Abstract
Social isolation is a potent predictor of poor health, mortality, and dementia risk. A great deal of research across national contexts provides causal evidence for these linkages and identifies key explanatory mechanisms through which isolation affects health. Research on social isolation recognizes that some people are more likely than others to be isolated, but over the past several decades, researchers have focused primarily on the consequences of isolation for health rather than a systematic assessment of the social conditions that foster isolation over the life course. In this article, we review the available evidence on inequities in social isolation and develop a conceptual framework to guide future research on structural systems that fuel social isolation over the life course. Future work in this area has the potential to identify root causes of inequality in social isolation, as well as targeted policy levers to reduce isolation in vulnerable populations.
Keywords: social isolation, disparities, life course, gender, race, ethnicity, sexuality, socioeconomic status
INTRODUCTION
Social connection to other people is fundamentally important to population health and well-being (Cacioppo & Patrick 2008, Umberson & Montez 2010). Social isolation, defined as the objective lack of social contact with others, is strongly associated with wide-ranging physical and mental health problems as well as increased risk for mortality and dementia (NASEM 2020a). Indeed, social isolation is as strongly associated with mortality risk as are smoking and obesity (Holt-Lunstad et al. 2017, Pantell et al. 2013). These findings are based on several decades of research that have drawn on the most sophisticated data and methods available and have examined a wide range of well-validated biomedical and psychosocial outcomes (NASEM 2020a). We now know a great deal about the biosocial mechanisms and pathways through which social isolation impacts health and mortality risk. Yet we know much less about socially patterned variation in who is most at risk for isolation, why some groups are more at risk of isolation than others, and when in the life course those risks emerge. This research gap is surprising given the strong evidence that social isolation contributes to health disadvantage, and because identifying socially patterned inequality in resources is a bedrock of sociological research.
This review focuses on what we know about inequities in social isolation in the United States and identifies future directions for research. Although other indicators of social position matter for isolation risk, we have focused particularly on race/ethnicity, gender, sexual orientation, and socioeconomic status (SES). We develop a conceptual framework to guide future research and to illustrate how inequality in isolation has its roots in the early life course and cascades over time to create accumulating disadvantage for some populations more than others. We must first understand which populations are most disadvantaged, as well as when and why they are disadvantaged, in order to address isolation as a public health concern and alleviate health disparities (Klinenberg 2016).
EVIDENCE LINKING SOCIAL ISOLATION TO HEALTH
In this article, we focus specifically on social isolation rather than other dimensions of social connection such as loneliness and social support. The key distinction between isolation and loneliness/support is that the former refers to the objective absence of social connections whereas the latter refers to subjective assessments about one’s social connections. The preponderance of the evidence indicates that social isolation is a stronger predictor of health/mortality than are support and loneliness, that objective and subjective assessments are not highly correlated (Coyle & Dugan 2012, Perissinotto & Covinsky 2014), and that isolation affects health/mortality net of subjective assessments about one’s social connections (Steptoe et al. 2013, Tanskanen & Anttila 2016). A related literature on social networks is distinguished from social isolation, per se, in that network analysts attend primarily to the composition of, and exchanges between, members of social networks (Cornwell & Schafer 2016, Perry et al. 2018), whereas social isolation considers connectivity based on network size, frequency of interaction, and participation in social activities and groups. The following review incorporates relevant network research that focuses on network size and predictors of network size.
As noted above, we have substantial evidence for a causal link between social isolation and health, including mortality risk. It is not only extreme levels of social isolation that increase risk; there is a dose-response relationship between isolation and health/mortality risk (Tanskanen & Anttila 2016, Yang et al. 2016). Moreover, isolation increases subsequent health/mortality risk net of baseline health status (Holt-Lunstad et al. 2015, Read et al. 2020, Steptoe et al. 2013). The link between isolation and health has been observed from adolescence through late life (Yang et al. 2016). As this evidence has been reviewed in comprehensive reports, meta-analyses, and articles, we will not review those studies in detail here (e.g., Holt-Lunstad et al. 2015, Penninkilampi et al. 2018, Valtorta et al. 2016). Figure 1, from a recent National Academies report on older populations, summarizes the basic components of the isolation/health process based on prior studies (NASEM 2020a).
Figure 1.
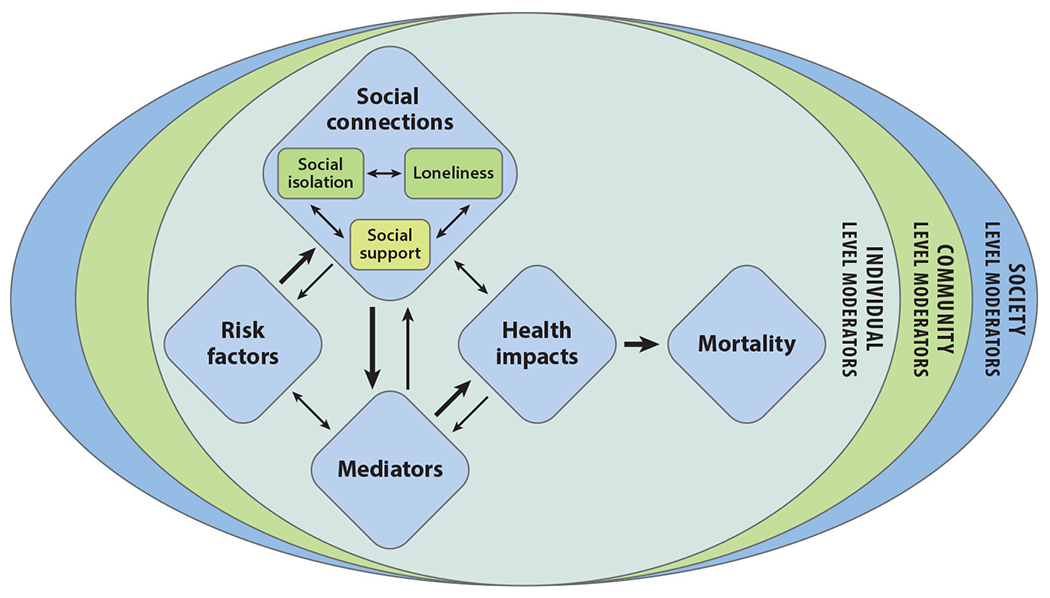
Social isolation and health model. Figure adapted with permission from NASEM (2020a); copyright 2020 National Academies of Sciences, Engineering, and Medicine; permission conveyed through Copyright Clearance Center, Inc.; retrieved from https://nap.nationalacadeimes.org/catalog/25663/social-isolation-and-loneliness-in-older-adults-opportunities-for-the opportunities-for-the.
Much of the research on social isolation and health has focused on identifying the interconnected biopsychosocial mechanisms (or pathways) that explain how isolation affects health. Many of these mechanisms are represented by the mediators indicated in Figure 1. Again, this evidence is reviewed elsewhere and we will not review it in detail here (e.g., NASEM 2020a). In brief, prior studies emphasize psychological mechanisms such as depression and anxiety, social mechanisms including stress, behavioral mechanisms such as drug and alcohol use, and biological mechanisms including immune and cardiovascular functioning (Uchino et al. 2012, Yang et al. 2013b).
Our main focus is on the social structural risk factors that shape social isolation, with a primary focus on sociodemographic risk factors. Certainly, risk factors for isolation have not been ignored in prior research, as they are included in Figure 1, but this is a box that needs to be unpacked. The term “risk factors” has been used to refer to wide-ranging concepts including sociodemographic characteristics, stressful life events, living alone, poor health, depression, chronic conditions, functional limitations, and cognitive impairment (Holt-Lunstad & Smith 2016, NASEM 2020a, Nicholson 2012). Some of these risk factors could also be classified as indicators of isolation (e.g., living alone), as mediators/mechanisms linking isolation and health (e.g., stressors), or as health consequences of isolation (e.g., chronic conditions). Moreover, most studies on social isolation include sociodemographic characteristics as control variables when predicting health outcomes, but sociodemographic characteristics shape the likelihood of experiencing risk factors for social isolation, and this is overlooked when sociodemographic characteristics are theorized as control variables. Prior research has inadvertently clouded the focus on sociodemographic risk factors—which indicate one’s structural position in society—as a predictor of isolation throughout life.
We argue that sociodemographic position is a fundamental cause of other risks that increase social isolation. People are born into social structural systems associated with race/ethnicity, gender, sexual orientation, and SES, and these systems then launch their life trajectories, including trajectories of risk for isolation throughout life.
UPSTREAM DETERMINANTS OF ISOLATION
Social determinants of health research emphasizes both upstream and downstream factors that influence health (Bharmal et al. 2015, Gehlert et al. 2008, Ratcliff 2017). Upstream determinants refer to social factors that are largely unmodifiable, such as sociodemographic characteristics, and to structural systems of stratification based on these characteristics. Downstream factors refer to sequelae that originate from social structural experiences and are more proximal determinants of health. Most research on social isolation has focused on isolation as a more downstream predictor of health and mortality, with additional attention to factors such as stress and health behaviors that might help to explain how isolation affects health. This focus on isolation as a determinant of health, while important, may have diverted attention from the structural systems and contexts that give rise to social isolation in the first place. Indeed, Link & Phelan (1995, p. 80) have argued that sociologists and epidemiologists attend too much to analyzing the proximal (downstream) determinants of health, while neglecting a focus on social structural factors that are fundamental causes of health, sometimes referred to as the “risk of risks.” They argue that an overemphasis on identifying the mechanisms through which social conditions influence health might lead social scientists to, “over time, lose interest in and come to neglect the importance of the social condition whose effect on health we originally sought to explain” (Link & Phelan 1995, p. 81). We suggest that this has occurred in the study of social isolation.
Sociologists and epidemiologists have engaged in a quest to identify the biosocial mechanisms linking social isolation to health rather than attending to the fundamental causes of isolation. Klinenberg (2016) recently made the case that identifying who is at risk for social isolation is an essential first step in addressing isolation as a public health problem. We underscore the importance of attending to fundamental causes when understanding the social distribution of isolation and its consequences for population health. We also add the need to identify why certain groups are more likely to experience social isolation and when in the life course this risk is greatest. In that spirit, we focus on race/ethnicity, gender, sexuality, and SES as structural systems (e.g., structural racism) that foster inequality in social isolation over the life course.
We emphasize the importance of considering change in patterns of social isolation over the life course because social conditions that influence social isolation vary throughout life. Notably, social isolation likely increases with age, although most of the evidence to this point is based on mid- to later-life populations and few studies examine changes in isolation earlier in the life course. In this article, we do not review the evidence on aging and social isolation in detail, as a National Academies report (NASEM 2020a) provides a comprehensive overview of this evidence for older populations, and points to social/psychological (e.g., retirement, bereavement) and biological (e.g., chronic conditions, pain, impaired mobility) factors that may contribute to isolation in later life. However, throughout this article, we report what is known about the intersection of age with race, ethnicity, gender, sexuality, and SES, and we underscore the need to take an intersectional view of social isolation as it begins to unfold early in the life course. Indeed, one recent longitudinal study, relying on data from the National Longitudinal Study of Adolescent to Adult Health (Add Health) and the Health and Retirement Study (HRS), shows that social isolation steadily increases from adolescence through later life, but at different rates as men and women enter midlife (Umberson et al. 2022). We now turn to a conceptual framework that might be used to organize future research in this area.
CONCEPTUAL FRAMEWORK FOR POPULATION INEQUITIES IN ISOLATION
Figure 2 illustrates the life course process by which structural systems may lead to higher levels of social isolation for some populations than others. This figure lays the framework for theorizing who is most at risk for social isolation, and why and how this disadvantage occurs, as well as when this disadvantage emerges and how it changes across the life course. The conceptual framework suggests that structural racism, structural sexism, heterosexism, and economic inequality are central to the production of inequities in social isolation as well as health inequities. Structural racism (Bailey et al. 2017, Brown & Homan 2022, Gee & Hicken 2021), structural sexism (Homan 2019), heterosexism (Hatzenbuehler 2016, Krieger 2020), and economic inequality (Pickett & Wilkinson 2015) refer to the totality of ways in which society is organized to privilege a dominant group (e.g., White individuals, men, heterosexual people) from the micro level to the macro level, in ways that fundamentally shape health inequities. As such, social isolation may be one specific pathway through which structural forms of inequality shape inequities in health.
Figure 2.
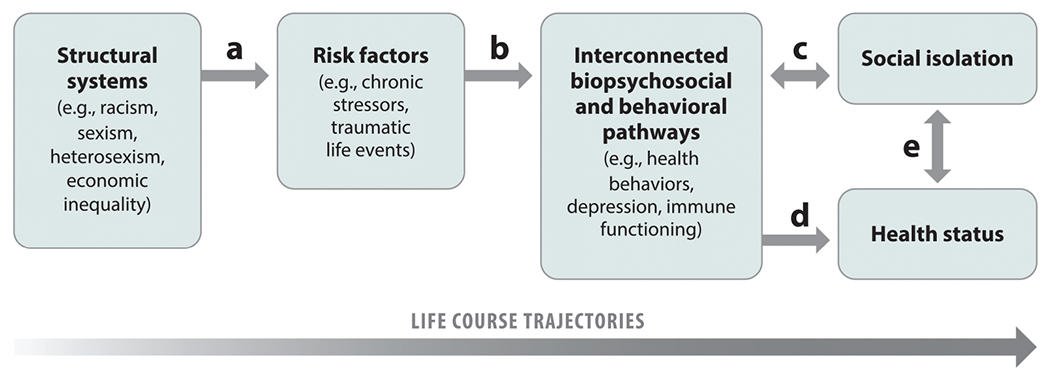
The social production of inequities in insolation over the life course. The figure presents a conceptual framework to guide studies on population inequities in isolation. The labeled arrows indicate pathways by which structural systems influence levels of social isolation over the life course.
All humans are born with a need and desire for social connection (Cacioppo & Patrick 2008). But we are born into structural systems that provide different levels of stress, opportunities, and constraints that influence our potential for social connection throughout life. For example, structural racism causes lower life expectancy for Black Americans, which then increases their risk for experiencing more family member deaths throughout life (Figure 2, arrow a). In turn, bereavement events may increase risk for self-isolation as a result of increased depression and anxiety (Figure 2, arrows b and c). The biosocial pathways stemming from bereavement, together with social isolation, can increase the likelihood of poor health (Figure 2, arrows d and e).
Attention to life course timing is crucial to this conceptual framework. Early life experiences launch trajectories of risk that are carried through late life. For example, children who experience early life trauma such as the death of a parent may be more likely to take drugs, drink heavily, or drop out of school; in turn, lower educational attainment (a social pathway) and substance use disorders (a behavioral pathway) may interfere with the formation and maintenance of long-term relationships (a social pathway)—all of which increase the risk for social isolation across the life course (Figure 2, arrow c). As people age, social isolation may exacerbate mental health problems and health-damaging behaviors (Figure 2, indicated by the double-headed arrow c), accelerating health decline. In addition to an indirect effect on health through social isolation (Figure 2, arrows c and e), interconnected biopsychosocial pathways also have a direct effect on health (Figure 2, arrow d). When drawing attention to structural systems and life course processes, the overarching story then becomes one of increasing advantage or disadvantage in social connectivity and health over the life course. Yet people often find ways to resist oppression, such as by creating families of choice or with religion/spirituality, in ways that may protect against social isolation, and these protective factors should also be systematically examined. Because some populations are more likely to be exposed to experiences that reduce social connectivity, the result is inequality in risk of social isolation over the life course. Inequality in isolation contributes to health risks but the doubleheaded arrow e in Figure 2 indicates that health problems may further exacerbate social isolation.
The processes through which structural systems shape isolation are likely to vary by race/ethnicity, gender, sexual orientation, and SES. Structural intersections further complicate the story as systems of racism, sexism, heterosexism, and classism are intersecting, overlapping, and reinforcing (Homan et al. 2021). For example, the experience of being a man or a woman is different for Black Americans compared with White Americans. Future research will need to attend to these complexities. Our primary goal in this article is to lay out a basic model than can be utilized to tell these stories of structural advantage or disadvantage in social isolation. We now turn to the available population-level evidence on race, gender, sexual orientation, and SES as predictors of social isolation; identify some of the major risk and protective factors associated with isolation across these groups; and underscore directions for future research in this area.
EVIDENCE OF INEQUITIES IN SOCIAL ISOLATION
Race/Ethnicity and Social Isolation
Research points to racial/ethnic inequities in the experience of social isolation, but large knowledge gaps remain. Many studies on social isolation merely include race/ethnicity as a control variable in models, precluding a deep understanding of which populations are most disadvantaged and why. Moreover, much of what we know about racial/ethnic inequalities in social isolation stems from research on samples of older adults. We know much less about racial/ethnic differences in social isolation in young adulthood or early midlife but, overall, studies suggest more isolation for Black and Hispanic populations. For example, using representative data from the National Health Interview Survey, Barger & Uchino (2017) report that Black and Hispanic adults over age 18 experience more social isolation than White adults. Another study using a cross-section of data from a national sample indicates that Black adults aged 30 to 90 are more likely than White adults to be unmarried and have fewer friends, and are less likely to attend group or club activities outside of church (Alcaraz et al. 2019). Data from the HRS (a representative longitudinal study of adults over 50) indicate that Black and Hispanic adults over age 50 experience greater social isolation than White adults in their baseline interview (Donnelly et al. 2021, Ertel et al. 2008, Yang et al. 2013a). However, a recent study using data from the National Health and Aging Trends Study—a representative longitudinal study of Medicare beneficiaries—found that Black and Hispanic adults aged 65 and older were less likely than White adults to experience isolation (Cudjoe et al. 2020).
We present data from Add Health (ages 12–42) and the HRS (ages 50+) in Figure 3 to illustrate mean levels of social isolation for White, Black, US-born Hispanic, and foreign-born Hispanic respondents. Following prior research (e.g., Yang et al. 2016), social isolation in Add Health was assessed across four domains: contact with parents (adolescence) or relationships status (adulthood), friend count, religious attendance, and volunteer activities. In HRS, we rely on a version of the Berkman-Syme Index developed by Yang et al. (2016), which assesses isolation across five domains: marital/cohabiting status; volunteer activities; and contact with parents, children, and neighbors. These results indicate racial/ethnic disadvantage in isolation in both datasets, with the greatest disadvantage for foreign-born Hispanics in the younger Add Health sample and for non-Hispanic Black respondents in the older HRS sample, net of controls for age, gender, educational attainment, and self-rated health.
Figure 3.
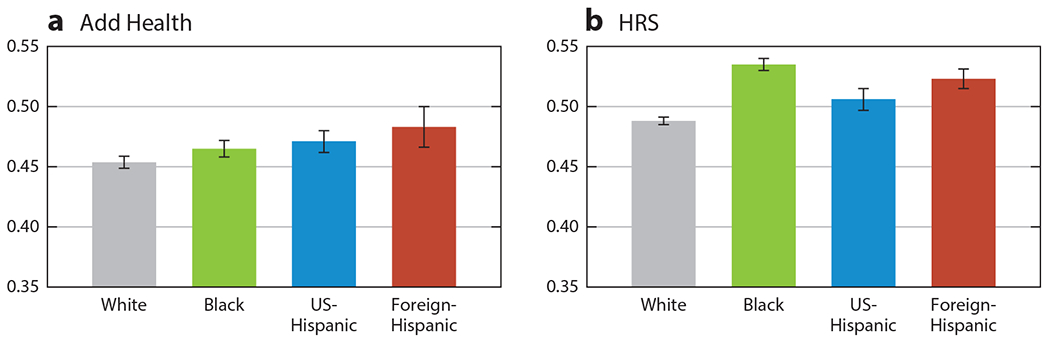
Race/ethnicity and social isolation. Measures are draw from Yang et al. (2016). The Add Health isolation scale assesses parent contact (in adolescence) or relationship status (age 18+), friend count, religious attendance, and volunteer activities. The HRS isolation scale assesses marital/cohabiting status, volunteer activities, contact with parents, contact with children, and contact with neighbors. Abbreviations: Add Health, National Longitudinal Study of Adolescent to Adult Health; HRS, Health and Retirement Study.
Inconsistent results in past studies may reflect differences by race/ethnicity in the specific items that comprise indices of social isolation, or in the age-specific composition of samples. For example, Black older adults have smaller social networks (Cornwell et al. 2008, Miyawaki 2015) and are more likely to experience network shrinkage (Cornwell 2015) and less social connection outside of church or religious settings (Liu 2011), are less likely to socialize with friends and family (Miyawaki 2015), and are more likely to have no living kin (Verdery & Margolis 2017) compared with White older adults. Miyawaki (2015) reports that Hispanic older adults also have smaller social networks and less participation at meetings and volunteering activities than White older adults. Thus, indices that rely more heavily on household composition and religious participation over social network size and participation in nonreligious activities may find lower risk of isolation among Black and Hispanic adults. Together, prior research suggests a unique combination of factors that could contribute to racial/ethnic differences in social isolation. Examining these items individually and in indices of isolation is essential to provide a holistic understanding of social isolation among Black, Hispanic, and White adults.
Overall, most of the available evidence indicates that Black and Hispanic older adults are more likely to experience social isolation than White older adults. However, we know very little about social isolation among Black, Hispanic, and White adults prior to midlife, or changes in social isolation across the life course by race/ethnicity. Moreover, we have very little systematic evidence about why Black and Hispanic adults may experience more isolation, including life events and stressors that may have roots early in the life course. Next, we discuss two primary risk factors for racial/ethnic inequities in social isolation (i.e., stress and major life events, health conditions and cognitive decline) in addition to one area of protection (i.e., certain aspects of social networks).
Stress and major life events.
As a result of systemic racism, Black and Hispanic Americans experience substantial stress and discrimination throughout life (Sternthal et al. 2011, Williams 2018). Life course exposure to stress is disproportionately experienced by Black and Hispanic compared with White Americans and includes such exposures as traumatic life events (e.g., criminal victimization, death of family members) and chronic stressors (e.g., financial strain). Differential exposure to stress is considered a key reason for racial/ethnic inequities in health and well-being (e.g., Boen 2020, Goosby et al. 2018, Sternthal et al. 2011), but differential exposure to stress may also contribute substantially to social isolation which, in turn, exacerbates health risk.
Bereavement, an example of a traumatic life event, may be a unique risk factor for the social isolation of racially minoritized populations. Exposure to bereavement is not experienced equally in the United States (Liu et al. 2022, Umberson & Donnelly 2022, Umberson et al. 2017), and an unequal burden of bereavement could reduce social networks (Cornwell 2015, Verdery & Margolis 2017) and contribute to inequity in social isolation. The stark inequity in exposure to bereavement puts Black and Hispanic adults at greater risk of social isolation given linkages between bereavement and isolation (NASEM 2020a, Umberson 2017). This may occur not only because bereavement means the literal elimination of key social ties but also because bereavement activates psychosocial processes (e.g., depression, anxiety, substance use) that are risk factors for social isolation (NASEM 2020a).
Health conditions and cognitive decline.
Compared to White Americans, Black and Hispanic Americans are more likely to have significant and chronic health conditions (e.g., Hummer & Hayward 2015, Williams et al. 2010) and dementia (e.g., Farina et al. 2020, Mayeda et al. 2016), which are known risk factors for social isolation (NASEM 2020a). For example, chronic conditions, functional limitations, and cognitive impairment may interfere with a person’s ability to engage with their social networks and/or attend activities outside the home, thereby increasing the risk of isolation (e.g., NASEM 2020a, Steptoe et al. 2013). Racial inequity in health conditions, then, can contribute to racial inequity in social isolation. Of course, there is a bidirectional relationship between isolation and health, as isolation also undermines health and contributes to the development of health conditions and dementia (e.g., Ertel et al. 2008, Penninkilampi et al. 2018, Read et al. 2020, Valtorta et al. 2016). In the context of racial inequity, Black and Hispanic people experience a higher risk of isolation and poor health than White Americans and, therefore, are more likely to be subjected to the cycle of isolation and poor health across the life course.
Protective social factors.
Black and Hispanic adults may experience some protections against isolation in later life. Although Black older adults have smaller social networks, they have more frequent contact with people in their network (Cornwell et al. 2008, Taylor et al. 2013) and are more likely to attend religious services (Cornwell et al. 2008, Taylor et al. 2019) compared with White older adults. Not only do Black older adults have more engagement with their religious congregations (Taylor et al. 2019), they are also more likely to use religion to cope with stress (Taylor et al. 2007). As such, stress may be less likely to result in isolation for Black older adults. However, we know little about how social networks may offer protection against isolation for Hispanic adults. For example, one study of New Mexico residents over age 60 found that Hispanic older adults are less likely to live alone than White older adults (Tomaka et al. 2006); thus, living arrangements may reduce the risk of isolation for Hispanic older adults.
Future directions.
Much remains to be known about relatively basic differences in social isolation across racial/ethnic groups. First, we need more attention to patterns of social isolation by race/ethnicity at every stage of the life course, including changes in these patterns and the reasons for these changes, as individuals age. Second, future research should consider how social identities and social contexts intersect to shape the risk of social isolation. As an example, racism and sexism are overlapping systems of oppression (e.g., Collins & Bilge 2020, Crenshaw 1991) that could jointly shape patterns of social isolation by race and gender. The risk of social isolation may also depend on nativity status; for example, prior research documents fewer social ties among Hispanic immigrants compared with US-born Hispanics (Viruell-Fuentes et al. 2013). Immigration may mean leaving behind family and friends, and language barriers may interfere with the formation of new social connections. Yet these patterns may change over the life course, as immigrants of any racial/ethnic group acquire greater language fluency and form new social ties. Third, there is a crucial knowledge gap about social isolation among other minoritized racial/ethnic groups, such as American Indians and Alaska Natives (AIAN). AIAN populations may be at great risk of social isolation given their high mortality rates (Ka’opua et al. 2011, US Dep. Health Hum. Serv. 2013), the high prevalence of chronic conditions (Braun & LaCounte 2014), and their greater exposure to stress and racial discrimination (Braun & LaCounte 2014, Walters et al. 2011).
An additional avenue for future research is to understand why certain racial/ethnic populations may experience greater risk of social isolation. This research should attend to risk factors explaining racial inequities in isolation ranging from the micro level (e.g., stress exposures, health behavior) to the meso level (e.g., neighborhood characteristics) and the macro level (e.g., policy environment, exclusion from institutions). Indeed, scholars call for more attention to the role of structural racism as a determinant of health (e.g., Brown & Homan 2022, Gee & Hicken 2021), and we suggest that structural racism may influence opportunities and constraints that lead to inequities in social isolation across the life course. Government policies and lack of legal protections that contribute to social isolation, and racial/ethnic inequities therein, should also be examined. For example, immigration policies that constrain access to resources such as education and public services are considered drivers of Hispanic health inequities (Hatzenbuehler et al. 2017, Philbin et al. 2018). These polices may disrupt social ties in ways that have lasting consequences for social connection. Historical policies and practices may also contribute to a legacy of social isolation in minoritized populations. For instance, family separation via the placement of native children in government-run residential schools has reverberating consequences for American Indian children throughout life and across generations (e.g., Braun & LaCounte 2014, Walters et al. 2011), in ways that likely contribute to social isolation. Understanding how structural racism is a root cause of social isolation is a crucial area for future research.
Gender and Social Isolation
Prior studies on isolation have been more likely to include a statistical control for gender rather than attend to gender as a predictor of isolation that may vary over the life course. The few studies that have considered gender as a predictor typically rely on cross-sectional data and focus on mid- to later-life populations. However, a recent study by Kamis & Copeland (2020) analyzed an adolescent sample and found that, compared with boys, girls have more friends. Overall, cross-sectional studies of midlife and older samples yield mixed results, with some suggesting women are more isolated than men (Naito et al. 2021), others suggesting men are more isolated than women (Chatters et al. 2018, Cudjoe et al. 2020), and still others reporting no difference (Kotwal et al. 2021). A National Academies report (NASEM 2020a) on social isolation suggests that studies with older samples are more likely to find higher levels of isolation among women than men. Inconsistencies about gendered patterns across prior studies may reflect cross-sectional designs and the unique age-specific composition of samples.
A recent longitudinal study considered gender differences in social isolation using data from adolescence through later life using Add Health and HRS data (Umberson et al. 2022). The results, shown in Figure 4, indicate that boys/men are more isolated in the younger Add Health sample and women are more isolated in the older HRS sample, net of controls for age, educational attainment, and self-rated health. Moreover, the gender gap in isolation grows from mid- to later life, with increasing disadvantage for women.
Figure 4.
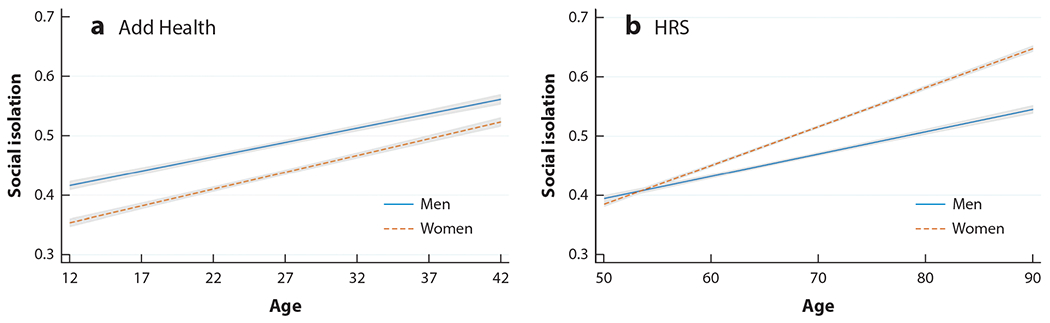
Gender and age trajectories of social isolation. Measures are drawn from Yang et al. (2016). The Add Health isolation scale assesses parent contact (in adolescence) or relationship status (age 18+), friend count, religious attendance, and volunteer activities. The HRS isolation scale assesses marital/cohabiting status, volunteer activities, contact with parents, contact with children, and contact with neighbors. Abbreviations: Add Health, National Longitudinal Study of Adolescent to Adult Health; HRS, Health and Retirement Study. Figure adapted from Umberson et al. (2022) with permission of SAGE Journals.
Figure 5 (building on results from Figure 4) illustrates how isolation patterns for men and women differ depending on their relationship status. Overall, men are more isolated than women from adolescence through later life, with one exception. Figure 5 shows that stably partnered women (but not never-married or previously partnered women) become more isolated than men after about age 65, perhaps because they are more likely to provide care to their aging spouses/partners. The degree of gender difference in isolation is greatest among the never-married, with men more isolated than women from young adulthood through late life. While stably partnered men and women are more isolated in young adulthood (perhaps due to family formation constraints), they have an advantage over their never-married peers as they grow older. These findings point to the importance of considering both life course and marital/partnership status variation in gendered patterns of isolation.
Figure 5.
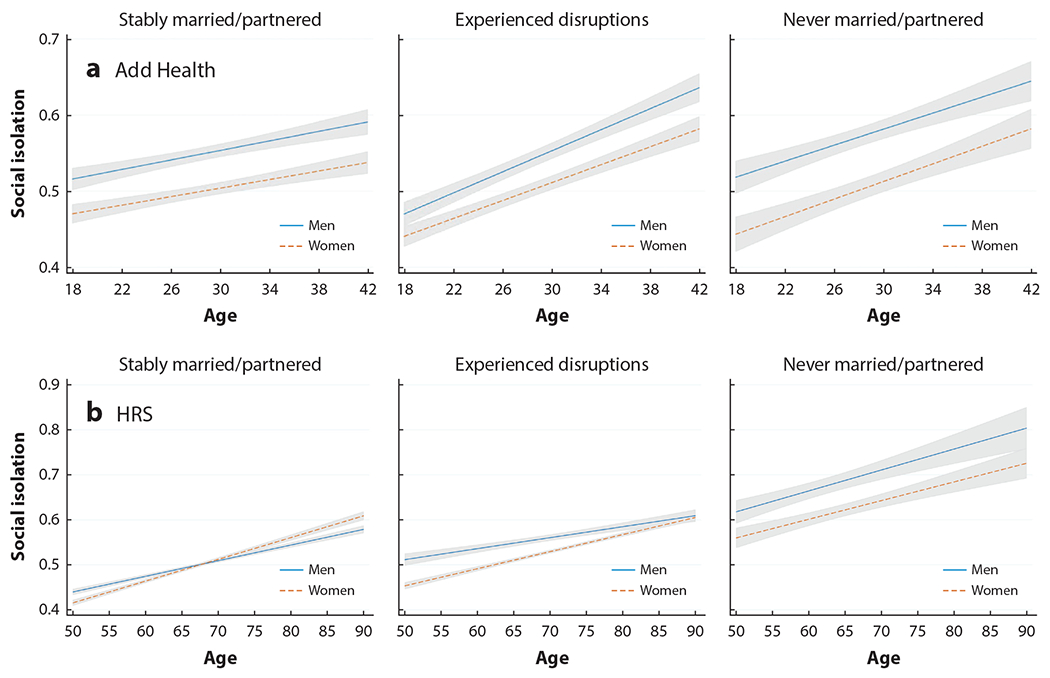
Age trajectories of social isolation by gender and relationship status. Measures are drawn from Yang et al. (2016). The Add Health isolation scale assesses parent contact (in adolescence) or relationship status (age 18+), friend count, religious attendance, and volunteer activities. The HRS isolation scale assesses marital/cohabiting status, volunteer activities, contact with parents, contact with children, and contact with neighbors. Abbreviations: Add Health, National Longitudinal Study of Adolescent to Adult Health; HRS, Health and Retirement Study. Figure adapted from Umberson et al. (2022) with permission of SAGE Journals.
A number of risk and protective factors help to shape levels of social isolation over the life course, in potentially different ways for men and women. Below, we briefly discuss two primary categories of risk and protective factors. The first category is marriage, family, and care work. The second category is health status.
Marriage, family, and care work.
Gender is a complicated predictor of social isolation, as some factors push women to be more connected to others (e.g., more responsibility for maintaining family relationships), whereas others may lead to more isolation for women (e.g., caregiving for spouses and older family members), and the balance of these factors shifts over the life course. Although marriage/partnership offers an important source of social connection for both men and women, being in a couple offers a different balance of risks and protective factors for men and women’s opportunities for social connection (Umberson et al. 2022). Within couples, women are more likely than men to maintain relationships with family and friends (Taylor 2011), which may reduce their isolation risk. Moreover, men are more likely than women to have no close confidants outside their marriage/partnership, making men more dependent on their partners for social connection (Taylor 2011) and exacerbating their risk of social isolation. Although women are more likely than men to become widowed (Carr & Utz 2020) and bereavement is a risk factor for isolation (NASEM 2020a), women’s more extensive social networks (Cornwell & Schafer 2016) may insulate women more than men following widowhood or divorce. On the other hand, women assume more responsibility for childcare (Dunatchik et al. 2021) and caregiving for aging spouses and other family members (Li & Loke 2013, Zivin & Christakis 2007), which may reduce engagement with friends and other social activities. For example, in later life, marriage may interfere with opportunities for social engagement if one’s spouse requires caregiving—a possibility that could help to explain why stably married women experience more isolation after age 65 (Umberson et al. 2022).
Health status.
Several health conditions are associated with increased risk for social isolation (NASEM 2020a). Some conditions, such as anxiety and depression, are more common for women than men through most of the life course (Girgus et al. 2017, McLean et al. 2011). Other conditions, such as cognitive impairment/dementia, chronic pain, and physical disabilities, are more prevalent among women in later life (Bartley & Fillingim 2013, Chêne et al. 2015, Freedman et al. 2016). The conditions that are more likely to affect women typically are nonfatal conditions that undermine quality of life. Thus, women live longer lives than men but in worse health (Read & Gorman 2010), and these long-term health conditions may put women at greater risk of social isolation. However, broader social networks and more/closer friendships/family ties (Cornwell & Schafer 2016, Russell & Taylor 2009) over the life course may protect women from social isolation even apart from these risk factors, but these possibilities have not been documented in prior research.
Future directions.
Future studies should identify the social conditions that foster increasing isolation over the life course and how they differ for men and women. For example, what is it about partnership status that alters the isolation trajectories of men and women in different ways—with greater disadvantage for unpartnered men throughout life and partnered women in later life? This means moving beyond the current focus on isolation in mid- to later life to focus on entire life course trajectories of isolation and how early social conditions contribute to subsequent life experiences that increase risk of social isolation for boys/men and girls/women.
An important avenue for future research is to attend to the role of structural sexism in shaping gendered patterns of isolation. For example, gendered wage and employment structures, as well as public policies and laws, shape work and family experiences (Bird & Rieker 2008, Homan 2019, Polivka 2017, Ridgeway 2011) that tend to disadvantage women. We have focused here on cisgender men and women, but future research should more broadly consider how other gender identities and gender transitions are associated with patterns of social isolation, with attention to the role of policies and practices that marginalize and exclude transgender people. Future studies can further address how gendered systems may operate differently in intersection with other structural systems, including race, class, and sexual orientation/gender identity.
Sexual Orientation and Social Isolation
Sexual orientation refers to “one’s enduring sexual attraction to male partners, female partners, or both” (VandenBos 2015, p. 974). Sexual orientation can include people who identify as straight or heterosexual (men attracted to women or vice versa), gay (men attracted to men), lesbian (women attracted to women), or bisexual (a person attracted to people of the same gender or another gender). The available evidence, although limited, suggests that lesbian, gay, and bisexual (LGB) people likely experience more social isolation than their non-LGB peers from adolescence through later life (Garcia et al. 2020; NASEM 2020b, 2022). Most studies are cross-sectional in design and focus on specific age groups rather than considering how patterns of isolation change over the life course of LGB people. Although prior studies indicate that the social experiences of LGB people vary by race, ethnicity, and gender identity (NASEM 2020b)—these patterns have not been well documented in relation to social isolation. Below, we briefly discuss three primary categories or risk and protective factors associated with sexual minority status that may, in turn, influence levels of social isolation over the life course. These include discrimination and stress, family relationships, and social policies.
Discrimination/stress.
Structural systems of heterosexism have resulted in laws, policies, and institutional practices that impose greater stress and disadvantage on LGB people (NASEM 2020b). Sexual orientation then shapes social experiences throughout life in ways that add to disadvantage in health and well-being (Hatzenbuehler 2009, Meyer 2003), and social isolation may be an important pathway to health disadvantage for sexual minorities (NASEM 2020b). The systemic influence of heterosexism begins early in the life course as adolescents often experience discrimination, social exclusion, and victimization as a result of their sexual orientation (Garcia et al. 2020, NASEM 2022). LGB youth are more likely to experience family rejection, homelessness, and abuse, as well as bullying and victimization at school (Moyano & del Mar Sánchez-Fuentes 2020, Parker et al. 2018, Robinson 2020)—social conditions that may increase risk for social isolation. These stressful experiences, explicated in the minority stress framework developed by Meyer (2003), may be especially formative early in the life course because they disrupt key developmental processes and milestones (e.g., developing a sense of identity and self-worth) that set the stage for strong social connections into adulthood and across the life course (Laursen & Hartl 2013). As a result of discrimination and stigma, LGB people often report hiding their identity (concealment, social invisibility) in ways that contribute to social isolation (Garcia et al. 2020). Moreover, stress and discrimination result in higher rates of depression and anxiety for LGB youth and adults, which could, in turn, lead to increased isolation (NASEM 2020b). Experiences of discrimination and stress continue into adulthood for sexual minority adults (Meyer 2003), which could have lasting implications for isolation across the life course.
Family relationships.
From adolescence through adulthood, LGB adults are more likely to experience strained relationships with their family of origin and, in adulthood, to see family members less frequently than their non-LGB peers (Reczek 2020). Due to legal, policy, and social constraints, LGB adults are less likely to be partnered or married, have fewer children, and are more likely to live alone (Espinoza 2011, Fredriksen-Goldsen 2018, Patterson 2019, Reczek 2020). These patterns of social connection through family ties may change for younger cohorts whose marital and parenting plans are more similar to those of heterosexual adults (Tate & Patterson 2019), yet this possibility has not been tested.
Protective family ties and social policies.
Having strong and supportive ties with parents and other adults in the early life course is a protective factor for the personal and social adjustment of LGB youth (Snapp et al. 2015, Watson et al. 2019). Many LGB people form “families of choice” with friendship networks they can rely on for support and connection (Wardecker & Matsick 2020). Being married is a protective factor in that it is an important source of social connection associated with better mental and physical health regardless of sexual orientation (LeBlanc et al. 2018, Umberson & Thomeer 2020). Laws and policies that support and protect the rights of LGB people have a significant and positive impact on social connection. For example, the legal right to marry and adopt children promotes family relationships, including closer ties with extended family (Reczek 2020). Moreover, school policies that support sexual minority students are associated with stronger and more supportive social networks for those students (Hatzenbuehler et al. 2014, NASEM 2022). Thus, although sexual minorities may experience stress, discrimination, and strained family relationships, they often form communities that can provide a buffer against social isolation.
Future directions.
Of the structural systems examined in this article, sexual orientation is the least well documented in relation to social isolation, particularly in relation to change over the life course. Thus, systematic documentation of these patterns is a critical first step. It is essential to go beyond the focus on LGB people to more broadly consider how structural systems of stigma and discrimination influence lifelong patterns of social isolation for other sexual and gender diverse populations. For example, prior studies show how the social experiences of transgender and bisexual populations diverge from those of gay and lesbian populations in ways that impact social connectivity (e.g., Johnson et al. 2020, Reczek 2020). Intersectionality of sexual orientation in relation to race, class, and gender should also be considered (NASEM 2020b, Reczek 2020).
Given recent changes in the social and legal landscape for LGB people, life course experiences of social isolation may be quite different across birth cohorts, yet prior research has not tested this possibility. Younger birth cohorts have experienced more legal protections and social acceptance than did older birth cohorts, and this may be protective for younger cohorts in ways that reduce social isolation. However, recent research finds that an improved social environment is not associated with reduced exposure to minority stress in younger birth cohorts (Meyer et al. 2021), and exposure to stress like violence and discrimination may contribute to social isolation. Moreover, LGB people are coming out at younger ages than did those in older cohorts (Floyd & Bakeman 2006, Martos et al. 2015, Meyer et al. 2021), which may present young people with novel social challenges. Age and cohort variation should be addressed in future studies of social isolation—there is a need to document patterns of isolation, address the structural reasons for those patterns, and consider how patterns have changed across historical time. Future studies of this type can more directly consider how legal/policy contexts influence social isolation across diverse populations. This will be particularly important in light of the drastic increase in recent legislation targeting the rights and autonomy of gender diverse populations. These details are needed to formulate effective screening for isolation risk as well as interventions and policies to reduce risk across diverse populations.
Socioeconomic Status and Social Isolation
Existing research on social isolation rarely focuses on inequities by SES (i.e., educational attainment, income, wealth). Instead, measures of SES are often included as control variables, precluding a nuanced examination of inequities in isolation across the life course and reasons why or how these inequities emerge. Despite these shortcomings, research generally shows that isolation tends to be greater among individuals with less education and income (Evans & Rubin 2022, Naito et al. 2021, Steptoe et al. 2013, Tanskanen & Anttila 2016). Moreover, lacking close kin is more common among older adults with low levels of wealth (Margolis & Verdery 2017), and older adults with less education are more likely to experience network shrinkage (Cornwell 2015). Evidence of inequities in social isolation by SES exists in samples from young adulthood to later life (Cudjoe et al. 2020, Evans & Rubin 2022, Naito et al. 2021, Steptoe et al. 2013, Tanskanen & Anttila 2016, Yang et al. 2013a). In sum, prior research indicates inequities in isolation by SES, yet we know very little about changes over the life course or reasons why lower-SES adults experience more isolation. We next discuss two key categories of risk and protective factors that may shape inequities in social isolation by SES: family/social support and health.
Family and social support.
SES can impact the quantity and quality of social relationships (Umberson & Montez 2010), shaping the likelihood of social isolation. For example, marriage can be protective of isolation and an important source of social support (NASEM 2020a), yet lower-SES individuals have less access to marriage (Umberson & Thomeer 2020) and are more likely to divorce if married (Martin 2006). The presence of social relationships may be especially important in later life, as higher-educated older adults are more likely than older adults with less education to have a living parent or spouse (Daw et al. 2016) and less educated older adults are more likely to experience the death of a confidant (Cornwell 2015). Although lower-SES adults may form close social networks (e.g., Gosling 2008, Warr 2005), limited economic and social resources tend to strain the relationships of lower-SES adults, with consequences for social connection (Evans & Rubin 2022). Taken together, adults with lower levels of SES may experience more social isolation due to inequities in the quantity and quality of social relationships across the life course.
Health.
SES, considered a fundamental cause of health inequities (Phelan et al. 2010), is a robust predictor of health and mortality (e.g., Montez & Brooks 2021, Zajacova & Lawrence 2018). Thus, people with lower levels of education, income, and wealth live shorter lives and live more of their lives with chronic conditions, dementia, and functional limitations (Bowen & González 2010, Crimmins et al. 2018, Montez & Hayward 2014). As previously discussed, health conditions and functional limitations are risk factors for social isolation (e.g., NASEM 2020a, Steptoe et al. 2013). Thus, the unequal burden of poor health and cognitive impairment among lower-SES adults may lead to inequities in social isolation by SES. Isolation, in turn, has robust consequences for subsequent health (e.g., Ertel et al. 2008, Penninkilampi et al. 2018, Read et al. 2020, Valtorta et al. 2016), trapping lower-SES adults in a vicious cycle of isolation and health challenges.
Future directions.
Future research should document experiences of isolation across the life course, with attention to changes over time as individuals age. For example, do the inequities in isolation remain stable over the life course or do they widen as (dis)advantage accumulates? Because SES can change, scholars should also aim to understand the consequences of social mobility for social isolation. Moreover, Black and White Americans often experience differential returns to SES (e.g., Boen 2016, Pearson 2008); as such, future research should consider exposure to isolation at the intersection of SES and race.
Because prior research often includes SES as a control variable, we know very little about why lower-SES individuals are more likely to be isolated. An important avenue for future research is to consider a range of explanatory factors for these inequities. In one of the few studies with a focus on SES in relation to isolation, Evans & Rubin (2022, p. 698) note that the “research points toward issues at a structural level, where the conditions of being within the lower classes create a trend toward lower social integration.” State- or country-specific income inequality, for example, could contribute to social conditions such as community mistrust and a lack of social cohesion (Pickett & Wilkinson 2015) that erode social connection. Examining the policies and practices that foster socioeconomic inequities in social isolation is a key area for future research.
CONCLUSION
Social isolation is increasingly recognized as a public health concern both in the United States and globally (Holt-Lunstad et al. 2017, Klinenberg 2016). We know a great deal about the impact of isolation on health, but we know much less about the social distribution of isolation across the life course. We have drawn on the bedrock sociological tenet that social structural systems differentially shape access to resources across populations in ways that promote inequity in social connectivity (Cornwell 2015). We argue that inequity in social isolation is a lifelong process with many of its roots in the early life course. Social isolation undermines health and quality of life across populations, yet some populations are more at risk of isolation than others because their social structural position fosters more isolation. Some countries are further along than the United States in recognizing this fact. The recent National Academies report (NASEM 2020a, pp. 86–87) on social isolation concludes, “while a fair number of international studies look at the status of at-risk populations in other countries … studies focusing on at-risk populations in the United States are sparse.” In this review, we provided an overview of current evidence about inequities in isolation and developed a conceptual framework to guide future research on who is most at risk of isolation, why they are at risk, and how this risk changes from childhood through later life.
What we know about the social distribution of isolation in the United States—across race/ethnicity, gender, sexual orientation, and SES—is limited, but the available evidence points to inequality. Although prior studies point to increasing risk of isolation at older ages, there is “disturbing evidence of a lifelong process of steadily declining social connection” (Umberson et al. 2022) that begins as early as adolescence, and the evidence reviewed in this article suggests inequities in isolation from adolescence through late life. Yet most prior research has been cross-sectional by design and focused on mid- to later-life populations. Although isolation research has focused on age more than any other individual-level characteristic as predictive of social isolation (NASEM 2020a), we need to understand socially patterned trajectories of isolation throughout the entire life course with attention to race, ethnicity, gender, sexuality, and SES—and their intersection with age.
Our review reveals several cross-cutting themes to drive future research in this area. First, we need basic documentation of life course trajectories of social isolation across populations, with special attention to the early life course. Second, studies need to explore when and why isolation emerges, accelerates, stabilizes, or even diminishes and how these patterns vary across populations. We need to identify specific risk and protective factors for isolation that vary across populations and over the life course. While prior research identifies several key factors associated with isolation that are known to differ across populations, they are rarely examined as explanations for population differences in isolation. These risk factors include overall stress exposure including minority stress/discrimination, stressful life events such as bereavement, care work and family demands, and physical/mental/cognitive health conditions and disabilities (NASEM 2020a,b). Notably, many of these risk factors have origins within the structural systems of racism, sexism, heterosexism, and income inequality In addition to these risk factors, we point to some factors that offer protection to minoritized populations, such as the creation of families of choice or engagement with religious communities. The power and resistance of marginalized populations is often overlooked yet has the potential to advance understanding of the social production of isolation. Third, in identifying risk and protective factors for social isolation across populations, we should attend to intersectionality in these processes, perhaps particularly the intersection of race/ethnicity and gender (Taylor et al. 2019). Fourth, it is essential to document patterns of isolation across diverse populations that are often excluded in studies of social isolation, particularly Latinx, AIAN, and gender diverse populations. Finally, when choosing or developing objective measures of social isolation, sociologists should be thoughtful about the divergent social experiences across gender, race/ethnicity, sexual orientation, and social class. For example, connection to friends (e.g., families of choice) may be more salient for sexual minority populations (NASEM 2020a, Reczek 2020), whereas religious connections may be more salient for Black Americans, especially Black women (Chatters et al. 2018). It is the overall level of social connection/absence of isolation that matters for population health (House et al. 1988).
Social isolation is increasingly recognized as a public health concern (Holt-Lunstad et al. 2017, Klinenberg 2016), but sociologists have largely focused on how social isolation affects health rather than documenting population patterns of isolation. Klinenberg (2016) has argued that it is imperative to identify who is most at risk of social isolation as a first step in addressing isolation as a public health concern and addressing disparities. This first step is essential if we are to screen and identify individuals at risk of isolation and develop policies to reduce the risk for social isolation across the life course. We have substantial evidence that policies and laws can have a positive impact on social connection. For example, marriage equality offered legal recognition and protection of marital relationships for same-sex couples and studies clearly show the positive mental and physical health benefits of this type of social connection (LeBlanc et al. 2018). Earlier in the life course, inclusive policies in schools reduce social isolation for LGBT youth (NASEM 2022). Equally important, policies and laws should “do no harm,” such that policies that increase relationship strain and/or decrease opportunities for social connection should be avoided (Umberson & Montez 2010). For example, policies that prohibit the discussion of sexual orientation in schools or deny transgender individuals access to gender affirming care may increase stress and reduce opportunities for social connection. Attending to the structural determinants of isolation is crucial to alleviate inequities in isolation.
ACKNOWLEDGMENTS
This research was supported, in part, by grants R01 AG69969, R37 AG076057, and P30 AG066614 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging.
Footnotes
The Annual Review of Sociology is online at soc.annualreviews.org
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- Alcaraz KI, Eddens KS, Blase JL, Diver WR, Patel AV, et al. 2019. Social isolation and mortality in US black and white men and women. Am. J. Epidemiol 188(1):102–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. 2017. Structural racism and health inequities in the USA: evidence and interventions. Lancet 389(10077):1453–63 [DOI] [PubMed] [Google Scholar]
- Barger SD, Uchino BN. 2017. Racial and ethnic variation in the association of social integration with mortality: ten-year prospective population-based US study. Sci. Rep 7(1):43874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartley EJ, Fillingim RB. 2013. Sex differences in pain: a brief review of clinical and experimental findings. Br. J. Anaesth 111(1):52–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharmal N, Derose KP, Felician MF, Weden MM. 2015. Understanding the upstream social determinants of health. Work. Pap., RAND Corp., Santa Monica, CA. https://www.rand.org/pubs/working_papers/WR1096.html [Google Scholar]
- Bird CE, Rieker PP. 2008. Gender and Health: The Effects of Constrained Choices and Social Policies. Cambridge, UK: Cambridge Univ. Press [Google Scholar]
- Boen C 2016. The role of socioeconomic factors in Black-White health inequities across the life course: point-in-time measures, long-term exposures, and differential health returns. Soc. Sci. Med 170:63–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen C 2020. Death by a thousand cuts: stress exposure and Black-White disparities in physiological functioning in late life. J. Gerontol. B 75(9):1937–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen ME, González HM. 2010. Childhood socioeconomic position and disability in later life: results of the Health and Retirement Study. Am. J. Public Health 100(S1):S197–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun KL, LaCounte C. 2014. The historic and ongoing issue of health disparities among native elders. Generations 38(4):60–69 [Google Scholar]
- Brown TH, Homan PA. 2022. Frontiers in measuring structural racism and its health effects. Health Serv. Res 57(3):443–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Patrick W. 2008. Loneliness: Human Nature and the Need for Social Connection. New York: W.W. Norton & Co. [Google Scholar]
- Carr D, Utz RL. 2020. Families in later life: a decade in review. J. Marriage Fam 82(1):346–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatters LM, Taylor HO, Nicklett EJ, Taylor RJ. 2018. Correlates of objective social isolation from family and friends among older adults. Healthcare 6(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chêne G, Beiser A, Au R, Preis SR,Wolf PA, et al. 2015. Gender and incidence of dementia in the Framingham Heart Study from mid-adult life. Alzheimer’s Dement. 11(3):310–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PH, Bilge S. 2020. Intersectionality. Cambridge, UK: Polity [Google Scholar]
- Cornwell B 2015. Social disadvantage and network turnover. J. Gerontol. B 70(1):132–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B, Laumann EO, Schumm LP. 2008. The social connectedness of older adults: a national profile. Am. Sociol. Rev 73(2):185–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B, Schafer MH. 2016. Social networks in later life. In Handbook of Aging and the Social Sciences (Eighth Edition), ed. George LK, Ferraro KF, pp. 181–201. Cambridge, MA: Academic [Google Scholar]
- Coyle CE, Dugan E. 2012. Social isolation, loneliness and health among older adults. J. Aging Health 24(8):1346–63 [DOI] [PubMed] [Google Scholar]
- Crenshaw K 1991. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanf. Law Rev 43(6):1241–99 [Google Scholar]
- Crimmins EM, Saito Y, Kim JK, Zhang YS, Sasson I, Hayward MD. 2018. Educational differences in the prevalence of dementia and life expectancy with dementia: changes from 2000 to 2010. J. Gerontol. B 73(suppl. 1):S20–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cudjoe TKM, Roth DL, Szanton SL,Wolff JL, Boyd CM, Thorpe RJ Jr. 2020. The epidemiology of social isolation: National Health and Aging Trends Study. J. Gerontol. B 75(1):107–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daw J, Verdery AM, Margolis R. 2016. Kin count(s): educational and racial differences in extended kinship in the United States. Popul. Dev. Rev 42(3):491–517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly R, Lin Z, Umberson D. 2021. Family member death, social isolation, and cardiometabolic health: racial disadvantage in the U.S Paper presented at the Annual Meeting of the Population Association of America, virtual meeting, May 5–8 [Google Scholar]
- Dunatchik A, Gerson K, Glass J, Jacobs JA, Stritzel H. 2021. Gender, parenting, and the rise of remote work during the pandemic: implications for domestic inequality in the United States. Gend. Soc 35(2):194–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertel KA, Glymour MM, Berkman LF. 2008. Effects of social integration on preserving memory function in a nationally representative US elderly population. Am. J. Public Health 98(7):1215–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinoza R 2011. The Diverse Elders Coalition and LGBT aging: connecting communities, issues, and resources in a historic moment. Public Policy Aging Rep. 21(3):8–12 [Google Scholar]
- Evans O, Rubin M. 2022. In a class on their own: investigating the role of social integration in the association between social class and mental well-being. Pers. Soc. Psychol. Bull 48(5):690–703 [DOI] [PubMed] [Google Scholar]
- Farina MP, Hayward MD, Kim JK, Crimmins EM. 2020. Racial and educational disparities in dementia and dementia-free life expectancy. J. Gerontol. B 75(7):e105–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd FJ, Bakeman R. 2006. Coming-out across the life course: implications of age and historical context. Arch. Sex. Behav 35(3):287–96 [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K 2018. Shifting social context in the lives of LGBTQ older adults. Public Policy Aging Rep. 28(1):24–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA,Wolf DA, Spillman BC. 2016. Disability-free life expectancy over 30 years: a growing female disadvantage in the US population. Am. J. Public Health 106(6):1079–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia J, Vargas N, Clark JL, Magaña Álvarez M, Nelons DA, Parker RG. 2020. Social isolation and connect-edness as determinants of well-being: global evidence mapping focused on LGBTQ youth. Glob. Public Health 15(4):497–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Hicken MT. 2021. Structural racism: the rules and relations of inequity. Ethn. Dis 31(Suppl):293–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehlert S, Sohmer D, Sacks T, Mininger C, McClintock M, Olopade O. 2008. Targeting health disparities: a model linking upstream determinants to downstream interventions. Health Aff. 27(2):339–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girgus JS, Yang K, Ferri CV. 2017. The gender difference in depression: are elderly women at greater risk for depression than elderly men? Geriatrics 2(4):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby BJ, Cheadle JE, Mitchell C. 2018. Stress-related biosocial mechanisms of discrimination and African American health inequities. Annu. Rev. Sociol 44:319–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosling VK. 2008. ‘I’ve always managed, that’s what we do’: social capital and women’s experiences of social exclusion. Sociol. Res. Online 13(1):1–14 [Google Scholar]
- Hatzenbuehler ML. 2009. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol. Bull 135(5):707–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML. 2016. Structural stigma: research evidence and implications for psychological science. Am. Psychol 71(8):742–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Birkett M, Van Wagenen A, Meyer IH. 2014. Protective school climates and reduced risk for suicide ideation in sexual minority youths. Am. J. Public Health 104(2):279–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Prins SJ, Flake M, Philbin M, Frazer MS, et al. 2017. Immigration policies and mental health morbidity among Latinos: a state-level analysis. Soc. Sci. Med 174:169–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Robles TF, Sbarra DA. 2017. Advancing social connection as a public health priority in the United States. Am. Psychol 72(6):517–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB. 2016. Loneliness and social isolation as risk factors for CVD: implications for evidence-based patient care and scientific inquiry. Heart 102(13):987–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. 2015. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci 10(2):227–37 [DOI] [PubMed] [Google Scholar]
- Homan P 2019. Structural sexism and health in the United States: a new perspective on health inequality and the gender system. Am. Sociol. Rev 84(3):486–516 [Google Scholar]
- Homan P, Brown TH, King B. 2021. Structural intersectionality as a new direction for health disparities research. J. Health Soc. Behav 62(3):350–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. 1988. Social relationships and health. Science 241(4865):540–45 [DOI] [PubMed] [Google Scholar]
- Hummer RA, Hayward MD. 2015. Hispanic older adult health & longevity in the United States: current patterns & concerns for the future. Daedalus 144(2):20–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson KC, LeBlanc AJ, Sterzing PR, Deardorff J, Antin T, Bockting WO. 2020. Trans adolescents’ perceptions and experiences of their parents’ supportive and rejecting behaviors. J. Couns. Psychol 67(2):156–70 [DOI] [PubMed] [Google Scholar]
- Kamis C, Copeland M. 2020. The long arm of social integration: gender, adolescent social networks, and adult depressive symptom trajectories. J. Health Soc. Behav 61(4):437–52 [DOI] [PubMed] [Google Scholar]
- Ka’opua LS, Braun KL, Browne CV, Mokuau N, Park C-B. 2011.Why are native Hawaiians underrepresented in Hawai‘i’s older adult population? Exploring social and behavioral factors of longevity. J. Aging Res 2011:701232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinenberg E 2016. Social isolation, loneliness, and living alone: identifying the risks for public health. Am. J. Public Health 106(5):786–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotwal AA, Cenzer IS, Waite LJ, Covinsky KE, Perissinotto CM, et al. 2021. The epidemiology of social isolation and loneliness among older adults during the last years of life. J. Adolesc. Health 69(11):3081–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N 2020. Measures of racism, sexism, heterosexism, and gender binarism for health equity research: from structural injustice to embodied harm—an ecosocial analysis. Annu. Rev. Public Health 41:37–62 [DOI] [PubMed] [Google Scholar]
- Laursen B, Hartl AC. 2013. Understanding loneliness during adolescence: developmental changes that increase the risk of perceived social isolation. J. Adolesc 36(6):1261–68 [DOI] [PubMed] [Google Scholar]
- LeBlanc AJ, Frost DM, Bowen K. 2018. Legal marriage, unequal recognition, and mental health among same-sex couples. J. Marriage Fam 80(2):397–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Loke AY. 2013. A spectrum of hidden morbidities among spousal caregivers for patients with cancer, and differences between the genders: a review of the literature. Eur. J. Oncol. Nurs 17(5):578–87 [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan J. 1995. Social conditions as fundamental causes of disease. J. Health Soc. Behav 1995:80–94 [PubMed] [Google Scholar]
- Liu H, Lin Z, Umberson D. 2022. Parental death and cognitive impairment: an examination by gender and race-ethnicity. J. Gerontol. B 77(6):1164–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L 2011. Social connections, diabetes mellitus, and risk of mortality among white and African-American adults aged 70 and older: an eight-year follow-up study. Ann. Epidemiol 21(1):26–33 [DOI] [PubMed] [Google Scholar]
- Margolis R,Verdery AM. 2017. Older adults without close kin in the United States. J. Gerontol. B 72(4):688–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin SP. 2006. Trends in marital dissolution by women’s education in the United States. Demogr. Res 15(20):537–60 [Google Scholar]
- Martos AJ, Nezhad S, Meyer IH. 2015. Variations in sexual identity milestones among lesbians, gay men, and bisexuals. Sex. Res. Soc. Policy 12(1):24–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayeda ER, Glymour MM,Quesenberry CP, Whitmer RA. 2016. Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimer’s Dement. 12(3):216–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, Hofmann SG. 2011. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res 45(8):1027–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull 129(5):674–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Russell ST, Hammack PL, Frost DM, Wilson BDM. 2021. Minority stress, distress, and suicide attempts in three cohorts of sexual minority adults: a U.S. probability sample. PLOS ONE 16(3):e0246827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyawaki CE. 2015. Association of social isolation and health across different racial and ethnic groups of older Americans. Ageing Soc. 35(10):2201–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez JK, Brooks JD. 2021. Educational attainment and adult health. In Handbook of Aging and the Social Sciences, ed. Ferraro KF, Carr D, pp. 83–98. Cambridge, MA: Academic. 9th ed. [Google Scholar]
- Montez JK, Hayward MD. 2014. Cumulative childhood adversity, educational attainment, and active life expectancy among U.S. adults. Demography 51(2):413–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyano N, del Mar Sánchez-Fuentes M. 2020. Homophobic bullying at schools: a systematic review of research, prevalence, school-related predictors and consequences. Aggress. Violent Behav 53:101441 [Google Scholar]
- Naito R, Leong DP, Bangdiwala SI, McKee M, Subramanian SV, et al. 2021. Impact of social isolation on mortality and morbidity in 20 high-income, middle-income and low-income countries in five continents. BMJ Glob. Health 6(3):e004124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NASEM (Natl. Acad. Sci. Eng. Med.). 2020a. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Washington, DC: Natl. Acad. Press; [PubMed] [Google Scholar]
- NASEM (Natl. Acad. Sci. Eng. Med.). 2020b. Understanding the Well-Being of LGBTQI+ Populations. Washington, DC: Natl. Acad. Press [Google Scholar]
- NASEM (Natl. Acad. Sci. Eng. Med.). 2022. Reducing Inequalities Between Lesbian, Gay, Bisexual, Transgender, and Queer Adolescents and Cisgender, Heterosexual Adolescents: Proceedings of a Workshop. Washington, DC: Natl. Acad. Press; [PubMed] [Google Scholar]
- Nicholson NR. 2012. A review of social isolation: an important but underassessed condition in older adults. J. Prim. Prev 33(2):137–52 [DOI] [PubMed] [Google Scholar]
- Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. 2013. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am. J. Public Health 103(11):2056–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker CM, Hirsch JS, Philbin MM, Parker RG. 2018. The urgent need for research and interventions to address family-based stigma and discrimination against lesbian, gay, bisexual, transgender, and queer youth. J. Adolesc. Health 63(4):383–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson CJ. 2019. Lesbian and gay parenthood. In Handbook of Parenting, ed. Bornstein MH, pp. 345–71. New York: Routledge. 3rd ed. [Google Scholar]
- Pearson JA. 2008. Can’t buy me whiteness: new lessons from the Titanic on race, ethnicity, and health. Du Bois Rev. 5(1):27–47 [Google Scholar]
- Penninkilampi R, Casey A-N, Singh MF, Brodaty H. 2018. The association between social engagement, loneliness, and risk of dementia: a systematic review and meta-analysis. J. Alzheimer’s Dis 66(4):1619–33 [DOI] [PubMed] [Google Scholar]
- Perissinotto CM, Covinsky KE. 2014. Living alone, socially isolated or lonely—what are we measuring? J. Gen. Intern. Med 29(11):1429–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry BL, Pescosolido BA, Borgatti SP. 2018. Egocentric Network Analysis: Foundations, Methods, and Models. Cambridge, UK: Cambridge Univ. Press [Google Scholar]
- Phelan JC, Link BG,Tehranifar P. 2010. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J. Health Soc. Behav 51(Suppl. 1):S28–40 [DOI] [PubMed] [Google Scholar]
- Philbin MM, Flake M, Hatzenbuehler ML, Hirsch JS. 2018. State-level immigration and immigrant-focused policies as drivers of Latino health disparities in the United States. Soc. Sci. Med 199:29–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett KE,Wilkinson RG. 2015. Income inequality and health: a causal review. Soc. Sci. Med 128:316–26 [DOI] [PubMed] [Google Scholar]
- Polivka LJ. 2017. Women and the crisis of care in the United States. Generations 41(4):29–35 [Google Scholar]
- Ratcliff KS. 2017. The Social Determinants of Health: Looking Upstream. Cambridge, UK: Polity [Google Scholar]
- Read JG, Gorman BK. 2010. Gender and health inequality. Annu. Rev. Sociol 36:371–86 [Google Scholar]
- Read S, Comas-Herrera A, Grundy E. 2020. Social isolation and memory decline in later-life. J. Gerontol. B 75(2):367–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reczek C 2020. Sexual- and gender-minority families: a 2010 to 2020 decade in review. J. Marriage Fam 82(1):300–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridgeway CL. 2011. Framed by Gender: How Gender Inequality Persists in the Modern World. Oxford, UK: Oxford Univ. Press [Google Scholar]
- Robinson BA. 2020. Coming Out to the Streets: LGBTQ Youth Experiencing Homelessness. Oakland: Univ. Calif. Press [Google Scholar]
- Russell D, Taylor J. 2009. Living alone and depressive symptoms: the influence of gender, physical disability, and social support among Hispanic and non-Hispanic older adults. J. Gerontol. B 64B(1):95–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snapp SD,Watson RJ, Russell ST, Diaz RM, Ryan C. 2015. Social support networks for LGBT young adults: low cost strategies for positive adjustment. Fam. Relat 64(3):420–30 [Google Scholar]
- Steptoe A, Shankar A, Demakakos P, Wardle J. 2013. Social isolation, loneliness, and all-cause mortality in older men and women. PNAS 110(15):5797–5801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternthal MJ, Slopen N,Williams DR. 2011. Racial disparities in health: How much does stress really matter? Du Bois Rev. 8(1):95–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanskanen J, Anttila T. 2016. A prospective study of social isolation, loneliness, and mortality in Finland. Am. J. Public Health 106(11):2042–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate DP, Patterson CJ. 2019. Desire for parenthood in context of other life aspirations among lesbian, gay, and heterosexual young adults. Front. Psychol 10. 10.3389/fpsyg.2019.02679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Jackson JS. 2007. Religious and spiritual involvement among older African Americans, Caribbean Blacks, and non-Hispanic Whites: findings from the National Survey of American Life. J. Gerontol. B 62(4):S238–50 [DOI] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Taylor HO. 2019. Race and objective social isolation: older African Americans, Black Caribbeans, and non-Hispanic Whites. J. Gerontol. B 74(8):1429–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Woodward AT, Brown E. 2013. Racial and ethnic differences in extended family, friendship, fictive kin, and congregational informal support networks. Fam. Relat 62(4):609–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE. 2011. Social support: a review. In The Oxford Handbook of Health Psychology, ed. Friedman HS, pp. 189–214. Oxford, UK: Oxford Univ. Press [Google Scholar]
- Tomaka J, Thompson S, Palacios R. 2006. The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. J. Aging Health 18(3):359–84 [DOI] [PubMed] [Google Scholar]
- Uchino BN, Bowen K, Carlisle M, Birmingham W. 2012. Psychological pathways linking social support to health outcomes: a visit with the “ghosts” of research past, present, and future. Soc. Sci. Med 74(7):949–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D 2017. Black deaths matter: race, relationship loss, and effects on survivors. J. Health Soc. Behav 58(4):405–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Donnelly R. 2022. The death of a child and parents’ psychological distress in mid to later life: racial/ethnic differences in exposure and vulnerability. J. Gerontol. B 77(8):1561–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Lin Z, Cha H. 2022. Gender and social isolation across the life course. J. Health Soc. Behav 63(3):319–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Montez JK. 2010. Social relationships and health: a flashpoint for health policy. J. Health Soc. Behav 51:S54–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Olson JS, Crosnoe R, Liu H, Pudrovska T, Donnelly R. 2017. Death of family members as an overlooked source of racial disadvantage in the United States. PNAS 114(5):915–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Thomeer MB. 2020. Family matters: research on family ties and health, 2010 to 2020. J. Marriage Fam 82(1):404–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Dep. of Health and Hum. Serv. 2013. Disparities. Indian Health Serv., Rockville, MD. https://www.ihs.gov/newsroom/factsheets/disparities [Google Scholar]
- Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. 2016. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 102(13):1009–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VandenBos GR, ed. 2015. APA Dictionary of Psychology. Washington, DC: Am. Psychol. Assoc. 2nd ed. [Google Scholar]
- Verdery AM, Margolis R. 2017. Projections of white and black older adults without living kin in the United States, 2015 to 2060. PNAS 114(42):11109–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viruell-Fuentes EA, Morenoff JD,Williams DR, House JS. 2013. Contextualizing nativity status, Latino social ties, and ethnic enclaves: an examination of the ‘immigrant social ties hypothesis.’ Ethn. Health 18(6):586–609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters KL, Mohammed SA, Evans-Campbell T, Beltrán RE, Chae DH, Duran B. 2011. Bodies don’t just tell stories, they tell histories: embodiment of historical trauma among American Indians and Alaska Natives. Du Bois Rev. 8(1):179–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardecker BM, Matsick JL. 2020. Families of choice and community connectedness: a brief guide to the social strengths of LGBTQ older adults. J. Gerontol. Nurs 46(2):5–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warr DJ. 2005. Social networks in a ‘discredited’ neighbourhood. J. Sociol 41(3):285–308 [Google Scholar]
- Watson RJ, Grossman AH, Russell ST. 2019. Sources of social support and mental health among LGB youth. Youth Soc. 51(1):30–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR. 2018. Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J. Health Soc. Behav 59(4):466–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR,Mohammed SA, Leavell J, Collins C. 2010. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann. N.Y. Acad. Sci 1186(1):69–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YC, Boen C, Gerken K, Li T, Schorpp K, Harris KM. 2016. Social relationships and physiological determinants of longevity across the human life span. PNAS 113(3):578–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YC, Li T, Ji Y. 2013a. Impact of social integration on metabolic functions: evidence from a nationally representative longitudinal study of US older adults. BMC Public Health 13(1):1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YC, McClintock MK, Kozloski M, Li T. 2013b. Social isolation and adult mortality: the role of chronic inflammation and sex differences. J. Health Soc. Behav 54(2):183–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A, Lawrence EM.2018. The relationship between education and health: reducing disparities through a contextual approach. Annu. Rev. Public Health 39:273–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zivin K, Christakis NA. 2007. The emotional toll of spousal morbidity and mortality. Am. J. Geriatr. Psychiatr 15(9):772–79 [DOI] [PubMed] [Google Scholar]


