Abstract
Background
Osteoporosis is an age-related metabolic disease which has a significant impact on bone health and overall quality of life. It is gaining importance as a major medical consideration with the rapid increase in geriatric population globally. It increases the risk of vertebral fractures, progressive spinal deformities and neurological complications, contributing significantly to morbidity and mortality. Increase in life expectancy and advancement of medical technology has led to an increase in the proportion of geriatric patients undergoing orthopaedic procedures. It is becoming vital to adequately evaluate, investigate and treat osteoporosis before planning spinal surgery, especially spinal fusions and instrumentation.
Content
Historically, osteoporosis was considered a contraindication to spine surgery adding to the burden of Disability Adjusted Life Years (DALYs) and mortality. Conversely, osteoporotic patients who underwent spine surgery were not adequately optimized, leading to an increase in failure and complication rates. Better understanding of the pathophysiology of osteoporosis and the biomechanics of an osteoporotic spine with knowledge of current standards of treatment of osteoporosis facilitate the timely and adequate management of this disease. Advances in surgical and anaesthetic techniques facilitate successful surgeries on high-risk elderly and osteoporotic patients with multiple comorbidities allowing for a significantly high predictability for long-term positive outcomes.This article discusses the biomechanics of the osteoporotic spine, the diagnosis and management of osteoporotic patients with spinal disease, and the new treatments, recommendations, surgical indications, strategies and advances in instrumentation in patients with osteoporosis who require spinal surgery.
Implications
In this article, the authors aim to provide a generalized overview for better understanding of the pathophysiological processes underlying osteoporosis in the vertebral column. This review provides a comprehensive set of guidelines for overall health and management of spine patients with pathologies, either caused by or compounded with osteoporosis. An overview of current techniques, strategies and technologies designed to address the challenges associated with spine surgery in osteoporotic patients is also outlined.
Sources
Content for this article has been sourced from routinely cited articles available via PubMed, from National Institute of Health consensus development conference, from the recommendations by World Health Organization technical report series, from previous articles by the authors and from the protocols established by the authors in their clinical practice based on experience and detailed case reviews.
Keywords: Vertebral compression fracture, Fragility fracture, Degenerative kyphosis, Degenerative scoliosis, Degenerative spondylolisthesis, Instrumentation, Stenosis, Osteoporosis, Osteoporotic vertebral fracture
Introduction
The earliest modern definition of osteoporosis given by the Consensus Development Conference, Copenhagen 1990, describes osteoporosis as ‘A systemic skeletal disease, characterized by low bone mass and micro-architectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture’ [1]. Osteoporosis is a major silent health burden in our society. Osteoporosis affects more the two hundred million women over the world. Studies estimate one in every four women in the eighth decade of life have osteoporosis. It is responsible for more than 8.9 million fractures every year, leading to an incidence of one osteoporotic fracture every 3 seconds. Globally, a third of the population of women crossing the age of 50 years may suffer from osteoporotic fractures, as may one-fifth of men crossing the age of 50 years [2]. Data on osteoporosis in India is limited to relatively regional studies. An estimated 20% of the 230 million Indians over the age of 50 years are osteoporotic women [3]. Osteoporosis has a prevalence of 8–62% among Indian women of various age groups as per these studies [4]. Osteoporotic fractures are most debilitating in the vertebral column. Other bones commonly fractured include hip bone and distal end of the radius. Osteoporosis in the vertebral column can contribute to reduction in height, acute to chronic back pain, challenges to activities of daily living, neurological weakness, radicular pain and frequently depression. Complications of osteoporotic vertebral compression fractures such as loss of bowel and bladder control, loss of ambulation significantly compromising an individual’s quality of life, loss of independence and dignity add to the burden of disability adjusted life years (DALY) [4]. With the increase in mean life expectancy and a growing proportion of geriatric population, the prevalence of osteoporosis is increasing exponentially. Consequently, the average age of patients requiring and undergoing spine surgery is also increasing [5].
Pathophysiology of Osteoporosis in the Vertebral Column
Osteoporosis is a metabolic bone disease with a multi-factorial and gradually progressive pathophysiology. Multiple mechanisms contribute to the development sequelae of osteoporotic vertebral fractures. Skeletal health and bone turnover, endocrine homeostasis and the neurological system are the chief factors involved. Osteoporotic alterations in bone metabolism are attributed to calcium, parathyroid hormone, 1,25-dihydroxy-cholecalciferol (vitamin D3), calcitonin and oestrogen-level changes. An imbalance in these systemic and local factors such as elevation of parathyroid hormone inducing a stimulation of bone resorption reduces bone mass and increases fragility. These patients often have deficient vitamin D3, which hinders intestinal calcium absorption and hampers deposition of inorganic matrix in the bone leading to reduced bone mass and fragility [5, 6].
Osteoporosis and menopause are often seen concomitantly, due to the loss of oestrogen which stimulates bone formation. Elderly postmenopausal women suffer the highest incidence of osteoporotic vertebral fractures compared to any other population.
Many other comorbidities also contribute in a direct or indirect manner to the sub-optimal deposition of calcium into the bone matrix, thereby reducing bone mass and causing fragility. Diabetes mellitus, obesity, long-standing illness, prolonged use of corticosteroids, poor nutrition and lack of regular exercise are some of the many risk factors identified as contributory factors in the pathogenesis of osteoporosis [6].
A combination of all the above-mentioned factors results in a decrease in bone mass, leading to weakness, hollowing and fragility of the vertebrae. These weakened vertebral bodies are unable to deal with the physiological stress of daily life activities like supporting erect posture of the body (anti-gravity functions), change of posture, lifting heavy objects, microtrauma and jerks related to activities of daily living. The inability to cope with these physiological stresses leads to the formation of microfractures within the matrix of the bones. These may not heal completely due to impaired bone homeostasis and new fractures keep developing with continued physiological stress. These are more likely to occur at junctional vertebral levels where the relatively immobile thoracic column transitions into the mobile lumbar vertebral column (D12, L1), due to physiological forces acting at these levels. This cycle of repeated sub-clinical insults and poor healing manifest as the common clinical presentation of osteoporosis in the vertebral column—generalized aches and pains, loss of height, gradually increasing kyphotic deformity, narrowing of the vertebral canal causing symptoms of spinal canal stenosis, etc. [6, 7].
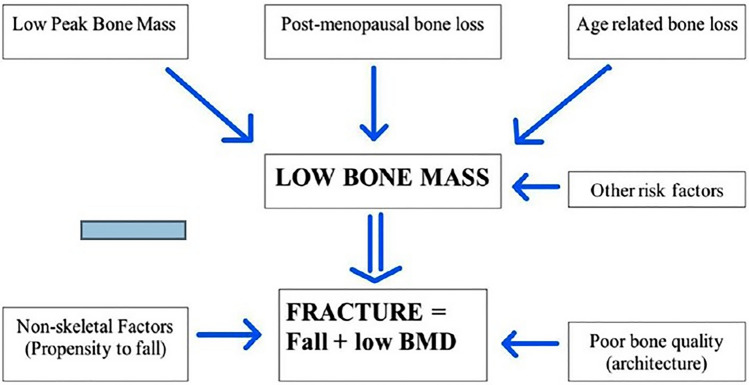
Age-related degenerative changes with other comorbidities such as poor sight, weakened muscles, poor coordination, unsteady gait and loss of balance lead to an increased propensity for slips and falls. A relatively minor trauma like slip and fall on an even floor may often be sufficient to cause a vertebral compression fracture (Fig. 1). Osteoporotic fractures have a classic mechanism of injury referred to as a trivial trauma: a force equal to or less than falling from a standing height. These fragility fractures or low-trauma fractures may be triggered by minimal physical strain such as pushing, pulling, bending forward to lift a heavy object or violent coughing or sneezing. Vertebral body fractures constitute the most common osteoporotic fractures, followed by hip and distal forearm fractures [4, 8].
Fig. 1.
Pathogenesis of osteoporotic vertebral fractures [4]
The pathophysiology of osteoporosis indicates that these fractures have a very limited healing potential, which may be further hampered by the presence of various comorbidities discussed above. Hence, osteoporotic vertebral fractures have a very high propensity for delayed healing or non-healing, paving the way for further complications associated with spinal column instability, neurological involvement, etc., which in their turn delay recovery, contribute to disability and worsen the quality of life. Vertebral fractures may lead to prolonged chronic pain, body height reduction, spinal deformities, compromised lung function and decline in quality of life and eventually contribute to mortality [4, 6, 8].
Biomechanics of the Osteoporotic Spine
In the course of daily physical activities, the vertebral column performs the dual function of flexibility and load bearing the body. Age-related degenerative changes alter the form and composition of each vertebral segment individually and globally significantly affecting the quality of life [9]. Studies have indicated that women above the age of 50 years lose as much as 50% of their bone mass and men lose up to 30% [10].
Low bone mass structurally weakens the bone, lowering its ability to withstand physiological stress. This ability is further challenged with each physiological cyclic loading, gradually leading to a state where the bone repair mechanisms are unable to keep up with the physiological demands. As a result, there is sub-optimal recovery after each insult, leading to thinner, open spicules replacing normal trabecular structure and reduction in horizontal cross-linking struts eventually compromising the buckling strength of the vertical trabeculae [7].
Osteoporosis affects trabecular bone earlier than cortical bone, compromising the load-bearing capacity of the vertebral body. The microarchitecture of a vertebral body shows greater density of trabeculae towards the posterior half of the body compared to the anterior half. Similarly, the inferior half of the vertebral body is supported by trabecular arches from the pedicles. This configuration predisposes the anterior half of the vertebral body to collapse and fracture with the posterior wall usually left intact. This anterior wedge configuration of a collapsed vertebral body causes a kyphotic deformity [7].
The vertebral body immediately adjacent to a fractured vertebra is at a higher risk of suffering an osteoporotic fracture causing a positive feedback cycle termed “vertebral fracture cascade” [11]. Multiple such anterior wedge compression fractures at sequential vertebral levels progressively worsen the kyphotic deformity, further aggravating the sagittal imbalance. An anterior wedge collapse at one level can contribute up to 10 degrees of worsening of deformity. Multiple sequential-level fractures can cause deformities as severe as 70 degrees in untreated elderly osteoporotic patients. As the kyphotic deformity progresses, there is anterior translation of the head and upper torso over the pelvis, further distorting the distribution of compressive loads over individual vertebrae [12]. This vicious cycle eventually progresses to advanced presentations including severe kyphotic–scoliotic deformities, imbalance of gait, loss of independent ambulation, significant neurological presentations like weakness and numbness of extremities, neurological claudication, bowel and bladder dysfunction, etc.
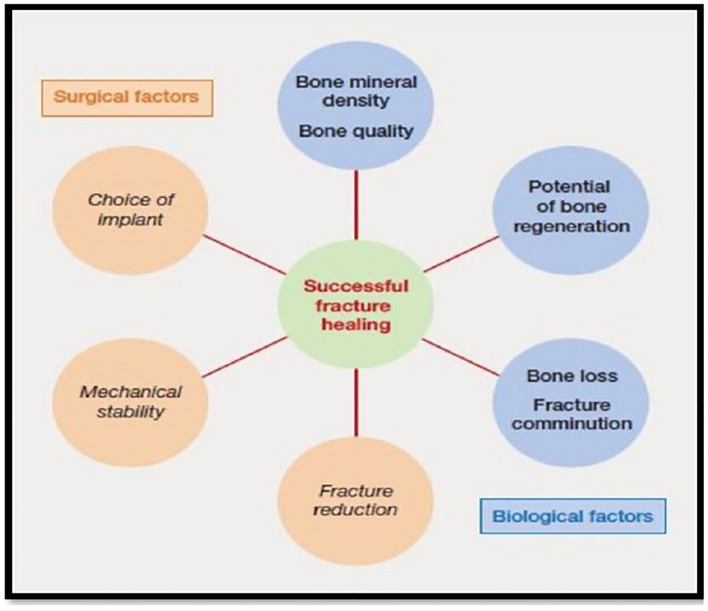
The physiological process of fracture healing involves a complex and well-balanced pattern of biochemical reactions following a definite temporal and spatial sequence, leading to regeneration of bone. This process may be influenced by multiple biological and mechanical factors (Fig. 2). Animal studies conducted on ovariectomized rodent models have shown delay in ossification, 20–40% decrease in callus area, disrupted mechanical properties of callus with decreased bending stiffness and peak failure load [13]. Although these studies are significant in understanding the biological effect of osteoporosis on fracture healing, human studies on the same are lacking. It is theorized that the loss of osteoblasts in the ageing osteoporotic skeleton is caused by a dwindling population of mesenchymal stem cells and a reduced ability to form osteoblastic progenitors [14].
Fig. 2.
Factors influencing fracture healing in osteoporotic bones [4, 15]
The efficient and effective treatment of osteoporotic vertebral fractures in patients with other complicating factors such as age and pre-existing comorbidities present an ever-growing challenge to the clinical orthopaedic practitioner. The insufficient bone stock, sub-optimal bone quality, poor healing potential, frequent fracture comminution and poor implant hold at affected and adjacent levels hamper effective fixation, stabilization and fusion of these fractures [4].
Clinical Presentation of Osteoporosis in the Vertebral Column
Early diagnosis and timely treatment have proven to be the gold standard for prevention and treatment of osteoporosis and its sequelae. Early osteoporosis may not present with any identifiable clinical symptoms. Consequently, a detailed medical history and thorough physical examination are vital. Advanced age, post-menopausal females, smoking and alcohol consumption, and malnutrition should be noted. Endocrinopathies such as thyroid/parathyroid disorders and Cushing’s disease; medications such as corticosteroids, anticoagulants, anticonvulsants and chemotherapeutic medications; malabsorption syndromes; bone marrow disorders; inflammatory disorders such as rheumatoid arthritis; connective tissue disorders like systemic lupus erythematosus; chronic infections: tuberculosis and osteomyelitis; other miscellaneous conditions such as immune compromised states, renal disease and organ transplantation should all be assessed as part of the initial clinical workup [4, 16].
The earliest clinical signs of an osteoporotic patient may be limited to generalized back pain, usually of the thoracolumbar and upper lumbar regions, loss of body height (more often noticed by relatives) and slowing of gait.
The most common presentation of osteoporosis in the vertebral column is pathological fractures. Osteoporotic fractures present as sudden acute midline pain after trivial trauma or any unusual strenuous movement [17, 18].
Symptoms Osteoporotic microfractures discussed earlier are most often painless and asymptomatic. However, an acute osteoporotic vertebral fracture caused after trivial trauma presents with acute, sharp pain. The pain is most commonly in the midline and bilateral paraspinal regions. At the thoracolumbar junction, it may radiate along the flanks anteriorly to the sub-costal regions. Fractures of lumbar vertebrae may have pain radiating to one or both gluteal regions. There is severe restriction of spinal flexibility.
Pain aggravates in sitting or standing position, often relieved in recumbent position. Pain often worsens with prolonged sitting or standing without support. Transitional pain, i.e. pain encountered during change of posture while standing from sitting position, lying down from seated position, sitting up from recumbent position or even turning in bed is a characteristic feature. Pain is exacerbated by increase in abdominal pressure like coughing, sneezing and straining during defecation. In the absence of neurological involvement, the gait may be slow, but remains physiological in character. Acute pain of a vertebral compression fracture decreases with time and the patient is often left with a dull aching lower back pain, which may be related to change in the biomechanics and sagittal balance of the vertebral column.
Signs Anterior wedge compression of vertebral bodies at the thoracic level aggravate kyphosis: Dowager’s hump, the characteristic stooped posture which is classical of osteoporosis. Reduction in height of the vertebral body is a painless chronic process, caused by the combined influence of osteoporotic vertebral collapse and age-related degeneration of intervertebral discs. Fractures at the lumbar level present as loss of lumbar lordosis. Patients with advanced spinal compression with vertebral fractures at multiple levels present with short trunk and acquired short stature, presenting as hunched posture and fingertips extending up to lower thigh or knees in standing position. In severe advanced cases, the lower ribs lie directly over the iliac crests.
Neurological features Acute osteoporotic fractures, usually being stable injuries (most commonly anterior wedge collapse), do not often present with neurological symptoms and signs. When present, thoracic and thoracolumbar junctional fractures present with pain radiating unilaterally or bilaterally along the costal margin of affected spinal nerve. Fractures at lumbar levels may cause radiating pain along one or both lower limbs. Involvement of spinal cord or cauda equina, presenting with features such as loss of bowel and bladder control, loss of balance while walking and saddle anaesthesia, is extremely rare and should immediately arouse suspicion towards other causes of pathological fractures. Often, patients may present with features of dynamic compression—while the patient is in supine position with kyphosis corrected, there are no signs or symptoms of neural compression. However, when the patient is in sitting or standing position, the kyphotic deformity aggravates, causing compression of the spinal cord, cauda equina or nerve roots, precipitating neurological features such as weakness, tingling, numbness in the extremities, unsteady gait and loss of balance while walking.
Long-term effects Progressive vertebral compression fractures at multiple levels reduce the volume of thoracic and abdominal cavities. Postural abnormalities adversely affect exercise tolerance. Abdominal fullness and bloating after minimal food intake are common. Gross kyphotic deformity at the thoracic level may contribute to compromise of pulmonary and cardiac function, especially in patients of pre-existing cardiovascular or pulmonary diseases [4, 17, 18].
Investigations
All patients presenting with risk factors of osteoporosis (post-menopausal women, elderly age group, diabetes mellitus, history of corticosteroid use, inflammatory arthritis, previous fragility fracture) must be thoroughly evaluated for osteoporosis.
General workup must include basic blood investigations such as blood counts, erythrocyte sedimentation rate, serum calcium, serum phosphate, serum vitamin D3, serum vitamin B12, serum parathyroid hormone, serum uric acid, serum creatinine, blood sugar levels, markers of inflammatory arthritis (rheumatoid arthritis factor, anti-cyclic citrullinated peptide, anti-nuclear antibody, human leucocyte antigen—b27 levels), serum protein electrophoresis for monoclonal band and others as per clinical history and suspicion.
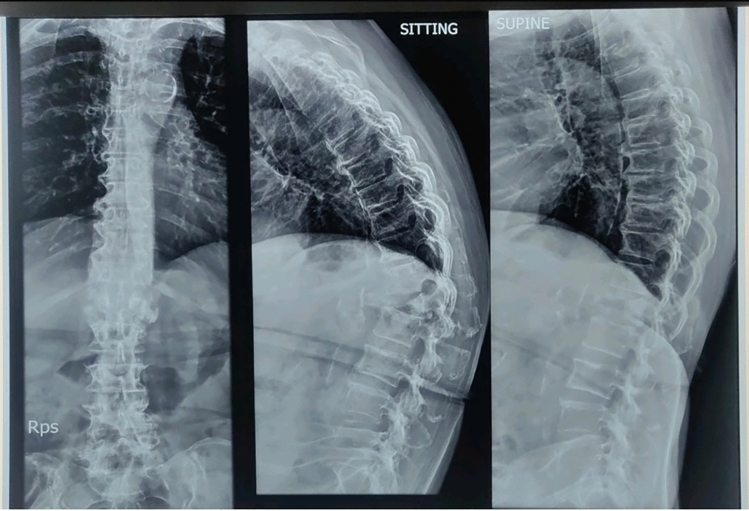
Radiographs Most patients presenting to an orthopaedic clinic are asked for radiographs which scan the area of pain/tenderness. Plain radiographs have the advantage of being easily available, less expensive and non-invasive. They may indicate features suspicious of osteoporosis, but have no value in diagnosis, quantification of disease or monitoring treatment. Thinned cortices, radiolucent trabeculae and shortened vertebral body height are indicative. Conditions such as multiple myeloma, metastatic disease, osteomalacia and infections have specific radiological appearances, which may indicate secondary osteoporosis [4]. In frank osteoporotic vertebral fractures, radiographs of the thoracolumbar spine in the anteroposterior, lateral sitting and lateral supine views should be obtained. These radiographs help identify vertebral compression fractures with decrease in height of the vertebral body. The dynamic views of radiographs identify any instability with increase in kyphosis seen in the loaded sitting position compared to off-loaded supine position (Fig. 3). The dynamic view radiographs may also elicit opening and closing of the fracture line showing “vacuum sign or Kummel’s lesion” which is considered pathognomic of an osteoporotic vertebral fracture (Fig. 4).
Fig. 3.
Thoracolumbar spine: increased kyphosis in sitting compared to supine position
Fig. 4.
Kummel sign with opening and closing on supine versus sitting radiograph
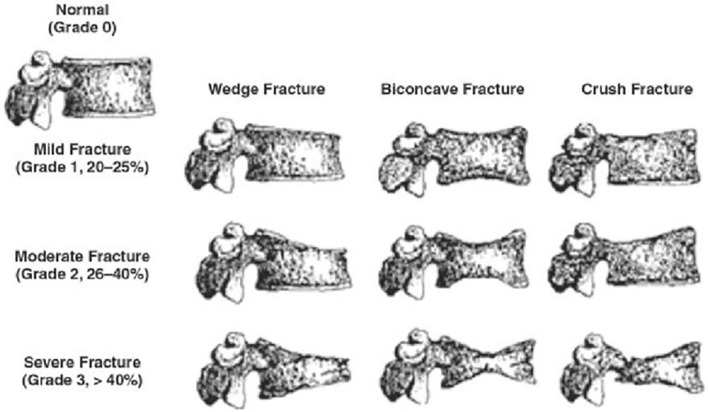
Digital radiographs are also useful for classifying the pattern of osteoporotic vertebral fractures and planning management. Genant et al. proposed a semi-quantitative system of assessing the severity of fractures based on lateral views of the spine [19]. Fractured vertebrae are each given a score from 0 to 3. Grade 0 indicates that the vertebral body has maintained its normal height. Grade 1 is suggestive of a mild fracture with 20–25% height reduction in the anterior column, middle or posterior column height of the vertebral body compared to the same or adjacent vertebrae. Grade 2 indicates a moderate fracture with 25–40% reduction and Grade 3 indicates a severe fracture with > 40% reduction in heights (anterior, middle or posterior) (Fig. 5). The Genant criteria have proved invaluable in minimizing false-positive diagnoses and ruling out physiological or degenerative wedging and congenital anomalies. It has also proved a valuable tool to plan management of vertebral osteoporotic fractures and decide between conservative versus surgical management.
Fig. 5.
Genant classification of osteoporotic vertebral fractures [19]
Bone densitometry Bone densitometry is the primary diagnostic modality in identifying osteoporosis. It is the most accessible tool for diagnosing and quantifying osteoporosis with high accuracy. The most common sites for assessing bone densitometry are the lumbar spine, the hips and the forearms. Two technologies are currently prevalent for measuring bone densitometry: dual-energy X-ray absorptiometry (DXA) and quantitative computed tomography (QCT). Various studies have shown QCT to be a more accurate tool to evaluate bone mineral density (BMD); however, the DXA scan is a far more easily available, standardized and cheaper tool. Hence, it is a commonly used and the World Health Organization (WHO)-approved modality with reproducible results. The results of bone densitometry are expressed as a T-score defined as the quantum of standard deviations (SD) of the test BMD above or below the average of the young adult reference population. A Z-score defines the standard deviations above or below the average in an age-matched reference population [4, 20]. The World Health Organization [WHO] guidelines define osteoporosis as a T-score value equal to or worse than − 2.5. A milder manifestation termed “low bone mass” or osteopenia is defined as a T-score ranging from − 1 to − 2.4. “Severe” or “established” osteoporosis indicates the presence of one or more documented osteoporotic fractures [4, 21, 22]. In addition to the diagnosis of osteoporosis, bone densitometry is also a valuable tool for measuring response to osteoporotic treatment. It is advisable to perform a bone densitometry in post-menopausal women and in elderly gentlemen above the age of 60 years (earlier in patients with factors predisposing to secondary osteoporosis), with a repeat scan every 2 years for early diagnosis of low bone mass and to monitor ongoing anti-osteoporotic therapy. It is also recommended that sequential scans be done using the same modality (DXA or QCT) and preferably the same machine for more accurate comparison and results.
Magnetic resonance imaging Magnetic resonance imaging (MRI) is not necessarily a diagnostic modality for osteoporosis or osteoporotic vertebral fractures. MRI studies done for other indications may incidentally suggest decreased bone mass and find silent vertebral fractures suggestive of osteoporosis. MRI as an imaging modality is only indicated in patients with neurological involvement to assess compression, if any, over the spinal cord, cauda equina and spinal nerve roots. It is also used as a diagnostic modality when suspecting a pathological fracture secondary to infection, bone tumours (primary or metastatic), myeloma, Paget’s disease or lymphoma. The MRI scans of an osteoporotic fracture are classically marked by the presence of bone marrow oedema seen on short tau inversion recovery sequences (STIR sequences) and fracture lines, with or without a Kummel’s lesion (Fig. 6) [23].
Fig. 6.
MRI showing vertebral body fracture, Kummel sign and marrow oedema
Computed tomography Computed tomography scans (CT scans) have limited application in the diagnosis of osteoporosis of the vertebral column and osteoporotic vertebral fractures except as a modality to identify occult fractures and for pre-operative planning, if indicated, in cases with coexisting degenerative spinal deformities.
Management of the Osteoporotic Vertebral Column
Although awareness of osteoporosis and its complications has been gaining importance across the medical community, timely management and adequate treatment are still shockingly lacking. Patients presenting with frank osteoporotic fractures are often treated as ordinary fractures and are not evaluated, investigated or treated for the primary concern, contributing to high morbidity and mortality. The goals of prevention and treatment are focused on decreasing fracture risk and proper fracture management.
Non-pharmacological Considerations
Dietary calcium The onset of osteoporosis has been linked to peak bone mass achieved during young adult life between the ages of 30 and 35 years. Studies have shown that a higher peak bone mass plays a significant role in delaying the onset of postmenopausal osteoporosis in women. Consequently, it is most important to maintain optimum levels of calcium and vitamin D3 in all age groups of growing children to the osteoporotic elderly. The National Osteoporosis Foundation has set forth guidelines recommending a daily dietary intake of 1200 mg of calcium for post-menopausal women and elderly men (beyond 70 years of age). Calcium supplementation has been proven to improve bone health and reduce fracture risk [4].
Dietary vitamin D3 Low exposure to sunlight and reduced dietary absorption with advancing age are common causes of vitamin D deficiency. A daily dietary intake of 800–1000 IU of vitamin D per day is considered sufficient for adults above 50 years. Often, vitamin D supplementation of 1000–2000 IU per day may be necessary to maintain even the minimum 30 ng/ml blood level of vitamin D. In addition to calcium and vitamin D3, it is also advisable to increase dietary intake of foods rich in vitamin B12 and vitamin E, as they have a direct effect on nerve and muscle health. Vitamin B12 and vitamin E are especially important in the Indian scenario, where a major proportion of the population has a chiefly vegetarian diet.
Regular exercise Bonaiuti et al., in a review published in 2002, postulated that aerobics, weight-bearing and resistance exercises significantly increased bone density at the spine. Similarly, walking and swimming significantly improved bone quality at the hip and spine [24].
Fall prevention Approximately, 30% of the population above 65 years of age suffers at least one fall per year. 10% of these falls result in serious injuries and 2% lead to fracture. Education and counselling regarding prevention of falls must be a standard protocol in daily clinical practice. It is important to counsel both patient and caregivers on this aspect. Common measures include: using visual and hearing aids, avoiding excessive medications, use of support bars and friction mats in slippery areas, removing uneven walking surfaces like carpets, use of guiding lights in the bedroom and bathroom during the night, hand rails on stairs, walking sticks or walkers as needed and quality footwear [4].
Osteoporotic vertebral fractures Most osteoporotic vertebral fractures do not present with gross vertebral column instability or neurological involvement. As a result, a majority of these fractures are treated conservatively. Conservative management of osteoporotic vertebral fractures mainly involves use of supportive orthoses and adequate pain management. The function of these orthoses and braces is to support the vertebral column, prevent excessive movement at the fracture site, reduce pain associated with fracture mobility, maintain correct posture and prevent further collapse of the fractured vertebra and promote healing of fracture in a physiological position preventing deformities. These orthoses have various designs based on the vertebral level affected. A thoracolumbar–sacral orthoses (TLSO) is used for fractures at the thoracic and thoracolumbar junctional levels. The Taylor’s brace was commonly used previously. However, the use of Taylor’s brace has largely been replaced in favour of the anterior spine hyperextension brace (ASH Brace), which is more effective in preventing forward stooping posture and further collapse of the fractured vertebral level. A frame-type lumbosacral belt is commonly used for fractures of the lower lumbar vertebrae. Certain lifestyle modifications like avoiding lifting heavy objects, excessive forward or lateral bending, squatting, sitting cross-legged, sitting on floor or low surfaces, avoiding violent coughing or sneezing and avoiding straining during motions are also advocated for patients with osteoporotic vertebral fractures. They are also advised to avoid jerks and twists to the vertebral column, including measures like use of walking aids, avoiding crowded places, avoiding jerky modes of travel or travelling on uneven roads, etc.
Pharmacological Treatment
Medical management of osteoporosis includes administration of agents which reduce bone loss and promote bone matrix deposition, thereby improving bone architecture and strength and reducing the risk of osteoporotic fractures.
The National Osteoporosis Foundation [2008] recommends institution of anti-osteoporotic treatment for:
patients with previous fragility fracture in hips or spine,
patients with a T-score of − 2.5 or lower at the femoral neck or spine, and
patients who have a T-score of between − 1.0 and − 2.5 at the femoral neck or spine and a 10-year hip fracture risk of ≥ 3% or a 10-year risk of a major osteoporosis-related fracture of ≥ 20% as assessed with the FRAX tool [25, 26].
Bisphosphonates
Bisphosphonates are anti-resorptive agents inhibiting osteoclasts and decreasing bone resorption. A reduction in the resorption of the remodeling space and secondary remineralization improves bone mass and reduces fracture risk.
Alendronate, risedronate, ibandronate, and zoledronic acid are routinely prescribed oral and injectable preparations. Oral bisphosphonates have some dosage specifications, which may cause difficulty in compliance. They must be ingested on empty stomach, in an erect position with considerable water intake, following which the patient must not lie down or consume any food or drink for a period of 45 min. This avoids the common side effect of gastric irritation. A drawback of oral bisphosphonates is poor intestinal absorption [27].
Zoledronic acid is recommended as an annual intravenous preparation given slowly over 20 min to an hour. Patients require monitoring up to 24 h post-administration, due to high risk of acute phase reactions. It is contraindicated in patients with renal compromise. Other side effects include musculoskeletal pain, hypocalcaemia and osteonecrosis of the jaw. It is recommended to avoid invasive dental treatments for patients on bisphosphonates [28].
The effects of bisphosphonates may last in the body for up to 6 months post-cessation of treatment. This provides an advantageous cover till a change of medication can be instituted. A long-term complication of bisphosphonate therapy in insufficiency fractures in long bones. It is recommended to provide treatment holidays for patients on long-term bisphosphonate therapy [29].
Calcitonin
Calcitonin is an anti-resorptive biological agent most commonly prescribed as a nasal spray. It has a relatively minor role in improving bone quality and reducing risk of vertebral fractures. Its role in non-vertebral fractures is unknown. It inhibits anti-resorptive effect of osteoclasts. Calcitonin is preferably given as one puff [200 International Units (IU)] daily in alternate nostrils for a period of 6 weeks with calcium and vitamin D3 supplementation. Occasionally, for acute painful osteoporotic fractures, twice a day dosage may be given in alternate nostrils for a period of 2 weeks, followed by the regular once a day dosage for a period of 4 weeks further. Alternately, 100 IU subcutaneous or intramuscular dose is recommended in patients unable to comply with the nasal administration. Calcitonin has an established analgesic effect on vertebral osteoporotic fracture-related pain [4].
Adverse effects include nasal irritation, occasional epistaxis and inadequate administration via the nasal route.
Teriparatide [rhPTH: 1,34]
Teriparatide is a partial analogue of parathyroid hormone that increases bone density and decreases fracture risk, mainly at the spine and the hip and to a lesser extent at non-vertebral regions. It is the only anabolic agent, with established bone density-building action currently approved for use in India. It acts on both trabecular and cortical bone by improving bone volume and trabecular and cortical thickness with an established improvement in bone microarchitecture. The anabolic action on both cortical and cancellous also improves callus formation and consolidation, promoting fracture healing.
A subcutaneous 20 µg [8 units] daily injection from a pre-filled metered syringe is the current standard recommendation. It is expensive compared to other agents. The syringe and medication require refrigeration and safe storage. Currently, the approved regimen in India is limited to a continuous stretch of 2 years throughout the life of the patient.
The use of teriparatide is contraindicated in patients who have had a history of malignancy at any stage during their lifetime, irrespective of the status of the malignancy (ongoing or cured).
Denosumab
It is a human monoclonal antibody that acts by inhibiting the RANK-ligand and providing anti-resorptive strengthening of bone. Current recommendation is a 6 monthly subcutaneous injection of 60 mg and is currently approved for use up to 10 years.
The effect of denosumab in the body lasts for 6 months following the last administered dose. Hence, it is vital to counsel patients and caregivers regarding the need for regularity in taking the due dose every 6 months.
Denosumab is a relatively expensive medication and has no proven anabolic activity. Adverse effects include hypocalcaemia, osteonecrosis of the jaw and a profile similar to bisphosphonates. It is contraindicated in patients with pre-existing hypocalcaemia and pregnant patients. Some studies report a higher infection rate post-denosumab administration compared to bisphosphonates [1, 4].
Raloxifene
Raloxifene is a selective oestrogen receptor modulator [SERM]. It has an anti-resorptive effect on the skeletal system and improves bone quality at the spine and the hip. Currently, use of raloxifene is not recommended due to high risk of thromboembolic events.
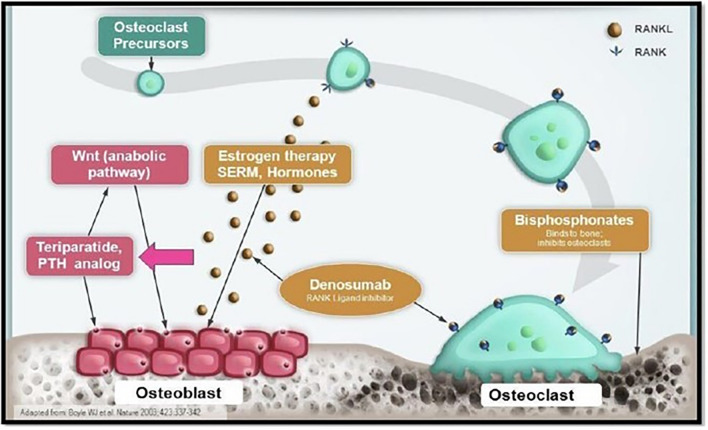
Figure 7 shows the mechanism of action of various anti-osteoporotic drugs [30].
Fig. 7.
Mechanism of action of anti-osteoporotic therapies [30]
Surgical Considerations
Increase in life expectancy and advancement of medical technology have led to an increase in the proportion of geriatric patients undergoing orthopaedic procedures. It has become vital to address the growing concerns of osteoporosis in these patients. Patients who require surgery for various spine problems may have coexisting osteoporosis. Conversely, there are patients who may require surgery to correct the direct sequelae of osteoporosis. In such cases, it becomes vital to address both osteoporotic and surgical concerns in such a manner that the treatment of one does not adversely affect the other. Safely offering spine surgery to a patient with compromised bone quality is a daunting task with a significantly higher risk–benefit ratio compared to non-osteoporotic population. An optimal bone quality is essential for any spine surgery to be successful including maintaining long-term stability of implant constructs, promoting success of fusions and prevention of future complications [31].
Recent studies have clearly outlined the favourable outcomes of surgical treatment over conservative management in terms of both quality of life and survival rate [32, 33]. Recent surgical and anaesthetic advances facilitate successful surgeries on high-risk elderly and osteoporotic patients with multiple comorbidities allowing for a significantly high predictability for long-term positive outcomes.
Peri-operative Optimization
Osteoporotic patients requiring surgery require optimal preparation while planning surgery. In a scenario of elective surgeries which would require bone instrumentation, it is preferable to initiate anti-osteoporotic treatment and defer surgery till the bone density can be built up adequately for safe and stable instrumentation.
There is conflicting data regarding the use of anti-resorptives during the peri-operative period. It is common practice to have a gap between administration of anti-resorptive agents and a surgical procedure (4 weeks for zoledronic acid and 2 weeks for denosumab) to minimize the risk of complications like osteonecrosis and to avoid the inflammatory cascade associated with use of bisphosphonates [34].
In cases where surgical intervention cannot be delayed, teriparatide can be started concomitantly without any risk of peri-operative complications.
Intra-operative
Osteoporotic bone is essentially a hollow bone with porous trabecular component and brittle cortices. Consequently, this bone provides very poor hold over any implant and has a very poor pullout strength. With decreasing bone matrix, the pedicles widen providing sub-optimal purchase over screws of standard diameter [31]. These factors contribute to an increased incidence of instrumentation failure, implant loosening and screw pullout. Poor bone matrix formation and healing capacity increase the risk of delay or failure of fusion and pseudo-arthrosis formation.
Recent studies indicate that the incidence of early complications in osteoporotic patients after spine surgery may be as high as 13%, including hematoma formation, pedicle fractures or adjacent-level collapse leading to compression over neural structures. There is also an increased risk of delayed complications such as implant failure, failure of fusion and formation of pseudo-arthrosis which may be as high as 11% [35].
The commonly used intra-operative modalities to ameliorate the incidence of complications in osteoporotic patients undergoing spine surgery are listed herewith:
Stabilization using multiple fixation points and combining multiple fixation strategies.
Augmentation of implant purchase in the bone with polymethyl methacrylate bone cement.
Use of dual-threaded pedicle screws.
Use of expansile screws to improve implant purchase and pullout strength.
Screws with hydroxyapatite coating to promote stronger bone–implant interface.
Larger diameter screws for better pedicular hold and achieving bi-cortical purchase.
Focusing on achieving optimal sagittal balance with acceptable compromise in coronal correction.
Longer posterior stabilization construct with screws at multiple vertebral levels above and below the fracture level [36].
Use of intra-operative neuromonitoring in indicated cases.
Use of adequate auto-bone graft, where indicated, to promote bone healing.
Post-operative Care and Follow-Up
A successful surgery on the operating table does not automatically guarantee good clinical outcomes in patients with osteoporosis. A successful surgery is merely the first step in the process of recovery and rehabilitation of the patient towards an independent pain-free quality of life. In the immediate post-operative period, it is often advisable to avoid over-enthusiastic physiotherapy and mobilization of the patient. Most osteoporotic patients are of geriatric age group with other debilitating comorbidities and reduced capacity to recover from a major surgical procedure. Delayed, gradual mobilization strictly with the support of external orthoses and walking aids if required, despite adequate internal stabilization, may be prudent in these cases.
Regular follow-up radiographs to check the position of the implants and to assess progress of fracture healing and intervertebral fusion is indicated as healing potential of bone is compromised in osteoporosis.
The patient and caregivers should be involved in all decision-making processes. They should be counselled in detail regarding the importance and need for continuing anti-osteoporotic medication, regular follow-up and monitoring of anti-osteoporotic treatment, the strict need to follow all precautions and the need for timely and adequate treatment of other existing comorbidities. They should also be made aware of the danger signs and when to reach out to health-care professionals at the earliest.
Conclusion
Osteoporosis is an insidious disease spectrum that significantly affects the vertebral column. Early diagnosis and treatment remain the mainstay in the armamentarium of the clinical orthopaedician. High index of suspicion, thorough clinical evaluation and regular monitoring and follow-up of high-risk patients as a routine practice cannot be understated. Most cases of osteoporosis affecting the vertebral column require conservative management; therefore, it is essential to involve the patient and the caregivers in the treatment process and ensure they understand the importance of complying with the therapeutic regimen. Detailed investigations and thorough pre-operative planning are a must while considering spine surgery in osteoporotic patients. Often, a multi-disciplinary team approach involving the orthopaedic surgeon, physician, anaesthetist, endocrinologist and neurophysician, as indicated, are of the utmost value. Technological advancements in surgical instruments and implants are not a substitute for sound orthopaedic and surgical principles.
Declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Consensus Development Conference [Copenhagen]. 1991. Diagnosis, prophylaxis and treatment of osteoporosis. The American Journal of Medicine, 90(1), 107–110. [DOI] [PubMed]
- 2.NIH Consensus Development Conference Osteoporosis prevention, diagnosis and therapy. JAMA. 2001;285(6):785–795. doi: 10.1001/jama.285.6.785. [DOI] [PubMed] [Google Scholar]
- 3.Malhotra N, Mithal A, et al. Osteoporosis in Indians. Indian Journal of Medical Research. 2008;127(3):263–268. [PubMed] [Google Scholar]
- 4.Agrawal P, Agrawal G. Osteoporosis in orthopaedics: Review of literature and clinical approach. The Indian Practitioner. 2020;73(5):26–43. [Google Scholar]
- 5.Kessenich C. The pathophysiology of osteoporotic vertebral fractures. Rehabilitation Nursing. 1997;22(4):192–195. doi: 10.1002/j.2048-7940.1997.tb02098.x. [DOI] [PubMed] [Google Scholar]
- 6.Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002;359:1929–1936. doi: 10.1016/S0140-6736(02)08761-5. [DOI] [PubMed] [Google Scholar]
- 7.Briggs A, Greig A, et al. The vertebral fracture cascade in osteoporosis: A review of aetiopathogenesis. Osteoporosis International. 2007;18:575–584. doi: 10.1007/s00198-006-0304-x. [DOI] [PubMed] [Google Scholar]
- 8.Harrison RA, Siminoski K, et al. Osteoporosis related kyphosis and impairments in pulmonary function: A systematic review. Journal of Bone and Mineral Research. 2007;22(3):447–457. doi: 10.1359/jbmr.061202. [DOI] [PubMed] [Google Scholar]
- 9.Ferguson SI, Steffen T. Biomechanics of the aging spine. European Spine Journal. 2003;12(2):97–103. doi: 10.1007/s00586-003-0621-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mazess RB. On aging bone loss. Clinical Orthopaedics. 1982;165:239–252. doi: 10.1097/00003086-198205000-00037. [DOI] [PubMed] [Google Scholar]
- 11.Lindsay R, Silverman S, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285(3):320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 12.Keller T, Harrison D. Prediction of osteoporotic spinal deformity. Spine. 2003;28(5):455–462. doi: 10.1097/01.BRS.0000048651.92777.30. [DOI] [PubMed] [Google Scholar]
- 13.Cortet B. Bone repair in osteoporotic bone: Postmenopausal and cortisone induced osteoporosis. Osteoporosis International. 2011;22:2007–2010. doi: 10.1007/s00198-011-1612-3. [DOI] [PubMed] [Google Scholar]
- 14.Cornell CN. Internal fracture fixation in patients with osteoporosis. Journal of American Academy of Orthopaedic Surgeons. 2003;11:109–119. doi: 10.5435/00124635-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Giannoudis P, Tzioupis C, et al. Fracture healing in osteoporotic fractures: Is it really different? A basic science perspective. Injury. 2007;38(1):590–599. doi: 10.1016/j.injury.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Tannirandorn P, Epstein S. Drug-induced bone loss. Osteoporosis International. 2000;11(8):637–659. doi: 10.1007/s001980070062. [DOI] [PubMed] [Google Scholar]
- 17.Glaser D, Kaplan F. Osteoporosis: Definition and clinical presentation. Spine. 1997;22(24):12S–16S. doi: 10.1097/00007632-199712151-00003. [DOI] [PubMed] [Google Scholar]
- 18.Thorngren K. Fractures in the elderly. Acta Orthopaedica Scandinavica. 1995;266(Suppl):208–210. doi: 10.3109/17453679509157694. [DOI] [PubMed] [Google Scholar]
- 19.Genant HK, Wu CY, et al. Vertebral fracture assessment using a semiquantitative technique. Journal of Bone and Mineral Research. 1993;8:1137–1148. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization . Technical report series 843. WHO; 1994. [PubMed] [Google Scholar]
- 21.Kanis JA, On Behalf of the World Health Organization Scientific Group. Technical report. World Health Organization collaborating centre for metabolic bone diseases, University of Sheffield; UK: 2007. Assessment of osteoporosis at the primary health-care level.
- 22.Sozen T, Ozisic L, et al. An overview and management of osteoporosis. European Journal of Rheumatology. 2017;4(1):46–56. doi: 10.5152/eurjrheum.2016.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Link T. Radiology of osteoporosis. Canadian Association of Radiologists Journal. 2016;67(1):28–40. doi: 10.1016/j.carj.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 24.Bonaiuti D, Shea B, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. The Cochrane Database of Systematic Reviews. 2002;2:CD000333. doi: 10.1002/14651858.CD000333. [DOI] [PubMed] [Google Scholar]
- 25.National Osteoporosis Foundation. 2008. Clinician’s guide to prevention and treatment of osteoporosis. http://www.nof.org/professionals/cliniciansguide_form.asp. Accessed 2009 Oct 22.
- 26.Dawson-Hughes B, Tosteson A, et al. National Osteoporosis Foundation Guide Committee. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporosis International. 2008;19:449–458. doi: 10.1007/s00198-008-0559-5. [DOI] [PubMed] [Google Scholar]
- 27.Riggs B, Parfit A. Drugs used to treat osteoporosis: The critical need for a uniform nomenclature based on their action on bone remodelling. Journal of Bone and Mineral Research. 2005;20(2):177–184. doi: 10.1359/JBMR.041114. [DOI] [PubMed] [Google Scholar]
- 28.Rizzoli R, Burlet, et al. Osteonecrosis of the jaw and bisphosphonate treatment for osteoporosis. Bone. 2008;42(5):841–847. doi: 10.1016/j.bone.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Allison M, Markman L, et al. Atypical incomplete femoral fractures in asymptomatic patients on long term bisphosphonate therapy. Bone. 2013;55(1):113–118. doi: 10.1016/j.bone.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 30.Boyle W, Simonet W, et al. Osteoclast differentiation and activation. Nature. 2003;423(6937):337–342. doi: 10.1038/nature01658. [DOI] [PubMed] [Google Scholar]
- 31.Fiani B, Newhouse A, et al. Special considerations to improve clinical outcomes in patients with osteoporosis undergoing spine surgery. International Journal of Spine Surgery. 2021;15(2):386–401. doi: 10.14444/8050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ritter M, Albohm M, et al. Life expectancy after total hip arthroplasty. Journal of Arthroplasty. 1998;13(8):874–875. doi: 10.1016/S0883-5403(98)90192-9. [DOI] [PubMed] [Google Scholar]
- 33.White A, Panjabi M. Clinical biomechanics of the spine. 2. Williams & Wilkins; 1990. [Google Scholar]
- 34.Hewitt RE, Lissina A, et al. The bisphosphonate acute phase response: Rapid and copious production of pro inflammatory cytokines by peripheral blood and T cells in response to amino bisphosphonates is inhibited by statins. Clinical and Experimental Immunology. 2005;139(1):101–111. doi: 10.1111/j.1365-2249.2005.02665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DeWald C, Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine (Phila Pa 1976) 2006;31(19):144–151. doi: 10.1097/01.brs.0000236893.65878.39. [DOI] [PubMed] [Google Scholar]
- 36.Tome-Bermejo F, Pinera A, et al. Osteoporosis and management of spinal degenerative disease (I) The Archives of Bone and Joint Surgery. 2017;5(5):272–282. [PMC free article] [PubMed] [Google Scholar]