Abstract
Introduction and importance:
Demons-Meigs syndrome is a rare condition characterized by the presence of a benign fibroma of the ovary, ascites, and pleural effusion. It is very uncommon, and the diagnosis is made with difficulty based on symptoms that usually mimic disseminated malignancy or tuberculosis, but imaging may confirm the diagnosis. The definitive treatment is laparotomy, after which the symptoms resolve.
Case presentation:
We present a 36-year-old female with Demons-Meigs’ syndrome with severe dyspnea who underwent an abdominal surgical exploration, which revealed ascites of 1500 ml and an ovarian fibroma weighing 7.5 kg and measuring 12 cm in length. There were no postoperative complications. CA-125 was undetectable at 3 months post-procedure.
Clinical discussion:
The most common symptoms are dyspnea, fever, fatigue, and weight loss. In low- and middle-income countries, patients usually present with late-stage disease. The treatment of choice for Demons-Meigs’ syndrome is exploratory laparotomy.
Conclusion:
This tumor is often misdiagnosed as a uterine myoma on sonography. The symptoms resolved, and the patient became asymptomatic after laparotomy and thoracocentesis. For this reason, when patients present with effusion and an abdominal mass, a thorough assessment should be done to confirm if it is Demons-Meigs’ syndrome, which can be completely cured by the removal of the tumor.
Keywords: case report, Demons-Meigs syndrome, giant ovarian fibroma, severe dyspnea
Introduction
Highlights
Demons-Meigs syndrome is a very challenging condition with high mortality and morbidity rates.
This condition is characterized by the presence of a benign fibroma of the ovary, ascites, and pleural effusion.
Computed tomography scan and X-ray are required for diagnosis and for decision, and histopathology confirms the diagnosis.
Exploratory laparotomy and thoracocentesis are gold-standard treatments.
Demons-Meigs’ syndrome was first described in 1887 by Demons and later in 1937 by Meigs, who arrived at the same finding about the association of pleural effusion, ascites, and benign ovarian fibroma. For this reason, this syndrome is also known as Demons-Meigs’ syndrome1. Although it is difficult to determine the incidence of Demons-Meigs’ syndrome, it has been reported that 0.20 per 100 000 women are diagnosed with ovarian sex cord-stromal tumors2. The following characteristics were selected by Meigs in 1945 to define the syndrome: The tumor is a benign fibroma of the ovary, and removal of the tumor must cure the patient3. An atypical case of Meigs’ syndrome was reported in 1990 by Martin et al.4 presenting as bilateral pleural effusion without ascites in a woman with a granulosa cell tumor. Meigs’ syndrome is a benign condition in which pleural effusion and ascites resolve with the removal of the ovarian mass5.
We present a Demons-Meigs syndrome with a giant fibroma of 7.5 kg associated with severe dyspnea in a 36-year-old female. This case has been reported in line with the SCARE criteria6.
Case presentation
A 36-year-old female P5+2 from a rural area presented with a distended abdomen and chest pain that had lasted 10 months. The onset was gradual, and the patient reported palpitations, weight loss, shortness of breath, a non-productive cough, and orthopnea. She had menarche at 14 years old and has had a regular menstrual cycle in history, in the premenopausal period. There was no other significant history.
On physical examination, she was sick-looking and in respiratory distress with tachypnea of 32 cycles per minute. She weighed 50 kg with a body mass index of 15.6 kg/m2 and features of mild dehydration. The blood pressure was 100/69 mmHg, pulse rate of 115 beats per minute, peripheral oxygen saturation of 90% on room air with right-sided chest dullness, decreased vocal resonance, and decreased breath sounds. Abdominal examinations revealed a globally distended abdomen and a nonmobile mass with slight tenderness in the lower quadrants. Percussion revealed a shifting dullness.
The hemoglobin was 9.4 g/dl, white blood cell count: 2.500×109/μl, red blood cell count: 3.230×109/μl, platelet count: 693/mm3, AST (aspartate aminotransferase): 11.4 μ/l, ALT (alanine aminotransferase): 2.0 μ/l, urea: 11.78 mg/dl, and creatinine: 0.58 mg/l. The coagulation profiles were within normal limits, viral markers [HBsAg (hepatitis B surface antigen) and anti-HCV (hepatitis C virus)] were negative, and the CA-125 level was 43 IU/ml (positive). Chest radiography revealed a right-sided pleural effusion (Fig. 1). Contrast-enhanced abdominal computed tomography scan revealed a huge predominantly cystic abdominopelvic mass arising from the right adnexa measuring 16×14×18 cm with a thick peripheral septa plus mild free peritoneal fluid and right pleural effusion (Fig. 2).
Figure 1.
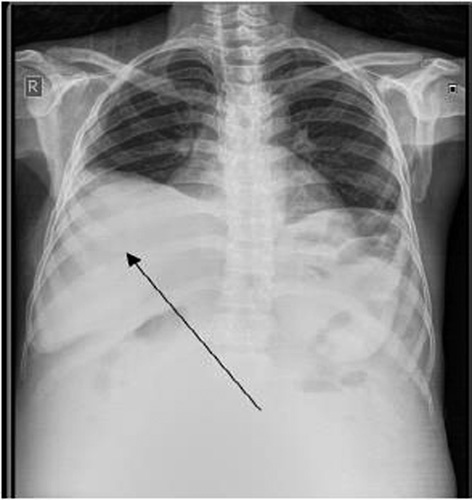
The chest X-ray shows on the right hemithorax image a pleural effusion (arrow).
Figure 2.
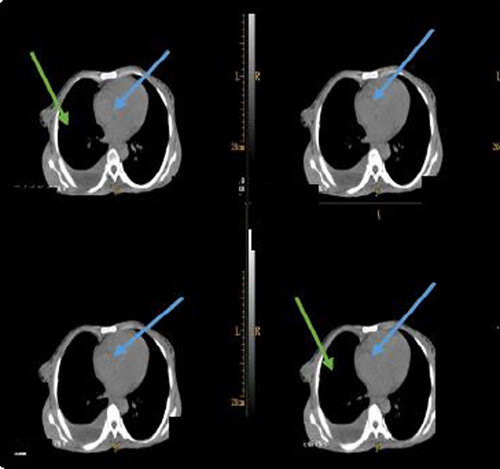
Computed tomography scan showing a huge cystic mass lesion in blue arrow, mild ascites in green arrow, and right pleural effusion.
A definitive diagnosis of giant ovarian mass (fibroma) was made. At laparotomy, a giant right ovarian tumor was removed. A right oophorectomy was also done. The left ovary was normal. The tumor weighed 7.5 kg, measuring 12 cm in diameter (Fig. 3). About 1500 ml of yellow fluid (ascites) was drained. Blood transfusion of 1 unit (250 ml of blood) was given during the operation. An abdominal drain was put in the right iliac fossa of the abdomen. Postoperatively, the patient received ceftriaxone 2 g once daily for 7 days, tramadol 100 mg twice daily for 2 days, and oxygen therapy 5 l/min for 2 days. The abdominal drain was removed on the 7th postoperative day. Thoracocentesis using an underwater seal drainage system was done for the management of dyspnea. There were no postoperative complications noted.
Figure 3.
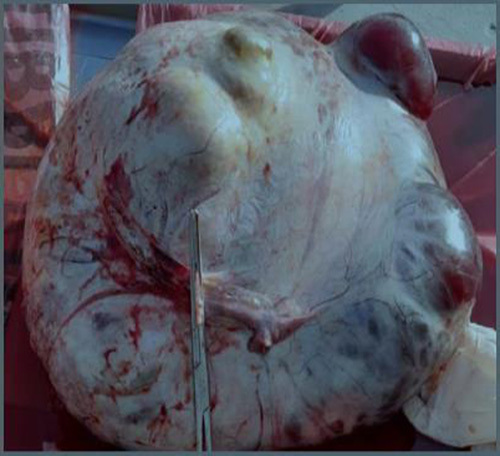
Shows dissected giant ovarian fibroma, weighing 7.5 kg with 38 cm of circumference.
The histopathological analysis of the ovarian tumor revealed a fibroma (a benign tumor composed of bundles of spindle-shaped cells arranged in a whorling pattern). The cells had a fibroblastic appearance with abundant collagen. Cytology testing of the pleural fluid showed no malignant cells. Three months later, CA-125 was undetectable. Clinical resolution was marked by a complete recovery of our patient and no recurrence of pleural or peritoneal effusion.
Discussion
Meigs’ syndrome is a rare condition defined by the presence of a benign tumor of the ovary, ascites, or pleural effusion. If either ascites or pleural effusion is present, it is defined as incomplete or pseudo-Meigs’ syndrome3,7. Ovarian fibroma is found in 2–5% of surgically removed ovarian tumors, and Meigs’ syndrome is observed in about 1%. Ascites are present in 10–15% of those with ovarian fibroma and pleural effusion in 1%, especially with a large lesion3,8. Fibromas are the most common of the sex cord-stromal tumors, which are benign solid neoplasms, usually unilateral, that primarily occur in postmenopausal women8,9. It is a tumor marker associated with ovarian carcinoma9. Immunohistochemical studies suggest that serum CA-125 elevation in patients with Meigs syndrome is caused by mesothelial expression of the antigen rather than by the fibroma10. In our case, the CA-125 level was 43 IU/ml.
The pathophysiology of peritoneal and pleural effusions has been the subject of many theories. Ascites and hydrothorax in Demons-Meigs syndrome are still a subject of discussion and conjecture. Although numerous pathophysiological hypotheses have been proposed, the vascular (venous and lymphatic) theory seems more compelling because it is unicast11. According to Dockerty and Masson, a pelvic tumor’s twisting in 1944 caused a partial occlusion of the venous return, which was the cause of ascites. Then, it transudates through the capsule as the serous fluid12.
According to Meigs et al., an increase in pressure in the intratumoral lymphatics causes fluid to seep through the peritoneum, which is the genesis of ascites. Transdiaphragmatic lymphatic pathways are hypothesized to be involved in the transport of peritoneal fluid to the pleural cavity. The right has a pleural effusion predominance since this network is more established on the right than on the left. The tumor edema brought on by compression or twisting of the fibroid on its axis is assumed to be the cause of the ascites11,13,14. The right hemithorax had hydrothorax, according to our case study.
The most common presenting symptoms are dyspnea (due to pleural effusion), fatigue, and weight loss. Usually, in low- and middle-income countries, extreme presentations of late-stage diseases occur due to the fragility of healthcare systems and also due to cultural and economic reasons11,15. The treatment of choice for Demons-Meigs’ syndrome is exploratory laparotomy, then thoracocentesis if pleural effusion is causing dyspnea. By definition of the syndrome, after tumor removal, the symptoms resolve, and the patients become asymptomatic5,13. However, considering that ovarian pathology is a benign disease, symptoms usually strongly mimic disseminated malignancy.
Conclusion
Giant ovarian fibromas in Demons-Meigs syndrome are an uncommon disease and usually associated with peritoneal and pleural effusion. The symptoms resolve and the patients become asymptomatic after removal of the tumor at laparotomy. When patients present with effusion and an abdominal mass, a thorough assessment should be done to confirm if it is Demons-Meigs syndrome, which can be completely cured by the removal of the tumor.
Ethical approval
Ethical approval is exempt/waived at our institution.
Consent
Written informed consent was obtained from the patient’s parents/legal guardian for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
There was no external funding source for this case report.
Author contribution
A.A.A., J.B.M., Y.A., and A.O.A.: managed the patient and wrote the first draft; A.A.O., J.M., and F.K.S.: helped in editing and reviewing the paper. All authors read and approved the final version to be published.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
Baanitse Munihire Jeannot.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 17 October 2023
Contributor Information
Abdifatah Abdi Ali, Email: drmaash30@gmail.com.
Baanitse Munihire Jeannot, Email: jeannotb001@gmail.com.
Anthony Ayotunde Olasinde, Email: olasindetony@gmail.com.
Yusuf Abdirizak, Email: drjalaal@hotmail.com.
Abdirahin Omar Amin, Email: Dr.abdirahimomar@gmail.com.
Joshua Muhumuza, Email: joshuablessed7@gmail.com.
Franck Katembo Sikakulya, Email: francksikakulya@gmail.com.
References
- 1.Brun JL. Demons syndrome revisited: a review of the literature. Gynecol Oncol 2007;105:796–800. [DOI] [PubMed] [Google Scholar]
- 2.Quirk JT, Natarajan N. Ovarian cancer incidence in the United States, 1992–1999. Gynecol Oncol 2005;97:519–523. [DOI] [PubMed] [Google Scholar]
- 3.Meigs JV. Fibroma of the ovary with ascites and hydrothorax; Meigs syndrome. Am J Obstet Gynecol 1954;67:962–985. [DOI] [PubMed] [Google Scholar]
- 4.Martin F, Brouche S, Haidar A. A propos d’un cas avec tumeur ovarienne de la granulosa. Rev Pneumol Clin 1990;46:123–124. [PubMed] [Google Scholar]
- 5.Kortekaas KE, Pelikan HM. Hydrothorax, ascites and an abdominal mass: not always signs of a malignancy: three cases of Meigs’ syndrome. J Radiol Case Rep 2018;12:17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha RA, Franchi T, Sohrab C, et al. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 2020;84:226–230. [DOI] [PubMed] [Google Scholar]
- 7.Antunes M, Pizzol D, Zambon M, et al. Giant ovarian fibroma with associated Meigs syndrome in low resources setting: a case report. J Surg Case Rep 2019;4:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thirkell D, Taylor JH, Ingram CG. Meig’s syndrome: a case report. J Coll Gen Pract 1963;6:400–407. [PMC free article] [PubMed] [Google Scholar]
- 9.Benjapibal M, Sangkarat S, Laiwejpithaya S, et al. Meigs’ syndrome with elevated serum CA125: case report and review of the literature. Case Rep Oncol 2009;2:61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krenke R, Maskey-Warzechowska M, Korczynski P, et al. Pleural effusion in Meigs’ syndrome – transudate or exudate? Systematic review of the literature. Medicine (Baltimore) 2015;94:e2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slaoui A, Lazhar H, Amail N, et al. Meigs syndrome: about an uncommon case report. Clin J Obstet Gynecol 2023;6:010–013. [Google Scholar]
- 12.Dockerty MB, Masson JC. Ovarian fibromas: a clinical and pathologic study of two hundred and eighty-three cases. Am J Obstet Gynecol 1944;47:741–752. [Google Scholar]
- 13.Meigs JV, Armstrong SH, Hamilton HH. A further contribution to the syndrome of fibroma of the ovary with fluid in the abdomen and chest, Meigs’ syndrome. Am J Obstet Gynecol 1943;46:19–37. [Google Scholar]
- 14.Berthiot G, Belair F, Marcon JM, et al. Syndrome de Demons-Meigs. Concoursmed 1989;111:427–431. [Google Scholar]
- 15.Handler CE, Fray RE, Snashall PD. Atypical Meigs’ syndrome. Thorax 1982;37:396–397. [DOI] [PMC free article] [PubMed] [Google Scholar]


