Abstract
Background
Injuries, the leading cause of death in children 1–17 years old, are often preventable. Injury patterns are impacted by changes in the child’s environment, shifts in supervision, and caregiver stressors. The objective of this study was to evaluate the incidence and proportion of injuries, mechanisms, and severity seen in Pediatric Emergency Departments (PEDs) during the COVID-19 pandemic.
Methods
This multicenter, cross-sectional study from January 2019 through December 2020 examined visits to 40 PEDs for children < 18 years old. Injury was defined by at least one International Classification of Disease-10th revision (ICD-10) code for bodily injury (S00–T78). The main study outcomes were total and proportion of PED injury-related visits compared to all visits in March through December 2020 and to the same months in 2019. Weekly injury visits as a percentage of total PED visits were calculated for all weeks between January 2019 and December 2020.
Results
The study included 741,418 PED visits for injuries pre-COVID-19 pandemic (2019) and during the COVID-19 pandemic (2020). Overall PED visits from all causes decreased 27.4% in March to December 2020 compared to the same time frame in 2019; however, the proportion of injury-related PED visits in 2020 increased by 37.7%. In 2020, injured children were younger (median age 6.31 years vs 7.31 in 2019), more commonly White (54% vs 50%, p < 0.001), non-Hispanic (72% vs 69%, p < 0.001) and had private insurance (35% vs 32%, p < 0.001). Injury hospitalizations increased 2.2% (p < 0.001) and deaths increased 0.03% (p < 0.001) in 2020 compared to 2019. Mean injury severity score increased (2.2 to 2.4, p < 0.001) between 2019 and 2020. Injuries declined for struck by/against (− 4.9%) and overexertion (− 1.2%) mechanisms. Injuries proportionally increased for pedal cycles (2.8%), cut/pierce (1.5%), motor vehicle occupant (0.9%), other transportation (0.6%), fire/burn (0.5%) and firearms (0.3%) compared to all injuries in 2020 versus 2019.
Conclusions
The proportion of PED injury-related visits in March through December 2020 increased compared to the same months in 2019. Racial and payor differences were noted. Mechanisms of injury seen in the PED during 2020 changed compared to 2019, and this can inform injury prevention initiatives.
Keywords: Pediatrics, Injury prevention, Injuries, Emergency department, Pandemic, Disparities
Introduction
Injuries are the leading cause of death and disability in children 1–17 years of age in the United States (US) (Centers for Disease Control and Prevention Injury Center of Injury Prevention and Control 2022). Infectious diseases and cancer, once primary contributors to pediatric deaths, have decreased with advancements in medical science, while injuries have become the leading cause of death (Cunningham et al. 2018). The environment, an interaction of physical, social, economic, cultural, and demographic components, affects a child’s risk of injury (Peek-Asa and Zwerling 2003). National disasters, global infectious disease burden, and economic crises are examples of environmental changes that have impacted pediatric injuries (Huang et al. 2011). The United States economic recession in 2007–2009 saw an increased in abusive head trauma in children (Huang et al. 2011; Wood et al. 2016). During this same time, disparities in traumatic injuries were seen as areas hit hardest with unemployment also had the highest hospital admission rates for trauma (Coughlin et al. 2018). During the Middle East Respiratory Syndrome (MERS) outbreak in June and July 2015, a study looking at ED utilization rates found that visits for pediatric injury increased by 4.1% compared to similar months in the two prior years (Paek et al. 2017). Studies have consistently shown that influencing these environmental factors are poverty level, access to needed goods and services, and personal and societal anxiety and fear (Drake and Rank 2009; Mack et al. 2018).
On March 13, 2020, the US declared a National Emergency due to the emergence of the novel coronavirus known as SARS-CoV-2 (or COVID-19) (Trump 2020). Within 1 month nearly all 50 states had enacted “shelter-in-place” orders requiring residents to stay within their homes. This resulted in a nationwide closure of schools, playgrounds, daycares, and all places of business deemed “non-essential”. A paradigm emerged where children were home for long periods of time with adult caregivers, who often were required to work full-time from home while also having to care for or provide schooling to children (Claudet et al. 2020). Studies assessing the first months of the pandemic demonstrated a profound decrease in pediatric emergency department (PED) visits (Finkelstein et al. 2021; Delaroche et al. 2021). Some hypothesized that increases in injuries would be demonstrated as a result of the conditions imposed by the pandemic, while others speculated a decrease (Gelder et al. 2020; Keays et al. 2020; Sutherland et al. 2020). The objective of this study was to examine changes in the epidemiology of pediatric injuries during the COVID-19 pandemic among children’s hospitals. We hypothesized that there would be a relative increase in the proportion of injury-related PED visits, with changing patterns of injury mechanism, due to behavior changes during the pandemic. Understanding how widespread environmental changes can influence injury patterns may be useful for informing further injury prevention efforts.
Methods
Study design and data collection
We conducted a multicenter, cross-sectional study of 40 hospital PEDs across the USA and Canada (Fig. 1). This work was supported by the Injury Free Coalition for Kids® (IFCK®), a hospital-based, community-oriented organization led by pediatric physicians, surgeons, and injury prevention specialists. The purpose of the IFCK® is to reduce all injuries to children. The study team comprised 36 hospitals from IFCK® sites and 4 from additional institutions. Study participation was offered to each IFCK® site and was optional. We included all visits to a PED for children less than 18 years of age presenting between January 1, 2019, and December 31, 2020, with an injury. Injury was defined by at least one International Classification of Disease-10th revision (ICD-10) code for bodily injury (S00–T78). We excluded any visit for the same injury within 7 days and those occurring as a complication of surgical and/or medical care (ICD-10 codes T80-88, Y65.8). The study was approved by the Institutional Review Boards at all sites.
Fig. 1.
Map of participating sites
Study protocol
Eligible subjects were identified retrospectively using instructions provided to each enrollment site in a standardized manual of operations (MOO) and data dictionary. All study variables were defined a priori. Each investigator received standardized training, and all data were abstracted directly from the electronic medical record at each institution and uploaded into a REDCap database housed at Cincinnati Children’s Hospital Medical Center, the study’s data coordinating site (Harris et al. 2009). Data were assessed for completeness and accuracy. Any noted discrepancies were reviewed with primary sites. Data sources included PED records, hospital admission records, trauma registries, and ICD-10 billing codes.
Patient characteristics
Demographic characteristics collected for each PED visit included age, sex, race, ethnicity, payor, hospital, region of the country, and home zip code. Race and ethnicity designations were typically based on self-report or hospital registration assignment, per institutional practice. Region was categorized using the US Census designations: Northeast (CT, DC, MA, NY, PA, RI), Midwest (IA, IL, IN, MO, MN, NE, OH), South (Al, AR, FL, GA, KY, TN, TX), West (AZ, CA, CO, OR, WA), and Canada. Injury-related variables included date/time of PED visit and hospital discharge, emergency severity index (ESI) code (range 1–5 with 1 assigned to the most urgent patients), trauma activation (yes/no), PED disposition, admission site (inpatient floor, intensive care unit, operating room, burn unit, psychiatric unit), and outcome (lived/died). PED disposition includes death in the PED, and conversely, outcome (lived/died) includes death at any point in the hospital encounter including after hospital admission. The first twenty ICD-10 codes that corresponded to bodily injury were collected. The first three ICD-10 codes for mechanism and intent of injury (V00–X58 = unintentional, X71–X83 = intentional self-harm, X92–Y09 = assault, Y21–Y33 = undetermined intent, Y35–Y38 = legal intervention) were recorded. For each hospital, the total number of PED visits seen for all causes by week was obtained.
Derived data
Injury severity scores (ISSs) were derived for each visit. The abbreviated injury scale (AIS) is anatomically based and consensus derived. It is the global lexicon of choice for injury severity determination and is used to generate an ISS (Association for the Advancement of Automotive Medicine (AAAM) 2008). The AIS documents each injury sustained by body region and severity on a 1 (minor) to 6 (maximal) scale. AIS scores were derived electronically using a validated map from all ICD-10-CM injury diagnosis codes for each visit (Loftis et al. 2005; Glerum and Zonfrillo 2019). ISSs were calculated by summing the squares of the AIS scores of the three most severely injured body regions with a possible ISS range of 0–75 (Association for the Advancement of Automotive Medicine (AAAM) 2008). If an injury is unsurvivable, denoted by an AIS of 6, the ISS is automatically assigned a value of 75. Additionally, an ISS of 0 indicates an injury where specific body region damage was absent, for example, poisoning and drownings.
A deprivation index was added to each patient encounter. The index, available for each US zip code, is formulated based on a principal components analysis of six American Community Survey measures from US census data (Brokamp et al. 2018, 2019). Those measures include the fraction of the population with income below poverty level, those over 25 year of age with a high school diploma (or equivalent), those with no health insurance, those receiving public assistance income or food stamps, the fraction of vacant homes, and the median household income in the past 12 months (Brokamp et al. 2018). The index provides a number 0 to 1 with 1 representing the most socioeconomically disadvantaged areas.
Data analysis
Data analysis was performed at the State University of New York Upstate Medical University. For comparisons of injuries and PED visits before (2019) and during the pandemic (2020), visits were limited to those occurring beginning week 12 of each calendar year, the first full week of the pandemic in 2020. We included visits occurring beginning March 17th in 2019 and March 15th in 2020. Weekly injury visits as a percentage of total PED visits were calculated for all weeks between January 2019 and December 2020 by dividing the total number of injury PED visits each week by the total number of PED visits each week and multiplying by one hundred. Three sites were unable to provide data on total PED visits by week and were excluded from this calculation. Descriptive statistics were calculated for demographic and clinical characteristics and were compared between 2019 and 2020 using Chi-square and t-tests, as appropriate, with p values < 0.05 deemed statistically significant. Race and ethnicity information were missing in 8% and 8.7% of cases, respectively, and were similar in 2019 and 2020. Descriptive statistics were used to characterize injury data overall and by week and year. The Centers for Disease Control and Prevention (CDC) National Center for Health Statistics Injury Diagnosis Matrices and External Cause-of-Injury (E-Code) Matrices were used to classify nature, mechanism, and intent of injury (Hedegaard et al. 2019, 2020). All statistical analyses were conducted using SAS® (version 9.4, SAS Institute, Inc., Cary, NC).
Results
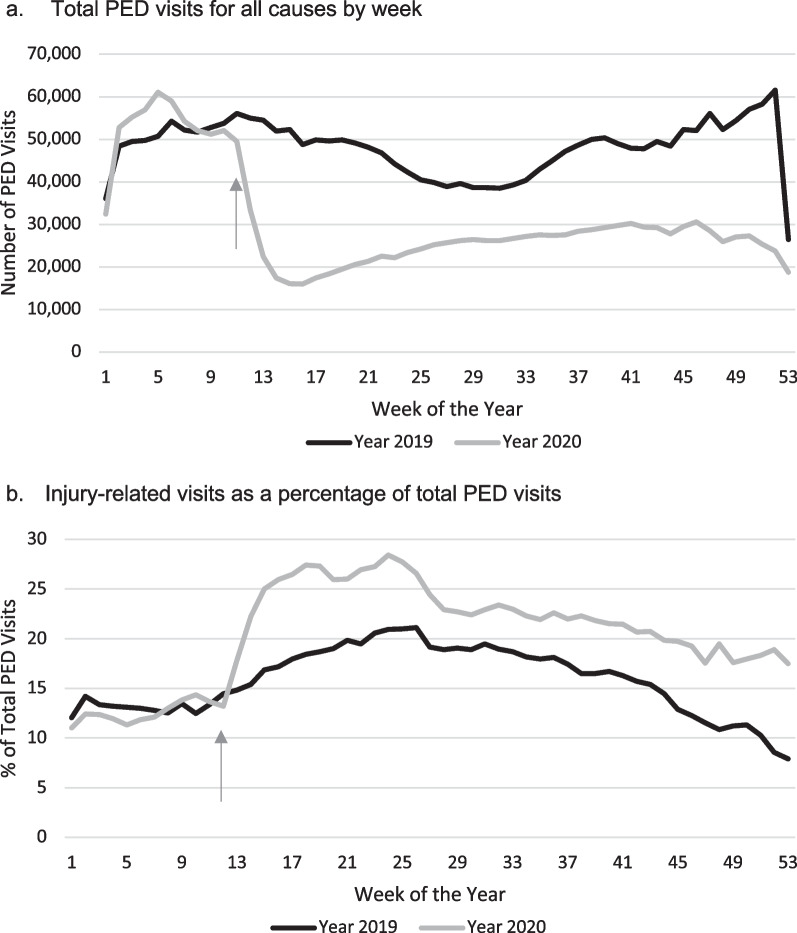
There were 4,181,297 total PED visits for all causes (injury and non-injury) from January 1, 2019, through December 31, 2020. This number represents data from 37 out of the 40 sites. Three sites were unable to contribute data for all causes of PED visits due to technical difficulty in data extraction from the site-specific electronic medical record. There was a 27.4% decrease in visits for all causes from March through December 2020 compared to the same months in 2019 (Fig. 2a).
Fig. 2.
Weekly trends in Pediatric Emergency Department (PED) visits. a Total PED visits for all causes by week. b Injury visits as a percentage of total PED visits. *Arrow denotes week 12 when the USA declared a National Emergency
There were 741,418 injury-related PED visits at 40 participating hospitals from January 1, 2019, through December 31, 2020. Focusing on injuries that occurred during the pandemic months, between March and December of 2019 and 2020 there were 589,083 injury-related PED visits (341,242 in 2019; 247,841 in 2020). There were 93,401 less visits for injuries during March to December 2020 compared to March to December 2019. Compared to the 27.4% decrease in ED visits for all causes, there was a 37.7% increase in the proportion of injury-related visits from March through December 2020 compared to the same months in 2019 (Fig. 2b).
Looking at data from March to December, children who presented to the PED for injuries during the COVID-19 pandemic in 2020 were younger (median age 6.3 years vs 7.3 in 2019), more frequently White, and privately insured (Table 1). The median deprivation index for patients evaluated for injuries decreased from 0.4 in 2019 to 0.3 in 2020 (p < 0.001). During the COVID-19 pandemic, there was a higher percentage of trauma activations (+ 1.5%) and patients triaged at ESI levels 1 and 2 (+ 2.5%). A higher percentage of patients presented to the PED in the evening or overnight (+ 2.5%).
Table 1.
Demographic and PED injury-related visit characteristics before and during the COVID-19 pandemic
| Characteristic | March–December 2019 (n = 341,242) | March–December 2020 (n = 247,841) | p value* |
|---|---|---|---|
| Age, No. (%), years | < 0.001 | ||
| < 1 | 20,717 (6.1) | 15,888 (6.4) | |
| 1–4 | 105,877 (31.0) | 87,418 (35.3) | |
| 5–9 | 86,769 (25.4) | 52,058 (25.0) | |
| 10–14 | 84,736 (24.8) | 52,901 (21.3) | |
| 15–18 | 43,143 (12.6) | 29,576 (11.9) | |
| Sex, No. (%) | < 0.001 | ||
| Male | 194,171 (56.9) | 138,592 (55.9) | |
| Female | 145,102 (42.5) | 108,500 (43.8) | |
| Unknown | 1,969 (0.6) | 749 (0.3) | |
| Race, No. (%)a | < 0.001 | ||
| White | 169,694 (49.7) | 133,135 (53.7) | |
| Black | 85,383 (25.0) | 57,775 (23.3) | |
| AI/AN | 1,177 (0.4) | 888 (0.4) | |
| Asian | 9,252 (2.7) | 6,504 (2.6) | |
| Multiple | 8,641 (2.5) | 7,027 (2.8) | |
| Other | 37,350 (11.0) | 24,619 (9.9) | |
| Unknown | 29,745 (8.7) | 17,893 (7.3) | |
| Ethnicity, No. (%)a | < 0.001 | ||
| Hispanic | 74,271 (21.8) | 50,385 (20.3) | |
| Non-Hispanic | 235,485 (69.0) | 177,476 (71.6) | |
| Unknown | 31,486 (9.2) | 19,980 (8.1) | |
| Payor, No. (%) | < 0.001 | ||
| Public | 176,606 (51.7) | 120,583 (48.7) | |
| Private | 108,976 (31.9) | 86,028 (34.7) | |
| Military | 4,083 (1.2) | 3,200 (1.3) | |
| Self | 13,142 (3.9) | 9,920 (4.0) | |
| Canadian | 8,594 (2.5) | 5,457 (2.2) | |
| International | 218 (0.1) | 100 (0.0) | |
| Other/unknown | 29,623 (8.7) | 22,553 (9.1) | |
| Deprivation Index (0–1) | |||
| Median (IQR) | 0.4 (0.3–0.4) | 0.3 (0.3–0.4) | < 0.001 |
| Triage ESI Code, No. (%) | < 0.001 | ||
| 1 | 3,635 (1.1) | 3,434 (1.4) | |
| 2 | 53,545 (15.7) | 44,365 (17.9) | |
| 3 | 122,556 (35.9) | 92,142 (37.2) | |
| 4 | 140,686 (41.2) | 95,281 (38.4) | |
| 5 | 14,340 (4.2) | 8,177 (3.3) | |
| Unknown | 6,480 (1.9) | 4,442 (1.8) | |
| Trauma activation, No. (%) | < 0.001 | ||
| Yes | 23,562 (6.9) | 20,706 (8.4) | |
| No | 238,841 (70.0) | 173,335 (69.9) | |
| Unknown | 78,839 (23.1) | 53,800 (21.7) | |
| Time of day PED visit, No. (%)b | < 0.001 | ||
| 8:00–15:59 | 113,554 (35.0) | 75,897 (32.5) | |
| 1600–23:59 | 169,740 (52.4) | 125,644 (53.7) | |
| 00:00–07:59 | 40,820 (12.6) | 32,323 (13.8) | |
| Day of PED visit, No. (%) | < 0.001 | ||
| Sunday | 50,649 (14.8) | 38,070 (15.4) | |
| Monday | 50,686 (14.9) | 36,498 (14.7) | |
| Tuesday | 48,358 (14.2) | 34,491 (13.9) | |
| Wednesday | 47,360 (13.9) | 33,929 (13.7) | |
| Thursday | 46,933 (13.8) | 34,047 (13.7) | |
| Friday | 47,987 (14.0) | 33,757 (13.6) | |
| Saturday | 49,269 (14.4) | 37,049 (15.0) | |
| Weekday | 24,1324 (70.7) | 172,722 (69.7) | |
| Weekend | 99,918 (29.3) | 75,119 (30.3) | |
| PED length of stay, hours, median (IQR)c | 3 (2–4) | 2 (2–4) | 0.691 |
| Hospital length of stay, hours, median (IQR)c | 36 (20–72) | 36 (20–75) | 0.006 |
| Region, No. (%) | < 0.001 | ||
| Northeast | 95,208 (27.9) | 71,879 (29.0) | |
| Midwest | 78,623 (23.1) | 60,139 (24.3) | |
| South | 102,463 (30.0) | 76,721 (31.0) | |
| West | 56,330 (16.5) | 33,640 (13.5) | |
| Canada | 8618 (2.5) | 5462 (2.2) |
AI/AN, American Indian/Alaskan Native; PED, Pediatric Emergency Department; ESI, emergency severity index
*Where the p value is listed on the characteristic line, the p value is representative of a difference noted in the category
aRace and ethnicity numbers may have some overlap as these are not all mutually exclusive
bMissing data from one site (n = 557,978)
cImprobable values for PED length of stay (> 48 h) and hospital length of stay (> 180 days) were excluded. This included n = 1892 in the PED length of stay and n = 83 in the hospital length of stay
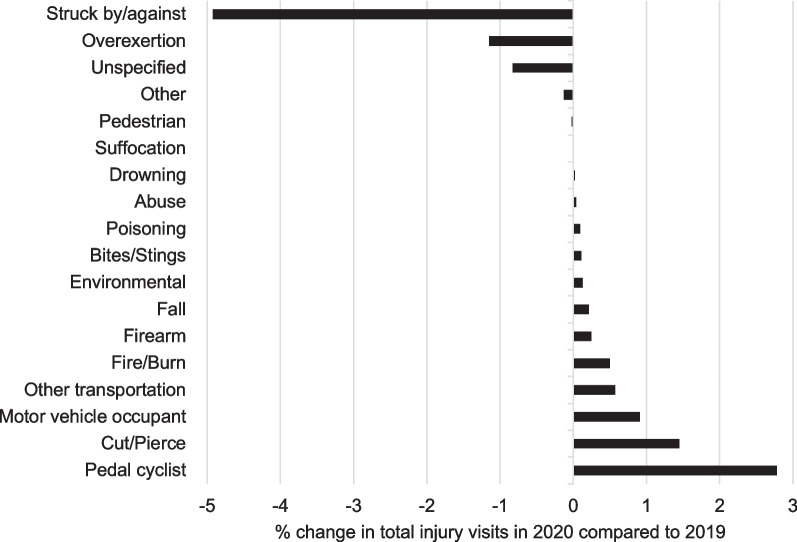
A higher proportion of injuries presenting to PEDs during the pandemic resulted in admission to the hospital (+ 2.2%) and intensive care unit (+ 0.9%) and in a greater percentage of deaths (+ 0.03%) (Table 2). The mean ISS increased marginally in 2020 compared to 2019; however, greater percentages of injuries shifted into the “moderate” to “very severe” ISS categories in 2020. Only 46.2% (274,404) of all injury-related visits had a mechanism/intent documented. Of those documented, there were more intentional self-harm (+ 0.4%) and fewer assaults (− 1.0%) in 2020 (Table 2). The top two reported mechanisms both years were falls and struck by/against. There was a decrease in the percentage of injuries caused by struck by/against and overexertion mechanisms in 2020 compared to 2019 (Fig. 3). Pedal cyclist injuries demonstrated the largest change of any mechanism (+ 2.8%) from 2019 to 2020. Other injuries which increased included cut/pierce, motor vehicle occupant crash, other transportation crash (including all-terrain vehicle), and fire/burn, which each had a > 0.5% increase in the proportion of PED visits in 2020 (Fig. 3). Notably, the proportion of injuries that were the result of a firearm increased nearly twofold (0.35–0.60%) from 2019 to 2020, and in 2020, 127 more children were injured by firearms compared to 2019.
Table 2.
Injury pattern characteristics before and during the COVID-19 pandemic
| Characteristic | March–December 2019 (n = 341,242) |
March–December 2020 (n = 247,841) |
p value* |
|---|---|---|---|
| ISS, mean (SD) | 2.2 (2.6) | 2.4 (2.9) | < 0.001 |
| ISS categories, No. (%) | < 0.001 | ||
| 0 | 96,729 (29.0) | 67,673 (27.9) | |
| 1–8 (Mild) | 226,040 (67.8) | 164,827 (68.1) | |
| 9–15 (Moderate) | 9089 (2.7) | 8160 (3.4) | |
| 16–24 (Severe) | 872 (0.3) | 865 (0.4) | |
| ≥ 25 (Very severe) | 485 (0.2) | 486 (0.2) | |
| Intent, No. (%)a | < 0.001 | ||
| Unintentional | 152,587 (95.7) | 108,716 (96.2) | |
| Intentional self-harm | 1687 (1.1) | 1744 (1.5) | |
| Assault | 4630 (2.9) | 2197 (1.9) | |
| Undetermined intent | 392 (0.2) | 345 (0.3) | |
| Legal intervention | 82 (0.1) | 24 (0.1) | |
| PED disposition, No. (%) | < 0.001 | ||
| Discharge | 298,190 (87.4) | 210,777 (85.0) | |
| Admit | 36,759 (10.8) | 32,149 (13.0) | |
| Died | 87 (0.0) | 122 (0.1) | |
| Otherb/unknown | 6206 (1.8) | 4793 (1.9) | |
| Admitting unit, No. (%)c | < 0.001 | ||
| Ward | 26,176 (71.2) | 22,736 (70.7) | |
| Intensive care unit | 4059 (11.0) | 3831 (11.9) | |
| Operating room | 3537 (9.6) | 2679 (8.3) | |
| Psychiatry | 966 (2.6) | 833 (2.7) | |
| Burn | 522 (1.5) | 452 (1.4) | |
| Unknown | 1499 (4.1) | 1618 (5.0) | |
| Status, No. (%) | < 0.001 | ||
| Lived | 317,254 (93.0) | 229,510 (92.6) | |
| Died | 335 (0.1) | 327 (0.1) | |
| Unknown | 23,653 (6.9) | 18,004 (7.3) |
PED, Pediatric Emergency Department; ISS, Injury Severity Score
*Where the p value is listed on the title line of the characteristic, the p value is representative of a difference noted in the category
aAmong n = 272,404 with classifiable external cause codes
b“Other” includes transfer to another facility for psychiatric admission, transfer to another hospital, and left prior to formal discharge
cAmong n = 68,908 patients admitted to hospital
Fig. 3.
Percentage change in mechanisms of injury in 2020 versus 2019. Among N = 243,969 visits with classifiable external cause codes
When considering types of bodily injuries, a lower percentage of injuries presenting to the PED had superficial contusions (− 1.7%) and internal organ injuries (− 0.4%) in 2020 compared to 2019. However, there were increases in lacerations (+ 4.9%), fractures/dislocations (+ 1.5%), poisonings (+ 1.3%), retained foreign bodies (+ 1.2%), burns (+ 0.5%), crush/amputations (+ 0.07%), and vascular injuries (+ 0.04%).
Discussion
During the first months of the COVID-19 pandemic, the world saw dramatic shifts in work, home, school, and recreational activities (Claudet et al. 2020). While visits to PEDs for all causes decreased across the country, we sought to evaluate the impact of this change on pediatric injuries specifically. We found that the number of PED visits for all causes decreased 27% across the first 9 months of the pandemic; however, the proportion of injury-related PED visits increased by 38%. A greater percentage of these injury-related visits resulted in hospital admissions and deaths. Mechanisms often due to recreational and sport activities (e.g., struck by/against and overexertion) decreased dramatically, whereas injuries from single-user activities (e.g., bicycle, all-terrain vehicles, horseback riding) increased. Proportions of firearm injuries, poisonings, and burns, which may have occurred at home, also increased.
Similar to prior studies, our data demonstrate a decrease in PED visits for all causes throughout the first 9 months of the pandemic (Finkelstein et al. 2021; Delaroche et al. 2021; Lowe et al. 2021; Romano et al. 2021). Specific to injuries, a study using data from an administrative database of children’s hospitals reported a 26.6% decrease in PED injury-related visits during the first year of the COVID-19 pandemic (Lowe et al. 2021). This study defined injury differently than our study. Our study examined all ED visits for any bodily injury using S and T ICD-10 codes, while the previous study identified injuries by mechanism. We found that among our 40 sites, 53.8% of the population was missing a billing code for mechanism. Thus, the previous study may have been an under-representation of all pediatric injuries.
The COVID-19 pandemic drew attention to US racial, ethnic, and socioeconomic disparities in infection rates, access to medical care, and vaccination status (Lowe et al. 2021; Romano et al. 2021; Kricorian and Turner 2021). Individuals with lower socioeconomic status, public insurance and those from marginalized populations were less likely to seek care in an ED during the pandemic (Lowe et al. 2021). This is in contrast to ED utilization prior to the pandemic where individuals with public insurance were more likely to utilize the ED for various reasons, such as less access to after-hours primary care (Sen et al. 2022; Chande et al. 1996). In our study, there was a decrease in the median deprivation index of those individuals who sought PED care in 2020, indicating less PED visits from socioeconomically disadvantaged areas. Additionally, we found that pediatric patients who were White and who had private insurance were a higher proportion of those presenting with an injury during the study pandemic year. Although reasons for this are not well understood, this may be related to the same reasons why those from marginalized populations had lower overall ED visits rates during the pandemic (Lowe et al. 2021).
Our data shows a higher proportion of PED injury-related visits were assigned ESI levels indicating more severe injuries and that a greater percentage were trauma activations during 2020 compared to the year prior. While the small difference in mean ISS between the 2 years represent minor injury and may not be clinically meaningful, we did find that a higher proportion of injuries shifted into the “moderate”-to-“very-severe” ISS categories. The triangulation of these elevated surrogates for injury severity, in addition to the 0.03% increase in the proportion of deaths, resulting in an additional 35 deaths in children, indicates that injuries were overall more severe and outcomes worse in our population during the pandemic. Our study population also demonstrated a 2.2% increase in the proportion of injuries requiring hospital admission and a nearly 1% increase in the percentage admitted to the intensive care unit during the COVID-19 pandemic. A similar pattern has been documented in a prior study (Wells et al. 2022). The significance of these increases is further highlighted when considering that hospitalizations decreased for all causes during the same timeframe (Pelletier et al. 2020).
We saw changes in the mechanisms of injury presenting to PEDs during the pandemic compared to the year prior. The proportion of injuries from being struck by/against and overexertion decreased in 2020. Sports-related injuries contribute to both mechanisms, and studies have shown a decrease in sports participation and sport-related injury visits to PEDs during the pandemic (Sabbagh et al. 2022; Post et al. 2022). Pedal cyclist saw the highest percentage increase in injuries in our population during the pandemic. Bicycle sales increased in 2020 and may be due to factors including more time doing single-user activities, an increasing desire for fitness, or a need for transportation with lesser perceived infection risk than some public options (Dowell and Hait 2021). Our findings are consistent with other studies reporting the same increase in cyclist injuries (Wells et al. 2022; Oudtshoorn et al. 2021).
In addition to these changes in injury mechanisms, we report additional increases in several other mechanism types including motor vehicle occupant crashes and firearm-related injuries. We found a nearly 1% increase in the proportion of injuries from motor vehicle occupant crashes. This same trend has been reported in other studies, including data from the National Highway Traffic Safety Administration showing a 6.8% increase in traffic fatalities for all ages in 2020 compared to 2019 (Chaudhari et al. 2022; Stewart 2020). Additionally, firearm injuries have gained increased national attention as they are now the number one cause of death in children over the age of 1 year (Lee et al. 2022). A multi-institutional study of nine Level 1 pediatric trauma centers found an 87% greater odds of injured pediatric patients presenting with a firearm injury during the pandemic compared to the year prior (Collings et al. 2022). Our study supports these findings with a nearly doubling of the percentage of injuries due to firearms seen in 2020 as compared to 2019. Prior studies have shown that firearm purchases increased during the pandemic and parents describe storing firearms in more accessible locations (Schleimer et al. 2021; Sokol et al. 2021). It is possible that children being home with more access to firearms may contribute to the increase. Regardless, the morbidity and mortality associated with this mechanism are great and thus must be a focus for policy and prevention efforts.
The intent of injury changed during the pandemic with increases in the proportion of injury-related PED visits that were categorized as intentional self-harm. These injuries are likely associated with depression and/or suicidal ideation (e.g., intention cutting) or suicide attempts. The effects of the COVID-19 pandemic on mental health have been staggering (Moreno et al. 2020; Hafstad and Augusti 2021). Experts in psychiatry warned early in the pandemic of the possible effects that social distancing, isolation, and fear might have on mental health and suicide rates (Gunnell et al. 2020; John et al. 2020). A renewed focus on mental health is imperative for children to begin to address and mitigate the effects of the pandemic. PEDs are often underequipped to address the increasing population of patients presenting for self-harm, which warrants further funding and investigation.
This study has a number of limitations. These data are retrospective and extracted from the electronic health records resulting in some missing information. We do not have information on disability or long-term outcomes. Injury mechanisms and intent were not consistently documented, or categorized as non-specific; therefore, we could not accurately classify all injury types. Information was also missing for some demographic characteristics, such as race and ethnicity. We searched for injuries based specifically on ICD-10 codes for injury type to provide a thorough review of all potential injuries, implemented robust quality assurance and control measures in the study protocol, and found that missing data were similar across the years, limiting bias. We also recognize that hospital resources and admitting units across institutions differ, which may have resulted in some misclassification. Finally, the data presented in this study are the representation of 40 hospitals, representing 25 states, across the USA and Canada, but are not population-based data. We recognize that there are several large databases that address pediatric injuries, including but not limited to the National Electronic Injury Surveillance System (NEISS), National Trauma Data Bank, and Web-based Injury Statistics Query and Reporting System. We chose to establish our own database as no single previously established database allowed for a comprehensive review of all injury types (including those admitted and discharged from the PED) and assessment of injury severity and complete demographics (including zip code data) in a timely manner. Children who present to non-pediatric-specific EDs were not included, and there may be variability in demographics, access to medical care, or safety practices in different regions of North America not captured in this study. Thus, there may be limitations to the generalizability of our findings. Nonetheless, this study represents a large sample size of pediatric patients presenting to PEDs with injuries with a wide geographic distribution to characterize injury patterns to children during the COVID-19 pandemic.
Conclusion
The COVID-19 pandemic in 2020 is associated with increases in the proportion of children presenting to PEDs for injuries compared to 2019, including increases by specific injury mechanism. There were differences by race and payor among those seeking care for injuries. The changes in the distribution of injury types and severity seen in the PED should be factored into the preparation for response to any pandemic, inclusive of prevention efforts. The understanding of changes in injury patterns associated with the COVID-19 pandemic can serve as a catalyst for future injury prevention initiatives including state and national policy injury-specific policy changes and informing community and hospital partnerships.
Acknowledgements
We would like to acknowledge the Injury Free Coalition for Kids organization for their support of this academic endeavor. Mackenzie Ferguson, Andrew Mason, Emiri Matsuda, Erin Matusik, Dawn Porter, Gia Ramsey Moritz, Andrew Richardson, Dr. Jonathan Rochlin, Olga Semenova, Norma-Jean Simon, and Melanie Stroud for assisting with data extraction at the primary site. Drs. Kirsten Bechtel, Emily Christison-Lagay, Zoabe Hafeez, Ms. Rebecca Melvin and Kristel Wetjen for assisting with data extraction and data management at this primary site. Jennifer Mull for assisting with data extraction and management and regulatory management at the primary site. Pam Hoogerwerf for assisting with data extraction and IRB submission at the primary site. Umme-Aiman Gurji and Drs. Stephanie Boyd, Hunaid Gurji, Elizabeth Powell for assisting with database management at the primary site. J. Morag MacKay, Hope Mullins, and Drs. Barbara Gaines, Michael Hirsh, Kimberly Kay Lopez, Laura Sartori, Claudia Yeung, David Guernsey for serving as site mentors for our authors.
Abbreviations
- US
United States
- PED
Pediatric Emergency Department
- IFCK
Injury Free Coalition for Kids
- ICD-10
International Classification of Disease-10th revision
- MOO
Manual of Operations
- ESI
Emergency Severity Index
- ISS
Injury Severity Score
- AIS
Abbreviated Injury Scale
- CDC
Centers for Disease Control and Prevention
Author contributions
HRH and WJP conceptualized and designed the study, designed the data collection instruments, coordinated and supervised data collection, drafted the initial manuscript, and critically reviewed and revised the manuscript. MF assisted with study conceptualization, data analysis, interpretation of data, and critically reviewed and revised the manuscript. DLA, PD, JOO, and PU conceptualized and designed the study, assisted with drafting the initial manuscript, and critically reviewed and revised the manuscript for important intellectual content. MRZ provided content expertise (injury severity score), assisted with drafting the initial manuscript, and critically reviewed and revised the manuscript for important intellectual content. ELJ and PC assisted with data collection and critically reviewed and revised the manuscript. MA, KB, S. Schroter, S. Strotmeyer, KAD, LKM, AMM, JD, RFL, BA, KAL, MV, MNL, AWK, KM, SMR, LKL, TCS, MMA, MH, MJ, AM, SCR, NGU, AB, MDH, TR, CJ, LM, QF, LDC, DJ, MTR, JMP, SC, and BKY coordinated and supervised data acquisition at their respective institutions and critically reviewed and revised the manuscript. All authors approved the submitted final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
Dr. Wendy J. Pomerantz received a grant from the Division of Emergency Medicine at Cincinnati Children’s Hospital Medical Center to support the Data Coordinating Center. The other authors received no additional funding. The funder did not participate in the work.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to limitations in the data use agreements with the 40 sites but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center (IRB#2020-0647), which served as the data coordinating center. The study was also approved the Institutional Review Board at each site individually. All methods were performed in accordance with the ethical standards as laid down in the Declaration of Helsinki and its later amendments. The study was approved with a waiver of consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Association for the Advancement of Automotive Medicine (AAAM). The Abbreviated Injury Scale (AIS) 2005—update 2008; 2008. [PMC free article] [PubMed]
- Brokamp C, Wolfe C, Lingren T, Harley J, Ryan P. Decentralized and reproducible geocoding and characterization of community and environmental exposures for multisite studies. J Am Med Inform Assoc. 2018;25(3):309–314. doi: 10.1093/jamia/ocx128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brokamp C, Beck AF, Goyal NK, Ryan P, Greenberg JM, Hall ES. Material community deprivation and hospital utilization during the first year of life: an urban population-based cohort study. Ann Epidemiol. 2019;30:37–43. doi: 10.1016/j.annepidem.2018.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Injury Center of Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). www.cdc.gov/injury/wisqars. Accessed 16 May 2022.
- Chande VT, Krug SE, Warm EF. ED utilization study. Pediatr Emerg Care. 1996;12(1):27–30. doi: 10.1097/00006565-199602000-00008. [DOI] [PubMed] [Google Scholar]
- Chaudhari PP, Anderson M, Ourshalimian S, et al. Epidemiology of pediatric trauma during the coronavirus disease-2019 pandemic. J Pediatr Surg. 2022;57(2):284–290. doi: 10.1016/j.jpedsurg.2021.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claudet I, Marchand-Tonel C, Ricco L, Houze-Cerfon C-H, Lang T, Brehin C. During the COVID-19 quarantine, home has been more harmful than the virus for children! Pediatr Emerg Care. 2020;36(9):e538–e540. doi: 10.1097/PEC.0000000000002205. [DOI] [PubMed] [Google Scholar]
- Collings AT, Farazi M, van Arendonk KJ, et al. The COVID-19 pandemic and associated rise in pediatric firearm injuries: a multi-institutional study. J Pediatr Surg. 2022;57(7):1370–1376. doi: 10.1016/j.jpedsurg.2022.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin K, Hayward RD, Fessler M, Edhayan E. Changes in trauma admission rates and mechanisms during recession and recovery: evidence from the Detroit metropolitan area. Int J Public Health. 2018;63(7):847–854. doi: 10.1007/s00038-018-1087-5. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Walton MA, Carter PM. The major causes of death in children and adolescents in the United States. N Engl J Med. 2018;379(25):2468–2475. doi: 10.1056/NEJMsr1804754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delaroche AM, Rodean J, Aronson PL, et al. Pediatric emergency department visits at US children’s hospitals during the COVID-19 pandemic. Pediatrics. 2021;127(4):e2020039628. doi: 10.1542/peds.2020-039628. [DOI] [PubMed] [Google Scholar]
- Dowell EKP, Hait AW. Surge in demand prompts bicycle shortages, higher prices. United States Census Bureau. 2021. census.gov/library/stories/2021/06/consumers-turn-to-biking-for-safe-fun-exercise-during-pandemic.html. Accessed 15 Aug 2022.
- Drake B, Rank MR. Children and youth services review the racial divide among American children in poverty: reassessing the importance of neighborhood. Child Youth Serv Rev. 2009;31(12):1264–1271. doi: 10.1016/j.childyouth.2009.05.012. [DOI] [Google Scholar]
- Finkelstein Y, Maguire B, Zemek R, et al. Effect of the COVID-19 pandemic on patient volumes, acuity, and outcomes in pediatric emergency departments a nationwide study. Pediatr Emerg Care. 2021;37(8):427–434. doi: 10.1097/PEC.0000000000002484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glerum KM, Zonfrillo MR. Validation of an ICD-9-CM and ICD-10-CM map to AIS 2005 update 2008. Inj Prev. 2019;25(2):90–92. doi: 10.1136/injuryprev-2017-042519. [DOI] [PubMed] [Google Scholar]
- Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafstad GS, Augusti EM. A lost generation? COVID-19 and adolescent mental health. Lancet Psychiatry. 2021;8(8):640–641. doi: 10.1016/S2215-0366(21)00179-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Johnson RL, Garnett MF, Thomas KE. The 2020 International Classification of Diseases, 10th Revision, Clinical Modification injury diagnosis framework for categorizing injuries by body region and nature of injury. National health statistics reports; no 150. Hyattsville, MD: National Center for Health Statistics; 2020. [PubMed]
- Hedegaard H, Johnson RL, Garnett MF, Thomas KE. The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) external cause-of-injury framework for categorizing mechanism and intent of injury. National health statistics reports; no 136. Hyattsville, MD: National Center for Health Statistics; 2019. [PubMed]
- Huang MI, O’Riordan MA, Fitzenrider E, McDavid L, Cohen AR, Robinson S. Increased incidence of nonaccidental head trauma in infants associated with the economic recession: clinical article. J Neurosurg Pediatr. 2011;8(2):171–176. doi: 10.3171/2011.5.PEDS1139. [DOI] [PubMed] [Google Scholar]
- John A, Pirkis J, Gunnell D, Appleby L, Morrissey J. Trends in suicide during the covid-19 pandemic. The BMJ. 2020;371:m4352. doi: 10.1136/bmj.m4352. [DOI] [PubMed] [Google Scholar]
- Keays G, Friedman D, Gagnon I. Pediatric injuries in the time of covid-19. Health Promot Chronic Dis Prev Can. 2020;40(11–12):336–341. doi: 10.24095/hpcdp.40.11/12.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kricorian K, Turner K. COVID-19 vaccine acceptance and beliefs among Black and Hispanic Americans. PLoS ONE. 2021;16(8):e0256122. doi: 10.1371/journal.pone.0256122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee LK, Douglas K, Hemenway D. Crossing lines—a change in the leading cause of death among U.S. children. New Engl J Med. 2022;386(16):1485–1487. doi: 10.1056/NEJMp2200169. [DOI] [PubMed] [Google Scholar]
- Loftis K, Price J, Gillich P, et al. Development of an expert based ICD-9-CM and ICD-10-CM map to AIS 2005 update 2008. Traffic Inj Prev. 2016;17(Supp 1):1–5. doi: 10.1080/15389588.2016.1191069. [DOI] [PubMed] [Google Scholar]
- Lowe J, Brown I, Duriseti R, et al. Emergency department access during covid-19: disparities in utilization by race/ethnicity, insurance, and income. West J Emerg Med. 2021;22(3):552–560. doi: 10.5811/westjem.2021.1.49279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack K, Ballesteros M, Sleet D, Williams D, Simon T. The epidemiology of unintentional and violence-related injury morbidity and mortality among children and adolescents in the United States. Int J Environ Res Public Health. 2018;15(4):616. doi: 10.3390/ijerph15040616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paek SH, Kim DK, Lee JH, Kwak YH. The impact of middle east respiratory syndrome outbreak on trends in emergency department utilization patterns. J Korean Med Sci. 2017;32(10):1576–1580. doi: 10.3346/jkms.2017.32.10.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek-Asa C, Zwerling C. Role of environmental interventions in injury control and prevention. Epidemiol Rev. 2003;25(1):77–89. doi: 10.1093/epirev/mxg006. [DOI] [PubMed] [Google Scholar]
- Pelletier JH, Rakkar J, Au AK, Fuhrman D, Clark RSB, Horvat CM. Trends in US Pediatric Hospital admissions in 2020 compared with the decade before the COVID-19 pandemic. JAMA Netw Open. 2021;4(2):e2037227. doi: 10.1001/jamanetworkopen.2020.37227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post EG, Rivera MJ, Doss D, Eberman LE. Parent decision-making regarding youth sport participation during the COVID-19 pandemic. J Community Health. 2022;47(4):687–696. doi: 10.1007/s10900-022-01078-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano SD, Blackstock AJ, Taylor EV, et al. Trends in racial and ethnic disparities in COVID-19 hospitalizations, by region-United States, March–December 2020. MMWR Morb Mortal Wkly Rep. 2021;70:560–565. doi: 10.15585/mmwr.mm7015e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabbagh RS, Shah NS, Kanhere AP, Hoge CG, Thomson CG, Grawe BM. Effect of the COVID-19 pandemic on sports-related injuries evaluated in US emergency departments. Orthop J Sports Med. 2022;10(2):1–10. doi: 10.1177/23259671221075373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleimer JP, McCort CD, Shev AB, et al. Firearm purchasing and firearm violence during the coronavirus pandemic in the United States: a cross-sectional study. Inj Epidemiol. 2021;8(1):1–10. doi: 10.1186/s40621-021-00339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen BP, Brisendine A, Yang N, Ghosh P. Disparities by race and insurance-status in declines in pediatric ED utilization during the COVID19 pandemic. PLoS ONE. 2022;17(2):e0262490. doi: 10.1371/journal.pone.0262490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol RL, Marineau L, Zimmerman MA, Rupp LA, Cunningham RM, Carter PM. Why some parents made firearms more accessible during the beginning of the COVID-19 pandemic: results from a national study. J Behav Med. 2021;44(6):867–873. doi: 10.1007/s10865-021-00243-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart T. Overview of motor vehicle crashes in 2020 (report No. DOT HS 813 266). National Highway Traffic Safety Administration. 2022.
- Sutherland M, McKenney M, Elkbuli A. Vehicle related injury patterns during the COVID-19 pandemic: What has changed? Am J Emerg Med. 2020;38(9):1710–1714. doi: 10.1016/j.ajem.2020.06.006. [DOI] [PubMed] [Google Scholar]
- Trump D. Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. Proclamations. 2020. https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/. Accessed 31 May 2020.
- van Gelder N, Peterman A, Potts A, et al. COVID-19: reducing the risk of infection might increase the risk of intimate partner violence. EClinicalMedicine. 2020;21:100348. doi: 10.1016/j.eclinm.2020.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Oudtshoorn S, Chiu KYC, Khosa J. Beware of the bicycle! An increase in paediatric bicycle related injuries during the COVID-19 period in Western Australia. ANZ J Surg. 2021;91(6):1154–1158. doi: 10.1111/ans.16918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells JM, Rodean J, Cook L, et al. Injury-related pediatric emergency department visits in the first year of COVID-19. Pediatrics. 2022;150(4):e2021054545. doi: 10.1542/peds.2021-054545. [DOI] [PubMed] [Google Scholar]
- Wood JN, French B, Fromkin J, et al. Association of pediatric abusive head trauma rates with macroeconomic indicators. Acad Pediatr. 2016;16(3):224–232. doi: 10.1016/j.acap.2015.05.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to limitations in the data use agreements with the 40 sites but are available from the corresponding author on reasonable request.