Abstract
Background:
First Nations children in Canada experience health inequities. We aimed to determine whether a self-report health app identified children’s needs for support earlier in their illness than would typically occur.
Methods:
Children (aged 8 to 18 yr) were recruited from a rural First Nation community. Children completed the Aaniish Naa Gegii: the Children’s Health and Well-being Measure (ACHWM) and then met with a local mental health worker who determined their risk status. ACHWM Emotional Quadrant Scores (EQS) were compared between 3 groups of children: healthy peers (HP) who were not at risk, those with newly identified needs (NIN) who were at risk and not previously identified, and a typical treatment (TT) group who were at risk and already receiving support.
Results:
We included 227 children (57.1% girls), and the mean age was 12.9 (standard deviation [SD] 2.9) years. The 134 children in the HP group had a mean EQS of 80.1 (SD 11.25), the 35 children in the NIN group had a mean EQS of 67.2 (SD 13.27) and the 58 children in the TT group had a mean EQS of 66.2 (SD 16.30). The HP group had significantly better EQS than the NIN and TT groups (p < 0.001). The EQS did not differ between the NIN and TT groups (p = 0.8).
Interpretation:
The ACHWM screening process identified needs for support among 35 children, and the associated triage process connected them to local services; the similarity of EQS in the NIN and TT groups highlights the value of community screening to optimize access to services. Future research will examine the impact of this process over the subsequent year in these groups.
Indigenous (First Nations, Inuit and Métis) children in Canada experience serious health inequities compared to non-Indigenous children.1–3 Rates of mental health crises are highest in northern and rural communities, where the rates of physician visits for mental health support are lowest.4 Indigenous children are often forced to seek treatment hundreds of kilometres away from home, creating a disconnect from family and natural helpers that is not conducive to healing. 5 One opportunity to improve the fit between the needs of children and local resources is by identifying emergent needs within the community6 and connecting these children to culturally based services within their communities.7
Indigenous health leaders are eager to improve children’s health outcomes8 and focus upstream on primary and secondary prevention (early intervention) critical in isolated communities. Early intervention is effective in high-risk youth populations.9,10 It is contingent on recognizing needs, which can be achieved through school-based screening, a recommended best practice for harm reduction,11,12 and aligns with several key guidance documents relevant to this population.13–15
We measured health using the Aaniish Naa Gegii: the Children’s Health and Well-being Measure (ACHWM).16–22 It is a self-report measure developed with and for Indigenous children aged 8 to 18 years19 to ensure solutions come from within each community.23,24 The ACHWM was developed through a series of 6 full-day focus groups with 38 Indigenous children in Wiikwemkoong Unceded Territory.19 As part of these sessions, children between the ages of 8 and 18 years completed photovoice activities to identify the core concepts of wellness that were important for them to include in a measure of health and well-being. These focus groups were grounded in teachings about wellness from local elders. The participants in each focus group used stickers to identify the importance of each concept and the results were pooled to form the item bank.
The ACHWM contains 62 questions representing the 4 quadrants of health following the medicine wheel teachings: spiritual, emotional, physical and mental (or intellectual). The medicine wheel reflects the holistic conception of health and well-being and is a framework that has been described elsewhere.25–27 The measure includes questions about spiritual (16 questions), emotional (24), physical (13), and mental or cognitive (9) health.28 The measure is completed on tablets in community and clinical contexts. It is culturally appropriate,18,20 is valid in comparison to the PedsQL (Pediatric Quality of Life Inventory) (r = 0.52, p = 0.0001),22 is reliable (Cronbach α = 0.93, test-retest intraclass correlation coefficient = 0.94),21 is sensitive,17 has strong psychometric performance as assessed by Rasch analysis29 and is supported by Health Canada.30 The ACHWM is not a diagnostic tool. Rather, the app provides an opportunity for Indigenous children to express their perceptions of health and leads to honest conversations with local health staff to promote wellness.
The app generates a summary score and 4 domain scores: spiritual quadrant score (SQS), emotional quadrant score (EQS), physical quadrant score (PQS) and mental (or intellectual) quadrant score (MQS). Note that the term “emotional health” is used in keeping with the Anishinaabe teachings and refers to “mental health” in Western society. The ACHWM is transforming the way Indigenous children are engaged in health assessment by initiating strengths-based conversations. It includes screening and triage processes17 that identify potential risk based on 1 highly concerning response or 2 moderately concerning responses, and expedites connections to local, culturally based supports for children. In addition, the ACHWM helps initiate strengths-based conversations about health with children.
Our aim was to determine whether the ACHWM16–22 was able to identify Indigenous children’s symptoms when they were emergent rather than urgent.
Methods
This study was conducted between 2016 and 2019 in a First Nation in Canada: Wiikwemkoong Unceded Territory, Ontario, Canada.
Design
This article reports the results of a prospective cohort study that compares the baseline health scores from community and clinical cohorts in a cross-sectional design. We follow the Strengthening the Reporting of Observational Studies in Epidemiology Statement reporting guidelines31 and aim to inform community health leaders, clinicians and a general academic audience.
Recruitment
Children between the ages of 8 and 18 years were recruited in Wiikwemkoong Unceded Territory. We aimed to recruit 250 children in the territory (approximately half of the target population) who were not receiving mental health treatment, to form the first cohort. This was done via information packages sent home from community schools and the recreation centre.32 The second cohort was expected to include 60 children currently undergoing mental health treatment based on referral records from previous years. This cohort was recruited by individual invitation at the Nadmadwin Mental Health Clinic in Wiikwemkoong Unceded Territory.32 This study was a community-based participatory action study in which the community members conducted the recruitment.
Sources of data
Participants in the first cohort completed the ACHWM in the community at local schools, a youth centre and community events. Their summary scores and flag counts were screened for acute symptoms in real time, using a previously validated algorithm.17 The term flags refers to responses suggesting potential risk (e.g., always feeling bullied and never having hope for their future). Each participant met with a local mental health worker to discuss their experience with the ACHWM. The mental health workers first celebrated each child’s unique strengths (e.g., asked each child to talk about the quadrant with the highest scores), then assessed the child’s emotional health through a clinical interview based on local practices. This cohort was divided into 2 groups based on the mental health worker’s clinical assessments of risk of a poor emotional health outcome; those who were not at risk were assigned to the healthy peers (HP) group and those who were at risk were assigned to the newly identified needs (NIN) group. We expected 45 of this cohort to be in the NIN group based on our previous research with this community.16,33 All children in the NIN group were provided immediate support and connected to local services for ongoing treatment.
The second cohort was recruited from the Nadmadwin Mental Health Clinic and formed the typical treatment (TT) group. They completed the ACHWM during one of their counselling sessions at Nadmadwin, at a time deemed appropriate by their therapist to ensure that the study did not delay access to urgently needed support. These children continued to receive mental health support according to their clinical plan.
Analysis
We aimed to determine whether the ACHWM would identify Indigenous children’s needs at a less severe stage. All analyses were conducted using Stata version 15. We used analysis of variance (ANOVA) to compare EQS (primary outcome) between the HP, NIN and TT groups, and when this global test was significant, results were followed up with post-hoc t test comparisons between pairs of groups. EQS is the sum of 24 emotional questions, rescaled from 0 to 100 where 100 indicates optimal health. Since the NIN group was not accessing emotional health supports before ACHWM completion, we hypothesized a priori that they would have higher EQS than the TT group.
In Anishinaabe teachings, health is a “wholistic” construct (the term wholistic is used to reflect the teachings from the community). Thus, we also explored differences between the 3 comparison groups in the ACHWM summary scores and the other 3 quadrants of health: spiritual, physical and mental (intellectual). We also explored the questions that contributed to screening positive for potential risk (defined as 1 highly concerning response or 2 moderately concerning responses) between groups.
Ethics approval
This study design was previously described32 and approved by the Laurentian University’s Research Ethics Board and the Wiikwemkoong Chief and Council. The data analyzed in this article were gathered with informed consent. The raw data will remain private to protect participants’ confidentiality and respect data sovereignty.34–36
Results
This protocol was adapted to ensure the optimal design and fit with community circumstances. Specifically, the recruitment period for the TT group was extended by approximately 1 year to generate a sufficient sample size (Table 1). Thus, data from the TT group were gathered approximately 1 year later than data from the HP and NIN groups.
Table 1:
Characteristics of the sample by group*
| Variable | Healthy peers | Newly identified needs | Typical treatment† |
|---|---|---|---|
| Proposed sample size | 205 | 45 | 60 |
| Sample size | 134 | 35 | 58 |
| Age, yr,‡ mean ± SD | 13.1 ± 2.8 | 13.1 ± 2.8 | 12.2 ± 3.1 |
| Female,§ % | 52.2 | 71.4 | 59.6 |
Note: ACHWM = Aaniish Naa Gegii: the Children’s Health and Well-being Measure, SD = standard deviation.
There were no missing data for variables of interest.
The number of days between start of treatment and completing the ACHWM was available for 42 of the children in the typical treatment group, who had a median interval of 3.5 (interquartile range 0–20) days, and 37% completed the ACHWM at the start of treatment.
There were no significant age differences between the groups (analysis of variance adjusted R2 = 0.0069, p = 0.2).
There were no significant gender differences between the groups (χ2 = 4.38, p = 0.1).
Sample characteristics
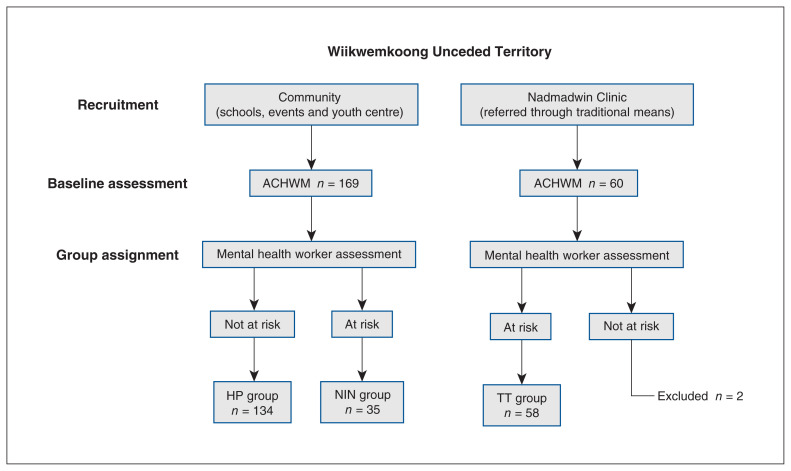
We included 227 children (57.1% girls), whose mean age was 12.9 (standard deviation [SD] 2.9) years, representing approximately 42% of the 545 band members aged 8 to 18 years living in Wiikwemkoong Unceded Territory (Band Council Secretary, Wiikwemkoong Unceded Territory: personal communication, 2016). There were 169 children in the community-based cohort who were considered to be healthy (not at risk). The tablet-based ACHWM screening process identified 54 (32.0%) children as potentially at risk within this community-based cohort. Local mental health worker determined that 31 were true positives, and 4 of the 115 negative results (3.5%) were false negatives (none of the 4 had serious health issues, and minimal treatment was required). Thus, 35 children (20.7% of the community cohort) formed the NIN group, leaving 134 in the HP reference group. There were 58 children recruited from the mental health clinic, all known to be at risk, who formed the TT group (median treatment duration of 3.5 [interquartile range 0–20] days). The creation of the 3 groups (HP, NIN and TT) is shown in Figure 1, and demographic characteristics are summarized in Table 1.
Figure 1:
Sampling results. Updated from Young et al.32 with permission from the International Journal of Indigenous Health. Note: ACHWM = Aaniish Naa Gegii: the Children’s Health and Well-being Measure, HP = healthy peers, NIN = newly identified needs, TT = typical treatment.
Age and gender differences between groups were explored and were not significant (Table 1). Further exploration identified a subtle trend in EQS in the pooled sample associated with age (a reduction of 0.85 points per year of age, 95% confidence interval [CI] −1.5 to 0.2). EQS values were similar between genders. The unadjusted results are reported here for ease of interpretation.
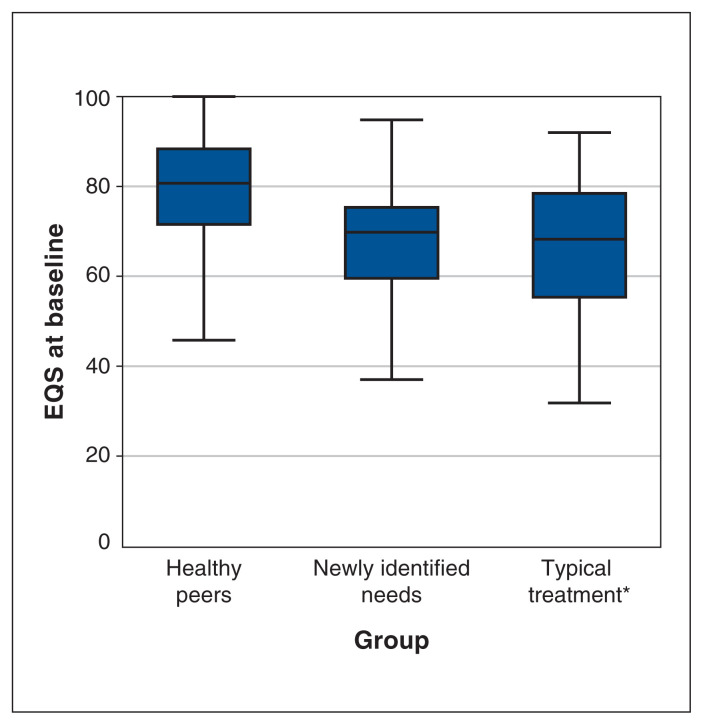
Differences in ACHWM quadrant scores between groups
The primary analysis identified a significant difference in EQS between groups (ANOVA p < 0.001), as shown in Figure 2. The mean EQS for the NIN group was 67.2 (SD 13.3) and was not significantly different (post hoc comparison p = 0.8) from the mean score of children in the TT group, who had a mean EQS value of 66.2 (SD 16.3). The mean difference between the NIN and TT groups was 1.0. The mean EQS values for the NIN and TT groups were both significantly lower than the mean EQS value from the HP group (post hoc comparison p < 0.001) of 80.1 (SD 11.25). These comparisons were repeated using the Welch adjustment for unequal variances, which confirmed that the NIN and TT groups had significantly lower mean EQS values than the HP group (p = 0.02 and p < 0.001, respectively) and that the NIN and TT groups did not differ from each other.
Figure 2:
Emotional Quadrant Scores (EQS) by group. *Outliers removed to protect confidentiality.
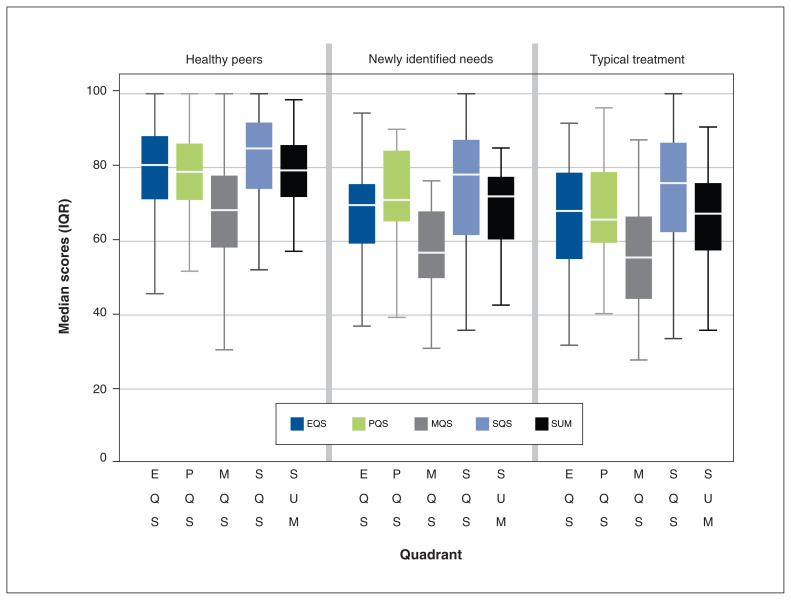
The mean scores by group for all quadrants of health and the summary score are presented in Table 2. Medians and interquartile ranges from these scores are shown in Figure 3.
Table 2:
Summary scores by group
| Mean ± SD | |||
|---|---|---|---|
| Healthy peers n = 134 |
Newly identified needs n = 35 |
Typical treatment n = 58 |
|
| Emotional quadrant | 80.13 ± 11.25 | 67.21 ± 13.27 | 66.24 ± 16.30 |
| Spiritual quadrant | 82.52 ± 12.04 | 74.83 ± 16.72 | 72.98 ± 17.33 |
| Physical quadrant | 78.69 ± 11.82 | 71.96 ± 12.77 | 69.04 ± 12.95 |
| Mental quadrant | 68.28 ± 13.08 | 58.07 ± 11.44 | 55.95 ± 14.07 |
| Summary | 78.70 ± 9.96 | 68.84 ± 11.47 | 67.07 ± 13.03 |
Note: SD = standard deviation.
Figure 3:
Distribution of scores by group. Note: EQS = Emotional Quadrant Scores, MQS = Mental Quadrant Scores, PQS = Physical Quadrant Scores, SQS = Spiritual Quadrant Scores, SUM = Summary Score Scores.
The HP group reported consistently higher (better) scores than the NIN and TT groups by more than 10.4 on average. These differences were significant (p < 0.001) and clinically meaningful across all quadrants.
The scores for the NIN group were higher by small amounts compared with the TT group in the spiritual, physical and mental quadrants, and the summary scores. These differences did not reach significance (p values ranged from 0.3 for physical to 0.5 for spiritual) and were not clinically meaningful. We also explored the number of flags for each child and the type of questions that were flagged. The median number of flags in the NIN group was 4 (IQR 2–6), compared with 2.5 (IQR 1–5) in the TT group and 0 (IQR 0–1) in the HP group. The flags most commonly raised by children in the NIN group were similar to those raised in the TT group.
Interpretation
We identified significantly better EQS (> 10 points) in the HP group compared with the NIN and TT groups. Similar differences were observed in the other quadrants. Thus, the ACHWM is able to clearly distinguish between healthy children and those who need support. Despite our prediction that the ACHWM might identify children’s need for support earlier in their illness, the EQS of the NIN group were not different from those of the TT group. To aid in interpretation, we computed the mean EQS in the pooled sample (HP, TT and NIN groups combined), which was 74.6 (95% CI 72.7–76.5), and is similar to the EQS of 74.4 (95% CI 72.5–76.3) that is considered typical in a First Nations population.16
A critically important finding is that we identified 20.7% of children in the community sample as being at risk of an adverse health outcome, and the results of the app aided in efficiently connecting them to local support services. Thus, the project has generated new opportunities for children who were not yet receiving support from the health system and may have experienced barriers in accessing support. Our results suggest that the ACHWM is a useful community-based screening and triage process grounded in youth needs and offers an effective secondary prevention strategy that expedites referrals to community services and supports stepped care.37
We note the summary scores in this community have increased over time, from 71.4 in 201322 to 72.5 in 2014,38 75.1 in 201539 and 76.7 in this study. Our results confirm screening reports of 17.5% and 18.2% from similar Wiikwemkoong Unceded Territory cohorts in 2014 and 2015,17 respectively, and extend that work by including all quadrant scores and a clinical comparison group.
We have explored the reasons for concern (i.e., flags). We noted that the NIN group had more flags (less favourable) than the TT group; these were related to personal safety (e.g., rarely feeling safe) and underscore the critical role of community-based health screening in Indigenous communities. Although 4 children who were at risk were missed by screening, their EQS were high (> 75), and they required minimal support. Thus, all serious emotional issues were detected by the ACHWM. The flag counts in the NIN group underscore the need for additional funding and human resources to support children whose symptoms may be less obvious yet clinically meaningful. Reaching out to children at this subacute phase has the potential to improve the effectiveness of community-based mental health services. However, the clinical assessment is far more efficient because the App identifies the subgroup most likely to be at risk and why.
In this article, we describe the health of a cohort of Indigenous children, including 35 children identified as newly in need of support compared with a clinical cohort. Data have been lacking for this population. All 3 groups were followed prospectively, and a subsequent article will report on the impact of ACHWM screening on health outcomes after 1 year.
Limitations
Our research was conducted with a single First Nation community and was limited to children for whom we obtained consent. This led to a relatively small sample (73% of the proposed sample) and may have introduced some consent bias. Thus, it may be difficult to generalize to Indigenous communities elsewhere in Canada. We encourage other communities to explore the app’s effectiveness in their local context. In addition, approximately one-third of participants completed the ACHMW at the start of treatment, with the others completing the measure partway through treatment.
Conclusion
The ACHWM screening process identified needs for support among 35 children, and the associated triage process connected them to local services. The ACHWM app gives Indigenous children a way to communicate their perceptions of health and screens for acute symptoms. Although the app did not identify children’s needs at a lower acuity level, it demonstrated a significant clinical impact in 3 important ways. First, the app detected the needs of many children (21% of the community sample) when they were emergent rather than urgent. Second, the ACHWM app and associated triage protocol triggered immediate referrals that connected children at risk to local and culturally appropriate supports. Third, this approach was a catalyst for strengths-based conversations between local mental health workers and school-aged children and facilitated connections that would not have otherwise been possible.
The ACHWM screening process aligns with the goals of Indigenous health leaders who are eager to improve the health outcomes of their children, particularly their mental wellness.8 The ACHWM offers a mechanism to reduce the number of children needing screening by a local mental health worker (some v. all), thus reducing the cost associated with screening and enhancing access to local mental health workers for children in greatest need. It also has the potential to optimize the allocation of scarce resources. However, it is crucial to recognize that funding inequities limit services in Indigenous communities and must be addressed so that the needs of all children can be met. Until the structural colonial barriers that drive inequities are dismantled, the best approach is to understand who is in the greatest need and connect them to care and support.6
Supplementary Material
Acknowledgements
The authors acknowledge Elder Rita Corbier for her support of this research and for sharing her wisdom with our team. The authors also acknowledge Sarah Seabrook and Thecla Neganegijig for assistance with the study.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: This is a community-based participatory action research project. As such there are many authors. Nancy Young and Mary Jo Wabano are the study leads and participated in all aspects of the study. Diane Jacko, Franco Momoli, Peter Szatmari, Lorrilee McGregor, Koyo Usuba, Annie Roy-Charland, Katherine Boydell and Kednapa Thavorn contributed to the design, participated in the advisory committee and contributed to the analysis and writing. Christopher Mushquash, Brenda Restoule, Renee Linklater and Skye Barbic contributed on the advisory committee, contributed to the interpretation of the analysis and supported the writing of the article. Marnie Anderson and Trisha Trudeau were the research assistants who supported the implementation of this project. Ranjeeta Mallick and Oxana Mian provided statistical support. Lauren Hawthorne, Alison Cudmore, Shanna Peltier and Jessica Denommee contributed to the data gathering and to writing the paper. Linda Kaboni, Natalie Neganegijig, Debbie Mishibinijima and Sylvia Recollet were part of the mental health team and were instrumental in guiding this study, assessing the children’s risk and providing necessary support. Marnie Anderson, Trish Trudeau, Cody Wassengeso, Katarina Djeletovic and Melissa Roy were critical supports in the community who assisted with study coordination and data gathering. All authors reviewed the article, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: This project was funded by a Child Health IMPACT grant from the Ontario SPOR Support Unit.
Data sharing: The raw data will remain private to protect participants’ confidentiality and respect data sovereignty.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/11/6/E1148/suppl/DC1.
References
- 1.First Nations and Inuit Health Strategic Plan: a shared path to improved health. Ottawa: Health Canada; 2012. [Google Scholar]
- 2.Canadian supplement to The State of the World’s Children 2009: Aboriginal children’s health — leaving no child behind. Toronto: Canadian UNICEF Committee, UNICEF Canada; 2009. [Google Scholar]
- 3.Adelson N. The embodiment of inequity: health disparities in Aboriginal Canada. Can J Public Health. 2005;96(Suppl 2):S45–61. doi: 10.1007/BF03403702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MHASEF Research Team. The mental health of children and youth in Ontario: a baseline scorecard. Toronto: ICES; 2015. [Google Scholar]
- 5.Oulanova O, Moodley R. Navigating two worlds: experiences of counsellors who integrate Aboriginal traditional healing practices. Can J Couns Psychother. 2010;44:346–62. [Google Scholar]
- 6.A comprehensive approach to suicide prevention. Oklahoma City (OK): Suicide Prevention Resource Center; 2019. [accessed 2019 Aug 12]. Available: www.sprc.org/effective-prevention/comprehensive-approach. [Google Scholar]
- 7.Assembly of First Nations National Youth Council. Calls to action on life promotion in First Nations communities. Ottawa: Assembly of First Nations; 2016. [Google Scholar]
- 8.First Nation mental wellness continuum framework: summary report. Ottawa: Health Canada; 2014. pp. 1–16. modified 2015 Jan 27. [Google Scholar]
- 9.Clifford AC, Doran CM, Tsey K. A systematic review of suicide prevention interventions targeting Indigenous peoples in Australia, United States, Canada and New Zealand. BMC Public Health. 2013;13:463. doi: 10.1186/1471-2458-13-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson J, Cox G, Malone A, et al. A systematic review of school-based interventions aimed at preventing, treating, and responding to suicide-related behavior in young people. Crisis. 2013;34:164–82. doi: 10.1027/0227-5910/a000168. [DOI] [PubMed] [Google Scholar]
- 11.Scott MA, Wilcox HC, Schonfeld IS, et al. School-based screening to identify at-risk students not already known to school professionals: the Columbia suicide screen. Am J Public Health. 2009;99:334–9. doi: 10.2105/AJPH.2007.127928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kutcher SP, Szumilas M. Youth suicide prevention. CMAJ. 2008;178:282–5. doi: 10.1503/cmaj.071315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Aboriginal Youth Suicide Prevention Strategy (NAYSPS) program framework. Ottawa: Health Canada; 2013. modified 2019 Dec 11. [Google Scholar]
- 14.Atkinson D. Considerations for Indigenous child and youth population mental health promotion in Canada. National Collaborating Centres for Public Health; 2017. [Google Scholar]
- 15.Mahler H, Epp J, Franklin W, et al. Ottawa charter for health promotion. Health Promot Int. 1986;1:405. [Google Scholar]
- 16.Wabano MJ, McGregor LF, Beaudin R, et al. Health profiles of First Nations children living on-reserve in Northern Ontario: a pooled analysis of survey data. CMAJ Open. 2019;7:E316–22. doi: 10.9778/cmajo.20180128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young NL, Jacko D, Wabano MJ, et al. A screening mechanism to recognize and support Aboriginal children. Can J Public Health. 2016;107:e399–403. doi: 10.17269/CJPH.107.5539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Young NL, Wabano MJ, Blight S, et al. Relevance of the Aboriginal children’s health and well-being measure beyond Wikwemikong. Rural Remote Health. 2017;17:3941. doi: 10.22605/rrh3941. [DOI] [PubMed] [Google Scholar]
- 19.Young NL, Wabano MJ, Burke TA, et al. A process for creating the Aboriginal Children’s Health and Well-being Measure (ACHWM) Can J Public Health. 2013;104:e136–41. doi: 10.1007/BF03405677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Young NL, Wabano MJ, Ritchie SD, et al. Assessing children’s interpretations of the Aboriginal Children’s Health and Well-being Measure (ACHWM) Health Qual Life Outcomes. 2015;13:105. doi: 10.1186/s12955-015-0296-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Young NL, Wabano MJ, Usuba K, et al. Reliability of the Aboriginal Children’s Health and Well-being Measure (ACHWM) Springerplus. 2016;5:2082. doi: 10.1186/s40064-016-3776-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young NL, Wabano MJ, Usuba K, et al. Validity of the Aboriginal Children’s Health and Well-Being Measure: Aaniish Naa Gegii? Health Qual Life Outcomes. 2015;13:148. doi: 10.1186/s12955-015-0351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saylor K, Blackstock C. Many hands, one dream: healthy Aboriginal children and young people. Paediatr Child Health. 2005;10:523–4. doi: 10.1093/pch/10.9.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandler MJ, Lalonde CE. Cultural continuity as a moderator of suicide risk among Canada’s First Nations. In: Kirmayer L, Valaskakis G, editors. Healing Traditions: The Mental Health of Aboriginal Peoples in Canada. Vancouver: University of British Columbia Press; 2008. pp. 221–48. [Google Scholar]
- 25.Hill DL. Sense of belonging as connectedness, American Indian worldview, and mental health. Arch Psychiatr Nurs. 2006;20:210–6. doi: 10.1016/j.apnu.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Isaak CA, Marchessault G. Meaning of health: the perspectives of Aboriginal adults and youth in a northern Manitoba First Nations community. Can J Diabetes. 2008;32:114–22. doi: 10.1016/S1499-2671(08)22008-3. [DOI] [PubMed] [Google Scholar]
- 27.Waldram JB, Herring DA, Young TK. Aboriginal health in Canada Historical, cultural and epidemiological perspectives. 2nd ed. Toronto: University of Toronto Press; 2006. pp. 1–352. [Google Scholar]
- 28.Usuba K, Russell J, Ritchie SD, et al. Evaluating the Outdoor Adventure Leadership Experience (OALE) program using the Aboriginal Children’s Health and Well-being Measure (ACHWM©) Journal of Outdoor and Environmental Education. 2019;22:187–97. [Google Scholar]
- 29.Barbic SP, Young NL, Usuba K, et al. Rasch Measurement Theory’s contribution to the psychometric properties of a co-created measure of health and wellness for Indigenous children and youth. J Clin Epidemiol. 2022;151:18–28. doi: 10.1016/j.jclinepi.2022.07.010. [DOI] [PubMed] [Google Scholar]
- 30.Young NL, Jacko D. Increasing the spread of the ACHWM: Aaniish Naa Gegil — the Children’s Health and Well-being Measure [grant] Ottawa: Health Care Policy and Strategies Program, Health Canada; 2021. [Google Scholar]
- 31.von Elm E, Altman DG, Egger M, et al. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 32.Young NL, Wabano MJ, Jacko D, et al. Community-based screening and triage versus standard referral of Aboriginal children: a prospective cohort study protocol. Int J Indig Health. 2018;13:65–86. [Google Scholar]
- 33.Young NL, Jacko D, Wabano MJ, et al. A screening mechanism to recognize and support at-risk Aboriginal children. Can J Public Health. 2016;107:e399–403. doi: 10.17269/CJPH.107.5539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schnarch B. Ownership, Control, Access and Possession (OCAP) or self-determination applied to research. A critical analysis of contemporary First Nations research and some options for First Nations communities. J Aborig Health. 2004;1:80–95. [Google Scholar]
- 35.First Nations Information Governance Centre. OCAP: Ownership, Control, Access and Possession sanctioned by the First Nations Information Governance Committee, Assembly of First Nations. Ottawa: National Aboriginal Health Organization; 2007. [Google Scholar]
- 36.Carroll SR, Garba I, Figueroa-Rodríguez O, et al. The CARE principles for Indigenous data governance. Data Sci J. 2020;19:1–12. [Google Scholar]
- 37.McDermott BM, Cobham VE. A stepped-care model of post-disaster child and adolescent mental health service provision. Eur J Psychotraumatol. 2014;5 doi: 10.3402/ejpt.v5.24294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Young NL, Wabano MJ, Usuba K, et al. Wikwemikong children’s health survey report results for the Health Centre (Cycle 1 July 2014) Sudbury (ON): Laurentian University; 2014. [Google Scholar]
- 39.Young NL, Mishibinijima D, Usuba K, et al. Wikwemikong children’s health survey report results for the Health Centre (Cycle 2 July 2015) Sudbury (ON): Laurentian University; 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.