Abstract
A cross-sectional study was conducted to (1) examine breastfeeding initiation and continuation rates, and; (2) investigate association between food insecurity and breast-feeding status, among low-income mothers. Mothers of infants two-months or younger were recruited from a local pediatric clinic serving primarily low-income families. Upon giving consent, mothers were interviewed in-person or over the phone in either English or Spanish. Of the total 92 mothers interviewed, 90% initiated breastfeeding, but only 24% were doing exclusive breastfeeding at 2 months of infant’s age. After controlling for socio-demographics, it was found that food-insecure mothers were less likely to continue with breastfeeding (β = −1.51, p = .024). Future research is warranted to understand pathways through which food insecurity affects breastfeeding and how this disparity can be prevented to ensure a safe and secure start for infants worldwide.
Background
Breast milk is widely recognized as the most complete form of nutrition for infants. Both the World Health Organization (WHO) and the American Academy of Pediatrics recommend practicing exclusive breastfeeding for the first six months of life and continuing it for up to two years of age or longer along with complementary foods (Breastfeeding Report Card, 2020; Recommendations for breastfeeding, 2017). Breastfeeding not only promotes optimal growth and development for infants, but it also helps mothers lose weight gained during pregnancy and reduces chronic disease burdens, such as type 2 diabetes and hypertension (Dieterich et al., 2012). Due to its many known benefits to children and mothers, promotion of breastfeeding has become a key public health strategy at a global level, and several policies and programs are promoted to improve breastfeeding rates worldwide. For instance, the Global Breastfeeding Collective led by WHO and UNICEF, involving partnership of more than 20 prominent international agencies, called for increased investment in breastfeeding to make the progress and raise the global rate of exclusive breastfeeding to at least 50 percent by 2025 (Breastfeeding: A smart investment, 2017).
In the U.S., around 83% of mothers initiate breastfeeding but only 57% are breastfeeding any or exclusively at six months of infant’s age (Breastfeeding Report Card, 2020). This pattern demonstrates that most mothers in the U.S. start out following the suggestion of breastfeeding their infant, but do not continue for the recommended period of time. Especially, women living below poverty, being younger, or being an African American are less likely to breastfeed or discontinue earlier than their counterparts (Meedya et al., 2010). A negative relationship has also been seen between maternal BMI and breastfeeding. In the review of literature, Amir and Donath (2007), found that overweight or obese mothers were two times more likely to discontinue breastfeeding earlier in comparison to women with a normal BMI.
Household food insecurity, or inconsistent access to a sufficient amount of high quality and nutritious food, is a significant predictor of poor health worldwide. Approximately 1.9 billion people at a global level experience moderate to severe levels of food insecurity, involving worry about the ability to afford food, eating very monotonous low-cost meals to severe levels of skipping meals and experiencing hunger. While the greatest number of food insecure people are in Sub-Saharan Africa and South Asia, moderate food insecurity is a major issue even in high-income countries.
In the U.S. over 30 million individuals, included in that over 10 million children, experience food insecurity at any given point. It is estimated that an additional 9.9 million people have become food insecure in the U.S. due to the COVID-19 pandemic (Hake et al., 2020). Especially, mothers or caretakers that typically play the primary role in managing food budget and household supply are more affected by food insecurity. Subsequently, food insecure mothers are more likely to experience high levels of stress, anxiety, and sleep disorders, which in turn has shown to affect parenting and feeding practices (Bronte-Tinkew et al., 2007; Gross et al., 2018).
Breastfeeding can ensure optimal nutrition and can protect infants from the negative effects of household food insecurity, but it is not yet clearly understood how food insecurity is associated with breastfeeding behaviors. In a qualitative study, Frank (2015a) found that food insecurity through increased stress, financial and housing issues led to early termination of breastfeeding. It has also been found that due to low-quality diet and feelings that their breast milk will be of poor quality and not an ideal food for their babies, food insecure mothers are less likely to breastfeed their infants (Gross et al., 2019). Even in low-income countries, food insecurity is shown to affect self-efficacy among mothers lowering their confidence in breastfeeding and the ability to nourish their infants. For instance, in a study in Haiti, researchers found that extremely food insecure women used exclusive breastfeeding as a last resort when there was not an alternate food source. Often, food insecure women perceived they were not producing enough milk and preferred to switch to formula and other feeding alternatives (Lesorogol et al., 2018). Considering breastfeeding can provide a secure source of high-quality food at no cost, as well as optimal nutrition and healthy start for low-income infants, understanding the role of food insecurity in breastfeeding has become a significant topic of interest. A convened joint working group of HHS and the USDA highlighted the need for studies addressing the impact of food insecurity on infant dietary intake, including breastfeeding (Raiten et al., 2014). Gaining a greater understanding of how food insecurity impacts breastfeeding is important for developing more specific recommendations and enhancing the breastfeeding rates in the U.S. There is very limited literature on breastfeeding behaviors among low-income, minority women, a group which is highly vulnerable to food insecurity.
Hence, we conducted a cross-sectional study to: (1) examine breastfeeding initiation and continuation rates, and; (2) investigate association between food insecurity and breastfeeding status, among low-income mothers. We also examined breastfeeding self-efficacy and to what extent it differed by breastfeeding status.
Materials and methods
The study we are presenting is part of a longitudinal project involving multiple interviews with mothers when their infants are 2, 4, 6, 9, and 12 months of age. In this paper, we are presenting the results of the first interview i.e. at 2 months of infant’s age. We conducted this study at a pediatric clinic under the approval of the Institutional Reviews Boards of the University of North Carolina-Greensboro and the partnering pediatric clinic. The target population of our study was low-income mothers and their infants. No household income criterion was set as such, since 85% of the clinic’s clients were Medicaid recipients representing household income at or below 133% of the federal poverty line. Mothers of infants were recruited from the pediatric clinic if they met the following selection criteria: (1) the mother is ≥18 years old, (2) she is the birth mother and main caretaker of the infant, (3) able to speak either English or Spanish, (4) the infant is singleton and (5) was at least 37 weeks’ gestation. Lastly, only infants with no major health issues or diet restrictions were eligible for the study. Mothers were recruited from the waiting area of the clinic at the time of their infant’s routine post-partum 15-day, 1-month, or 2-month appointments. During this waiting time, research staff introduced themselves and provided details about the study to mothers. Upon interest and meeting the eligibility criteria, mothers were asked to fill out and sign the consent forms to participate in the interviews. Prior to the COVID-19 epidemic, the 2-month interviews were conducted face-to-face in a private office at the pediatric clinic. Majority of the in-person interviews were conducted before or after the appointment, except some mothers (5%) came in outside of their clinic appointments for the interview due to factors such as time constraints and transportation.
In response to the start of the COVID-19 epidemic in March 2020, oral consent was sought, and all interviews were conducted over the phone. Of the total 93 interviews, 67 were conducted in-person between August 2019 and March 2020, while the remaining 26 were conducted over the phone between March and May 2020. Upon completion of an approximately 30-minute interview, mothers received a grocery store gift card (physical or electronic) as an incentive. The research team consisted of both English and Spanish-speaking graduate and undergraduate research assistants who received hands-on training in interviewing techniques through role-playing, reviewing and pilot testing of the survey instrument.
Measures
The interview questionnaire included the following five main sections: (1) Socio-demographics; (2) Household food security status; (3) Breastfeeding and other feeding practices; (4) Breastfeeding self-efficacy; and, (5) Mother’s BMI.
Socio-demographics: Under this section information such as mother’s age, household size, monthly income, ethnicity, and participation in the food assistance programs was collected.
Household food security: Food security was measured using the USDA’s 10 item Adult Household Food Security Survey Module. This survey inquiries about food affordability and if situations related to food shortage were occurring among adults in the household. This scale is used in reference to a specific time period and this study used a time reference of 30 days.
Breastfeeding and other feeding practices: Under this section, questions were asked to inquire about the initiation and current status of breastfeeding. If the mother was breastfeeding, questions were asked to assess intensity i.e., exclusive, or partial breastfeeding.
Breastfeeding self-efficacy: To measure this, a 14-item Breastfeeding Self-Efficacy Scale-Short Form (BSES-SF) validated in both English and Spanish was used. Each of the 14 items are rated on a 5-point Likert scale, with responses ranging from not at all confident (1) to very confident (5). Total scores range from 14 to 70, with higher scores representing higher levels of self-efficacy for breastfeeding.
Mother’s Body Mass Index: Prior to COVID-19 (i.e., prior to March 2020), mothers’ height and weight were measured at the end of the in-person interview using standardized anthropometric procedures described in the WIC training manual (USDA, 2010). Bodyweight was measured using a digital scale (Tanita BWB-800; accurate to 0.1 kg) and height was measured using a portable stadiometer (SECA 213; accurate to 0.1cm). Both the measurements were recorded in duplicate, and the mean was used to calculate the Body Mass Index (BMI). The research team received training on how to accurately measure the height and weight of an adult women. After March 2020, self-reported height and weight were recorded from the mothers during the phone interviews.
Analyses
All data was collected using REDCap electronic data capture tools hosted at University of North Carolina-Greensboro (Harris et al., 2009, 2019), and were analyzed using SPSS (IBM, version 26), and the “boot” (Canty & Ripley, 2020) and “Resource Selection” (Lele et al., 2019) packages as implemented in R (R Core Team, 2020). Descriptive statistics and frequencies were calculated overall and by current breastfeeding status. Chi-squared and exact tests were used to examine differences in breastfeeding rate by demographic characteristics.
The association between food insecurity and current breastfeeding status after controlling for socio-demographics was tested using a 2-step hierarchical, binary logistic regression i.e. demographic and anthropometric variables were entered in step-1, and food insecurity status was entered in step-2. Ethnicity was broken down into 3 categories: African American (referent), Hispanic, and Non-Hispanic White/Other. Hence, coefficients associated with identification as Hispanic or Non-Hispanic White/Other represent differences in log-odds of breastfeeding compared to identification as African American. The Hosmer-Lemeshow Test was used to assess adequacy of model fit at each step. Changes in classification accuracy from step-1 to step-2 were used to assess the practical impact of the addition of food insecurity to the model.
The extent to which breastfeeding self-efficacy varied by breastfeeding status was tested using Ordinary Least Squares regression. However, self-efficacy scores exhibited severe negative skew in our sample, and inspection of residuals using Q-Q plots further indicated possible violation of the assumption of normality. Therefore, bootstrapping was carried out with 10,000 replications, and bias-corrected 95% confidence intervals were calculated to inform decisions about precision and statistical significance.
Results
Among total 92 participants, the average age was 28 years with an average household size of around 4 and a reported monthly household income of about $2,149 (Table 1). By race/ethnicity 44.7% were African American and 38.3% were Hispanic women, while the remaining 16% were non-Hispanic White or other racial/ethnic groups such as Pacific Islanders. A majority of the participants were receiving WIC (80%) and 42% were participating in the Supplemental Nutrition Assistance Program or SNAP. As shown in Table 1, 52% of the women were single or divorced and about half of them were either GED certified, or had high school or less education. At the time of the two-month interviews, 49% mothers were working either full or part-time. In the case of BMI status, 22.8% were normal weight while the remaining were either overweight or obese.
Table 1.
Socio-demographic characteristics of mother and infant dyads living in Guilford County, nC (n = 92).
| Socio-demographic characteristics | overall | Currently breastfeedingb | not currently breastfeedingc | P |
|---|---|---|---|---|
| mean (SD)a | ||||
| Mothers age (in years) | 28.4 (6.3) | 29.1 (6.4) | 26.5 (5.6) | .057 |
| Household size | 4.6 (1.9) | 4.4 (1.6) | 5.1 (2.5) | .272 |
| Monthly household income ($) | $2,156.27 ($1,351.79) | $2,144.28 ($1,145.07) n (%)a | $2,187.00 ($1,808.27) | .917 |
| Ethnicity | .001 | |||
| african american | 41 (44.6) | 28 (41.8) | 13 (52.0) | |
| non-Hispanic White | 7 (7.6) | 2 (3.0) | 5 (20.0) | |
| Hispanic White | 35 (38.0) | 32 (47.7) | 3 (12.0) | |
| other | 9 (9.8) | 5 (7.5) | 4 (16.0) | |
| Participation in WIC | 80 (84.8) | 56 (83.6) | 22 (88.0) | .697 |
| Participation in SNAP | 39 (41.3) | 23 (34.3) | 15 (60.0) | .047 |
| Marital status | .037 | |||
| Single/Divorced | 48 (52.2) | 30 (44.8) | 18 (72.0) | |
| married/living with partner | 44 (47.8) | 37 (55.2) | 7 (28.0) | |
| Education | .390 | |||
| less than High School diploma | 17 (18.5) | 14 (20.9) | 3 (12.0) | |
| High School/GeD | 37 (40.2) | 27 (40.3) | 10 (40.0) | |
| Some College | 16 (17.4) | 9 (13.4) | 7 (28.0) | |
| Undergraduate or Graduate degree | 22 (23.9) | 17 (25.4) | 5 (20.0) | |
| Employment status | .059 | |||
| employed full/part time/self | 32 (34.8) | 19 (28.4) | 12 (48.0) | |
| Unemployed | 14 (15.2) | 8 (11.9) | 6 (24.0) | |
| Stay home/not looking for a job | 48 (52.2) | 40 (59.7) | 7 (28.0) | |
| Parity | .981 | |||
| Primiparous | 40 (44.0) | 30 (44.8) | 10 (41.7) | |
| multiparous | 51 (56.0) | 37 (55.2) | 14 (58.3) | |
| BMI status | .218 | |||
| normal | 21 (22.8) | 18 (26.9) | 3 (12) | |
| overweight/obese | 71 (77.1) | 49 (73.1) | 22 (88.0) |
numbers were rounded to one decimal point.
Breastfeeding at 2 months of infant’s age; either exclusive or mixed.
Did not initiate or discontinued exclusive or any breastfeeding at 2 months of infant’s age.
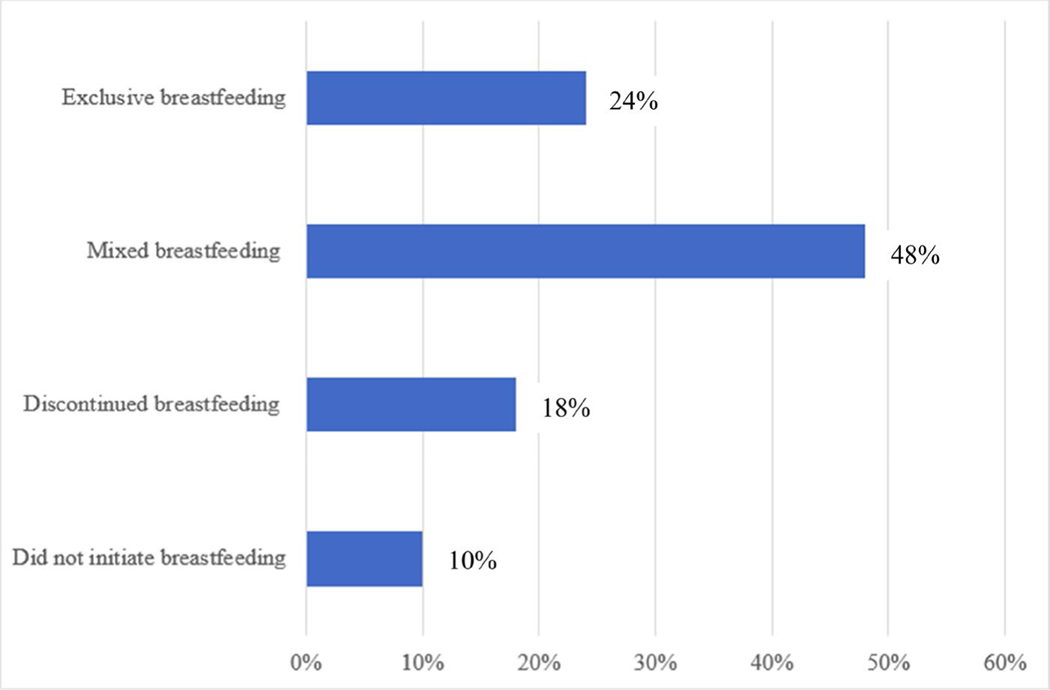
As shown in Figure 1, 10% of the participants did not initiate any breastfeeding and 18% had discontinued breastfeeding at 2 months of infant’s age. Among the remaining participants 48% implemented mixed feeding methods, while only 24% were doing exclusive breastfeeding when their infants were 2 months old. In comparing socio-demographic characteristics by breastfeeding status, as shown in Table 1, older women were more likely to breastfeed (any or exclusive) at 2-month of infant’s age (p < .00). Additionally, breastfeeding rates were highest among Hispanics and also significantly more common among multiparous women than their counterparts. A difference in breastfeeding was also seen by BMI, with significantly lower percentage of overweight/obese women breastfeeding when infants were about 2 months old (p = 0.218). A significant difference was also seen by participation in SNAP, with significantly lower breastfeeding was seen among those who were receiving SNAP than those who were not (p = 0.047). In estimating prevalence of food insecurity, it was found that 15.1% of the participants were experiencing some level of food insecurity. By severity, 10.8% were experiencing moderate level and the remaining 4.3% of food insecure women reported experiencing severe level of food insecurity representing disrupted eating pattern and hunger. In estimating the bivariate relationship, food insecurity was not significantly associated with discontinuation of breastfeeding at 2 months. However, in a 2-step hierarchical, binary logistic regression model, it was found that food insecurity was significantly associated with a lower likelihood of breastfeeding at 2 months of infant’s age (β = −1.51, p = .024) after accounting for other sociodemographic variables. Further, as shown in Table 2, participants identifying as Hispanic were more likely to breastfeed their baby at 2-months compared to African Americans (β = 2.22, p = .027). Regardless of ethnic identification, mothers who were married or living with a partner (β = 1.72, p = .036) and though marginally significant, mothers with normal BMI (β = 1.79, p = .057), were also more likely to breastfeed at 2-months. The results from step 1 suggested that there was essentially no association between household income and breastfeeding within this sample (β = 0.13e − 3, p = .587); therefore, this variable was dropped, and the step 1 model was re-estimated. In testing, model fit at steps 1 and 2 revealed no evidence of misfit (p > .05).
Figure 1.
Description of breastfeeding initiation and intensity rate at 2 months of infants age among low-income mothers (n = 92)
Table 2.
examination of the role of food insecurity in predicting breastfeeding status at 2 months of infant’s age after controlling for key sociodemographic variables (n = 92)a.
| Characteristics | Step 1 |
Step 2 |
||||
|---|---|---|---|---|---|---|
| β (SE) | p | OR | β (SE) | p | OR | |
| Constant | −0.14 (0.59) | .819 | 0.873 | 0.20 (0.62) | .754 | 1.216 |
| mother’s age (in years) | 0.09 (0.05) | .095 | 1.096 | 0.10 (0.06) | .077 | 1.109 |
| total household size (adults & children) | −0.28 (0.17) | .085 | 0.753 | −0.31 (0.17) | .069 | 0.731 |
| BmI | 1.77 (0.96) | .065 | 5.881 | 1.79 (0.94) | .057 | 5.975 |
| ethnicity—Hispanic | 1.63 (0.92) | .076 | 5.101 | 2.22 (1.00) | .027 | 9.162 |
| ethnicity—White/other | −1.75 (0.86) | .043 | 0.175 | −1.74 (0.87) | .047 | 0.176 |
| married/living with Partner | 1.43 (0.77) | .064 | 4.179 | 1.72 (0.82) | .036 | 5.604 |
| education | −0.19 (0.60) | .749 | 0.826 | −0.31 (0.63) | .619 | 0.732 |
| Parity | 1.04 (0.67) | .120 | 2.833 | 1.33 (0.70) | .058 | 3.777 |
| food in/security | – | −1.51 (0.67) | .024 | 0.220 | ||
2-step hierarchical binary logistic regression test; mother’s age, monthly household income and household size were continuous variables. BmI or Body Mass Index—overweight/obese BmI (0) vs. Normal weight (1); Ethnicity: African American (referent group), non-Hispanic White and other groups were merged; Marital Status: Single/Divorced (0) vs. married/living with partner; Education: High-School or less education (0) vs. more than high school (1); Parity: Multiparous (0) vs. Nulliparous (1); Food security: (full, 0) vs. mild, moderate or severe insecurity, (1); OR = odds ratio.
In analyzing breastfeeding self-efficacy and to what extent it varies by breastfeeding status, we found that breastfeeding self-efficacy ranged from minimum 18 to a maximum possible score of 70 (Mean = 58.16, SD = 14.27). As expected, breastfeeding self-efficacy was significantly higher among those who were breastfeeding compared to those who discontinued before infant was 2 months of age or did not initiate any breastfeeding (F(1, 86) = 91.51, p < .001). Mothers who initiated but discontinued breastfeeding were asked an open-ended question on the main reason for their discontinuation. In reviewing the responses, majority of the mothers (70%) reported difficulty producing enough milk or felt that it was not enough for the baby.
Discussion and conclusion
Despite strong evidence and efforts put in to promoting breastfeeding there is still a major gap in its practice, especially among low-income mothers. In our study, we found that 90% of women initiated breastfeeding, which is comparable to the national average of about 85% (Breastfeeding Report Card, 2020). In the recent nationally representative study of NHANES, the breastfeeding rate estimated was 75%, however, a significantly lower rate was found among African Americans (Orozco et al., 2020). This racial/ethnic disparity was also found in our analysis, with African American mothers about 2 times less likely to breastfeed at 2 months of infant’s age. In the review of the racial/ethnic disparities in breastfeeding, Herrick et al. (2016) concluded that there is an overall improvement in breastfeeding rates among African American women, but still a significant gap remains in breastfeeding continuation rate. This disparity highlights the importance of reducing breastfeeding barriers among African American mothers. In our review of studies on barriers and facilitators of breastfeeding, we found that African American women experience several barriers, including historical, social and structural barriers. Specifically, we found that African American women are more likely to experience mistreatment and bias from providers and receive contradictory information about breastfeeding (Kaufman et al., 2010; Evans et al., 2011). Further, researchers have reported that compared to White women, African American women are less likely to receive breastfeeding advice and support from a food assistance programs, such as WIC (Beal et al., 2003). In the WIC based study, Gross et al. found that weekly breastfeeding peer counseling through 16-weeks postpartum alone or along with breastfeeding promotion videos and educational materials was helpful in promoting continuation of breastfeeding among African American mothers (Gross et al., 1998).
Though marginally significant, we found in the multivariate model that mothers’ having a BMI defined as overweight and obese was a risk factor for not breastfeeding. Amir and Donath (2007) have also found that women with an overweight and obese BMI are about 2 times less likely to breastfeeding at 6 months compared with women with a normal BMI. In examining why mothers with an overweight and obese BMI are less likely to breastfeed, the review by Thompson et al. (2012) highlights that psychosocial issue of poor self-image, lack of comfort and societal stigma associated with maternal obesity play a larger role than any physiological issue.
Importantly, we found that food insecurity works against breastfeeding. This is worrisome, because food insecure mothers generally operate on limited household budget, and breastfeeding can ensure full security and optimal nutrition for their infants. In an in-depth qualitative study involving 20 low-income mothers, the researcher found that mothers recognized the benefits of breastfeeding and the high cost of formula was often a driving factor for initiation of breastfeeding. However, the perception of being unable to produce enough milk or worrying that their milk was not of good quality were the most prominent reasons for discontinuing breastfeeding (Frank, 2015b).
In comparing our results with other studies, Orr et al. (2018) in an epidemiological study involving 10,450 women also found that early discontinuation of breastfeeding was common among food insecure compared to secure women. Dinour et al. (2020) also found that significant drop out in breastfeeding occurred for food insecure mothers around 4 to 6 weeks postpartum. By specifically focusing on low-income and mainly minority women, we add to the current literature confirming food insecurity is a risk factor in providing a healthy start to infants by negatively affecting breastfeeding.
Based on the results of this study, we add to the evidence that the negative relationship exists between food insecurity and continuation of breastfeeding. Moving forward a tailored breastfeeding intervention is warranted to promote breastfeeding and a healthier start for infants living in low-income households. Further, an in-depth study to explore the mechanism in which stress due to food insecurity mediates discontinuation of breastfeeding would provide more insight in how to best address this disparity. Since, even at an international level, breastfeeding is critical in achieving Sustainable Development Goals set by the United Nations. For instance, breastfeeding is a vital in achieving Goal # 2 and Goal # 3—which are focused on ending hunger, improving nutrition and promoting health and wellbeing (Pérez-Escamilla, 2017). In a joint message, the WHO and UNICEF also noted that breastfeeding, by supporting physical and cognitive development, can also help in achieving Goal # 4 targeting inclusive education and lifelong learning (Lake & Chan, 2016).
Our study has several limitations. Midway through the study there was a change in the interview method due to the COVID-19 pandemic. The interview was originally conducted face-to-face with a research member measuring participants height and weight, but the last one-third of interviews were conducted over the phone with self-reported height and weight. Also, due to the COVID-19, there was an increase in food insecurity which might have further affected our results. Our study represents a small sample size and nonrandom recruitment of mothers from one pediatric clinic; thus, the study results might not be fully representative of the general population. However, our preliminary study does add to the current limited literature examining breastfeeding behaviors specifically among low-income and racial/ethnic diverse women.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Amir LH, & Donath S. (2007). A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy and Childbirth, 7(1). 10.1186/1471-2393-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beal AC, Kuhlthau K, & Perrin JM (2003). Breastfeeding advice given to African American and white women by physicians and WIC counselors. Public Health Reports, 118(4), 368–376. 10.1016/S0033-3549(04)50264-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breastfeeding (Policy Statement). (2020). AAFP Home. https://www.aafp.org/about/policies/all/breastfeeding-policy-statement.html
- Breastfeeding Report Card. (2020, September 17). Retrieved September 9, 2020, from https://www.cdc.gov/breastfeeding/data/reportcard.htm [Google Scholar]
- Breastfeeding: A smart investment. UNICEF. (2017, July 27). https://sites.unicef.org/breastfeeding/ [Google Scholar]
- Bronte-Tinkew J, Zaslow M, Capps R, Horowitz A, & Mcnamara M. (2007). Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. The Journal of Nutrition, 137(9), 2160–2165. 10.1093/jn/137.9.2160 [DOI] [PubMed] [Google Scholar]
- Canty A, & Ripley BD (2020). boot: Bootstrap R (S-plus) functions. R Package Version, 1, 3–25. [Google Scholar]
- Dieterich CM, Felice JP, O’Sullivan E, & Rasmussen KM (2012, November 12). Breastfeeding and health outcomes for the mother-infant dyad.https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/23178059/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinour LM, Rodas EIR, Amutah-Onukagha NN, & Doamekpor LA (2020). The role of prenatal food insecurity on breastfeeding behaviors: Findings from the United States pregnancy risk assessment monitoring system. International Breastfeeding Journal, 15(1). 10.1186/s13006-020-00276-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans K, Labbok M, & Abrahams SW (2011). WIC and breastfeeding support services: Does the mix of services offered vary with race and ethnicity? Breastfeeding Medicine, 6(6), 401–406. 10.1089/bfm.2010.0086 [DOI] [PubMed] [Google Scholar]
- Frank L. (2015a). Exploring infant feeding pratices in food insecure households: What is the real issue? Food and Foodways, 23(3), 186–209. 10.1080/07409710.2015.1066223 [DOI] [Google Scholar]
- Frank L. (2015b). The breastfeeding paradox. Food, Culture & Society, 18(1), 107–129. 10.2752/175174415X14101814953927 [DOI] [Google Scholar]
- Gross RS, Mendelsohn AL, & Messito MJ (2018). Additive effects of household food insecurity during pregnancy and infancy on maternal infant feeding styles and practices. Appetite, 130, 20–28. 10.1016/j.appet.2018.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross RS, Mendelsohn AL, Arana MM, & Messito MJ (2019). Food insecurity during pregnancy and breastfeeding by low-income Hispanic mothers. Pediatrics, 143(6), e20184113. 10.1542/peds.2018-4113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross SM, Caulfield LE, Bentley ME, Bronner Y, Kessler L, Jensen J, & Paige DM (1998). Counseling and motivational videotapes increase duration of breast-feeding in African-American WIC participants who initiate breast-feeding. Journal of the American Dietetic Association, 98(2), 143–148. 10.1016/S0002-8223(98)00037-6 [DOI] [PubMed] [Google Scholar]
- Hake M, Dewey A, Englehard E, Strayer M, Harper TJ, Summerfelt T, … Gunderson C. (2020, October 30). The impact of coronavirus on food insecurity. Feeding America https://www.feedingamerica.org/research/coronavirus-hunger-research [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, & Duda SN (2019, May 9). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. 10.106/j.jbi.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick K, Rossen L, Kit B, Wang C, & Ogden C. (2016, August 1). Trends in breastfeeding initiation and duration by birth weight among US children, 1999–2012. Retrieved September 30, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6400210/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman L, Deenadayalan S, & Karpati A. (2010). Breastfeeding ambivalence among low-income African American and Puerto Rican women in north and central Brooklyn. Maternal and Child Health Journal, 14(5), 696–704. 10.1007/s10995-009-0499-519644744 [DOI] [PubMed] [Google Scholar]
- Lake A, & Chan M. (2016). Breastfeeding: A key to sustainable development UNICEF and WHO joint message for World Breastfeeding Week 2016. World Breastfeeding Week. https://worldbreastfeedingweek.org/2016/ [Google Scholar]
- Lele SR, Keim JL, & Solymos P. (2019, July 22). ResourceSelection: Resource selection (probability) functions for use-availability data. R package version 0.3–5. https://CRAN.R-project.org/package=ResourceSelection [Google Scholar]
- Lesorogol C, Bond C, Dulience SJ, & Iannotti L. (2018). Economic determinants of breastfeeding in Haiti: The effects of poverty, food insecurity, and employment on exclusive breastfeeding in an urban population. Maternal & Child Nutrition, 14(2), e12524. 10.1111/mcn.12524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meedya S, Fahy K, & Kable A. (2010). Factors that positively influence breastfeeding duration to 6 months: A literature review. Women and Birth, 23(4), 135–145. 10.1016/j.wombi.2010.02.002 [DOI] [PubMed] [Google Scholar]
- Orozco J, Echeverria SE, Armah SM, & Dharod JM (2020). Household food insecurity, breastfeeding, and related feeding practices in US infants and toddlers: Results from NHANES 2009–2014. Journal of Nutrition Education and Behavior, 52(6), 588–594. 10.1016/j.jneb.2020.02.011 [DOI] [PubMed] [Google Scholar]
- Orr SK, Dachner N, Frank L, & Tarasuk V. (2018). Relation between household food insecurity and breastfeeding in Canada. Canadian Medical Association Journal, 190(11), E312–E319. 10.1503/cmaj.170880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Escamilla R. (2017). Food security and the 2015–2030 sustainable development goals: From human to planetary health: Perspectives and opinions. Current Developments in Nutrition, 1(7), e000513. 10.3945/cdn.117.000513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing. Austria. https://www.R-project.org/ [Google Scholar]
- Raiten DJ, Raghavan R, Porter A, Obbagy JE, & Spahn JM (2014). Executive summary: Evaluating the evidence base to support the inclusion of infants and children from birth to 24 mo of age in the dietary guidelines for Americans—“the B-24 Project”. The American Journal of Clinical Nutrition, 99(3), 663S–691S. 10.3945/ajcn.113.072140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson LA, Zhang S, Black E, Das R, Ryngaert M, Sullivan S, & Roth J. (2012). The association of maternal pre-pregnancy body mass index with breastfeeding initiation. Maternal and Child Health Journal, 17(10), 1842–1851. 10.1007/s10995-012-1204-7 [DOI] [PubMed] [Google Scholar]
- USDA. (2010, June). Anthropometric training manual for division of women, infants, and children. WicWorks Resource System. https://wicworks.fns.usda.gov/training [Google Scholar]
- What are the recommendations for breastfeeding? (2017, January 31). Retrieved September 12, 2020, from https://www.nichd.nih.gov/health/topics/breastfeeding/conditioninfo/recommendations [Google Scholar]