Abstract
Autoimmune thyroid disorders (AITD) represent the most frequent of all autoimmune disorders. Their aetiopathogenesis is incompletely understood, but most likely multifactorial. Early life stress can have long-lasting effects on the immune system. The aim of the present study was to investigate, for the first time, whether patients with AITD are more frequently affected by early life stress. A total of N = 208 women were recruited into a case–control study. Of these, n = 78 (median age: 53, interquartile range: 15) were patients recruited from a thyroid outpatient clinic with confirmed Hashimoto’s thyroiditis, Graves’ disease, or AITD not otherwise specified. The remaining n = 130 age- and BMI-matched women (median age: 53, interquartile range: 12) were recruited from the general population. Early life stress was measured with the Childhood Trauma Questionnaire. Patients with AITD did not differ from controls regarding sexual abuse, physical abuse, and physical neglect. However, a greater number of patients reported emotional neglect (29.7% vs. 19.5%) and emotional abuse (41.3% vs. 32%). This study provides initial evidence for emotional neglect and abuse as potential risk factors for the development of AITD. Prospective confirmation of these findings could pave the way for the development of interventions to prevent AITD in predisposed individuals.
Subject terms: Thyroid diseases, Risk factors
Introduction
Autoimmune thyroid disorders (AITD) are the most frequent of all autoimmune disorders1,2, with Hashimoto’s thyroiditis and Graves’ disease representing its most severe forms3,4. The hypothalamic-pituitary-thyroid is regulated at multiple levels, including the release of hypothalamic thyrotropin-releasing hormone from the hypothalamus, thyroid stimulating hormone from the pituitary, and the thyroid hormones triiodothyronine and thyroxine from the thyroid gland. Moreover, the activation of thyroid hormones is governed by deiodinases, with type II deiodinase converting inactive thyroxine into active triiodothyronine. Both Hashimoto’s thyroiditis and Graves’ disease present with lymphocytic infiltration of the thyroid gland1,5,6. Hashimoto’s thyroiditis is predominantly characterised by a T cell-mediated immune response leading to thyroid destruction and, consequently, often presents with hypothyroidism4–7. Additionally, thyroid autoantibodies against thyroid peroxidase and thyroglobulin are often detected5,6,8,9. By contrast, Graves’ disease is primarily characterised by an antibody-mediated immune response leading to thyroid hormone overproduction. This causes hyperthyroidism due to the presence of thyroid-stimulating hormone receptor antibodies4,10–12. Older individuals are more frequently affected by AITD3 and women have a seven to eighteen times higher risk of developing AITD2,3. Given that AITD are chronic diseases that often require lifelong medication13,14, it is important to identify risk factors for their prevention.
Although the mechanisms that trigger autoimmunity against the thyroid are unclear, the aetiopathogenesis of AITD is, presumably, multifactorial1,9,15–17. Twin studies have confirmed the role of genetic factors in AITD18–20, with heritability estimates between 70 and 80%16,19. In addition, several environmental risk factors have been identified, including smoking, viral and bacterial infections, iodine intake, medication1,9,16,17,21, as well as vitamin D and selenium deficiency9, different environmental pollutants17,21 and external and internal irradiation1,17. Furthermore, there is increasing evidence that psychosocial stress is associated with the development of AITD17,22. Whereas the role of stress in the onset of Graves’ disease has been confirmed by numerous studies4,22, much less is known about a potential relationship between stress and Hashimoto’s thyroiditis. Importantly, similar to depression23,24, accumulating research not only suggests a relationship between stress in adulthood and AITD, but also between early life stress and AITD25–30.
In line with this notion, there is long-standing evidence that early life stress leads to altered immune functioning. This is presumably mediated by the two major stress-responsive systems, the sympathetic nervous system and the hypothalamic–pituitary–adrenal axis31,32. Both systems engage in a crosstalk with the immune system, and in manifold ways. For instance, catecholamines and glucocorticoids, the end products of these two systems, have been shown to induce a shift in the Th1/Th2 balance and release of pro- and anti-inflammatory cytokines, which may constitute a possible explanation for the development of AITD22,33,34. In line with this, numerous studies have found an association between early life stress and chronic low-grade inflammation in adulthood, both in healthy samples25–27 and in individuals with depression35–37. Furthermore, early life stress also seems to have a direct effect on the hypothalamic-pituitary-thyroid axis. For instance, elevated levels of thyroid-stimulating hormone have been observed in women with childhood sexual abuse28. Finally, individuals exposed to childhood trauma had an increased risk of developing autoimmune disorders29 and of developing thyroid disorders30.
In sum, there is considerable evidence which suggests that early life stress is involved in the aetiopathogenesis of AITD. However, to date, no studies have examined this potential link. The aim of the present case–control study was thus to investigate whether patients with AITD and healthy controls differ in the amount of experienced early life stress. It was hypothesised that patients with AITD would have higher rates of early life stress than healthy controls.
Results
Participant characteristics
Sociodemographic and lifestyle characteristics of the patients and the healthy controls are reported in Table 1. On average, the women in the sample were of middle age (median age: 53, interquartile range: 13), had a vocational education or a college/university degree (80%), were mothers of two children (interquartile range: 2), had a normal Body Mass Index (median: 22, interquartile range: 4; 26% were overweight and 5% were obese), and were non-smokers (87%). The patients and the controls did not differ in any of the sociodemographic and lifestyle variables, except for menopausal status, with more patients being in the perimenopausal phase (statistical trend).
Table 1.
Sociodemographic and lifestyle characteristics of patients with autoimmune thyroid diseases (AITD) and healthy controls.
| Patients (n = 78) | Healthy controls (n = 130) | p | |||
|---|---|---|---|---|---|
| n (%) | Mdn (IQR) | n (%) | Mdn (IQR) | ||
| Age (years) | 53 (15) | 53 (12) | 0.18 | ||
| BMI | 23 (5) | 22 (4) | 0.40 | ||
| Children (number) | 2 (2) | 2 (2) | 0.61 | ||
| Smoking (yes) | 12 (15) | 15 (12) | 0.42 | ||
| Menopause status* | 0.08 | ||||
| Pre | 30 (39) | 56 (43) | |||
| Peri | 14 (18) | 10 (8) | |||
| Post | 33 (43) | 64 (49) | |||
| AITD | |||||
| Hashimoto’s thyroiditis | 52 (67) | ||||
| Graves’ disease | 8 (10) | ||||
| Not otherwise specified | 18 (23) | ||||
Group comparisons were conducted using two-sided Mann–Whitney U tests and Pearson’s Chi-squared tests.
Mdn median, IQR interquartile range, BMI body mass index, AITD autoimmune thyroid diseases.
*Patients were categorised by self-report, whereas healthy controls were categorised by the Stages of Reproductive Aging Workshop + 10 (STRAW) criteria56: (1) pre if the menstrual cycle was regular, (2) peri if the cycle length was variable > 7 days or interval between cycles > 60 days, and (3) if there was no bleeding within 12 months.
Within the patient group, 67% of the women were diagnosed with Hashimoto’s thyroiditis (E.06.3), 10% with Graves’ disease (E05.0), and 23% with an AITD not otherwise specified (E06.9). The average age at diagnosis was 51 ± 11 and 54% had a family history of AITD. Two thirds of the patients were currently taking thyroid medication (e.g., l-thyrox, Euthyrox, Eltroxin) and 72% were euthyroid. With regard to comorbid diseases, 13% of the patients had a cardiovascular disease, 4% had an inflammatory disease, 4% had a metabolic disease, 6% suffered from recurrent headaches and 12% suffered from an affective disorder.
Early life stress in patients with autoimmune thyroid disorders versus healthy controls
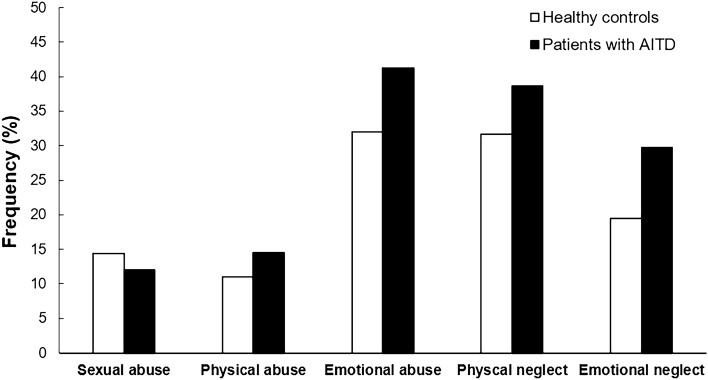
As is evident from Fig. 1, patients with AITD did not differ from healthy controls in terms of moderate to severe trauma regarding sexual abuse (12% vs. 14.4%; Χ2 = 0.231, p = 0.32), physical abuse (14.5% vs. 11%; Χ2 = 0.524, p = 0.24), and physical neglect (38.7% vs. 31.7%; Χ2 = 1.003, p = 0.16). However, a greater proportion of patients reported emotional abuse (41.3% vs. 32%; Χ2 = 1.779, p = 0.091, w = 0.092) and emotional neglect (29.7% vs. 19.5%; Χ2 = 2.695, p = 0.051, w = 0.114).
Figure 1.
Frequencies of childhood trauma (Childhood Trauma Questionnaire; CTQ) in patients with autoimmune thyroid disorders (AITD) and healthy controls. Group comparisons were conducted using one-sided Pearson’s Chi-squared tests. A greater proportion of patients reported emotional abuse (41.3% vs. 32%; Χ2 = 1.779, p = 0.091, w = 0.092) and emotional neglect (29.7% vs. 19.5%; Χ2 = 2.695, p = 0.051, w = 0.114).
Discussion
The main finding of this study is that female patients with AITD tended to have a higher frequency of emotional abuse and emotional neglect when compared to healthy controls. There were no differences between the two groups regarding other forms of childhood trauma. These findings will be discussed in the following paragraphs.
This is the first study to examine childhood trauma in AITD. Compared to a norm sample of German women of similar age38, the prevalence of emotional neglect in women with AITD was more than twice as high (29.7% vs. 13.4%) and the prevalence of emotional abuse was more than three times as high (41.3% vs. 10.9%), while the other forms did not show such marked differences. This suggests that emotional forms of childhood trauma may be particularly important risk factors for AITD. Notably, the prevalence of emotional neglect was also slightly higher in the healthy control group when compared to the norm sample (19.5% vs. 13.4%) and this was even more pronounced for emotional abuse (32% vs. 10.9%)38.
Our finding is in line with previous research showing that less obvious forms of maltreatment, such as emotional abuse and neglect, can have equally significant consequences for individuals’ development and health39. Childhood neglect has indeed been found to have long-term effects on children’s cognitive, social-emotional and behavioural development40. Moreover, it has also been demonstrated to affected children’s neuroendocrine stress response system up into adulthood41–43. Interestingly, there is evidence that different childhood trauma types lead to different changes in the hypothalamic–pituitary–adrenal axis and in the immune system44. In a meta-analysis of this literature, sexual and physical abuse were significantly associated with elevated tumour necrosis factor α and interleukin 6 concentrations, whereas neglect was primarily associated with elevated C-reactive protein levels45. It thus appears as if different types of childhood trauma were associated with different health outcomes. Interestingly, one study found elevated C-reactive protein levels in individuals with various types of hypo- and hyperthyroidism46, although other studies in Hashimoto thyroiditis or Graves’ disease could not confirm this association47,48. The jury is thus still out on whether long-lasting effects of emotional early life stress on immune functioning may facilitate the onset of AITD in combination with genetic and other environmental factors (e.g., stress in adulthood).
This study presents with a number of strengths. First and foremost, it is the first study investigating the association between early life stress and AITD. To this end, a state-of-the-art instrument was used to assess childhood trauma in five domains. However, a number of limitations should also be mentioned. First, the patient sample size was relatively small and smaller than the healthy control sample, which may have contributed to the borderline significant findings. Related to this, it was not possible to undertake group comparisons between patients with Hashimoto’s thyroiditis and Graves’ disease. Further, large-scale studies which are specifically designed for such case–control comparisons are thus warranted. Second, the female patient group in this study means that the results cannot be generalised to the male population and to individuals of other genders. Although, based on the extant literature, we do not expect that the relationship between early life stress and autoimmunity differs according to gender25–27,29, the present findings warrant replication in samples of non-female patients with AITD. Third, due to the lack of laboratory testing in the control group, inflammatory markers, thyroid parameters, and related antibodies could not be assessed. Therefore, potentially ongoing inflammatory processes and the presence of subclinical hypo-/hyperthyroidism and elevated antibodies in the control group cannot be excluded and may have obfuscated any further group differences. However, it should be mentioned that, due to the strict inclusion criteria, the control group had a particularly high health status. Finally, the retrospective study design and the fact that we used a self-reported instrument to assess childhood trauma does not allow to exclude potential memory biases regarding the reporting of childhood trauma.
In sum, the present study provides initial, tentative evidence for emotional early life stress as a potential risk factor for the development of AITD. Measures mitigating the detrimental effects of emotional early life stress may thus be considered to prevent the development of AITD. These could target individuals with family histories of autoimmune disorders who report early life stress, but have not yet developed AITD. Similar to other lifestyle variables which constitute risk factors for AITD, this could mean that predisposed individuals are advised to actively manage their stress (e.g., by efficacious programmes such as mindfulness-based stress reduction). This could not only have beneficial effects on the immune system49 and, potentially, on the hypothalamic-pituitary-thyroid axis50, but also help to prevent depression and anxiety, which frequently feature in these conditions51,52. However, further, large-scale cohort studies are necessary to replicate and extend the herein reported findings before such measures could potentially be considered.
Methods
Participants and protocol
A total of N = 208 women were recruited into a case–control study. Of these, n = 78 were patients with AITD. The patients were recruited at the Thyroid Center Zurich, which constitutes the largest outpatient clinic exclusively specialising in thyroid diseases in Switzerland. Autoimmune thyroid disorders were diagnosed by a thyroid specialist (HE) and based on clinical features, laboratory testing (serum levels of thyroid-stimulating hormone, free triiodothyronine, and free thyroxine, as well as thyroglobulin antibodies, thyroid peroxidase antibodies and/or thyroid-stimulating hormone receptor antibodies), and sonographic morphology and perfusion. All patients who had a diagnosis of Hashimoto’s thyroiditis (E.06.3), Graves’ disease (E05.0), or AITD not otherwise specified (E06.9), which represented the bulk of AITD at the outpatient clinic, were asked whether they would be interested in taking part in the study. Further inclusionary criteria were being fluent in German and between 40 and 75 years of age. Patients who met these criteria were asked to fill in the Childhood Trauma Questionnaire, as detailed below. In addition, a total of n = 130 women from a study on healthy ageing were used as healthy controls. This sample has previously been described in detail53. In brief, women between the age of 40 and 75 who had to be free of any somatic diseases (including acute infections) or mental disorders were recruited via flyers and advertisements in newspapers and social media. Importantly, both samples were recruited during the same time period (i.e., from 2017 to 2020) and in the same geographical area (i.e., the Canton of Zurich).
Written informed consent was obtained for participation in both studies and the study protocol was approved by the Ethics Committee of the Canton of Zurich (BASEC 2021-00983). All methods were performed in accordance with the relevant guidelines and regulations.
Psychological data
The short version of the Childhood Trauma Questionnaire38,54 was used to measure early life stress. The Childhood Trauma Questionnaire is one of the most frequently used psychometric instruments to assess early life stress worldwide. It has been extensively validate and also proven to be reliable (Cronbach’s alpha ≥ 0.89) and valid (e.g., regarding its factorial structure and correlation with trauma-associated disorders) in German-speaking samples55. It has 25 items assessed on a five-point Likert scale (from 1 to 5) and distinguishes five trauma domains consistent with the consensus definition of childhood trauma38: emotional neglect, physical neglect, emotional abuse, physical abuse, and sexual abuse. Example items are: “When I was growing up, people in my family looked out for each other” (emotional neglect, reversed item), “When I was growing up, my parents were too drunk or high to take care of the family” (physical neglect), “When I was growing up, people in my family called me things like stupid, lazy, or ugly” (emotional abuse), “When I was growing up, I was punished with a belt, a board, a cord, or some other hard object” (physical abuse), “When I was growing up, someone tried to touch me in a sexual way, or tried to make me touch them” (sexual abuse). The presence vs. absence of childhood trauma was determined based on validated cut-off scores for moderate to severe trauma38. These were ≥ 15 for emotional neglect, ≥ 8 for physical neglect, ≥ 10 for emotional abuse, ≥ 8 for physical abuse, and ≥ 8 for sexual abuse.
Medical data
The medical data extracted from the clinic’s data base consisted of diagnoses, thyroid parameters (thyroid-stimulating hormone, free triiodothyronine, free thyroxine, antibodies), and information about thyroid medication intake.
Laboratory analyses
Thyroid parameters (i.e., thyroid-stimulating hormone, free triiodothyronine, free thyroxine, antibodies) were determined in the biochemical laboratory at the Thyroid Center Zurich, which is an outpatient clinic located in a large hospital. Blood was collected by means of venepuncture and all samples were processed and analysed in loco before being entered into the data base.
Statistical analyses
Assuming a medium effect size (α = 0.05, 1 − β = 0.80), an a priori power analysis resulted in a total sample size of N = 88. Due to deviation from a normal distribution and/or missing homoscedasticity, all continuous variables were analysed by means of Mann–Whitney U tests. Chi-squared tests were computed to compare patients and controls in terms of dichotomous variables. All analyses were conducted using the Statistical Package for the Social Sciences (SPSS) 25, and the main analyses were tested one-tailed with a significance level of α < 0.05.
Acknowledgements
We would like to acknowledge the most valuable help of Cornelia Bolkart, Marion Kadura, Dominik Fluekiger, Vivienne Hug, and Nicole Koch-Etterli in conducting the study.
Author contributions
H.E., Su.F., and U.E. conceived and designed the study. A.C., F.M., Se.F., L.M., and E.G. acquired the data. A.C. analysed and interpreted the data. A.C. and Su.F. drafted the article and revised it critically for important intellectual content. All authors approved the final version of the article.
Funding
Parts of the study were funded by the URPP Dynamics of Healthy Aging Research Priority Program.
Data availability
Data is not publicly available due to ethical reasons. Further enquiries can be directed to the corresponding author.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Antonelli A, Ferrari SM, Corrado A, Di Domenicantonio A, Fallahi P. Autoimmune thyroid disorders. Autoimmun. Rev. 2015;14:174–180. doi: 10.1016/j.autrev.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 2.Shapira Y, Agmon-Levin N, Shoenfeld Y. Defining and analyzing geoepidemiology and human autoimmunity. J. Autoimmun. 2010;34:J168–177. doi: 10.1016/j.jaut.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 3.McLeod DS, Cooper DS. The incidence and prevalence of thyroid autoimmunity. Endocrine. 2012;42:252–265. doi: 10.1007/s12020-012-9703-2. [DOI] [PubMed] [Google Scholar]
- 4.Bagnasco M, Bossert I, Pesce G. Stress and autoimmune thyroid diseases. Neuroimmunomodulation. 2006;13:309–317. doi: 10.1159/000104859. [DOI] [PubMed] [Google Scholar]
- 5.Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N. Engl. J. Med. 2003;348:2646–2655. doi: 10.1056/NEJMra021194. [DOI] [PubMed] [Google Scholar]
- 6.Dayan CM, Daniels GH. Chronic autoimmune thyroiditis. N. Engl. J. Med. 1996;335:99–107. doi: 10.1056/NEJM199607113350206. [DOI] [PubMed] [Google Scholar]
- 7.Ralli M, et al. Hashimoto's thyroiditis: An update on pathogenic mechanisms, diagnostic protocols, therapeutic strategies, and potential malignant transformation. Autoimmun. Rev. 2020;19:102649. doi: 10.1016/j.autrev.2020.102649. [DOI] [PubMed] [Google Scholar]
- 8.Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017;390:1550–1562. doi: 10.1016/S0140-6736(17)30703-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Effraimidis G, Wiersinga WM. Mechanisms in endocrinology: Autoimmune thyroid disease: Old and new players. Eur. J. Endocrinol. 2014;170:R241–252. doi: 10.1530/EJE-14-0047. [DOI] [PubMed] [Google Scholar]
- 10.De Leo S, Lee SY, Braverman LE. Hyperthyroidism. Lancet. 2016;388:906–918. doi: 10.1016/S0140-6736(16)00278-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gianoukakis AG, Khadavi N, Smith TJ. Cytokines, Graves' disease, and thyroid-associated ophthalmopathy. Thyroid. 2008;18:953–958. doi: 10.1089/thy.2007.0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Antonelli A, et al. Graves' disease: Clinical manifestations, immune pathogenesis (cytokines and chemokines) and therapy. Best Pract. Res. Clin. Endocrinol. Metab. 2020;34:101388. doi: 10.1016/j.beem.2020.101388. [DOI] [PubMed] [Google Scholar]
- 13.Caturegli P, De Remigis A, Rose NR. Hashimoto thyroiditis: Clinical and diagnostic criteria. Autoimmun. Rev. 2014;13:391–397. doi: 10.1016/j.autrev.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 14.Quadbeck B, Hormann R, Janssen OE, Mann K. Drug treatment of immune hyperthyroidism (Basedow disease). Patient selection, long-term follow-up and prevention of recurrence. Internist (Berl) 2003;44:440–448. doi: 10.1007/s00108-003-0876-x. [DOI] [PubMed] [Google Scholar]
- 15.Medici M, Visser WE, Visser TJ, Peeters RP. Genetic determination of the hypothalamic–pituitary–thyroid axis: Where do we stand? Endocr. Rev. 2015;36:214–244. doi: 10.1210/er.2014-1081. [DOI] [PubMed] [Google Scholar]
- 16.Wiersinga WM. Clinical relevance of environmental factors in the pathogenesis of autoimmune thyroid disease. Endocrinol. Metab. (Seoul) 2016;31:213–222. doi: 10.3803/EnM.2016.31.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tanda ML, et al. Thyroid autoimmunity and environment. Horm. Metab. Res. 2009;41:436–442. doi: 10.1055/s-0029-1215568. [DOI] [PubMed] [Google Scholar]
- 18.Brix TH, Kyvik KO, Hegedus L. A population-based study of chronic autoimmune hypothyroidism in Danish twins. J. Clin. Endocrinol. Metab. 2000;85:536–539. doi: 10.1210/jcem.85.2.6385. [DOI] [PubMed] [Google Scholar]
- 19.Brix TH, Hegedus L. Twin studies as a model for exploring the aetiology of autoimmune thyroid disease. Clin. Endocrinol. 2012;76:457–464. doi: 10.1111/j.1365-2265.2011.04318.x. [DOI] [PubMed] [Google Scholar]
- 20.Hansen PS, Brix TH, Iachine I, Kyvik KO, Hegedus L. The relative importance of genetic and environmental effects for the early stages of thyroid autoimmunity: A study of healthy Danish twins. Eur. J. Endocrinol. 2006;154:29–38. doi: 10.1530/eje.1.02060. [DOI] [PubMed] [Google Scholar]
- 21.Eschler DC, Hasham A, Tomer Y. Cutting edge: The etiology of autoimmune thyroid diseases. Clin. Rev. Allergy Immunol. 2011;41:190–197. doi: 10.1007/s12016-010-8245-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mizokami T, Wu Li A, El-Kaissi S, Wall JR. Stress and thyroid autoimmunity. Thyroid. 2004;14:1047–1055. doi: 10.1089/thy.2004.14.1047. [DOI] [PubMed] [Google Scholar]
- 23.Hammen C. Stress and depression. Annu. Rev. Clin. Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 24.Humphreys KL, et al. Child maltreatment and depression: A meta-analysis of studies using the Childhood Trauma Questionnaire. Child Abuse Negl. 2020;102:104361. doi: 10.1016/j.chiabu.2020.104361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coelho R, Viola TW, Walss-Bass C, Brietzke E, Grassi-Oliveira R. Childhood maltreatment and inflammatory markers: A systematic review. Acta Psychiatr. Scand. 2014;129:180–192. doi: 10.1111/acps.12217. [DOI] [PubMed] [Google Scholar]
- 26.Elwenspoek MMC, Kuehn A, Muller CP, Turner JD. The effects of early life adversity on the immune system. Psychoneuroendocrinology. 2017;82:140–154. doi: 10.1016/j.psyneuen.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 27.Danese A, Lewis SJ. Psychoneuroimmunology of early-life stress: The hidden wounds of childhood trauma? Neuropsychopharmacology. 2017;42:99–114. doi: 10.1038/npp.2016.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bunevicius A, Leserman J, Girdler SS. Hypothalamic-pituitary-thyroid axis function in women with a menstrually related mood disorder: Association with histories of sexual abuse. Psychosom. Med. 2012;74:810–816. doi: 10.1097/PSY.0b013e31826c3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dube SR, et al. Cumulative childhood stress and autoimmune diseases in adults. Psychosom. Med. 2009;71:243–250. doi: 10.1097/PSY.0b013e3181907888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fuller-Thomson E, Kao F, Brennenstuhl S, Yancura LA. Exploring gender differences in the association between childhood physical abuse and thyroid disorders. J. Aggress. Maltreat. T. 2013;22:590–610. doi: 10.1080/10926771.2013.803508. [DOI] [Google Scholar]
- 31.McEwen BS. Protective and damaging effects of stress mediators. N. Engl. J. Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 32.Fagundes CP, Glaser R, Kiecolt-Glaser JK. Stressful early life experiences and immune dysregulation across the lifespan. Brain Behav. Immun. 2013;27:8–12. doi: 10.1016/j.bbi.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsatsoulis A. The role of stress in the clinical expression of thyroid autoimmunity. Ann. N. Y. Acad. Sci. 2006;1088:382–395. doi: 10.1196/annals.1366.015. [DOI] [PubMed] [Google Scholar]
- 34.Elenkov IJ, Chrousos GP. Stress, cytokine patterns and susceptibility to disease. Baillieres Best Pract. Res. Clin. Endocrinol. Metab. 1999;13:583–595. doi: 10.1053/beem.1999.0045. [DOI] [PubMed] [Google Scholar]
- 35.Wang AK, Miller BJ. Meta-analysis of cerebrospinal fluid cytokine and tryptophan catabolite alterations in psychiatric patients: Comparisons between schizophrenia, bipolar disorder, and depression. Schizophr. Bull. 2018;44:75–83. doi: 10.1093/schbul/sbx035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Osimo EF, et al. Inflammatory markers in depression: A meta-analysis of mean differences and variability in 5,166 patients and 5,083 controls. Brain Behav. Immun. 2020;87:901–909. doi: 10.1016/j.bbi.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mac Giollabhui N, Ng TH, Ellman LM, Alloy LB. The longitudinal associations of inflammatory biomarkers and depression revisited: Systematic review, meta-analysis, and meta-regression. Mol. Psychiatry. 2021;26:3302–3314. doi: 10.1038/s41380-020-00867-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iffland B, Brahler E, Neuner F, Hauser W, Glaesmer H. Frequency of child maltreatment in a representative sample of the German population. BMC Public Health. 2013;13:980. doi: 10.1186/1471-2458-13-980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Egeland B. Taking stock: Childhood emotional maltreatment and developmental psychopathology. Child Abuse Negl. 2009;33:22–26. doi: 10.1016/j.chiabu.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 40.Hildyard KL, Wolfe DA. Child neglect: Developmental issues and outcomes. Child Abuse Negl. 2002;26:679–695. doi: 10.1016/s0145-2134(02)00341-1. [DOI] [PubMed] [Google Scholar]
- 41.Blaisdell KN, Imhof AM, Fisher PA. Early adversity, child neglect, and stress neurobiology: From observations of impact to empirical evaluations of mechanisms. Int. J. Dev. Neurosci. 2019;78:139–146. doi: 10.1016/j.ijdevneu.2019.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brindle RC, Pearson A, Ginty AT. Adverse childhood experiences (ACEs) relate to blunted cardiovascular and cortisol reactivity to acute laboratory stress: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2022;134:104530. doi: 10.1016/j.neubiorev.2022.104530. [DOI] [PubMed] [Google Scholar]
- 43.Khoury JE, Bosquet Enlow M, Plamondon A, Lyons-Ruth K. The association between adversity and hair cortisol levels in humans: A meta-analysis. Psychoneuroendocrinology. 2019;103:104–117. doi: 10.1016/j.psyneuen.2019.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kuhlman KR, Chiang JJ, Horn S, Bower JE. Developmental psychoneuroendocrine and psychoneuroimmune pathways from childhood adversity to disease. Neurosci. Biobehav. Rev. 2017;80:166–184. doi: 10.1016/j.neubiorev.2017.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: A meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-alpha. Mol. Psychiatry. 2016;21:642–649. doi: 10.1038/mp.2015.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Czarnywojtek A, et al. The role of serum C-reactive protein measured by high-sensitive method in thyroid disease. Arch. Immunol. Ther. Exp. (Warsz) 2014;62:501–509. doi: 10.1007/s00005-014-0282-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rao NL, et al. Salivary C-reactive protein in Hashimoto's thyroiditis and subacute thyroiditis. Int. J. Inflamm. 2010;2010:514659. doi: 10.4061/2010/514659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chu CH, et al. Change of visfatin, C-reactive protein concentrations, and insulin sensitivity in patients with hyperthyroidism. Metabolism. 2008;57:1380–1383. doi: 10.1016/j.metabol.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 49.Rosenkranz MA, et al. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain Behav. Immun. 2013;27:174–184. doi: 10.1016/j.bbi.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fischer S, et al. Effects of acute psychosocial stress on the hypothalamic–pituitary–thyroid (HPT) axis in healthy women. Psychoneuroendocrinology. 2019;110:104438. doi: 10.1016/j.psyneuen.2019.104438. [DOI] [PubMed] [Google Scholar]
- 51.Fischer S, Ehlert U. Hypothalamic–pituitary–thyroid (HPT) axis functioning in anxiety disorders. A systematic review. Depress. Anxiety. 2018;35:98–110. doi: 10.1002/da.22692. [DOI] [PubMed] [Google Scholar]
- 52.Bauer M, Goetz T, Glenn T, Whybrow PC. The thyroid–brain interaction in thyroid disorders and mood disorders. J. Neuroendocrinol. 2008;20:1101–1114. doi: 10.1111/j.1365-2826.2008.01774.x. [DOI] [PubMed] [Google Scholar]
- 53.Fiacco S, Mernone L, Ehlert U. Psychobiological indicators of the subjectively experienced health status—Findings from the Women 40+ Healthy Aging Study. BMC Womens Health. 2020;20:16. doi: 10.1186/s12905-020-0888-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bernstein DP, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–190. doi: 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 55.Wingenfeld K, et al. The German version of the Childhood Trauma Questionnaire (CTQ): Preliminary psychometric properties. Psychother. Psychosom. Med. Psychol. 2010;60:442–450. doi: 10.1055/s-0030-1247564. [DOI] [PubMed] [Google Scholar]
- 56.Harlow SD, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: Addressing the unfinished agenda of staging reproductive aging. J. Clin. Endocrinol. Metab. 2012;97:1159–1168. doi: 10.1210/jc.2011-3362. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is not publicly available due to ethical reasons. Further enquiries can be directed to the corresponding author.