Abstract
Innominate artery injury is an uncommon consequence of blunt trauma to the neck due to its protected position behind the thorax. A 38-year-old male presented as a trauma with a right-sided pseudoaneurysm emanating from the distal innominate artery after falling from a three-story building. On imaging, he also had a bovine arch. He underwent hybrid repair with covered stent placement from the common carotid into the innominate artery, carotid-subclavian bypass, and plugging of the subclavian artery. The patient recovered with no cerebral insult, neurological deficits, or rupture. Post-traumatic innominate artery pseudoaneurysms can successfully be repaired via a hybrid surgical approach.
Keywords: Amplatzer plug, Blunt traumatic injury, Hybrid surgery, Innominate artery, Pseudoaneurysm, Stent
Innominate artery injury makes up 8% to 18%1 of traumatic arch injuries, with 85% of lesions in the proximal portion.2,3 Additionally, 16% of the United States population have a type II bovine arch with a left common carotid origin from the innominate artery.4 No consensus exists for traumatic innominate artery pseudoaneurysm repair; the approach varies on injury location. End-to-side grafting from ascending aorta to distal innominate is used for injuries close to the isthmus, and stent grafts are used for mid-innominate lesions.2 Distal lesions require complex reconstructions.2 Endovascular innominate repair carries a mortality of 9% vs open at 19%.5 Thus, risks of complex endovascular approaches at the bifurcation must be weighed against increased mortality in open repair.
We describe hybrid repair of a traumatic distal pseudoaneurysm of the innominate artery in a type II bovine arch. Publication consent was obtained, and identifying information has been omitted.
Case
A 38-year-old male fell from a three-story building. He presented as a trauma to an outside hospital and was moving all extremities. His Glasgow Coma Scale (GCS) was 8 before intubation. No intracranial injury was reported. Outside computerized tomography (CT) scan reported a grade V liver laceration, right brachiocephalic pseudoaneurysm with dissection into the common carotid, mandible fracture, and C7 transverse-process fracture. He was hypertensive to 233/125 and started on an esmolol drip. He had no pertinent medical or surgical history.
He was transferred to our facility with a GCS of 3T, and elevated white blood count (20.9 × 109), aspartate transaminase (307 IU/L), alanine transaminase (333 IU/L), prothrombin time (17 seconds), international normalized ratio (1.3), creatinine (1.3 mg/dL), and calcium (7.9 mg/dL). Physical exam showed palpable radial pulses, strong left carotid pulse, and diminished right carotid pulse. Blood pressure was 87/67 mmHg, and 1 unit of packed red blood cells was transfused. Repeat CT angiogram (CTA) showed pseudoaneurysmal dilatation of the distal innominate artery at the right common carotid and subclavian artery bifurcation. A small dissection flap extended into the common carotid with no evidence of thrombosis or rupture (Fig 1).
Fig 1.
Computed tomography angiography (CTA) showing pseudoaneurysm (yellow arrow) of the distal innominate artery at the bifurcation of the right common carotid and subclavian artery in axial (A), coronal (B), and sagittal (C) views. A small dissection flap extends into the common carotid artery. There is no evidence of thrombosis or rupture. The pseudoaneurysm measures 2.5 cm at its widest point.
He was taken to a hybrid operating room 6 hours after transfer for a three-part hybrid repair. An 8-cm incision above the clavicle was made, and the common carotid artery was exposed. Five thousand units of heparin were given due to concern for the liver laceration, which was reclassified to grade II on repeat CTA, and the maximum activated clotting time during the case was 237 seconds. A 6-0 Prolene purse string was placed 9 cm distal to the innominate bifurcation on the common carotid, and retrograde access was performed. Angiogram demonstrated dynamic compression of the carotid artery by a distal brachiocephalic pseudoaneurysm (Fig 2, A). We upsized to an 8 × 11 sheath through which an 8L × 59 mm VBX (Gore) was deployed across the lesion from the carotid into the brachiocephalic trunk. Due to the arterial size difference, we post-dilated the VBX proximally to 10 mm (Gore). However, the graft migrated distally during balloon placement (Fig 2, B). We then placed a 10 × 39 mm VBX stent graft and post-dilated to 12 mm with good coverage of the lesion and exclusion of the right subclavian (Fig 2, C). We next performed a carotid-subclavian bypass by extending our initial exposure. A 6-mm Dacron graft (Invista) was anastomosed to the subclavian artery. The graft was tunneled retro-jugularly and anastomosed to the common carotid 6 cm from the subclavian artery-common carotid artery bifurcation, just proximal to the access site. Finally, a 6-0 Prolene purse string was placed in the subclavian artery distal to the graft for retrograde access. Angiogram showed filling of the vertebral, right internal mammary artery, and subclavian arteries along with the pseudoaneurysm (Fig 3, A). An Amplatzer-2 12 × 9 mm plug (Abbott) was placed distal to the injury and proximal to the right internal mammary artery and vertebral artery. Angiogram showed excellent exclusion of the pseudoaneurysm with the plug (Fig 3, B). Protamine was given, and a Jackson-Pratt drain was placed over the subclavian fat pad. Total procedure time was 230 minutes with estimated blood loss of 200 mL. The patient was transferred to the surgical intensive care unit (ICU).
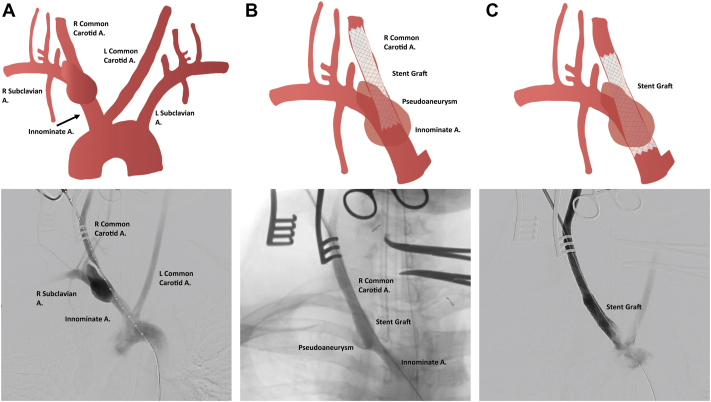
Fig 2.
Illustrations and angiograms of the first stage of the procedure. A, Initial angiogram shows distal innominate artery pseudoaneurysm with filling of both the common carotid artery and right subclavian artery. The left common carotid artery can be seen taking off the proximal portion of the innominate, classifying this patient as having a bovine arch. B, After placement of an 8L × 59 mm VBX across the lesion from carotid to the normal brachiocephalic trunk and post dilation to 10 mm, the stent appeared to have migrated distally. The pseudoaneurysm can be seen filling. C, After extension with a 10 × 39 mm VBX and post-dilation to 12 mm, angiogram shows suitable coverage of the lesion with no filling of the pseudoaneurysm and exclusion of the right subclavian artery from the brachiocephalic. A, Artery.
Fig 3.
Illustrations and angiograms of the third stage of the procedure. A, Retrograde angiogram from the right subclavian artery shows filling of the vertebral, right internal mammary artery (RIMA), and carotid-subclavian bypass graft with contrast seen in the pseudoaneurysm. B, After placement of an Amplatzer-2 12 × 9 mm plug distal to the injury and proximal to the RIMA and vertebral artery angiogram shows filling of the vertebral, RIMA, and carotid-subclavian bypass graft with exclusion of the pseudoaneurysm. A, Artery.
He did well postoperatively. On postoperative day 1, he had an intact neuro exam and motor function when sedation was paused. CTA and ultrasound obtained in the postoperative period showed no evidence of new dissection, and both stent and bypass were widely patent. On postoperative day 6, Plastic and Reconstructive Surgery performed closed treatment of the mandibular fracture with interdental fixation. He eventually underwent ICU-to-ICU transfer to an outside hospital and was discharged home 3 weeks later on aspirin 81 mg and prophylactic enoxaparin 30 mg twice daily. He was seen by vascular surgery 2 months postoperatively and was fully neurologically intact with palpable radial pulses bilaterally.
Discussion
Innominate artery pseudoaneurysms are a rare consequence of blunt trauma. No consensus exists for their repair. Approaches depend on injury location along the artery and patient anatomy. We report a unique case of distal innominate artery pseudoaneurysm in a bovine arch that was excluded via hybrid repair.
Several special considerations arose in this case. The liver laceration was initially classified as a grade V, and due to concerns about bleeding,6 we were cautious with heparin administration intraoperatively. Therefore, we did not clamp the carotid during stent graft deployment. We also had umbilical tape and a Rumel tourniquet distal to the sheath to protect the brain. We back-bled the sheath to evacuate any debris prior to opening the Rumel. The carotid was only clamped during the anastomoses of the carotid-subclavian bypass. Second, we decided that revascularizing the right subclavian artery in this healthy patient was paramount as he was young and the case was urgent rather than emergent,7,8 so we also plugged the proximal subclavian as it was partially filling the pseudoaneurysm. Further, any delayed carotid-subclavian would be more complicated by a redo exposure, so we decided to proceed with the bypass at the same time. Finally, the patient’s bovine arch made manipulation of the proximal innominate artery less favorable (ie, crossing the arch,9 disrupting plaque from disordered flow10,11). Thus, we employed retrograde carotid artery access to avoid the challenges of navigating the arch.
Only two cases discuss repair of distal innominate artery injuries. Cai et al reported a pseudoaneurysm with rupture at the innominate bifurcation. Through right femoral and brachial artery access, two “kissing” grafts were placed from the innominate into right carotid and subclavian arteries.12 This avoids open surgery risks but can present with gutter leak if not sized appropriately. Szalay et al reported an innominate-axillary artery bypass with ligation of the right common carotid.13 However, this required a sternotomy. Additionally, Regina et al reported a non-traumatic distal innominate repair in a patient with Takayasu’s arteritis. She received a carotid-subclavian bypass with covered stent graft from the innominate into the common carotid artery. However, completion angiogram showed exclusion of the aneurysm and plugging of the subclavian artery was not needed.14 There are multiple approaches for distal innominate artery repair. Thus, patient anatomy, comorbidities, and presentation, along with operator preference drive decision-making.
Conclusion
We present a patient with traumatic distal innominate artery pseudoaneurysm in a bovine arch treated via covered stent graft from the common carotid artery, carotid-subclavian bypass, and subclavian artery plugging. Hybrid repair is a feasible approach for blunt vascular injuries in the neck.
From the Vascular and Endovascular Surgery Society
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Barbero C., Ricci D., Boffini M., Rinaldi M. Traumatic heart and great vessels injuries. J Thorac Dis. 2019;11(Suppl 2):S192–S195. doi: 10.21037/jtd.2018.10.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Connor J.V., Byrne C., Scalea T.M., Griffith B.P., Neschis D.G. Vascular injuries after blunt chest trauma: diagnosis and management. Scand J Trauma Resusc Emerg Med. 2009;17:42. doi: 10.1186/1757-7241-17-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jia W., Liu J.-L., Li J.-Y., et al. Treatment strategy for traumatic innominate arterial injury. Chin J Traumatol. 2020;23:10–14. doi: 10.1016/j.cjtee.2019.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moorehead P.A., Kim A.H., Miller C.P., Kashyap T.V., Kendrick D.E., Kashyap V.S. Prevalence of bovine aortic arch configuration in adult patients with and without thoracic aortic pathology. Ann Vasc Surg. 2016;30:132–137. doi: 10.1016/j.avsg.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Bishop M.A., Akbani M.J. StatPearls [Internet] StatPearls Publishing; 2022. Innominate artery injury. [Google Scholar]
- 6.Rostas J.W., Manley J., Gonzalez R.P., et al. The safety of low molecular-weight heparin after blunt liver and spleen injuries. Am J Surg. 2015;210:31–34. doi: 10.1016/j.amjsurg.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 7.Murphy E.H., Dimaio J.M., Dean W., Jessen M.E., Arko F.R. Endovascular repair of acute traumatic thoracic aortic transection with laser-assisted in-situ fenestration of a stent-graft covering the left subclavian artery. J Endovasc Ther. 2009;16:457–463. doi: 10.1583/09-2746.1. [DOI] [PubMed] [Google Scholar]
- 8.van der Weijde E., Saouti N., Vos J.A., Tromp S.C., Heijmen R.H. Surgical left subclavian artery revascularization for thoracic aortic stent grafting: a single-centre experience in 101 patients. Interact Cardiovasc Thorac Surg. 2018;27:284–289. doi: 10.1093/icvts/ivy059. [DOI] [PubMed] [Google Scholar]
- 9.Burzotta F., Nerla R., Pirozzolo G., et al. Clinical and procedural impact of aortic arch anatomic variants in carotid stenting procedures. Catheter Cardiovasc Interv. 2015;86:480–489. doi: 10.1002/ccd.25947. [DOI] [PubMed] [Google Scholar]
- 10.Faggioli G.L., Ferri M., Freyrie A., et al. Aortic arch anomalies are associated with increased risk of neurological events in carotid stent procedures. Eur J Vasc Endovasc Surg. 2007;33:436–441. doi: 10.1016/j.ejvs.2006.11.026. [DOI] [PubMed] [Google Scholar]
- 11.Faggioli G., Ferri M., Rapezzi C., Tonon C., Manzoli L., Stella A. Atherosclerotic aortic lesions increase the risk of cerebral embolism during carotid stenting in patients with complex aortic arch anatomy. J Vasc Surg. 2009;49:80–85. doi: 10.1016/j.jvs.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 12.Li X., Shu C., Li Q.M., Fang K., Li M., Cai W. Innominate artery bifurcation pseudoaneurysm repair by “kissing stent-grafts technique”: a case report. J Med Case Rep. 2018;12:352. doi: 10.1186/s13256-018-1840-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howe K.L., Guirgis M., Woodman G., et al. Blunt innominate artery trauma requiring repair and carotid ligation. Trauma Case Rep. 2017;12:24–27. doi: 10.1016/j.tcr.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angiletta D., Marinazzo D., Guido G., Fullone M., Pulli R., Regina G. Eight-year follow-up of endovascular repair of a brachiocephalic trunk aneurysm due to Takayasu. J Vasc Surg. 2012;56:504–507. doi: 10.1016/j.jvs.2012.02.031. [DOI] [PubMed] [Google Scholar]