Abstract
The application of new technologies in medical education still lags behind the extraordinary advances of AI. This study examined the understanding, attitudes, and perspectives of Vietnamese medical students toward AI and its consequences, as well as their knowledge of existing AI operations in Vietnam. A cross-sectional online survey was administered to 1142 students enrolled in undergraduate medicine and pharmacy programs. Most of the participants had no understanding of AI in healthcare (1053 or 92.2 %). The majority believed that AI would benefit their careers (890 or 77.9 %) and that such innovation will be used to oversee public health and epidemic prevention on their behalf (882 or 77.2 %). The proportion of students with satisfactory knowledge significantly differed depending on gender (P < 0.001), major (P = 0.003), experience (P < 0.001), and income (P = 0.011). The percentage of respondents with positive attitudes significantly differed by year level (P = 0.008) and income (P = 0.003), and the proportion with favorable perspectives regarding AI varied considerably by age (P = 0.046) and major (P < 0.001). Most of the participants wanted to integrate AI into radiology and digital imaging training (P = 0.283), while the fifth-year students wished to learn about AI in medical genetics and genomics (P < 0.001, 4.0 ± 0.8). The male students had 1.898 times more adequate knowledge of AI than their female counterparts, and those who had attended webinars/lectures/courses on AI in healthcare had 4.864 times more adequate knowledge than those having no such experiences. The majority believed that the barrier to implementing AI in healthcare is the lack of financial resources (83.54 %) and appropriate training (81.00 %). Participants saw AI as a “partner” rather than a “competitor”, but the majority of low knowledge was recorded. Future research should take into account the way to integrate AI into medical training programs for healthcare students.
Keywords: Artificial intelligence, AI, Healthcare student, KAP, Vietnam
1. Introduction
Artificial intelligence (AI) is described as “the theory and development of computer systems capable of performing tasks ordinarily requiring human intellect, such as visual perception, speech recognition, decision-making, and language translation” [1,2]. AI is possibly the longest standing and most extensive domain of computer science, dealing with all elements that simulate cognitive abilities for real-world problem solving and the development of machine learning and human-like reasoning [3]. It can mimic cognitive operations, such as image recognition, speech recognition, and annotation generation [4].
Over the past few decades, AI has received unprecedented attention [5] and has been touted as a gateway to the Fourth Industrial Revolution [[6], [7], [8]]. Its use in the healthcare sector has significantly grown because of increasing amounts of data and processing power [9], and it has enabled practitioners to overcome the problems encountered in the provision of medical services [10]. Many health issues, such as eye disorders, pneumonia, and breast and skin malignancies, can now be reliably identified via a rapid assessment of medical images using AI technology [9,[11], [12], [13]]. AI applications can also detect coronary heart disease through the analysis of echocardiography [14]; uncover mental events and neurological diseases, such as Parkinson's disease, from voice samples [15]; facilitate the diagnosis of polyps and tumors in the digestive system [16]; and perform certain procedural tasks, such as knotting during robotic surgery [17]. These AI capabilities extend to assisting the healthcare industry in management, diagnosis, treatment planning, medical education, medical record mining, drug formulation, and evaluation classification [[18], [19], [20], [21]]. Nevertheless, despite the current dominance of AI as a topic in scientific conferences and documents, its clinical use remains in its early stages. Modern medicine struggles to use new technological tools, including those supported by AI, to gather, evaluate, and use the vast amount of knowledge needed to solve specific clinical problems, such as establishing diagnoses, screening patient, making treatment decisions, and predicting treatment outcomes [22].
It is important for physicians to understand the potential of AI and the issues associated with it to make informed decisions and provide comprehensive treatment [23,24]. Clinicians and health informatics professionals who design AI applications must have a solid knowledge of the basic ideas of the technology to apply and filter AI-based judgments [1]. Depending on the algorithms, data sources, and methods used, the application of AI in healthcare can lead to unintended consequences and misleading conclusions [25]. Such sound scientific principles that underpin emerging technologies in healthcare should be disseminated to medical students, who are the future of the industry, to stimulate innovation [19]. Notwithstanding the increasing interest in new innovations, medical education continues to lag behind the phenomenal advances of AI [4]. Several calls to action have been made [[26], [27], [28]], but the incorporation of AI training into undergraduate medical education (UME) has been slow. Meanwhile, reduced exposure to AI causes anxiety among undergraduate medical students, thereby influencing their future career decisions [29,30]. Accordingly, investigating the general attitudes and current knowledge base of healthcare students can be a powerful avenue through which to identify areas of concern and an essential reference for making decisions to incorporate AI into UME [31]. However, before applying AI widely in healthcare and education, some of the issues that must be addressed include patient privacy, ethical considerations, black box issues, the reliability of input data, confounding factors, and adversarial attacks [32]. Therefore, an equally important task is to acknowledge the obstacles and limitations of AI before using this technology to derive and interpret results.
Several attempts have been made to poll physicians, physicians in training, and medical students about their perceptions and attitudes regarding AI's incorporation into healthcare, as well their levels of familiarity with AI platforms and applications in clinical practice [33]. The first study involving medical students, published in 2018, was aimed at understanding opinions regarding AI inclusion in radiology and medicine [34]. The majority of participants agreed that AI will revolutionize and improve radiology. Another study reported that medical students are not interested in using AI to replace radiologists [33]. Similar results were found in research conducted in a medical school in Pakistan and 17 medical schools in Canada, where medical students exhibit positive feelings about AI [6,29]. A recent study in the UK investigated medical students' views about AI and their choice of radiology as a specialty [30]. In general, the students do not believe that they are equipped to practice alongside such technology, but because they are aware of its importance of AI, they look forward to guidance on this topic.
Many studies have been devoted to illuminating how AI algorithms can assist in improving education [[35], [36], [37], [38], [39]], but those focusing on the integration of AI into medical education remains limited. Information about students' knowledge, attitudes, and perspectives on the role of AI in healthcare as well as students' desires for access to AI is fundamental to widespread adoption and highlights the valuable evidence for educational policymakers regarding AI education in healthcare as well as the necessity of the interdisciplinary collaboration of healthcare stakeholders to plan for AI-based training. Besides, the dissemination of modern scientific and technological principles will serve as a basis to stimulate innovation in the field of healthcare, in which students are the core force, the future of the health industry. To address this deficiency, the current research examined the understanding, attitudes, and perspectives of southern Vietnamese medical students toward AI and its consequences. It also assessed their comprehension of existing AI activities in Vietnam.
2. Materials and methods
2.1. Research design
This study is a descriptive, cross-sectional, observational, quantitative, and analytical research conducted at the Pham Ngoc Thach University of Medicine (PNTU) in Ho Chi Minh City, Vietnam in March 2023. It was conducted following the quality standards stipulated in the Appraisal tool for Cross-Sectional Studies [40].
2.2. Study participants and sample size
2.2.1. Study participants
The study was targeted toward male and female students enrolled in undergraduate programs in medicine and pharmacy at PNTU. Those who were willing to participate in the study were recruited, whereas those who returned an incomplete questionnaire, provided unsatisfactory answers to an exclusion-related question, and provided a single response to all questions were excluded from the analyses.
2.2.2. Sample size
A single-population proportion formula [41] was used to estimate the minimum sample size (N) required for this work. A 95 % confidence interval (Zα/2 = 1.96), a 5 % margin of error (d), and a 10 % non-response rate were assumed. This process yielded a target sample size of 423 participants.
2.3. Data collection
2.3.1. Scale translation, validity, and reliability
This study adapted a well-structured, self-administered questionnaire from previous studies after a thorough examination of the literature [[42], [43], [44], [45]]. The questionnaire was initially prepared in English, after which it was translated to local Vietnamese languages by two independent translators. The two Vietnamese translations were compared to identify their differences and the shortcomings arising in the translation process. Solutions to these shortcomings were found, after which the suitability of the questionnaires for Vietnamese students was confirmed. The consistency of content, clarity and suitability of meanings of the two versions were preserved through the back-translation to the original form.
The draft questionnaire consisted of 62 items. We ran an experimental survey with 114 participants by using convenience sampling to assess the usability and technical effectiveness of the instrument, as well as ensure its validity and reliability. The internal consistency of the sub-scales was determined using exploratory factor analysis, through which we found a factor loading = 0.350 (Kaiser-Meyer-Olkin (KMO) = 0.680, p-value = 0.001) and Cronbach's alpha values ranging from 0.650 to 0.750. We also carried out confirmatory factor analysis (Chi-Square (CMIN/df) = 1.469, Goodness of fit index (GFI) = 0.770, Comparative fit index (CFI) = 0.823, Root means square error of approximation (RMSEA) = 0.064, and P-value of close fit (PCLOSE) = 0.028). The appropriate domains and items for incorporation in the questionnaire were selected.
2.3.2. Procedure
A web-based online poll was designed, for which the corresponding questionnaire was created on the Google Forms platform. The self-report questionnaire and an invitation to participate in the study were distributed through social media to recruit eligible participants. Snowball sampling was performed by sharing the survey URL with members of the participants’ networks.
The goal and methodology of the study were disclosed on the main page of the survey. Before accessing the questionnaire, respondents were required to affirm their readiness to voluntarily participate via an informed consent form. They were informed of their right to withdraw from participation at any time and given the researchers' contact information in case they had questions or concerns. Individuals who gave consent were instructed to click on the “accept” button and complete the questionnaire. All the data were anonymized and processed using a coding scheme. The participants’ personal information was kept confidential, encrypted, and used only for the purposes of the research. A total of 1805 individuals were eligible to participate, but only 1142 returned complete questionnaires.
2.4. Measurements
The survey consisted of 46 items, including multiple-choice items that were to be rated on five- and three-point Likert scales. The questions centered on five broad topics, namely, demographic information, perspectives, attitudes, knowledge and barriers.
2.4.1. Demographic information
The section on demographics consisted of questions regarding age, gender, year level, experience participating in seminars/lectures/courses, sources of information about the application of AI, monthly personal income, and willingness to pay for an AI-based course. The data were presented as numbers, percentages, mean values, interquartile ranges, and standard deviations.
2.4.2. Perspectives toward AI
This sub-scale was composed of 14 questions about perspectives regarding AI issues, including personalization, AI application in hospitals and community healthcare centers, and other AI topics of interest. “Agree” or “strongly agree” responses were given a score of 1, whereas “neutral”, “disagree or strongly disagree” responses were scored 0. Scores greater than 3 were considered indicative of favorable perspectives, and responses pertaining to AI topics of interest were not graded (Table S1 in the Supplementary materials).
2.4.3. Attitudes toward AI
This sub-scale consisted of 17 questions about attitudes toward AI (including one that was repeated as an exclusion question). The questions revolved around common influence, career effects, challenges, and education. Responses of neutrality and disagreement or strong disagreement were scored 0, whereas “agree” or “strongly agree” answers were assigned a score of 1. Scores greater than 8 were regarded as reflective of good attitudes (Table S1 in the Supplementary materials).
2.4.4. Knowledge of AI
This sub-scale had six questions about general knowledge of AI, including knowledge of AI as a whole, machine learning, deep learning, and AI in the medical field. “Yes” and “no” or “somewhat” responses were scored 1 and 0, respectively. Scores exceeding 3 were regarded as pointing to good knowledge (Table S1 in the Supplementary materials).
2.4.5. Barriers to the implementation of AI in healthcare
This sub-scale has one multiple-choice question about barriers, and the results were expressed as a graph of percentages. The participants were also instructed to answer 16 questions about attitudes, 14 about their opinions, and 6 regarding their knowledge of AI using a five-point Likert scale. Each “strongly disagree”, “disagree”, and “neutral” response was scored with 0 points, whereas each “agree” and “strongly agree” answer was given 1 point. The students’ attitudinal score was calculated on the basis of their total scores; that is, if a student obtained 50 % of the maximum possible total score, they were classified as having positive attitudes. The same calculations were performed in the assessment of knowledge and perspectives [46].
2.5. Data management and statistical analyses
2.5.1. Data management
Data cleansing, coding, editing, and sorting were conducted in Microsoft Excel 2019, and an Excel file containing all the variables were imported into IBM's Statistical Package for the Social Sciences [SPSS] version 20.0. Before the analyses, the completed questionnaires were checked for completeness, consistency, and accuracy.
2.5.2. Statistics analyses
Descriptive analysis was carried out, and the results were organized in tables and figures illustrating frequencies and percentages. Cronbach's alpha coefficient was used to assess the scale's internal consistency. To investigate the statistical association between the categorical variables, a chi-square test was performed. The variables were examined using a 95 % confidence interval, and a p-value<0.05 was considered significant. Depending on the normality of the data, Mann-Whitney and Kruskal-Wallis tests were conducted. In addition, univariate logistic regression was carried out to predict AI outcome metrics, such as knowledge, attitudes, and viewpoints, on the basis of the participants' baseline characteristics. The regression employed unadjusted odds ratios and their respective 95 % confidence intervals.
2.6. Ethical considerations
Ethical approval was granted by the Ethics Committee of Pham Ngoc Thach University of Medicine (No. 847/TĐHYKPNT-HĐĐĐ). The participants voluntarily took part in the survey, and their commitment to participate was documented. They were informed that all collected data would be kept anonymous and confidential and that they would be used only for scientific research purposes.
3. Results
Table 1 shows that among the respondents, 268 (23.5 %) were completing a pharmacy program, and 874 (76.5 %) were medical students. Most of them (659 or 57.7 %) were 18–21 years old. The majority (676 or 59.2 %) were females, and 312 (27.3 %) were in their second year of study.
Table 1.
Baseline characteristics of the study population (n = 1142).
| Characteristics | n (%) | Characteristics | n (%) |
|---|---|---|---|
| Gender | Income (US$c per month) | ||
| Male | 466 (40.8) | None | 387 (33.9) |
| Female | 676 (59.2) | <60 | 241 (21.1) |
| Age | n (%) | 60-<120 | 253 (22.2) |
| 18-21 | 659 (57.7) | 120-<180 | 131 (11.5) |
| 22-25 | 473 (41.4) | 180-<240 | 82 (7.2) |
| 26-29 | 10 (0.9) | ≥240 | 48 (4.1) |
| Mean (SDa) | 21.3 (1.7) | WTPdfor the basic AIecourse (1 day) (US$) | |
| Range [Min - Max] | [[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]] | Not engaged | 72 (6.3) |
| IQRb [Q1 - Q3] | [[20], [21], [22]] | Engaged for free | 771 (67.5) |
| University year | <40 | 254 (22.2) | |
| First year | 208 (18.2) | 40-<80 | 38 (3.3) |
| Second year | 312 (27.3) | 80-<120 | 3 (0.3) |
| Third year | 160 (14.0) | ≥120 | 4 (0.4) |
| Fourth year | 224 (19.6) | Source of information | |
| Fifth year | 128 (11.2) | From peers/friends/mentors/teachers | 1219 |
| Sixth year | 110 (9.7) | From the media/social media and movie | 2144 |
| Majors | From webinars/lectures/formal training | 437 | |
| Medicine | 874 (76.5) | Attended any webinar/lecture/course on AI in healthcare | |
| Pharmacy | 268 (23.5) | Yes | 125 (10.9) |
| No | 1017 (89.1) | ||
Note.
SD: Standard Deviation.
IQR: Interquartile range.
US$1 = VND23,559 (Source: Vietnamese Ministry of Finance: Exchange rate for foreign currencies in February 2023).
WTP: Willingness to pay.
AI: Artificial intelligence.
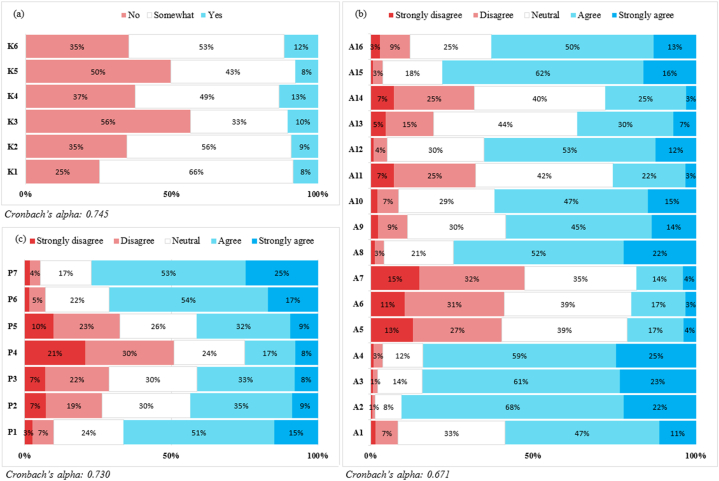
The descriptive statistics related to the students’ KAP are presented in Fig. 1. Among them, 1053 (92.2 %) had no understanding of AI in healthcare [Fig. 1(a)], but 890 (77.9 %) and 882 (77.2 %) expressed the beliefs that AI will benefit their careers and will be used to oversee public health and epidemic prevention on their behalf, respectively [Fig. 1(b and c)].
Fig. 1.
The responses patterns of (a) knowledge, (b) attitudes, and (c) perspectives regarding AI (n = 1142)
Note: K1–K6, A1-A16 and P1–P7 representative of questions pertaining to knowledge, attitudes, and perspectives (see Table S1 in the Supplementary materials); A1-A4, A8-A10, A12, A15, P6–P7: The percentage of the “strongly disagree” level in Fig. 1(b) and (c) is less than or equal 2 %.
Table 2 shows the differences in KAP regarding AI depending on various baseline variables. The proportion of students with good AI knowledge significantly differed across genders (P < 0.001), majors (P = 0.003), experiences (P < 0.001), and incomes (P = 0.011). The proportion of students with positive attitudes significantly differed depending on year level (P = 0.008) and income (P = 0.003), while the percentage of respondents with favorable perspectives significantly differed by age (P = 0.046) and major (P < 0.001).
Table 2.
KAP toward AI (based on general information).
| Characteristics |
Knowledge toward of Artificial intelligence |
Attitude toward of Artificial intelligence |
Perspectives toward of Artificial intelligence |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Poor |
Good |
p-value |
Negative |
Positive |
p-value |
Poor |
Good |
p-value |
|
| n (%) | n (%) | n (%) | |||||||
| Gender | 0.001* | 0.628 | 0.547 | ||||||
| Male | 172 (15.1) | 294 (25.7) | 219 (19.2) | 247 (21.6) | 206 (18.0) | 260 (22.8) | |||
| Female | 352 (30.8) | 324 (28.4) | 307 (26.9) | 369 (32.3) | 312 (27.3) | 364 (31.9) | |||
| Age | 0.430 | 0.088 | 0.046* | ||||||
| 18-21 | 293 (25.7) | 366 (32.0) | 290 (25.4) | 369 (32.3) | 271 (23.7) | 388 (34.0) | |||
| 22-25 | 249 (21.8) | 224 (19.6) | 232 (20.3) | 241 (21.1) | 241 (21.1) | 232 (20.3) | |||
| 26-29 | 2 (0.2) | 8 (0.7) | 4 (0.4) | 6 (0.5) | 6 (0.5) | 4 (0.4) | |||
| Majors | 0.003* | 0.631 | 0.001* | ||||||
| Pharmacy | 137 (12.0) | 131 (11.5) | 129 (11.3) | 139 (12.2) | 97 (8.5) | 171 (15.0) | |||
| Medicine | 387 (33.9) | 487 (42.6) | 397 (34.8) | 477 (41.8) | 421 (36.9) | 453 (39.7) | |||
| University year | 0.464 | 0.008* | 0.080 | ||||||
| First year | 85 (7.4) | 123 (10.8) | 82 (7.2) | 126 (11.0) | 97 (8.5) | 111 (9.7) | |||
| Second year | 137 (12.0) | 175 (15.3) | 141 (12.3) | 171 (15.0) | 120 (10.5) | 192 (16.8) | |||
| Third year | 81 (7.1) | 79 (6.9) | 80 (7.0) | 80 (7.0) | 67 (5.9) | 93 (8.1) | |||
| Fourth year | 110 (9.6) | 114 (10.0) | 121 (10.6) | 103 (9.0) | 109 (9.5) | 115 (10.1) | |||
| Fifth year | 59 (5.2) | 69 (6.0) | 63 (5.5) | 65 (5.7) | 67 (5.9) | 61 (5.3) | |||
| Sixth year | 52 (4.6) | 58 (5.1) | 39 (3.4) | 71 (6.2) | 58 (5.1) | 52 (4.6) | |||
| Attended any webinar/lecture/course on AIain healthcare | 0.001* | 0.312 | 0.261 | ||||||
| Yes | 21 (1.8) | 104 (9.1) | 57 (5.0) | 68 (6.0) | 52 (4.6) | 73 (6.4) | |||
| No | 503 (44.0) | 514 (45.0) | 469 (41.1) | 548 (48.0) | 466 (40.8) | 551 (48.2) | |||
| Income (US$b per month) | 0.011* | 0.003* | 0.060 | ||||||
| None | 193 (16.9) | 194 (17.0) | 193 (16.9) | 194 (17.0) | 185 (16.2) | 202 (17.7) | |||
| <60 | 119 (10.4) | 122 (10.7) | 122 (10.7) | 119 (10.4) | 103 (9.0) | 138 (12.1) | |||
| 60 -<120 | 114 (10.0) | 139 (12.2) | 95 (8.3) | 158 (13.8) | 112 (9.8) | 141 (12.3) | |||
| 120 -<180 | 55 (4.8) | 76 (6.7) | 64 (5.6) | 67 (5.9) | 63 (5.5) | 68 (6.0) | |||
| 180 -<240 | 30 (2.6) | 52 (4.6) | 27 (2.4) | 55 (4.8) | 29 (2.5) | 53 (4.6) | |||
| ≥ 240 | 13 (1.1) | 35 (3.1) | 25 (2.2) | 23 (2.0) | 26 (2.3) | 22 (1.9) | |||
Note.
AI: Artificial intelligence.
US$1 = VND23,559 (Source: Vietnamese Ministry of Finance: Exchange rate for foreign currencies in January 2023), *p-value <0.05.
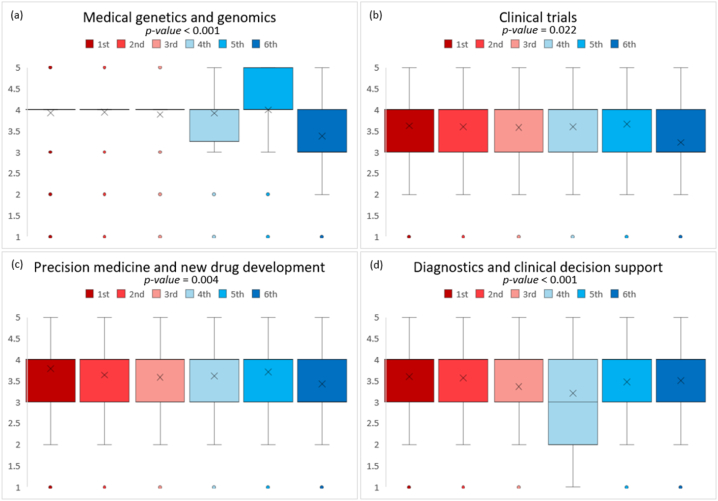
The mean scores related to the AI topics that the students wanted to integrate into their educational programs are shown in Fig. 2. Most of the participants wanted to integrate AI into radiology and digital imaging training (P = 0.283), whereas the fifth-year students wished to learn about AI in medical genetics and genomics (P < 0.001, 4.0 ± 0.8).
Fig. 2.
Desired AI topics of different year level students in the academic curriculum: (a) Medical genetics and genomics, (b) Clinical trials, (c) Precision medicine and new drug development, (d) Diagnotics and clinical decision support.
Note: 1st: first-year student; 2nd: second-year student; 3rd: third-year student; 4th: fourth-year student; 5th: five-year student; 6th: sixth-year student.
The prediction results on the sample's KAP, determined on the basis of the demographic variables, are presented in Table 3. Gender (P < 0.001), experience of webinars/lectures/courses on AI in healthcare (P < 0.001), and personal income equal to or greater than US$240 per month (P = 0.002) significantly affected knowledge of AI. The male students had 1.898 times more adequate knowledge of AI than their female counterparts, and the students who had attended webinars/lectures/courses on AI in healthcare had 4.864 times more adequate knowledge of AI than those who had no such experience. The students with incomes equal to or greater than US$240 per month had 2.928 times more adequate knowledge of AI than the students with no income. Income was the only significant factor affecting attitudes toward AI (P < 0.01). Specifically, those earning incomes of US$60 to less than US$120 and US$180 to less than US$240 had 1.659 and 2.049 times more positive attitudes than the students with no income, respectively. All the other variables had nonsignificant effects on attitudes. Major (P = 0.001) and a personal income of US$180 to less than US$240 (P = 0.018) significantly affected AI perspectives. The pharmacy students had 0.605 times more favorable perspectives regarding AI than the medical students, and those with incomes of US$180 to less than US$240 had 1.842 times more favorable impressions of the technology than the students with no income.
Table 3.
Binary logistic regression between baseline characteristics and KAP regarding AI.
| Characteristics |
Knowledge toward of Artificial intelligence |
Attitude toward of Artificial intelligence |
Perspectives toward of Artificial intelligence |
||||||
|---|---|---|---|---|---|---|---|---|---|
| p-value | ORa | 95%CIb | p-value | OR | 95%CI | p-value | OR | 95%CI | |
| Gender | |||||||||
| Female | Ref. | Ref. | Ref. | ||||||
| Male | 0.001 | 1.898 | 1.470–2.454 | 0.700 | 0.953 | 0.745–1.219 | 0.126 | 1.212 | 0.947–1.552 |
| Age | |||||||||
| 18-21 | 0.462 | Ref. | 0.365 | Ref. | 0.281 | Ref. | |||
| 22-25 | 0.652 | 0.841 | 0.395–1.787 | 0.163 | 0.599 | 0.292–1.230 | 0.136 | 0.577 | 0.280–1.189 |
| 26-29 | 0.384 | 2.258 | 0.360–14.146 | 0.372 | 0.499 | 0.109–2.294 | 0.228 | 0.393 | 0.086–1.794 |
| Majors | |||||||||
| Medicine | Ref. | Ref. | Ref. | ||||||
| Pharmacy | 0.195 | 1.220 | 0.903–1.648 | 0.740 | 1.051 | 0.784–1.408 | 0.001 | 0.605 | 0.448–0.816 |
| University year | |||||||||
| First year | 0.522 | Ref. | 0.021 | Ref. | 0.426 | Ref. | |||
| Second year | 0.262 | 0.809 | 0.559–1.171 | 0.164 | 0.774 | 0.539–1.111 | 0.042 | 1.453 | 1.013–2.084 |
| Third year | 0.087 | 0.681 | 0.438–1.057 | 0.073 | 0.676 | 0.441–1.037 | 0.460 | 1.176 | 0.766–1.805 |
| Fourth year | 0.365 | 0.682 | 0.298–1.561 | 0.804 | 0.904 | 0.410–1.997 | 0.277 | 1.554 | 0.701–3.445 |
| Fifth year | 0.532 | 0.757 | 0.317–1.811 | 0.929 | 1.038 | 0.452–2.387 | 0.502 | 1.331 | 0.578–3.068 |
| Sixth year | 0.219 | 0.569 | 0.232–1.397 | 0.142 | 1.913 | 0.805–4.543 | 0.371 | 1.480 | 0.627–3.493 |
| Attended any webinar/lecture/course on AIbin healthcare | |||||||||
| No | Ref. | Ref. | Ref. | ||||||
| Yes | 0.001 | 4.864 | 2.964–7.981 | 0.937 | 1.016 | 0.691–1.492 | 0.351 | 1.203 | 0.816–1.773 |
| Income (US$c per month) | |||||||||
| None | 0.014 | Ref. | 0.003 | Ref. | 0.195 | Ref. | |||
| <60 | 0.920 | 1.017 | 0.727–1.425 | 0.851 | 0.969 | 0.699–1.343 | 0.231 | 1.224 | 0.880–1.703 |
| 60 -<120 | 0.214 | 1.235 | 0.885–1.723 | 0.003 | 1.659 | 1.194–2.304 | 0.278 | 1.197 | 0.865–1.658 |
| 120 -<180 | 0.206 | 1.316 | 0.859–2.016 | 0.890 | 1.029 | 0.684–1.548 | 0.751 | 1.068 | 0.709–1.610 |
| 180 -<240 | 0.028 | 1.781 | 1.065–2.979 | 0.006 | 2.049 | 1.229–3.417 | 0.018 | 1.842 | 1.110–3.057 |
| ≥240 | 0.002 | 2.928 | 1.472–5.824 | 0.929 | 0.973 | 0.527–1.793 | 0.570 | 0.836 | 0.452–1.549 |
| Constant | 0.293 | 0.808 | 0.157 | 1.326 | 0.123 | 1.360 | |||
Note.
OR: Odds ratio.
95 % CI: 95 % confidence interval, bAI: Artificial intelligence.
US$1 = VND23,559 (Source: Vietnamese Ministry of Finance: Exchange rate for foreign currencies in January 2023).
The most common cause of failure of AI implementation in the medical field is the lack of financial resources (83.54 %) and not disinterest in the technology among students (20.67 %) (Fig. S1 in the Supplementary materials).
4. Discussion
4.1. Role of AI
The Vietnam Ministry of Health has issued Decision No. 4888/QD-BYT about the applications and development of smart health care during 2019–2025, which underlines the importance of the application of digital technologies, including AI, in the healthcare sector [47]. AI is expected to considerably influence the future of medicine in general. This technology is becoming more ubiquitous in modern industry and daily life, and it is being employed more frequently in healthcare. For example, it is involved in healthcare administration, predictive medicine, patient data and diagnostics, and clinical decision making [48]. AI in healthcare may assist practitioners tasked a variety of patient care and administrative responsibilities, enabling them to improve existing solutions and more quickly address problems. Disease diagnosis and treatment have been at the forefront of AI in healthcare for the past 50 years. In many aspects of this ecosystem, AI may increase accuracy, precision, and results while saving time. It may also help with laboratory diagnosis, clinical diagnosis, imaging analysis, research investigations, financial administration, documentation, workflow simplification, and other healthcare-related tasks. Some of the AI approaches used in the healthcare industry include machine learning (ML), deep learning, and natural language processing [49].
4.2. Principal findings
4.2.1. Existing understanding of AI
The participants' KAP was the focus of this research. There were 1142 participants (undergraduate medical and pharmacy students), of which 59.2 % were females. In the sample, there were more males (294 vs. 172) with better knowledge of AI compared with the females (324 vs. 352) (P < 0.001). These results correspond with a study in Germany conducted [50]. In the current study, the students acquired application information on AI mostly from the media/social media and movies (56.4 %). In US and Lebanese research involving 173 medical students and clinicians and 206 students, this percentage reached 72 % and 81.1 %, respectively [43,51]. In general, the participants’ knowledge of AI in medicine was low because most of them had never participated in webinars/lectures/courses (89.1 %, odds ratio [OR] = 4.864, P < 0.001). These results are consistent with those of Kansal et al. [44], who found that 83.5 % of medical students have never participated in such educational offerings and that they have limited knowledge of the applications and limitations of AI (79.6 % and 82.8 %, respectively).
4.2.2. Attitudes toward AI
4.2.2.1. General attitudes
The results showed that the majority of the students who had positive attitudes toward AI believe that such innovation will render medicine more interesting, reduce workload, and improve and revolutionize the practice of undergraduate medical and pharmacy students. Similar findings were reported in other studies involving medical students [44,46,[52], [53], [54], [55], [56]]. In the present work, the results varied according to income (P = 0.003) but not according to gender. The income difference was regarded as indicative of the participants having had the opportunity to directly encounter AI technology. The absence of a difference between gender validates the idea that both males and females are interested in medical AI technology.
4.2.2.2. Impact of AI on doctors and pharmacists
Contrary to anecdotes about students being fearful of the advent of AI, the findings indicated that more than 79 % of the participants believed that in the near future, there will still be a need for doctors and pharmacists. However, nearly three-quarters of them also argued that their medical education was not sufficiently preparing them for work with AI tools (74 %) and that the Vietnamese healthcare system was not currently well equipped to deal with the challenges related to the technology (72 %). Similarly, Mehta et al. reported that 79 % of respondents disagreed that their medical education effectively equips them to work alongside AI technologies, and 63 % disagreed that the Canadian healthcare system is now well positioned to deal with AI-related concerns [42].
4.2.2.3. New challenges raised
According to the findings of Mehta et al. [42], the significant majority of students believe that AI will be confronted with ethical, societal, and equitability concerns (98 %, 95 %, and 78 %, respectively). The same belief was expressed by our participants (74 %, 59 %, and 62 %, respectively). They are concerned about who will be responsible when medical events occur and that the rapid growth of AI technology will increase unemployment [57]; unstable social order; labor strikes; rallies for the right to work and live; adverse social phenomena, such as theft, gambling, drug addiction, and prostitution. From these, societal unrest and even political instability are possible. Finally, because of the high costs incurred from investing in AI technology, medical services will become increasingly expensive, affecting access to healthcare services.
4.2.2.4. On the need for education
Among the participants, 78 % felt that understanding AI is advantageous for doctors and pharmacists, consistent with previous research [45,46,50,53,55,56]. However, the students expressed the desire to learn about AI comfortably and effectively as an elective, rather than a compulsory, subject (65 % and 37 %, respectively). The AI-related topics of interest to most of the students in all year levels included radiology and digital imaging, disease prediction models, and individualized health data/device monitoring, which were also believed to be the issues that most strongly affect the medical field today. Students of different year levels varied in terms of their interest in medical genetics and genomics [Fig. 2(a)], clinical trials [Fig. 2(b)], precision medicine and new drug development [Fig. 2(c)], and diagnostics and clinical decision support [Fig. 2(d)]. This finding is attributed to the amount of theoretical knowledge acquired by the students over the years. More specifically, diagnostics and clinical decision support were least favored by the respondents because these issues partly influence the political opinions and self-determination rights of doctors and pharmacists. Of the sample, 93.7 % were willing to take AI courses in one day, and among these students, 26.2 % were willing to pay for such classes.
4.3. Perspectives regarding AI capabilities
4.3.1. Individual health
AI is important in the customization process because it enables humans to collect data rapidly and correctly with considerable detail. These developments, in turn, translate to improved treatment efficiency and time conservation. Some aspects of patient care piqued the students’ interest. Specifically, they had mixed feelings about whether AI can produce individualized treatment plans for patients, with only 44 % believing this is a likely occurrence and 41 % convinced that it can formulate personalized drug prescriptions. According to Canadian research, 29 % of participants believe AI can tailor treatment plans for patients, and 53 % believe that it can customize medications for patients [42].
4.3.2. Health systems and population health
After the initial outbreak of COVID-19 period, students expressed positive views about the effectiveness of AI in public care (78 % and 71 %) such as facilitating public care delivery, communication and collection of vaccination information of the people. In terms of mental aspects, however, the participants stated that it would be difficult for AI to perform as well as humans with respect to behaviors such as empathizing with patients (75 %) and providing psychological counseling (59 %). Similar findings were found among respondents in a provincial survey in Canada [42]. The current students' ideas on AI capabilities were consistent with their views on how AI will affect the medical professional environment, with the respondents generally believing that some disciplines will be more strongly affected than others. These results varied according to major (P < 0.001, OR = 0.605) but not according to year level. The findings regarding the variations between students of various disciplines show that medical students have a higher level of technological literacy than pharmacy students. The lack of a gap between year levels reinforced the notion that modern medical education does not encompass knowledge or comprehension of AI. The students’ qualitative replies supported the belief that AI will not replace doctors in the “art of caring” [58].
4.4. Barriers to implementing AI in healthcare
The major causes of failure in AI implementation in Vietnam included the lack of adequate knowledge and awareness of the technology, disinterest in the field, poor training, the absence of a dedicated curriculum, low financial resources, and the lack of technological advancements. Given that the country is an agricultural and developing nation, most of the participants believed that the barriers to implementing AI in healthcare stem from the lack of financial resources (83.54 %) and appropriate training (81.00 %). Conversely, a study conducted on students and physicians in Pakistan [45] revealed that the strongest obstacle to AI integration in healthcare is lack of understanding (63 %).
4.5. Implications
AI in medicine is a fascinating topic that has the potential to substantially impact future generations of professionals [59]. The students were aware that AI is a prominent issue in the medical field, and they obtained much of their knowledge through online browsers or social media. Most of them did not regard AI as a danger or were unconcerned about job displacement; rather, they saw AI as a “collaborator” rather than “competition” [56]. Nevertheless, they still expressed a desire to learn cutting-edge AI and stay up to date on the latest advances possibly because of the belief that AI-savvy doctors may supplant those who do not employ this technology in this competitive profession [60].
Medical and pharmaceutical schools are falling behind in terms of educating their students on the fundamental ideas and uses of AI and providing technical assistance for the work of basic ML testing. Communication, empathy, and a deep and caring relationship with a patient have long been the foundations of both medicine and pharmacy. Avoiding the loss of human touch in the profession necessitates preserving these fundamentals as AI is integrated into clinical practice. Healthcare students have more stringent schedules and are more susceptible to stress than their peers pursuing other degrees [61]. Some components of conventional curricula may have to be transitioned out to make space for AI and avoid excessive responsibilities. Integrating AI-based content into UME will require time and flexibility because technology evolves at the same rate as biological knowledge. A critical strategy, therefore, is to equip educators in such a way that enables them to teach various components of AI technology. Furthermore, more research should be conducted to determine what adjustments are conceivable. Relevant insights would also be derived from studies that concentrate on the perspectives of staff, academic institutions, and accrediting bodies regarding the value and practicality of incorporating AI into medical curricula. A recently established scale (i.e., MAIRS-MS) for assessing medical students’ preparedness for AI in medicine might be a good starting point [62].
4.6. Strengths and weaknesses
Previous studies that looked into medical students’ perspectives on AI focused on certain specializations [32,50,52,56,63,64]. Our research is distinct from these studies in that the investigation centered on AI in both medicine and pharmacy as opposed to sub-specializations such as radiology or surgery. Our research provided critical insights into the incorporation of AI courses in the curricula of underdeveloped nations, such as Vietnam. This is an important yet unexplored matter among medical students, and clarifying it contributes to a better understanding of the situation and the identification of remedies. To the best of our knowledge, this research is the first to highlight KAP concerning AI in medical education in a Southeast Asian country.
Notwithstanding the above-mentioned achievements, our study is also encumbered with limitations. First, the findings may not be representative of the overall student population in the nation. Second, self-selection bias may have occurred, as only students and teachers with interest in AI and advanced medical technologies were involved in it. Finally, the questionnaire was distributed online rather than in person, which may have contributed to selection bias and altered the results. Because this is an online study, the sample population is not typical of PNTU's undergraduate students.
5. Conclusion
This study investigated medical and pharmaceutical students' KAP about AI and the impediments to AI application in healthcare in Vietnam. The majority of the participants expressed positive attitudes and views and were excited to learn more about the fundamentals and applications of AI in medicine. With the growth of AI in every aspect of life, including healthcare, incorporating AI-related courses into medical school curricula has become a critical requirement. Delays in teaching AI to medical students might leave them unprepared to deal with future risks and obstacles encountered at personal and professional levels. Students’ eagerness to learn about AI might be interpreted as a positive indicator on which to capitalize. On the basis of our research and earlier surveys conducted in other countries, we emphasize the critical need to include AI-related issues in medical school curricula.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
CRediT authorship contribution statement
Nguyen Truong Minh: Writing – review & editing, Writing – original draft, Validation, Software, Methodology, Formal analysis, Data curation. Trung Quang Vo: Writing – review & editing, Visualization, Supervision, Project administration, Conceptualization. Hien Thi Bich Tran: Writing – review & editing, Visualization, Supervision, Conceptualization. Hiep Thanh Nguyen: Visualization, Supervision, Conceptualization. Van Nu Hanh Pham: Visualization, Supervision, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
TRUNG QUANG VO reports administrative support, article publishing charges, equipment, drugs, or supplies, statistical analysis, travel, and writing assistance were provided by Pham Ngoc Thach University of Medicine. TRUNG QUANG VO reports a relationship with Pham Ngoc Thach University of Medicine that includes: employment. No conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e22653.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Sapci A.H., Sapci H.A. Artificial intelligence education and tools for medical and health informatics students: systematic review. JMIR Med. Educ. 2020;6(1) doi: 10.2196/19285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.LeCun Y., Bengio Y., Hinton G. Deep learning, Nature. 2015;521(7553):436–444. doi: 10.1038/nature14539. [DOI] [PubMed] [Google Scholar]
- 3.Holzinger, et al. Causability and explainability of artificial intelligence in medicine. Wiley Interdiscip. Rev. Data. Min. Knowl. Discov. 2019;9(4):e1312. doi: 10.1002/widm.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee J., et al. Artificial intelligence in undergraduate medical education: a scoping review. Acad. Med. 2021;96(11S):S62–S70. doi: 10.1097/ACM.0000000000004291. [DOI] [PubMed] [Google Scholar]
- 5.Yamada K., Mori S. The day when computers read between lines. Jpn. J. Radiol. 2019;37(5):351–353. doi: 10.1007/s11604-019-00833-3. [DOI] [PubMed] [Google Scholar]
- 6.Abid S., et al. Artificial intelligence: medical students' attitude in district Peshawar Pakistan. Pak. J. Public Health. 2019;9(1):19–21. [Google Scholar]
- 7.Waymel Q., et al. Impact of the rise of artificial intelligence in radiology: what do radiologists think? Diagn. Interv. Imaging. 2019;100(6):327–336. doi: 10.1016/j.diii.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 8.Ooi S.K.G., et al. Attitudes toward artificial intelligence in radiology with learner needs assessment within radiology residency programmes: a national multi-programme survey. Singap. Med. J. 2021;62(3):126. doi: 10.11622/smedj.2019141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Topol E.J. High-performance medicine: the convergence of human and artificial intelligence. Nat. Med. 2019;25(1):44–56. doi: 10.1038/s41591-018-0300-7. [DOI] [PubMed] [Google Scholar]
- 10.Kansal R., et al. Differences in knowledge and perspectives on the usage of artificial intelligence among doctors and medical students of a developing country: a cross-sectional study. Cureus. 2022;14(1) doi: 10.7759/cureus.21434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hainc N., et al. The bright, artificial intelligence-augmented future of neuroimaging reading. Front. Neurol. 2017;8:489. doi: 10.3389/fneur.2017.00489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang D., et al. 2016. Deep Learning for Identifying Metastatic Breast Cancer. arXiv Preprint arXiv:05718. [Google Scholar]
- 13.Esteva A., et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115–118. doi: 10.1038/nature21056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siegersma K., et al. Artificial intelligence in cardiovascular imaging: state of the art and implications for the imaging cardiologist. Neth. Heart J. 2019;27(9):403–413. doi: 10.1007/s12471-019-01311-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bedi G., et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1(1):1–7. doi: 10.1038/npjschz.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jin H.-Y., Zhang M., Hu B. Techniques to integrate artificial intelligence systems with medical information in gastroenterology. Artif. Intell. Gastrointest. Endosc. 2020;1(1):19–27. [Google Scholar]
- 17.Kassahun Y., et al. Surgical robotics beyond enhanced dexterity instrumentation: a survey of machine learning techniques and their role in intelligent and autonomous surgical actions. Int. J. Comput. Assist. Radiol. Surg. 2016;11(4):553–568. doi: 10.1007/s11548-015-1305-z. [DOI] [PubMed] [Google Scholar]
- 18.Jiang F., et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc. Neurol. 2017;2(4) doi: 10.1136/svn-2017-000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kolachalama V.B., Garg P.S. Machine learning and medical education. NPJ Digit. Med. 2018;1(1):54. doi: 10.1038/s41746-018-0061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meskó B., Görög M. A short guide for medical professionals in the era of artificial intelligence. NPJ Digit. Med. 2018;3(1):126. doi: 10.1038/s41746-020-00333-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davenport T., Kalakota R. The potential for artificial intelligence in healthcare. Future Hosp. J. 2019;6(2):94. doi: 10.7861/futurehosp.6-2-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmes J., Sacchi L., Bellazzi R. Artificial intelligence in medicine. Ann. R. Coll. Surg. Engl. 2004;86:334–338. doi: 10.1308/147870804290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rajkomar A., Dean J., Kohane I. Machine learning in medicine. N. Engl. J. Med. 2019;380(14):1347–1358. doi: 10.1056/NEJMra1814259. [DOI] [PubMed] [Google Scholar]
- 24.Hashimoto D.A., et al. Artificial intelligence in surgery: promises and perils. Ann. Surg. 2018;268(1):70–76. doi: 10.1097/SLA.0000000000002693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Char D.S., Shah N.H., Magnus D. Implementing machine learning in health care-addressing ethical challenges. N. Engl. J. Med. 2018;378(11):981. doi: 10.1056/NEJMp1714229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wartman S.A. The empirical challenge of 21st-century medical education. Acad. Med. 2019;94(10):1412–1415. doi: 10.1097/ACM.0000000000002866. [DOI] [PubMed] [Google Scholar]
- 27.Wartman S.A., Combs C.D. Reimagining medical education in the age of AI. AMA J. Ethics. 2019;21(2):146–152. doi: 10.1001/amajethics.2019.146. [DOI] [PubMed] [Google Scholar]
- 28.Wartman S.A., Combs C.D. Medical education must move from the information age to the age of artificial intelligence. Acad. Med. 2018;93(8):1107–1109. doi: 10.1097/ACM.0000000000002044. [DOI] [PubMed] [Google Scholar]
- 29.Gong B., et al. Influence of artificial intelligence on Canadian medical students' preference for radiology specialty: a national survey study. Acad. Radiol. 2019;26(4):566–577. doi: 10.1016/j.acra.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 30.Sit C., et al. Attitudes and perceptions of UK medical students towards artificial intelligence and radiology: a multicentre survey. Insights Imaging. 2020;11(1):1–6. doi: 10.1186/s13244-019-0830-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paranjape K., et al. Introducing artificial intelligence training in medical education. JMIR Med. Educ. 2019;5(2) doi: 10.2196/16048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kelly C.J., et al. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 2019;17(1):195. doi: 10.1186/s12916-019-1426-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wood E.A., et al. Are we ready to integrate artificial intelligence literacy into medical school curriculum: students and faculty survey. J. Med. Educ. Curric. Dev. 2021;8 doi: 10.1177/23821205211024078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pinto Dos Santos D., et al. Medical students' attitude towards artificial intelligence: a multicentre survey. Eur. Radiol. 2019;29(4):1640–1646. doi: 10.1007/s00330-018-5601-1. [DOI] [PubMed] [Google Scholar]
- 35.McArthur D., Lewis M., Bishary M. The roles of artificial intelligence in education: current progress and future prospects. J. Educ. Technol. 2005;1(4):42–80. [Google Scholar]
- 36.Popenici S.A., Kerr S. Exploring the impact of artificial intelligence on teaching and learning in higher education. Research Res. Pract. Technol. Enhanc. Learn. 2017;12(1):1–13. doi: 10.1186/s41039-017-0062-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bayne S. Teacherbot: interventions in automated teaching. Teach. High. Educ. 2015;20(4):455–467. [Google Scholar]
- 38.dit Dariel O.J.P., et al. Developing the serious games potential in nursing education. Nurse Educ. Today. 2013;33(12):1569–1575. doi: 10.1016/j.nedt.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 39.Nye B.D. Intelligent tutoring systems by and for the developing world: a review of trends and approaches for educational technology in a global context. Int. J. Artif. Intell. Educ. 2015;25(2):177–203. [Google Scholar]
- 40.Downes M.J., et al. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS) BMJ Open. 2016;6(12) doi: 10.1136/bmjopen-2016-011458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krejcie R.V., Morgan D.W. Determining sample size for research activities. Educ. Psychol. Meas. 1970;30(3):607–610. [Google Scholar]
- 42.Mehta N. medRxiv; 2021. Knowledge of and Attitudes on Artificial Intelligence in Healthcare: a Provincial Survey Study of Medical Students. [Google Scholar]
- 43.Wood E.A., Ange B.L., Miller D.D. Are we ready to integrate artificial intelligence literacy into medical school curriculum: students and faculty survey. J. Med. Educ. Curric. Dev. 2021;8 doi: 10.1177/23821205211024078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kansal R., et al. Differences in knowledge and perspectives on the usage of artificial intelligence among doctors and medical students of a developing country: a cross-sectional study. Cureus. 2022;14(1) doi: 10.7759/cureus.21434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ahmed Z., et al. Knowledge, attitude, and practice of artificial intelligence among doctors and medical students in Pakistan: a cross-sectional online survey. Ann. Med. Surg. 2022;76 doi: 10.1016/j.amsu.2022.103493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swed S., et al. Knowledge, attitude, and practice of artificial intelligence among doctors and medical students in Syria: a cross-sectional online survey. Front. Artif. Intell. 2022;5 doi: 10.3389/frai.2022.1011524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.The Ministry of Health, accessed date: 04/01/2023, Decision: Introducing the Scheme for Application and Development of Smart Healthcare Information Technology for the 2019 - 2025 Period, retrieved from https://thuvienphapluat.vn/van-ban/EN/Cong-nghe-thong-tin/Decision-4888-QD-BYT-2019-the-scheme-for-application-of-smart-healthcare-information-technology/428330/tieng-anh.aspx.
- 48.Secinaro S., et al. The role of artificial intelligence in healthcare: a structured literature review. BMC Med. Inf. Decis. Making. 2021;21(1):125. doi: 10.1186/s12911-021-01488-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alugubelli R. Exploratory study of artificial intelligence in healthcare. Int. J. Innov. Eng. Res. Technol. 2016;3(1):1–10. [Google Scholar]
- 50.Pinto Dos Santos D., et al. Medical students' attitude towards artificial intelligence: a multicentre survey. Eur. Radiol. 2019;29(4):1640–1646. doi: 10.1007/s00330-018-5601-1. [DOI] [PubMed] [Google Scholar]
- 51.Doumat G., et al. Knowledge and attitudes of medical students in Lebanon toward artificial intelligence: a national survey study. Front. Artif. Intell. 2022;5 doi: 10.3389/frai.2022.1015418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Park C.J., Paul H.Y., Siegel E.L. Medical student perspectives on the impact of artificial intelligence on the practice of medicine. Curr. Probl. Diagn. Radiol. 2021;50(5):614–619. doi: 10.1067/j.cpradiol.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 53.Teng M., et al. Health care students' perspectives on artificial intelligence: countrywide survey in Canada. JMIR Med. Educ. 2022;8(1) doi: 10.2196/33390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jha N., et al. Undergraduate medical students' and interns' knowledge and perception of artificial intelligence in medicine. Adv. Med. Educ. Pract. 2022;13:927. doi: 10.2147/AMEP.S368519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu D.S., et al. Perceptions of US medical students on artificial intelligence in medicine: mixed methods survey study. JMIR Med. Educ. 2022;8(4) doi: 10.2196/38325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bisdas S., et al. Artificial intelligence in medicine: a multinational multi-center survey on the medical and dental students' perception. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.795284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Civaner M.M., et al. Artificial intelligence in medical education: a cross-sectional needs assessment. BMC Med. Educ. 2022;22(1):1–9. doi: 10.1186/s12909-022-03852-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnston S.C. Anticipating and training the physician of the future: the importance of caring in an age of artificial intelligence. Acad. Med. 2018;93(8):1105–1106. doi: 10.1097/ACM.0000000000002175. [DOI] [PubMed] [Google Scholar]
- 59.El-Azhary R.A. The inevitability of change. Clin. Dermatol. 2019;37(1):4–11. doi: 10.1016/j.clindermatol.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 60.Brady A.P., Neri E. Artificial intelligence in radiology—ethical considerations. Diagnostics. 2020;10(4):231. doi: 10.3390/diagnostics10040231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kiziela A., et al. Distress and resilience associated with workload of medical students. J. Ment. Health. 2019;28(3):319–323. doi: 10.1080/09638237.2018.1521922. [DOI] [PubMed] [Google Scholar]
- 62.Karaca O., Çalışkan S.A., Demir K. Medical artificial intelligence readiness scale for medical students (MAIRS-MS)-development, validity and reliability study. BMC Med. Educ. 2021;21:1–9. doi: 10.1186/s12909-021-02546-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.van Hoek J., et al. A survey on the future of radiology among radiologists, medical students and surgeons: students and surgeons tend to be more skeptical about artificial intelligence and radiologists may fear that other disciplines take over. Eur. J. Radiol. 2019;121 doi: 10.1016/j.ejrad.2019.108742. [DOI] [PubMed] [Google Scholar]
- 64.Brandes G.I.G., et al. Impact of artificial intelligence on the choice of radiology as a specialty by medical students from the city of São Paulo. Radiol. Bras. 2020;53:167–170. doi: 10.1590/0100-3984.2019.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.