Abstract
Background:
Cysts, primarily epidermal and trichilemmal, are commonly seen in clinical practice. Rupture, infection, inflammation, and rarely malignant transformation may complicate the cysts. This study aims to analyze the clinicohistological features of cutaneous cysts.
Materials and Methods:
A retrospective review of patients with the diagnosis of cyst confirmed on histopathology over the past two years (2020–2021) was performed. Clinical details comprised of age, gender, site of involvement, size, duration, and associated symptoms. Histological examination included cyst wall lining, type of keratinization, complications like rupture, inflammation, foreign body giant cell reaction, calcification, and malignant change.
Results:
A total of 324 cases with mean age of 37.9 years and equal gender distribution were identified. Most frequent diagnosis was epidermal cyst in 89.8%, followed by trichilemmal cyst in 8.9% of cases. Rare types included follicular hybrid cyst, verrucous cyst, vellus hair cyst, and steatocystoma. Most common complication was cyst rupture in 54.3% of epidermal cysts. Proliferating epidermal and proliferating trichilemmal cysts were noted in one and two cases, respectively. Two cases revealed malignancy arising in the wall of epidermal cyst.
Limitations:
The retrospective study design and non-availability of follow-up data, especially for proliferating cysts and cysts with malignant transformation were the main limitations of this study.
Conclusion:
Histopathologic examination of excised cutaneous cysts is paramount in reaching accurate diagnosis of the type of cyst and associated secondary changes to enable appropriate management.
Keywords: Epidermal cyst, malignant tumor, proliferating epidermal cyst, proliferating trichilemmal cyst, trichilemmal cyst
Introduction
A wide variety of cysts may present in the skin, though majority are epidermal and few are trichilemmal.[1] Acute inflammation resulting in cyst wall rupture and subsequent foreign body giant cell reaction is a potential complication, particularly in epidermal cysts. Other secondary changes include the proliferation of epithelium, viral cytopathic reaction, malignant transformation, and calcification. Proliferating epithelial cysts, comprising of proliferating epidermal cyst (PEC), and proliferating trichilemmal cyst (PTC) are benign tumors with locally aggressive and potentially malignant behavior.[2] About 1%–2.2% of cysts show malignant transformation, of which squamous cell carcinoma (SCC) has been noted in 70% and basal cell carcinoma (BCC) in 10% of cases.[3,4] Follicular hybrid cyst is an uncommon lesion that is composed of two or more components of the pilosebaceous unit.[5] There is paucity of large studies on histopathological characteristics of cutaneous cysts and their associated complications.
Materials and Methods
All cases with histopathological diagnosis of cutaneous cyst from January 2020 to December 2021 were included. Clinical data including age, gender, duration, site of involvement, size of the lesion, and associated symptoms were retrieved from patients' records. Hematoxylin and eosin stained sections were reviewed by two dermatopathologists, and the following features were noted: nature of cyst lining, type of keratinization, cyst rupture with secondary inflammation, foreign body giant cell reaction, calcification, and any tumor arising in cyst wall.
Results
A total of 324 cases of cutaneous cysts were studied. Of these, 291 (89.8%) were categorized as epidermal cysts, 29 (8.9%) as trichilemmal cysts, 2 (0.6%) as follicular hybrid cysts, and 1 each (0.3%) as steatocystoma and vellus hair cyst. Mean age of the patients was 37.9 years, and prevalence was almost equal in males and females.
Epidermal cysts
Clinical findings
The mean age of presentation was 40.9 years, and the most prevalent age group was 35–45 years. Males were more commonly affected than females (Males: Females - 1.2:1). Main site of involvement was trunk in 114 (39.2%), followed by head and neck in 59 (20.3%) cases. Mean duration of the lesions was 8.4 years, and mean size was 3.2 cm × 2.1 cm. Erythema and pain were associated in 54 (18.5%) lesions.
Histopathological findings [Table 1]
Table 1.
Histopathological findings in epidermal cysts
| Epidermal cysts | n=291 (%) |
|---|---|
| Ruptured cyst with inflammation | 158 (54.3%) |
| Foreign body giant cell reaction | 3 (1%) |
| Cholesterol clefts and hemosiderin | 2 (0.68%) |
| Pseudoepitheliomatous hyperplasia | 1 (0.34%) |
| Verrucous cyst | 1 (0.34%) |
| Proliferating epidermal cyst | 1 (0.34%) |
| Basal cell carcinoma | 1 (0.34%) |
| Squamous cell carcinoma | 1 (0.34%) |
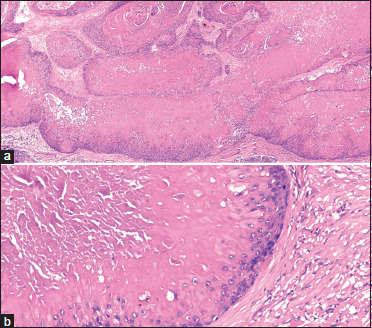
Epidermal cyst is lined by stratified squamous epithelium with the presence of granular layer and contains laminated keratin [Supplementary Figure 1 (179.1KB, tif) ]. Ruptured cyst with acute/chronic inflammation was noted in 158 (54.3%) epidermal cysts [Figure 1a, Supplementary Figures 2a (359.1KB, tif) and b (359.1KB, tif) ]. Foreign body giant cell reaction to keratin occurred in three cases [Figure 1b]. Cholesterol clefts and hemosiderin deposits in ruptured cyst lining were seen in two cases [Supplementary Figure 3 (179.1KB, tif) ]. Pseudoepitheliomatous hyperplasia (PEH) of cyst wall was present in one case [Supplementary Figures 4a (342.8KB, tif) and b (342.8KB, tif) ]. An epidermal cyst on back revealed hyperkeratosis, parakeratosis, hypergranulosis, irregular coarse keratohyalin granules, and papillomatosis [Supplementary Figures 5a (810.1KB, tif) and b (810.1KB, tif) ]. Stratum spinosum showed koilocytes with vacuolated cytoplasm, pyknotic nuclei, and perinuclear halo [Supplementary Figure 5c (810.1KB, tif) ]. Real-time polymerase chain reaction showed high-risk human papillomavirus (HPV) types-16 and 59. Based on these findings, a diagnosis of verrucous cyst was considered. PEC diagnosed in one case, showed multiple cystic areas with proliferating epithelium. The proliferative areas were composed of bland squamous epithelium with cells showing pale eosinophilic cytoplasm and small nuclei, granular layer, and loose keratin. The cyst epithelium revealed parakeratosis, hyperkeratosis, hypergranulosis, acanthosis, and papillomatosis. The epithelium proliferated both towards the periphery into surrounding dermis and also into the lumen [Figures 2a and 2b]. In an epidermoid cyst presenting on shoulder, the cyst wall showed 4–5 cell thick layer of squamous epithelium. The cyst lining gave rise to nests of basaloid cells with peripheral palisading and retraction artifact. Melanin pigment was present within tumor nests and stroma [Figures 3a and 3b]. This was diagnosed as BCC arising in epidermal cyst. Another epidermal cyst showed proliferation of squamous epithelium of the wall, invading into the dermis with atypia of keratinocytes and keratin pearl formation, suggestive of SCC in epidermal cyst [Figures 4a and 4b, Supplementary Figures 6a (610.1KB, tif) and b (610.1KB, tif) ].
Figure 1.
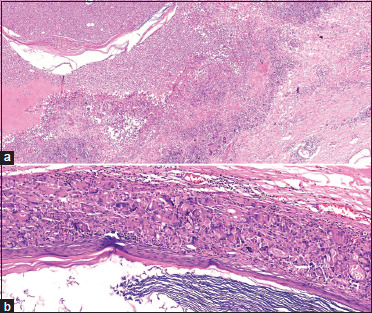
(a) Cyst wall of the epidermis is completely destroyed by acute inflammatory exudate. Only fibers of laminated keratin are seen as remnant of cyst wall (Hematoxylin and eosin, x20) (b) Epidermal cyst with severe foreign body giant cell reaction in the wall, which is forming a continuous layer surrounding the cyst. Laminated keratin can be seen in the lumen (Hematoxylin and eosin, x100)
Figure 2.
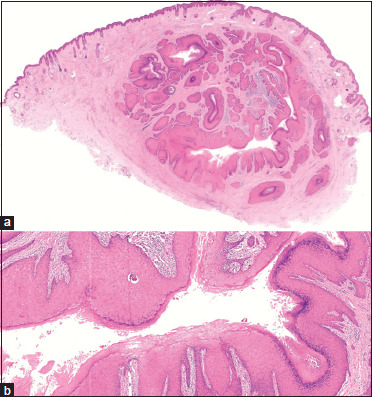
Proliferating epidermal cyst (a) Multiple cystic spaces lined by proliferating squamous epithelium with the presence of granular cell layer and laminated keratin (Hematoxylin and eosin, x20) (b) The cyst epithelium shows hyperkeratosis, parakeratosis, hypergranulosis, acanthosis, and papillomatosis. The cells have eosinophilic cytoplasm and uniform small nuclei. The proliferating epithelium is seen extending into the cyst lumen (Hematoxylin and eosin, x50)
Figure 3.
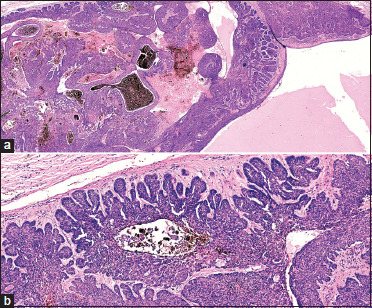
Basal cell carcinoma arising in epidermal cyst (a) The cyst wall is lined with 4–5 layered thick stratified squamous epithelium and contains proteinaceous fluid in its lumen. Nests of basaloid cells are originating from the basal layer of the cyst wall. The stroma contains clumps of melanin pigment (Hematoxylin and eosin, x100) (b) Tumor cells are infiltrating the cyst wall. The cells show hyperchromatic nuclei, scanty cytoplasm, and peripheral palisading and are separated from the stroma by retraction artifact (Hematoxylin and eosin, x200)
Figure 4.
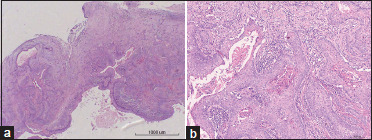
Squamous cell carcinoma arising in epidermal cyst (a) Epidermal cyst lined by stratified squamous epithelium shows nests of atypical epithelial cells (Hematoxylin and eosin, x40) (b) Extension of neoplastic epithelium into the cyst wall. Keratin pearl formation is conspicuous (Hematoxylin and eosin, x100)
Trichilemmal cysts
Clinical findings
Mean age of the patients was 47.7 years, and most frequent age group was 45–55 years. Female predilection was seen (Females: Males- 2.1:1). Majority of the lesions were located on scalp in 24 (82.7%) patients. Mean duration of the cysts was 12.7 years, and mean size was 2.4 cm × 2.2 cm.
Histopathological findings [Table 2]
Table 2.
Histopathological findings in trichilemmal cysts
| Trichilemmal cysts | n=29 (%) |
|---|---|
| Ruptured cyst with inflammation | 4 (13.8) |
| Calcification | 3 (10.3) |
| Proliferating trichilemmal cyst | 2 (6.9) |
| Parakeratin and few keratohyalin granules | 2 (6.9) |
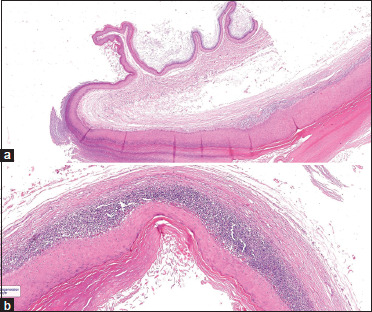
Characteristic features were sudden compact amorphous keratinization of the epithelial cells that cover the cyst wall without a granular layer (trichilemmal keratinization) [Supplementary Figure 7a (358.1KB, tif) ]. In two (6.9%) cases, trichilemmal cyst showed parakeratosis and few keratohyalin granules focally [Supplementary Figure 7b (358.1KB, tif) ]. Ruptured cyst with chronic inflammatory infiltrate was noted in four (13.8%) and calcification in three (10.3%) patients. PTC was diagnosed in two (6.9%) cases, which showed proliferation of solid epithelial masses with pushing borders. Bands of squamous epithelium demonstrated trichilemmal keratinization and were separated by fibrous stroma. The epithelium was seen to proliferate towards the lumen of the cyst. There were single to few layers of basal cells, which matured into large polygonal cells with eosinophilic cytoplasm and homogenous keratin [Figures 5a and 5b].
Figure 5.
Proliferating trichilemmal cyst (a) Predominant solid bands of proliferating squamous epithelium separated by stroma. The epithelium tends to proliferate inwards towards the cyst lumen (Hematoxylin and eosin, x100) (b) The cells with abundant eosinophilic cytoplasm are abruptly melting away into the central keratinous mass without the formation of granular layer (Hematoxylin and eosin, x200)
Follicular hybrid cysts
Clinical findings
There were two cases, a 38-year-old female with cyst on face of 5 years duration and a 45-year-old male with cyst on scalp of 12 years duration.
Histopathological findings
In the first case, the upper portion was consistent with epidermal cyst, with sharp transition to lower portion, which was identical to trichilemmal cyst [Figure 6a]. An unusual finding was presence of vacuolar degeneration of basal layer of cyst epithelium, colloid bodies, and band-like lichenoid infiltrate [Figure 6b]. The second case revealed multiple cystic spaces lined by squamous epithelium, composed of large pale-looking cells with abrupt keratinization to dense homogenous keratin, suggestive of trichilemmal cyst. There was sharp transition of cyst epithelium to basophilic cells, which had lost nuclei to form ghost cells, along with calcification of keratin [Supplementary Figure 8a (600.3KB, tif) -c (600.3KB, tif) ].
Figure 6.
(a) Hybrid cyst showing features of epidermal cyst and trichilemmal cyst. Laminated keratin and granular layer in the epithelial lining are seen in the upper part of the cyst wall, which is transitioning into features of trichilemmal cyst in the lower right part (Hematoxylin and eosin, x20) (b) Cyst wall shows dense band of lymphocytes at the interface of epithelium with the connective tissue (Hematoxylin and eosin, ×50)
Discussion
Epidermal cyst is the most common cutaneous cyst. It is mostly asymptomatic unless secondarily infected.[6] When inflamed, cyst ruptures leading to dense inflammatory response. Foreign body giant cell reaction to extruded keratinous contents is also evoked in response to rupture of uninflamed cysts.[6] Trichilemmal cyst is derived from isthmus of external root sheath of hair follicle.[7]
In a clinicopathologic analysis of cutaneous cysts, Kamyab et al.[1] reported epidermal cysts as most common in 47.8%, followed by trichilemmal cysts in 23.8% of patients. The average age of the patients was 42 years. This is in contrast to our study, where although majority of the cysts were epidermal, they constituted 89.8% of total cysts, while trichilemmal cysts accounted for only 8.9% of all cases. Mean age at presentation was younger, that is 37.9 years.
Epidermal cysts have been reported most frequently in the age group of 16–30 years,[1] though in our study they were most prevalent in relatively older age group (35–45 years). Male preponderance was in accordance with the previous report. Trunk was the most common site affected in our study, in contrast to face in earlier study.[1] Complications like rupture and inflammation were recorded in 22.8% of epidermal cysts,[1] in contrast to 54.2% in the present study.
Trichilemmal cysts were most common in the age group of 45–55 years in our study, while age group of 31–60 years was mostly affected in a previous study.[1] Female preponderance and predominant scalp involvement were consistent with that reported by Kamyab et al.[1] Ruptured cyst with inflammation was recorded in 13.8% of cases in the present study. This is concordant with a previous study that described inflammatory reaction due to rupture of cyst much less frequently in trichilemmal cysts (14.85%) than in epidermal cysts (50%).[7] Calcification has been documented in 24% of trichilemmal cysts,[7] while it was noted in 10.3% of our patients
Epidermal cyst with histological features of HPV infection and the presence of HPV DNA is known as verrucous cyst.[8] HPV infection can occur in a pre-existing epidermal cyst or affect infundibular cells directly. Palmo-plantar epidermal verrucous cysts have shown positivity for HPV-60 and 57.[9] We found high-risk types, HPV-16 and 59 in one case.[10]
Among proliferating epithelial cysts, we found one case of PEC and two cases of PTC. Sau et al.[2] described 96 cases of proliferating epithelial cysts, of which 33 were epidermal and 63 trichilemmal. In a recent retrospective study, PEC was documented in 0.4% and PTC in 1.8% of all mucocutaneous cysts.[1] Men are commonly affected, and anogenital area is frequently involved in PEC. Malignant change can occur in 20% of lesions.[2] PTC is a benign tumor that originates from an existing trichilemmal cyst after trauma or inflammation or de novo on scalp in elderly women.[11]
We found one case each of BCC (reported previously)[12] and SCC in the absence of any predisposing factors. BCC has been reported to develop in 0.1% of epidermal cysts.[4] The possible explanation for BCC originating from epidermal cyst lies in their common origin from infundibular portion of hair follicles. Majority of the cases occurred on extra-facial sites.[13] It is possible that repeated mechanical irritation may play a role. Long-standing cysts are likely to be associated with malignant degeneration. The incidence of SCC arising in epidermal cysts is 0.011 to 0.045%.[14] Majority of the cases have been reported on head and neck.[15] Chronic inflammation is postulated to play a role.[14] Excision followed by histologic examination should be done for large, ulcerated, rapidly growing cysts, those that recur or do not respond symptomatically to medical therapy to exclude any underlying malignancy.[14]
Follicular hybrid cyst is a combination of various cysts originating from either infundibulum, isthmus or inferior region of pilosebaceous unit.[16] The most frequent combination is epidermal cyst and trichilemmal cyst (60% cases), with predominant distribution on the scalp and face.[5] Follicular hybrid cyst of trichilemmal cyst and pilomatricoma has been reported in one case.[17] Lichenoid interface dermatitis in the lining of epidermal cysts is uncommon.[18] We observed lichenoid tissue reaction in a follicular hybrid cyst, which has not been described before.
Limitations
The retrospective study design and non-availability of follow-up data, especially for proliferating cysts and cysts with malignant transformation were the main limitations of this study.
Conclusion
The present study highlights the varied histopathological findings in epidermal, trichilemmal, and hybrid cysts, including complications like rupture, inflammation, calcification, and unusual features like PEH, verrucous cyst, proliferating cysts, and malignant tumors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Typical epidermal cyst lined by squamous epithelium with the presence of granular layer and laminated keratin (Hematoxylin and eosin, x100)
(a) Ruptured epidermal cyst showing chronic inflammation and presence of foreign body giant cells in the cyst wall. Laminated keratin can be seen in the lumen (Hematoxylin and eosin, x40). (b) Ruptured epidermal cyst with chronic inflammatory infiltrate and foreign body giant cells in the cyst wall (Hematoxylin and eosin, x100)
Epidermal cyst with ruptured epithelium and presence of cholesterol clefts and hemosiderin pigment in the cyst wall as a sign of old hemorrhage (Hematoxylin and eosin, x100)
(a) Epidermal cyst showing extensive irregular elongation of rete ridges (Hematoxylin and eosin, x50). (b) Pseudoepitheliomatous hyperplasia of the lining of epidermal cyst with keratinization of central zone. No atypical nuclear changes are seen (Hematoxylin and eosin, x100)
Verrucous cyst (a) Bird's eye view showing epidermoid cyst in toto located intradermally (Hematoxylin and eosin, x20). (b) The presence of epidermal papillae in longitudinal and cross sections projecting into the cystic cavity. Epithelium of cyst lining as well as papillae show marked hypergranulosis and thick enveloping keratinous material (Hematoxylin and eosin, x100). (c) Cyst lining showing marked koilocytosis, hypergranulosis, parakeratosis, and thick layer of orthokeratin (Hematoxylin and eosin, x200)
Squamous cell carcinoma arising in epidermal cyst (a) The cyst lining can be seen growing into the cyst wall as nests and islands of neoplastic cells (Hematoxylin and eosin, x100). (b) Neoplastic epithelium with abnormal keratinization in the center (Hematoxylin and eosin, x200)
(a) Typical pilar cyst lined by squamous epithelium showing swollen cells merging into trichilemmal type of keratin. Granular layer is absent (Hematoxylin and eosin, x200). (b) Pilar cyst can sometimes show the presence of parakeratosis and few keratohyalin granules in the epithelial cells (Hematoxylin and eosin, x100)
Hybrid cyst (a) Trichilemmal cyst showing differentiation of epithelium towards pilomatricoma (Hematoxylin and eosin, x40). (b) Trichilemmal cyst showing basaloid cell proliferation, ghost cells, and calcification of keratin products (Hematoxylin and eosin, x100). (c) Trichilemmal cyst showing swollen epithelial cells of cyst lined with trichilemmal keratin (Hematoxylin and eosin, x100)
References
- 1.Kamyab K, Kianfar N, Dasdar S, Salehpour Z, Nasimi M. Cutaneous cysts: A clinicopathologic analysis of 2,438 cases. Int J Dermatol. 2020;59:457–62. doi: 10.1111/ijd.14808. [DOI] [PubMed] [Google Scholar]
- 2.Sau P, Graham JH, Helwig EB. Proliferating epithelial cysts. Clinicopathological analysis of 96 cases. J Cutan Pathol. 1995;22:394–406. doi: 10.1111/j.1600-0560.1995.tb00754.x. [DOI] [PubMed] [Google Scholar]
- 3.Delacretaz J. Keratotic basal-cell carcinoma arising from an epidermoid cyst. J Dermatol Surg Oncol. 1977;3:310–1. doi: 10.1111/j.1524-4725.1977.tb00299.x. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka M, Terui T, Sasai S, Tagami H. Basal cell carcinoma showing connections with epidermal cysts. J Eur Acad Dermatol Venereol. 2003;17:581–2. doi: 10.1046/j.1468-3083.2003.00807.x. [DOI] [PubMed] [Google Scholar]
- 5.Takeda H, Miura A, Katagata Y, Mitsuhashi Y, Kondo S. Hybrid cyst: Case reports and review of 15 cases in Japan. J Eur Acad Dermatol Venereol. 2003;17:83–6. doi: 10.1046/j.1468-3083.2003.00633.x. [DOI] [PubMed] [Google Scholar]
- 6.Nigam JS, Bharti JN, Nair V, Gargade CB, Deshpande AH, Dey B, et al. Epidermal cysts: A clinicopathological analysis with emphasis on unusual findings. Int J Trichology. 2017;9:108–12. doi: 10.4103/ijt.ijt_16_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leppard BJ, Sanderson KV. The natural history of trichilemmal cysts. Br J Dermatol. 1976;94:379–90. doi: 10.1111/j.1365-2133.1976.tb06115.x. [DOI] [PubMed] [Google Scholar]
- 8.Meyer LM, Trying SK, Little WP. Verrucous cyst. Arch Dermatol. 1991;127:1810–2. [PubMed] [Google Scholar]
- 9.Richey PM, Ferguson NN, Stone MS. Verrucous cyst: Possible precursor of proliferating epidermoid cyst. J Cutan Pathol. 2019;46:457–9. doi: 10.1111/cup.13443. [DOI] [PubMed] [Google Scholar]
- 10.Khullar G, Chandra M, Bhargava A. Verrucous epidermoid cyst on the back containing high risk human papillomaviruses-16 and 59. Australas J Dermatol. 2021;62:e133–4. doi: 10.1111/ajd.13416. [DOI] [PubMed] [Google Scholar]
- 11.Satyaprakash AK, Sheehan DJ, Sangueza OP. Proliferating trichilemmal tumors: A review of the literature. Dermatol Surg. 2007;33:1102–8. doi: 10.1111/j.1524-4725.2007.33225.x. [DOI] [PubMed] [Google Scholar]
- 12.Khullar G, Agarwal D, Chandra M. Basal cell carcinoma arising from an epidermoid cyst: A histopathological surprise. Indian Dermatol Online J. 2020;12:351–2. doi: 10.4103/idoj.IDOJ_357_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harada T, Fukumoto T, Shimizu H, Nishigori C. Basal cell carcinoma developed from an epidermal cyst: A case report and review of the literature. Dermatol Reports. 2021;13:9273. doi: 10.4081/dr.2021.9273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Veenstra JJ, Choudhry S, Krajenta RJ, Eide MJ. Squamous cell carcinoma originating from cutaneous cysts: The Henry Ford Experience and review of the literature. J Dermatolog Treat. 2016;27:95–8. doi: 10.3109/09546634.2015.1054779. [DOI] [PubMed] [Google Scholar]
- 15.Frank E, Macias D, Hondorp B, Kerstetter J, Inman JC. Incidental squamous cell carcinoma in an epidermal inclusion cyst: A case report and review of the literature. Case Rep Dermatol. 2018;10:61–8. doi: 10.1159/000487794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Requena L, Sanchez Yus E. Follicular hybrid cysts. An expanded spectrum. Am J Dermatopathol. 1991;13:228–33. doi: 10.1097/00000372-199106000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Miyake H, Hara H, Shimojima H, Suzuki H. Follicular hybrid cyst (trichilemmal cyst and pilomatricoma) arising within a nevus sebaceus. Am J Dermatopathol. 2004;26:390–3. doi: 10.1097/00000372-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Hossler EW, Wilson ML, Dalton SR, Elston DM. Lichenoid inflammation in cutaneous cysts. Am J Dermatopathol. 2010;32:640–1. doi: 10.1097/DAD.0b013e3181cf341f. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Typical epidermal cyst lined by squamous epithelium with the presence of granular layer and laminated keratin (Hematoxylin and eosin, x100)
(a) Ruptured epidermal cyst showing chronic inflammation and presence of foreign body giant cells in the cyst wall. Laminated keratin can be seen in the lumen (Hematoxylin and eosin, x40). (b) Ruptured epidermal cyst with chronic inflammatory infiltrate and foreign body giant cells in the cyst wall (Hematoxylin and eosin, x100)
Epidermal cyst with ruptured epithelium and presence of cholesterol clefts and hemosiderin pigment in the cyst wall as a sign of old hemorrhage (Hematoxylin and eosin, x100)
(a) Epidermal cyst showing extensive irregular elongation of rete ridges (Hematoxylin and eosin, x50). (b) Pseudoepitheliomatous hyperplasia of the lining of epidermal cyst with keratinization of central zone. No atypical nuclear changes are seen (Hematoxylin and eosin, x100)
Verrucous cyst (a) Bird's eye view showing epidermoid cyst in toto located intradermally (Hematoxylin and eosin, x20). (b) The presence of epidermal papillae in longitudinal and cross sections projecting into the cystic cavity. Epithelium of cyst lining as well as papillae show marked hypergranulosis and thick enveloping keratinous material (Hematoxylin and eosin, x100). (c) Cyst lining showing marked koilocytosis, hypergranulosis, parakeratosis, and thick layer of orthokeratin (Hematoxylin and eosin, x200)
Squamous cell carcinoma arising in epidermal cyst (a) The cyst lining can be seen growing into the cyst wall as nests and islands of neoplastic cells (Hematoxylin and eosin, x100). (b) Neoplastic epithelium with abnormal keratinization in the center (Hematoxylin and eosin, x200)
(a) Typical pilar cyst lined by squamous epithelium showing swollen cells merging into trichilemmal type of keratin. Granular layer is absent (Hematoxylin and eosin, x200). (b) Pilar cyst can sometimes show the presence of parakeratosis and few keratohyalin granules in the epithelial cells (Hematoxylin and eosin, x100)
Hybrid cyst (a) Trichilemmal cyst showing differentiation of epithelium towards pilomatricoma (Hematoxylin and eosin, x40). (b) Trichilemmal cyst showing basaloid cell proliferation, ghost cells, and calcification of keratin products (Hematoxylin and eosin, x100). (c) Trichilemmal cyst showing swollen epithelial cells of cyst lined with trichilemmal keratin (Hematoxylin and eosin, x100)


