Eur J Appl Physiol. 2003;90:275–282. doi: 10.1007/s00421-003-0955-7. [DOI] [PubMed] [Google Scholar]
- 35.Goubel F. Changes in mechanical properties of human muscle as a result of spaceflight. Int J Sports Med. 1997;18(Suppl 4):S285–S287. doi: 10.1055/s-2007-972727. [DOI] [PubMed] [Google Scholar]
- 36.Schneider SV, LeBlanc AD, Taggart LC. Bone and mineral metabolism. In: Nicogossian AE, Huntoon CL, Pool SL, editors. Space physiology and medicine. Philadelphia: A Waverly Company; 1994. [Google Scholar]
- 37.Rambaut PC, Johnston RS. Prolonged weightlessness and calcium loss in man. Acta Astronaut. 1979;6:1113–1122. doi: 10.1016/0094-5765(79)90059-6. [DOI] [PubMed] [Google Scholar]
- 38.Rambaut PC, Leach CS, Whedon GD. A study of metabolic balance in crewmembers of Skylab IV. Acta Astronaut. 1979;6:1313–1322. doi: 10.1016/0094-5765(79)90123-1. [DOI] [PubMed] [Google Scholar]
- 39.Whedon GD, Lutwak L, Rambaut PC, Whittle MW, Smith MC, Reid J, Leach CS, Stadler CR, Stanford DD. Mineral and nitrogen metabolic studies, experiment M701. In: Johnson RS, Dietlein LE, editors. Biomedical results from Skylab NASA SP-377. Washinton, DC: NASA; 1977. [Google Scholar]
- 40.Lang T, LeBlanc A, Evans H, Lu Y, Genant H, Yu A. Cortical and trabecular bone mineral loss from the spine and hip in long-duration spaceflight. J Bone Miner Res. 2004;19:1006–1012. doi: 10.1359/JBMR.040307. [DOI] [PubMed] [Google Scholar]
- 41.LeBlanc AD, Spector ER, Evans HJ, Sibonga JD. Skeletal responses to space flight and the bed rest analog: a review. J Musculoskelet Neuronal Interact. 2007;7:33–47. [PubMed] [Google Scholar]
- 42.Smith SM, Zwart SR. Nutritional biochemistry of spaceflight. Adv Clin Chem. 2008;46:87–130. doi: 10.1016/S0065-2423(08)00403-4. [DOI] [PubMed] [Google Scholar]
- 43.Oganov VS, Schneider VS. Skeletal system. In: Nicogossian AE, Gazenko OG, editors. Space biology and medicine. Reston: American Institute of Aeronautics and Astronautics; 1996. [Google Scholar]
- 44.LeBlanc A, Schneider V, Shackelford L, West S, Oganov V, Bakulin A, Voronin L. Bone mineral and lean tissue loss after long duration space flight. J Musculoskelet Neuronal Interact. 2000;1:157–160. [PubMed] [Google Scholar]
- 45.Miyamoto A, Shigematsu T, Fukunaga T, Kawakami K, Mukai C, Sekiguchi C. Medical baseline data collection on bone and muscle change with space flight. Bone. 1998;22:79S–82S. doi: 10.1016/S8756-3282(98)00020-9. [DOI] [PubMed] [Google Scholar]
- 46.Kapitonova MY, Kuznetsov SL, Salim N, Othman S, Kamauzaman TM, Ali AM, Nawawi HM, Nor-Ashikin MN, Froemming GR. Morphological and phenotypical characteristics of human osteoblasts after short-term space mission. Bull Exp Biol Med. 2014;156:393–398. doi: 10.1007/s10517-014-2357-8. [DOI] [PubMed] [Google Scholar]
- 47.Smith SM, Heer M, Shackelford LC, Sibonga JD, Spatz J, Pietrzyk RA, Hudson EK, Zwart SR. Bone metabolism and renal stone risk during International Space Station missions. Bone. 2015;81:712–720. doi: 10.1016/j.bone.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 48.Watenpaugh DE, Ballard RE, Breit GA, Bernauer EM, Blomqvist CG, Hargens AR. Calf venous compliance measured with head-up tilt equals supine calf compliance. J Gravit Physiol. 1995;2:P21–P22. [PubMed] [Google Scholar]
- 49.Hargens AR, Richardson S. Cardiovascular adaptations, fluid shifts, and countermeasures related to space flight. Respir Physiol Neurobiol. 2009;169(Suppl 1):S30–S33. doi: 10.1016/j.resp.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 50.Tanaka K, Abe C, Awazu C, Morita H. Vestibular system plays a significant role in arterial pressure control during head-up tilt in young subjects. Auton Neurosci. 2009;148:90–96. doi: 10.1016/j.autneu.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 51.Tanaka K, Abe C, Sakaida Y, Aoki M, Iwata C, Morita H. Subsensory galvanic vestibular stimulation augments arterial pressure control upon head-up tilt in human subjects. Auton Neurosci. 2012;166:66–71. doi: 10.1016/j.autneu.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 52.Tanaka K, Tokumiya S, Ishihara Y, Kohira Y, Katafuchi T. Compression stocking length effects on arterial blood pressure and heart rate following head-up tilt in healthy volunteers. Nurs Res. 2014;63:435–438. doi: 10.1097/NNR.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 53.Larsen PN, Moesgaard F, Madsen P, Pedersen M, Secher NH. Subcutaneous oxygen and carbon dioxide tensions during head-up tilt-induced central hypovolaemia in humans. Scand J Clin Lab Invest. 1996;56:17–24. doi: 10.3109/00365519609088583. [DOI] [PubMed] [Google Scholar]
- 54.Guyton AC. Nervous regulation of the circulation, and rapid control of arterial pressure. In: Guyton AC, editor. Textbook of medical physiology. Philadelphia: W.B. Saunders; 1991. [Google Scholar]
- 55.Kirsch KA, Baartz FJ, Gunga HC, Rocker L. Fluid shifts into and out of superficial tissues under microgravity and terrestrial conditions. Clin Investig. 1993;71:687–689. doi: 10.1007/BF00209721. [DOI] [PubMed] [Google Scholar]
- 56.Draeger J, Schwartz R, Groenhoff S, Stern C. Self-tonometry under microgravity conditions. Aviat Space Environ Med. 1995;66:568–570. [PubMed] [Google Scholar]
- 57.Prisk GK, Guy HJ, Elliott AR, Deutschman RA, 3rd, West JB. Pulmonary diffusing capacity, capillary blood volume, and cardiac output during sustained microgravity. J Appl Physiol. 1993;75:15–26. doi: 10.1152/jappl.1993.75.1.15. [DOI] [PubMed] [Google Scholar]
- 58.Buckey JC, Jr, Gaffney FA, Lane LD, Levine BD, Watenpaugh DE, Wright SJ, Yancy CW, Jr, Meyer DM, Blomqvist CG. Central venous pressure in space. J Appl Physiol. 1996;81:19–25. doi: 10.1152/jappl.1996.81.1.19. [DOI] [PubMed] [Google Scholar]
- 59.Lathers CM, Riddle JM, Mulvagh SL, Mukai C, Diamandis PH, Dussack LG, Bungo MW, Charles JB. Echocardiograms during six hours of bedrest at head-down and head-up tilt and during space flight. J Clin Pharmacol. 1993;33:535–543. doi: 10.1002/j.1552-4604.1993.tb04700.x. [DOI] [PubMed] [Google Scholar]
- 60.Sundblad P, Spaak J, Kaijser L. Time courses of central hemodynamics during rapid changes in posture. J Appl Physiol. 2014;116:1182–1188. doi: 10.1152/japplphysiol.00690.2013. [DOI] [PubMed] [Google Scholar]
- 61.Norsk P. Gravitational stress and volume regulation. Clin Physiol. 1992;12:505–526. doi: 10.1111/j.1475-097X.1992.tb00355.x. [DOI] [PubMed] [Google Scholar]
- 62.Gabrielsen A, Pump B, Bie P, Christensen NJ, Warberg J, Norsk P. Atrial distension, haemodilution, and acute control of renin release during water immersion in humans. Acta Physiol Scand. 2002;174:91–99. doi: 10.1046/j.1365-201X.2002.00932.x. [DOI] [PubMed] [Google Scholar]
- 63.Bettinelli D, Kays C, Bailliart O, Capderou A, Techoueyres P, Lachaud JL, Vaida P, Miserocchi G. Effect of gravity on chest wall mechanics. J Appl Physiol. 2002;92:709–716. doi: 10.1152/japplphysiol.00644.2001. [DOI] [PubMed] [Google Scholar]
- 64.Edyvean J, Estenne M, Paiva M, Engel LA. Lung and chest wall mechanics in microgravity. J Appl Physiol. 1991;71:1956–1966. doi: 10.1152/jappl.1991.71.5.1956. [DOI] [PubMed] [Google Scholar]
- 65.Estenne M, Gorini M, Van Muylem A, Ninane V, Paiva M. Rib cage shape and motion in microgravity. J Appl Physiol. 1992;73:946–954. doi: 10.1152/jappl.1992.73.3.946. [DOI] [PubMed] [Google Scholar]
- 66.Leach CS, Alexander WC. Endocrine, electrolyte and fluid volume changes associated with Apollo missions. In: Johnston LF, Dietlein LF, Berry CA, editors. Biomedical results from Apollo. Washington, DC: NASA; 1975. [Google Scholar]
- 67.Leach CS, Rambaut PPC. Biomedical responses of the Skylab crewmen: an overview. In: Johnston LF, Dietlein LF, editors. Biomedical results from Skylab. Washington, DC: NASA; 1977. [Google Scholar]
- 68.Leach CS. Fluid control mechanisms in weightlessness. Aviat Space Environ Med. 1987;58:A74–A79. [PubMed] [Google Scholar]
- 69.Alfrey CP, Udden MM, Leach-Huntoon C, Driscoll T, Pickett MH. Control of red blood cell mass in spaceflight. J Appl Physiol. 1996;81:98–104. doi: 10.1152/jappl.1996.81.1.98. [DOI] [PubMed] [Google Scholar]
- 70.Perhonen MA, Franco F, Lane LD, Buckey JC, Blomqvist CG, Zerwekh JE, Peshock RM, Weatherall PT, Levine BD. Cardiac atrophy after bed rest and spaceflight. J Appl Physiol. 2001;91:645–653. doi: 10.1152/jappl.2001.91.2.645. [DOI] [PubMed] [Google Scholar]
- 71.Levine BD, Pawelczyk JA, Ertl AC, Cox JF, Zuckerman JH, Diedrich A, Biaggioni I, Ray CA, Smith ML, Iwase S, Saito M, Sugiyama Y, Mano T, Zhang R, Iwasaki K, Lane LD, Buckey JC, Jr, Cooke WH, Baisch FJ, Eckberg DL, Blomqvist CG. Human muscle sympathetic neural and haemodynamic responses to tilt following spaceflight. J Physiol. 2002;538:331–340. doi: 10.1113/jphysiol.2001.012575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lee SM, Feiveson AH, Stein S, Stenger MB, Platts SH. Orthostatic intolerance after ISS and space shuttle missions. Aerosp Med Hum Perform. 2015;86:A54–A67. doi: 10.3357/AMHP.EC08.2015. [DOI] [PubMed] [Google Scholar]
- 73.Levine BD. Neural control of the cardiovascular system in space. In: Buckey JC, Homick JL, editors. The Neurolab Spacelab mission: neuroscience research in space. Houston: NASA; 2003. [Google Scholar]
- 74.Buckey JC, Jr, Lane LD, Levine BD, Watenpaugh DE, Wright SJ, Moore WE, Gaffney FA, Blomqvist CG. Orthostatic intolerance after spaceflight. J Appl Physiol. 1996;81:7–18. doi: 10.1152/jappl.1996.81.1.7. [DOI] [PubMed] [Google Scholar]
- 75.Fritsch-Yelle JM, Whitson PA, Bondar RL, Brown TE. Subnormal norepinephrine release relates to presyncope in astronauts after spaceflight. J Appl Physiol. 1996;81:2134–2141. doi: 10.1152/jappl.1996.81.5.2134. [DOI] [PubMed] [Google Scholar]
- 76.Kawada T, Sugimachi M. Open-loop static and dynamic characteristics of the arterial baroreflex system in rabbits and rats. J Physiol Sci. 2016;66:15–41. doi: 10.1007/s12576-015-0412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Meck JV, Waters WW, Ziegler MG, deBlock HF, Mills PJ, Robertson D, Huang PL. Mechanisms of postspaceflight orthostatic hypotension: low alpha1-adrenergic receptor responses before flight and central autonomic dysregulation postflight. Am J Physiol Heart Circ Physiol. 2004;286:H1486–H1495. doi: 10.1152/ajpheart.00740.2003. [DOI] [PubMed] [Google Scholar]
- 78.Waters WW, Ziegler MG, Meck JV. Postspaceflight orthostatic hypotension occurs mostly in women and is predicted by low vascular resistance. J Appl Physiol. 2002;92:586–594. doi: 10.1152/japplphysiol.00544.2001. [DOI] [PubMed] [Google Scholar]
- 79.Tanaka K, Ito Y, Ikeda M, Katafuchi T. RR interval variability during galvanic vestibular stimulation correlates with arterial pressure upon head-up tilt. Auton Neurosci. 2014;185:100–106. doi: 10.1016/j.autneu.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 80.Yates BJ, Kerman IA. Post-spaceflight orthostatic intolerance: possible relationship to microgravity-induced plasticity in the vestibular system. Brain Res Brain Res Rev. 1998;28:73–82. doi: 10.1016/S0165-0173(98)00028-9. [DOI] [PubMed] [Google Scholar]
- 81.Hallgren E, Migeotte PF, Kornilova L, Deliere Q, Fransen E, Glukhikh D, Moore ST, Clement G, Diedrich A, MacDougall H, Wuyts FL. Dysfunctional vestibular system causes a blood pressure drop in astronauts returning from space. Sci Rep. 2015;5:17627. doi: 10.1038/srep17627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hallgren E, Kornilova L, Fransen E, Glukhikh D, Moore ST, Clement G, Van Ombergen A, MacDougall H, Naumov I, Wuyts FL. Decreased otolith-mediated vestibular response in 25 astronauts induced by long-duration spaceflight. J Neurophysiol. 2016;115:3045–3051. doi: 10.1152/jn.00065.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Morita H, Abe C, Tanaka K (2016) Long-term exposure to microgravity impairs vestibulo-cardiovascular reflex. Sci Rep (in press) [DOI] [PMC free article] [PubMed]
- 84.MacNeilage PR, Turner AH, Angelaki DE. Canal–otolith interactions and detection thresholds of linear and angular components during curved-path self-motion. J Neurophysiol. 2010;104:765–773. doi: 10.1152/jn.01067.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Scherer H, Clarke AH. The caloric vestibular reaction in space. Physiological considerations. Acta Otolaryngol. 1985;100:328–336. doi: 10.3109/00016488509126556. [DOI] [PubMed] [Google Scholar]
- 86.Reschke MR, Bloomberg JJ, Harm DL, Huebner WP, Krnavek JM, William H. Visual-vestibular integration as a function of adaptation to space flight and return to Earth. In: Sawin CF, Taylor GR, Smith WL, editors. Extended duration orbiter medical project. Houston: NASA; 1999. [Google Scholar]
- 87.Moore ST, Clement G, Raphan T, Cohen B. Ocular counterrolling induced by centrifugation during orbital space flight. Exp Brain Res. 2001;137:323–335. doi: 10.1007/s002210000669. [DOI] [PubMed] [Google Scholar]
- 88.Clement G, Moore ST, Raphan T, Cohen B. Perception of tilt (somatogravic illusion) in response to sustained linear acceleration during space flight. Exp Brain Res. 2001;138:410–418. doi: 10.1007/s002210100706. [DOI] [PubMed] [Google Scholar]
- 89.Paloski WH, Black FO, Reschke MF, Calkins DS, Shupert C. Vestibular ataxia following shuttle flights: effects of microgravity on otolith-mediated sensorimotor control of posture. Am J Otol. 1993;14:9–17. [PubMed] [Google Scholar]
- 90.Paloski WH, Reschke MF, Black FO, Doxey DD, Harm DL. Recovery of postural equilibrium control following spaceflight. Ann N Y Acad Sci. 1992;656:747–754. doi: 10.1111/j.1749-6632.1992.tb25253.x. [DOI] [PubMed] [Google Scholar]
- 91.Gilbert CA, Stevens PM. Forearm vascular responses to lower body negative pressure and orthostasis. J Appl Physiol. 1966;21:1265–1272. doi: 10.1152/jappl.1966.21.4.1265. [DOI] [PubMed] [Google Scholar]
- 92.Musgrave FS, Zechman FW, Mains RC. Changes in total leg volume during lower body negative pressure. Aerosp Med. 1969;40:602–606. [PubMed] [Google Scholar]
- 93.Convertino VA. Lower body negative pressure as a tool for research in aerospace physiology and military medicine. J Gravit Physiol. 2001;8:1–14. [PubMed] [Google Scholar]
- 94.Bevegard S, Castenfors J, Lindblad LE. Effect of changes in blood volume distribution on circulatory variables and plasma renin activity in man. Acta Physiol Scand. 1977;99:237–245. doi: 10.1111/j.1748-1716.1977.tb10375.x. [DOI] [PubMed] [Google Scholar]
- 95.Charles JB, Lathers CM. Summary of lower body negative pressure experiments during space flight. J Clin Pharmacol. 1994;34:571–583. doi: 10.1002/j.1552-4604.1994.tb02009.x. [DOI] [PubMed] [Google Scholar]
- 96.Gazenko OG, Genin AM, Egorov AD. Summary of medical investigations in the U.S.S.R. manned space missions. Acta Astronaut. 1981;8:907–917. doi: 10.1016/0094-5765(81)90061-8. [DOI] [PubMed] [Google Scholar]
- 97.Goswami N, Loeppky JA, Hinghofer-Szalkay H. LBNP: past protocols and technical considerations for experimental design. Aviat Space Environ Med. 2008;79:459–471. doi: 10.3357/ASEM.2161.2008. [DOI] [PubMed] [Google Scholar]
- 98.Charles JB, Fritsch-Yelle JM, Whitson PA, Wood ML, Brown TE, Fortner GW. Cardiovascular deconditioning. In: Sawin CF, Taylor GR, Smith WL, editors. Extended duration orbiter medical project. Houston: NASA; 1999. [Google Scholar]
- 99.Murthy G, Watenpaugh DE, Ballard RE, Hargens AR. Supine exercise during lower body negative pressure effectively simulates upright exercise in normal gravity. J Appl Physiol. 1994;76:2742–2748. doi: 10.1063/1.357578. [DOI] [PubMed] [Google Scholar]
- 100.Schneider SM, Lee SM, Feiveson AH, Watenpaugh DE, Macias BR, Hargens AR (2016) Treadmill exercise within lower body negative pressure protects leg lean tissue mass and extensor strength and endurance during bed rest. Physiol Rep 4 [DOI] [PMC free article] [PubMed]
- 101.Schneider SM, Watenpaugh DE, Lee SM, Ertl AC, Williams WJ, Ballard RE, Hargens AR. Lower-body negative-pressure exercise and bed-rest-mediated orthostatic intolerance. Med Sci Sports Exerc. 2002;34:1446–1453. doi: 10.1097/00005768-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 102.Watenpaugh DE. Nocturnal lower body positive pressure to counteract microgravity-induced cardiac remodeling/atrophy. J Appl Physiol. 2002;92:2222–2223. doi: 10.1152/japplphysiol.01016.2001. [DOI] [PubMed] [Google Scholar]
- 103.Watenpaugh DE, Ballard RE, Schneider SM, Lee SM, Ertl AC, William JM, Boda WL, Hutchinson KJ, Hargens AR. Supine lower body negative pressure exercise during bed rest maintains upright exercise capacity. J Appl Physiol. 2000;89:218–227. doi: 10.1152/jappl.2000.89.1.218. [DOI] [PubMed] [Google Scholar]
- 104.Watenpaugh DE, O’Leary DD, Schneider SM, Lee SM, Macias BR, Tanaka K, Hughson RL, Hargens AR. Lower body negative pressure exercise plus brief postexercise lower body negative pressure improve post-bed rest orthostatic tolerance. J Appl Physiol. 2007;103:1964–1972. doi: 10.1152/japplphysiol.00132.2007. [DOI] [PubMed] [Google Scholar]
- 105.Zwart SR, Hargens AR, Lee SM, Macias BR, Watenpaugh DE, Tse K, Smith SM. Lower body negative pressure treadmill exercise as a countermeasure for bed rest-induced bone loss in female identical twins. Bone. 2007;40:529–537. doi: 10.1016/j.bone.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Macaulay TR, Brandon R, Macias BR, Lee SMC, Boda WL, Watenpaugh DE, Hargens AR. Treadmill exercise within lower-body negative pressure attenuates simulated spaceflight-induced reductions of balance abilities in men but not women. npj Microgravity. 2016;2:1–8. doi: 10.1038/npjmgrav.2016.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dorfman TA, Levine BD, Tillery T, Peshock RM, Hastings JL, Schneider SM, Macias BR, Biolo G, Hargens AR. Cardiac atrophy in women following bed rest. J Appl Physiol. 2007;103:8–16. doi: 10.1152/japplphysiol.01162.2006. [DOI] [PubMed] [Google Scholar]
- 108.Cavanagh PR, Genc KO, Gopalakrishnan R, Kuklis MM, Maender CC, Rice AJ. Foot forces during typical days on the international space station. J Biomech. 2010;43:2182–2188. doi: 10.1016/j.jbiomech.2010.03.044. [DOI] [PubMed] [Google Scholar]
- 109.Boda WL, Watenpaugh DE, Ballard RE, Hargens AR (2000) Supine lower body negative pressure exercise simulates metabolic and kinetic features of upright exercise. J Appl Physiol (1985) 89: 649–654 [DOI] [PubMed]
- 110.Lambertz D, Perot C, Kaspranski R, Goubel F. Effects of long-term spaceflight on mechanical properties of muscles in humans. J Appl Physiol. 2001;90:179–188. doi: 10.1152/jappl.2001.90.1.179. [DOI] [PubMed] [Google Scholar]
- 111.Hayes J. The first decade of ISS exercise: lessons learned on expeditions 1–25. Aerosp Med Hum Perform. 2015;86:A1–A6. doi: 10.3357/AMHP.EC01.2015. [DOI] [PubMed] [Google Scholar]
- 112.Smith SM, Heer MA, Shackelford LC, Sibonga JD, Ploutz-Snyder L, Zwart SR. Benefits for bone from resistance exercise and nutrition in long-duration spaceflight: evidence from biochemistry and densitometry. J Bone Miner Res. 2012;27:1896–1906. doi: 10.1002/jbmr.1647. [DOI] [PubMed] [Google Scholar]
- 113.Kozlovskaya IB, Yarmanova EN, Yegorov AD, Sepantsov VI, Fomina EV, Tomilovaskaya ES. Russian countermeasure system for adverse effects of microgravity on long-duration ISS flights. Aerosp Med Hum Perform. 2015;86:A24–A31. doi: 10.3357/AMHP.EC04.2015. [DOI] [PubMed] [Google Scholar]
- 114.Sibonga JD, Cavanagh PR, Lang TF, LeBlanc AD, Schneider VS, Shackelford LC, Smith SM, Vico L. Adaptation of the skeletal system during long-duration spaceflight. Clin Rev Bone Miner Metab. 2008;5:249–261. doi: 10.1007/s12018-008-9012-8. [DOI] [Google Scholar]
- 115.Schneider SM, Amonette WE, Blazine K, Bentley J, Lee SM, Loehr JA, Moore AD, Jr, Rapley M, Mulder ER, Smith SM. Training with the International Space Station interim resistive exercise device. Med Sci Sports Exerc. 2003;35:1935–1945. doi: 10.1249/01.MSS.0000093611.88198.08. [DOI] [PubMed] [Google Scholar]
- 116.Loehr JA, Lee SM, English KL, Sibonga J, Smith SM, Spiering BA, Hagan RD. Musculoskeletal adaptations to training with the advanced resistive exercise device. Med Sci Sports Exerc. 2011;43:146–156. doi: 10.1249/MSS.0b013e3181e4f161. [DOI] [PubMed] [Google Scholar]
- 117.Fitts RH, Trappe SW, Costill DL, Gallagher PM, Creer AC, Colloton PA, Peters JR, Romatowski JG, Bain JL, Riley DA. Prolonged space flight-induced alterations in the structure and function of human skeletal muscle fibres. J Physiol. 2010;588:3567–3592. doi: 10.1113/jphysiol.2010.188508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gopalakrishnan R, Genc KO, Rice AJ, Lee SM, Evans HJ, Maender CC, Ilaslan H, Cavanagh PR. Muscle volume, strength, endurance, and exercise loads during 6-month missions in space. Aviat Space Environ Med. 2010;81:91–102. doi: 10.3357/ASEM.2583.2010. [DOI] [PubMed] [Google Scholar]
- 119.English KL, Lee SMC, Loehr JA, Ploutz-Snyder RJ, Ploutz-Snyder LL. Isokinetic strength changes following long-duration spaceflight on the ISS. Aerosp Med Hum Perform. 2015;86:A68–A77. doi: 10.3357/AMHP.EC09.2015. [DOI] [PubMed] [Google Scholar]
- 120.Smith SM, Zwart SR, Heer M, Hudson EK, Shackelford L, Morgan JL. Men and women in space: bone loss and kidney stone risk after long-duration spaceflight. J Bone Miner Res. 2014;29:1639–1645. doi: 10.1002/jbmr.2185. [DOI] [PubMed] [Google Scholar]
- 121.Leblanc A, Matsumoto T, Jones J, Shapiro J, Lang T, Shackelford L, Smith SM, Evans H, Spector E, Ploutz-Snyder R, Sibonga J, Keyak J, Nakamura T, Kohri K, Ohshima H. Bisphosphonates as a supplement to exercise to protect bone during long-duration spaceflight. Osteoporos Int. 2013;24:2105–2114. doi: 10.1007/s00198-012-2243-z. [DOI] [PubMed] [Google Scholar]
- 122.Russell RG. Bisphosphonates: the first 40 years. Bone. 2011;49:2–19. doi: 10.1016/j.bone.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 123.Gupta A, March L. Treating osteoporosis. Aust Prescr. 2016;39:40–46. doi: 10.18773/austprescr.2016.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Czerwinski E. New options of pharmacological treatment of osteoporosis. Ortop Traumatol Rehabil. 2006;8:367–371. [PubMed] [Google Scholar]
- 125.Hadji P, Minne H, Pfeifer M, Bourgeois P, Fardellone P, Licata A, Devas V, Masanauskaite D, Barrett-Connor E. Treatment preference for monthly oral ibandronate and weekly oral alendronate in women with postmenopausal osteoporosis: a randomized, crossover study (BALTO II) Joint Bone Spine. 2008;75:303–310. doi: 10.1016/j.jbspin.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 126.Crandall CJ, Aragaki AK, LeBoff MS, Li W, Wactawski-Wende J, Cauley JA, Margolis KL, Manson JE (2016) Calcium plus vitamin D supplementation and height loss: findings from the Women’s Health Initiative Calcium and Vitamin D clinical trial. Menopause (in press) [DOI] [PMC free article] [PubMed]
- 127.Chandler TJ, Stone MH. The squat exercise in athletic conditioning: a review of the literature. Natl Strength Cond Assoc J. 1991;13:51–58. [Google Scholar]
- 128.Nikawa T, Ishidoh K, Hirasaka K, Ishihara I, Ikemoto M, Kano M, Kominami E, Nonaka I, Ogawa T, Adams GR, Baldwin KM, Yasui N, Kishi K, Takeda S. Skeletal muscle gene expression in space-flown rats. FASEB J. 2004;18:522–524. doi: 10.1096/fj.03-0419fje. [DOI] [PubMed] [Google Scholar]
- 129.Allum JH, Honegger F. Interactions between vestibular and proprioceptive inputs triggering and modulating human balance-correcting responses differ across muscles. Exp Brain Res. 1998;121:478–494. doi: 10.1007/s002210050484. [DOI] [PubMed] [Google Scholar]
- 130.Britton TC, Day BL, Brown P, Rothwell JC, Thompson PD, Marsden CD. Postural electromyographic responses in the arm and leg following galvanic vestibular stimulation in man. Exp Brain Res. 1993;94:143–151. doi: 10.1007/BF00230477. [DOI] [PubMed] [Google Scholar]
- 131.Ray CA, Monahan KD. The vestibulosympathetic reflex in humans: neural interactions between cardiovascular reflexes. Clin Exp Pharmacol Physiol. 2002;29:98–102. doi: 10.1046/j.1440-1681.2002.03614.x. [DOI] [PubMed] [Google Scholar]
- 132.Nakamura Y, Matsuo S, Hosogai M, Kawai Y. Vestibular control of arterial blood pressure during head-down postural change in anesthetized rabbits. Exp Brain Res. 2009;194:563–570. doi: 10.1007/s00221-009-1732-6. [DOI] [PubMed] [Google Scholar]
- 133.Akima H, Katayama K, Sato K, Ishida K, Masuda K, Takada H, Watanabe Y, Iwase S. Intensive cycle training with artificial gravity maintains muscle size during bed rest. Aviat Space Environ Med. 2005;76:923–929. [PubMed] [Google Scholar]
- 134.Iwase S. Effectiveness of centrifuge-induced artificial gravity with ergometric exercise as a countermeasure during simulated microgravity exposure in humans. Acta Astronaut. 2005;57:75–80. doi: 10.1016/j.actaastro.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 135.Iwasaki K, Shiozawa T, Kamiya A, Michikami D, Hirayanagi K, Yajima K, Iwase S, Mano T. Hypergravity exercise against bed rest induced changes in cardiac autonomic control. Eur J Appl Physiol. 2005;94:285–291. doi: 10.1007/s00421-004-1308-x. [DOI] [PubMed] [Google Scholar]
- 136.Yang Y, Baker M, Graf S, Larson J, Caiozzo VJ. Hypergravity resistance exercise: the use of artificial gravity as potential countermeasure to microgravity. J Appl Physiol. 2007;103:1879–1887. doi: 10.1152/japplphysiol.00772.2007. [DOI] [PubMed] [Google Scholar]
- 137.Shiba N, Matsuse H, Takano Y, Yoshimitsu K, Omoto M, Hashida R, Tagawa Y, Inada T, Yamada S, Ohshima H. Electrically stimulated antagonist muscle contraction increased muscle mass and bone mineral density of one astronaut—initial verification on the International Space Station. PLoS One. 2015;10:e0134736. doi: 10.1371/journal.pone.0134736. [DOI] [PMC free article] [PubMed] [Google Scholar]


