Abstract
We present a case of medication-induced priapism that was refractory to conventional urologic methods and required treatment with a caverno-saphenous bypass. The patient had been misusing an injectable erectile dysfunction medication consisting of alprostadil, papaverine, and phentolamine (Trimix), resulting in multiple episodes of priapism. His initial episodes of priapism were successfully treated with the traditional urologic algorithm, including phenylephrine, aspiration, and distal shunting. However, due to his continued medication misuse, these became ineffective, requiring proximal shunt surgery. Priapism requiring an extra-anatomic bypass is exceedingly rare. Following our proximal shunt surgery, he maintained partial sexual function, and his bypass remained patent.
Keywords: Recurrent priapism, Caverno-saphenous shunt
Priapism is a rare condition, affecting 1.5 per 100,000 men annually in the United States, with 25% of cases induced by medication. Priapism begins with smooth muscle relaxation of the cavernosal tissue, ultimately leading to decreased venous outflow as the peripheral emissary veins occlude. The two major types of priapism are ischemic and nonischemic. The former type, also known as low-flow, anoxic, or veno-occlusive priapism, can lead to a compartment syndrome with tissue hypoxia and structural damage of erectile tissue. The duration of ischemia has been found to be associated with subsequent erectile dysfunction, with an incidence as high as 90% in ischemic priapism lasting >24 hours.1
The American Urological Association management algorithm begins with the injection of phenylephrine, a sympathomimetic drug that combats normal erection physiology, in which cavernous smooth muscle relaxation allows for filling of the corpora cavernosal sinuses and causes venous outflow obstruction. Phenylephrine injection and aspiration with irrigation are successful in ≤81% of cases of priapism.2 Patients with ischemic priapism that does not respond to repeated medical therapy are referred for intrapenile shunts, including T-shunting, the Barry shunt (deep dorsal vein graft to the corpora cavernosa), and the Quackel shunt (corpora cavernosa to the corpora spongiosum). The Grayhack procedure is a venous extra-anatomic shunt that connects the proximal corpora cavernosa to the great saphenous vein (GSV). Given the high success rate of medical management of priapism and the more common use of intrapenile shunts, the caverno-saphenous shunt is rarely indicated and has been described only a few times. In the present report, we describe the successful use of this vascular bypass in a patient with priapism refractory to conventional urologic treatment methods. The patient provided written informed consent for the report of his case details and imaging studies.
Case report
A 60-year-old man presented with persistent erection of 10 hours’ duration secondary to the use of an injectable erectile dysfunction medication consisting of alprostadil, papaverine, and phentolamine (Trimix). He had no prior medical or surgical history but notably had been seen in our emergency department for the same issue 2 years prior and was successfully treated with a bedside aspiration procedure. During that visit in 2019, he reported frequent sustained erections that were self-treated with injectable phenylephrine. These episodes were always linked to his misuse of the injectable medications in multiple ways, including taking it with sildenafil (Viagra), using it multiple times a day, and reinjecting it after having self-administered the reversal agent. He had been warned to avoid these medications all together but was nonadherent with the recommendation, and each visit for priapism required more invasive treatment than the last due to the progressive penile damage from the repeated ischemic insults.
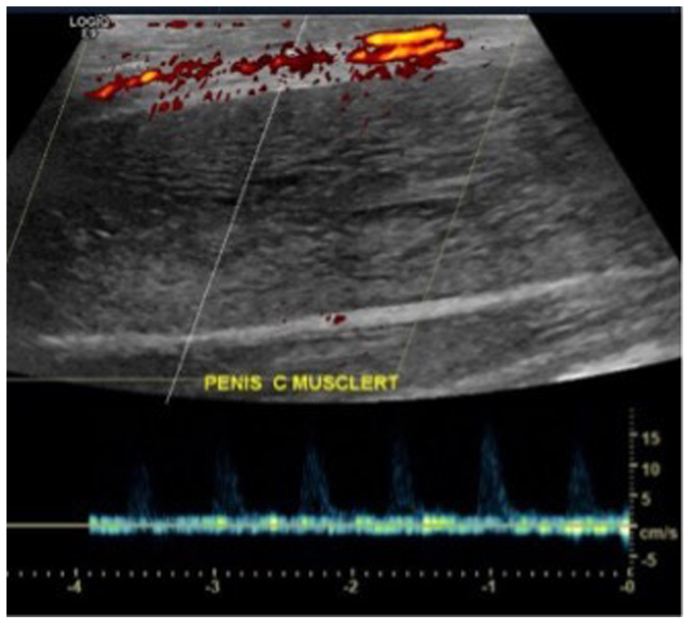
At his current presentation, urology had attempted conservative management with cold packs, antiplatelet therapy, and phenylephrine injection. However, detumescence was fleeting, and he was admitted to the hospital for corporal irrigation and T-shunting with transglanular tunneling. His postoperative detumescence lasted for 4 hours before his painful erection recurred the next morning (Fig 1). Penile Doppler ultrasound was obtained due to concerns for tissue ischemia after 24 hours of sustained erection and confirmed no arterial flow within the corpora cavernosa (Fig 2). The vascular service was consulted for consideration of a proximal shunt via a vascular bypass, known as the caverno-saphenous shunt.
Fig 1.
Photograph showing recurrent erection after distal shunting procedure.
Fig 2.
Penile Doppler ultrasound confirmed no arterial flow within the corpora cavernosa.
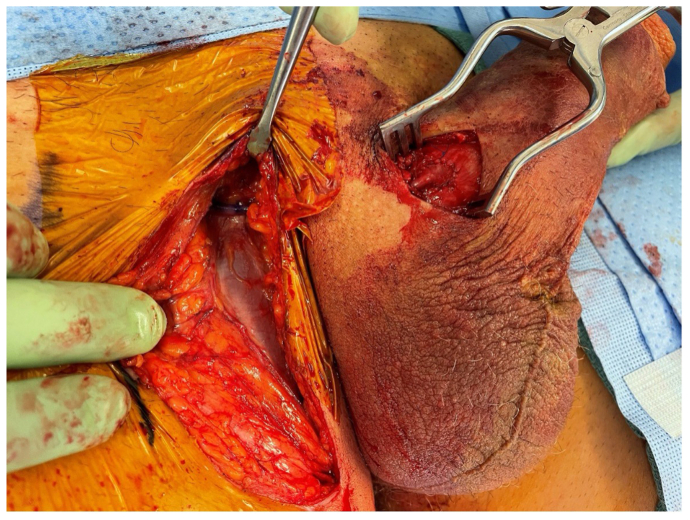
Preoperative bilateral lower extremity vein mapping found a GSV diameter of 4.3 mm on the right and 3.7 mm on the left. Intraoperative ultrasound was used to confirm this before performing an incision over the saphenofemoral junction. A total of 10 cm of the GSV was mobilized and ligated distally. A second skin incision was made at the right base of the penis to expose tense corpora cavernosa and Buck's fascia (Fig 3). A lateral elliptical corporotomy was created and dilated to allow for drainage of dark blood clots from within the corpora cavernosa. The penis was compressed until bright red blood drained, indicating adequately oxygenated blood flow. Next, 3000 U of heparin was administered by anesthesia. The mobilized GSV was then rotated medially and tunneled under the skin toward the corporotomy, where it was heparinized (Fig 4). An anastomosis was created between the vein and tunica albuginea using 5-0 Prolene suture (Ethicon), which spanned 10 mm in diameter. The completed caverno-saphenous bypass is demonstrated in Fig 5, in which full distension of the vein is visualized. Patency of the new shunt was tested with compression of the penis and listening for the coinciding Doppler signal (Supplementary Video 1, online only). Detumescence was maintained throughout the procedure and after skin closure (Fig 6). He had no further episodes of priapism during his hospital stay. On postoperative day 1, the penis was noted to be hyperemic and partially erect but neither firm nor painful. He was prescribed 2.5 mg of rivaroxaban and 375 mg of aspirin for 30 days and discharged.
Fig 3.
Skin incision at the base of the penile shaft, exposing Buck's fascia of the tense corpora cavernosa.
Fig 4.
Intraoperative photograph showing the right great saphenous vein (GSV) swung medially and tunneled within the subcutaneous tissue to meet the corporotomy, where it was heparinized in preparation for the anastomosis.
Fig 5.
Intraoperative photograph showing an anastomosis created between the right great saphenous vein (GSV) and tunica albuginea to establish the caverno-saphenous shunt.
Fig 6.
Detumescence was sustained after completion of the anastomosis and closure of the skin incision.
At subsequent follow-up visits, the patient reported partial maintenance of sexual activity in that he could sustain only a semi-erection. However, he did not experience any recurrent episodes of priapism. He insisted on shunt reversal, because the erectile dysfunction was significantly affecting his quality of life. We strongly advised against this, because we thought it would lead to recurrent priapism but, ultimately, accepted the patient's request. The shunt was surgically reversed 6 months after his original surgery. The bypass was cut down and exposed to allow a right-angle dissector underneath, and 2-0 silk ties were used to ligate the vein. During his postoperative clinic visit, he reported improvement in his sexual function and no further issues with sustained erections.
Discussion
The treatment of priapism follows a stepwise algorithm arranged from least to most invasive. The time spent in each step is dependent on clinical judgment, because early decompression is critical in preventing destructive changes in the penile tissue.
In 1968, Grace and Winter3 conservatively treated 21 patients with sedation, cold compresses, heparin, anesthesia, with treatment successful only for 5 of them. The caverno-saphenous shunt operation, first described by Grayhack et al4 in 1964, allows for drainage of the cavernosa through an autologous shunt into venous drainage of the lower extremity. Ihekwaba and Lawani5 described a case of sickle cell hemoglobinopathy-induced priapism and another of idiopathic priapism, both of which resulted in potency within 6 months of the operation. In contrast, Lehtonen and Tenhunen6 discussed three cases of idiopathic priapism treated with venous shunting, all of which resulted in impotence. Truly normal erections postoperatively have rarely been recorded.
Occlusion of the venous bypass resulting in premature closure of the shunt is the most feared complication. Lue and Garcia7 described two cases of ischemic priapism treated with shunting procedures, both of which recurred the next morning due to postoperative thrombosis. These patients then treated with 325 mg of aspirin and 5000 U of heparin perioperatively, which achieved sustained detumescence. The caverno-saphenous venous bypass presented in the present case was confirmed to be widely patent on the patient's return to the operating room for his reversal procedure, which could be attributed to the antithrombotic therapy he received.
Although, to the best of our knowledge, this is the first reported case in which the bypass was later ligated, we do not advise this. The ischemic changes to penile tissue can be permanent, and no reliable method is available for determining whether the revascularized tissue has fully recovered. The reversal procedure, therefore, risks insufficient venous outflow and recurrent priapism. Moreover, the caverno-saphenous shunt is currently the last known step in the algorithm for the treatment of priapism; thus, no options remain if it fails.
Disclosures
None
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
Additional material for this article may be found online at .www.jvscit.org
Appendix
Additional material for this article may be found online at .www.jvscit.org
Appendix (online only)
Intraoperative Doppler ultrasound was used to evaluate flow within the caverno-saphenous shunt.
References
- 1.Pryor J., Akkus E., Alter G., et al. Priapism. J Sex Med. 2004;1:116–120. doi: 10.1111/j.1743-6109.2004.10117.x. [DOI] [PubMed] [Google Scholar]
- 2.Montague D.K., Jarow J., Broderick G.A., et al. Members of the erectile dysfunction guideline update panel; americal urological association. American urological association guideline on the management of priapism. J Urol. 2003;170:1318–1324. doi: 10.1097/01.ju.0000087608.07371.ca. [DOI] [PubMed] [Google Scholar]
- 3.Grace D.A., Winter C.C. Priapism: an appraisal of management of twenty-three patients. J Urol. 1968;99:301–310. doi: 10.1016/S0022-5347(17)62697-1. [DOI] [PubMed] [Google Scholar]
- 4.Grayhack J.T., McCullough W., O'Conor V.J., Trippel O. Venous bypass to control priapism. Invest Urol. 1964;1:509–513. [PubMed] [Google Scholar]
- 5.Ihekwaba F.N., Lawani J. Caverno-saphenous shunt in the treatment of priapism. Postgrad Med J. 1981;57:132–135. doi: 10.1136/pgmj.57.664.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lehtonen T., Tenhunen A. Treatment of idiopathic priapism by Grayhack's caverno-saphenous shunt. Scand J Urol Nephrol. 1973;7:233–235. doi: 10.3109/00365597309133709. [DOI] [PubMed] [Google Scholar]
- 7.Lue T.F., Garcia M. Should perioperative anticoagulation be an integral part of the priapism shunting procedure? Transl Androl Urol. 2013;2:316–320. doi: 10.3978/j.issn.2223-4683.2013.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative Doppler ultrasound was used to evaluate flow within the caverno-saphenous shunt.