Abstract
Objective
To investigate symptomatic and preventive medication use according to age and frailty in Australian and Japanese nursing homes (NHs).
Methods
Secondary cross-sectional analyses of two prospective cohort studies involving 12 Australian NHs and four Japanese NHs. Frailty was measured using the FRAIL-NH scale (non-frail 0–2; frail 3–6; most-frail 7–14). Regular medications were classified as symptomatic or preventive based on published lists and expert consensus. Descriptive statistics were used to compare the prevalence and ratio of symptomatic to preventive medications.
Results
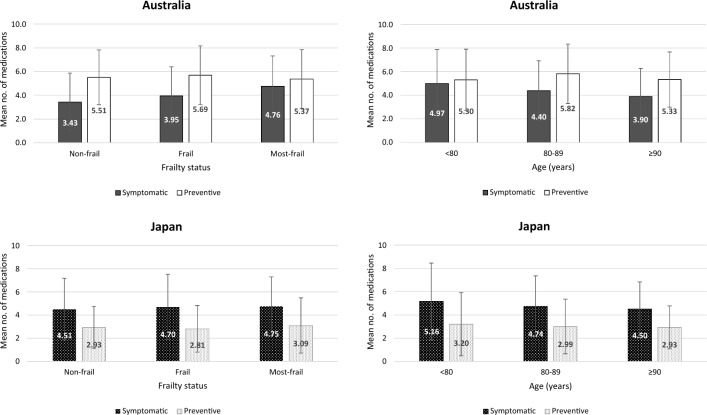
Overall, 550 Australian residents (87.7 ± 7.3 years; 73.3% females) and 333 Japanese residents (86.5 ± 7.0 years; 73.3% females) were included. Australian residents used a higher mean number of medications than Japanese residents (9.8 ± 4.0 vs 7.7 ± 3.7, p < 0.0001). Australian residents used more preventive than symptomatic medications (5.5 ± 2.5 vs 4.3 ± 2.6, p < 0.0001), while Japanese residents used more symptomatic than preventive medications (4.7 ± 2.6 vs 3.0 ± 2.2, p < 0.0001). In Australia, symptomatic medications were more prevalent with increasing frailty (non-frail 3.4 ± 2.6; frail 4.0 ± 2.6; most-frail 4.8 ± 2.6, p < 0.0001) but less prevalent with age (< 80 years 5.0 ± 2.9; 80–89 years 4.4 ± 2.6; ≥ 90 years 3.9 ± 2.5, p = 0.0042); while preventive medications remained similar across age and frailty groups. In Japan, there was no significant difference in the mean number of symptomatic and preventive medications irrespective of age and frailty.
Conclusions
The ratio of symptomatic to preventive medications was higher with increasing frailty but lower with age in Australia; whereas in Japan, the ratio remained consistent across age and frailty groups. Preventive medications remained prevalent in most-frail residents in both cohorts, albeit at lower levels in Japan.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40520-023-02600-x.
Keywords: Aged, Frailty, Nursing home, Polypharmacy, Medication review, Deprescribing
Introduction
Frailty is a state of reduced physiological reserve characterized by an increased vulnerability to medication-related harm and adverse outcomes including falls, delirium, and hospitalization [1]. Frailty may act as an effect modifier by modifying the risks and benefits of chronic medications [2]. It is estimated that over three quarters of residents in nursing homes (NHs) are frail [3]. Prescribing in this population is often guided by recommendations from disease-specific clinical guidelines that are based on research conducted in robust adults [2, 4, 5]. These recommendations are often extrapolated to NH settings despite residents being underrepresented or excluded from clinical trials [6]. This may expose residents to potential medication-related harm [2]. Prescribing in this setting is further complicated by the presence of complex multimorbidity and polypharmacy [1, 5].
A systematic review reported that residents of NHs received an average of 3.8–16.6 medications daily with a wide range in prevalence of symptomatic and preventive medications [7]. Gastrointestinal agents, diuretics, and analgesics were among the most prescribed medications [7]. As frailty progresses, residents’ goals of care may shift from chronic disease prevention to prioritize comfort-oriented care with management of symptoms to maintain quality of life [2, 8]. Optimizing medication management in this population involves balancing the use of symptomatic and preventive medications [2, 6]. There is increasing interest in frailty screening to identify residents who are most susceptible to adverse drug events and may benefit from a medication review [1, 5]. Incorporating frailty screening into medication review is consistent with international guidelines that recommend regular reassessment of the risk-to-benefit profile of individual regimens [1, 4, 5].
Existing studies examining patterns of symptomatic and preventive medication use have focused on people with advanced dementia in hospital and palliative care settings [9–11]. A European cross-sectional study of 4121 residents found that frailty was associated with higher prevalence of symptomatic medications (e.g., laxatives, analgesics), while preventive medications (e.g., bisphosphonates, vitamin D) were more prevalent among non-frail residents [12]. Despite recognition that transitions in frailty status may influence prescribing decisions, there is a lack of non-European studies comparing symptomatic and preventive medication use in the context of frailty. The objective of this study was to investigate the use of symptomatic and preventive medications according to age and frailty among residents of Australian and Japanese NHs.
Methods
Study design
This was a secondary cross-sectional analyses of baseline data collected from two independent prospective cohort studies in Australia and Japan. Both countries have an aging population for which optimizing medication management in long-term care has been identified as a policy priority [13, 14].
Settings
Residential aged care services (RACS) in Australia, synonymous with NHs or long-term care facilities (LTCFs) in other countries, provide care and supported accommodation for people who can no longer live independently at home [15]. Medications are prescribed by general practitioners (GPs) who attend the RACS periodically but are not directly employed by aged care providers [15]. Medications are dispensed and packed by off-site community pharmacists into dose administration aids (e.g., multi-dose drug dispensing, blister packs) to facilitate administration by credentialed aged care staff [15].
Special NHs or Tokuyo in Japan are similar to RACS in Australia (i.e., permanent residence for adults with high long-term care needs). In contrast to Australia, medications are prescribed by primary care physicians who are contracted by the NHs. Community pharmacists dispense the medications and nursing staff manage the administration of medications. Medication cost is subsidized for residents in both countries.
Data collection
In Australia, data were collected as part of the Frailty In Residential Sector over Time (FIRST) study, a prospective cohort study involving 12 RACS in South Australia [16]. All 12 RACS were operated by a large not-for-profit aged care provider. Residents staying for eight weeks or more were eligible to participate. Residents with a life expectancy of less than three months and those not capable of completing baseline assessments in English were excluded. Baseline data were collected from March to October 2019 by trained registered nurses. Comorbidities were based on documented diagnoses drawn from resident records. Activities of daily living (ADL) was assessed using Katz ADL [17]. Cognitive status was assessed using the Dementia Severity Rating Scale (DSRS) irrespective of dementia diagnosis [18]. Supplementary Table 1 details the full description of the scales. Of the 561 Australian residents included in the cohort study, 550 residents completed baseline assessments. The cohort was comparable to the average Australian NH population in terms of age (88 vs 85 years) and sex (73% vs 66%) [19].
In Japan, data were collected from a prospective cohort study involving four NHs located in Tokyo and Kanagawa prefecture. All four NHs were serviced by a large hospital and LTCF group. Residents were invited by NH staff to participate in the study. Residents receiving medications from other hospitals or clinics, and those with incomplete medication records were excluded. Baseline data were collected from October to December 2020 by trained NH staff. Comorbidities were based on documented diagnoses drawn from resident records. ADL was assessed using the Japanese "Independence in Daily Living in Older People with Disabilities" scale [20]. Cognitive status was assessed using the Japanese "Independence in Daily Living in Older People with Dementia" scale [21]. Of the 372 Japanese residents included in the cohort study, 333 residents completed baseline assessments. The cohort was comparable to the average Japanese NH population in terms of age (87 vs 86 years) and sex (73% vs 78%) [22].
Frailty assessment
Frailty status was assessed using the FRAIL-NH scale in both Australia (English version) [23] and Japan (Japanese version) [24]. FRAIL-NH has been previously translated and back-translated into Japanese [24]; both versions are identical apart from the language [3]. Both the Australian and Japanese cohorts used the same seven FRAIL-NH domains (fatigue, resistance, ambulation, incontinence, loss of weight, nutritional approach, and help with dressing) to calculate residents’ frailty scores. Each domain is assigned a score of 0–2 points, with a total score ranging from 0 to 14. FRAIL-NH has similar predictive properties to Fried’s phenotype and Frailty Index [3]. The scale has been shown to be predictive of adverse outcomes including falls, hospitalization, and mortality among residents of NHs [3]. The same frailty categories were used for both cohorts: non-frail (0–2); frail (3–6); and most-frail (7–14). These cut-offs were previously established using receiver operating characteristic curves to determine the FRAIL-NH score that maximized sensitivity and specificity in predicting frailty based on Frailty Index [16]. Using the same FRAIL-NH domains and cut-offs in Australia and Japan facilitated comparison between cohorts and frailty groups.
Medications
Data on all regular medications including oral, inhaled, topical, parenteral, dietary, and herbal supplements were extracted. The following data were recorded: active ingredient, strength, dose, frequency, and formulation. In Australia, data were extracted from residents’ regular medication charts which provide the most current medication administration records. The overall quality and accuracy of data entries were individually reviewed and evaluated by the research team. In Japan, medication dispensing data were extracted from electronic health records. Medications were coded according to their Anatomical Therapeutic Chemical (ATC) classifications [43]. Different strengths of the same medication, or combination medications that share a single ATC code were counted as one medication. Pro re nata (PRN) or as needed medications were not included.
Medications were categorized as symptomatic or preventive based on published lists and international expert consensus among four clinical pharmacists, two geriatricians, and a pharmacoepidemiologist [9, 10, 25, 26]. All medications were categorized using the same consensus list (Supplementary Table 2). Symptomatic medications were defined as medications predominantly used for comfort or symptom control (including medications used for the prophylaxis of short-term or acute events not associated with death [e.g., urinary tract infection]). Preventive medications were defined as medications predominantly used for long-term prevention or worsening of a disease or condition (including medications used for primary or secondary prevention of death/events associated with death [e.g., stroke]).
Statistical analysis
Resident characteristics were presented as frequencies with percentages and means with standard deviations (SD). Categorical variables were compared using chi-square tests and continuous variables were compared using independent t-tests. Descriptive statistics were used to compare the prevalence and ratio of symptomatic to preventive medications stratified by age and frailty. One-way analysis of variance (ANOVA) was used to determine differences in mean number of medications between age and frailty groups. We performed a sensitivity analysis by excluding Japanese residents who died within three months of baseline data collection. This was because the Australian cohort did not include residents with an estimated life expectancy of less than three months. Statistical significance was set at p < 0.05. Analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) in Australia and Stata 17 (Stata Corp., College Station, TX) in Japan.
Ethical considerations
The Australian study was approved by the University of Adelaide Human Research Ethics Committee (H-2018-247), South Australian Department for Health and Wellbeing Human Research Ethics Committee (HREC/20/SAH/15), Department of Human Services External Request Evaluation Committee (EREC/RMS0432), and Monash University Human Research Ethics Committee (23620). The Japanese study was approved by the ethical review board of the Institute for Health Economics and Policy, Japan (R2-002). Written informed consent was obtained from all residents or their next-of-kin.
Results
In total, 550 Australian residents (87.7 ± 7.3 years; 73.3% female) and 333 Japanese residents (86.5 ± 7.0 years; 73.3% female) were included in the data analysis (Table 1). The mean FRAIL-NH scores were 6.3 ± 3.2 in Australia and 7.3 ± 3.6 in Japan (p < 0.0001). Both Australia and Japan had similar proportions of non-frail residents (12.4% vs 12.9%). In Australia, the proportion of frail and most-frail residents were evenly distributed (42.0% vs 45.6%); whereas in Japan, there were considerably more residents who were most-frail than frail (61.9% vs 25.2%). In Australia, there was a higher proportion of most-frail residents among those aged < 80 years (57.9%) compared to those aged 80–89 years (42.5%) and ≥ 90 years (44.7%) (Supplementary Fig. 1). Prevalence of dementia was similar across age groups (34.0–39.5%) but was higher among most-frail (48.8%) compared to non-frail (20.6%) and frail (28.8%) residents in the Australian cohort. In Japan, the proportion of most-frail residents ranged from 57.8 to 65.9% across age groups. Prevalence of dementia was higher with age (55.6% in < 80 years; 70.3% in 80–89 years; 74.8% in ≥ 90 years) and frailty (55.8% in non-frail; 64.3% in frail; 75.2% in most-frail) in the Japanese cohort.
Table 1.
Baseline characteristics of residents
| Characteristics | Australia (n = 550) | Japan (n = 333) | p-value |
|---|---|---|---|
| Age, mean (SD) | 87.7 (7.3) | 86.5 (7.0) | 0.02 |
| < 80 years, n (%) | 76 (13.8) | 45 (13.5) | |
| 80–89 years, n (%) | 228 (41.5) | 165 (49.5) | |
| ≥ 90 years, n (%) | 246 (44.7) | 123 (36.9) | |
| Sex, n (%) | 1.00 | ||
| Female | 403 (73.3) | 244 (73.3) | |
| Male | 147 (26.7) | 89 (26.7) | |
| Comorbidities, n (%)a | |||
| Coronary heart disease | 155 (28.3) | 39 (11.7) | < 0.0001 |
| Stroke | 161 (29.4) | 118 (35.4) | 0.06 |
| Dementia | 202 (36.9) | 233 (70.0) | < 0.0001 |
| Diabetes | 131 (23.9) | 74 (22.2) | 0.59 |
| Polypharmacy (≥ 9 meds), n (%) | 332 (60.4) | 137 (41.1) | < 0.0001 |
| No. of medications, mean (SD) | 9.8 (4.0) | 7.7 (3.7) | < 0.0001 |
| Symptomatic | 4.3 (2.6) | 4.7 (2.6) | 0.01 |
| Preventive | 5.5 (2.5) | 3.0 (2.2) | < 0.0001 |
| FRAIL-NH score, mean (SD) | 6.3 (3.2) | 7.3 (3.6) | < 0.0001 |
| Non-frail (0–2), n (%) | 68 (12.4) | 43 (12.9) | |
| Frail (3–6), n (%) | 231 (42.0) | 84 (25.2) | |
| Most-frail (7–14), n (%) | 251 (45.6) | 206 (61.9) | |
| Activities of daily living (ADL), n (%)b,c | |||
| Moderately/fully independent | 7 (1.3) | 7 (2.1) | N/A |
| Not independent | 543 (98.7) | 326 (97.9) | N/A |
| Cognitive status, n (%)d,e | |||
| No/minimal impairment | 133 (24.2) | 102 (30.6) | N/A |
| Cognitive impairment | 417 (75.8) | 231 (69.4) | N/A |
N/A not applicable; SD standard deviation
Full description of scales available in Supplementary Table 1
aAustralia: data available for n = 547 only
bAustralia: Katz ADL (Not independent 0–2; Moderately/fully independent 3–6)
cJapan: "Independence in Daily Living in Older People with Disabilities" [Japanese original scale] (Not independent: Ranks A, B and C; Moderately/fully independent: Rank J)
dAustralia: Dementia Severity Rating Scale (DSRS) (No/minimal impairment 0–11; Cognitive impairment 12–54)
eJapan: "Independence in Daily Living in Older People with Dementia" [Japanese original scale] (No impairment: Independent, Ranks I and II; Cognitive impairment: Ranks III, IV and M)
Overall, Australian residents used a higher mean number of medications than Japanese residents (9.8 ± 4.0 vs 7.7 ± 3.7, p < 0.0001). Australian residents used more preventive than symptomatic medications (5.5 ± 2.5 vs 4.3 ± 2.6, p < 0.0001), while Japanese residents used more symptomatic than preventive medications (4.7 ± 2.6 vs 3.0 ± 2.2, p < 0.0001). In Australia, the mean number of symptomatic medications was higher with increasing frailty (non-frail 3.4 ± 2.6; frail 4.0 ± 2.6; most-frail 4.8 ± 2.6, p < 0.0001) but lower with age (< 80 years 5.0 ± 2.9; 80–89 years 4.4 ± 2.6; ≥ 90 years 3.9 ± 2.5, p = 0.0042), while preventive medications remained similar across age and frailty groups (Supplementary Table 3a). This corresponded to a higher ratio of symptomatic to preventive medications among frailer Australian residents (non-frail 0.62; frail 0.69; most-frail 0.89) (Fig. 1), but a lower ratio with age (< 80 years 0.94; 80–89 years 0.76; ≥ 90 years 0.73). In Japan, there was no significant difference in the mean number of symptomatic and preventive medications across age and frailty groups. Consequently, the ratio of symptomatic to preventive medications was largely consistent across age and frailty groups in Japan (1.54–1.67).
Fig. 1.
Mean number of symptomatic and preventive medications according to frailty status and age
Symptomatic medications
The most prevalent medication classes stratified by age and frailty are presented in Table 2. Among symptomatic medications, paracetamol (69.1%), proton pump inhibitors (PPIs) (46.0%), and contact laxatives (32.9%) were most prevalent in Australia; while osmotic laxatives (56.5%), PPIs (44.4%), and contact laxatives (33.9%) were most prevalent in Japan. The top five medications within each country were similar across age and frailty groups although variations in the prevalence were observed. Paracetamol use was more prevalent among frailer Australian residents (non-frail 60.3%, frail 63.6%, most-frail 76.5%), while the overall prevalence among Japanese residents was only 3.6%. PPIs were most prevalent among non-frail (48.5%) compared to frail (47.2%) and most-frail (44.2%) Australian residents; whereas the opposite was observed in Japan (non-frail 34.9%; frail 33.3%; most-frail 51.0%). Buprenorphine patches and pregabalin were only prevalent in non-frail Australian residents, while benzodiazepines were only prevalent in Australian residents > 80 years. Yokukansan (Japanese herbal medication [Kampo] commonly used for behavioral and psychological symptoms of dementia) [27] was only prevalent in non-frail Japanese residents, while Z-drugs were only prevalent in frail Japanese residents.
Table 2.
Most prevalent medication classes stratified by frailty status and age
| Medications (Prevalence, %) | ||
|---|---|---|
| Australia | Japan | |
| Symptomatic | ||
| Overall | Paracetamol (69.1) | Osmotic laxative (56.5) |
| PPI (46.0) | PPI (44.4) | |
| Contact laxative (32.9) | Contact laxative (33.9) | |
| Ocular lubricant (27.3) | White petrolatum (32.7) | |
| Osmotic laxative (26.5) | Topical heparinoid (27.9) | |
| Frailty status | ||
| Non-Frail | Paracetamol (60.3) | Osmotic laxative (65.1) |
| PPI (48.5) | PPI; Contact laxative (34.9) | |
| Ocular lubricant (23.5) | White petrolatum (32.6) | |
| Contact laxative (20.6) | Topical heparinoid (30.2) | |
| Buprenorphine patch; Pregabalin & derivativesa (14.7) | Yokukansan (14.0) | |
| Frail | Paracetamol (63.6) | Osmotic laxative (56.0) |
| PPI (47.2) | Topical heparinoid (38.1) | |
| Ocular lubricant (25.1) | PPI; Contact laxative (33.3) | |
| Contact laxative (23.4) | White petrolatum (29.8) | |
| Osmotic laxative (21.6) | Z-drug (16.7) | |
| Most-frail | Paracetamol (76.5) | Osmotic laxative (54.9) |
| Contact laxative (45.0) | PPI (51.0) | |
| PPI (44.2) | Contact laxative; White petrolatum (34.0) | |
| Osmotic laxative (36.3) | Topical heparinoid (23.3) | |
| Ocular lubricant (30.3) | GI stimulant; Probiotic (17.5) | |
| Age (years) | ||
| < 80 | Paracetamol (68.4) | Osmotic laxative (46.7) |
| PPI (47.4) | PPI (44.4) | |
| Contact laxative (34.2) | White petrolatum (40.0) | |
| Osmotic laxative (32.9) | Topical heparinoid (35.6) | |
| Benzodiazepine (25.0) | Contact laxative (20.0) | |
| 80–89 | Paracetamol (67.5) | Osmotic laxative (59.4) |
| PPI (51.3) | PPI (43.6) | |
| Contact laxative (34.6) | Contact laxative; White petrolatum (33.3) | |
| Ocular lubricant (25.9) | Topical heparinoid (29.1) | |
| Osmotic laxative (21.9) | GI stimulant; Probiotic (14.5) | |
| ≥ 90 | Paracetamol (70.7) | Osmotic laxative (56.1) |
| PPI (40.7) | PPI (45.5) | |
| Contact laxative (30.9) | Contact laxative (39.8) | |
| Ocular lubricant (30.1) | White petrolatum (29.3) | |
| Osmotic laxative (28.9) | Topical heparinoid (23.6) | |
| Medications (Prevalence, %) | ||
|---|---|---|
| Australia | Japan | |
| Preventive | ||
| Overall | Vitamin D (52.0) | CCB (36.6) |
| Antiplatelet (40.0) | Antiplatelet (24.3) | |
| Statin (33.6) | Loop diuretic (19.2) | |
| Loop diuretic (31.1) | Anticholinesterase (17.4) | |
| Beta-blocker (26.2) | ARB (17.1) | |
| Frailty status | ||
| Non-Frail | Statin (52.9) | CCB (37.2) |
| Vitamin D (47.1) | Antiplatelet (20.9) | |
| Antiplatelet (38.2) | Thyroid hormone (16.3) | |
| Beta-blocker (32.4) | Statin; Loop diuretic (14.0) | |
| Loop diuretic (30.9) | Vitamin D; Vitamin B12; Xanthine oxidase inhibitor (11.6) | |
| Frail | Vitamin D (50.2) | CCB (41.7) |
| Antiplatelet (44.2) | Antiplatelet (22.6) | |
| Statin (36.8) | Anticholinesterase; ARB (19.0) | |
| Loop diuretic (34.2) | Potassium (14.3) | |
| Beta-blocker (28.6) | Loop diuretic (13.1) | |
| Most-frail | Vitamin D (55.0) | CCB (34.5) |
| Antiplatelet (36.7) | Antiplatelet (25.7) | |
| Loop diuretic (28.3) | Loop diuretic (22.8) | |
| Statin (25.5) | Anticholinesterase (18.4) | |
| SSRI (23.9) | ARB (18.0) | |
| Age (years) | ||
| < 80 | Vitamin D (61.8) | Antiplatelet (31.1) |
| Statin (44.7) | CCB (26.7) | |
| Antiplatelet (36.8) | Anticholinesterase; ARB (17.8) | |
| SNRI and mirtazapine (23.7) | Direct factor Xa inhibitor; Valproate (15.6) | |
| Loop diuretic; SSRI (21.1) | Statin (13.3) | |
| 80–89 | Vitamin D (46.5) | CCB (38.8) |
| Antiplatelet (40.8) | Antiplatelet (22.4) | |
| Statin (39.9) | Loop diuretic (16.4) | |
| Loop diuretic (32.5) | Anticholinesterase; ARB (15.8) | |
| Beta-blocker (29.8) | Statin (11.5) | |
| ≥ 90 | Vitamin D (54.1) | CCB (37.4) |
| Antiplatelet (40.2) | Loop diuretic (27.6) | |
| Loop diuretic (32.9) | Antiplatelet (24.4) | |
| Beta-blocker (27.6) | Anticholinesterase (19.5) | |
| Statin (24.4) | ARB (18.7) | |
aDerivatives include levetiracetam, lamotrigine, topiramate (N03AX); ARB, angiotensin II receptor blocker (C09CA); CCB, dihydropyridine calcium channel blocker (C08CA); GI stimulant, gastrointestinal stimulant (A03FA); PPI, proton pump inhibitor (A02BC); SNRI, selective noradrenaline reuptake inhibitor (N06AX); SSRI, selective serotonin reuptake inhibitor (N06AB); Yokukansan, traditional Japanese herbal medication for changed behaviors. Full list of ATC codes used available in Supplementary Table 4
Preventive medications
Among preventive medications, vitamin D supplements (52.0%), antiplatelets (40.0%), and statins (33.6%) were most prevalent in Australia; while dihydropyridine calcium channel blockers (CCBs) (36.6%), antiplatelets (24.3%), and loop diuretics (19.2%) were most prevalent in Japan. In Australia, a consistent pattern was observed whereby statins, vitamin D, antiplatelets, and loop diuretics were among the top preventive medications across age and frailty groups. In contrast, the overall prevalence of statins and vitamin D in Japan was only 9.4% and 8.1%, respectively. In Japan, a consistent pattern was also observed whereby CCBs, antiplatelets, and loop diuretics were among the top preventive medications across age and frailty groups. Japanese residents were more commonly prescribed CCBs, while Australian residents were more commonly prescribed beta-blockers. Anticholinesterase use was only prevalent among frail (19.0%) and most-frail (18.4%) Japanese residents. Conversely, overall prevalence of anticholinesterase use (8.0%) was minimal in Australia.
Sensitivity analysis
In the sensitivity analysis excluding 10 (3.0%) Japanese residents who died within three months of baseline data collection, there remained no significant difference in the mean number of symptomatic and preventive medication use in all age and frailty groups (Supplementary Table 3b). The ratio of symptomatic to preventive medications in the adjusted analysis (1.52–1.67) was similar to the main analysis (1.54–1.67) across age and frailty groups in Japan.
Discussion
This is the first study to compare symptomatic and preventive medication use according to age and frailty in Australian and Japanese NHs. Overall, Australian residents used a higher mean number of medications than Japanese residents. Australian residents used more preventive than symptomatic medications, while the opposite was observed for Japanese residents. Preventive medications were prevalent across all age and frailty groups in both cohorts. The ratio of symptomatic to preventive medications was higher with increasing frailty in Australia but was consistent irrespective of frailty status in Japan.
In Australia, symptomatic medication use was more prevalent with higher frailty levels but less prevalent with advanced age; whereas in Japan, symptomatic medication use was similar across age and frailty groups. Australian findings were in line with a European study that reported a higher prevalence of symptomatic medications among residents who were frail compared to non-frail [12]. This may be because clinicians gave greater consideration to frailty than chronological age in their treatment decision-making. Clinicians may prioritize symptom control over intensive treatment of chronic diseases in frail and most-frail residents. While frailty is characterized by an age-related decline in physiological systems, frailty and age are not synonymous [1, 2]. Frailty may be a better predictor of medication response than chronological age [2, 6]. Interestingly, the Australian cohort had a lower proportion of most-frail residents in those ≥ 90 years compared to younger age groups. Prevalence of dementia was lower in Australian residents ≥ 90 years when compared across age groups, but higher in most-frail residents when compared across frailty groups. Previous studies have reported high symptom burden including pain, constipation, and fatigue among residents with dementia [28, 29]. This may lead to increased use of symptomatic medications to manage symptom burden, which may partly explain the higher ratio of symptomatic to preventive medication use in the Australian cohort with increasing frailty but not with older age. In the Japanese cohort, the higher use of symptomatic over preventive medications across all age and frailty groups may also be attributable to the higher overall prevalence of dementia.
There was no significant difference in the mean number of preventive medications across age and frailty groups in both cohorts. This contrasted with the European findings that reported a lower number of preventive medications among frail compared to non-frail residents [12]. Among the top five preventive medication classes in the Australian and Japanese cohorts, four were cardiovascular medications. The higher prevalence of antiplatelets, statins, and loop diuretics in Australia compared to Japan likely reflects the higher prevalence of coronary heart disease in the cohort (Australia 28.3%; Japan 11.7%). Japanese residents were more likely to be prescribed CCBs partly due to the lower risks of adverse events [30, 31]. Japanese residents also had a considerably lower prevalence of vitamin D use (Japan 8.1%; Australia 52.0%), which may reflect initiatives in Australian NHs to increase vitamin D supplementation [32]. Prevalence of anticholinesterase use was low in Australia (8.0%) but high in Japan (17.4%). This may be partly explained by the lower prevalence of documented dementia diagnoses in the Australian (36.9%) compared to the Japanese cohort (70.0%).
There has been increasing interest among some Australian and Japanese clinicians in deprescribing [33–35]. The lower prevalence of statins among most-frail compared to non-frail and frail residents in both cohorts may partly be due to deprescribing upon reassessment of the individual risk-to-benefit profile. Residents with advanced frailty often have limited life expectancy and may have a lower likelihood of achieving maximum therapeutic benefit from long-term preventive treatments [2, 8]. Our findings suggest a potential opportunity to deprescribe chronic medications for which potential harms outweigh benefits among frail residents. However, existing disease-specific clinical guidelines rarely recommend how or when to deprescribe medications that are unnecessary or no longer appropriate [36]. This is despite evidence of potential over-treatment of chronic conditions such as hypertension and diabetes in long-term care settings [37, 38]. Tools such as the Screening Tool of Older Persons Prescriptions in Frail adults with limited life expectancy (STOPPFrail) [39] and the Screening Tool for Older Person’s Appropriate Prescriptions for Japanese (STOPP-J) [40] criteria list medications that may be suitable for deprescribing.
There may be greater opportunity to deprescribe preventive medications in Australia than in Japan. It is not clear whether Japanese residents had preventive medications deprescribed at or prior to NH admission, or to what extent the least frail Japanese residents may benefit from medication continuation. Qualitative focus groups and interviews with Australian and Japanese healthcare professionals would be worthwhile to explore possible reasons for the differences observed. Recent position statements emphasize the value of medication review to ensure alignment of regimens to residents’ goals of care [1, 5, 6]. Frailty screening may complement the use of approaches such as the Supportive and Palliative Care Indicators Tool (SPICT) in identifying residents for review [41]. Overall, 21.5% of Australian residents received a pharmacist-led medication review within 90 days of NH admission [42]. Moving forward, comprehensive medication reviews may focus on individualizing treatment based on residents’ frailty status and changing goals of care.
Strengths and limitations
Medication data were sourced from dispensing and administration records, providing an accurate reflection of residents’ actual medication use compared to prescription records. Both cohorts used the same seven FRAIL-NH domains and cut-off scores for frailty assessment. Validated tools were used to describe baseline characteristics although different tools were used to measure ADL and cognitive status in the two cohorts. The comparability of both cohorts was established with similarities in age, sex, and prevalence of diabetes. However, differences were observed in the documented prevalence of dementia diagnoses and coronary heart disease. Both cohorts were comparable to the respective national average NH population in terms of age and sex. The sample size in both cohorts was relatively small; therefore, it was not possible to generalize the patterns of medication use to all Australian and Japanese residents. Some residents who were most-frail may have been omitted from the Australian cohort as those with a life expectancy of less than three months were excluded.
Similar to other studies utilizing medication data, information on treatment indication was not available and so it was not possible to assess the clinical appropriateness of medication regimens for individual residents. A comprehensive and holistic evaluation at the resident level would be required to determine the appropriateness of individual symptomatic and preventive medications. Some medications may be used for both symptomatic and preventive purposes. Therefore, the medication categorization was an approximation based on multidisciplinary consensus and previously published lists. It is not clear to what extent the pattern of medication use in each country may reflect underlying cultural predispositions to specific chronic conditions. Given that the analyses were cross-sectional, it was not possible to determine whether the lower prevalence of some chronic medications (e.g., statins) were due to deprescribing among frailer residents. Some preventive medications may indeed be necessary in frail residents.
Conclusions
Australian residents used more preventive than symptomatic medications, while Japanese residents used more symptomatic than preventive medications. The ratio of symptomatic to preventive medications was higher with increasing frailty but lower with age in Australia; whereas in Japan, the ratio remained consistent across age and frailty groups. Preventive medications remained prevalent in most-frail residents in both cohorts, albeit at lower levels in Japan. Identification of frail residents may assist with targeting initiatives to deprescribe long-term preventive medications for which potential harms outweigh benefits, while assessing the need for medications to manage symptoms and optimize quality of life.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors gratefully acknowledge the FIRST Study collaborators: Terry Shortt for supporting the study coordination and contributing to the study design; Hilary Ashby for supporting the study coordination; Jean Zhang, Victoria Foy, and Kim Testi for conducting the collection of data and informed consent; Tina Cooper and Leonie Robson for contributing to the study design; and Tina Cooper and Merridy Baylis for reviewing the manuscript. The authors also acknowledge Professor Sirpa Hartikainen and Professor Anna-Maija Tolppanen for their contributions to the international expert consensus panel discussion.
Author contributions
SJL, JSB, and SL contributed to the study conception and design. Material preparation and data collection were performed by SJL, SH and ADJ. Data analyses were performed by SJL and SH. All authors were involved with the interpretation of data. The first draft of the manuscript was written by SJL. All authors were involved with critical revision of the manuscript and approved the final submission.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The research was supported by the National Health and Medical Research Council (NHMRC) Centre of Research Excellence in Frailty and Healthy Ageing, Australia; and Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research (KAKENHI, Grant 22K10406). The FIRST Study and ADJ were funded through project funding to RV from the Healthy Ageing Research Consortium funded by the South Australian Department for Innovation and Skills, Hospital Research Foundation and Resthaven Inc. SJL was supported by a postgraduate research scholarship funded by Monash University, and the Australian Government Research Training Program Scholarship. JSB was supported by the NHMRC Boosting Dementia Research Leadership Fellowship. All funding sources were not involved in the study design, methods, analysis, or preparation of the research.
Availability of data and materials
The authors confirm that all relevant data are included in the article and supplementary file.
Code availability
Not applicable.
Declarations
Conflict of interest
SH belongs to an endowed chair funded by donations from Mr. Kazuteru Noguchi, JSH, Towa Pharmaceutical, Sawai Pharmaceutical, and Ain Pharmaciez, and received research funding from SOMPO Care Inc. outside of this work. RV was previously a board member and a member of the clinical governance committee of Resthaven Inc. RV has received honorarium for participation in workgroups from HealthConsult Pty Ltd in relation to an Australian Government funded project. In the past, RV has received honoraria, speakers and educational grants in various combinations from Nutricia, Abbott and Nestlé. JSB has received grant funding or consulting funds from the NHMRC, Medical Research Future Fund, Victorian Government Department of Health and Human Services, Dementia Australia Research Foundation, Yulgilbar Foundation, Aged Care Quality and Safety Commission, Dementia Centre for Research Collaboration, Pharmaceutical Society of Australia, Society of Hospital Pharmacists of Australia, GlaxoSmithKline Supported Studies Programme, Amgen, and several aged care provider organizations unrelated to this work. All grants and consulting funds were paid to the employing institution.
Ethics approval
The Australian study was approved by the University of Adelaide Human Research Ethics Committee (H-2018-247), South Australian Department for Health and Wellbeing Human Research Ethics Committee (HREC/20/SAH/15), Department of Human Services External Request Evaluation Committee (EREC/RMS0432), and Monash University Human Research Ethics Committee (23620). The Japanese study was approved by the ethical review board of the Institute for Health Economics and Policy, Japan (R2-002).
Consent to participate
Written informed consent was obtained from all residents or their substitute decision-maker.
Consent for publication
All authors approved the final manuscript for publication. All participants and/or their substitute decision-maker provided consent for publication of de-identified data.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dent E, Lien C, Lim WS, et al. The Asia-Pacific clinical practice guidelines for the management of frailty. J Am Med Dir Assoc. 2017;18:564–575. doi: 10.1016/j.jamda.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Onder G, Vetrano DL, Marengoni A, et al. Accounting for frailty when treating chronic diseases. Eur J Intern Med. 2018;56:49–52. doi: 10.1016/j.ejim.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 3.Liau SJ, Lalic S, Visvanathan R, et al. The FRAIL-NH scale: systematic review of the use, validity and adaptations for frailty screening in nursing homes. J Nutr Health Aging. 2021;25:1205–1216. doi: 10.1007/s12603-021-1694-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boyd C, Smith CD, Masoudi FA, et al. Decision making for older adults with multiple chronic conditions: executive summary for the American Geriatrics Society guiding principles on the care of older adults with multimorbidity. J Am Geriatr Soc. 2019;67:665–673. doi: 10.1111/jgs.15809. [DOI] [PubMed] [Google Scholar]
- 5.Turner G, Clegg A. Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing. 2014;43:744–747. doi: 10.1093/ageing/afu138. [DOI] [PubMed] [Google Scholar]
- 6.Liau SJ, Lalic S, Sluggett JK, et al. Medication management in frail older people: consensus principles for clinical practice, research, and education. J Am Med Dir Assoc. 2021;22:43–49. doi: 10.1016/j.jamda.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Jokanovic N, Tan EC, Dooley MJ, et al. Prevalence and factors associated with polypharmacy in long-term care facilities: a systematic review. J Am Med Dir Assoc. 2015;16:e1–e12. doi: 10.1016/j.jamda.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Liau SJ, Bell JS. Frailty status and cognitive function should guide prescribing in long-term care facilities. Sr Care Pharm. 2021;36:469–473. doi: 10.4140/TCP.n.2021.469. [DOI] [PubMed] [Google Scholar]
- 9.Ma G, Downar J. Noncomfort medication use in acute care inpatients comanaged by palliative care specialists near the end of life: a cohort study. Am J Hosp Palliat Care. 2014;31:812–819. doi: 10.1177/1049909113506981. [DOI] [PubMed] [Google Scholar]
- 10.Molist Brunet N, Sevilla-Sánchez D, Amblàs Novellas J, et al. Optimizing drug therapy in patients with advanced dementia: a patient-centered approach. Eur Geriatr Med. 2014;5:66–71. doi: 10.1016/j.eurger.2013.10.011. [DOI] [Google Scholar]
- 11.Poudel A, Yates P, Rowett D, Nissen LM. Use of preventive medication in patients with limited life expectancy: a systematic review. J Pain Symptom Manage. 2017;53:1097–1110 e1. doi: 10.1016/j.jpainsymman.2016.12.350. [DOI] [PubMed] [Google Scholar]
- 12.Villani ER, Vetrano DL, Liperoti R, Palmer K, Denkinger M, van der Roest HG, et al. Relationship between frailty and drug use among nursing homes residents: results from the SHELTER study. Aging Clin Exp Res. 2021;33:2839–2847. doi: 10.1007/s40520-021-01797-z. [DOI] [PubMed] [Google Scholar]
- 13.Australian Commission on Safety and Quality in Health Care (2021) National baseline report on quality use of medicines and medicines safety—phase 1: residential aged care. Available from https://www.safetyandquality.gov.au/our-work/medication-safety/quality-use-medicines. Accessed 23 Apr 2023
- 14.Ikegami N. Financing long-term care: lessons from Japan. Int J Health Policy Manage. 2019;8:462–466. doi: 10.15171/ijhpm.2019.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sluggett JK, Ilomäki J, Seaman KL, et al. Medication management policy, practice and research in Australian residential aged care: current and future directions. Pharmacol Res. 2017;116:20–28. doi: 10.1016/j.phrs.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 16.Jadczak AD, Robson L, Cooper T, et al. The Frailty In Residential Sector over Time (FIRST) study: methods and baseline cohort description. BMC Geriatr. 2021;21:99. doi: 10.1186/s12877-020-01974-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shelkey M, Wallace M. Katz index of independence in activities of daily living (ADL) Director. 2000;8:72–73. [PubMed] [Google Scholar]
- 18.Clark CM, Ewbank DC. Performance of the Dementia Severity Rating Scale: a caregiver questionnaire for rating severity in Alzheimer disease. Alzheimer Dis Assoc Disord. 1996;10:31–39. [PubMed] [Google Scholar]
- 19.Australian Institute of Health and Welfare (2023) GEN aged care data: people using aged care. Available from https://www.gen-agedcaredata.gov.au/Topics/People-using-aged-care. Accessed 30 Apr 2023
- 20.Tsuboi A, Murakami T, Kurumadani H, et al. Relationship between criteria for evaluating the degree of independence of disabled elderly persons in performing activities of daily living. Occup J. 2002;21:455–462. [Google Scholar]
- 21.Hisano S. The relationship between Revised Hasegawa Dementia Scale (HDS-R), Mini-Mental State Examination (MMSE) and Bed-Fast Scale, Dementia Scale. Jpn J Geriatr Psychiatry. 2009;20:883–891. [Google Scholar]
- 22.Bureau of Social Welfare Tokyo Metropolitan Government (2020) Results of the survey on the operational status of facility and residential service providers for FY 2019. Available from https://www.fukushi.metro.tokyo.lg.jp/kourei/shisaku/28jigyoshachosa/. Accessed 1 May 2023
- 23.Kaehr E, Visvanathan R, Malmstrom TK, et al. Frailty in nursing homes: the FRAIL-NH scale. J Am Med Dir Assoc. 2015;16:87–89. doi: 10.1016/j.jamda.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Sakata N, Hamada S, Tsuchiya R, et al. Development of FRAIL-NH scale Japanese version. Nihon Ronen Igakkai Zasshi. 2021;58:164–166. doi: 10.3143/geriatrics.58.164. [DOI] [PubMed] [Google Scholar]
- 25.van der Meer HG, Taxis K, Pont LG. Changes in prescribing symptomatic and preventive medications in the last year of life in older nursing home residents. Front Pharmacol. 2017;8:990. doi: 10.3389/fphar.2017.00990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shafiee Hanjani L, Hubbard RE, Freeman CR, et al. Medication use and cognitive impairment among residents of aged care facilities. Intern Med J. 2021;51:520–532. doi: 10.1111/imj.14804. [DOI] [PubMed] [Google Scholar]
- 27.Hyde AJ, May BH, Dong L, et al. Herbal medicine for management of the behavioural and psychological symptoms of dementia (BPSD): a systematic review and meta-analysis. J Psychopharmacol. 2017;31:169–183. doi: 10.1177/0269881116675515. [DOI] [PubMed] [Google Scholar]
- 28.Tan EC, Jokanovic N, Koponen MP, et al. Prevalence of analgesic use and pain in people with and without dementia or cognitive impairment in aged care facilities: a systematic review and meta-analysis. Curr Clin Pharmacol. 2015;10:194–203. doi: 10.2174/157488471003150820144958. [DOI] [PubMed] [Google Scholar]
- 29.Amjad H, Snyder SH, Wolff JL, et al. Before hospice: symptom burden, dementia, and social participation in the last year of life. J Palliat Med. 2019;22:1106–1114. doi: 10.1089/jpm.2018.0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hattori Y, Hamada S, Yamanaka T et al (2022) Drug prescribing changes in the last year of life among homebound older adults: national retrospective cohort study. BMJ Support Palliat Care. Epub 2022 Jul 13 [DOI] [PubMed]
- 31.Ishida T, Oh A, Hiroi S, et al. Current use of antihypertensive drugs in Japanese patients with hypertension: analysis by age group. Geriatr Gerontol Int. 2018;18:899–906. doi: 10.1111/ggi.13276. [DOI] [PubMed] [Google Scholar]
- 32.Walker P, Kifley A, Cameron ID (2018) Focus on the implementation of vitamin D supplements in Australian residential aged care facilities (RACFs) summary report. Available from https://cdpc.sydney.edu.au/wp-content/uploads/2019/06/Implementation-of-Vitamin-D-in-Residential-Aged-Care-Facilities-Summary-Report.pdf. Accessed 1 Mar 2022
- 33.The Royal Australian College of General Practitioners (2019) RACGP aged care clinical guide (Silver Book), 5th edn Part A. Deprescribing. Available from https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/silver-book/part-a/deprescribing. Accessed 3 Mar 2022
- 34.Scott IA, Reeve E, Hilmer SN. Establishing the worth of deprescribing inappropriate medications: are we there yet? Med J Aust. 2022;217:283–286. doi: 10.5694/mja2.51686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iijima K, Arai H, Akishita M, et al. Toward the development of a vibrant, super-aged society: the future of medicine and society in Japan. Geriatr Gerontol Int. 2021;21:601–613. doi: 10.1111/ggi.14201. [DOI] [PubMed] [Google Scholar]
- 36.Sawan M, Reeve E, Turner J, et al. A systems approach to identifying the challenges of implementing deprescribing in older adults across different health-care settings and countries: a narrative review. Expert Rev Clin Pharmacol. 2020;13:233–245. doi: 10.1080/17512433.2020.1730812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE study. JAMA Intern Med. 2015;175:989–995. doi: 10.1001/jamainternmed.2014.8012. [DOI] [PubMed] [Google Scholar]
- 38.Stasinopoulos J, Wood SJ, Bell JS, et al. Potential overtreatment and undertreatment of type 2 diabetes mellitus in long-term care facilities: a systematic review. J Am Med Dir Assoc. 2021;22:1889–97.e5. doi: 10.1016/j.jamda.2021.04.013. [DOI] [PubMed] [Google Scholar]
- 39.Curtin D, Gallagher P, O'Mahony D. Deprescribing in older people approaching end-of-life: development and validation of STOPPFrail version 2. Age Ageing. 2021;50:465–471. doi: 10.1093/ageing/afaa159. [DOI] [PubMed] [Google Scholar]
- 40.Kojima T, Mizukami K, Tomita N, et al. Screening tool for older persons' appropriate prescriptions for Japanese: report of the Japan Geriatrics Society Working Group on “Guidelines for medical treatment and its safety in the elderly". Geriatr Gerontol Int. 2016;16:983–1001. doi: 10.1111/ggi.12890. [DOI] [PubMed] [Google Scholar]
- 41.Highet G, Crawford D, Murray SA, et al. Development and evaluation of the Supportive and Palliative Care Indicators Tool (SPICT): a mixed-methods study. BMJ Support Palliat Care. 2014;4:285. doi: 10.1136/bmjspcare-2013-000488. [DOI] [PubMed] [Google Scholar]
- 42.Sluggett JK, Bell JS, Lang C, Corlis M, Whitehead C, Wesselingh SL, et al. Variation in provision of collaborative medication reviews on entry to long-term care facilities. J Am Med Dir Assoc. 2021;22:148–155.e1. doi: 10.1016/j.jamda.2020.10.027. [DOI] [PubMed] [Google Scholar]
- 43.WHO Collaborating Centre for Drug Statistics Methodology (2022) ATC/DDD Index. Available from https://www.whocc.no/atc_ddd_index/. Accessed 20 Oct 2022
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that all relevant data are included in the article and supplementary file.
Not applicable.