ABSTRACT
The advent of virtual reality (VR) in education offers unique possibilities for facilitating cooperative learning strategies, particularly in fields demanding intricate spatial understanding, such as gross anatomy. This study investigates the impact of integrating cooperative learning strategies within a VR-based gross anatomy curriculum, focusing on enhancing students’ anatomy knowledge and skills. We analyzed the performance of two cohorts of first-year nursing students across five semesters (2016–2020), where traditional learning methods were used in the first three semesters (2016–2018), and a VR-based cooperative learning approach was adopted in the last two semesters (2019–2020). Our findings suggest that the VR-based cooperative learning group achieved significantly higher scores in their gross anatomy laboratory courses compared to their counterparts learning through traditional methods. This research provides valuable insights into how the integration of VR technology and cooperative learning strategies can not only enhance learning outcomes but also improve the VR learning experience by reducing motion sickness. It accentuates the potential of VR-based cooperative learning as an impactful educational tool in anatomy education. Future research should further explore the optimal integration of VR and cooperative learning strategies in diverse course types and their potential to enhance educational outcomes and the learning experience.
KEYWORDS: cooperative learning, virtual reality, gross anatomy, medical education
INTRODUCTION
Anatomy is a crucial subject in nursing education as it imparts a fundamental understanding of the human body’s structure and function, which is essential for providing effective patient care (1). Generally, anatomy lectures and gross anatomy laboratories are two types of traditional anatomy education that have been used for many years (2). Anatomy lectures involve a didactic lecture of structures in the human body that focuses on the description of form or how body structures at different levels look and function (3). Gross anatomy studies macroscopic structures, which involve cadaveric dissection and learning about topographical structural anatomy. Learning from human cadavers has advantages such as enhancing active and visual learning, preparing students for encounters with death and clinical practice, and understanding the relationship between patients’ symptoms and pathologies (4). However, cadavers are fragile and expensive; additionally, they require maintenance, and their availability is limited (5).
Nowadays, the methods of teaching anatomy have drastically shifted with the arrival of computers and the internet (6). Educational technology has changed the way people engage and interact with learning materials. It creates a powerful environment where students can use their innate learning abilities to grasp complex concepts and acquire knowledge through observation, imitation, and participation (7). The study found that a balance between memorization with understanding and visualization is necessary for the successful learning of anatomy in medicine and other disciplines (8). Additionally, using virtual three-dimensional (3D) models for teaching resulted in nearly 75% of medical students ranking it as equal to, better, or much better than traditional anatomy lectures, textbooks, and literature (9).
The COVID-19 pandemic has significantly impacted anatomy education, leading to a decrease in cadaver availability owing to an increased number of medical students (10). Consequently, the use of technologies such as virtual reality (VR) and augmented reality in anatomy classes has become increasingly popular as they facilitate interactive and collaborative learning. VR can fully immerse the user’s senses in a synthetic environment that mimics real-world properties through high-resolution graphics (11, 12), allowing students to understand anatomical structures three-dimensionally, similar to cadaver dissection (13). While conventional education methods aim to include visual and auditory aspects of learning, VR training facilitates interactive learning and practical work, enhancing student motivation, situational awareness, and understanding of spatial and structural anatomy (14). The integration of cooperative learning strategies within a VR-based gross anatomy learning environment could further amplify these benefits by promoting active participation, collaboration, and communication among peers (15).
The purpose of this study is to explore the impact of implementing cooperative learning strategies within a VR-based gross anatomy learning environment on students’ anatomy knowledge and skills. Many educational studies have been conducted with VR because of its combined aspects of interactive learning and practical work and its positive effect on learning skills (16). However, the effectiveness of cooperative learning strategies within VR-based anatomy education compared to traditional anatomy lectures and gross anatomy laboratories remains unknown.
METHODS
Study design and setting
The study population consisted of undergraduate first-year nursing school students enrolled in a human anatomy course. The semester was 18 weeks long, and the students attended 4 hours of anatomy training each week (2 hours of anatomy lectures and 2 hours of gross anatomy laboratory work) in 2020. Lectures were presented by anatomy professors in classrooms via slides and VR software. In the gross anatomy laboratory, students practice utilizing the VR anatomy software and observing well-dissected cadavers. VR-based teaching methods were conducted for two semesters (2019–2020), which were compared to traditional methods from the previous three-semester years (2016–2018) to prevent bias. Taiwan, being among the few countries that successfully contained the COVID-19 pandemic (17), served as the backdrop for this study. Besides the VR intervention, there has been no significant change during these 5 years.
Research participants and interventions
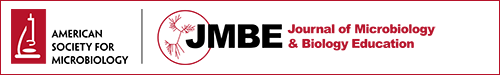
A total of 201 students enrolled in a human anatomy course participated in this study, with 80 students in the VR-based cooperative learning group and 121 students in the traditional group. None of the participants had any motor or sensory impairment or suffered a brain injury. Furthermore, none of them were treated with medication that could potentially impair their physical functioning. First, students had to familiarize themselves with the function and reception of VR devices for anatomical learning. We utilized 3D Organon Anatomy (HTC DeepQ, New Taipei City, Taiwan) for self-learning coursework. The VR-based cooperative learning approach integrated several components, including positive interdependence, individual accountability, promotive interaction, appropriate use of social skills, and group processing (15). Students were organized into small groups and engaged in activities that promoted collaboration and communication while exploring anatomical structures in the virtual environment. During the anatomy course, we gave them two homework assignments monthly (using the question bank from the National Examination for Physicians) via Google Classroom. As a final project, the students made a microfilm to introduce an anatomical topic (e.g., the tour of cranial nerves, yoga anatomy, or how the love hormone works) through 3D Organon and used Zuvio, a Taiwanese-language platform for instructors and students, for mutual evaluation (Fig. 1).
Fig 1.
VR-based learning workflow, including becoming familiar with the device, learning, coursework, examinations, and survey questionnaire.
HTC Vive Pro (HTC, New Taipei City, Taiwan), a professional head-mounted display (HMD), was used for structural demonstrations. Students were given HTC Focus PLUS (HTC), which are portable immersive VR glasses. Using software features, students visually examined different anatomical regions, exploring various layers. They had the opportunity to observe cadaver photos and read supplementary theoretical information regarding the structure they were viewing in VR. Students could also view VR materials on their own smartphones or tablets. After the final examination, they answered 13 symptom-based motion sickness questions in a questionnaire specifically developed for VR-based learning using an HMD (18).
Student performance
The data used for students’ academic performance assessments were collected through two types of examinations. In the laboratory examination, students were given 25 cadaver-pinned structures to identify. They were asked to write specific answers (e.g., acromial of the scapula, deltoid muscle, cephalic vein, trochlear nerve, or amygdala) within a time limit that allowed 30 seconds per question. This study emphasizes the evaluation of students’ performance in the gross anatomy laboratory, where the cooperative learning strategy within the VR-based learning environment was primarily applied.
Statistical analysis
Data were analyzed using SPSS version 26.0 software (IBM Corp., NY, USA). All data were shown as the mean ± standard deviation and percentage. The χ (continuity correction for 2 × 2 tables, Fisher’s exact test for expected value less than 5) and Student’s t-tests were used to compare background characteristics and motion sickness symptoms. A linear multivariate regression model was used to test the effect of the method effect (traditional and VR-based methods), sex (male and female), and the interaction between these factors in the observed variance in students’ performance (scores). All statistical assessments were two-sided, and the significance level was defined as P < 0.05. According to the sample size calculation (19), for linear regression analysis (alpha level, 0.05 with the Bonferroni method), the power of this study was 0.82.
RESULTS
Participants
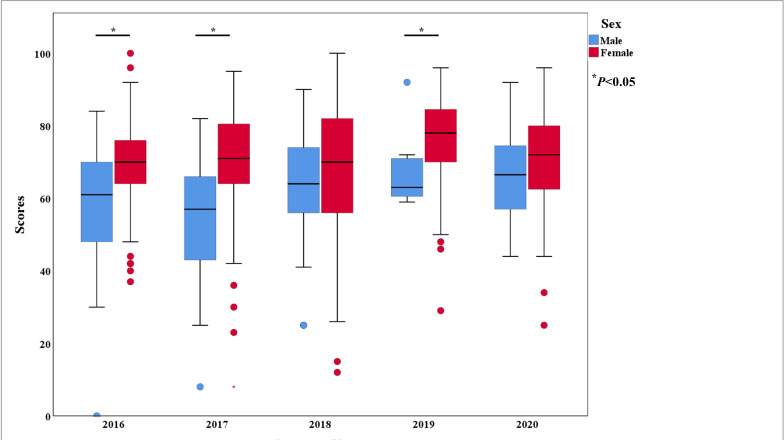
This study included a total of 201 first-year nursing students from 2016 to 2020, comprising 80 students (39.8%) who received VR-based teaching methods with cooperative learning strategies from 2019 to 2020 and 121 students (60.2%) who underwent traditional teaching methods from 2016 to 2018. Table 1 summarizes the academic performance according to participants’ demographic characteristics. The results indicated that students using VR-based learning had significantly higher scores than those using traditional methods (P < 0.001 in male students, P < 0.001 in female students). A total of 169 female (84.1%) students obtained higher scores than male students in both VR-based and traditional learning methods (P = 0.015 and P < 0.001, respectively). In summary, our study demonstrated that VR-based anatomy learning significantly improved student performance compared to traditional methods, especially for female students.
TABLE 1.
Academic performance of participants according to demographic characteristics (2016–2020)
| Variable | VR-based learning | P value | |
|---|---|---|---|
| Yes (n = 80, 39.8%) | No (n = 121, 60.2%) | ||
| Sexa | |||
| Male (n = 32) | 71.8 ± 13.1 | 56.3 (20.3) | <0.001 |
| Female (n = 169) | 78.9 ± 13.2 | 65.8 (15.7) | <0.001 |
| P value | 0.015 | <0.001 | |
| Semestersb | NAc | ||
| 2016 (n = 43) | 0 | 66.9 (17.6) | |
| 2017 (n = 39) | 0 | 62.9 (17.2) | |
| 2018 (n = 39) | 0 | 62.9 (17.3) | |
| 2019 (n = 37) | 81.7 ± 11.5 | 0 | |
| 2020 (n = 43) | 74.6 ± 14.1 | 0 | |
| Midterma | 79.9 ± 13.2 | 67.9 ± 16.5 | <0.001 |
| Finala | 75.8 ± 13.4 | 60.6 ± 16.6 | <0.001 |
| Overalla | 77.9 ± 13.4 | 64.2 ± 16.9 | <0.001 |
Student’s t-test.
Fisher’s exact test.
NA, not available.
Traditional and VR-based learning
In previous semesters (2016–2018) with traditional anatomical learning, teachers introduced a specific topic using PowerPoint and the class textbook in 2-hour lectures. This was followed by introducing the corresponding structures on a cadaver in the laboratory for 2 hours. In VR-based learning (2019–2020), students were divided into small groups to engage in cooperative learning activities using VR Focus PLUS for self-learning outside of class. To improve adaptation to the VR device and promote collaboration, we provided group-based homework assignments twice a month to each group. Furthermore, each group was required to prepare a 10-minute video introducing an anatomical system (e.g., https://youtu.be/5BN3kUmILkc). Examples of titles included “The Tour of Cranial Nerve,” “The Muscle Movement of Weightlifting,” and “How to Perform Colonoscopy.” Figure 2 displays the changing trends in scores for each semester (semester years) in the gross anatomy laboratory. As can be seen from the graph, after implementing the VR-based cooperative learning approach in 2019, there was a significant upward trend in the scores of gross anatomy laboratory students.
Fig 2.
Box plot of anatomy examination scores by different semester years. The distribution of student anatomy scores after using the VR device in 2020 compared with student scores in traditional methods from previous semester years (2017–2019). *P < 0.05.
VR-based participants’ characteristics and potential health risks
Concerning the VR experience, 72 out of the 80 participants had never previously used a VR device (90%). On average, after use, students reported a satisfaction score of 4.72 (out of 5.0). Eighty-seven percent of the students became accustomed to the VR device within the first 30 minutes (Table 2). Notably, about two-thirds of the medical students (65%) experienced discomfort symptoms—including eye fatigue (53.8%), dizziness (42.5%), headaches (16.3%), and disorientation (5%)—within the first 30 minutes of using the VR application (Table 3), which affected their concentration. These issues were not significant between the sexes and may have arisen owing to unfamiliarity with the VR device. One student said, “The homework training will help me to familiarize myself with the device but using it for long hours will affect my study concentration.” Another student added, “The immersive environment can cause a headache for me, but the ‘Mix Reality’ display mode will alleviate the situation.” Intriguingly, female students seemed to experience more discomfort while using the VR device, but the difference was not significant.
TABLE 2.
Academic performance of VR-based participants
| Characteristics | n (%) | Overall scores | P value |
|---|---|---|---|
| Has used VR device | 0.81 | ||
| Yes | 8 (10.0) | 77.9 ± 14.2 | |
| No | 72 (90.0) | 76.8 ± 12.3 | |
| Time taken to familiarize with VR device (minutes) | 0.64 | ||
| ≤30 | 70 (87.5) | 78.5 ± 11.6 | |
| >30 | 10 (12.5) | 76.6 ± 14.3 | |
| Time taken to experience discomfort (minutes) | 0.20 | ||
| ≤30 | 54 (67.5) | 79.9 ± 13.2 | |
| >30 | 26 (32.5) | 75.8 ± 13.3 |
TABLE 3.
Motion sickness symptoms experienced after using the VR device
| Symptoms | N (%) | P valuea | |
|---|---|---|---|
| Male (n = 12) | Female (n = 68) | ||
| Eye fatigue | 5 (41.7) | 38 (55.9) | 0.53 |
| Dizziness | 4 (33.3) | 30 (44.1) | 0.54 |
| Headache | 3 (25.0) | 10 (14.7) | 0.40 |
| Disorientation | 1 (8.3) | 3 (4.4) | 0.68 |
| Nausea | 0 (0.0) | 4 (5.8) | 0.99 |
| Tinnitus | 0 (0.0) | 3 (4.4) | 0.99 |
| Sweating | 6 (50.0) | 29 (42.0) | 0.76 |
| Blurred vision | 0 (0.0) | 2 (2.9) | 0.99 |
Fisher’s exact test.
The factors influencing students’ academic performance
To understand the factors affecting students’ academic performance in gross anatomy, we conducted a univariate analysis of VR, gender, and a course on the distribution of midterm, final, and overall scores (the average of midterms and final scores). Table 4 shows that VR-based learning and female students had significantly higher scores in the midterm, final, and overall performances compared to traditional teaching and male students (P < 0.001). However, in the multivariate regression analysis (Table 5), Model 1 shows that VR-based learning had a significant positive impact on students’ academic performance (overall, β = 13.64, P < 0.001). In Model 2, which added the gender variable based on Model 1, the results show that in addition to VR-based learning, female students also had significantly higher scores (overall, β = 8.51, P < 0.001). In Model 3 interaction analysis, after controlling for learning method and gender, the results revealed that there was no interaction between VR learning and the sex effect, indicating no differences in the effectiveness of VR learning based on sex.
TABLE 4.
Univariate analysis of factors that influence academic performance
| Variables | Academic performance | ||
|---|---|---|---|
| Midterm | Final | Overall | |
| VR-based learning | |||
| Yes (n = 80) | 73.6 ± 13.4 | 72.6 ± 11.6 | 73.1 ± 12.5 |
| No (n = 121) | 68.6 ± 14.5 | 67.3 ± 16.5 | 67.9 ± 15.6 |
| P value | 0.001 | <0.001 | <0.001 |
| Sex | |||
| Male (n = 32) | 61.3 ± 14.9 | 62.7 ± 17.2 | 62.1 ± 16.1 |
| Female (n = 169) | 72.3 ± 13.5 | 70.6 ± 14.3 | 71.4 ± 13.9 |
| P value | <0.001 | <0.001 | <0.001 |
TABLE 5.
Multivariate analysis of factors influencing the academic performance of VR-based learning
| Models | Academic performance | ||
|---|---|---|---|
| Midterm β (P) | Final β (P) | Overall β (P) | |
| Model 1, r2 | 0.13 (<0.001) | 0.19 (<0.001) | 0.15 (<0.001) |
| VR based | 12.10 (<0.001) | 15.18 (<0.001) | 13.64 (<0.001) |
| Model 2, r2 | 0.18 (0.001) | 0.22 (0.01) | 0.19 (<0.001) |
| VR based | 11.96 (<0.001) | 15.07 (<0.001) | 13.51 (<0.001) |
| Sex—female | 9.39 (0.001) | 7.63 (<0.01) | 8.51 (<0.001) |
| Model 3 | |||
| VR based | 6.23 (0.58) | 28.50 (0.13) | 17.36 (0.33) |
| Sex—female | 5.10 (0.56) | 17.68 (0.05) | 11.39 (0.07) |
| VR × sex | 3.11 (0.60) | 7.28 (0.23) | 2.09 (0.63) |
DISCUSSION
The COVID-19 pandemic has significantly impacted not only medical education but also cadaveric-based curricula globally (20, 21). To maintain social distance, online learning has become a major knowledge delivery method (22). Anatomy courses were forced to change from conventional large-group lectures and cadaveric dissection laboratories to online courses (23). With contact hours decreasing, digital learning resources for teaching in medical schools have garnered praise, despite the other effects of the pandemic (24). In this study, we implemented a VR-based learning strategy that enhanced students’ academic performance in gross anatomy examinations compared to traditional learning methods.
A recent survey involving 983 medical students assessed their satisfaction with virtual teaching during the COVID-19 crisis (25). The results indicated that students were satisfied with it, citing improved communication, increased knowledge and skills, professional growth, and ease of assignment submission. Another study demonstrated that VR-based preoperative 3D simulation increased students’ understanding of detailed anatomy, thereby proving to be a useful educational tool (26). Our study similarly indicates the potential benefits of incorporating VR-based learning strategies in anatomy education, especially during times when traditional methods are less feasible owing to public health concerns.
While using VR, users may experience symptoms of motion sickness, leading to time wastage and frustration, eventually affecting their motivation if they lack guidance. In this study, we strategically guided students to operate the VR device by giving them homework and mandating a final video recording. Thereafter, few symptoms persisted, which indicates that our strategy efficiently alleviated the discomfort caused by the device. However, studies have shown that women are more sensitive to VR motion cybersickness and less likely to overcome it (27, 28). In our study, there were no significant differences in the time taken by students of different sexes to familiarize themselves with the VR device or to experience discomfort (Table 2). Additionally, the motion sickness symptoms did not show any significant differences between the sexes. This suggests that motion sickness can be counteracted through habituation protocols and practice. The study also revealed that personalized interpupillary distance could mitigate sickness, especially among females (27, 29). However, there is limited evidence regarding sex-based differences in symptom severity.
Further research could focus on understanding these differences and developing strategies to minimize discomfort for all users, ensuring a more effective and inclusive VR learning experience.
Our study delves into the differentiated impacts of VR-based learning, taking into consideration various factors. As per univariate and multivariate analyses, VR-based learning has significantly improved students’ academic performance, irrespective of gender (Table 5). A key takeaway from these findings is the possibility that VR-based learning implementation might yield more benefits in certain course types, such as practical courses requiring hands-on experience or complex spatial comprehension (14). The immersive nature of VR facilitates students’ better visualization and understanding of complex anatomical structures and relations, especially in gross anatomy laboratory courses. This stands in contrast to the more theoretical content typically presented in lecture courses (30). Moreover, cooperative learning strategies implemented within the VR-based environment promote collaboration among students. This not only facilitates peer learning but also cultivates critical soft skills like teamwork and communication (15). In conclusion, our study underscores the potential of VR-based cooperative learning as an effective educational tool, particularly in gross anatomy laboratory courses. However, there is a need for more in-depth research to explore the factors contributing to the success of VR-based learning in different course types, such as the interplay between cognitive demands, teaching methods, and student engagement. Future research should strive to investigate the underlying factors responsible for the differential effectiveness of VR-based cooperative learning across various course types, aiming to optimize its implementation for superior educational outcomes.
Limitations of the study
There are three limitations to this study that should be considered when interpreting the results. First, the study included a limited number of participants from a single medical school, which may affect the generalizability of the results. However, we ensured that the sample was representative of the student population in terms of gender and course type. Future studies should involve larger and more diverse samples from multiple institutions to better understand the effectiveness of VR-based learning in various settings. Second, potential selection bias could have influenced the effectiveness assessment of VR-based cooperative learning in our study, as the students who participated might have already held a specific interest in VR technology. To further ensure the reliability of our findings and minimize any potential bias from single-term performance anomalies, we used student performance data from two academic terms. This incorporation of multiple terms’ performance data allowed us to provide a more comprehensive view of the benefits and effectiveness of VR-based cooperative learning in gross anatomy education. Third, although we accounted for gender, there may have been other confounding variables that we did not control for, such as students’ previous experience with VR technology (31).
Despite these limitations, our study rigorously examined the impact of VR-based learning on academic performance while controlling for crucial factors and providing valuable insights for future research. To address these limitations, future research should aim to conduct larger, multicentered, and more diverse studies that control for additional confounding variables, assess long-term outcomes, and consider factors like user experience, instructor quality, and cost-effectiveness.
Conclusion
Despite the success and effectiveness of the VR-based system, using cadaveric material (the first patient) is still a crucial part of students’ development toward becoming medical or biomedical professionals (32). Anatomy curricula teach students more than just anatomy, promoting professionalism and empathy (33). Our study demonstrated that using the VR system initiated a positive transformation in anatomy teaching, supporting medical education during the COVID-19 pandemic. Immersive VR enhanced spatial knowledge of anatomical structures and led to significantly higher laboratory scores compared to the traditional method. To maximize the potential of this innovative learning system, teachers and students should collaboratively endeavor to master the use of this tool, overcome its limitations, and harness the benefits it offers for medical education.
ACKNOWLEDGMENTS
The authors thank the Medical Affairs Bureau (MAB) and Higher Education SPROUT Project Office in the National Defense Medical Center for supporting this study. They are also grateful to all anatomy students who agreed to complete the survey.
This work was supported by the MAB of the Ministry of National Defense (grant numbers MND-MAB-110–049 and MND-MAB-D-111–072 awarded to M.-H.C.).
No potential conflict of interest was reported by the author(s).
Contributor Information
Ming-Hsien Chiang, Email: ph870101@mail.ndmctsgh.edu.tw.
Stanley Maloy, San Diego State University, San Diego, California, USA.
ETHICS APPROVAL
The study was conducted in accordance with the Declaration of Helsinki and was granted ethical approval by the Tri-Service General Hospital ethical committee (reference number C202205089). Informed written consent was obtained from all patients prior to their enrollment in this study.
DATA AVAILABILITY
The data for statistical analysis was available in a public, open-access repository:
https://osf.io/tu36z/files/osfstorage/650c67facf3dc931caad1680.
REFERENCES
- 1. Connolly SA, Gillingwater TH, Chandler C, Grant AW, Greig J, Meskell M, Ross MT, Smith CF, Wood AF, Finn GM. 2018. The anatomical society’s core anatomy syllabus for undergraduate nursing. J Anat 232:721–728. doi: 10.1111/joa.12782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Azer SA, Eizenberg N. 2007. Do we need dissection in an integrated problem-based learning medical course? Perceptions of first- and second-year students. Surg Radiol Anat 29:173–180. doi: 10.1007/s00276-007-0180-x [DOI] [PubMed] [Google Scholar]
- 3. Lochner L, Wieser H, Waldboth S, Mischo-Kelling M. 2016. Combining traditional anatomy lectures with e-learning activities: how do students perceive their learning experience? Int J Med Educ 7:69–74. doi: 10.5116/ijme.56b5.0369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fruhstorfer BH, Palmer J, Brydges S, Abrahams PH. 2011. The use of plastinated prosections for teaching anatomy—the view of medical students on the value of this learning resource. Clin Anat 24:246–252. doi: 10.1002/ca.21107 [DOI] [PubMed] [Google Scholar]
- 5. McLachlan JC, Patten D. 2006. Anatomy teaching: ghosts of the past, present and future. Med Educ 40:243–253. doi: 10.1111/j.1365-2929.2006.02401.x [DOI] [PubMed] [Google Scholar]
- 6. Chevrel JP. 1995. The modern teaching of modern anatomy. Surg Radiol Anat 17:285–286. doi: 10.1007/BF01795182 [DOI] [PubMed] [Google Scholar]
- 7. Goodyear P, Retalis S. 2010. Technology-enhanced learning: Design patterns and pattern languages. doi: 10.1163/9789460910623 [DOI] [Google Scholar]
- 8. Pandey P, Zimitat C. 2007. Medical students’ learning of anatomy: memorisation, understanding and visualisation. Med Educ 41:7–14. doi: 10.1111/j.1365-2929.2006.02643.x [DOI] [PubMed] [Google Scholar]
- 9. Petersson H, Sinkvist D, Wang C, Smedby O. 2009. Web-based interactive 3D visualization as a tool for improved anatomy learning. Anat Sci Educ 2:61–68. doi: 10.1002/ase.76 [DOI] [PubMed] [Google Scholar]
- 10. Saverino D. 2021. Teaching anatomy at the time of COVID-19. Clin Anat 34:1128. doi: 10.1002/ca.23616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moro C, Štromberga Z, Raikos A, Stirling A. 2017. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ 10:549–559. doi: 10.1002/ase.1696 [DOI] [PubMed] [Google Scholar]
- 12. Jeffries PR, Bushardt RL, DuBose-Morris R, Hood C, Kardong-Edgren S, Pintz C, Posey L, Sikka N. 2022. The role of technology in health professions education during the COVID-19 pandemic. Acad Med 97:S104–S109. doi: 10.1097/ACM.0000000000004523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Iwanaga J, Loukas M, Dumont AS, Tubbs RS. 2021. A review of anatomy education during and after the COVID-19 pandemic: revisiting traditional and modern methods to achieve future innovation. Clin Anat 34:108–114. doi: 10.1002/ca.23655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aasekjær K, Gjesdal B, Rosenberg I, Bovim LP. 2023. Virtual reality (VR) in anatomy teaching and learning in higher Healthcare education, p 117–129. In Akselbo I, Aune I (ed), How can we use simulation to improve Competencies in nursing? Springer International Publishing, Cham. doi: 10.1007/978-3-031-10399-5 [DOI] [Google Scholar]
- 15. Johnson DW, Johnson RT. 2009. An educational psychology success story: social interdependence theory and cooperative learning. Educ Res 38:365–379. doi: 10.3102/0013189X09339057 [DOI] [Google Scholar]
- 16. Nicholson DT, Chalk C, Funnell WRJ, Daniel SJ. 2006. Can virtual reality improve anatomy education? A randomised controlled study of a computer‐generated three‐dimensional anatomical ear model. Med Educ 40:1081–1087. doi: 10.1111/j.1365-2929.2006.02611.x [DOI] [PubMed] [Google Scholar]
- 17. Chiu TF, Chu D, Huang SJ, Chang M, Liu Y, Lee JJ. 2021. Facing the coronavirus pandemic: an integrated continuing education program in Taiwan. Int J Environ Res Public Health 18:2417. doi: 10.3390/ijerph18052417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ames SL, Wolffsohn JS, McBrien NA. 2005. The development of a symptom questionnaire for assessing virtual reality viewing using a head-mounted display. Optom Vis Sci 82:168–176. doi: 10.1097/01.opx.0000156307.95086.6 [DOI] [PubMed] [Google Scholar]
- 19. Faul F, Erdfelder E, Buchner A, Lang AG. 2009. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160. doi: 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- 20. McWatt SC. 2021. Responding to COVID-19: a thematic analysis of students’ perspectives on modified learning activities during an emergency transition to remote human anatomy education. Anat Sci Educ 14:721–738. doi: 10.1002/ase.2136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sandhu P, de Wolf M. 2020. The impact of COVID-19 on the undergraduate medical curriculum. Med Educ Online 25:1764740. doi: 10.1080/10872981.2020.1764740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Das S, Al Mushaiqri M. 2021. Anatomy online teaching during COVID-19 pandemic: the need for responsive anatomy learning ecosystem. Anat Sci Educ 14:428–429. doi: 10.1002/ase.2082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ahmed H, Allaf M, Elghazaly H. 2020. COVID-19 and medical education. Lancet Infect Dis 20:777–778. doi: 10.1016/S1473-3099(20)30226-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wilcha RJ. 2020. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ 6:e20963. doi: 10.2196/20963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kaur N, Dwivedi D, Arora J, Gandhi A. 2020. Study of the effectiveness of e-learning to conventional teaching in medical undergraduates amid COVID-19 pandemic. Natl J Physiol Pharm Pharmacol 10:1. doi: 10.5455/njppp.2020.10.04096202028042020 [DOI] [Google Scholar]
- 26. Wada Y, Nishi M, Yoshikawa K, Higashijima J, Miyatani T, Tokunaga T, Takasu C, Kashihara H, Ishikawa D, Yoshimoto T, Shimada M. 2020. Usefulness of virtual three-dimensional image analysis in Inguinal hernia as an educational tool. Surg Endosc 34:1923–1928. doi: 10.1007/s00464-019-06964-y [DOI] [PubMed] [Google Scholar]
- 27. Fulvio JM, Ji M, Rokers B. 2021. Variations in visual sensitivity predict motion sickness in virtual reality. Entertainment Comput 38:100423. doi: 10.1016/j.entcom.2021.100423 [DOI] [Google Scholar]
- 28. Grassini S, Laumann K. 2020. Are modern head-mounted displays sexist? A systematic review on gender differences in HMD-mediated virtual reality. Front Psychol 11:1604. doi: 10.3389/fpsyg.2020.01604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stanney K, Fidopiastis C, Foster L. 2020. Virtual reality is sexist: but it does not have to be. Front Robot AI 7:4. doi: 10.3389/frobt.2020.00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chen S, Zhu J, Cheng C, Pan Z, Liu L, Du J, Shen X, Shen Z, Zhu H, Liu J, Yang H, Ma C, Pan H. 2020. Can virtual reality improve traditional anatomy education programmes? A mixed-methods study on the use of a 3D skull model. BMC Med Educ 20:395. doi: 10.1186/s12909-020-02255-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhao G, Fan M, Yuan Y, Zhao F, Huang H. 2021. The comparison of teaching efficiency between virtual reality and traditional education in medical education: a systematic review and meta-analysis. Ann Transl Med 9:252. doi: 10.21037/atm-20-2785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Smith CF, Martinez-Álvarez C, McHanwell S. 2014. The context of learning anatomy: does it make a difference? J Anat 224:270–278. doi: 10.1111/joa.12089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Evans DJR, Pawlina W, Lachman N. 2018. Human skills for human[istic] anatomy: an emphasis on nontraditional discipline-independent skills. Anat Sci Educ 11:221–224. doi: 10.1002/ase.1799 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data for statistical analysis was available in a public, open-access repository:
https://osf.io/tu36z/files/osfstorage/650c67facf3dc931caad1680.