Abstract
Background
Increased digital health and social care services are generally considered to improve people’s access to services. However, not everyone can equally access and use these resources. Health and social care professionals should assess clients’ suitability for digital solutions, but to succeed, they need information about what to evaluate and how.
Objective
This scoping review aimed to identify evaluation tools that professionals can use when assessing clients’ suitability for digital health and social care. We summarized the dimensions and the practical usefulness of the instruments.
Methods
The MEDLINE (Ovid), CINAHL, Web of Science, and ASSIA databases were searched in February 2023 following the Joanna Briggs Institute’s Manual for Evidence Synthesis. Studies were included if they focused on health and social care clients and professionals, examined clients’ suitability for using digital health or social care, and applied related assessment methods in the direct client work of professionals. Studies focusing primarily on instruments intended for research use without clear applicability to professionals’ practical contexts were excluded. Details of the eligible studies were extracted, and qualitative content analysis according to the research objectives was performed.
Results
A total of 19 articles introducing 12 different assessment instruments intended for the health care context were included in the review. No instruments were found for evaluating the suitability for digital social care. The instruments contained 60 dimensions of the client’s suitability for digital health, which reflected four perspectives: (1) skill-based suitability, (2) suitability based on general ability to maintain health, (3) suitability based on attitude and experience, and (4) suitability based on practical matters. The described practical usefulness of the instruments included professionals’ possibility to (1) identify clients most in need of education and support, (2) direct and recommend the right clients for the right digital services, (3) ensure that clients can use digital health, (4) improve effectiveness and maximize the provision of digital health, (5) develop and redesign services, and (6) empower clients.
Conclusions
Based on the diverse assessment instruments available and the dimensions they measure, there seems to be no comprehensive evaluation tool for assessing clients’ prerequisites to use digital solutions. It is important to further develop comprehensive screening tools applicable to professionals’ busy work (both in health and social care) with defined threshold values for suitability.
Keywords: access, accessibility, assessment, clients, digital health, digital social care, eHealth, evaluation tool, evaluation, evaluator, instrument, knowledge synthesis, patients, professionals, review methodology, review methods, scoping, social care, suitability
Introduction
To achieve the vision of better health and well-being for all, the need to strengthen health and social care services by applying digital technologies is well-recognized worldwide [1,2]. One of the primary goals of digitalization in health and social care is increased access to services [3,4]. Digital health and social care refers to the use of digital technologies to support the delivery of services with the aim of promoting individuals’ health and well-being and managing health conditions or risks [1,5]. Digital health and social care encompass a wide range of technologies, such as remote receptions and interventions, mobile health, websites supporting health and well-being, client and patient portals, remote monitoring systems, and wearables. These technologies have aimed to increase flexibility in the provision of services, help clients access services remotely, and reduce the need for in-person visits [6]. Moreover, digital technologies can enable clients to communicate effectively and easily with their service providers [7] and manage their own health and well-being more actively [4,8], which also belong to the strategic goals of digitalization [1,9].
The results achieved from the provision of digital technologies do not only depend on their quality but also on clients and health or social care professionals, who have a significant role as end users [10,11]. While increased digitalization is generally seen as increasing access to services, not everyone can use these resources equitably. Numerous factors, such as insufficient skills, available equipment and space, lack of interest or knowledge of available digital services, and lack of support, among others, can make it difficult for many to benefit from digital health and social care [12,13]. In the health care context, having sufficient digital health literacy (also known as eHealth literacy [eHL]) has been seen as an essential prerequisite [14]. It is defined as a set of skills required in the use of digital technologies to search, acquire, understand, evaluate, communicate, apply, and create health-related information to improve the quality of life [15].
Professionals have a key role in promoting the use of digital health and social care, for example, by referring clients to digital services [16] and actively providing information, support, and encouragement for use [17]. Increased digitalization has also induced other new tasks for professionals, such as identifying whether clients’ situations and circumstances favor the use of digital services [18]. When considering the use of a digital solution, professionals need to be able to evaluate the client’s individual needs and potential barriers [19], as well as their willingness and capabilities for use [20]. To successfully fulfill this task, professionals should know what they should evaluate and how. Otherwise, professionals’ own competence, attitudes, or preferences can determine whether they recommend digital services to their clients and promote their use [11,21].
A considerable number of studies have been conducted to identify factors that could predict clients’ adoption and use of digital services, such as telemedicine consultations [22], mobile health tools [23], and patient portals [16]. The information obtained on the associated factors could, in principle, be used by professionals when evaluating the client’s suitability for using digital health and social care. However, it may also lead to making generalizations and assumptions about suitability without individual assessment. Stereotypical thinking about suitable users (eg, based on age) increases the risk that some clients who could use and benefit from digital services might remain unrecognized. Therefore, appropriate evaluation tools are needed for the various factors that may affect the client’s use of digital services.
The aim of this review was to identify available evaluation tools that health and social care professionals can use when assessing a client’s suitability for digital health and social care. The review addresses the following research questions:
What instruments are available for health and social care professionals to assess a client’s suitability for digital health and social care?
What dimensions (factors) are included in the instruments to assess a client’s suitability for digital health and social care?
What is the described practical usefulness of the instruments for the professionals’ work?
Methods
We conducted a scoping literature review by following the Joanna Briggs Institute’s Manual for Evidence Synthesis [24].
Eligibility Criteria
Eligibility criteria were defined based on the population, concept, and context framework [24]. Population included were health and social care clients and professionals (ie, care providers). Concept was clients’ suitability for using digital health or social care and methods that can be used to assess it, such as existing instruments or guidelines. Context was the direct client work of health and social care professionals for which the assessment method had to be intended or applied. Studies were excluded if the assessment method was intended mainly for research use (such as national or cross-national population–based surveys) and if its usefulness or applicability to professionals’ work or a practical context was not described.
Types of Sources
This review considered peer-reviewed empirical studies (quantitative, qualitative, or mixed methods), systematic literature reviews, and papers presenting instrument development or evaluation. Other types of papers, such as policy documents, protocols, or discussion papers, were excluded as they were not seen to provide as reliable information as peer-reviewed scientific publications. Due to the rapid progress of digitalization in the past decade [25], we limited the search to studies published between 2012 and 2023 with an English abstract and full text.
Search Strategy
A total of 4 databases were selected, which were assumed to contain relevant articles to answer the research question: MEDLINE (Ovid), CINAHL, Web of Science, and ASSIA. First, a preliminary search was conducted in CINAHL to identify relevant search terms. Then, the expertise of a research librarian was used in the optimization of search words and strategies in the selected databases. Search strategies were tested in CINAHL and MEDLINE (Ovid) and refined before performing final searches in all 4 databases in February 2023. The reference lists of the included studies were screened for potential additional publications. The search strategy for databases is presented in Table S1 in Multimedia Appendix 1 [26-44].
Study Selection
The search records were transferred to the reference management system Zotero (Corporation for Digital Scholarship) to remove duplicates. First, 2 reviewers (AMK and LV) independently conducted title and abstract screenings of the publications. Then, both reviewers screened the full texts of the publications and provided reasons for their exclusion. In both phases, studies with conflicting decisions were rescreened and solved by consensus between the reviewers.
Data Extraction
The following data were extracted from the studies: (1) authors, publication year, and country; (2) study aim; (3) methodology and participants; (4) instruments, dimensions, and number of items; (5) associations of the values obtained with the instrument with the use of digital health and social care or other relevant findings; and (6) practical usefulness for professionals.
Data Analysis
As recommended in scoping reviews, in addition to counting frequencies for the studies’ demographics, we used qualitative content analysis for each research question [24,45]. The method allowed for identifying and creating an overall picture of the key content areas of the assessment of the client’s suitability for digital health and social care, as well as the practical usefulness of the instruments for professionals’ work. First, all the individual expressions corresponding to the research questions were extracted from the text, and their content was simplified and clarified. Then, these “codes” were classified into categories based on similarity [46]. Preliminary categorization was done by the first author (AMK), after which the names and contents of the categories were evaluated by the coauthors to ensure consensus.
Retrieval of Studies
A total of 1346 studies were identified (MEDLINE [Ovid], n=418; CINAHL, n=324; Web of Science, n=513; and ASSIA, n=91). After removing duplicates (n=677), a total of 669 studies were included in the title and abstract screening. Based on the inclusion and exclusion criteria, 623 studies were excluded, and 46 were retrieved for full-text evaluation. Finally, 19 studies were included in the data extraction process. Figure 1 illustrates the flowchart of the selection process.
Figure 1.
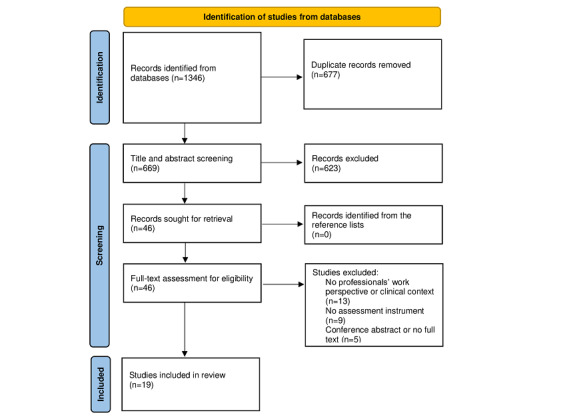
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram describing the selection process.
Results
Description of the Studies
Of the studies included (n=19), a total of 6 originated from North America, and other regions were Asia (n=5), Europe (n=4), Australia (n=3), and the Middle East (n=1; Table S2 in Multimedia Appendix 1). The studies were published between 2012 and 2023, with nearly half of them (n=9) within the past 3 years (2020 or after). Most of the studies (n=15) aimed to adapt a certain measuring instrument to a specific client group and conduct validity and reliability testing (ie, psychometric properties and psychometric validation). The rest aimed to develop a measuring instrument (n=2), evaluate the usability of combining several instruments (n=1), and evaluate the content and response process of an instrument (n=1). All studies were conducted in the health care context, and none of the studies dealt with the client’s suitability for digital social care. Thus, all studies considered instruments assessing clients’ suitability for using digital health. Most of the studies used quantitative methods (n=17), only 1 used a qualitative method, and 1 used mixed methods. More than half of the included studies were targeted at clients with different health conditions or disabilities, such as chronic diseases (n=6), cardiovascular diseases (n=3), cancer (n=1), and autism (n=1). A total of 5 studies did not specify the condition of the participants but included clients visiting hospital outpatient clinics, primary care clinics, family practice or internal medicine physicians, or clients undergoing day surgery or needing magnetic resonance imaging or computerized tomography. Additionally, in 3 studies, participants were identified from registers.
Instruments Assessing Client’s Suitability for Using Digital Health
The studies introduced 12 instruments that were described to measure the client’s potential and suitability for using digital health from slightly different perspectives (Table 1). The most-used instrument in the studies was the eHealth Literacy Scale (eHEALS; n=8). A total of 3 studies used the eHealth Literacy Questionnaire, and 2 studies included the Health Literacy Questionnaire. All the remaining studies included a different instrument: the eHealth Literacy Scale, eHealth Literacy Assessment Toolkit (eHLA), Readiness and Enablement Index for Health Technology Instrument (READHY), Condition-Specific eHealth Literacy Scale for Diabetes (CeHLS-D), Digital Health Care Literacy Scale (DHLS), Telehealth Music Therapy Screening Tool, Digital Health Technology Literacy Assessment Questionnaire (DHTL-AQ), Digital Health Literacy Instrument (DHLI), and the Transactional eHealth Literacy Instrument (TeHLI). All the instruments were based on self-assessment, except for DHLI, which also included performance-based items. Table 1 summarizes the description of the instruments, including the context for using them.
Table 1.
Summary of the instruments included in the studies.
| Instrument | General descriptiona | Participants and context of the studies using the instrument | Original source or developer of the instrument |
| eHealth Literacy Scale (eHEALS) | Measures perceived skills and comfort in using digital technology to access, evaluate, and apply eHealth information to address health concerns | Patients with one or more chronic diseases [26,27], patients undergoing day surgery [28], medical imaging outpatients [29], patients diagnosed with heart failure [30], patients receiving internal medicine care [31], patients with considerable risk for cardiovascular disease [32], and older adults participating in a bone health intervention [33] | Norman and Skinner, 2006 [47] |
| eHealth Literacy Questionnaire (eHLQ) | Measures health literacy of individuals in the context of digital health technologies | Patients with chronic disease [34], clients from primary care medical clinics [35], and patients with cancer [48] | Kayser et al, 2018 [48] |
| Health Literacy Questionnaire (HLQ) | Measures an individual’s capacity to effectively use health information and services | Patients with considerable risk for cardiovascular disease [32] and patients with cancer [36] | Osborne et al, 2013 [49] |
| Electronic Health Literacy Scale (e-HLS) and e-HLS-CHIb | Multidimensional instrument that measures aspects of interactive literacy and critical evaluation skills in addition to the skills needed to search for and understand the information provided by electronic sources | Patients with stroke conditions [37] | Seckin et al, 2019 [50] |
| eHealth Literacy Assessment Toolkit (eHLA) | Combines 7 instruments to assess the individual’s competencies related to health and competencies related to digital solutions | Patients from the hospital outpatient clinic and a sample from the general population | Karnoe et al, 2018 [38] |
| Readiness and Enablement Index for Health Technology (READHY) | Multidimensional tool that characterizes individuals’ level of health technology readiness by combining 3 instruments: eHealth Literacy Questionnaire, selected dimensions from the Health Education Impact Questionnaire, and the Health Literacy Questionnaire | Cancer rehabilitation context | Kayser et al, 2019 [36] |
| Condition-Specific eHealth Literacy Scale for Diabetes (CeHLS-D) | Measures eHealth literacy specific for people with type 2 diabetes, including cognitive actions for internet diabetes information and abilities to digital communication | People with type 2 diabetes | Lee et al, 2022 [39] |
| Digital Health Care Literacy Scale (DHLS) | Short 3-item screening tool that measures the basic skills necessary for using digital health services, including telehealth | Caregivers of young children visiting a pediatric primary care clinic | Nelson et al, 2022 [40] |
| Transactional eHealth Literacy Instrument (TeHLI) | Multidimensional instrument that measures individuals’ perceived skills related to their capacity to understand, exchange, evaluate, and apply health information from various online sources and multimedia | Patients with COPDc | Paige et al, 2019 [41] |
| Telehealth music therapy screening tool (TMTST) | Screening tool that measures clients’ circumstances that can make them more (or less) suitable for telehealth music therapy. The tool also measures factors related to the professionals and their ability to provide telehealth. | Individuals with autism | Williams et al, 2023 [42] |
| Digital Health Technology Literacy Assessment Questionnaire (DHTL-AQ) | Measures the person’s knowledge- and skill-based competencies required for the use and adoption of digital health technology, services, and data. The focus and context of DHTL-AQ are in technology, including mobile devices and apps, health IT, and telehealth. | Patients with and those without chronic disease | Yoon et al, 2022 [43] |
| Digital Health Literacy Instrument (DHLI) | Measures a broad range of skills essential to using eHealth applications, including the ability to interact on the internet. | General (Dutch) population | Van der Vaart and Drossaert, 2017 [44] |
aDetailed information on the dimensions and factors of the instruments and the number of items is presented in Table S2 in Multimedia Appendix 1.
be-HLS-CHI: Chinese version of Electronic Health Literacy Scale.
cCOPD: chronic obstructive pulmonary disease.
Dimensions Included in the Instruments to Assess Client’s Suitability
The number of dimensions (factors) per instrument varied between 1 (eHEALS and DHLS) and 13 (READHY), and the total number of items per instrument varied between 3 (DHLS) and 79 (eHLA). Altogether, 60 individual dimensions were included in the instruments (Table 2). Based on the content analysis, the dimensions were formed into 13 subcategories and further into the following four upper categories embodying different perspectives on the client’s suitability for digital health: (1) skill-based suitability, (2) suitability based on general ability to maintain health, (3) suitability based on attitude and experience, and (4) suitability based on practical matters and implementation. Table 2 shows the categorization of the dimensions in the instruments.
Table 2.
Categorization of the dimensions in the instruments measuring client’s suitability for digital health.
| Upper category and subcategory | Individual dimension (name of the instrument) | |
| Skill-based suitability | ||
|
|
Acquiring and processing web-based information for health |
|
|
|
Technical skills required to use digital health |
|
|
|
Ability to communicate on the internet |
|
| Suitability based on general health maintenance ability | ||
|
|
Health literacy (ie, the ability to acquire and process health-related information) |
|
|
|
Health-maintaining activity (ie, the ability to take care of one’s own health and attitude toward illness) |
|
|
|
Knowledge of the health care system |
|
|
|
Individual’s social context and network |
|
| Attitude and experience-based suitability | ||
|
|
Comfort and confidence to use digital health |
|
|
|
Safety and trust in digital health |
|
|
|
Attitudes toward digital health |
|
| Suitability based on practical matters and implementation | ||
|
|
Technological tools and environment for the use of digital health |
|
|
|
Difficulties in using in-person services |
|
aC-eHEALS: Chinese version of the eHealth Literacy Scale.
bDHLI: Digital Health Literacy Instrument.
ceHEALS: eHealth Literacy Scale.
deHL: eHealth literacy.
eTeHLI: Transactional eHealth Literacy Instrument.
fDHTL-AQ: Digital Health Technology Literacy Assessment Questionnaire.
ge-HLS: Electronic Health Literacy Scale.
hREADHY: Readiness and Enablement Index for Health Technology.
ieHLQ: eHealth Literacy Questionnaire.
jCeHLS-D: Condition-Specific eHealth Literacy Scale for Diabetes.
keHLA: eHealth Literacy Assessment Toolkit.
lDHLS: Digital Health Care Literacy Scale.
mTMTST: Telehealth Music Therapy Screening Tool.
nICT: Information and communication technology.
oHLQ: Health Literacy Questionnaire.
pheiQ: Health Education Impact Questionnaire.
The assessment of “skill-based suitability” included the most dimensions (n=24) and consisted of a client’s ability to acquire and process web-based information for health, the technical skills required to use digital services, and the ability to communicate on the internet. A high number of dimensions (n=20) also focused on the assessment of the clients’ “suitability based on general ability to maintain health,” including health literacy (ie, the ability to acquire and process health-related information), health-maintaining activity (ie, the ability to take care of one’s own health and attitude toward illness), knowledge of the health care system, and the social context and network. The third upper category, “suitability based on attitude and experience,” consisted of 11 dimensions that covered clients’ comfort and confidence to use digital health, in addition to safety and trust and attitudes toward digital health. The least dimensions (n=5) were included in the fourth upper category, “suitability based on practical matters and implementation,” which covered the assessment of technological tools and environment for the use of digital health and possible difficulties in using in-person services.
Practical Usefulness of the Instruments
From the point of view of the practical usefulness of the instruments for professionals’ work, many of the studies emphasized the instrument’s screening features [27,28,33,36,39,40,43], such as being convenient and brief (eHEALS, CeHLS-D, and DHLS), not burdensome for clients, and easy for professionals to use and complete in a busy clinical setting (CeHLS-D and DHTL-AQ). A total of 19 aspects regarding the practical usefulness of the instruments were described in the studies. Based on the content analysis, six categories were formed that represented different perspectives on how the instruments and the information obtained with them could be used in practice: (1) identifying clients most in need of education, assistance, and support; (2) directing and recommending the right clients for the right digital services; (3) ensuring that the patient can use digital health; (4) improving effectiveness and maximizing the provision of digital health; (5) developing and redesigning systems and services; and (6) empowering clients. Table 3 provides a summary of the described usefulness aspects, and more detailed information is provided in the data extraction table (Table S2 in Multimedia Appendix 1).
Table 3.
Practical usefulness of the instruments described in the studies.
| Perspectives of practical usefulness and the description of usefulness aspects | Instrument | |
| Identifying clients most in need of educational interventions, assistance, and support | ||
| Identifying clients with a low eHLa level [29,39] | CeHLS-Db and eHEALSc | |
| Identifying clients who may be unaware of their need for assistance [44] | DHLId | |
| Identifying clients who are at risk of being marginalized [36] | READHYe | |
| Helping in targeting interventions and additional support for those most in need [40] | DHLSf | |
| Helping in giving appropriate advice on how to evaluate web-based sources [29] | eHEALS | |
| Informing about the need to provide recommendations about reliable sources to avoid getting misleading information [39] | CeHLS-D | |
| Informing about the need to guide clients to reliable web-based sources to reduce their need to evaluate the contents [29] | eHEALS | |
| Directing and recommending the right clients for the right digital services | ||
| Supporting decisions about which clients are eligible to participate and could benefit from particular eHealth interventions or solutions [30,38,42,44] | DHLI, eHLAg, TMTSTh, and eHEALS | |
| Informing about which clients are likely to use digital health in the future [31] | eHEALS | |
| Helping in directing clients to services that match their health attitudes, preferences, and skills [41] | TeHLIi | |
| Helping in directing clients to services that will promote their self-care and well-being [27] | eHEALS | |
| Ensuring that a patient can use digital health | ||
| Helping in ensuring clients’ readiness and ability to use and engage with technology [34,36] | eHLQj and READHY | |
| Informing about how clients identify, judge, and use digital health resources [37] | e-HLSk | |
| Informing about whether the patient’s eHL level enables the use of digital health in self-care after a procedure [28] | eHEALS | |
| Improving the effectiveness and maximizing the provision of digital health | ||
| Helping in making telehealth therapy more effective (for a specific patient group) [42] | TMTST | |
| Maximizing professionals’ ability to provide therapy through telehealth [42] | TMTST | |
| Optimizing the benefits of eHealth with suitable interventions that facilitate the clients’ access, understanding, and use of information [33] | eHEALS | |
| Developing and redesigning systems and services | ||
| Helping to improve the quality and effectiveness of care by designing more adaptive care and health-promoting programs and digital health interventions that better match users’ health needs [34,35,37] | eHLQ and e-HLS | |
| Empowering clients | ||
| Finding ways to better empower clients to take care of their own health with digital resources [26] | eHEALS | |
aeHL: eHealth literacy.
bCeHLS-D: Condition-Specific eHealth Literacy Scale for Diabetes.
ceHEALS: eHealth Literacy Scale.
dDHLI: Digital Health Literacy Instrument.
eREADHY: Readiness and Enablement Index for Health Technology.
fDHLS: Digital Health Care Literacy Scale.
geHLA: eHealth Literacy Assessment Toolkit.
hTMTST: Telehealth Music Therapy Screening Tool.
iTeHLI: Transactional eHealth Literacy Instrument.
jeHLQ: eHealth Literacy Questionnaire.
ke-HLS: Electronic Health Literacy Scale.
Only 1 study, by He et al [37], provided a cutoff point for the values obtained with the instrument (ie, what values are considered low or high, or how the values obtained should be interpreted and used in practice), which could help professionals make decisions about the client’s suitability. A total of 7 studies [26,31,33,40,41,43,44] examined whether the results obtained with the instrument are actually associated with the clients’ use of, or ability to use, digital health (ie, criterion validity). Patients with a higher eHL level were reported as having a higher interest in using internet-based information channels [26], a higher likelihood of adopting and using a personal health record [31] and the internet [33], and perceiving sufficient self-efficacy and knowledge to find and use internet-based health information [27] compared to patients with a lower level of eHL. Higher transactional eHL scores were associated with higher active and interactive internet-based health information–seeking, fewer challenges in information-seeking, and higher perceived usefulness of the internet for health-related purposes [41]. A lower digital health literacy score was associated with less experience with digital health and a lower likelihood of owning digital tools [40]. A few studies highlighted the need to investigate these associations and the predictive value of the instruments in the future [27,32,36,38].
Discussion
Principal Findings
This scoping review aimed to identify available evaluation tools that health and social care professionals can use when assessing clients’ suitability for digital health and social care. More precisely, the purpose was to review the dimensions (factors) included in the instruments and the described practical usefulness of the instruments for professionals’ work. The 19 studies included in the review covered 5 different continents, which reflects the currency and importance of the topic worldwide. A substantial part of the studies was published after 2020, which can be thought to reflect the COVID-19 era. The variety of digital services in health and social care grew exponentially during the pandemic [51,52], simultaneously increasing the need to evaluate the possibilities and challenges of different user groups to use and benefit from these services [12]. This review identified 12 different assessment instruments that could be used for this purpose. Interestingly, none of them were developed or placed in the context of social care. However, this does not mean that the discovered instruments and their dimensions, particularly in areas such as technical skills, remote communication, attitudes, or existing facilities, for example, cannot also be used to assess suitability for digital social care. Since developing and testing entirely new instruments is a lengthy process, it would be beneficial to consider and explore the applicability of the identified suitability dimensions in the context of social work. All the instruments were based on subjective self-assessment, except for DHLI, which additionally included performance-based items that tested the client’s ability to apply the skills in a fictional situation [44]. It is clear that future studies would benefit from considering more objective methods to evaluate the determinants that may influence an individual’s engagement with digital health [14].
From the identified instruments, it was possible to distinguish numerous dimensions that measured different aspects of a client’s suitability for digital health. The highest number of individual dimensions focused on clients’ skills, particularly the ability to access, evaluate, process, and use web-based health-related information, or in other words, digital health literacy, or eHL. The fact that dimensions related to eHL were included in several instruments most likely reflects its perceived weight and importance when assessing a client’s potential to use and benefit from digital health. Several studies reported that the eHL level is associated with the client’s digital service use [26,27,31,33], and a recent literature review also concluded that eHL has a positive correlation with health-promoting behavior patterns [53]. Both of these findings reinforce the relevance of its assessment. However, focusing only on eHL does not provide an overall picture of the skills needed to use digital health. According to this review, professionals should also consider the client’s technical skills (eg, familiarity with technology and computer use and the ability to use apps) and the skills needed for internet-based communication, which is seen as an essential part of transactional eHL [41,54].
In this review, the client’s general ability to maintain health emerged as another central assessment area. This finding is logical because, as digital health technologies become more common, clients are increasingly expected to actively participate in managing their health and well-being by using them [1,4]. Thus, clients need sufficient health literacy in the context of digital health [55]. This refers to multiple competencies related to “accessing, understanding, appraising, and applying health information in the domains of health care, disease prevention, and health promotion” [56], which were well-displayed in the reviewed instruments (Table 2). The association between health literacy and digital health use was not reported in the included studies. However, previous research suggests that health literacy is connected to the person’s tendency to search for health-related information on the internet [55,57] and the use of health apps and patient portals [58]. Based on these results, professionals could simultaneously promote the use of digital health by assessing clients’ health literacy and striving to improve a possible low literacy level. In addition to health literacy, this review suggests that attention should be paid to clients’ overall health-maintaining activity, including the skills and techniques to manage health issues and the ability to monitor their own condition and take appropriate steps for self-care. Moreover, the client’s familiarity with the health care system, concepts, and terminology was present in the instruments, which indicates that the ability to navigate the health care system is recognized as an important competency for clients to take advantage of digital health.
The role of dimensions related to attitudes and experiences was notably small in the instruments, given that previous studies have emphasized their importance in experiencing the benefits of digital health [12,59]. While 2 instruments included dimensions measuring clients’ motivation, confidence, and comfort to use digital health [36,38], a few more considered the perceived safety and trust issues of digital health [36,37,41,44]. Previous research especially supports the assessment of the latter aspects, as security, privacy, and confidentiality issues have been found to be considerable barriers to the use of digital health, especially among different vulnerable groups [12,60,61]. Another important finding in the examined instruments is their almost negligible focus on practical matters, such as the necessary equipment and facilities to use digital health, which were only considered in 1 instrument [42]. It is essential to ensure that the client can use digital health in a private setting, as it could prevent violations of personal data privacy and improve a secure user experience [12,62].
From the point of view of the practical usefulness of the instruments, the studies hardly provided any thresholds for the values obtained (eg, what is considered high and low value) that could help professionals make informed decisions for clients’ care plans. The aspects of practical usefulness described in the studies were mainly based on the views of the authors. The most frequently mentioned aspects were the instrument’s ability to help professionals target the right digital solutions to the clients for whom they were suitable [27,30,31,38,41,42,44] and identify the clients who needed the most support, training, and assistance [29,36,39,40,44]. Only 1 study disclosed that, with the information obtained, professionals could better empower clients to take care of their own health with digital resources [26]. Based on the fact that the concept of empowerment has been increasingly discussed in connection with the rapid spread of digital health [63], it could have been expected to emerge more often in the studies. From a practical usefulness perspective, it is also important to consider that the concept of digital health encompasses a wide range of solutions and services, where client suitability, required skills, and other prerequisites can vary. For example, interactive services with professionals may demand different conditions than those used entirely independently and without interactive elements. Therefore, it is important to further consider the importance and applicability of the identified assessment areas when guiding clients to various digital services in the future.
Finally, it is worth considering whether the correct approach is to discuss the client’s suitability for using digital health and social care or whether the discussion should focus on the suitability of digital services for the clients. Developing digital services that are easy to use and accessible for everyone is a key goal [64], and equal access is a central (although only 1 among many) contributing factor in realizing digital health equity [65,66]. Digital health technologies have already increased the unequal distribution of health care services to some extent [67]. Thus, it is important that people are still offered the opportunity for face-to-face transactions if they do not have the necessary skills, willingness, or facilities to act digitally. The professionals’ role in making this assessment is crucial, and they need easy-to-use and valid tools that comprehensively assess the clients’ prerequisites for using digital solutions. It is still, however, important to note that the purpose of the assessment is not to exclude anyone from digital services but to help identify possible needs for support and take appropriate measures to remove barriers to use. Whether professionals have the required skills and sufficient time allocated for this in addition to their already heavy workload is another matter that requires further consideration.
Limitations
Although we used several databases in the review, used the expertise of a research librarian, and worked in a group to discover eligible studies, it cannot be ruled out that some relevant instruments may have been missing. The lack of a manual search of relevant journals may have also limited the results of this review. Furthermore, this review excluded studies published in non-English journals, which may narrow the perspective on the topic. Finally, when using the conclusions of this review, one must acknowledge the limitations associated with the scoping review method, meaning the lack of formal quality appraisal of the included studies.
Conclusions
This scoping review highlighted the need for comprehensive evaluation tools that can assess clients’ suitability for digital health and social care. While 12 assessment instruments were identified, none of them were developed specifically for social care. The dimensions included in the instruments emphasized the variety of required digital skills, a person’s general ability to maintain health, attitudes, and experiences, as well as practical matters such as equipment requirements. The studies also raised various aspects of the instruments’ practical usefulness, such as the ability to target appropriate digital solutions, identify support needs, and promote optimal use. However, the lack of defined suitability thresholds for values obtained (indicating a person’s likelihood of successfully using digital services) hinders informed decision-making when selecting suitable services for the client. Professionals play a crucial role in promoting clients’ use of digital technologies and need comprehensive and user-friendly tools to evaluate their ability to use digital solutions. In the future, it is necessary to further examine how different instruments and their dimensions predict clients’ use of digital health and social care. This information could ensure that the assessment would focus on the most relevant and essential factors related to the clients. Finally, the usability of the found instruments should be considered from the perspective of digital social services, as many themes (such as technical skills, remote communication, social support, existing facilities, or security issues) can equally be pivotal in supporting a client’s ability to benefit from digital social care. However, it is possible that the client profile in social services differs from those in need of health care, and digital social work possesses some unique characteristics that may not all be adequately captured by digital health dimensions. This emphasizes the possible need to develop and use separate assessment methods.
Acknowledgments
This work was supported by the Strategic Research Council at the Academy of Finland (grant 352501). The funding source was not involved in the review design, analysis, interpretation of findings, writing of the article, or in the decision to submit the article for publication.
Abbreviations
- CeHLS-D
Condition-Specific eHealth Literacy Scale for Diabetes
- DHLI
Digital Health Literacy Instrument
- DHLS
Digital Health Care Literacy Scale
- DHTL-AQ
Digital Health Technology Literacy Assessment Questionnaire
- eHEALS
eHealth Literacy Scale
- eHL
eHealth literacy
- eHLA
eHealth Literacy Assessment Toolkit
- READHY
Readiness and Enablement Index for Health Technology
- TeHLI
Transactional eHealth Literacy Instrument
Search strategies and included studies.
PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) checklist.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Global strategy on digital health 2020-2025. World Health Organization. 2020. [2023-04-25]. https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf .
- 2.World Health Organization. World Health Organization; 2018. [2023-04-30]. Digital technologies: shaping the future of primary health care. https://apps.who.int/iris/bitstream/handle/10665/326573/WHO-HIS-SDS-2018.55-eng.pdf?sequence=1&isAllowed=y . [Google Scholar]
- 3.Barbosa W, Zhou K, Waddell E, Myers T, Dorsey ER. Improving access to care: telemedicine across medical domains. Annu Rev Public Health. 2021;42:463–481. doi: 10.1146/annurev-publhealth-090519-093711. https://www.annualreviews.org/doi/10.1146/annurev-publhealth-090519-093711 . [DOI] [PubMed] [Google Scholar]
- 4.eHealth: digital health and care. European Commission. 2019. [2023-04-25]. https://health.ec.europa.eu/ehealth-digital-health-and-care/overview_en .
- 5.Ronquillo Y, Meyers A, Korvek SJ. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Digital health. [PubMed] [Google Scholar]
- 6.Lundgren A, Ormstrup VL, Bogason Á, Penje O, Jokinen JC, Wang S, Norlen G, Heleniak T, Löfving L. Digital health care and social care: regional development impacts in the Nordic countries. Nordic Co-operation. 2020. [2023-11-24]. https://norden.diva-portal.org/smash/record.jsf?pid=diva2%3A1478007&dswid=-5318 .
- 7.Løberg IB. Efficiency through digitalization? How electronic communication between frontline workers and clients can spur a demand for services. Gov Inf Q. 2021;38(2):101551. doi: 10.1016/j.giq.2020.101551. https://sciencedirect.com/science/article/pii/S0740624X20303300?via%3Dihub . [DOI] [Google Scholar]
- 8.Naslund JA, Aschbrenner KA, Araya R, Marsch LA, Unützer J, Patel V, Bartels SJ. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. Lancet Psychiatry. 2017;4(6):486–500. doi: 10.1016/S2215-0366(17)30096-2. https://europepmc.org/abstract/MED/28433615 .S2215-0366(17)30096-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Information to support well-being and service renewal. eHealth and eSocial strategy 2020. Ministry of Social Affairs and Health. 2015. [2023-04-25]. https://julkaisut.valtioneuvosto.fi/bitstream/handle/10024/74459/URN_ISBN_978-952-00-3575-4.pdf .
- 10.Pita-Barros P, Bourek A, Brouwer W, Lehtonen L. European Commission. Assessing the Impact of Digital Transformation of Health Services. Report of the EXPH (Expert Panel on effective ways of investing in Health) 2019. [2023-05-01]. https://health.ec.europa.eu/system/files/2019-11/022_digitaltransformation_en_0.pdf .
- 11.Bucci S, Berry N, Morris R, Berry K, Haddock G, Lewis S, Edge D. "They are not hard-to-reach clients. We have just got hard-to-reach services." Staff views of digital health tools in specialist mental health services. Front Psychiatry. 2019;10:344. doi: 10.3389/fpsyt.2019.00344. https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00344/full . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaihlanen AM, Virtanen L, Buchert U, Safarov N, Valkonen P, Hietapakka L, Hörhammer I, Kujala S, Kouvonen A, Heponiemi T. Towards digital health equity—a qualitative study of the challenges experienced by vulnerable groups in using digital health services in the COVID-19 era. BMC Health Serv Res. 2022;22(1):188. doi: 10.1186/s12913-022-07584-4. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-022-07584-4 .10.1186/s12913-022-07584-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lyles CR, Wachter RM, Sarkar U. Focusing on digital health equity. JAMA. 2021;326(18):1795–1796. doi: 10.1001/jama.2021.18459.2785583 [DOI] [PubMed] [Google Scholar]
- 14.Faux-Nightingale A, Philp F, Chadwick D, Singh B, Pandyan A. Available tools to evaluate digital health literacy and engagement with eHealth resources: a scoping review. Heliyon. 2022;8(8):e10380. doi: 10.1016/j.heliyon.2022.e10380. https://www.cell.com/heliyon/fulltext/S2405-8440(22)01668-1?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS2405844022016681%3Fshowall%3Dtrue .S2405-8440(22)01668-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griebel L, Enwald H, Gilstad H, Pohl AL, Moreland J, Sedlmayr M. eHealth literacy research-Quo vadis? Inform Health Soc Care. 2018;43(4):427–442. doi: 10.1080/17538157.2017.1364247. [DOI] [PubMed] [Google Scholar]
- 16.Kainiemi E, Vehko T, Kyytsönen M, Hörhammer I, Kujala S, Jormanainen V, Heponiemi T. The factors associated with nonuse of and dissatisfaction with the national patient portal in Finland in the era of COVID-19: population-based cross-sectional survey. JMIR Med Inform. 2022;10(4):e37500. doi: 10.2196/37500. https://medinform.jmir.org/2022/4/e37500 .v10i4e37500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karisalmi N, Kaipio J, Kujala S. The role of healthcare personnel in motivating and guiding patients in the use of eHealth services. Finn J Ehealth Ewelfare. 2018;10(2-3):210–220. doi: 10.23996/fjhw.69145. https://journal.fi/finjehew/article/view/69145 . [DOI] [Google Scholar]
- 18.Kaihlanen AM, Laukka E, Nadav J, Närvänen J, Saukkonen P, Koivisto J, Heponiemi T. The effects of digitalisation on health and social care work: a qualitative descriptive study of the perceptions of professionals and managers. BMC Health Serv Res. 2023;23(1):714. doi: 10.1186/s12913-023-09730-y. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-023-09730-y .10.1186/s12913-023-09730-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Galpin K, Sikka N, King SL, Horvath KA, Shipman SA, AAMC Telehealth Advisory Committee Expert consensus: telehealth skills for health care professionals. Telemed J E Health. 2021;27(7):820–824. doi: 10.1089/tmj.2020.0420. https://www.liebertpub.com/doi/epdf/10.1089/tmj.2020.0420 . [DOI] [PubMed] [Google Scholar]
- 20.Jarva E, Oikarinen A, Andersson J, Tuomikoski AM, Kääriäinen M, Meriläinen M, Mikkonen K. Healthcare professionals' perceptions of digital health competence: a qualitative descriptive study. Nurs Open. 2022;9(2):1379–1393. doi: 10.1002/nop2.1184. https://onlinelibrary.wiley.com/doi/10.1002/nop2.1184 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al Salman A, Fatehi A, Crijns TJ, Ring D, Doornberg JN. Surgeon preferences are associated with utilization of telehealth in fracture care. Eur J Trauma Emerg Surg. 2023;49(1):261–272. doi: 10.1007/s00068-022-02065-z. https://link.springer.com/article/10.1007/s00068-022-02065-z .10.1007/s00068-022-02065-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dahlgren C, Dackehag M, Wändell P, Rehnberg C. Determinants for use of direct-to-consumer telemedicine consultations in primary healthcare-a registry based total population study from Stockholm, Sweden. BMC Fam Pract. 2021;22(1):133. doi: 10.1186/s12875-021-01481-1. https://bmcprimcare.biomedcentral.com/articles/10.1186/s12875-021-01481-1 .10.1186/s12875-021-01481-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacob C, Sezgin E, Sanchez-Vazquez A, Ivory C. Sociotechnical factors affecting patients' adoption of mobile health tools: systematic literature review and narrative synthesis. JMIR Mhealth Uhealth. 2022;10(5):e36284. doi: 10.2196/36284. https://mhealth.jmir.org/2022/5/e36284 .v10i5e36284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, Godfrey CM, Khalil H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–2126. doi: 10.11124/JBIES-20-00167. https://journals.lww.com/jbisrir/fulltext/2020/10000/updated_methodological_guidance_for_the_conduct_of.4.aspx .02174543-202010000-00004 [DOI] [PubMed] [Google Scholar]
- 25.Marwaha JS, Landman AB, Brat GA, Dunn T, Gordon WJ. Deploying digital health tools within large, complex health systems: key considerations for adoption and implementation. NPJ Digit Med. 2022;5(1):13. doi: 10.1038/s41746-022-00557-1. https://www.nature.com/articles/s41746-022-00557-1 .10.1038/s41746-022-00557-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang A, Schulz PJ. The measurements and an elaborated understanding of Chinese eHealth Literacy (C-eHEALS) in chronic patients in China. Int J Environ Res Public Health. 2018;15(7):1553. doi: 10.3390/ijerph15071553. https://www.mdpi.com/1660-4601/15/7/1553 .ijerph15071553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paige SR, Krieger JL, Stellefson M, Alber JM. eHealth literacy in chronic disease patients: an item response theory analysis of the eHealth Literacy Scale (eHEALS) Patient Educ Couns. 2017;100(2):320–326. doi: 10.1016/j.pec.2016.09.008. https://www.sciencedirect.com/science/article/abs/pii/S0738399116304189?via%3Dihub .S0738-3991(16)30418-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dale JG, Lüthi A, Skaraas BF, Rundereim T, Dale B. Testing measurement properties of the Norwegian version of Electronic Health Literacy Scale (eHEALS) in a group of day surgery patients. J Multidiscip Healthc. 2020;13:241–247. doi: 10.2147/JMDH.S242985. https://www.dovepress.com/testing-measurement-properties-of-the-norwegian-version-of-electronic--peer-reviewed-fulltext-article-JMDH .242985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hyde LL, Boyes AW, Evans TJ, Mackenzie LJ, Sanson-Fisher R. Three-factor structure of the eHealth literacy scale among magnetic resonance imaging and computed tomography outpatients: a confirmatory factor analysis. JMIR Hum Factors. 2018;5(1):e6. doi: 10.2196/humanfactors.9039. https://humanfactors.jmir.org/2018/1/e6/ v5i1e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin CY, Broström A, Griffiths MD, Pakpour AH. Psychometric evaluation of the persian eHealth Literacy Scale (eHEALS) among elder Iranians with heart failure. Eval Health Prof. 2020;43(4):222–229. doi: 10.1177/0163278719827997. [DOI] [PubMed] [Google Scholar]
- 31.Noblin AM, Wan TTH, Fottler M. The impact of health literacy on a patient's decision to adopt a personal health record. Perspect Health Inf Manag. 2012;9(Fall):1–13. https://europepmc.org/abstract/MED/23209454 . [PMC free article] [PubMed] [Google Scholar]
- 32.Richtering SS, Morris R, Soh SE, Barker A, Bampi F, Neubeck L, Coorey G, Mulley J, Chalmers J, Usherwood T, Peiris D, Chow CK, Redfern J. Examination of an eHealth literacy scale and a health literacy scale in a population with moderate to high cardiovascular risk: rasch analyses. PLoS One. 2017;12(4):e0175372. doi: 10.1371/journal.pone.0175372. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0175372 .PONE-D-16-18163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chung SY, Nahm ES. Testing reliability and validity of the eHealth Literacy Scale (eHEALS) for older adults recruited online. Comput Inform Nurs. 2015;33(4):150–156. doi: 10.1097/CIN.0000000000000146. https://europepmc.org/abstract/MED/25783223 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen YC, Cheng C, Osborne RH, Kayser L, Liu CY, Chang LC. Validity testing and cultural adaptation of the eHealth Literacy Questionnaire (eHLQ) among people with chronic diseases in Taiwan: mixed methods study. J Med Internet Res. 2022;24(1):e32855. doi: 10.2196/32855. https://www.jmir.org/2022/1/e32855 .v24i1e32855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheng C, Elsworth GR, Osborne RH. Validity evidence of the eHealth Literacy Questionnaire (eHLQ) part 2: mixed methods approach to evaluate test content, response process, and internal structure in the Australian community health setting. J Med Internet Res. 2022;24(3):e32777. doi: 10.2196/32777. https://www.jmir.org/2022/3/e32777 .v24i3e32777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kayser L, Rossen S, Karnoe A, Elsworth G, Vibe-Petersen J, Christensen JF, Ried-Larsen M, Osborne RH. Development of the multidimensional readiness and enablement index for health technology (READHY) tool to measure individuals' health technology readiness: initial testing in a cancer rehabilitation setting. J Med Internet Res. 2019;21(2):e10377. doi: 10.2196/10377. https://www.jmir.org/2019/2/e10377/ v21i2e10377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.He Y, Guo L, Zauszniewski JA, Wei M, Zhang G, Lei X, Liu Y. A reliability and validity study of the electronic health literacy scale among stroke patients in China. Top Stroke Rehabil. 2023;30(3):272–280. doi: 10.1080/10749357.2021.2016100. [DOI] [PubMed] [Google Scholar]
- 38.Karnoe A, Furstrand D, Christensen KB, Norgaard O, Kayser L. Assessing competencies needed to engage with digital health services: development of the eHealth literacy assessment toolkit. J Med Internet Res. 2018;20(5):e178. doi: 10.2196/jmir.8347. https://www.jmir.org/2018/5/e178/ v20i5e178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee EH, Lee YW, Lee KW, Kim HJ, Hong S, Kim SH, Kang EH. Development and psychometric evaluation of a new brief scale to measure eHealth literacy in people with type 2 diabetes. BMC Nurs. 2022;21(1):297. doi: 10.1186/s12912-022-01062-2. https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-022-01062-2 .10.1186/s12912-022-01062-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nelson LA, Pennings JS, Sommer EC, Popescu F, Barkin SL. A 3-item measure of digital health care literacy: development and validation study. JMIR Form Res. 2022;6(4):e36043. doi: 10.2196/36043. https://formative.jmir.org/2022/4/e36043 .v6i4e36043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Paige SR, Stellefson M, Krieger JL, Miller MD, Cheong J, Anderson-Lewis C. Transactional eHealth literacy: developing and testing a multi-dimensional instrument. J Health Commun. 2019;24(10):737–748. doi: 10.1080/10810730.2019.1666940. https://europepmc.org/abstract/MED/31583963 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams NMR, Hurt-Thaut C, Thaut MH. Novel screening tool and considerations for music therapists serving autistic individuals via telehealth: qualitative results from a survey of clinicians' experiences. J Music Ther. 2022;59(4):368–393. doi: 10.1093/jmt/thac009.6967074 [DOI] [PubMed] [Google Scholar]
- 43.Yoon J, Lee M, Ahn JS, Oh D, Shin SY, Chang YJ, Cho J. Development and validation of digital health technology literacy assessment questionnaire. J Med Syst. 2022;46(2):13. doi: 10.1007/s10916-022-01800-8. https://link.springer.com/article/10.1007/s10916-022-01800-8 .10.1007/s10916-022-01800-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.van der Vaart R, Drossaert C. Development of the digital health literacy instrument: measuring a broad spectrum of health 1.0 and health 2.0 skills. J Med Internet Res. 2017;19(1):e27. doi: 10.2196/jmir.6709. https://www.jmir.org/2017/1/e27/ v19i1e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pollock D, Peters MDJ, Khalil H, McInerney P, Alexander L, Tricco AC, Evans C, de Moraes ÉB, Godfrey CM, Pieper D, Saran A, Stern C, Munn Z. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid Synth. 2023;21(3):520–532. doi: 10.11124/JBIES-22-00123. https://journals.lww.com/jbisrir/fulltext/2023/03000/recommendations_for_the_extraction,_analysis,_and.7.aspx .02174543-990000000-00076 [DOI] [PubMed] [Google Scholar]
- 46.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x.JAN4569 [DOI] [PubMed] [Google Scholar]
- 47.Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res. 2006;8(4):e27. doi: 10.2196/jmir.8.4.e27. https://www.jmir.org/2006/4/e27/ v8i4e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kayser L, Karnoe A, Furstrand D, Batterham R, Christensen KB, Elsworth G, Osborne RH. A multidimensional tool based on the eHealth literacy framework: development and initial validity testing of the eHealth Literacy Questionnaire (eHLQ) J Med Internet Res. 2018;20(2):e36. doi: 10.2196/jmir.8371. https://www.jmir.org/2018/2/e36/ v20i2e36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ) BMC Public Health. 2013;13:658. doi: 10.1186/1471-2458-13-658. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-658 .1471-2458-13-658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seçkin G, Hughes S, Yeatts D, Degreve T. Digital pathways to positive health perceptions: does age moderate the relationship between medical satisfaction and positive health perceptions among middle-aged and older internet users? Innov Aging. 2019;3(1):igy039. doi: 10.1093/geroni/igy039. https://academic.oup.com/innovateage/article/3/1/igy039/5288188?login=false .igy039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ting DSW, Carin L, Dzau V, Wong TY. Digital technology and COVID-19. Nat Med. 2020;26(4):459–461. doi: 10.1038/s41591-020-0824-5. https://www.nature.com/articles/s41591-020-0824-5 .10.1038/s41591-020-0824-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Keesara S, Jonas A, Schulman K. COVID-19 and health care's digital revolution. N Engl J Med. 2020;382(23):e82. doi: 10.1056/NEJMp2005835. https://www.nejm.org/doi/10.1056/NEJMp2005835 . [DOI] [PubMed] [Google Scholar]
- 53.Kim K, Shin S, Kim S, Lee E. The relation between eHealth literacy and health-related behaviors: systematic review and meta-analysis. J Med Internet Res. 2023;25:e40778. doi: 10.2196/40778. https://www.jmir.org/2023/1/e40778 .v25i1e40778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paige SR, Stellefson M, Krieger JL, Anderson-Lewis C, Cheong J, Stopka C. Proposing a transactional model of eHealth literacy: concept analysis. J Med Internet Res. 2018;20(10):e10175. doi: 10.2196/10175. https://www.jmir.org/2018/10/e10175/ v20i10e10175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim H, Xie B. Health literacy in the eHealth era: a systematic review of the literature. Patient Educ Couns. 2017;100(6):1073–1082. doi: 10.1016/j.pec.2017.01.015. https://www.sciencedirect.com/science/article/abs/pii/S0738399117300150?via%3Dihub .S0738-3991(17)30015-0 [DOI] [PubMed] [Google Scholar]
- 56.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-12-80 .1471-2458-12-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Manganello J, Gerstner G, Pergolino K, Graham Y, Falisi A, Strogatz D. The relationship of health literacy with use of digital technology for health information: implications for public health practice. J Public Health Manag Pract. 2017;23(4):380–387. doi: 10.1097/PHH.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 58.Mackert M, Mabry-Flynn A, Champlin S, Donovan EE, Pounders K. Health literacy and health information technology adoption: the potential for a new digital divide. J Med Internet Res. 2016;18(10):e264. doi: 10.2196/jmir.6349. https://www.jmir.org/2016/10/e264/ v18i10e264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Heponiemi T, Gluschkoff K, Leemann L, Manderbacka K, Aalto AM, Hyppönen H. Digital inequality in Finland: access, skills and attitudes as social impact mediators. N Media Soc. 2021;25(9):2475–2491. doi: 10.1177/14614448211023007. https://journals.sagepub.com/doi/10.1177/14614448211023007 . [DOI] [Google Scholar]
- 60.Liberati E, Richards N, Parker J, Willars J, Scott D, Boydell N, Pinfold V, Martin G, Dixon-Woods M, Jones P. Remote care for mental health: qualitative study with service users, carers and staff during the COVID-19 pandemic. BMJ Open. 2021;11(4):e049210. doi: 10.1136/bmjopen-2021-049210. https://bmjopen.bmj.com/content/11/4/e049210 .bmjopen-2021-049210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Melchiorre MG, Papa R, Rijken M, van Ginneken E, Hujala A, Barbabella F. eHealth in integrated care programs for people with multimorbidity in Europe: insights from the ICARE4EU project. Health Policy. 2018;122(1):53–63. doi: 10.1016/j.healthpol.2017.08.006. https://www.sciencedirect.com/science/article/pii/S0168851017302063?via%3Dihub .S0168-8510(17)30206-3 [DOI] [PubMed] [Google Scholar]
- 62.Houser SH, Flite CA, Foster SL. Privacy and security risk factors related to telehealth services—a systematic review. Perspect Health Inf Manag. 2023;20(1):1f. https://europepmc.org/abstract/MED/37215337 .phim0020-0001b [PMC free article] [PubMed] [Google Scholar]
- 63.Risling T, Martinez J, Young J, Thorp-Froslie N. Evaluating patient empowerment in association with eHealth technology: scoping review. J Med Internet Res. 2017;19(9):e329. doi: 10.2196/jmir.7809. https://www.jmir.org/2017/9/e329/ v19i9e329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Henni SH, Maurud S, Fuglerud KS, Moen A. The experiences, needs and barriers of people with impairments related to usability and accessibility of digital health solutions, levels of involvement in the design process and strategies for participatory and universal design: a scoping review. BMC Public Health. 2022;22(1):35. doi: 10.1186/s12889-021-12393-1. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-12393-1 .10.1186/s12889-021-12393-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lyles CR, Nguyen OK, Khoong EC, Aguilera A, Sarkar U. Multilevel determinants of digital health equity: a literature synthesis to advance the field. Annu Rev Public Health. 2023;44:383–405. doi: 10.1146/annurev-publhealth-071521-023913. https://www.annualreviews.org/doi/10.1146/annurev-publhealth-071521-023913 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Richardson S, Lawrence K, Schoenthaler AM, Mann D. A framework for digital health equity. NPJ Digit Med. 2022;5(1):119. doi: 10.1038/s41746-022-00663-0. https://www.nature.com/articles/s41746-022-00663-0 .10.1038/s41746-022-00663-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yao R, Zhang W, Evans R, Cao G, Rui T, Shen L. Inequities in health care services caused by the adoption of digital health technologies: scoping review. J Med Internet Res. 2022;24(3):e34144. doi: 10.2196/34144. https://www.jmir.org/2022/3/e34144 .v24i3e34144 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategies and included studies.
PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) checklist.


