Abstract
Introduction
Dental implants have been used in a variety of conventional technique-based forms for many years which had its own drawbacks. With the advent of cone beam CT, proper surgical and prosthetic planning is possible now a days. To achieve ideal implant placement, good prosthetic fabrication and overall successful prognosis computer fabricated guide aided surgery have been developed.
Aim and Objective
The aim of this study was to compare and evaluate the accuracy of implant placement in partially edentulous patients with conventional free hand technique and computer fabricated guide of implant placement by comparing pre- and post-CBCT data.
Methods
The present split mouth study design was conducted with forty sample size on twenty randomly selected patients who were treated with bilateral partially edentulous sites requiring dental implants. Patients were treated with both conventional (free hand) technique and computer fabricated 3D guide aided technique of implant placement. Comparison of accuracy of implant placement was done by comparing the pre- and postoperative CBCT data in terms of mean coronal deviation, mean apical deviation and mean angular deviation.
Results and Conclusion
The results showed that there is no statistically significant difference between mean coronal deviation, mean apical deviation and mean angular deviation of planned and placed implants in both conventional technique (free hand technique) and computer fabricated 3D guide aided implant placement technique. Hence, this study concluded that conventional technique of implant placement is equally efficient in comparison with computer fabricated guide aided surgery in terms of accuracy of implant placement.
Keywords: Dental implant, Surgical guide, Partial edentulism, CBCT
Introduction
Implant dentistry is a unique way to restore the stomatognathic system to a normal contour, function and esthetics along with significant improvement in the quality of patient’s life.
Dental implants have been placed by a variety of techniques for many years, with each has its own drawbacks.
Improper implant positioning with an incidence greater than 10% is reported which can result in esthetic, biological and technical complications and can, in extreme situations, render the desired prosthetic rehabilitation impossible to achieve [1]. With the advent of CBCT in technological development, proper preoperative planning for position, number and angulation of implant is done to achieve surgically and prosthetically driven optimum results. CBCT scans help in the planning of oral implants like; they enable measurement of the distance between the alveolar crest and mandibular canal to avoid impingement of inferior alveolar nerve, avoid perforation of the mandibular posterior lingual undercut, assess the density and quality of bone and help in planning of the oral implant in the maxilla with special attention to the nasopalatine canal and maxillary sinus [2].
The literature highlights the use of surgical template in implantology to be more precise compared with the free-hand method [3–5]. In computer fabricated guide aided implant surgical technique, image analysis of both maxilla and mandible is obtained by cone beam CT in different planes. Implant related software is used for the image analysis, and a surgical stent evaluation is performed to establish the targeted implant position for desired results. The accuracy assessment between planned and placed implant position is based upon comparing the preoperative and postoperative CBCT data over the treatment plan.
The null hypothesis was that the computer fabricated guide aided surgery is more efficient in accuracy of implant placement when compared with conventional free hand technique.
Materials and Methodology
The present comparative study was conducted from Jan 2020 to June 2021 with 40 sample size on 20 patients reporting to the outpatient for the treatment of their missing teeth on both sides of either upper or lower jaw with healthy systemic and oral status; and without severe alveolar bone atrophy, major alveolar hard and/or soft tissue deficiency, mouth opening restriction, heavy smoking (> 10 cigarettes per day) and parafunctional habits were included in the study. The patients were selected irrespective of sex, social status, caste and creed.
Source of Data
A total of 20 adult patients with bilateral partial edentulism on either upper or lower jaw were included. In this split mouth study, the same patient served as the control and test site.
Control site On one side was treated by using conventional technique (free hand technique) of implant placement.
Test site Contralateral side was treated by using computer fabricated 3D guide aided technique of implant placement.
Armamentarium
Perforated impression trays (Metallic).
Addition silicone putty impression material with light body.
Chlorhexidine gluconate, mouth wash (0.12%)
Preoperative antibiotics and premedications.
CBCT-based computer fabricated surgical guide.
Physiodispenser with micromotor.
20:1 contra-angle reduction handpiece with internal and external cooling.
Densah burs for sinus lift procedure wherever required.
Bone graft and bio-resorbable healing membrane if required.
Osstem implants of width of 4–4.5 mm and length 8–8.5 mm.
Osstem implants kit (both one guide and taper kit).
Other surgical instruments used routinely for incision, flap reflection and suturing.
Platelet rich fibrin (PRF) Centrifuge System.
3–0 silk suture.
Workflow of Design and Fabrication of Cone Beam CT Image-Based 3D Templates
For preoperative planning, the initial oral situation of the patients was recorded by means of cone beam computed tomography.
In addition, a 3D dataset was generated in stereolithography format with scanning the master casts. The information of patient’s intraoral soft tissue surface was saved as Surface Tessellation Language (STL) file, and Patient’s hard tissue information was obtained by taking CBCT which is saved as Digital imaging and communications in medicine (DICOM) file.
CBCT DICOM data, STL file and the 3D dataset of the master casts were then fed into the Blue Sky Bio software.
In accordance with the principles of backward planning and to simulate the final prosthetic restoration, virtual dental crowns were prepared in terms of form, size and position to perfectly restore the dental arch. Implants were then virtually placed according to the final position of the prosthetic crown.
The standardized preoperative planning was transferred to a surgical template that was then printed in 3D.
Surgical Technique
Preoperative Management
After proper planning and selection, patient was recalled on the day of appointment. Informed consent was taken, and vitals of the patient were noted. Premedication (Tab. Augmentin 625 mg, Tab. Novagesic-SP, Cap. Pantop-DSR) was given to the patient 30 min to 1 h before the surgical procedure. Patient was asked to rinse with 0.12% chlorhexidine gluconate mouth wash for one minute preoperatively. Patient was shifted to minor OT and seated comfortably in the dental chair.
Implant Placement on Control Site
Patient was prepared under strict aseptic conditions and was scrubbed with 5% povidone-iodine solution both extraorally and intraorally. Proper draping of the patient was done using sterile sheets, exposing the area to be operated. Local anesthesia in the required area was given using lignocaine hydrochloride 2% with adrenaline (1:200,000). After achieving the proper local anesthesia, intraoral crestal incision in the selected area of implant placement was given. Mucoperiosteal flaps were elevated buccally and palatally/lingually. Osstem taper kit (Fig. 1) was used for osteotomy preparation. Initial site of implant placement was marked with a pilot drill, used at a drill speed of 800–900 rpm with copious sterile saline irrigation. Twist drills of progressively increasing diameters were used according to the length and diameter of implant to be placed. Angulations were checked with paralleling pins.
Fig. 1.

Osstem taper kit
The implant of selected diameter and length was then placed in the prepared socket, using motorized insertion tool. Final placement of the implant was done at subcrestal level using torque motorized insertion tool wrench at 25–30 N/cm was ensured sufficient bone implant contact (BIC). After this, the implant was covered with cover screw. The mucosa was adapted over the implant and sutured with 3–0 silk suture.
Implant Placement on Test Site
Patient was prepared under strict aseptic conditions and was scrubbed with 5% povidone-iodine solution both extraorally and intraorally. Proper draping of the patient was done using sterile sheets, exposing the area to be operated. Local anesthesia in the required area was given using lignocaine hydrochloride 2% with adrenaline (1:200000). After achieving the proper local anesthesia, computer fabricated surgical guide was placed in the edentulous area and stabilized with the help of dentulous part (Fig. 2). Osstem one guide kit (Fig. 3) was used for osteotomy procedure. Flapless technique was followed, and tissue was punched at the predetermined operative site by using tissue punch from the one guide kit. Initial site of implant placement was marked with a pilot drill, used at a drill speed of 800–900rpm with copious sterile saline irrigation. Twist drills of progressively increasing diameters were used according to the length and diameter of implant to be placed. Whole of the osteotomy procedure was done through the surgical guide. The depth was checked after using each twist drill with the help of depth gauge.
Fig. 2.
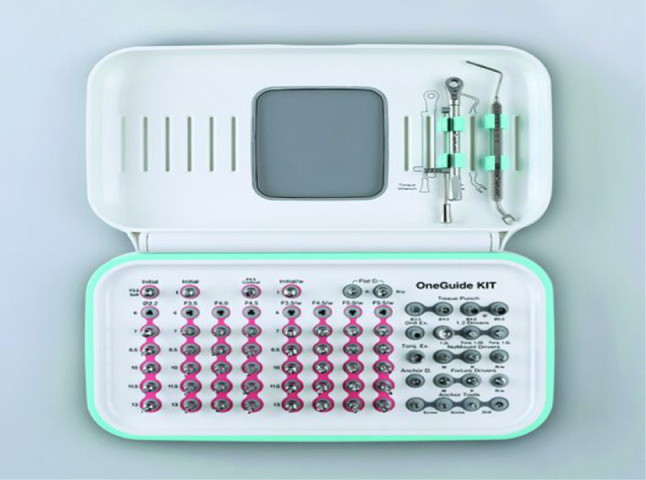
Osstem one guide kit
Fig. 3.
Computer fabricated 3D guide implant placement
Following the same technique repeated as earlier described. After this, the implant was covered with cover screw. The mucosa was adapted over the implant and sutured with 3-0 silk suture if required.
Data Collection
Six months after placing the implant with digital surgical guide or conventional free hand technique, CBCT was taken to evaluate the implant accuracy.
The parameters of implant placement that were measured and compared are:
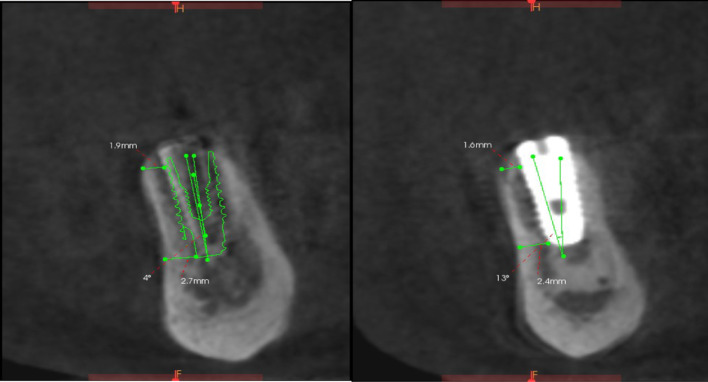
The coronal deviation (in mm), apical deviation (in mm) and angle deviation (in °) of planned implant and inserted implant were measured to evaluate the accuracy using NNT software (Figs. 4, 5).
Fig. 4.
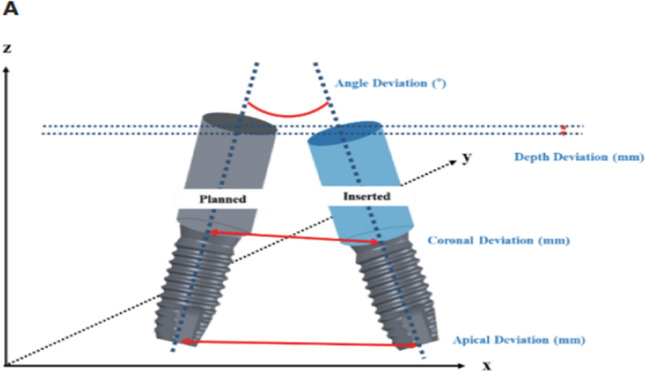
Illustrations of the deviations between planned and inserted implant
Fig. 5.
Treatment evaluation showing the deviation between preoperative and postoperative implant position
Statistical Analysis
After comparing the preoperative and postoperative CBCT data, the following results were obtained (Table 1; Figs. 6, 7).
Table 1.
Site wise placement of implants
| Site | No. of implants | Percentage |
|---|---|---|
| Maxillary anterior | 6 | 10 |
| Maxillary posterior | 20 | 33.33 |
| Mandibular anterior | 7 | 11.67 |
| Mandibular posterior | 27 | 45 |
Fig. 6.
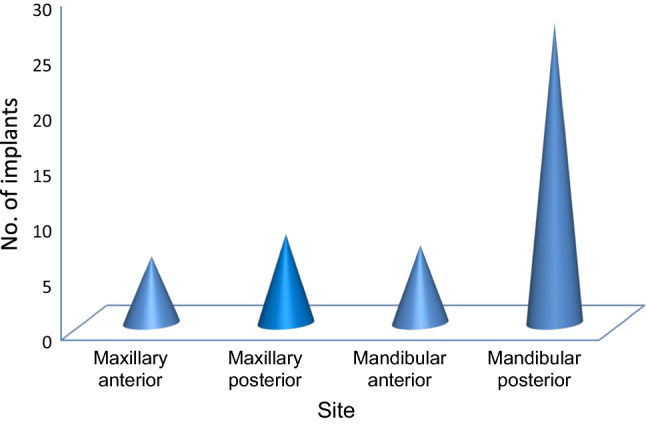
Site wise placement of implants
Fig. 7.
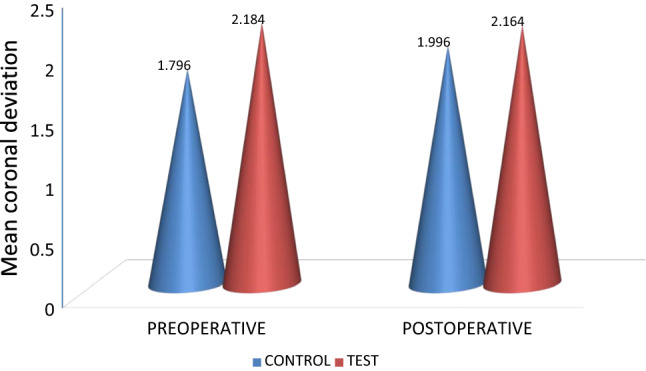
Comparison of Coronal deviation taken preoperatively and postoperatively using paired T test
Table 2 summarizes the coronal deviation seen in control and test site preoperatively with mean of 1.796 ± 1.09 and 2.184 ± 0.79, respectively, and postoperatively with mean of 1.996 ± 1.13 and 2.164 ± 0.91, respectively, compared using paired T test with t-value − 1.411 and p value 0.165 preoperatively and t-value − 0.568 and p value 0.573 postoperatively. The p value of the compared data is greater than 0.05 which makes the test clinically insignificant (Fig. 8).
Table 2.
Comparison of Coronal deviation taken preoperatively and postoperatively using paired T test
| Coronal deviation | Control site | Test site | Difference | t-value | p value | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Preoperative | 1.796 | 1.095 | 2.184 | 0.799 | − 0.388 | − 1.411 | 0.165 |
| Postoperative | 1.996 | 1.132 | 2.164 | 0.918 | − 0.168 | − 0.568 | 0.573 |
Fig. 8.
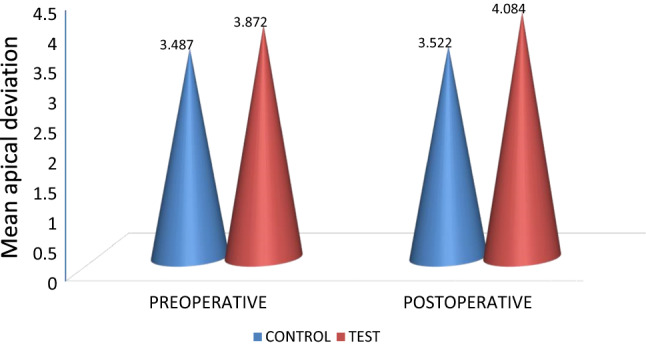
Comparison of apical deviation taken preoperatively and postoperatively using paired T test
Table 3 summarizes the apical deviation seen in control and test sites preoperatively with mean of 3.487 ± 1.22 and 3.872 ± 1.52, respectively, and postoperatively with mean of 3.522 ± 1.66 and 4.084 ± 1.88, respectively, compared using paired T test with t-value − 0.956 and p value 0.344 preoperatively and t-value − 1.093 and p value 0.280 postoperatively. The p value of the compared data is greater than 0.05 which makes the test clinically insignificant (Fig. 9).
Table 3.
Comparison of Apical deviation taken preoperatively and postoperatively using paired T test
| Apical deviation | Control site | Test site | Difference | t-value | p value | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Preoperative | 3.487 | 1.2263 | 3.872 | 1.5326 | − 0.385 | − 0.956 | 0.344 |
| Postoperative | 3.522 | 1.6602 | 4.084 | 1.8830 | − 0.562 | − 1.093 | 0.280 |
Fig. 9.
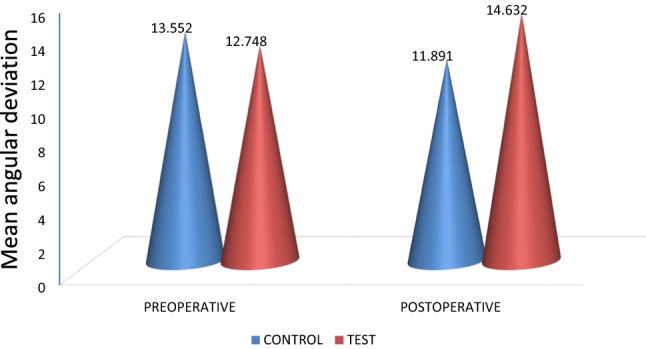
Comparison of angular deviation taken preoperatively and postoperatively using paired T test
Table 4 summarizes the angular deviation seen in control and test site preoperatively with mean of 13.552 ± 8.05 and 12.748 ± 9.04, respectively, and postoperatively with mean of 11.891 ± 7.53 and 14.632 ± 8.69, respectively, compared using paired T test with t-value 0.324 and p value 0.747 preoperatively and t-value − 1.163 and p value 0.251 postoperatively. The p value of the compared data is greater than 0.05 which makes the test clinically insignificant.
Table 4.
Comparison of Angular deviation taken preoperatively and postoperatively using paired T test
| Angular deviation | Control site | Test site | Difference | t-value | p value | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Preoperative | 13.552 | 8.0506 | 12.748 | 9.041 | 0.804 | 0.324 | 0.747 |
| Postoperative | 11.891 | 7.5305 | 14.632 | 8.690 | − 2.740 | − 1.163 | 0.251 |
Results
The preoperative and postoperative values of mean and standard deviation of all three parameters of accuracy of implant placement, i.e., coronal deviation (p = 0.251), apical deviation (p = 0.280) and angular deviation (p = 0.573) of both control and test sites were compared by using paired T test to calculate the p value and concluded that there was no statistically significant difference in terms of accuracy of implant placement with conventional technique and computer fabricated 3D guide aided implant surgical technique (p > 0.05).
Discussion
In this present study, accuracy of implant placement was evaluated for guided vs conventional technique. Mistakes in the positioning of the implant are one of the main errors in implant dentistry. The precise and prosthetically functional placement of the implant is of utmost importance if reliable sustainability is to be maintained. It is not enough to perform preoperative planning. A good outcome can only be obtained by precisely transferring preoperative virtual planning to the clinical situation [6].
When implants are placed free hand without the surgical guide, the surgeon’s experience seems to be the more relevant factor. Experienced surgeons show significantly less mesiodistal angular deviations when implant preparation performed without use of surgical guide [7]. It has frequently been reported that the level of experience influences the outcome of treatment. Results from the study by Cho et al. support this statement [8]. A prospective, multicentric clinical study with 2641 placed implants demonstrated a certain learning curve. Less experienced clinicians failed more frequently compared with experienced clinicians [9]. In 2008, Van de Velde observed how the final position achieved by students differed significantly from the one that was achieved by specialists [10]. By contrast, Kohavi et al. found that clinical experience does not correlate with treatment outcome. However, in this study, the experienced clinicians were accompanied by faculty members so bias of years of clinical experience is ruled out [11].
Current trend in dental implant surgery is to further improve the conventional surgical techniques, by reducing the total rehabilitation time and by using less invasive surgical technique. With guided implant protocol, implant site scan be decided before surgery according to bone volume and quality, location of anatomical structures (nerves, vessels and sinuses) prosthetic and esthetic evaluation. Additionally, an accurate implant surgery planning allows sometimes to avoid bone augmentation procedures and hence, reduces the overall treatment time [12].
In order to transfer the planned implant position information to the clinical situation, two types of computer-generated surgical guides are available, static and dynamic.
STATIC—type of surgical guide uses CBCT generated computer aided design and stents with metal tubes, and a surgical system that uses coordinated instrumentation to place implant using the same. Advantages of static guide is increased predictability, reduced invasiveness of surgical procedures, less healing period, decreased treatment time and increased patient satisfaction (Fig. 4).
DYNAMIC—type of surgical guide system involves transferring the selected implant position to the surgical area via visual imaging tool on a monitor. Advantage of using dynamic guided implant surgery is that it allows the surgeon to adjust the implant position in real time [13].
In the present study, we used static type of surgical guide instead of dynamic type because dynamic surgical guide system is more costly and not easily available.
Further, a in vivo study has shown that using anchor microscrews can increase the seating and functional stability of computer fabricated 3D guide during drilling process of implant placement [14]. But we used static guide without anchor microscrews due to lack of availability from laboratory.
Based on the results of the screened literature, it has been found that there is lack of high level of scientific studies that could compare conventional implant protocols (free hand) with digital workflows [15–17]. Our study is one of its kind in which we compare the accuracy of implant placement with conventional surgical technique (free hand) and 3D guided surgical technique based upon CBCT data.
Implant planning was done with the help of preoperative CBCT data and NNT software. Postoperative CBCT was done after six months for all the patients of both sites, and various parameters of accuracy of implant placement were compared with the preoperative CBCT records in terms of mean coronal deviation, mean apical deviation and mean angular deviation of planned and placed implant.
The results of our study are in accordance with the study conducted by Colombo et al. [16]. They performed a study based upon randomized controlled trials to know about the clinical application and effectiveness of guided surgery in comparison with traditional procedures and found results to be statistically non-significant [17].
A clinical study done by Cunha et al. [17], a total of 61 implants were analyzed and compared for mean coronal deviation, apical deviation, angular deviation and central deviation of planned and placed implant, found no statistically significant difference in accuracy of implant placement with computer guided implant surgery using prototype surgical guides [18].
On the contrary, Filius et al. [18] found the benefits of full three-dimensional computer guided virtual workflow to place implants in oligodontia patients. They concluded that application of computer designed surgical guide enables predictable implant placement in patients with oligodontia, where bone quality and limited interdental space can be a challenge for implant placement [19].
The possible explanation to this is that in our study, static type of surgical guide has been used for implant placement instead of full three-dimensional computer guided virtual work flow (Dynamic guide system) used in this study conducted by Filius et al. [18]. This difference in guide design supposedly influenced significant accuracy in dynamic guide system [12] giving contradictory results to our study [13, 19].
Additionally, Zhou et al. [19] systematically reviewed and analyzed the current literature regarding clinical accuracy of guided implant surgery. They concluded that the position of guide, guide fixation, type of guide and flap approach could influence the accuracy of computer guided implant surgery [20]. In our study, tooth and tissue support was taken and anchor screws were not used to fix the surgical guide in place. This probably caused micro movement of template during surgery which may be thought to have deviated the planned implant position.
Colombo et al. [16] studied the review which included only randomized controlled trials (RCTs) focusing on subjects treated with digital workflow for implant placement compared to conventional procedures. The results concluded that there were no statistically significant differences between clinical cases treated with digital protocols and those treated with conventional one hence supporting our study [17].
From this point of view, in majority of clinical situations, conventional free hand implant placement can be considered a good option where guided system cannot be used.
Conclusion
This study concluded that in terms of accuracy of dental implant placement, there is no statistically significant difference between conventional technique (free hand) of implant placement and computer fabricated guide aided implant placement technique.
However, further comparative analysis should be done in static versus dynamic implant guide-based system with and without anchor screws to look into the actual pros and cons associated herewith to reach a more conclusive outlook.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The ethical clearance for conducting the study was obtained from ethical committee of the institution.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tallarico M, Scrascia R, Annucci M, Meloni SM, Lumbau AI, Koshovari A, Xhanari E, Martinolli M. Errors in implant positioning due to lack of planning: a clinical case report of new prosthetic materials and solutions. Materials. 2020;13(8):1883. doi: 10.3390/ma13081883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta J, Ali SP. Cone beam computed tomography in oral implants. Natl J Maxillofac Surg. 2013;4(1):2. doi: 10.4103/0975-5950.117811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nickenig HJ, Wichmann M, Hamel J, Schlegel KA, Eitner S. Evaluation of the difference in accuracy between implant placement by virtual planning data and surgical guide templates versus the conventional free-hand method—a combined in vivo–in vitro technique using cone-beam CT (Part II) J Cranio-Maxillofac Surg. 2010;38(7):488–493. doi: 10.1016/j.jcms.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 4.Vermeulen J. The accuracy of implant placement by experienced surgeons: guided vs freehand approach in a simulated plastic model. Int J Oral Maxillofac Implants. 2017;32(3):617–624. doi: 10.11607/jomi.5065. [DOI] [PubMed] [Google Scholar]
- 5.Arısan V, Karabuda CZ, Mumcu E, Özdemir T. Implant positioning errors in freehand and computer-aided placement methods: a single-blind clinical comparative study. Int J Oral Maxillofac Implants. 2013;28(1):190–204. doi: 10.11607/jomi.2691. [DOI] [PubMed] [Google Scholar]
- 6.Alevizakos V, Mitov G, Stoetzer M, von See C. A retrospective study of the accuracy of template-guided versus freehand implant placement: a nonradiologic method. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128(3):220–226. doi: 10.1016/j.oooo.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Payer M, Kirmeier R, Jakse N, Pertl C, Wegscheider W, Lorenzoni M. Surgical factors influencing mesiodistal implant angulation. Clin Oral Implant Res. 2008;19(3):265–270. doi: 10.1111/j.1600-0501.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 8.Cho UH, Yu W, Kyung HM. Root contact during drilling for microimplant placement: effect of surgery site and operator expertise. Angle Orthod. 2010;80:130–136. doi: 10.2319/011509-535.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lambert PM, Morris HF, Ochi S. Positive effect of surgical experience with implants on second-stage implant survival. J Oral Maxillofac Surg. 1997;55:12–18. doi: 10.1016/S0278-2391(16)31192-2. [DOI] [PubMed] [Google Scholar]
- 10.Van de Velde T, Glor F, De Bruyn H. A model study on flapless implant placement by clinicians with a different experience level in implant surgery. Clin Oral Implants Res. 2008;19:66–72. doi: 10.1111/j.1600-0501.2007.01423.x. [DOI] [PubMed] [Google Scholar]
- 11.Kohavi D, Azran G, Shapira L, Casap N. Retrospective clinical review of dental implants placed in a university training program. J Oral Implantol. 2004;30:23–29. doi: 10.1563/1548-1336(2004)030<0023:RCRODI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Cristache CM, Gurbanescu S. Accuracy evaluation of a stereolithographic surgical template for dental implant insertion using 3D superimposition protocol. Int J Dent. 2017 doi: 10.1155/2017/4292081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Block MS, Emery RW. Static or dynamic navigation for implant placement choosing the method of guidance. J Oral Maxillofac Surg. 2016;74(2):269–277. doi: 10.1016/j.joms.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 14.Mai HN, Lee DH. Effects of supporting conditions and anchor microscrew on the stabilization of the implant guide template during the drilling process: an in vitro study. J Prosthet Dent. 2020;124(6):727–e1. doi: 10.1016/j.prosdent.2020.06.033. [DOI] [PubMed] [Google Scholar]
- 15.Pozzi A, Tallarico M, Marchetti M, Scarfò B, Esposito M. Computerguided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomized controlled trial. Eur J Oral Implantol. 2014;7(3):229–42. [PubMed] [Google Scholar]
- 16.Vercruyssen M, Van de Wiele G, Teughels W, Naert I, Jacobs R, Quirynen M. Implant-and patient-centred outcomes of guided surgery, a 1-year follow-up: an RCT comparing guided surgery with conventional implant placement. J Clin Period Ontol. 2014;41(12):1154–1160. doi: 10.1111/jcpe.12305. [DOI] [PubMed] [Google Scholar]
- 17.Colombo M, Mangano C, Mijiritsky E, Krebs M, Hauschild U, Fortin T. Clinical applications and effectiveness of guided implant surgery: a critical review based on randomized controlled trials. BMC Oral Health. 2017;17(1):1–9. doi: 10.1186/s12903-017-0441-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cunha RM, Souza FÁ, Hadad H, Poli PP, Maiorana C, Carvalho PSP. Accuracy evaluation of computer-guided implant surgery associated with prototyped surgical guides. J Prosthet Dent. 2021;125(2):266–272. doi: 10.1016/j.prosdent.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 19.Filius MA, Kraeima J, Vissink A, Janssen KI, Raghoebar GM, Visser A. Three-dimensional computer-guided implant placement in oligodontia. Int J Implant Dent. 2017;3(1):1–8. doi: 10.1186/s40729-017-0090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou W, Liu Z, Song L, Kuo CL, Shafer DM. Clinical factors affecting the accuracy of guided implant surgery—a systematic review and meta-analysis. J Evid Based Dental Pract. 2018;18(1):28–40. doi: 10.1016/j.jebdp.2017.07.007. [DOI] [PubMed] [Google Scholar]