Abstract
Introduction
We present a case of a fourteen year old girl who presented with a large intra-nasal mass to the ENT team at a district general hospital in the UK.
Presentation of case
The girl presented predominantly with nasal obstruction and some symptoms of allergic rhinitis. Imaging revealed a large lesion abutting the skull base and causing bony remodelling with marked septal deviation. Based both on CT and MRI imaging, the reporting (non-head and neck) radiologist suggested inverted papilloma as a differential diagnosis. Intra-operative exploration in fact revealed a very large left middle turbinate mucocele extending to the left frontal sinus. The mass was excised endoscopically without complications.
Discussion
Although concha bullosa of the middle turbinate of the nose are common, development of a mucocele within them is far less common and for such a mucocele to develop to this size in a child is extremely rare. The egg shell lining of the lesion can be a tell-tale sign of their aetiology when taken alongside other radiological factors. This case highlights challenges in radiological diagnosis of intra-nasal masses in children, which can lead to delays and increased anxiety.
Conclusion
When assessing nasal masses in children it is important to keep a wide differential due to the challenges of diagnosis. A close conversation should be had with local head and neck radiologists and, of course, where there is a unilateral nasal mass tissue sampling is essential and may be taken as part of a full excision where clinically indicated.
Keywords: Concha Bullosa, Mucocele, Middle Turbinate, Nasal Mass, Case Report
INTRODUCTION
This represents a case of child with a very large mucocele of the left middle turbinate who presented to the ENT team within a district general hospital with nasal obstruction and early nasal deformity. CT and MRI scans of the sinuses did not initially provide a clear diagnosis and when surgery was initially planned it was with the possible diagnosis of inverted papilloma in mind. Ultimately the mass was safely excised surgically using an endoscopic technique.
CASE REPORT
This fourteen year old girl presented to ENT with nasal obstruction and frequent sneezing for several years. She complained of frequently feeling short of breath leading to a reduction in physical activity. On examination she had a large fleshy mass filling the left nasal cavity, which could just about be distinguished from the inferior turbinate. The mass was causing right deflection of the nasal septum. RAST blood testing revealed severe allergy to grass, tree pollen and house dust mite. She did not responded adequately to nasal douching, oral antihistamines and topical nasal steroid sprays.
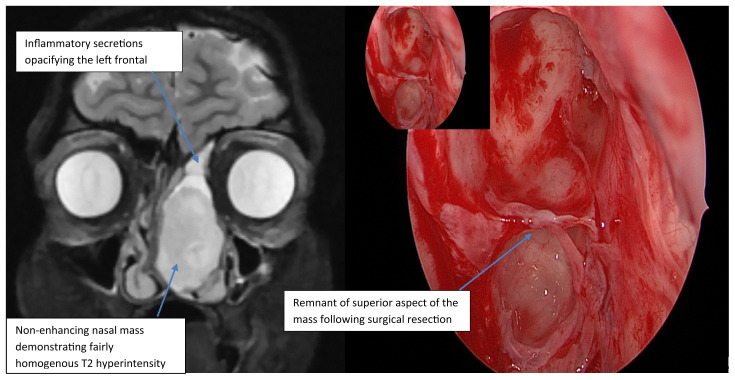
An MRI sinuses followed by a CT sinuses with contrast were arranged. The MRI (Figure 1a,1b) demonstrated a large, well demarcated, minimally lobulated ovoid lesion within the left side of the nasal cavity. It measured 28 mm anteroposteriorly, 20 mm mediolaterally and 34 mm craniocaudally. It returned a fairly homogenous T2 hyperintensity, but less than that of paranasal inflammatory disease. It demonstrated no enhancement. There was resultant displacement of the nasal septum to the right and of the left lateral nasal cavity wall to the left. The lesion was seen to abut the inferior medial aspect of the left orbit but without orbital invasion. There were inflammatory secretions opacifying the left frontal sinus. The lesion was not seen to abut the skull base. Appearances were felt to be most consistent with an inverted papilloma.
Figure 1a and 1b.
Coronal slice of contrast enhanced MRI through level of left nasal mass. 2b shows intraoperative photograph of the left frontal recess region following excision of lesion
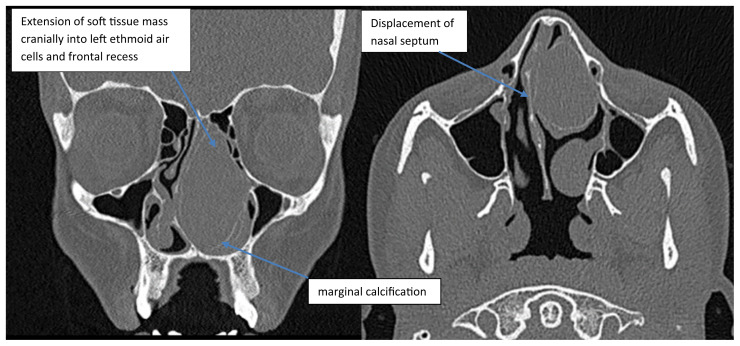
The CT scan (Figures 2a,2b) went on to confirm that the lesion extended cranially into left ethmoidal air cells and frontal sinus. There was clear evidence of thin marginal calcification suggesting its origin was from the middle turbinate. Bony displacement and remodelling was evident with the nasal septum being markedly displaced to the right side and medial wall of left maxillary sinus being displaced laterally. The CT found obliteration of the osteomeatal complexes bilaterally with mild mucosal disease in the maxillary antra and left ethmoid air cells. On balance these findings were again felt most likely to represent inverted papilloma.
Figure 2a and 2b.
Non-contrast enhanced CT of the sinuses. Coronal (1a) and Axial (1b) slices through large left nasal mass
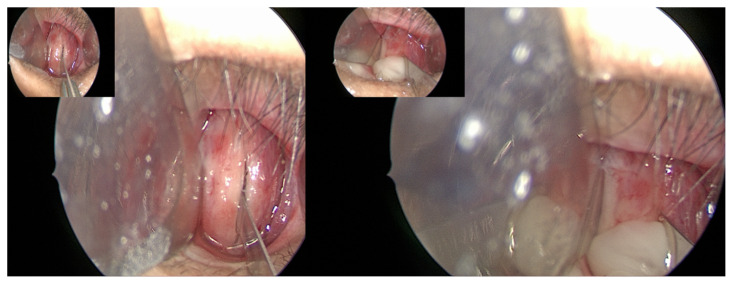
The patient was consented and booked for endoscopic sinus surgery. Intraoperative exploration revealed a very large left middle turbinate mucocele extending to the left frontal sinus. Photos demonstrate incision of the mass and evacuation of the thick mucous contents. The mass was excised endoscopically up to the roof of the frontal sinus. The stump of the middle turbinate insertion on the lateral nasal wall was cauterised with bipolar (10 Watts). The septum was pushed over to midline, but a formal septoplasty will be scheduled once the patient reaches adulthood (Figure 3a,3b).
Figure 3a and b.
Intra-op photographs demonstrating incision into thick anterior wall of concha bullosa and the subsequent drainage of thick mucopus
DISCUSSION
A pneumatized middle turbinate, or a concha bullosa, is a common anatomical variation with a documented prevalence of around 35% (with a range 14–53%) [1]. Pneumatisation of the middle turbinate occurs as part of an extension of the normal process of pneumatization of the ethmoid bone. Most commonly the middle turbinate will be pneumatized by cells from the anterior ethmoid sinus [2], which usually drain into the hiatus semilunaris. There have, though, been reports of pneumatisation from posterior ethmoid air cells as well. Because of the open communication with the ethmoid sinuses and nasal cavity, they can be similarly affected by any mucosal inflammatory disease [2]. In this case there was a background of allergic rhinitis. Uncommonly concha bullosa can become fluid-filled forming a mucocele or, if infected, a mucopyocele. In contrast with other types of mucocele, a mucocele inside a turbinate has an epithelial lining [3]. In their prospective radiological study, Kalairais et al. [2] found that only 2% of patients who had a concha bullosa on CT were found to have a mucocele of the concha bullosa.
According to data from a summary of previous case series [4], the most frequently cited symptoms are nasal obstruction (86%), headache (45%) and rhinorrhoea (36%) . The data suggests a mean age of presentation of 37 with these being exceptionally rare in children. Due to the size, anatomical distortion and associated bony remodelling, mucoceles can often be radiologically mistaken for neoplasms.
The bony rim, present in this case, is often considered the main CT finding that would point to the abnormality being directly related to the turbinate [4] and can be seen in images of similar but smaller example detailed by Eloy et al [5]. This illustrates the importance of CT when assessing sinonasal pathology. It is important to say, however, that there may be an absence of the bony rim in these cases, which is probably due to pressure related remodelling and can contribute to radiological misdiagnoses. Kalairais et al. [4] point out that any secretions within a CB will have a mucoid attenuation of 10–18 HU in the CT scan, which may help to further characterise a soft tissue mass. Although in any unilateral lesion such this, surgical excision for histology would almost certainly be indicated, misdiagnosis in early stages is likely to add to patient anxiety and could potentially lead to mismanagement. Unfortunately, as pointed out by Khalife et al [4], these consequences are difficult to avoid due to a lack of guidelines on this rare pathology.
TEACHING POINT
Although the diagnosis is rare, in a child with a large nasal mass, particularly where there is marginal calcification, mucocele of the middle turbinate is a diagnosis that should be on the list of differentials.
Footnotes
CONSENT: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request
DISCLOSURES: There are no conflicts of interest.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
- 1.Stallman JS, Lobo JN, Som PM. The incidence of concha bullosa and its relationship to nasal septal deviation and paranasal sinus disease. AJNR Am J Neuroradiol. 2004;25(9):1613–1618. [PMC free article] [PubMed] [Google Scholar]
- 2.Kalaiarasi R, Ramakrishnan V, Poyyamoli S. Anatomical variations of the middle turbinate concha bullosa and its relationship with chronic sinusitis: a prospective radiologic study. Int Arch Otorhinolaryngol. 2018;22(3):297–302. doi: 10.1055/s-0038-1625978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fuglsang M, Sørensen LH, Petersen KB, Jesper B. 10-year-old with concha bullosa pyogenic mucocele. BMJ Case Rep. 2018;2018:bcr-2018-224417. doi: 10.1136/bcr-2018-224417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khalife S, Marchica C, Zawawi F, Daniel SJ, Manoukian JJ, Tewfik MA. Concha bullosa mucocele: a case series and review of the literature. Allergy Rhinol (Providence) 2016;7(4):233–243. doi: 10.2500/ar.2016.7.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eloy P, Heylen G, Minavnina J, Ouattassi N. Middle turbinate primary mucocele in a child masquerading as a nasal tumour. B-ENT. 2016;12(2):159–163. [PubMed] [Google Scholar]