Abstract
Background
Digital health solutions hold the potential for supporting general practitioners in decision-making, and include telemedicine systems, decision support systems, patient apps, wearables, fitness trackers, etc.
Aim
This review aimed to identify digital solutions developed for, tested, or implemented in general practice to support the decisions of GPs in disease detection and management, using Denmark as an example country of a universal healthcare setting.
Methods
This study was conducted as a rapid review. The primary search included a database search conducted in Embase and MEDLINE. The supplementary search was conducted in Infomedia and additionally included a snowball search in reference lists and citations of key articles identified in the database search. Titles were screened by two reviewers.
Results
The review included 15 studies as key articles describing a total of 13 digital solutions for decision support in general practice in Denmark. 1.123 titles were identified through the database search and 240 titles were identified through the supplementary and snowball search.
Conclusions
The review identified 13 digital solutions for decision support in general practice in a Danish healthcare setting aimed at detection and/or management of cancer, COPD, type 2 diabetes, depression, liver disease or multiple lifestyle-related diseases. Implementation aspects should be reported more transparently in future publications to enable applicability of digital solutions as decision support to aid general practitioners in disease detection and management.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-023-02234-y.
Keywords: Digital solutions, Digital health, Decision support, Decision aid, General practice, Primary care
Introduction
Digital health interventions provide new approaches for utilizing health data in the prevention, diagnosis, and management of diseases [1]. Digital health covers a wide range of digital solutions such as telemedicine systems, decision support systems, patient apps, wearables and fitness trackers, etc. [2]. Digital health interventions can support healthcare providers in disease detection and prevention by providing prompts or alerts for patients at high risk of disease.
In this review, Denmark is used as an example country with universal healthcare coverage, as all citizens have access to needed medical services, which are primarily tax-funded [3]. Danish citizens have free access to a general practitioner (GP), who acts as a gatekeeper for referrals to specialist or hospital care [4], and 96% of Danes have contact with their GP over a three-year period [5]. Access to care in the secondary healthcare sector is also free, providing that the patient received a referral from their GP, ands GPs are therefore usually the first point-of-contact to the healthcare system [4]. GPs are self-employed, and general practices are funded through contracts with public authorities [4]. Practices are usually fairly small, consisting of 2–3 GPs plus nurses and secretaries, serving 1500–1800 patients per GP [4, 6].
Danish general practices are overall fully digitized, with patient records and clinical data communication between general practice, hospitals, and pharmacies fully computerized [4]. Further, digital consultations are available in general practice [4], and Denmark tops the list in an OECD comparison of European countries in eHealth adoptions [7], which overall suggests that the Danish general practice setting is quite mature in terms of digitization. The gatekeeper role that GPs occupy in the Danish healthcare system makes general practice eligible for implementation of digital health interventions to improve the early detection of patients at risk of diseases in a Danish context [4].
Digital solutions can be implemented into GP software systems as decision support systems to alert GPs of patients at high risk of disease, and aid GP decisions for referrals to diagnostic procedures or treatment initiation at specialists/the hospital. To our knowledge, there is at present no available record of digital decision support systems in general practice in Denmark. Therefore, this rapid review aimed to identify digital solutions developed for, tested, or implemented in general practice to support the decisions of GPs in disease detection and management, using Denmark as an example country of a universal healthcare setting with a fully digitized general practice sector [4, 7]. Findings from this review may be relevant to other countries with similar digitized universal healthcare systems.
Methods
This study was conducted as a rapid review, and reported according to PRISMA guidelines where applicable [8]. The PRISMA checklist was provided in supplementary material 1.
Data sources
The databases Embase, MEDLINE, and Infomedia were included as data sources.
Search strategy
The search was divided into a database search and a supplementary search. The database search was performed in Embase and MEDLINE using a Boolean search strategy. The strategy consisted of three blocks: Denmark (block 1) AND General practice (block 2) AND Digital solutions for decision support (block 3). Each block consisted of keywords that were combined with the operator OR. The block search was conducted using the operator AND between the blocks. Keywords for blocks 1 and 2 were chosen after consultation with a research librarian from the library of the University of Southern Denmark. Further, keywords for block 3 were chosen from validated health app filters [9] and adapted to the current search strategy in collaboration with the research librarian. The search strategies are available in supplementary material 2.
The supplementary search was performed in Infomedia with Danish sources including the Danish Medical Journal and Dagens Medicin. The motivation for the supplementary search was to leave the search strategy open to sources that were not necessarily peer reviewed, but could still describe digital solutions relevant to the aim of this review. Infomedia was searched using the following keywords: digitale løsninger (digital solutions). Grey literature was included in the supplementary search to ensure a broad perspective on the field.
The supplementary search also included a snowball search examining reference lists and citation searches of relevant key articles.
Publication dates were limited to 2010–2022 and searches were limited to English or Danish language.
This review differentiates terminologically between studies and articles throughout the presentation of findings. Studies were defined as peer-reviewed scientific studies identified through the database search. Articles were defined as sources identified in the supplementary search which included grey literature such as news articles etc.
Defining decision support
This review defines decision support or aid for GPs as the dissemination of patients’ healthcare information to GPs to provide an information base in consultations and patient care, or as the automatic identification of patients at risk of disease. This could, for example, be a digital tool that alerts GPs of high-risk patients, thus informing GP decision-making and possibly enhancing diagnostic accuracy in general practice. To clarify the definition, this review defines digital solutions for decision support as material/tools made available to the GP through electronic software systems and not as analogue material (e.g. on-paper tools).
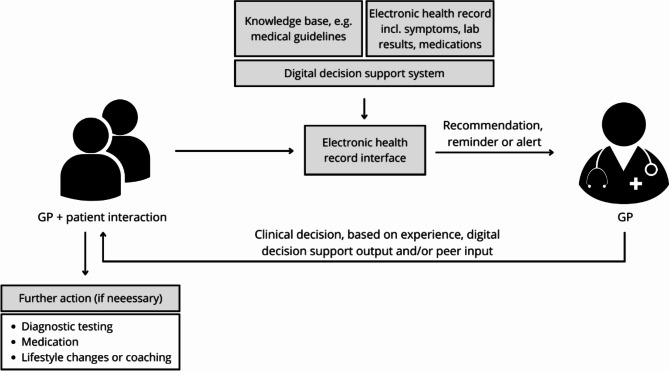
Figure 1 below depicts how digital decision support could be used in a Danish GP setting. Depicted is the setting of a consultation between a GP and a patient. The basis of any care decision is clinical experience, medical guidelines, symptoms, lab results, medication information etc. Digital decision support contributes to the GP’s decision-making by generating a reminder, recommendation, alert etc. which the GP may consider in combination with other clinical information in deciding upon any further action for the patient. The decision rests ultimately with the GP.
Fig. 1.
Example of a digital decision support system in a Danish GP setting
Inclusion and exclusion criteria
The inclusion criteria were as follows:
Digital solution e.g. pop-up, app, etc.
Decision support or aid for GPs.
Danish setting.
General practice setting.
Published after 2010.
Peer reviewed (Only applied to database search).
The exclusion criteria were as follows:
Foreign setting (non-Danish).
Published before 2010.
Not peer-reviewed (Only applied to database search, grey literature was included in the supplementary search).
Hospital setting or other non-GP settings (e.g. municipal health centers).
If the inclusion or exclusion criteria could not be assessed on abstract alone publications were included for full-text screening.
Risk-of-bias assessment
As this rapid review did not aim to evaluate intervention effects, but only to identify digital solutions developed for or implemented in a Danish general practice setting, a risk-of-bias assessment was deemed unnecessary [10].
Screening process
Two reviewers, Anne Clausen (AC) and Emilie Rosenfeldt Christensen (ERC) dual-screened 20% of titles and abstracts of studies identified through the database search, with conflict resolution. One reviewer (AC) screened the remaining abstracts and the second reviewer (ERC) screened all excluded abstracts and resolved any conflicts if needed [11]. All articles from the supplementary Infomedia search were dual-screened. The snowball search was conducted independently by both reviewers and findings were discussed until an agreement was reached.
3. Results
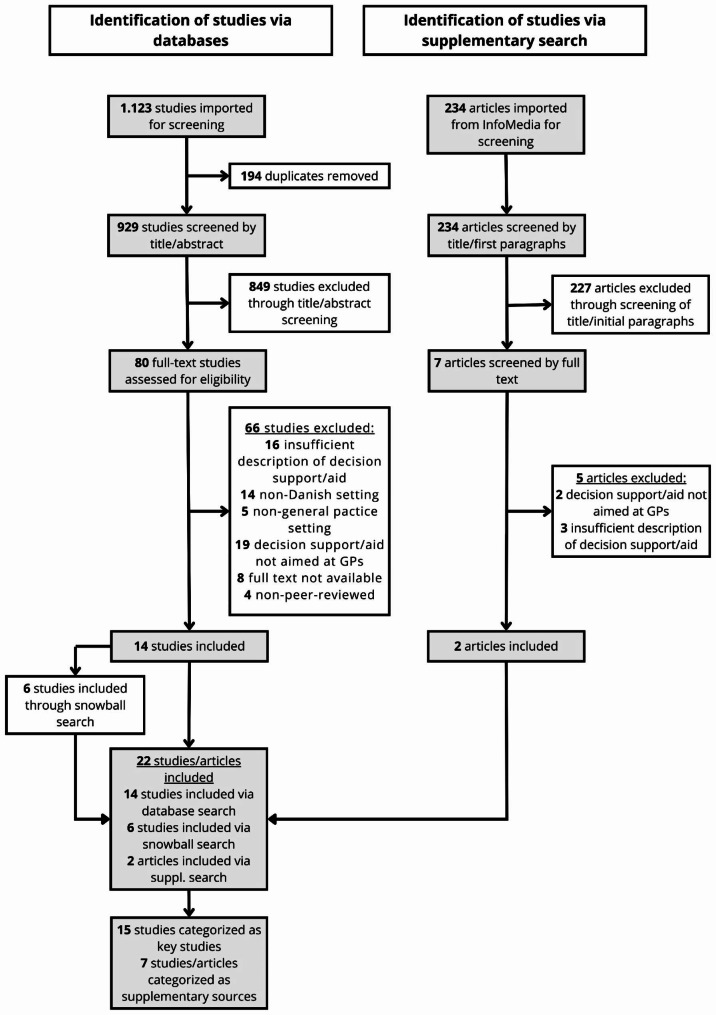
The flow of the screening process is shown in Fig. 2 and described in detail in the following.
Fig. 2.
Flow diagram of the screening process
A total of 1.123 studies were identified through the database search. After removing 194 duplicates, 929 studies were screened on title and abstract. Through the title and abstract screening, 849 studies were excluded based on the criteria outlined above. If the inclusion and exclusion criteria could not be assessed through the title or abstract alone the study was included for full-text screening for further investigation. A total of 80 studies were screened by full text, of which 66 were excluded based on the following: insufficient description of decision support/aid (n = 16), non-Danish setting (n = 14), non-general practice setting (n = 5), decision support/aid not aimed at GPs (n = 19), full text not available (n = 8), and non-peer-reviewed (n = 4). The remaining 14 studies were included in the review as key articles.
The supplementary search in Infomedia identified 234 articles, which were screened on title and first paragraphs. After the assessment of the title and first paragraphs, 227 articles were excluded based on the criteria outlined above except for the criteria of peer review as grey literature was permitted for inclusion. The full text was retrieved and screened for 7 articles, of which 5 were excluded for the following reasons: decision support/aid not aimed at GPs (n = 2) and insufficient description of decision support/aid (n = 3). The 2 remaining articles described solutions that had already been identified through the primary database search. These 2 articles were therefore included only as supplementary sources for the description of the identified digital solutions.
Through snowball search 6 studies were included. After assessment in full text, one of these studies was included in the review as a key article as it described a digital solution not identified by the primary database search, while the remaining 5 were included as supplementary sources.
A total of 15 studies [12–26] were included in the review as key studies and 7 studies/articles [27–33] were included as supplementary sources for further description of identified digital solutions. The characteristics of the 15 key studies are outlined in Table 1.
Table 1.
Characteristics of key studies
| Author | Study aim | Study population | Participant groups | Targeted condition(s) | Digital solution component(s) | Study period | Outcome measure(s) |
|---|---|---|---|---|---|---|---|
| Mukai et al. (2012) [12] | To test whether access to existing information can be increased by inserting a hyperlink into electronic test results | n = 300 GPs |
1. Standard communication (n = 100) 2. Standard communication and 1 email (n = 100) 3. Standard communication and 2 emails (n = 100) |
Breast cancer | Hyperlink / information technology | 1 February 2009 to 31 October 2009 | Self-reported use of hyperlink |
| Schroll et al. (2012) [13] | To describe the changes in quality of care in general practice using the program | n = 14.173 patientsa / 196 practices |
1. Patients with two HbA1c measurements (n = 7.988) 2. Patients with two blood pressure measurements (n = 5.805) 3. Patients with two cholesterol measurements (n = 7.123) |
Type 2 Diabetes | Electronic data capture tool and report server | October 2009 to October 2010 | Proportion of diabetes cases classified as either controlled or uncontrolled based on different parameters |
| Smidth et al. (2013) [14] | To test the impact of a model for a Chronic Obstructive Pulmonary Disease (COPD) management program | n = 1.372 patients |
1. Intervention group (n = 458) 2. Control group (n = 376) 3. External control group (n = 538) |
COPD | Patient identification algorithm | November 2008 to November 2010 | Program adherence measured through the use of specific services, as well as the use of out-of-hours services, hospital admissions, etc. |
| Mukai et al. (2013) [15] | To test whether a web-based clinical decision support system affects PSA testing in general practice | n = 348 practices / 740 GPs |
1. Intervention group (n = 114 practices / 247 GPs) 2. Control group (n = 243 practices / 493 GPs) |
Prostate cancer | Clinical decision support system | 1 January 2010 to 30 Jun 2011 | Number of PSA tests (age-standardized) per 1000 men per general practice |
| Kristiansen et al. (2017) [16] | To test the effect of reminders to GPs regarding missed follow-up after abnormal cervical cytology results | n = 152.551 patients |
1. Before group (n = 33.020) 2. Transition group (n = 52.363) 3. After group (n = 60.725) |
Cervical cancer | Electronic reminder system | 1 January 2009 to 30 May 2014 | Proportion of abnormal cervical cytologies without follow-up |
| Christensen et al. (2018) [17] | To examine the unfolding of the TeleCare North program in three different healthcare settings | n = 15 health professionals |
1. Municipal nurses (n = 5) 2. Hospital nurses (n = 2) 3. Lung physicians (n = 2) 4. GPs (n = 6) |
COPD | Telemonitoring system | February 2014 to February 2015 | Qualitative measures based on interviews, observations, and document studies |
| Krog et al. (2018) [18] | To identify barriers and facilitating factors to using the web-based tool | n = 9 GPs / 8 practices | N/A | Depression | Telemedicine intervention | February 2017 to April 2017 | Qualitative measures based on interview responses |
| Winthereik et al. (2018) [19] | To develop and conduct pilot testing of an intervention supporting end-of-life care | Unclearc |
1. CMEd meeting attendants (n = 120 GPs) 2. EDS sign-ups (n = 50 GPs) |
Cancer and COPD | CMEd and clinical decision support system | Spring 2014 |
Questionnaires, interviews, and emails to gage GP experiences Data regarding EDSe use Patient-related outcomes, e.g. number of terminal declarations, prescriptions, and home deaths |
| Mønsted (2019) [20] | To examine challenges related to achieving veracity in development and use of a stratification algorithm | n = 13 patients and 5 GPs | N/A | Multiple lifestyle-related diseasesf | Stratification algorithm | 2016 | Qualitative measures based on interview responses |
| Larsen et al. (2019) [21] | To examine attendance in a targeted preventive program and the characteristics of patients who took up the program | n = 2.661 patients |
1. Patients diagnosed and/or receiving medical treatment for lifestyle-related disease(n = 699) 2. Patients at high risk of lifestyle-related disease - advised to consult GP (n = 582) 3.Patients engaging in risk behavior - advised to schedule phone-based counseling (n = 618) 4.Patients not exhibiting risk behaviors and not receiving medical treatment (n = 762) |
Multiple lifestyle-related diseasesf | Stratification algorithm and personal health profile | April 2016 to December 2016 | Attendance, defined as attending a GP medical examination or telephone-based counselling |
| Broholm-Jørgensen et al. (2020) [22] | To examine preventive health dialogues from both GP and patient perspectives | n = 11 patients 7 GPsg | N/A | Multiple lifestyle-related diseasesf | Stratification algorithm, digital support system, and personal health profile | 2016 | Qualitative measures based on interviews and observations |
| Soerensen et al. (2021) [23] | To develop and validate an AI model to predict 90-day cancer risk based on blood tests | n = 6.592 analytical profilesh |
1. Development cohort (n = 5.224) 2. Validation cohort (n = 1.368) |
Cancer | AI model | 29 November 2011 to 1 March 2020 | Cancer diagnosis within 90 days of blood test |
| Jakobsen et al. (2021) [24] | To describe behavior, test feasibility, and identify important factors in digital lifestyle coaching of patients with type 2 Diabetes | n = 15 health professionals / 4 practices |
1. Practice nurses (n = 6) 2. GPs (n = 9) |
Type 2 Diabetes | Digital lifestyle coaching and treatment | August 2019 to September 2019 | Qualitative measures based on interviews |
| Charles et al. (2022) [25] | To examine whether participation in the program increased the probability of GPs prescribing lipid-lowering medication | n = 9.071 patients and 300 GPs |
1. Patients attending one of the 165 ‘exposed’ GPs (n = 5.135) 2. Patients attending one of the 135 ‘control’ ‘GPs (n = 3.936) |
Type 2 Diabetes | Electronic disease management program | 2011 to 2013 | Odds ratio, describing the odds of receiving a prescription for lipid-lowering medication |
| Blanes-Vidal et al. (2022) [26] | To develop and evaluate AI models capable of predicting significant liver stiffness | n = 3.352 patients |
1. Training, validation, and testing data set (n = 3.017) 2. Hold-out dataset (n = 335) |
Liver disease | AI models | 2013 to 2020 | Area Under the Curve, accuracy, sensitivity, specificity, positive predictive value, and negative predictive value |
a: Patients may be included in multiple participants groups
b: Pilot testing only. Development phase not included
c: The article does not state how many GPs participated in both the CMEd meeting and EDSe system
d: Continued Medical Education
e: Electronic Decision Support
f: Hypertension, Hyperlipidemia, Chronic Obstructive Pulmonary Disease, type 2 Diabetes Mellitus, Cardiovascular disease, and general risk behavior identification
g: Study included 10 observations of preventive health dialogues, 11 interviews with patients, and 7 interviews with GPs. However, it is not stated whether the patients and GPs participating in health dialogues and interviews are the same
h: Blood test profiles, consisting of various laboratory analyses
The 15 key studies described 13 digital solutions for decision support in general practice. The characteristics of the 13 digital solutions are outlined in Table 2. Further elaborations of each digital solution can be found in supplementary material 3.
Table 2.
Digital solution characteristics
| Digital solution | Solution type | Targeted condition(s) | Disease incidence/prevalence in Denmark | Local / national | Purpose | Status |
|---|---|---|---|---|---|---|
| Hyperlink in electronic test communication [12] | Hyperlink / ICTa | Breast cancer | 4.870 incident cases per year (mean from years 2016–2020) [34]. 74.235 prevalent cases at the end of 2019 [34]. | Central Denmark Region | To increase access to existing, patient-oriented information about the disease and its treatment via the web for GPs. | Tested in 148 GP clinics from June to October 2009 |
| Data Capture Module (DCM) for improvement of diabetes care through the National Danish General Practice Database (DAMD) [13] | Pop-ups, diabetes feedback reports on a report server, and access to an online display of data capture | Type 2 diabetes | 252.516 prevalent cases as of 2017, equivalent to 4.8% of the Danish population [35]. Approximately 18.700 incident cases per year [35]. | Nationwide | To provide GPs access to updated data on the quality of care from their own practice, to identify patients that are not optimally treated. | From April 2011 every Danish GP was obliged within two years to participate in the DCM. |
| Disease management program (DMP) for Chronic Obstructive Pulmonary Disease (COPD) [14, 27, 28] | DMP including a patient identification algorithm and clinical decision support system | COPD | Prevalence is estimated to 300.000 to 400.000 patients and approximately 14% among individuals aged 35 years and above [36]. | Ringkoebing-Skjern Municipality, Denmark | To change/improve the management of COPD in general practice. Effect was measured on planned and additional preventive consultations, performed spirometries, and admissions. | RCT conducted from November 2008 to December 2010 |
| Online decision support system for Prostate-Specific Antigen (PSA) tests [15] | Hyperlink in an electronic medical record system | Prostate cancer | 4.542 incident cases per year (mean from years 2016–2020) [37]. 45.610 prevalent cases at the end of 2019 [37]. | Central Denmark Region | To aid GPs in deciding if a patient should have a PSA test done, to guide the interpretation of PSA results, or to guide the pathway in a fast-track diagnostic program. | Tested in 114 practices from January 1st 2010 to June 30th 2011 |
| GP reminders on follow-up of abnormal cervical cytology [16] | Electronic GP reminder | Cervical cancer | 342 incident cases per year (mean from years 2016–2020) [38]. 8.962 prevalent cases at the end of 2019 [38]. | Nationwide | To reduce loss to follow-up in cervical cancer screening | Implemented in 2012 |
| TeleCare North [17, 29] | Telemonitoring patient data made available to GPs through an electronic monitoring database | COPD | Prevalence is estimated to 300.000 to 400.000 patients and approximately 14% among individuals aged 35 years and above [36]. | North Denmark Region | To improve the management of COPD patients by providing GPs with telemonitoring data on oxygen level, blood pressure, pulse, weight, and symptoms to support GP decision-making. | Implemented in 2012–2014 |
| Electronic Major Depression Inventory (eMDI) [18] | Through WebPatient the eMDI score is automatically returned to the GP’s electronic patient record upon filling out from patients | Depression | It is estimated that around 10% of the adult Danish population has depression (estimated on 2013 data) [39]. This is equivalent to around 300.000-375.000 prevalent cases [40]. | Nationwide | To test psychometric testing of potentially depressive patients in general practice through a telemedicine solution | WebPatient and the possibility to order eMDI testing was implemented nationally in 2015 |
| Electronic Decision Support (EDS) to support end-of-life care [19] | The EDS consisted of a pop-up window in the patient’s medical record and a list of patients with end-of-life needs and key elements in their care | Cancer and COPD | COPD prevalence is estimated to 300.000 to 400.000 patients and approximately 14% among individuals aged 35 years and above [36]. | Central Denmark Region | To support end-of-life care in general practice for patients with cancer or COPD | Pilot-tested in the Central Denmark Region in 2014 |
| Early Detection and Prevention (TOF) [20–22, 32, 33] | Patient results from a risk stratification model and a digital data collection tool were made available to GPs through a digital health folder | Multiple lifestyle-related diseases | Not applicable as the definition included a range of lifestyle-related diseases and risk behavior. | Varde and Haderslev municipalities | To develop a health intervention for early detection of citizens at risk of developing lifestyle-related disease and initiation of preventive care | TOF pilot study took place from September 2016 to December 2016 |
| AI to identify patients at risk of cancer [23] | AI risk score to predict cancer within 90 days | Cancer | 45.205 incident cancer cases as of 2020 [41]. 362.715 prevalent cases as of 2020 [41]. | Region of Southern Denmark | The AI risk score could be a useful tool in decision-making and support GP triage. | Developed on data from the period November 29th 2011 to December 31st 2018. Not yet tested or implemented in general practice. |
| Digital individualized coaching and lifestyle treatment intervention of T2D (DICTA) [24, 30, 31] | The intervention comprises, among other elements, an algorithm-based decision support for GPs implemented in the GP software system XMO | Type 2 diabetes | 252.516 prevalent cases as of 2017, equivalent to 4.8% of the Danish population [35]. Approximately 18.700 incident cases per year [35]. | Region of Southern Denmark and Region Zealand | The algorithm-based decision support can support GPs in prescribing the correct medical treatment. |
The intervention was developed with GPs and pilot-tested in general practices in the Region of Southern Denmark in 2019. The intervention is rolled out in a RCT running from January 2021 to end in 2023. |
| Electronic patient data overview with alerts for management of T2D patients [25] | Electronic overview of T2D patients including red flags for patients not receiving treatment as recommended by guidelines. | Type 2 diabetes | 252.516 prevalent cases as of 2017, equivalent to 4.8% of the Danish population [35]. Approximately 18.700 incident cases per year [35]. | Nationwide | To increase GP prescriptions of lipid-lowering drugs in T2D patients. | The overview was available to Danish GPs in the period from 2011 to 2014. |
| AI for identification of liver fibrosis patients (LiverAID models) [26] | AI algorithm to predict liver stiffness. | Liver fibrosis | Approximately 1000 incident cases per year of alcoholic liver cirrhosis and an estimated prevalence of 12–14.000 [42]. For non-alcoholic fatty liver disease, there is an estimated prevalence of around 1.000.000 individuals [43]. | Region of Southern Denmark | The LiverAID models could be used for the early detection of patients with asymptomatic chronic liver diseases in primary care. | The LiverAID models were developed with data from patients recruited in the period 2013 to 2020. Not yet tested or implemented in general practice. |
a: Information and communication technology
Knowledge summary
This rapid review identified 15 key studies (Table 1) describing 13 digital solutions (Table 2) for decision support in general practice in Denmark. The 13 solutions were aimed at the following disease areas: cancer (n = 5), COPD (n = 3), type 2 diabetes (n = 3), depression (n = 1), liver disease (n = 1), and multiple lifestyle-related diseases (n = 1). Of the 13 solutions, 4 were either developed, tested, or implemented on a national scale and 9 in a limited number of regions or municipalities. As this review did not include an investigation of implementation status beyond what was reported in the identified literature, it was overall not possible to evaluate the current implementation status of the digital solutions as of 2022 (Table 2). Over the course of the inclusion period (2010–2022), there was a progression in the digital solutions as they appeared more complex in recent years. The first study from 2012 described a simple hyperlink solution inserting hyperlinks into electronic test communication [12], whereas the latest study from 2022 described an advanced AI model for the identification of liver disease [26].
Study strengths & limitations
A methodological strength of this rapid review is the use of dual screening to avoid the subjective bias of using a single reviewer. This was applied in both the primary database search and the supplementary search including the snowball search. The dual-screening reduces the risk of missing key material as two reviewers independently reviewed search materials. The snowball search is a methodological strength as it provides a broad overview of the subject area through citation and reference list searches thereby possibly uncovering relevant material that was not identified through the database search. Further, a strength is the inclusion of feasibility and development studies to achieve a thorough understanding of the included digital solutions and preserve an open scope toward novel approaches. Lastly, researchers of various backgrounds contributed to the generation of this paper, which improved the quality of the final work.
A limitation of this review could be the applied definition of decision support. The definition is relatively broad which possibly means that solutions categorized as decision support for this review may not be categorized as such by others. A methodological limitation is that included studies did not undergo quality assessment which may result in variations of study design, sample size, and outcome measures making it difficult to summarize findings. However, as this rapid review did not aim to evaluate intervention effects, a quality assessment was deemed unnecessary [10]. Furthermore, it can be discussed if the search in MEDLINE and Embase was sufficient or other databases like PubMed should have been included as well. We do not necessarily believe that this is a methodological limitation to this review as the applied health app filters were developed for and validated in these databases [9], and some search techniques are not supported by PubMed. Additionally, the Cochrane Handbook recommends MEDLINE and Embase as search engines for systematic literature searches [44]. However, we do recognize that there might be a difference of opinions about this topic. Another limitation of this rapid review is that it does not include an investigation, beyond the identified literature, of whether the identified digital solutions were ever fully implemented or are still in use as of 2022.
The potential impact of digital solutions in the healthcare system should be considered. The potential impact will necessarily depend on country setting and the organisational structure of the specific healthcare system. In the Danish example, general practice acts as the gateway to the healthcare system, which means that GPs can refer to patient care at hospitals and specialists. In the Danish GP-setting, digital solutions can aid GPs in decision-making in referral for patient care in other segments of the healthcare system by providing a knowledge base or providing prompts/alerts for individuals at potential risk of disease. On one hand, this potential can favour the argument that a strategic goal of improved early detection of disease is realistically achieved as referrals for patient care e.g. at the hospital or at specialist clinics will be supported by an additional knowledge base. On the other hand, it should be considered whether multiple decision support tools could create an information overload that will hamper successful implementation. When implementing digital solutions in the healthcare system it should therefore be carefully considered what the health priorities are in the specific healthcare setting. Continuing the discussion of the potential impact of digital solutions, it should also be addressed whether these tools may contribute to over- or underdiagnosis. Imprecise tools or solutions which do not consider important factors could result in misleading support to healthcare professionals, leading to incorrect or missed diagnosis [45]. Additionally, overreliance on digital solutions may lead to overdiagnosis, as the tools identify patients which would not otherwise have sought medical attention and who do not require treatment [46]. As such, these potential issues underline the need for these tools to be used only as decision support, in conjunction with the GPs own critical assessment.
Conclusion
In conclusion, this review identified 13 digital solutions for decision support in general practice in a universal healthcare setting in Denmark. The digital solutions covered a range of disease areas (cancer (n = 5), COPD (n = 3), type 2 diabetes (n = 3), depression (n = 1), liver disease (n = 1) and multiple lifestyle-related diseases (n = 1)). Of the 13 solutions, 4 were developed, tested, or implemented on a national scale, and the remaining 9 on a local scale (regional or municipal). The review identified digital solutions with great potential for supporting decision-making in general practice, however, a key learning point is a lack of focus of these studies on how digital solutions are tested, evaluated, and adapted for implementation purposes in general practice. Implementation status could be more transparently reported in publications to enable comparisons across digital solutions and evaluate applicability in general practice. Future studies should consider implementation aspects as part of unfolding the potential of digital solutions as decision support to aid general practitioners in disease detection and management.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
A special thanks to the University of Southern Denmark Library for helping with search strategies.
Abbreviations
- COPD
Chronic Obstructive Pulmonary Disease
- OECD
Organisation for Economic Co-operation and Development
- GP
General Practice
- GPs
General Practitioners
- PSA
Prostate Specific Antigen
- N/A
Not Applicable
- CME
Continued Medical Education
- EDS
Electronic Decision Support
- AI
Artificial Intelligence
- ICT
Information and Communication Technology
- DCM
Data Capture Module
- DMP
Disease Management Programme
- RCT
Randomized Controlled Trial
- eMDI
Electronic Major Depression Inventory
- TOF
Early Detection and Prevention (in Danish:Tidlig Opsporing og Forebyggelse)
- T2D
Type 2 Diabetes
Author contributions
AC, ERC and KHR contributed to the concept.All authors contributed to the design.AC and ERC carried out the literature search and screening.AC and ERC wrote the manuscript and prepared tables and figures.All authors performed critical revision of the manuscript.All authors read and approved the final manuscript.
Funding
This work did not receive any funding.
Open access funding provided by University of Southern Denmark
Data Availability
Search strings are provided in supplementary material to enable reproducibility of literature searches.
Declarations
Ethics approval
Not applicable as the manuscript does not include patient data.
Consent for publication
Not applicable as the manuscript does not include patient data.
JS has participated in scientific advisory boards for Novo Nordic, Roche, Astra-Zeneca, GlaxoSmith Kline Pharma, he is editor for Promedicin.dk and holds grants from EU, the Danish Research council and numerous other funds.
BA reports grants and personal fees from UCB, grants and personal fees from Kyowa-Kirin UK, personal fees from Amgen, grants from Novartis, grants and personal fees from Pharmacosmos, outside the submitted work.
Competing interests
AC, ERC, PRJ and KHR have declared that no competing interests exist.JS has participated in scientific advisory boards for Novo Nordic, Roche, Astra-Zeneca, GlaxoSmith Kline Pharma, he is editor for Promedicin.dk and holds grants from EU, the Danish Research council and numerous other funds.BA reports grants and personal fees from UCB, grants and personal fees from Kyowa-Kirin UK, personal fees from Amgen, grants from Novartis, grants and personal fees from Pharmacosmos, outside the submitted work.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Anne Clausen and Emilie Rosenfeldt Christensen Shared co-first authorship.
References
- 1.WHO guideline Recommendations on Digital Interventions for Health System Strengthening. Geneva: World Health Organization. ; 2019 [22.06.2022]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541905/. [PubMed]
- 2.Classification of Digital Health Interventions v 1.0. Geneva: World Health Organization. ; 2018 [22.06.2022]. Available from: https://apps.who.int/iris/bitstream/handle/10665/260480/WHO-RHR-18.06-eng.pdf?sequence=1&isAllowed=y.
- 3.Pedersen KM, Andersen JS, Søndergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25(Suppl 1):34–8. doi: 10.3122/jabfm.2012.02.110216. [DOI] [PubMed] [Google Scholar]
- 4.Laugesen K, Ludvigsson JF, Schmidt M, Gissler M, Valdimarsdottir UA, Lunde A, et al. Nordic Health Registry-Based Research: a review of Health Care systems and Key registries. Clin Epidemiol. 2021;13:533–54. doi: 10.2147/CLEP.S314959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sundheds- og Ældreministeriet (Ministry of Health and Senior Citizens). Befolkningens kontakter til almen praksis (Population Contacts to General Practice) 2016 [07.11.2023]. [Available from: https://sum.dk/Media/4/9/02-Befokningens-kontakter-til-almen-praksis.pdf.
- 6.Praktiserende Lægers Organisation (General Practitioners’ Organisation). PLO Faktaark 2022 (PLO Fact Sheet 2022) 2023 [07.11.2023]. Available from: https://laeger.dk/media/1e3cuftt/plo_faktaark_2022.pdf.
- 7.OECD . eHealth adoption in general practice and in hospitals. Health at a glance: Europe 2016: state of Health in the EU cycle. Paris: OECD Publishing; 2016. [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayiku L, Hudson T, Glover S, Walsh N, Adams R, Deane J, et al. The NICE MEDLINE and Embase (Ovid) health apps search filters: development of validated filters to retrieve evidence about health apps. Int J Technol Assess Health Care. 2020;37:e16. doi: 10.1017/S026646232000080X. [DOI] [PubMed] [Google Scholar]
- 10.Tricco AC, Langlois EV, Straus SE, Alliance for Health P, Systems R, World Health O. Rapid reviews to strengthen health policy and systems: a practical guide. Geneva: World Health Organization; 2017 2017.
- 11.Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2021;130:13–22. doi: 10.1016/j.jclinepi.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mukai TO, Bro F, Fenger-Grøn M, Olesen F, Vedsted P. Use of hyperlinks in electronic test result communication: a survey study in general practice. BMC Med Inf Decis Mak. 2012;12(1):114. doi: 10.1186/1472-6947-12-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schroll H, Christensen RD, Thomsen JL, Andersen M, Friborg S, Søndergaard J. The Danish model for improvement of Diabetes care in general practice: impact of automated collection and feedback of patient data. Int J Family Med. 2012;2012:208123. doi: 10.1155/2012/208123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smidth M, Christensen MB, Fenger-Grøn M, Olesen F, Vedsted P. The effect of an active implementation of a Disease management programme for Chronic Obstructive Pulmonary Disease on healthcare utilization–a cluster-randomised controlled trial. BMC Health Serv Res. 2013;13:385. doi: 10.1186/1472-6963-13-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mukai TO, Bro F, Olesen F, Vedsted P. To test or not: a registry-based observational study of an online decision support for prostate-specific antigen tests. Int J Med Inform. 2013;82(10):973–9. doi: 10.1016/j.ijmedinf.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 16.Kristiansen BK, Andersen B, Bro F, Svanholm H, Vedsted P. Impact of GP reminders on follow-up of abnormal cervical cytology: a before-after study in Danish general practice. Br J Gen Pract. 2017;67(661):e580–e7. doi: 10.3399/bjgp17X691913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christensen JKB. The Emergence and Unfolding of Telemonitoring Practices in Different Healthcare Organizations. Int J Environ Res Public Health. 2018;15(1). [DOI] [PMC free article] [PubMed]
- 18.Krog MD, Nielsen MG, Le JV, Bro F, Christensen KS, Mygind A. Barriers and facilitators to using a web-based tool for diagnosis and monitoring of patients with depression: a qualitative study among Danish general practitioners. BMC Health Serv Res. 2018;18(1):503. doi: 10.1186/s12913-018-3309-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winthereik AK, Neergaard MA, Jensen AB, Vedsted P. Development, modelling, and pilot testing of a complex intervention to support end-of-life care provided by Danish general practitioners. BMC Fam Pract. 2018;19(1):91. doi: 10.1186/s12875-018-0774-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mønsted T. Achieving veracity: a study of the development and use of an information system for data analysis in preventive healthcare. Health Inf J. 2018;25(3):491–9. doi: 10.1177/1460458218796665. [DOI] [PubMed] [Google Scholar]
- 21.Larsen LB, Sondergaard J, Thomsen JL, Halling A, Sønderlund AL, Christensen JR, et al. Step-wise approach to prevention of chronic Diseases in the Danish primary care sector with the use of a personal digital health profile and targeted follow-up – an assessment of attendance. BMC Public Health. 2019;19(1):1092. doi: 10.1186/s12889-019-7419-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Broholm-Jørgensen M, Langkilde SM, Tjørnhøj-Thomsen T, Pedersen PV. Motivational work’: a qualitative study of preventive health dialogues in general practice. BMC Fam Pract. 2020;21(1):185. doi: 10.1186/s12875-020-01249-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soerensen PD, Christensen H, Gray Worsoe Laursen S, Hardahl C, Brandslund I, Madsen JS. Using artificial intelligence in a primary care setting to identify patients at risk for cancer: a risk prediction model based on routine laboratory tests. Clin Chem Lab Med. 2021. [DOI] [PubMed]
- 24.Jakobsen PR, Christensen JR, Nielsen JB, Søndergaard J, Ejg Jarbøl D, Olsen MH et al. Identification of important factors affecting Use of Digital individualised coaching and treatment of type 2 Diabetes in General Practice: a qualitative feasibility study. Int J Environ Res Public Health. 2021;18(8). [DOI] [PMC free article] [PubMed]
- 25.Charles MH, Thomsen JL, Christensen B, Pulleyblank R, Kongstad LP, Olsen KR. Use of electronic patient data overview with alerts in primary care increases prescribing of lipid-lowering medications in patients with type 2 Diabetes. Diabetologia. 2022;65(2):286–90. doi: 10.1007/s00125-021-05598-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blanes-Vidal V, Lindvig KP, Thiele M, Nadimi ES, Krag A. Artificial intelligence outperforms standard blood-based scores in identifying liver fibrosis patients in primary care. Sci Rep. 2022;12(1):2914. doi: 10.1038/s41598-022-06998-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smidth M, Christensen MB, Olesen F, Vedsted P. Developing an active implementation model for a chronic Disease management program. Int J Integr Care. 2013;13:e020. doi: 10.5334/ijic.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smidth M, Sokolowski I, Kærsvang L, Vedsted P. Developing an algorithm to identify people with Chronic Obstructive Pulmonary Disease (COPD) using administrative data. BMC Med Inf Decis Mak. 2012;12(1):38. doi: 10.1186/1472-6947-12-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jungersen DR. 4500 nordjyske KOL-patienter tilbydes behandling i eget hjem. Ugeskriftetdk. 2012.
- 30.Jakobsen PR. Digital coaching af patienter med type 2-diabetes og klinisk beslutningsstøtte til almen praksis (DICTA). Månedsskrift for almen praksis. 2021.
- 31.Sjøgren K. Digital løsning skal lette praktiserende lægers arbejde med diabetespatienter. Dagens Medicin. 2021.
- 32.Larsen LB, Sonderlund AL, Sondergaard J, Thomsen JL, Halling A, Hvidt NC, et al. Targeted prevention in primary care aimed at lifestyle-related Diseases: a study protocol for a non-randomised pilot study. BMC Fam Pract. 2018;19(1):124. doi: 10.1186/s12875-018-0820-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thilsing T, Sonderlund AL, Sondergaard J, Svensson NH, Christensen JR, Thomsen JL, et al. Changes in Health-Risk Behavior, Body Mass Index, Mental Well-Being, and risk status following participation in a stepwise web-based and Face-to-Face Intervention for Prevention of Lifestyle-Related Diseases: Nonrandomized Follow-Up Cohort Study. JMIR Public Health Surveill. 2020;6(3):e16083. doi: 10.2196/16083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kræftens Bekæmpelse. Statistik om brystkræft 2022 [13.12.2022]. Available from: https://www.cancer.dk/brystkraeft-mammacancer/statistik-brystkraeft/.
- 35.Videnscenter for diabetes. Diabetes i tal 2020 [13.12.2022]. Available from: https://videncenterfordiabetes.dk/viden-om-diabetes/generelt-om-diabetes/diabetes-i-tal.
- 36.Lægehåndbogen. KOL 2021 [13.12.2022]. Available from: https://www.sundhed.dk/sundhedsfaglig/laegehaandbogen/lunger/tilstande-og-sygdomme/obstruktive-lungesygdomme/kol/.
- 37.Kræftens Bekæmpelse. Statistik om prostatakræft 2022 [13.12.2022]. Available from: https://www.cancer.dk/prostatakraeft/statistik-prostatakraeft/.
- 38.Kræftens Bekæmpelse. Statistik om livmoderhalskræft 2022 [13.12.2022]. Available from: https://www.cancer.dk/livmoderhalskraeft-collumcancer/statistik-livmoderhalskraeft/.
- 39.Hvidberg MF, Johnsen SP, Davidsen M, Ehlers L. A Nationwide Study of Prevalence Rates and characteristics of 199 chronic conditions in Denmark. Pharmacoecon Open. 2020;4(2):361–80. doi: 10.1007/s41669-019-0167-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Psykiatrifonden. Depression 2022 [13.12.2022]. Available from: https://psykiatrifonden.dk/diagnoser/depression#toc-udbredelse.
- 41.Kræftens Bekæmpelse. Kræft i Danmark 2022 2022 [13.12.2022]. Available from: https://www.cancer.dk/dyn/resources/File/file/9/9699/1665127828/kraeft-i-danmark-2022-bog-singlepages-3udg.pdf.
- 42.Lægehåndbogen, Leversygdom. alkoholisk 2019 [13.12.2022]. Available from: https://www.sundhed.dk/sundhedsfaglig/laegehaandbogen/mave-tarm/tilstande-og-sygdomme/lever/leversygdom-alkoholisk/.
- 43.Hansen CD, Lindvig KP, Grønbæk H, Gluud LL, Thiele M, Krag A. Management of non-alcoholic fatty Liver Disease. Ugeskr Laeger. 2022;184(42). [PubMed]
- 44.Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I et al. Searching for and selecting studies. Cochrane Handbook for Systematic Reviews of Interventions2019. p. 67–107.
- 45.Graham Kennedy A. Avoiding over- and underdiagnosis. Diagnosis: a Guide for Medical trainees. Oxford University Press; 2021.
- 46.Institute for Quality and Efficiency in Health Care (IQWiG). What is overdiagnosis? InformedHealth.org [Internet]; 2006 [07.11.2023]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430655/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Search strings are provided in supplementary material to enable reproducibility of literature searches.