Abstract
Purpose
The purpose of this study was to determine whether a relationship exists between body mass index (BMI), specifically obesity, and surgical outcomes for open carpal tunnel release. Obesity is correlated with increased incidence of carpal tunnel syndrome; however, the effect of obesity on after release recovery has not been examined.
Methods
This study used a retrospective review of patient charts (n = 142). BMI was calculated based on height and weight measurements, and patients were grouped based on their BMI into the following categories: healthy BMI (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), obesity class one (30–34.9 kg/m2) (OB1), obesity class (2 35–39.9 kg/m2) (OB2), or obesity class three (40+ kg/m2) (OB3). Data were then complied on surgical outcomes by assessing preoperative pain, postoperative pain at 2 and 6 weeks, postoperative joint stiffness, wound healing time, and infection status. Data were analyzed using chi-square analyses and multivariable logistic regression to assess the differences in treatment outcomes while controlling for possible confounding variables.
Results
Age at the time of release was found to be inversely correlated with BMI. Healthy BMI patients (n = 19) underwent release at an average age of 59.1 years, whereas OB3 (n = 30) underwent release at an average age of 46.9 years. The odds of improvement in pain were significantly lower in all three obesity groups when compared with healthy BMI at both 2 and 6 weeks after operation.
Conclusions
Our results indicate that obesity may be positively correlated with earlier incidence of carpal tunnel syndrome requiring surgical intervention. These data also indicate the increased rates of postoperative complications in obese patients, particularly patients with OB3. Patients with OB3 need to understand these risks before undergoing open release. Further study should examine the impact of type 2 diabetes on carpal tunnel release recovery.
Clinical relevance
The information included in this study may be used to guide surgeons and patients when considering the effect and potential improvement in outcomes that may come from addressing patient BMI before open carpal tunnel surgery.
Key words: Open carpal tunnel release, Pain, Recovery, Wrist surgery
Carpal tunnel syndrome (CTS) is the most common upper-extremity nerve entrapment resulting in transient and/or permanent sensory and motor deficit and pain.1 CTS causes decreased ability to perform daily tasks associated with a decreased quality of life.2 This disorder is a multifactorial condition with etiologies related to occupation, anatomy, and idiopathic causes.3, 4, 5 Occupational causes include jobs that involve prolonged and repeated wrist flexion, whereas anatomic causes include malformations of the bone or soft tissue near the carpal tunnel.1,4, 5, 6 CTS is believed to result primarily from compression of the median nerve within the carpal tunnel deep to the flexor retinaculum.1,4 Secondarily, compression of arteries that supply this nerve and the surrounding area may limit blood flow and cause further deficit.4,5 Median nerve compression presents as pain or paresthesia in the radial three fingers, weakness in the thenar eminence, and eventual atrophy of the thenar muscles apart from adductor pollicus.6
CTS is typically diagnosed on physical examination using various maneuvers (Phalen maneuver, Tinel’s sign, and median nerve compression test). Although strong evidence exists to support diagnosis using these methods, moderate evidence exists supporting the use of electrodiagnostic testing and nerve imaging in the assistance of this diagnosis.7,8 Initial treatment consists of splinting, physical therapy, improved ergonomics, or corticosteroid injections.9 The treatments most supported by the data, as documented by the American Academy of Orthopaedic Surgeons, are steroid injection and carpal tunnel release (CTR) surgery.8,10 If surgical intervention is used, the procedure is low risk, in an optimized patient, and successfully reduces pain and paresthesia in most patients.11
Risk factors for CTS include sex, diabetes mellitus, family history, age, and trauma to the wrist.3,5,12 Incidence increases in pregnant and breastfeeding women suggest that hormonal differences may explain some CTS variance.13 Increased body mass index (BMI) is also associated with increased rates of CTS in many studies; this may be due to increased adiposity in the wrist, leading to decreased space for the median nerve beneath the flexor retinaculum.12,14,15 In a study, Gunes and Ozeren15 recommended weight loss for individuals experiencing CTS because it may help alleviate some symptoms.16 This study focuses on the relationship between BMI and CTR recovery.
Although the correlation between BMI and CTS is clear, the effect of BMI on CTR recovery has not been clearly defined.7,11,15,17 Due to the high correlation between high BMI and carpal tunnel syndrome incidence, the effects of BMI on CTR recovery must be clarified.17,18 This retrospective study will examine the relationship between BMI and CTR recovery by examining postoperative pain, numbness, and joint stiffness.
Methods
After obtaining institutional review board approval, patient charts from the past 5 years were examined. This study used a retrospective review of patient charts at a major academic medical center. Trauma cases, pregnant women, and individuals younger than 18 of age were excluded due to the known effects on surgical outcomes and trauma-associated CTR presenting a confounding variable. The data included 155 consecutive patient charts; however, 12 patients were excluded due to hand or wrist trauma immediately before CTR. The remaining 143 patients were eligible for the study. The data were extracted from the electronic medical record by one medical student via the visit notes at the two preoperative visits, the operative note, and the two postoperative visits. Any patient who had missing portions of the aforementioned medical records was excluded from the analysis. All procedures consisted of open CTR procedures with patients under general anesthesia or monitored anesthesia care performed by two board-certified orthopedic hand surgeons. The two hand surgeons exclusively performed open CTR under general anesthesia or monitored anesthesia care; therefore, endoscopic CTR procedures and local anesthesia procedures were not included the study.
Body mass index was calculated using height and weight data on the day of the preoperative appointment from patient charts, after which patients were grouped according to the following BMI classification: underweight BMI < 18.4 kg/m2 (n = 0), healthy BMI = 18.5–24.9 kg/m2 (n = 19), overweight BMI = 25–29.9 kg/m2 (n = 27), obesity class 1 (OB1) BMI = 30.0–34.9 kg/m2 (n = 33), obesity class 2 (OB2) BMI = 35.0–39.9 kg/m2 (n = 33), and obesity class 3 (OB3) BMI = 40+ kg/m2 (n = 30). Patient charts were examined for demographic data and comorbidities including diabetes mellitus, hypertension, cardiovascular disease, pulmonary disease, and hypothyroidism. Any patients who underwent multiple procedures in one visit were treated as one case. However, any patients who underwent multiple CTR procedures during separate surgical encounters were treated as distinct cases.
Patients were seen 2 and 6 weeks after CTR because this is standard practice follow-up recommendation for many institutions and surgeons when no complications are noted.19,20 Visual analog scale pain scores for nerve compression pain were recorded at each visit after the attending physician explained the difference between incisional pain and nerve compression pain to the patient. Patients reported any postoperative numbness, qualitative stiffness, or nerve compression pain. Wound time to healing, infection rates, and complications were also examined after surgery.
We used Stata/MP version 17.0 for all analyses. We summarized our sample using descriptive statistics including mean with standard deviation or median with interquartile range for continuous variables and number with percentage for categorical variables. We performed preliminary analyses of the relationships between covariates and BMI using one-way analysis of variance, chi-square, or Fisher’s exact tests.
We performed the Kruskal–Wallis equality of populations rank test to test the hypotheses that postoperative scores of pain, stiffness, and numbness were no different across the categories of BMI. We interpreted the results without ties, which by default assigned the average rank to tied values. We also performed simple ordinal logistic regression or chi-square analyses to test for differences in outcomes across sex, race/ethnicity, diabetic status, hypertensive status, pulmonary disease, cardiovascular disease, hypothyroidism, and participation in postoperative physical therapy. Finally, we performed multivariable ordinal logistic regression to assess differences in the odds of nerve compression pain improvement at 2- and 6-week follow-ups across BMI categories while controlling for possible confounders. We used multivariable logistic regression models to do the same for postoperative stiffness and digital numbness. We elected α = 0.05 a priori as the threshold for statistical significance and calculated 95% confidence intervals to accompany point estimates and P values. The data were powered to .8 in connection with these analyses per industry standard and the recommendation of the facility biostatistician.
The distribution of patients across BMI categories was fairly even with more than 20% of patients in each of the obesity categories (OB1, OB2, and OB3). The healthy BMI category had the fewest patients (13.3%) and was used as the comparison group in regression analyses.
Results
Demographic variables
In total, 143 patients were included in the study with a mean age of 51 years. Most were women (70%) and Caucasian (51%). The mean age at the time of surgery was 51.39 years with a standard deviation of 14.77 years across all groups. The mean age at the time of surgery was significantly younger in OB3 patients when compared with healthy patients (P = .04; Table 1).
Table 1.
The Impact of BMI Classification on Patient Age at the Time of CTR
| Healthy (n = 19) | Overweight (n = 27) | OB1 (n = 33) | OB2 (n = 33) | OB3 (n = 30) | |
|---|---|---|---|---|---|
| Age at CTR (y) | 59.1 | 51.9 | 52.1 | 50 | 46.9 |
Operative outcome variables
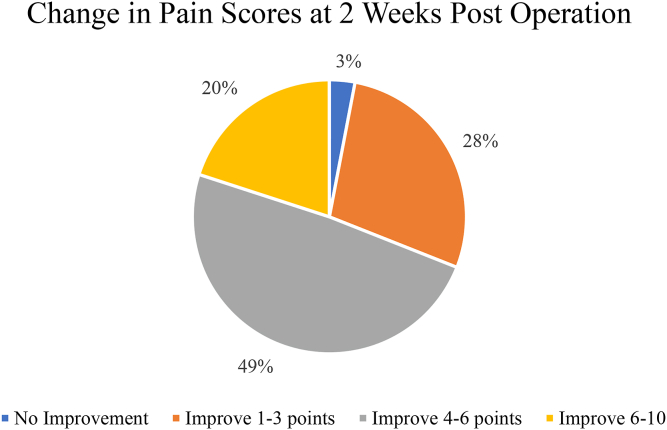
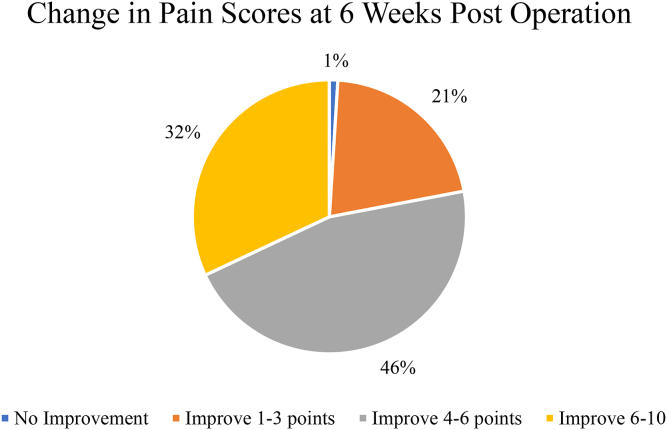
All patients reported 8+/10 nerve compression pain during the preoperative period. At the 2-week follow-up, four (3%) patients reported no improvement in nerve compression pain, whereas 40 (28%) reported an improvement of 1–3 points on a ten-point pain scale. Almost half of the sample reported improvement in nerve compression pain of 4–6 points (n = 70, 48.9%), and 29 (20%) reported an improvement of 6–10 points. At the 6-week follow-up, the trend continued toward improvement. Only one patient (1%) documented no resolution in nerve compression pain, and 46 (32%) patients noted an improvement of 6–10 points from the initial preoperative measurement. The largest proportion of patients reported improvement in nerve compression pain at this time point (n = 66, 46.2%). However, three patients exist with missing information on this outcome at the 6-week follow-up. Finally, 51 (36%) patients reported joint stiffness at follow-up, and 82 (57%) reported digital numbness at the 6-week follow-up appointment (Figs. 1 and 2).
Figure 1.
Changes in pain perception at the 2-week postoperative appointment.
Figure 2.
Changes in pain perception at the 6-week postoperative appointment.
Operative outcome analysis
Postoperative nerve compression pain at the 2-week follow-up
On Kruskal–Wallis analysis, a statistically significant difference was observed in the degree of improvement in pain at the 2-week follow-up across BMI categories. Simple ordinal logistic regression demonstrated no statistically significant differences in the odds of postoperative pain improvement at the 2-week follow-up. Furthermore, patients were grouped by if they attended physical therapy or not by review of the patient chart. A statistically significant increase was observed in the likelihood of pain relief and functionality if the patient had attended and adhered to physical therapy. Of the 143 patients, 79 (55%) attended physical therapy and 64 (45%) patients did not. Given this finding and the significant relationship between BMI category and physical therapy, we included it as a confounder in our multivariable model. Diabetes, cardiovascular disease, pulmonary disease, hypertension, and hypothyroidism were all included as possible confounders in the multivariable analysis.
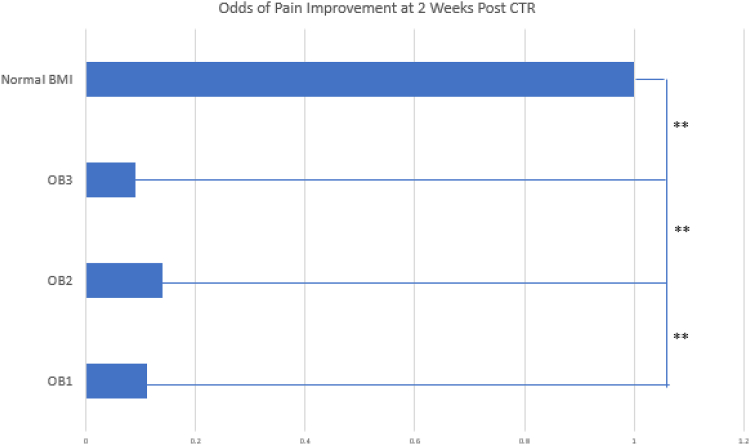
Our multivariable ordinal logistic regression model demonstrated that the odds of improvement in pain were statistically significantly lower in all three obesity categories when compared with healthy BMI patients. Patients in the OB1 group had a 11% chance of achieving the same improvement of pain that the healthy BMI patients had. Additionally, patients in the OB2 group had a 14% chance and the OB3 group had 9% the odds of reaching the same improvement in pain that the healthy BMI group patients had. The healthy group was much more likely to have improvement in postoperative pain when compared with the obese groups. All these analyses controlled for patient participation in physical therapy, which itself was not statistically significant once included in the multivariable model. No statistically significant difference was observed in the odds of improvement in pain at the 2-week follow-up among patients in the overweight category when compared those in the healthy BMI category (Fig. 3).
Figure 3.
This figure illustrates the odds of improvement in pain at the 2-week postoperative appointment. The odds of improvement in the healthy BMI group were set at 1 for reference. ∗∗ indicates P < .005.
Postoperative nerve compression pain at the 6-week follow-up
The results on the Kruskal–Wallis analysis were similar at the 6-weeks follow-up. A statistically significant difference was observed in the degree of improvement for pain across BMI categories. Simple ordinal logistic regression demonstrated no statistically significant difference in the odds of pain improvement at this time point across sexes. However, statistically significant differences exist in the odds of pain improvement among African American patients when compared with Caucasian, as well as across physical therapy groups. We included both variables in our multivariable model.
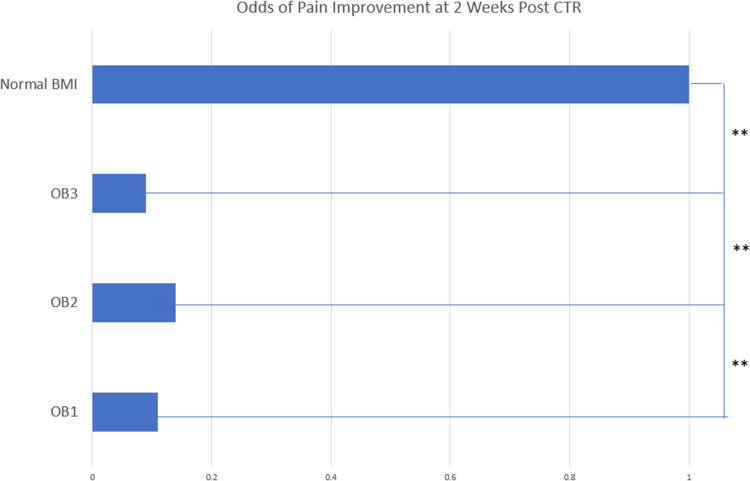
On multivariable ordinal logistic regression, we found that the odds of greater improvement of pain at the 6-week follow-up were statistically significantly lower among patients in the obesity categories compared with healthy BMI when physical therapy participation and race were held constant. Patients in the OB1 group had 17% odds of reaching the same level of pain that the healthy BMI group attained, whereas OB2 patients had 10% odds. The odds of improvement were the lowest in the OB3 group at 6% when compared with the healthy BMI group. Finally, African American patients had significantly lower odds to have full function and no pain after surgery. No statistically significant difference was observed in the odds of improvement among patients in the Hispanic group (compared with Caucasian) or among those who were categorized as overweight (compared with those with healthy BMI) (Fig. 4).
Figure 4.
This figure illustrates the odds of improvement in pain at the 6-week postoperative appointment. The odds of improvement in the healthy BMI group were set at 1 for reference. ∗∗ indicates P < .005.
Postoperative joint stiffness
Analysis with the Kruskal–Wallis test demonstrated a statistically significant difference in postoperative joint stiffness across BMI categories. After controlling for physical therapy participation, a statistically significant difference in the odds of postoperative joint stiffness among patients in the OB3 group when compared with healthy BMI was found. The odds were not significantly higher for joint stiffness in patients in the overweight, OB1, or OB2 groups when controlling for physical therapy participation. However, data may be confounded due to physician physical therapy referral patterns. Joint stiffness was also reported by the patient to the physician at the 6-week postoperative appointment, and therefore, it is not quantifiable (Table 2).
Table 2.
Rates of Postoperative Joint Stiffness 6 Weeks After Operation
| Healthy (n = 19) | Overweight (n = 27) | OB1 (n = 33) | OB2 (n = 33) | OB3 (n = 30) | |
|---|---|---|---|---|---|
| Postoperative stiffness | 15% | 19% | 33% | 39% | 61% |
Postoperative digital numbness
Similar to postoperative joint stiffness, we found a statistically significant difference in postoperative digital numbness across BMI categories on simple Kruskal–Wallis analysis at 6 weeks after operation. No statistical differences were observed in postoperative numbness occurrence across sexes or race/ethnicities, although a statistically significant difference was noted across physical therapy groups. We found that the odds of postoperative numbness were statistically significantly higher in all three obesity groups. The odds of postoperative digital numbness among patients in the OB1 and OB2 groups were 10.27 and 6.23 times higher than those in the healthy BMI category, respectively. The OB3 group was 30.66 times more likely than the healthy group to have postoperative numbness.
Discussion
This analysis indicates that patients with obesity, particularly class 3 obesity, are more likely to experience poorer surgical outcomes immediately after CTR. This may be seen from our data that were powered to show an increased incidence of postoperative numbness, decreased rates of nerve compression pain relief, and increased rates of wrist stiffness. Our data also showed that obese patients begin to experience CTS symptoms at a younger age when compared with healthy weight controls. Although it was previously known that BMI is associated with increased rates of CTS and that weight loss would be the greatest preventative care, this study further illustrates the importance of promoting healthy BMIs in a clinical setting before open CTR. These data points suggest that aspects of obesity contribute to poorer recovery suggesting causes beyond the scope of this study.
Although we acknowledge that our population might provide insights into the potential effect on a greater population, the external validity is unknown. Additionally, because data were only collected 6 weeks after surgery, we recognize that full healing might not have occurred. Nerve conduction tests were also not performed, which could present a source of error. Although obese patients might experience worse symptoms initially after surgery, these patients might have achieved similar results to lower BMI groups a year after surgery. We additionally note that not all possible variables that affect CTR outcomes were included in this analysis. Details on workers’ compensation and mental illness were not gathered. Further studies can evaluate the impact of other comorbidities and conditions that affect surgical outcomes.
Our study shows an increased risk of negative postoperative outcomes in higher BMI populations, suggesting that this may be important to take note of before attempting such an approach for treatment of CTS. We recognize that no patient should be turned away from surgery on account of their weight but instead informed of all the possibilities available that may provide the best outcome. From these results, we conjecture that depending on the severity of symptoms, it may be beneficial for overweight patients who present with mild CTS to receive counseling on the potential for improvement in symptomatology that could stem from weight loss. Taking these data into account may lead surgeons to consider the effect and potential improvement in outcomes that may come from addressing patient weight before surgery. This postponement could alleviate symptoms and avoid the risk of adverse surgical outcomes associated with high BMI.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly to this article.
References
- 1.Miyamoto H., Morizaki Y., Kashiyama T., Tanaka S. Grey-scale sonography and sonoelastography for diagnosing carpal tunnel syndrome. World J Radiol. 2016;8(3):281–287. doi: 10.4329/wjr.v8.i3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atroshi I., Gummesson C., Johnsson R., Sprinchorn A. Symptoms, disability, and quality of life in patients with carpal tunnel syndrome. J Hand Surg Am. 1999;24(2):398–404. doi: 10.1016/s0363-5023(99)70014-6. [DOI] [PubMed] [Google Scholar]
- 3.Genova A., Dix O., Saefan A., Thakur M., Hassan A. Carpal tunnel syndrome: a review of literature. Cureus. 2020;12(3) doi: 10.7759/cureus.7333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Razavi A.S., Karimi N., Bashiri F. The relationship of serum lipid profiles and obesity with the severity of carpal tunnel syndrome. Pan Afr Med J. 2021;39:90. doi: 10.11604/pamj.2021.39.90.27234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kokubo R., Kim K. [Carpal Tunnel Syndrome:Diagnosis and Treatment] No Shinkei Geka. 2021;49(6):1306–1316. doi: 10.11477/mf.1436204516. [DOI] [PubMed] [Google Scholar]
- 6.Wipperman J., Goerl K. Carpal tunnel syndrome: diagnosis and management. Am Fam Physician. 2016;94(12):993–999. [PubMed] [Google Scholar]
- 7.Padua L., Coraci D., Erra C., et al. Carpal tunnel syndrome: clinical features, diagnosis, and management. Lancet Neurol. 2016;15(12):1273–1284. doi: 10.1016/S1474-4422(16)30231-9. [DOI] [PubMed] [Google Scholar]
- 8.Management of Carpal Tunnel Syndrome Evidence-Based Clinical Practice Guidelines. American Academy of Orthopaedic Surgeons.
- 9.Viera A.J. Management of carpal tunnel syndrome. Am Fam Physician. 2003;68(2):265–272. [PubMed] [Google Scholar]
- 10.Green D.P., MacKay B.J., Seiler S.J., Fry M.T. Accuracy of carpal tunnel injection: a prospective evaluation of 756 patients. Hand (N Y) 2020;15(1):54–58. doi: 10.1177/1558944718787330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang L. Guiding treatment for carpal tunnel syndrome. Phys Med Rehabil Clin N Am. 2018;29(4):751–760. doi: 10.1016/j.pmr.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 12.Lampainen K., Shiri R., Auvinen J., Karppinen J., Ryhanen J., Hulkkonen S. Weight-related and personal risk factors of carpal tunnel syndrome in the Northern Finland birth cohort 1966. J Clin Med. 2022;11(6):1510. doi: 10.3390/jcm11061510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nordstrom D.L., Vierkant R.A., DeStefano F., Layde P.M. Risk factors for carpal tunnel syndrome in a general population. Occup Environ Med. 1997;54(10):734–740. doi: 10.1136/oem.54.10.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nageeb R.S., Shehta N., Nageeb G.S., Omran A.A. Body mass index and vitamin D level in carpal tunnel syndrome patients. Egypt J Neurol Psychiatr Neurosurg. 2018;54(1):14. doi: 10.1186/s41983-018-0009-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gunes M., Ozeren E. Effect of age and body mass index on surgical treatment outcomes in patients with carpal tunnel syndrome. Turk Neurosurg. 2021;31(1):83–87. doi: 10.5137/1019-5149.JTN.29704-20.2. [DOI] [PubMed] [Google Scholar]
- 16.Adebayo P.B., Mwakabatika R.E. F-wave parameters and body mass index in carpal tunnel syndrome. Brain Behav. 2021;11(4) doi: 10.1002/brb3.2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gundlach B.K., Robbins C.B., Lawton J.N., Lien J.R. Wound healing complications in diabetic patients undergoing carpal tunnel and trigger finger releases: a retrospective cohort study. J Hand Surg Am. 2021;46(12):1057–1063. doi: 10.1016/j.jhsa.2021.05.009. [DOI] [PubMed] [Google Scholar]
- 18.Wall J.C., Jr., Wall H.P., Osemwengie B.O., MacKay B.J. The impact of obesity on orthopedic upper extremity surgery. Orthop Clin North Am. 2018;49(3):345–351. doi: 10.1016/j.ocl.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 19.Ratzon N., Schejter-Margalit T., Froom P. Time to return to work and surgeons’ recommendations after carpal tunnel release. Occup Med (Lond) 2006;56(1):46–50. doi: 10.1093/occmed/kqi194. [DOI] [PubMed] [Google Scholar]
- 20.Open Carpal Tunnel Release Post-Op Guidelines . UVA Hand Center-Therapy. University of Virginia School of Medicine; 2015. [Google Scholar]