Dialysis facility closures have been uncommon in the United States, affecting <1% of patients receiving dialysis annually.1 Yet, recent changes in the financing and delivery of dialysis may change this. One large dialysis provider reported closing 58 facilities in the final quarter of 2022.2 Financial pressures related to national reimbursement reforms, a changing payer mix, staffing shortages, and a shift toward the use of home dialysis modalities could increase the risk of facility closures.
Dialysis facility closures disrupt ongoing relationships between patients and dialysis facility staff that may be important for the delivery of high-quality care. Care transitions after dialysis facility closures are associated with an increased risk of hospitalizations, missed dialysis treatments, and a marginal increase in mortality.3 Dialysis facility closures are more likely to affect health outcomes among patients of Black race and having Medicaid.4
In addition to diminishing patient health outcomes, dialysis facility closures might force patients to travel farther to receive dialysis. Because patients must receive dialysis three to four times per week, many patients choose to travel to the facility closest to where they live. Decreased quality of life is associated with longer travel distance to receive dialysis,5 and patients may switch dialysis modalities or move to a lower-quality facility to avoid it.6,7 In this study, we examine changes in the distance that patients travel for in-center hemodialysis after dialysis facility closures.
We examined data from the US national dialysis registry and applied a previously described method to identify dialysis facilities that closed between 2001 and 2015 and the date of each closure.4 We used information on population density around facilities to identify remote areas, defined as small-town, rural, and micropolitan areas. We limited our analysis to closed facilities in remote areas where density of facilities is low and travel distance to dialysis facilities is most likely to change when patients switch to another facility. We considered Medicare beneficiaries as affected by a closure if they received dialysis within 30 days of all patients leaving a closed facility.
Patient demographic and health characteristics came from Medicare enrollment data and claims from the 6 months before facility closures. We used dialysis facility addresses and zip code centroids of patient residences to estimate driving distances before and after facility closures. For each patient, we calculated their change in one-way distance traveled. Distribution of travel distances were examined separately among facilities in rural/small-town and micropolitan areas. We used multivariable logistic regression to assess the odds of one-way travel distance increasing by ≥10 or ≥20 miles as a function of patient, geographic, and dialysis facility characteristics.
In total, 213 facilities in remote areas closed during the study period. Among 2675 Medicare beneficiaries who were affected, 1269 (47%) lived in rural/small-town areas. The mean age of affected patients was 64 years, with 45% of patients being female, 31% Black race, 5.3% other race, and 7.7% Hispanic ethnicity. Before facility closure, 10.2% of patients were in their first year of dialysis, 49% were eligible for Medicaid, 73% received dialysis at for-profit facilities, and 46% received dialysis at the two largest dialysis chains. Compared with a prior analysis of patients receiving dialysis during a similar period,4 this cohort included older patients and fewer patients of Black race and Hispanic ethnicity.
The median one-way travel distance in remote areas was 6.3 miles (interquartile range [IQR], 1.3–18.6) before facility closures and 16.3 miles (IQR, 2.6–28.8) after closures. After closure, the average distance traveled in remote areas increased by 6.9 miles, with a median increase of 0.8 miles (IQR, −0.1 to 14.2). In micropolitan areas, only 16% of patients had an increase in travel distance of ≥10 miles. In rural/small-town areas, 44% of patients experienced a ≥10-mile increase in travel distance (Figure 1).
Figure 1.
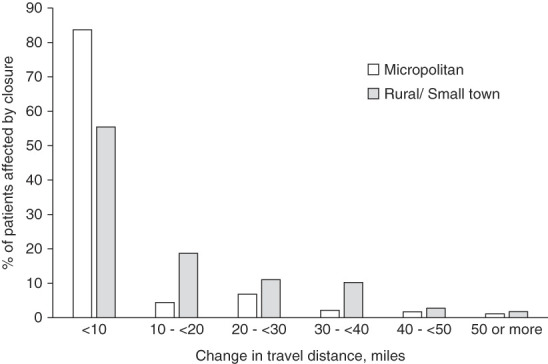
Distribution of changes in travel distance. Outlier patients who traveled >300 miles to dialysis facilities either before or after closure were excluded from the analysis. Population density is from census tract–based Rural–Urban Commuting Area codes. In micropolitan areas, primary commuting flows are to an urban cluster of 10,000–50,000 population. In small-town areas, primary commuting flows are to an urban cluster of 2500–10,000 population. In rural areas, primary commuting does not flow to an urban cluster. The average increase in distance traveled was 10.5 miles in small-town/rural areas and 3.7 miles in micropolitan areas. The median increase in distance traveled was 6.6 miles (IQR, 0–20.5) in small-town/rural areas and 0.2 miles (IQR, −0.2 to 2.2) in micropolitan areas. IQR, interquartile range.
In a fully adjusted model, changes in travel distance varied geographically. The odds of a ≥10-mile increase in one-way travel distance were four-fold higher (odds ratio [OR], 4.4; 95% confidence interval [CI], 3.5 to 5.4) in small-town areas and five-fold higher (OR, 5.6; 95% CI, 4.2 to 7.5) in rural areas relative to micropolitan areas. The odds of a ≥10-mile increase in travel distance were smaller after the closure of hospital-based facilities (OR, 0.4; 95% CI, 0.3 to 0.5) when compared with independently owned, nonhospital facilities. Other patient demographic, health, socioeconomic, and dialysis facility characteristics examined (including race, ethnicity, and Medicaid eligibility) were not independently associated with changes in travel distances after dialysis facility closures. The results were similar when examining a ≥20-mile increase in travel distance.
In summary, the distance traveled to receive dialysis increased among patients living in remote areas after dialysis facility closures. Increases in travel distance were most pronounced among patients living in rural/small-town areas. Increased travel distance after facility closures could have detrimental effects on the well-being of US patients receiving dialysis. Together with previous findings that dialysis facility closures were associated with increased hospitalizations,3 increased travel distances underscore the importance of ensuring that case mix, rural, and low-volume payment adjustment policies help to maintain access to care for patients living in remote areas.
Acknowledgments
This work was conducted under a data use agreement between K.F. Erickson and the National Institutes for Diabetes and Digestive and Kidney Diseases (NIDDK). An NIDDK officer reviewed the manuscript and approved it for submission. The data reported here have been supplied by the United States Renal Data System. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US government. The research protocol was approved by an Institutional Review Board at Baylor College of Medicine.
Disclosures
K.F. Erickson reports consultancy for Acumen LLC, and Boehringer Ingelheim; honoraria from Columbia University, Dialysis Clinic, Inc., Satellite Healthcare, UC Irvine, and University of Missouri; advisory or leadership roles as an American Journal of Kidney Diseases editorial board member, CJASN editorial board member, American Society of Nephrology Public Policy Board's Quality Committee member, and Seminars in Dialysis editorial board member; research funding from Health Care Service Corporation's Affordability Cures grant; and travel funds from KDIGO. All remaining authors have nothing to disclose.
Funding
This work was supported by ASN Foundation for Kidney Research from Carl W. Gottschalk Research Scholar Grant (K.F. Erickson).
Author Contributions
Conceptualization: Kevin F. Erickson, Abiodun Oluyomi, Omar Rosales.
Data curation: Kevin F. Erickson, Abiodun Oluyomi.
Formal analysis: Kevin F. Erickson, Jingbo Niu, Abiodun Oluyomi, Omar Rosales, Melandrea Worsley.
Funding acquisition: Kevin F. Erickson.
Investigation: Kevin F. Erickson, Jingbo Niu, Abiodun Oluyomi, Melandrea Worsley.
Methodology: Kevin F. Erickson, Jingbo Niu, Abiodun Oluyomi, Omar Rosales.
Project administration: Kevin F. Erickson, Abiodun Oluyomi.
Resources: Kevin F. Erickson, Abiodun Oluyomi, Omar Rosales.
Software: Kevin F. Erickson, Jingbo Niu, Abiodun Oluyomi, Omar Rosales.
Supervision: Kevin F. Erickson, Abiodun Oluyomi.
Validation: Kevin F. Erickson.
Visualization: Kevin F. Erickson, Jingbo Niu, Abiodun Oluyomi, Omar Rosales, Melandrea Worsley.
Writing – original draft: Kevin F. Erickson.
Writing – review & editing: Kevin F. Erickson, Jingbo Niu, Abiodun Oluyomi, Omar Rosales, Melandrea Worsley.
References
- 1.Erickson KF, Zhao B, Ho V, Winkelmayer WC. Employment among patients starting dialysis in the United States. Clin J Am Soc Nephrol. 2018;13(2):265–273. doi: 10.2215/CJN.06470617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DaVita Inc. DaVita Inc. 4th Quarter 2022 Results. DaVita Inc.; 2023. [Google Scholar]
- 3.Niu J, Saeed MK, Winkelmayer WC, Erickson KF. Patient health outcomes following dialysis facility closures in the United States. J Am Soc Nephrol. 2021;32(10):2613–2621. doi: 10.1681/ASN.2021020244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norouzi S, Zhao B, Awan A, Winkelmayer WC, Ho V, Erickson KF. Bundled payment reform and dialysis facility closures in ESKD. J Am Soc Nephrol. 2020;31(3):579–590. doi: 10.1681/ASN.2019060575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moist LM Bragg-Gresham JL Pisoni RL, et al. Travel time to dialysis as a predictor of health-related quality of life, adherence, and mortality: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2008;51(4):641–650. doi: 10.1053/j.ajkd.2007.12.021 [DOI] [PubMed] [Google Scholar]
- 6.Pattharanitima P El Shamy O Chauhan K, et al. The association between prevalence of peritoneal dialysis versus hemodialysis and patients' distance to dialysis-providing facilities. Kidney360. 2021;2(12):1908–1916. doi: 10.34067/kid.0004762021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salerno S Gremel G Dahlerus C, et al. Understanding the tradeoffs between travel burden and quality of care for in-center hemodialysis patients. Med Care. 2022;60(3):240–247. doi: 10.1097/mlr.0000000000001684 [DOI] [PubMed] [Google Scholar]


