Abstract
Whole body plethysmography (WBP) is used to quantify pulmonary function in conscious, unrestrained mice. We determined currently whether time of day and environmental lighting influence day-to-day reproducibility of pulmonary function, and quantifed the necessary habituation time in the WBP chamber. Two-month-old male C57BL6 and mdx mice (n = 8/group, reverse light cycle), were examined on consecutive days using a calibrated WBP chamber and manufacturer software was used to calculate respiratory measures. Respiratory data stabilized between 5–10 min for all variables. Mice exhibited time of day respiratory differences, performing more forceful and less frequent breaths midday (11:45 a.m. and 3:00 p.m.) compared to 7:30 a.m. WBP performed in darkened conditions elicited more forceful breathing than lit conditions. Day-to-day reproducibility during controlled conditions ranged from r 2 = 0.58 to 0.62 for the functional measures. Findings indicate reproducible respiratory data are obtainable following a 15-min chamber habituation and standardization of time of day and room lighting.
Keywords: Mdx, Respiration, Whole body plethysmography
Introduction
Whole body plethysmography (WBP) has been used for decades to estimate respiratory function in animals [1–3]. Interest in WBP has proved particularly important for mouse models where animal size and temperament are not conducive to direct determination of pulmonary function [4–6]. The ever present problem with WBP is that pulmonary outcomes are based on plethysmograph pressure changes, and in this regard the relationship between WBP chamber pressure and lung mechanics may be tenuous. While determination of respiratory rate is not overly problematic, accurate tidal volume (V T) estimates are influenced dramatically by subtle changes in pulmonary mechanics and fluctuations in barometric pressure (reviewed in [7]). Moreover, Adler et al. demonstrated that unrestrained plethysmography may be inconsistent between mouse strains and emphasize the need for appropriate control groups [2, 5, 8, 9]. Despite limitations, the advantage of WBP over invasive respiratory measures is that WBP outcomes are not confounded by animal restraint or anesthesia [7]. Further, WBP can be conducted over time, which makes longitudinal investigations with repeated measures possible; something not feasible with more invasive approaches. As such, WBP has been used extensively to gain serial measures of respiratory function in a variety of mammalian models of disease, including mouse strains [4, 10–14].
Strategic attention to chamber design has partially overcome validity concerns in WBP due to potentially confounding temperature fluctuations (reviewed in [15]). The sealed whole body plethysmography design provides for accurate assessment of temperature and humidity, and is thought to mitigate much erroneous influence of barometric variations between animal and chamber [7]. The other broad consideration for WBP validity pertains to mechanical influences in chamber pressure, primarily related to breathing-related pressure oscillations. This latter point of pressure oscillations impacts chamber airflow and is particularly important in examination of mice because tidal volume is low and ventilator rate high. Often overlooked, however, is the influence of animal activity on the resulting WBP pulmonary outcomes. Further, we are not aware of standardized procedural recommendations to account for the influence of behavioral factors on WBP reproducibility.
Considerations for WBP to estimate respiratory function in mice should account for environmental factors that influence animal movement, and ultimately respiratory estimates. As such, the influence of acute containment within the WBP chamber, light/dark cycles, and time of day all impact mouse behavior and may influence WBP estimates of respiratory function. Accordingly, we undertook the current study to determine the extent to which variations in WBP chamber habituation, ambient lighting, and time of day impacted respiratory function of mice during WBP examination. To address this we performed a series of experiments using two strains of mice and measured pulmonary function. We sought to identify a methodological approach whereby standardization of chamber habituation period, time of day and lighting used during WBP could be implemented in order to obtain reproducible day-to-day measures of pulmonary function.
Methods
Animals
Prior to study, approval of animal use was granted by the Auburn University Institutional Care and Use Committee. All experiments were performed in accordance with animal use guidelines established by the American Physiological Society. Two-month-old C57BL10 and mdx mice were purchased from an approved animal vendor and were housed within the University Biological Research Facility at 23 °C on a reverse light cycle (12 h:12 h, lights off beginning at 6:00 a.m.). All animals received at least two WBP chamber habituation cycles of 45 min prior to testing for this investigation.
Buxco plethsmography device
The Buxco whole body plethysmograph consists of four independent chambers allowing mice to move freely during assessment. Each chamber is approximately 400 ml in total volume and contains an integrated temperature and humidity probe along with a pressure-sensitive diaphragm in order to determine minute pressure fluctuations. Pressure changes within the chamber are known to come from two primary sources, the first of which is gas compression due to pressure changes in the thoracic gas which produce inspiratory and expiratory flow. In addition, pressure changes within the WBP chamber are due to changes in gas humidification and temperature from air movement between the chamber and the lungs. In this regard the reader is directed to an insightful review on the topic [16]. At the top of each chamber is a Halcyon™ pneumotachograph to measure the rate of air flow. While past studies were thought to be limited by inconsistencies within plethysmograph measurements due to extraneous background noise, this new device exhibits reduced baseline ambient noise up to 25 times (Buxco Research Systems, Wilmington, NC). The device was calibrated according to manufacturer instructions prior to all data collection installments. Mice were housed within the WPB chamber fully conscious and unrestrained.
Respiratory variables were calculated using Fine Point software (Buxco Research Systems, Wilmington, NC). While the Fine Point software calculates more than 40 respiratory variables, it was used currently to assess respiratory rate, tidal volume, minute ventilation, peak inspiratory flow, peak expiratory flow, inspiratory time, expiratory time, and relaxation time between breaths, as these variables were most relevant to our work. Respiratory values were calculated using proprietary software. Relative to this technique, however, respiratory rate was derived from the number of inspiration-expiration combinations registered in a minute. Tidal volume is determined from the volume of air moved per breath and minute ventilation is the product of respiratory rate and tidal volume. Peak inspiratory flow and peak expiratory flow represent the highest flow rate measured during the respective inspiration and expiration phases of a breath. The corresponding inspiratory and expiratory times were quantified according to the duration of a breath spent in inhalation or exhalation, respectively. As a working definition, relaxation time is the time required to expire 74 % of the tidal volume [16]. WBP respiratory chambers were cleaned thoroughly with water and alcohol between each use to better eliminate animal scents as a confounding factor.
Experimental design and data reduction
Four experiments were performed in total and each mouse participated in each experiment. Time stabilization analyses were performed to quantify the time duration needed before calculated respiratory values reached a plateau following mouse placement in the WBP chamber. This understanding is important as it would provide a standard familiarization time needed before data collection could begin. Next, we determined the effect of time of time of day on respiratory measures as well as light cycle. These considerations are important as they influence animal movement within the WBP chamber and are likely to introduce methodological variation when uncontrolled within a study design. Finally, using constraints derived from the time stabilization, time of day, and light cycle experiments, day-to-day reproducibility experiments were performed under optimized conditions. The key dependent variables for the four experiments were Buxco calculated values for respiratory rate (breaths/min), relative tidal volume (ml/kg body weight), minute ventilation (ml/min), expiratory volume (ml), inspiratory volume (ml), peak inspiratory flow (ml/s), peak expiratory flow (ml/s), and time to relaxation (s).
WBP chamber habituation time
Mice were placed in plethysmography chambers for 30 min. Analyses were begun within a minute of placing mice in the respiratory chamber. All data collection was performed during the dark phase of a reverse light cycle and within a common 2-h time window. Due to the breath-to-breath variability characteristic of WBP, individual breath data were not used: a standard practice for this technique [7]. At the conclusion of the data collection, raw data were converted to tabular data files and reduced into 1- and 5-min averages using Microsoft Excel (Redmond, WA).
Time of day and WBP
A cohort of mice was examined at 4 times (7:30 a.m., 11:45 a.m., 3:00 p.m., and 6:00 p.m.) during a single day. Mice were placed in the WBP chamber for 45 min, where the first 20 min was used for habituation (15 min based on time stabilization findings + 5 min buffer), and the final 25 min for data analysis. Calculated respiratory values were averaged over the 25-min data collection period.
WBP and lighting
On two separate days, mice were placed in the WBP chambers during the dark portion of their dark/light cycle to examine the potential influence of light on calculated respiratory values. WBP tests were performed in both lit (fluorescent overhead lighting, “light”) or darkened (“dark”) conditions. Mice were introduced into the chambers for 45 min and analyzed data collected from the final 25 min as described above. Sampling times were performed within a common 2-h time window in order to eliminate time of day effects on calculated respiratory values.
Day-to-day reproducibility
Based on the above experiments we determined that for a given study, mice should be examined within a common 2-h time window. Moreover, mice should be habituated to the WBP chamber for at least 15 min prior to data collection. Finally, a consistent light/dark approach should be used during all data collection. To determine the reproducibility of WBP under these conditions, mice were examined on 2 consecutive days under identical, standardized conditions. Mice were examined within a 2-h time window during the dark phase of their light cycle. Sampling was performed for 45 min as described above.
Statistical analysis
One-way ANOVA with repeated measures was used to analyze between group differences for the time stabilization and time of day study arms. The dark/light study arm data were examined using a paired t-test. Pearson product moment correlations were performed to analyze day-to-day findings. When appropriate, Tukey post hoc analyses were performed. All statistical analyses were performed using SPSS software (IBM, Armonk, NY). p was set a priori to ≤0.05.
Results
Animal characteristics
All mice (C57 n = 8/group; mdx n = 8/group) completed each of the four study experiments. Both C57 and mdx mice were of similar weights at the time of analysis (C57: 24.9 ± 1.3 g; mdx: 26.3 ± 1.5 g; p = 0.07).
Time stabilization analyses
Data for all measures were reduced in 1- and 5-min averages, with respiratory rate values presented as an example in Fig. 1a (1-min averages) and Fig. 1b (5-min averages), respectively. To accomplish this, all of the values in a given range (1 or 5 min) were averaged to arrive at a single value for that time range. Due to the natural fluctuations in variable calculation that were present in 1-min averages, 5-min averages were used to determine stability time points. No strain-dependent differences were noted between C57 and mdx mice (data not shown), and as such, inter-strain data were combined for these calculations. Statistical outcomes indicate that 6 of 8 respiratory variables exhibited time-dependent differences. Table 1 presents time stabilization in 5-min increments for the 6 respiratory variables expressing change during the 30-min chamber habituation. Specifically, respiratory rate (p < 0.001), minute ventilation (p < 0.001), expiratory time (p = 0.004), peak inspiratory flow (p = 0.002), peak expiratory flow (p = 0.002) and time to relaxation (p = 0.009) are reported in Table 1. In contrast, only tidal volume (p = 0.081) and inspiratory time (p = 0.166) were statistically unaltered during the 30-min measurement period. For the 6 respiratory variables where changes were detected, post hoc analysis revealed that once placed in the chamber, respiratory values stabilized within 10 min for all but time to relaxation, which stabilized by 15 min. In total these data suggest that for C57 and mdx mice, at least 15 min of chamber habituation is required before stable respiratory variable calculations are observed.
Fig. 1.
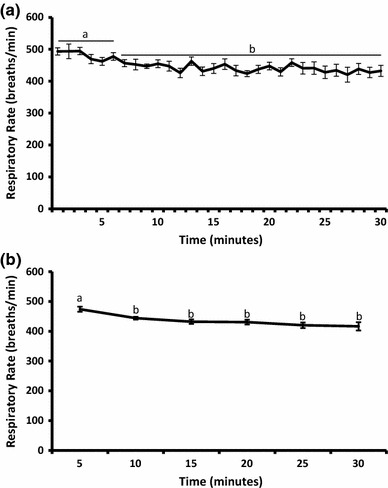
Time to data stabilization — respiratory rate. Mice were placed in a respiratory chamber for 30 min and the time to stabilization was determined. Data were synthesized into 1-min averages (a), and 5-min averages (b). Data are presented as mean ± SEM. Letters a, b denote statistically different time points. Statistical differences p ≤ 0.05
Table 1.
Time stabilization for chamber habituation quantified in 5-min intervals
| Variable | Minutes to observance of stable data |
|---|---|
| Respiratory rate | 10 |
| Minute ventilation | 10 |
| Expiratory time | 10 |
| Peak inspiratory flow | 10 |
| Peak expiratory flow | 10 |
| Time to relaxation | 15 |
Time of day analyses
Pulmonary function measures were examined four times (7:30 a.m., 11:45 a.m., 3:00 p.m. and 6:00 p.m.) during the dark phase of a 12-h reverse light cycle where lights were turned off at 6:00 a.m. As with time stabilization experiments, no strain-dependent differences were observed and so inter-strain data are combined for these analyses. Table 2 presents the time of day averages for the respiratory variable examined. Data analyses indicate a significant time of day effect was present for 6 of 8 calculated respiratory variables. Respiratory rate (p = 0.037), relative tidal volume (p = 0.014), minute ventilation (p = 0.013), and peak expiratory flow (p = 0.014) increased from our first observation at 7:30 a.m. and peaked at 3:00 p.m. At 6:00 p.m. these measures were statistically similar to 7:30 a.m. Corresponding to these findings, expiratory time (p = 0.038) and time to relaxation (p = 0.020) decreased significantly with shortest times evident at 3:00 p.m. as compared to 7:30 a.m. At 6:00 p.m. mean expiratory time and time to relaxation values were again similar to 7:30 a.m. observations. Finally, inspiratory time (p = 0.180) and peak inspiratory flow (p = 0.065) were similar across the four observation periods.
Table 2.
Respiratory measures quantified at different times of the day
| Variable | 7:30 a.m. | 11:45 a.m. | 3:00 p.m. | 6:00 p.m. | p value |
|---|---|---|---|---|---|
| Respiratory rate | 378 ± 2a | 411 ± 16a | 432 ± 19b | 403 ± 25a | 0.037 |
| Tidal vol/wt (ml/kg*100) | 1.21 ± 0.12a | 1.31 ± 0.14b,c | 1.35 ± 0.15b | 1.20 ± 0.16a,c | 0.014 |
| Minute ventilation (ml/min) | 94.7 ± 7.89a | 109.5 ± 7.63b | 118.1 ± 8.77b | 109.3 ± 9.46a | 0.013 |
| Expiratory time (s) | 0.14 ± .01a | 0.11 ± 0.01b | 0.11 ± 0.01b | 0.13 ± 0.01a,b | 0.038 |
| Inspiratory time (s) | 0.06 ± 0.004 | 0.05 ± 0.003 | 0.05 ± 0.002 | 0.06 ± 0.004 | 0.180 |
| Peak inspiratory flow (ml/s) | 7.79 ± 0.51 | 8.52 ± 0.54 | 9.05 ± 0.54 | 8.73 ± 0.63 | 0.065 |
| Peak expiratory flow (ml/s) | 4.48 ± 0.39a | 5.14 ± 0.42b | 5.41 ± 0.45c | 5.08 ± 0.43b | 0.014 |
| Time to relaxation (s) | 0.07 ± .01a | 0.06 ± 0.003b | 0.06 ± 0.01b | 0.07 ± 0.01a,b | 0.020 |
Data are mean ± SEM
a,b,cdenote statistically different time points. Statistical differences p ≤ 0.05
Dark and light environment effect on respiratory values
Mice were examined within a common 2-h time window (during the light cycle dark phase) on consecutive days to quantify the potential impact of room lighting on respiratory values. Table 3 presents average responses in lit and dark room environments. Ambient lighting impacted 5 of 8 calculated respiratory variables. Specifically, respiratory rate (p = 0.046), tidal volume (p = 0.003), minute ventilation (p = 0.003), peak inspiratory flow (p = 0.004), and peak expiratory flow (p = 0.049) were higher in the dark condition as compared to light. Expiratory time (p = 0.211), inspiratory time (p = 0.114), and time to relaxation (p = 0.142) were numerically lower in the light versus dark condition, but failed to reach statistical significance.
Table 3.
Respiratory function in light and dark conditions
| Variable | Dark | Light | p value |
|---|---|---|---|
| Respiratory rate | 456 ± 35 | 409 ± 59 | 0.046 |
| Tidal vol/wt (ml) | 0.29 ± 0.03 | 0.24 ± 0.02 | 0.003 |
| Minute ventilation (ml/min) | 132 ± 16 | 103 ± 17 | 0.003 |
| Expiratory time (s) | 0.10 ± 0.02 | 0.11 ± 0.02 | 0.211 |
| Inspiratory time (s) | 0.048 ± 0.001 | 0.051 ± 0.003 | 0.114 |
| Peak inspiratory flow (ml/s) | 9.97 ± 0.37 | 8.40 ± 0.31 | 0.004 |
| Peak expiratory flow (ml/s) | 6.16 ± 0.35 | 5.27 ± 0.30 | 0.049 |
| Time to relaxation (s) | 0.06 ± 0.01 | 0.07 ± 0.01 | 0.142 |
Data are mean ± SEM
Day-to-day reproducibility
Based on the findings from the time stabilization, time of day and dark/light study arms, mice were examined on consecutive days to determine reproducibility of the WBP for estimating respiratory function. Mice were examined between 7:00 and 9:00 a.m. in a dark environment. Respiratory values were examined for 45 min, with the first 20 min used to habituate to the respiratory chamber and data from the final 25 min being used to calculate the final outcomes for the 8 respiratory variables. Table 4 presents day-to-day respiratory values averaged during the final 25 min of data sampling. Findings reveal that when performed in a standardized environment, statistically reproducible respiratory values were achieved for all variables; whereas these relationships were not statistically significant when conducted in non-standard conditions (data not shown). This conclusion is supported by the associated r 2 and corresponding p values (below the α ≤ 0.05 threshold chosen a priori).
Table 4.
Day-to-day reproducibility of respiratory values
| Variable | Day 1 | Day 2 | r 2 | p value |
|---|---|---|---|---|
| Respiratory rate | 414 ± 8.36 | 416 ± 9.67 | 0.591 | <0.000 |
| Tidal vol (ml) | 0.23 ± 0.01 | 0.25 ± 0.01 | 0.594 | <0.000 |
| Minute ventilation (ml/min) | 97.5 ± 4.36 | 104 ± 5.40 | 0.612 | 0.003 |
| Expiratory time (s) | 0.115 ± 0.004 | 0.113 ± 0.004 | 0.474 | 0.005 |
| Inspiratory time (s) | 0.051 ± 0.001 | 0.051 ± 0.001 | 0.751 | <0.000 |
| Peak inspiratory flow (ml/s) | 8.60 ± 0.31 | 7.76 ± 0.51 | 0.473 | 0.019 |
| Peak expiratory flow (ml/s) | 5.26 ± 0.27 | 5.15 ± 0.29 | 0.410 | 0.014 |
| Time to relaxation (s) | 0.066 ± 0.003 | 0.065 ± 0.003 | 0.334 | 0.037 |
Data are mean ± SEM. Reported p values relate to the r 2 values demonstrating day-to-day reproducibility for each of the respiratory variables examined
Discussion
WBP in vivo for the estimation of respiratory performance has been performed for many years in a variety of mammalian species, including mice [4, 11–13]. The advantage of this technique is that it enables physiologically and clinically relevant estimates of respiratory function in conscious unrestrained animals [5, 17]. The key finding of the current study is that by controlling several testing parameters, WBP determination of respiratory function can be easily and reproducibly estimated. In the current study our day-to-day coefficients of determination were between 0.334 and 0.751 (and corresponding p values significant) for the respiratory variables examined. The current findings provide novel insight into a methodological approach for WBP for the measurement of respiratory function. Hence, these findings indicate that data produced using WBP can be improved by standardized testing conditions, which will mitigate variability inherent to the technique. The caveat that underpins the reproducibility observed currently is that findings are contingent upon several methodological considerations: that C57BL and mdx mice (used currently) be habituated to the WBP chamber for at least 15 min prior to data collection, that measures be performed at a common time of day, and that consistent ambient lighting conditions be used.
Mouse behavior and WBP
The current goal of demonstrating whether estimates of respiratory function could be achieved reliably was dependent upon eliminating confounding aspects of the testing procedure during WBP scans. Given that mice and other rodents are sensitive to novel confinement scenarios [5, 17], we habituated all mice to the respiratory chambers on two occasions prior to data collection. Moreover, the chambers were cleaned thoroughly between trials to further eliminate the influence of the impact of residual scent on mouse behavior in the WPB chamber.
As applied to behavior and WBP, mouse strain is an important consideration. Spontaneous mouse behavior is heavily influenced by strain [18, 19]. As such, we recommend using mice of a common background to eliminate strain-dependent behavior differences. Based on this rationale we used of C57 (C57BL/10SnJ) and mdx (C56BL/10ScSn-Dmd < mdx >/J) strains in the current investigation, which have been examined previously by WBP [11, 12]. As expected for 2-month-old C57 and mdx mice, a period generally prior to respiratory dysfunction, we did not observe baseline differences in estimated respiratory function (data not shown). Based on this finding, calculated values from C57 and mdx mice were combined for subsequent analyses.
WBP chamber habituation time
Our first experiment was to determine habituation time needed prior to initiation of data analysis. Prior to study, we observed that many similar investigations featuring WBP analyses do not report habituation times [8, 20]. Others report times between 5 and 10 min [6, 11, 17, 21, 22]. Given that these approaches were not validated as reported, we performed a series of experiments where mice with prior WBP exposure were examined for 30 min. Findings from our study indicate that 7 of 8 estimated respiratory values were stable by 10 min following placement in the chamber, and one value stabilized between 10 and 15 min. These findings suggest that previous WBP experiments may include variability due to an inadequate habituation period. For our subsequent experiments we chose to add a margin of safety in this regard and employed a 20-min chamber habituation time before inclusion of data for final calculations. Note that our choice to examine a 25-min time window exceeds that of most previously published studies [6, 10–12, 17, 21] that include these methodological details, with many fewer study findings having comparable chamber habituation times reported in published protocols [4, 13]. Based upon the aforementioned impact of strain on mouse behavior, other investigators are encouraged to verify WBP habituation times in other mouse strains as it may impact respiratory function directly [11–13] or indirectly through activity levels [18, 19].
Time of day and WBP
Our second set of experiments examined time of day influence on WBP estimates on the resulting respiratory measures. Findings in our reverse light cycle housed mice indicate that early and late in the 12-h reverse light cycle (7:30 a.m. and 6:00 p.m.), mice exhibited a less frequent and shallower breathing pattern. This finding is consistent with understanding of nocturnal species housed on a reverse light cycle. Collectively, we observed increases of 14 % respiratory rate, 12 % tidal volume, 25 % minute ventilation, and 21 % peak expiratory flow at 3:00 p.m. as compared to 7:30 a.m. Based on these time-dependent findings, high throughput analysis may be limited when using WBP devices (most commercial systems allow for measurement of 4 chambers simultaneously) in that our data suggest that mice be examined within a common 2-h time window. Careful examination of published literature revealed no reporting of when mice were measured, though it is likely that in the name of efficiency many, if not most investigators, conducted experiments throughout the day. If this assumption about prior data collection is correct, then time of day variations in breathing patterns may impact calculated respiratory values in one of two ways. First, if mice from all treatments were examined across the day, then the observed error would likely be elevated as compared to values collected within a common time window. Second, if mice were not equally dispersed throughout the day, then results may be skewed toward false positive or false negative outcomes, depending on when animal groups were investigated.
WBP and lighting
Based on the fact that mice are nocturnal, we housed our animals on a reverse light cycle in order to examine them during the typical human work day. We tested the influence of ambient lighting on WBP respiratory function. Findings from the current study revealed that, as expected, calculated respiration data were blunted when the experiment was performed in a lit room during the active portion of the photoperiod. Specifically, in mice observed in a lit room during their scheduled dark phase, we observed a 10 % drop in respiratory rate, a 17 % drop in tidal volume, a 22 % drop in minute ventilation, a 16 % drop in peak inspiratory flow, and a 14 % drop in peak expiratory flow. These findings are not surprising given the nocturnal nature of mice, and indicate an innate inclination to rest in lit conditions. As such, we recommend that, unless otherwise indicated for a particular study design, WBP measures be performed in a darkened room during the active portion of the photoperiod and in a lit room during the resting hours.
Study limitations
In addition to the need to verify the current findings in other mouse models, several study limitations require clarification. First, WBP is often applied with use of aerosolized compounds to induce airway challenge [10], a methodological aspect not included in this methodological investigation. Whether use of inhalants would require additional habituation time and be influenced differently by time of day or ambient lighting is not currently known. Moreover, respiratory function is also influenced by sex and age, biological considerations that were not examined in this investigation as all mice were of the same age and sex.
Conclusions
In summary, the findings of this study reveal that despite the known technical limitations in WBP for estimation of respiratory function in conscious, unrestrained mice, the technique can be refined and is reproducible. Reproducible outcomes were obtained when values were averaged over a 25-min collection period and were dependent upon an adequate chamber habituation time exceeding 15 min, occurred within a common 2-h time window, and occurred during the dark phase of a reverse light cycle. While we have not examined the impact of sex [23], age [22], or the influence of airway challenges [10], in a variety of other mouse models [13], the current study design serves as a methodological model for further investigation of WBP for estimation of respiratory function and potentially as a standard for measurement of respiratory function in C57 and mdx mice.
Acknowledgement
Funded by Duchene Alliance Grant 100065 to JS and JQ.
Compliance with ethical standards
Conflict of interest
There are no conflicts of interest to report.
References
- 1.Diamond L, O’Donnell M. Pulmonary mechanics in normal rats. J Appl Physiol Respir Environ Exerc Physiol. 1977;43(6):942–948. doi: 10.1152/jappl.1977.43.6.942. [DOI] [PubMed] [Google Scholar]
- 2.Enhorning G, van Schaik S, Lundgren C, Vargas I. Whole-body plethysmography, does it measure tidal volume of small animals? Can J Physiol Pharmacol. 1998;76(10–11):945–951. doi: 10.1139/y99-002. [DOI] [PubMed] [Google Scholar]
- 3.Onodera M, Kuwaki T, Kumada M, Masuda Y. Determination of ventilatory volume in mice by whole body plethysmography. Jpn J Physiol. 1997;47(4):317–326. doi: 10.2170/jjphysiol.47.317. [DOI] [PubMed] [Google Scholar]
- 4.Hernandez AB, Kirkness JP, Smith PL, Schneider H, Polotsky M, Richardson RA, Hernandez WC, Schwartz AR. Novel whole body plethysmography system for the continuous characterization of sleep and breathing in a mouse. J Appl Physiol. 2012;112(4):671–680. doi: 10.1152/japplphysiol.00818.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lundblad LK, Irvin CG, Adler A, Bates JH. A reevaluation of the validity of unrestrained plethysmography in mice. J Appl Physiol. 2002;93(4):1198–1207. doi: 10.1152/japplphysiol.00080.2002. [DOI] [PubMed] [Google Scholar]
- 6.Rasid O, Chirita D, Iancu AD, Stavaru C, Radu DL. Assessment of routine procedure effect on breathing parameters in mice by using whole-body plethysmography. J Am Assoc Lab Anim Sci. 2012;51(4):469–474. [PMC free article] [PubMed] [Google Scholar]
- 7.Mortola JP, Frappell PB. Measurements of air ventilation in small vertebrates. Respir Physiol Neurobiol. 2013;186(2):197–205. doi: 10.1016/j.resp.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Adler A, Cieslewicz G, Irvin CG. Unrestrained plethysmography is an unreliable measure of airway responsiveness in BALB/c and C57BL/6 mice. J Appl Physiol. 2004;97(1):286–292. doi: 10.1152/japplphysiol.00821.2003. [DOI] [PubMed] [Google Scholar]
- 9.Mitzner W, Tankersley C. Interpreting Penh in mice. J Appl Physiol. 2003;94(2):828–831. doi: 10.1152/japplphysiol.00815.2002. [DOI] [PubMed] [Google Scholar]
- 10.Hamelmann E, Schwarze J, Takeda K, Oshiba A, Larsen GL, Irvin CG, Gelfand EW. Noninvasive measurement of airway responsiveness in allergic mice using barometric plethysmography. Am J Respir Crit Care Med. 1997;156(3 Pt 1):766–775. doi: 10.1164/ajrccm.156.3.9606031. [DOI] [PubMed] [Google Scholar]
- 11.Huang P, Cheng G, Lu H, Aronica M, Ransohoff RM, Zhou L. Impaired respiratory function in mdx and mdx/utrn(+/−) mice. Muscle Nerve. 2011;43(2):263–267. doi: 10.1002/mus.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ishizaki M, Suga T, Kimura E, Shiota T, Kawano R, Uchida Y, Uchino K, Yamashita S, Maeda Y, Uchino M. Mdx respiratory impairment following fibrosis of the diaphragm. Neuromuscul Disord. 2008;18(4):342–348. doi: 10.1016/j.nmd.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Tankersley CG, Fitzgerald RS, Levitt RC, Mitzner WA, Ewart SL, Kleeberger R. Genetic control of differential baseline breathing pattern. J Appl Physiol. 1997;82(3):874–881. doi: 10.1152/jappl.1997.82.3.874. [DOI] [PubMed] [Google Scholar]
- 14.Vanoirbeek JA, Rinaldi M, De Vooght V, Haenen S, Bobic S, Gayan-Ramirez G, Hoet PH, Verbeken E, Decramer M, Nemery B, Janssens W. Noninvasive and invasive pulmonary function in mouse models of obstructive and restrictive respiratory diseases. Am J Respir Cell Mol Biol. 2010;42(1):96–104. doi: 10.1165/rcmb.2008-0487OC. [DOI] [PubMed] [Google Scholar]
- 15.Frazer JS, Frazer DG. Noninvasive pulmonary function screening in spontaneously breathing rodents: an engineering systems perspective. Pharmacol Ther. 2011;131(3):359–368. doi: 10.1016/j.pharmthera.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Bates JH, Irvin CG. Measuring lung function in mice: the phenotyping uncertainty principle. J Appl Physiol. 2003;94(4):1297–1306. doi: 10.1152/japplphysiol.00706.2002. [DOI] [PubMed] [Google Scholar]
- 17.DeLorme MP, Moss OR. Pulmonary function assessment by whole-body plethysmography in restrained versus unrestrained mice. J Pharmacol Toxicol Method. 2002;47(1):1–10. doi: 10.1016/S1056-8719(02)00191-0. [DOI] [PubMed] [Google Scholar]
- 18.Knab AM, Bowen RS, Moore-Harrison T, Hamilton AT, Turner MJ, Lightfoot JT. Repeatability of exercise behaviors in mice. Physiol Behav. 2009;98(4):433–440. doi: 10.1016/j.physbeh.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lightfoot JT, Turner MJ, Debate KA, Kleeberger SR. Interstrain variation in murine aerobic capacity. Med Sci Sport Exerc. 2001;33(12):2053–2057. doi: 10.1097/00005768-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Morrey JD, Siddharthan V, Wang H, Hall JO. Respiratory insufficiency correlated strongly with mortality of rodents infected with West Nile virus. PLoS One. 2012;7(6):e38672. doi: 10.1371/journal.pone.0038672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bates JH, Thompson-Figueroa J, Lundblad LK, Irvin CG. Unrestrained video-assisted plethysmography: a noninvasive method for assessment of lung mechanical function in small animals. J Appl Physiol. 2008;104(1):253–261. doi: 10.1152/japplphysiol.00737.2007. [DOI] [PubMed] [Google Scholar]
- 22.Wesson DW, Varga-Wesson AG, Borkowski AH, Wilson DA. Respiratory and sniffing behaviors throughout adulthood and aging in mice. Behav Brain Res. 2011;223(1):99–106. doi: 10.1016/j.bbr.2011.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulz H, Johner C, Eder G, Ziesenis A, Reitmeier P, Heyder J, Balling R. Respiratory mechanics in mice: strain and sex specific differences. Acta Physiol Scand. 2002;174(4):367–375. doi: 10.1046/j.1365-201x.2002.00955.x. [DOI] [PubMed] [Google Scholar]


