Key Clinical Message
Extrapulmonary lymphangioleiomyomatosis (LAM) can present as incidental nodal LAM in gynecological surgery specimens, that warrants systemic investigation and follow‐up of concurrent and subsequent development of pulmonary and extrapulmonary LAM.
Keywords: gynecology, lymph nodes, Lymphangioleiomyomatosis, pathology
1. CASE PRESENTATION
65‐year‐old female presented with vaginal bleeding and lower abdominal pain. She underwent total hysterectomy, bilateral salpingo‐oophorectomy, and pelvic lymphadenectomy, and the postoperative diagnosis was determined as uterine endometrioid carcinoma, Grade 2, pT2, pN0, cM0, pStage II, based on the TNM Classification of Malignant Tumors, 8th edition. Although preoperative computed tomography (CT) scan did not reveal clear enlargement of lymph nodes, pathological examination of a dissected common iliac lymph node revealed multiple lesions, maximally 5 mm in size, that consist of bundles of spindle cells and nests of epithelioid cells, with grainy, eosinophilic cytoplasm, ovoid nuclei with small nucleoli (Figure 1A,C). The cells did not reveal atypia, mitotic activity nor necrosis, and morphologically distinct from primary endometrioid carcinoma. Immunohistochemistry showed characteristic D2‐40 (podoplanin) positive lymphatic endothelium lining the bundles of spindle cells and nests of epithelioid cells (Figure 1B,D). α‐smooth muscle actin (α‐SMA), estrogen receptor (ER), and cytoplasmic β‐catenin were diffusely positive, but cytokeratin (AE1/AE3) and CD34 were negative. Taken together, diagnosis of nodal lymphangioleiomyomatosis (LAM) was made. Melanocytic markers such as HMB45 and Melan‐A, which are often positive in LAM, were positive only in a few cells in this case. Postoperative follow‐up systemic investigation did not reveal other suspected LAM lesions including lung.
FIGURE 1.
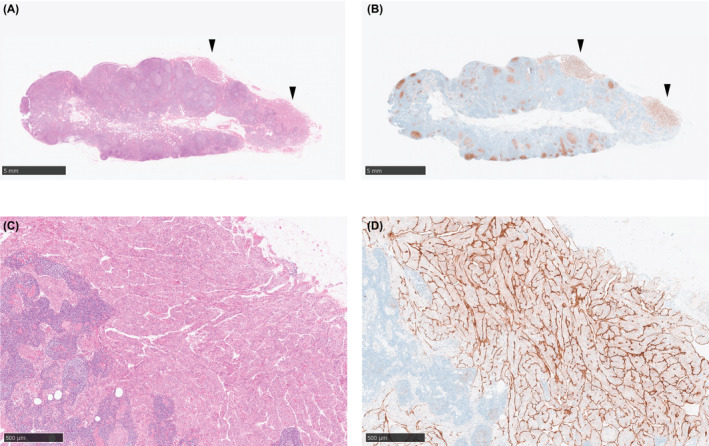
Nodal lymphangioleiomyomatosis (LAM) in a common iliac lymph node. (A, C) Hematoxylin and eosin (HE) staining showed the bundles of spindle cells and nests of epithelioid cells in a common iliac lymph node. (B, D) D2‐40 (podoplanin) expression in the lymphatic endothelium lining the spindle‐cell bundles and epithelioid‐cell nests. (A, B) Loupe images capturing the whole lymph node. Representative LAM lesions are shown with black arrowheads. Scale bar: 5 mm. (C, D) Representative magnified views. Scale bar: 500 μm.
2. DISCUSSION
LAM is a rare systemic disease that affect mostly women of childbearing age, characterized by proliferation of smooth muscle‐like cells (LAM cells). Although LAM often manifests as progressive formation of pulmonary parenchymal cysts, extrapulmonary LAM can involve other organs, including mediastinum, retroperitoneum, uterus, intraperitoneal and/or pelvic lymph nodes, with or without pulmonary involvement. 1
Incidental nodal LAM can be found in 0.46% of the lymph nodes of gynecologic surgical specimens. 2 Cases of incidental nodal LAM with subsequent development of pulmonary LAM have been reported, 2 , 3 including the development of pulmonary LAM 7 years post initial identification of nodal LAM, 2 warranting precautious attention and long‐term follow‐up.
When nodal LAM was identified, it would be prudent to systemically investigate and follow‐up concurrent and subsequent development of pulmonary and extrapulmonary LAM.
Acronyms: CT: computed tomography, LAM: lymphangioleiomyomatosis, ER: Estrogen Receptor, CD: Cluster of Differentiation, α‐SMA: smooth muscle actin, HMB: Human Melanoma Black, HE: Hematoxylin and eosin.
AUTHOR CONTRIBUTIONS
Yuki Muroyama: Conceptualization; formal analysis; investigation; project administration; validation; visualization; writing – original draft; writing – review and editing. Chihiro Inoue: Formal analysis; investigation; validation; writing – review and editing. Fumiyoshi Fujishima: Formal analysis; investigation; project administration; resources; supervision; validation; writing – review and editing. Shogo Shigeta: Investigation; project administration; writing – review and editing. Junko Hasegawa‐Minato: Investigation; writing – review and editing. Muneaki Shimada: Supervision; writing – review and editing. Takashi Suzuki: Investigation; project administration; resources; supervision; validation; writing – review and editing.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
This study was approved by the Tohoku University Hospital Institutional Review Board (number 33853).
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
We thank all the staffs of Department of Pathology, Department of Gynecology, and Institutional Review Board of Tohoku University Hospital, and all the staffs of Department of Anatomic Pathology and Department of Obstetrics and Gynecology, Tohoku University Graduate School of Medicine, for their support.
Muroyama Y, Inoue C, Fujishima F, et al. ExcLAMation marks in a pelvic lymph node. Clin Case Rep. 2023;11:e8339. doi: 10.1002/ccr3.8339
DATA AVAILABILITY STATEMENT
Not applicable.
REFERENCES
- 1. Matsui K, Tatsuguchi A, Valencia J, et al. Extrapulmonary lymphangioleiomyomatosis (LAM): clinicopathologic features in 22 cases. Hum Pathol. 2000;31(10):1242‐1248. doi: 10.1053/hupa.2000.18500 [DOI] [PubMed] [Google Scholar]
- 2. Kuno I, Yoshida H, Shimizu H, et al. Incidental lymphangioleiomyomatosis in the lymph nodes of gynecologic surgical specimens. Eur J Obstetrics Gynecol Reproduct Biol. 2018;231:93‐97. doi: 10.1016/j.ejogrb.2018.10.027 [DOI] [PubMed] [Google Scholar]
- 3. Remo A, Zanella C, Parcesepe P, et al. Diagnostic management of occult nodal lymphangioleiomyomatosis detected during pelvic cancer staging. Localized finding or systemic disease? Sarcoidosis Vasculitis Diffuse Lung Dis. 2019;36(1):33‐38. doi: 10.36141/svdld.v36i1.7110 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


