Abstract
Objectives
This scoping review aims to map the literature on goal-setting tools in adult rehabilitation, exploring their characteristics, target users and supporting evidence to inform practice and future research in this area.
Methods
We completed a comprehensive search of four databases to identify relevant articles on tools for goal setting in rehabilitation. We followed Arkey and O’Malley's scoping review process to guide article selection, data extraction and data analysis.
Results
We identified a total of 165 studies that reported on 55 different goal-setting tools, including tools for goal selection and goal documentation (n = 31), goal setting and intervention planning (n = 15), and for measuring the quality of the goal-setting process (n = 9). Over half of the tools were primarily designed for use in rehabilitation of physical disabilities (n = 32). Some tools fell under multiple sub-categories based on their characteristics as follows: 22 framework tools, 12 interview tools, 9 outcome measurement tools for goal achievement, 6 outcome measurement tools for goal quality and 25 documentation tools. The majority of goal-setting instruments targeted goals at the level of activity and participation (n = 51) and aimed to facilitate a client-centred or shared decision-making approach to rehabilitation planning (n = 46).
Conclusions
This study provides a comprehensive overview of existing goal-setting tools, highlighting their characteristics, target users and identified needs. These findings can enhance practitioners’ awareness of the range of goal-setting tools available and can enable more effective utilization of these tools in clinical practice. Further research should investigate how clinicians can combine multiple tools to deliver goal setting.
Keywords: Goal setting, rehabilitation, scoping review, goal-setting tool, shared decision-making
Introduction
Clinical practice guidelines usually advocate for the integration of goal setting in the rehabilitation process.1–3 Goal setting is thought to enhance clients’ motivation and engagement in rehabilitation and to improve communication and collaboration between healthcare practitioners and clients, ultimately leading to accelerated recovery and better health outcomes.4,5 Various approaches have been proposed to increase the involvement of rehabilitation clients in the goal-setting process in order to facilitate shared decision-making.6,7 However, certain barriers still impede application of collaborative goal setting in some practice areas. These barriers include challenges around understanding and meeting clients’ information needs, 7 limitations in clients’ communication or cognitive abilities, and limitations in therapists’ skills or knowledge to apply goal setting effectively. 4 Notably, following an audit of goal-setting practice across seven rehabilitation wards, Saito et al. 8 found that 79% of goals set by occupational therapists did not align with clients’ perceived goals. This study, and others like it,10,184 suggests that there remains a need for further investigation into the best tools to facilitate therapist communication and client engagement in the goal-setting process. 8
In this study, the term ‘goal-setting tool’ is used to refer to a specific test, guide, interview, questionnaire, or other structured method of clinical interaction, which is designed to support the goal-setting process or to evaluate outcomes arising from it. Goal-setting tools may aid in problem identification, shared goal prioritization, treatment progress monitoring, measurement of goal achievement, or active client involvement. Previous systematic reviews have suggested that tools designed to aid client involvement in clinical processes can enhance the meaningful involvement of older adults in clinical decision-making and rehabilitation clients in individualized, person-centred goal setting – although the choice of which tool is best to use in which setting remain somewhat unclear. 9 Indeed, although various goal-setting tools have been developed,11,12 there is a lack of comprehensive reviews detailing their characteristics and supporting their application in clinical practice. The objective of this scoping review therefore was to identify all existing goal-setting tools and to categorize their key features in order to guide future research on the development of effective strategies and tools for goal setting in clinical practice.
Methods
This scoping review followed Arksey and O’Malley’s framework, 13 which comprises a five-step process as follows: (a) identification of review questions; (b) identification of relevant studies; (c) selection of studies; (d) data extraction; and (e) summarization and reporting of results. The reporting of this review adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses – Extension for Scoping Reviews checklist. The completed forms are attached in Supplemental material 1. 14
The aim of this scoping review was to address the following four research questions related to the use of goal-setting tools in adult rehabilitation as follows:
What tools have been developed to support or enhance goal setting in adult rehabilitation?
How are these goal-setting tools used and in which contexts?
What are the characteristics of these goal-setting tools?
What future research needs to be conducted to better understand the impact of these goal-setting tools on the quality of goal setting and on improved health outcomes?
We included all studies published in English that reported on any tools used to support goal setting in adult (>18 years) rehabilitation. Rehabilitation, in this context, refers to strategies or interventions aimed at mitigating the effects of impairments, activity limitations or participation restrictions in individuals with various health conditions. 28 To be included in the review, articles needed to focus on tools specifically designed to assist in different aspects of goal setting, including goal selection, goal documentation, planning or pursuit of goal achievement, measurement of goal attainment, or assessment of the quality of the goal-setting process. We excluded studies that only used activity monitoring or step counts as a goal of therapy and studies that investigated intervention programs, technologies, websites or other applications primarily designed for purposes other than goal setting, but with minor goal-setting features. Furthermore, we excluded papers that primarily focused on describing theories underpinning goal setting. All articles, except for study protocols, conference abstracts, book chapters and theses, were eligible for inclusion. There were no exclusions based on methodological quality assessment, and no restrictions were placed on the publication year.
We conducted a comprehensive literature search of four databases, Scopus, PubMed, MEDLINE and ProQuest, from inception to 28 February 2023. The search involved identifying articles which used three main terms (‘tool’, ‘goal’ and ‘rehabilitation’), synonyms of these terms, or other related terminology (see Supplemental material 2 for details). To ensure the inclusion of appropriate studies, two or more authors independently reviewed each title and abstract to exclude duplicate or irrelevant studies. We subsequently retrieved all full-text publications, and two authors independently screened the full text for inclusion, identifying and recording reasons for exclusion of ineligible studies. We resolved any disagreements through discussion or, when required, consultation with a third review author.
Two authors (YO and KT) collaboratively developed a data extraction template, which was further refined through discussions with the other authors. Using this template, all authors contributed to extracting data from assigned articles. Both YO and KT reviewed the accuracy of the extracted information from all assigned articles. Any discrepancies or differences in extracted data were resolved through discussions involving at least two authors. We extracted data on both the characteristics of the included study and on the characteristics of the goal-setting tools. For the study characteristics, we collected information on the country of the first author’s affiliation, study design, study setting, sample size and patient population. Regarding the goal-setting tools, we collected data on the name of the identified tool, intended user, intended patient population, intended purpose, type of tool, intended domain of goals (i.e. body function or structure, activity or participation or environmental factors), type of decision-making involved, description of the tool and study findings.
We grouped each goal-setting tool into one of three categories as follows:
Tools for goal selection and documentation: These were tools specifically designed to facilitate the goal-setting process, which had a primary focus on setting goals but which sometimes included elements that could be used as outcome measures. The main aim of these tools was to support the identification and documentation of goals.
Tools for goal setting and intervention delivery: These were tools that had been designed to facilitate the planning and development of goal-directed interventions. While these tools also could sometimes support the goal-setting process, their main focus was on enabling and guiding interventions that were aligned with the identified goals.
Tools for measuring the quality of goal setting: These were tools that were designed to primarily focus on evaluating the quality of goal setting. They are intended to help assess the effectiveness and appropriateness of the goal-setting process from the perspective of therapists, clients, or other stakeholders.
We then grouped each goal-setting tool across a range of sub-categories. These sub-categories were developed iteratively by the two lead authors (YO and KT) following evaluation and discussion of the preliminary review findings, and were not mutually exclusive – in other words, a single approach to goal setting could be positively identified as belonging to any number of these sub-categories. These additional sub-categories of goal-setting tools were as follows:
Goal-setting frameworks: This sub-category referred to a structured approach or model that provided guidance for users to follow a specific way of goal setting. This included step-by-step guides to goal setting and goal-setting approaches based on principles of engagement with clients.
Interview tools: Interview tools were resources or instruments that facilitated or guided semi-structured interviews in order to assist with gathering information relevant to the goal-setting process.
Outcome measures (goal achievement): Tools under this sub-category allowed users to measure goal attainment or achievement. These tools assessed the extent to which the goals had been accomplished or the desired outcomes had been realized.
Outcome measures (goal-setting quality): Tools under this sub-category enabled users to measure the quality of goal setting or other aspects related to the goal-setting process. These tools might be used to evaluate the effectiveness, appropriateness, or value of the goal-setting process or of the goals themselves. They were designed to provide insights into the quality or characteristics of the goals set.
Documentation tools: This sub-category of tools included any physical or digital resource, excluding information and communications technology, that enabled the user to take notes for goal setting or to record goals that were set. Examples included paper-based forms, templates or digital documents specifically designed for documenting goals.
Information and Communications Technology tools: This sub-category referred to any tools that used digital technology to enable the storage, retrieval, manipulation, transmission, or reception of information. In the context of goal setting, Information and Communications Technology tools include digital platforms, software, applications or devices that had functionalities for goal setting.
Regarding the target patient population, we grouped each tool into the one of four broad categories of medical conditions as follows:
Physical disability: Tools designed for individuals with physical disabilities that affect their physical condition, such as mobility, physical capacity, range of motion and strength (e.g. brain injury, spinal cord injuries, cerebral palsy, cardiovascular disabilities and visual impairments).
Psychiatric disability: Tools aimed at individuals with psychological problems that impacted their mental well-being, including their thoughts, emotions and behaviours (e.g. depression, eating disorders, schizophrenia and bipolar disorder).
Age-related disability: Tools intended for use with individuals who are described as ‘older’ or ‘elderly’ or are aged over 65 years old. These tools were specifically tailored to address the unique needs and challenges associated with aging.
Others/specified condition: Tools that were specifically designed for addressing the needs of individuals with a single particular medical condition (e.g. aphasia, pain, or cancer).
We also extracted data on the target domain of the goal-setting process (body structure or body function, activity or participation, environmental factors, or non-specific – according to the International Classification of Functioning, Disability and Health categories), 15 the type of decision-making involved (e.g. client-centred or shared decision-making; therapist-led, caregiver-centred, or unclear), and the intended users of the tool (e.g. physiotherapy, occupational therapy, physician or psychologist, other healthcare professional, or clients or caregiver). While a scoping review does not typically require an in-depth analysis of specific evidence types, we wanted to map out the spread of evidence supporting the effectiveness of different goal-setting tools to achieve improvements in either the rehabilitation process (e.g. degree of client engagement) or health outcomes. In order to report on the highest quality evidence of effectiveness, we focused on studies that used randomized control trial designs. The aim of this aspect of the analysis was to evaluate the spread of existing evidence on the effectiveness of these tools and to identify gaps in the evidence base to guide future research.
Results
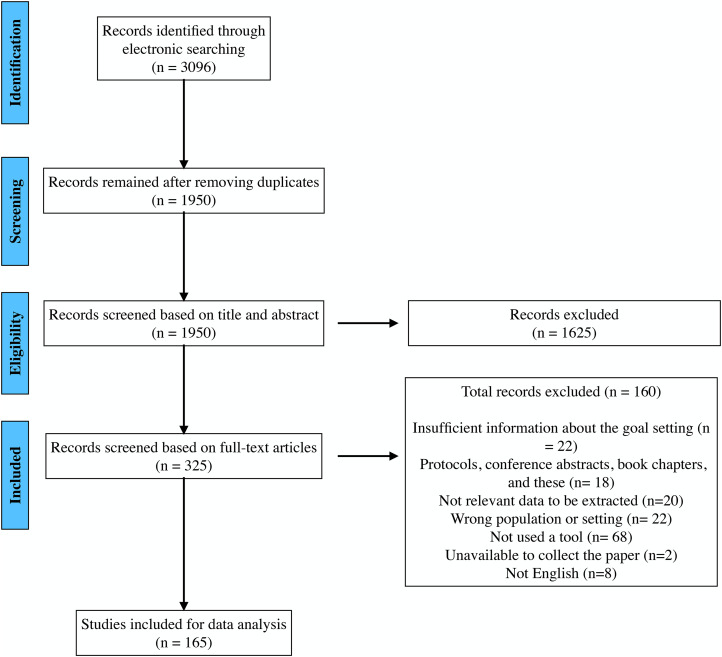
The initial search yielded a total of 1950 records, which were narrowed down to 165 full text articles for final analysis. The screening process and reasons for exclusions are reported in Figure 1. The majority of the articles (119/165) were published in the last decade. The identified study designs included 47 observational studies, 26 qualitative studies, 21 review papers (including narrative reviews, literature reviews and scoping reviews), 16 randomized controlled trials, 12 case studies, 11 systematic reviews, 10 mixed methods studies, 2 surveys, 14 articles with unclear designs and 6 other research designs (such as simulated studies, prospective descriptive studies, comparative designs, clinical audits, non-controlled interventions and practical guides).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram displays article selection process.
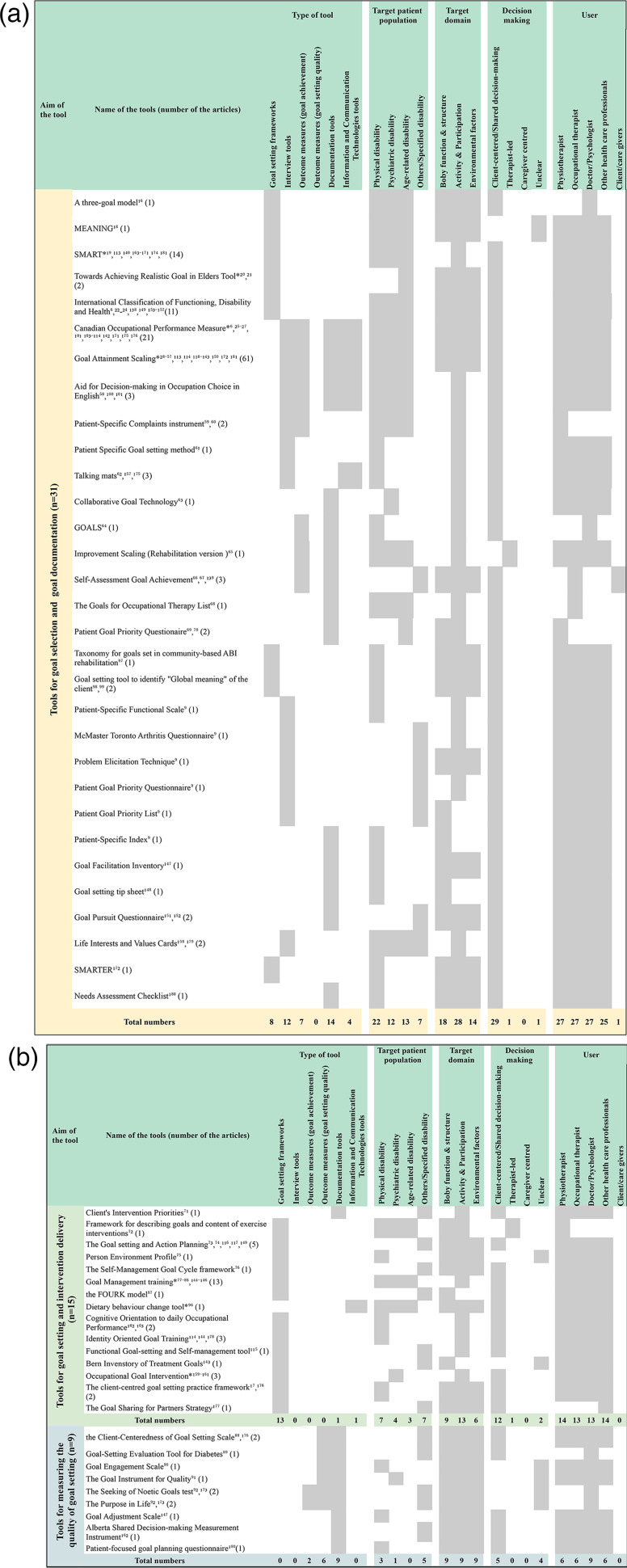
Identified goal-setting tools along with their respective characteristics are shown in Figure 2 (a detailed description of each tool can be found in Supplemental material 3). A total of 55 distinct goal-setting tools were identified among the 165 articles.
Figure 2.
(a and b) Identified goal-setting tools with their respective characteristics.
Characteristics of the identified goal-setting tools
Of the 55 identified goal-setting tools, 56% (31/55) were tools for goal selection and goal documentation, and 27% (15/55) were for goal setting and intervention delivery, while the remaining 16% (9/55) were for measuring the quality of goal setting. These tools were tested across various patient populations, including those with as follows: physical disabilities (32/55), psychiatric disabilities (17/55), age-related disabilities (16/55) and other/specific medical conditions (19/55). The majority of the identified tools appeared to be not specifically intended for use by a particular health profession.
Six of the identified tools were described and studied in five or more articles. These included Goal Attainment Scaling including Goal Attainment Scaling for Major Depressive Disorder and Goal Attainment Scaling for Upper Limb Spasticity28–57,113,114,118–143,150,172,181 (n = 61), Canadian Occupational Performance Measure6,25–27,101,103–114,142,171,175,176 (n = 21), Goal Management Training77–86,144–146 (n = 13), International Classification of Functioning, Disability and Health6,22–24,138,149,153–157 (n = 11) and the Goal setting and Action Planning73,74,116,117,149 (n = 5). Interestingly, none of the identified tools intended for measuring the quality of goal setting were supported by more than two research studies, potentially indicating limited evidence for such tools.
Many of the identified tools met the criteria for multiple sub-category types, but included as follows: 22 goal-setting frameworks, 12 interview tools, nine outcome measures for goal achievement, six outcome measures for goal-setting quality and 25 documentation tools. The majority of the tools categorized as being for goal setting and intervention delivery appeared to be framework tools, whereas no framework tools were identified in the tools categorized as outcome measures of goal-setting quality.
Only five of the identified tools made use of information and communications technology for goal setting, four of which were categorized as tools for goal selection and goal documentation. These included Canadian Occupational Performance Measure,6,25–27,101,103–114,142,171,175,176 Goal Attainment Scaling,28–57,113,114,118–143,150,172,181 Aid for Decision-making in Occupational Choice in English58,100,101 and Talking mats.62,157,175 Of note: Goal-setting tools that included an Information and Communications Technology format appeared to be primarily designed for use in an in-person context and not specifically for remote use (i.e. for rehabilitation services provided by telerehabilitation).
The majority of tools targeted goals set at the level of activity and participation (51/55) and involved a client-centred or shared decision-making approach to goal selection (46/55). Some tools supported goals being set at the level of body function or body structure (36/55) or which targeted environmental factors (29/55). A minority of tools (2/55) enabled a therapist-led approach to goal setting. There were no tools specifically designed for caregiver-centred decision-making.
Research evidence on the effectiveness of goal-setting tools
Of the identified 55 goal-setting tools, only seven had been studied via randomized control trial methods, indicated by an asterisk (*) in Figure 2. The tools supported by randomized control trials included as follows: Goal Management Training (n = 6)77,79,81,83,85,86; Goal Attainment Scaling (n = 4)36,57,126,130; SMART (n = 2)163,170; Towards Achieving Realistic Goal in Elders Tool (n = 1) 21 ; Dietary Behaviour Change Tool (n = 1) 96 ; Canadian Occupational Performance Measure (n = 1) 108 ; and Occupational Goal Intervention (n = 1). 160 The majority of research providing evidence to support use of the identified tools involved non-randomized control trial design or observational methods, indicating lower levels of evidence regarding the effectiveness of the approach. One of the tools, Goal Attainment Scaling, was only used to measure outcomes in randomized control trials rather than using randomized control trial methods to test the effectiveness of the tool to improve the rehabilitation process or patient outcomes.36,57,126,130 Two other tools, Canadian Occupational Performance Measure 108 and SMART,163,170 were used as part of a goal-direct approach to rehabilitation (i.e. for goal-directed cognitive rehabilitation, 108 goal-directed interval walking training, 163 and goal-directed low back pain rehabilitation 170 ) so did not provide evidence of the effectiveness of goal setting in isolation of the rest of a comprehensive rehabilitation programme. The remaining identified tools (Goal Management Training77,79,81,83,85,86; Towards Achieving Realistic Goal in Elders Tool 21 ; Dietary Behaviour Change Tool 96 ; and Occupational Goal Intervention 160 ) all investigated the effectiveness of an approach to goal setting on changes in one or more health outcomes compared to a control group that did not receive goal setting.
Among the randomized control trials that investigated the goal-setting tools as primary interventions compared to control groups, Parsons et al. 21 evaluated the impact of Towards Achieving Realistic Goal in Elders Tool, a goal facilitation tool, on health-related quality of life, social support and physical function in community-dwelling older people receiving home care. The study concluded that the use of Towards Achieving Realistic Goal in Elders Tool led to significant improvements in health-related quality of life in the intervention group and helped individualize activities tailored to the participants’ needs and goals.
Several randomized control trials have investigated the effectiveness of Goal Management Training to address problems with executive functioning among different populations.77–86 For example, randomized control trials supported the effectiveness of Goal Management Training alone in improving executive functioning and daily activity performance in patients with spina bifida 83 and chronic acquired brain injury. 81 Other studies supported the effectiveness of combining Goal Management Training with other interventions to improve executive functioning. 79 These included a randomized control trial by Casaletto et al. 77 showing that a combination of Goal Management Training and metacognitive training had significant effects on everyday multitasking and metacognitive performance. Similarly, Levine et al. 79 compared an expanded version of Goal Management Training to another intervention, Brain Health Workshop, among patients recovering from brain disease, and found that Goal Management Training was efficacious in the rehabilitation of executive function. Additionally, a randomized control trial by Bertens et al. 85 supported the effectiveness of Goal Management Training combined with errorless learning for training complex daily tasks in brain-injured patients with executive dysfunction.
Discussion
This scoping review aimed to increase awareness of available goal-setting tools in rehabilitation and to provide insights into their characteristics in order to assist practitioners to utilize them more confidently and effectively in clinical practice. This discussion will focus on the three categories of goal-setting tools as follows: (a) tools for goal selection and goal documentation; (b) tools for goal setting and rehabilitation planning; and (c) tools for measuring the quality of goal setting.
In the category of tools for goal selection and goal documentation (see Figure 2(a)), several frameworks were identified that can enhance understanding of goals and goal setting. These goal-setting tools help improve the clarity and focus of goal setting by providing theoretical guidance and by highlighting important factors to consider. They can save time and simplify the goal-setting process. Furthermore, seven of these tools (see Figure 2(a)) not only support the goal-setting process but also can be used as outcome measures to evaluate goal achievement. These tools can support evidence-based intervention delivery and enhance the therapy planning process. 95 The majority of identified goal-setting tools are applicable across various medical conditions and target activity and participation domains. These tools facilitate client-centred or shared decision-making approaches and can be easily integrated into clinical practice without extensive training. Additionally, four of these tools (see Figure 2(a)) are available in a digital format, which may make them easier for health professionals to integrate into practice. The use of Information and Communications Technology in goal setting may facilitate client engagement, providing a platform for expressing ideas and opinions about goals, establishing collaborative structures, and managing the complexity of goal setting. 12
In the category of tools for goal setting and intervention delivery (see Figure 2(b) upper), the majority of tools (13/15) were identified as frameworks designed to guide the integration of goal setting into rehabilitation planning. These frameworks offer theories and evidence-based methods that support the participants to work on goal-directed therapy by facilitating goal-directed behaviours. For example, Goal Management Training77–86,144–146 is a framework that involves a five-stage process to address impairments in a person's capacity to engage in goal-directed behaviour. Similarly, Goal Setting and Action Planning73,74,116,117,149 is designed to support informed decision-making about goal adjustment or goal disengagement by undertaking four stages as follows: (a) goal negotiation and setting; (b) action planning and coping planning; (c) action; and (d) appraisal, feedback and decision-making. It has been reported that many health professionals find it challenging to negotiate with clients and family members around the selection of realistic, achievable and personally meaningful goals. 90 By incorporating these goal-setting frameworks into clinical practice, therapists can promote goal-directed behaviours and strengthen their therapeutic alliance with clients, with the ultimate aim of improving rehabilitation outcomes.
In the category of tools for measuring the quality of goal setting (see Figure 2(b) lower), nine different tools were identified. These tools provide valuable insights into the goal-setting process and can contribute to improving the quality of goal setting in rehabilitation practice. One example is the Client-Centredness of Goal Setting scale,88,176 which was specifically designed to help therapists assess the extent to which goal setting aligns with client-centred principles, facilitating a collaborative and client-driven approach to goal setting. By incorporating the client’s input and incorporating their responses into the goal-setting process, therapists can ensure that goals are meaningful and tailored to the individual’s needs and preferences. Other tools (see Figure 2(b) lower) offer additional dimensions for evaluating the quality of goal setting. These tools assess various aspects of goal setting, including goal engagement, the pursuit of meaningful goals, the alignment of goals with personal values and the effectiveness of shared decision-making. This evaluation process can inform the therapeutic process, improve the client’s experience and optimize goal attainment and overall rehabilitation outcomes.
While this scoping review provides valuable insights into goal-setting tools in rehabilitation, there are several limitations that need to be acknowledged. One limitation is that this review was not designed to investigate the psychometric properties of the identified tools. Validity and reliability assessments are crucial for ensuring the effectiveness and applicability of these tools in clinical practice. Future research should focus on evaluating the psychometric properties of tools that have been developed to measure rehabilitation outcomes or the quality of goal-setting processes. Another limitation is the exclusion of grey literature (i.e. conference papers or research theses) from this review, which may have resulted in the omission of relevant information on the most recent goal-setting tools. Additionally, this review focused only on English-language tools, so potentially missed information about goal-setting tools that have been developed in other languages. Despite these limitations, this scoping review lays the groundwork for future research in the field of goal-setting tools in rehabilitation. The identified tools offer clinicians a starting point for selecting appropriate tools based on their specific needs and objectives. Further research should explore the combination of different goal-setting tools to address the diverse needs of patient populations in various settings. By understanding how different goal-setting tools can be used together for greatest effect, clinicians can develop comprehensive and tailored approaches to goal setting in rehabilitation, with the ultimate aim of improving person-centred rehabilitation outcomes.
Clinical messages.
With over 50 goal-setting tools available, clinicians can select from a wide range of approaches to meet the specific needs of their area of clinical practice.
Goal-setting tools facilitate collaborative goal setting, measure therapy outcomes and track progress.
The right goal-setting tools can support planning, delivery and evaluation of rehabilitation interventions.
Understanding the characteristics and quality of goal-setting tools can help selection of the right tool for the right client in the right rehabilitation context.
Supplemental Material
Supplemental material, sj-docx-1-cre-10.1177_02692155231197383 for Characteristics of goal-setting tools in adult rehabilitation: A scoping review by Yuho Okita, Yuko Kawaguchi, Yuki Inoue, Kanta Ohno, Tatsunori Sawada, William Levack and Kounosuke Tomori in Clinical Rehabilitation
Supplemental material, sj-docx-2-cre-10.1177_02692155231197383 for Characteristics of goal-setting tools in adult rehabilitation: A scoping review by Yuho Okita, Yuko Kawaguchi, Yuki Inoue, Kanta Ohno, Tatsunori Sawada, William Levack and Kounosuke Tomori in Clinical Rehabilitation
Supplemental material, sj-pdf-3-cre-10.1177_02692155231197383 for Characteristics of goal-setting tools in adult rehabilitation: A scoping review by Yuho Okita, Yuko Kawaguchi, Yuki Inoue, Kanta Ohno, Tatsunori Sawada, William Levack and Kounosuke Tomori in Clinical Rehabilitation
Footnotes
Author contributions: YO led study conception, study design, analysis and interpretation of data, drafted the manuscript and revised content based on feedback. KT assisted with study conception and design, interpretation of data and provided critical revision of drafts. YK, YI, KO and TS contributed to the article screening, data charting and interpretation process. WL played a role in refining the study findings and contributing to the writing of the manuscript. All authors approved the final version of the manuscript. YO is responsible for the integrity of this work as a whole.
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was supported by Grant-in-Aid for Scientific Research (B) [19H03875].
ORCID iD: Yuho Okita https://orcid.org/0000-0002-8455-3301
Supplemental material: Supplemental material for this article is available online.
References
- 1.Goble A, Worcester M. Best Practice Guidelines for Cardiac Rehabilitation and Secondary Prevention. Department of Human Services 1999.
- 2.Moore JL, Potter K, Blankshain K, et al. A core set of outcome measures for adults with neurologic conditions undergoing rehabilitation. J Neurol Phys Ther 2018; 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Teasell R, Salbach NM, Foley N, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part one: rehabilitation and recovery following stroke; 6th edition update 2019. Int J Stroke 2020; 15(7)(7): 763–788. [DOI] [PubMed] [Google Scholar]
- 4.Rosewilliam S, Roskell CA, Pandyan A. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin Rehabil 2011; 25: 501–514. [DOI] [PubMed] [Google Scholar]
- 5.Sugavanam T, Mead G, Bulley C, et al. The effects and experiences of goal setting in stroke rehabilitation – a systematic review. Disabil Rehabil 2013; 35: 177–190. [DOI] [PubMed] [Google Scholar]
- 6.Leach E, Cornwell P, Fleming J, et al. Patient centered goal-setting in a subacute rehabilitation setting. Disability Rehabil 2009; 32: 1–14. [DOI] [PubMed] [Google Scholar]
- 7.Rutten LJF, Arora NK, Bakos AD, et al. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns 2005; 57: 250–261. [DOI] [PubMed] [Google Scholar]
- 8.Saito Y, Tomori K, Sawada T, et al. Determining whether occupational therapy goals match between pairs of occupational therapists and their clients: a cross-sectional study. Disabil Rehabil 2019; 25: 1–6. [DOI] [PubMed] [Google Scholar]
- 9.Stevens A, Beurskens A, Köke A, et al. The use of patient-specific measurement instruments in the process of goal-setting: a systematic review of available instruments and their feasibility. Clin Rehabil 2013; 27: 1005–1019. [DOI] [PubMed] [Google Scholar]
- 10.Nijhuis BJ, Reinders-Messelink HA, de Blécourt AC, et al. Goal setting in Dutch paediatric rehabilitation. Are the needs and principal problems of children with cerebral palsy integrated into their rehabilitation goals? Clin Rehabil 2008; 22: 348–363. [DOI] [PubMed] [Google Scholar]
- 11.van Seben R, Reichardt L, Smorenburg S, et al. Chapter 7 Goal-setting instruments in geriatric rehabilitation: a systematic review. J Frailty Aging 2017; 6(1): 37–45. [DOI] [PubMed] [Google Scholar]
- 12.Strubbia C, Levack WMM, Grainger R, et al. Use of technology in supporting goal setting in rehabilitation for adults: a scoping review. BMJ Open 2020; 10: e041730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8: 19–32. [Google Scholar]
- 14.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169: 467. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. International classification of functioning, disability and health : ICF. World Health Organization, https://apps.who.int/iris/handle/10665/42407 (2001, accessed 22 June).
- 16.Vermunt NP, Harmsen M, Elwyn G, et al. A three-goal model for patients with multimorbidity: a qualitative approach. Health Expect 2018; 21: 528–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prescott S, Fleming J, Doig E. Rehabilitation goal setting with community dwelling adults with acquired brain injury: a theoretical framework derived from clinicians’ reflections on practice. Disabil Rehabil 2018; 40: 2388–2399. [DOI] [PubMed] [Google Scholar]
- 18.Ford P. Rehabilitation goal setting theory, practice and evidence. Occup Med (Chic Ill) 2015; 65: 261–261. [Google Scholar]
- 19.Bovend’Eerdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil 2009; 23: 352–361. [DOI] [PubMed] [Google Scholar]
- 20.Parsons JGM, Parsons MJG. The effect of a designated tool on person-centred goal identification and service planning among older people receiving homecare in New Zealand. Health Soc Care Community 2012; 20: 653–662. [DOI] [PubMed] [Google Scholar]
- 21.Parsons J, Rouse P, Robinson EM, et al. Goal setting as a feature of homecare services for older people: does it make a difference? Age Ageing 2012; 41: 24–29. [DOI] [PubMed] [Google Scholar]
- 22.Constand MK, MacDermid JC. Applications of the International Classification of Functioning, Disability and Health in goal-setting practices in healthcare. Disabil Rehabil 2014; 36: 1305–1314. [DOI] [PubMed] [Google Scholar]
- 23.Siegert RJ, Levack W. Rehabilitation goal setting: theory, practice, and evidence. Boca Raton: Crc Press/Taylor & Francis Group, 2015. [Google Scholar]
- 24.Meesters J, Hagel S, Klokkerud M, et al. Goal-setting in multidisciplinary team care for patients with rheumatoid arthritis: an international multi-center evaluation of the contents using the International Classification of Functioning, Disability and Health as a reference. J Rehabil Med 2013; 45: 888–899. [DOI] [PubMed] [Google Scholar]
- 25.Wressle E, Eeg-Olofsson A-M, Marcusson J, et al. Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J Rehabil Med 2002; 34: 5–11. [DOI] [PubMed] [Google Scholar]
- 26.Hauken MA, Holsen I, Fismen E, et al. Participating in life again. Cancer Nurs 2014; 37: E48–E59. [DOI] [PubMed] [Google Scholar]
- 27.Doig E, Fleming J, Kuipers P, et al. Clinical utility of the combined use of the Canadian occupational performance measure and goal attainment scaling. Am J Occup Ther 2010; 64: 904–914. [DOI] [PubMed] [Google Scholar]
- 28.Hurn J, Kneebone I, Cropley M. Goal setting as an outcome measure: a systematic review. Clin Rehabil 2006; 20: 756–772. [DOI] [PubMed] [Google Scholar]
- 29.Chew J, Chong MS, Tay L, et al. Outcomes of a multimodal cognitive and physical rehabilitation program for persons with mild dementia and their caregivers: a goal-oriented approach. Clin Interv Aging 2015; 10: 1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stolee P, Awad M, Byrne K, et al. A multi-site study of the feasibility and clinical utility of goal attainment scaling in geriatric day hospitals. Disabil Rehabil 2012; 34: 1716–1726. [DOI] [PubMed] [Google Scholar]
- 31.Jennings M. Clinical report: evaluating the efficacy of a group audiologic rehabilitation program for adults with hearing loss using a goal attainment scaling approach. Can J Speech-Lang Pathol Audiol 2009; 33(3): 146. [Google Scholar]
- 32.Baggio L, Buckley DJ. Detecting change in patient outcomes in a rural ambulatory rehabilitation service: the responsiveness of Goal Attainment Scaling and the Lawton Scale. Aust Health Rev 2016; 40. [DOI] [PubMed] [Google Scholar]
- 33.Ottenbacher KJ, Cusick A. Discriminative versus evaluative assessment: some observations on goal attainment scaling. Am J Occup Ther 1993; 47: 349–354. [DOI] [PubMed] [Google Scholar]
- 34.Milne JL, Robert M, Tang S, et al. Goal achievement as a patient-generated outcome measure for stress urinary incontinence. Health Expect 2009; 12: 288–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brock K, Black S, Cotton S, et al. Goal achievement in the six months after inpatient rehabilitation for stroke. Disabil Rehabil 2009; 31: 880–886. [DOI] [PubMed] [Google Scholar]
- 36.Rockwood K, Howlett S, Stadnyk K, et al. Responsiveness of goal attainment scaling in a randomized controlled trial of comprehensive geriatric assessment. J Clin Epidemiol 2003; 56: 736–743. [DOI] [PubMed] [Google Scholar]
- 37.Bouwens SFM, van Heugten CM, Verhey FRJ. Review of goal attainment scaling as a useful outcome measure in psychogeriatric patients with cognitive disorders. Dement Geriatr Cogn Disord 2008; 26: 528–540. [DOI] [PubMed] [Google Scholar]
- 38.Scott AH, Haggarty EJ. Structuring goals via goal attainment scaling in occupational therapy groups in a partial hospitalization setting. Occup Ther Ment Health 1984; 4: 39–58. [Google Scholar]
- 39.Hartman D, Borrie MJ, Davison E, et al. Use of goal attainment scaling in a dementia special care unit. Am J Alzheimer’s Dis 1997; 12: 111–116. [Google Scholar]
- 40.Ayvat E, Kılınç ÖO, Ayvat F, et al. The use of goal attainment scaling (GAS) in the rehabilitation of ataxic patients. Neurol Sci 2018; 39: 893–901. [DOI] [PubMed] [Google Scholar]
- 41.Tabak NT, Link PC, Holden J, et al. Goal attainment scaling: tracking goal achievement in consumers with serious mental illness. Am J Psychiatr Rehabil 2015; 18: 173–186. [Google Scholar]
- 42.Lewis TF, Larson MF, Korcuska JS. Strengthening the planning process of motivational interviewing using goal attainment scaling. J Ment Health Couns 2017; 39: 195–210. [Google Scholar]
- 43.Khan F, Pallant JF, Turner-Stokes L. Use of goal attainment scaling in inpatient rehabilitation for persons with multiple sclerosis. Arch Phys Med Rehabil 2008; 89: 652–659. [DOI] [PubMed] [Google Scholar]
- 44.Weidenbohm K, Parsons M, Dixon R. Goal attainment scaling: a tool for use in evaluation of services for older people. NZ J Occup Ther 2005; 52(2): 9–14. [Google Scholar]
- 45.Fisher K, Hardie RJ. Goal attainment scaling in evaluating a multidisciplinary pain management programme. Clin Rehabil 2002; 16: 871–877. [DOI] [PubMed] [Google Scholar]
- 46.Eftekhar P, Mochizuki G, Dutta T, et al. Goal attainment scaling in individuals with upper limb spasticity post stroke. Occup Ther Int 2016; 23: 379–389. [DOI] [PubMed] [Google Scholar]
- 47.Zweber B, Malec J. Goal attainment scaling in post-acute outpatient brain injury rehabilitation. Occup Ther Health Care 1990; 7: 45–53. [DOI] [PubMed] [Google Scholar]
- 48.Bouwens SF, van Heugten CM, Verhey FR. The practical use of goal attainment scaling for people with acquired brain injury who receive cognitive rehabilitation. Clin Rehabil 2009; 23: 310–320. [DOI] [PubMed] [Google Scholar]
- 49.Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil 2009; 23: 362–370. [DOI] [PubMed] [Google Scholar]
- 50.Mannion AF, Caporaso F, Pulkovski N, et al. Goal attainment scaling as a measure of treatment success after physiotherapy for chronic low back pain. Rheumatology 2010; 49: 1734–1738. [DOI] [PubMed] [Google Scholar]
- 51.Gaasterland CMW, van der Weide MCJ, Roes KCB, et al. Goal attainment scaling as an outcome measure in rare disease trials: a conceptual proposal for validation. BMC Med Res Methodol Epub ahead of print December 2019; 19. 10.1186/s12874-019-0866-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kolip P, Schaefer I. Goal attainment scaling as a tool to enhance quality in community-based health promotion. Int J Public Health 2013; 58: 633–636. [DOI] [PubMed] [Google Scholar]
- 53.Ashford S, Turner-Stokes L. Rehabilitation goal setting: theory, practice and evidence. 1st ed. Boca Raton: CRC Press, 2014. [Google Scholar]
- 54.Forbes DA. Goal attainment scaling: a responsive measure of client outcomes. J Gerontol Nurs 1998; 24: 34–40. [DOI] [PubMed] [Google Scholar]
- 55.Krasny-Pacini A, Hiebel J, Pauly F, et al. Goal attainment scaling in rehabilitation: a literature-based update. Ann Phys Rehabil Med 2013; 56: 212–230. [DOI] [PubMed] [Google Scholar]
- 56.Ertzgaard P, Ward A, Wissel J, et al. Practical considerations for goal attainment scaling during rehabilitation following acquired brain injury. J Rehabil Med 2011; 43: 8–14. [DOI] [PubMed] [Google Scholar]
- 57.Herdman KA, Vandermorris S, Davidson S, et al. Comparable achievement of client-identified, self-rated goals in intervention and no-intervention groups: reevaluating the use of goal attainment scaling as an outcome measure. Neuropsychol Rehabil 2019; 29: 1600–1610. [DOI] [PubMed] [Google Scholar]
- 58.Levack W, Tomori K, Takahashi K, et al. Development of an English-language version of a Japanese iPad application to facilitate collaborative goal setting in rehabilitation: a Delphi study and field test. BMJ Open 2018; 8: e018908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stevens A, Moser A, Köke A, et al. The use and perceived usefulness of a patient-specific measurement instrument in physiotherapy goal setting. A qualitative study. Musculoskeletal Sci Pract 2017; 27: 23–31. [DOI] [PubMed] [Google Scholar]
- 60.Stevens A, Köke A, van der Weijden T, et al. The development of a patient-specific method for physiotherapy goal setting: a user-centered design. Disabil Rehabil 2018; 40: 2048–2055. [DOI] [PubMed] [Google Scholar]
- 61.Stevens A, Köke A, van der Weijden T, et al. Ready for goal setting? Process evaluation of a patient-specific goal-setting method in physiotherapy. BMC Health Serv Res Epub ahead of print 31 August 2017; 17. 10.1186/s12913-017-2557-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bornman J, Murphy J. Using the ICF in goal setting: clinical application using Talking Mats®. Disability and Rehabil: Assistive Technol 2006; 1: 145–154. [DOI] [PubMed] [Google Scholar]
- 63.Clarke SP, Oades LG, Crowe TP, et al. Collaborative goal technology: theory and practice. Psychiatr Rehabil J 2006; 30: 129–136. [DOI] [PubMed] [Google Scholar]
- 64.Conrad N, Doering BK, Rief W, et al. Looking beyond the importance of life goals. The personal goal model of subjective well-being in neuropsychological rehabilitation. Clin Rehabil 2010; 24: 431–443. [DOI] [PubMed] [Google Scholar]
- 65.Smith A, Cardillo JE, Smith SC, et al. Improvement scaling (rehabilitation version). Med Care 1998; 36: 333–347. [DOI] [PubMed] [Google Scholar]
- 66.Brubaker L, Khullar V, Piault E, et al. Goal attainment scaling in patients with lower urinary tract symptoms: development and pilot testing of the self-assessment goal achievement (SAGA) questionnaire. Int Urogynecol J 2011; 22: 937–946. [DOI] [PubMed] [Google Scholar]
- 67.Khullar V, Marschall-Kehrel D, Espuna-Pons M, et al. European content validation of the self-assessment goal achievement (SAGA) questionnaire in patients with overactive bladder. Int Urogynecol J 2013; 24: 1529–1536. [DOI] [PubMed] [Google Scholar]
- 68.Custer MG, Huebner RA, Freudenberger L, et al. Client-chosen goals in occupational therapy: strategy and instrument pilot. Occup Ther Health Care 2013; 27: 58–70. [DOI] [PubMed] [Google Scholar]
- 69.Åsenlöf P, Denison E, Lindberg P. Behavioral goal assessment in patients with persistent musculoskeletal pain. Physiother Theory Pract 2004; 20: 243–254. [Google Scholar]
- 70.Asenlof P, Siljeback K. The patient goal priority questionnaire is moderately reproducible in people with persistent musculoskeletal pain. Phys Ther 2009; 89: 1226–1234. [DOI] [PubMed] [Google Scholar]
- 71.Cisneros E, Moreno A, Léveillé G, et al. The Client’s Intervention Priorities (CIP)©: a person-centered tool to support goal setting during interdisciplinary neurorehabilitation. Cogent Psychology Epub ahead of print 1 January 2019; 6. 10.1080/23311908.2019.1603614 [DOI] [Google Scholar]
- 72.Leeden Mvd, Bart Staal J, Beekman E, et al. Development of a framework to describe goals and content of exercise interventions in physical therapy: a mixed method approach including a systematic review. Phys Ther Rev 2014; 19: 1–14. [Google Scholar]
- 73.Scobbie L, McLean D, Dixon D, et al. Implementing a framework for goal setting in community based stroke rehabilitation: a process evaluation. BMC Health Serv Res Epub ahead of print 24 May 2013; 13. 10.1186/1472-6963-13-190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Scobbie L, Brady MC, Duncan EAS, et al. Goal attainment, adjustment and disengagement in the first year after stroke: a qualitative study. Neuropsychol Rehabil 2020; 31: 1–19. [DOI] [PubMed] [Google Scholar]
- 75.Amsters DI, Kendall MB, Kuipers P, et al. The person-environment profile: preliminary development of a clinical tool for enhancing goal-based rehabilitation programs. Rehabil Process Outcome 2016; 5: RPO.S40455. [Google Scholar]
- 76.Langford A, Sawyer D, Gioimo S, et al. Patient-centered goal setting as a tool to improve diabetes self-management. Sci Diabetes Self-Manage Care 2007; 33. [DOI] [PubMed] [Google Scholar]
- 77.Casaletto KB, Moore DJ, Woods SP, et al. Abbreviated goal management training shows preliminary evidence as a neurorehabilitation tool for HIV-associated neurocognitive disorders among substance users. Clin Neuropsychol 2016; 30: 107–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stamenova V, Levine B. Effectiveness of goal management training® in improving executive functions: a meta-analysis. Neuropsychol Rehabil 2019; 29: 1569–1599. [DOI] [PubMed] [Google Scholar]
- 79.Levine B, Schweizer TA, O’Connor C, et al. Rehabilitation of executive functioning in patients with frontal lobe brain damage with goal management training. Front Hum Neurosci 2011; 5: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Levaux M-N, Larøi F, Malmedier M, et al. Rehabilitation of executive functions in a real-life setting: goal management training applied to a person with schizophrenia. Case Rep Psychiatry 2012; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tornås S, Løvstad M, Solbakk A-K, et al. Rehabilitation of executive functions in patients with chronic acquired brain injury with goal management training, external cuing, and emotional regulation: a randomized controlled trial. J Int Neuropsychol Soc 2016; 22: 436–452. [DOI] [PubMed] [Google Scholar]
- 82.Waid-Ebbs JK, Daly J, Wu SS, et al. Response to goal management training in veterans with blast-related mild traumatic brain injury. J Rehabil Res Dev 2014; 51: 1555–1566. [DOI] [PubMed] [Google Scholar]
- 83.Stubberud J, Langenbahn D, Levine B, et al. Goal management training improves everyday executive functioning for persons with spina bifida: self-and informant reports six months post-training. Neuropsychol Rehabil 2014; 24: 26–60. [DOI] [PubMed] [Google Scholar]
- 84.Levine B, Dt S, Winocur G, et al. Cognitive rehabilitation in the elderly: effects on strategic behavior in relation to goal management. J Int Neuropsychol Soc Epub ahead of print 13 December 2006; 13. 10.1017/s1355617707070178 [DOI] [PubMed] [Google Scholar]
- 85.Bertens D, Kessels RPC, Fiorenzato E, et al. Do old errors always lead to new truths? A randomized controlled trial of errorless goal management training in brain-injured patients. J Int Neuropsychol Soc 2015; 21: 639–649. [DOI] [PubMed] [Google Scholar]
- 86.Stubberud J, Langenbahn D, Levine B, et al. Goal management training of executive functions in patients with spina bifida: a randomized controlled trial. J Int Neuropsychol Soc 2013; 19: 672–685. [DOI] [PubMed] [Google Scholar]
- 87.Haley KL, Cunningham KT, Barry J, et al. Collaborative goals for communicative life participation in aphasia: the FOURC model. Am J Speech-Lang Pathol 2019; 28: 1–13. [DOI] [PubMed] [Google Scholar]
- 88.Doig E, Prescott S, Fleming J, et al. Reliability of the client-centeredness of goal setting (C–COGS) scale in acquired brain injury rehabilitation. Am J Occup Ther 2016; 70: 7004290010p1. [DOI] [PubMed] [Google Scholar]
- 89.Teal CR, Haidet P, Balasubramanyam AS, et al. Measuring the quality of patients’ goals and action plans: development and validation of a novel tool. BMC Med Inform Decis Mak Epub ahead of print December 2012; 12. 10.1186/1472-6947-12-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.D’Cruz K, Unsworth C, Roberts K, et al. Engaging patients with moderate to severe acquired brain injury in goal setting. Int J Ther Rehabil 2016; 23: 20–31. [Google Scholar]
- 91.Clarke SP, Crowe TP, Oades LG, et al. Do goal-setting interventions improve the quality of goals in mental health services? Psychiatr Rehabil J 2009; 32: 292–299. [DOI] [PubMed] [Google Scholar]
- 92.Brunelli C, Bianchi E, Murru L, et al. Italian validation of the Purpose In Life (PIL) test and the Seeking Of Noetic Goals (SONG) test in a population of cancer patients. Support Care Cancer 2012; 20: 2775–2783. [DOI] [PubMed] [Google Scholar]
- 93.Vermunt NPCA, Harmsen M, Westert GP, et al. Collaborative goal setting with elderly patients with chronic disease or multimorbidity: a systematic review. BMC Geriatr Epub ahead of print 31 July 2017; 17. http://dx.doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Elston A, Barnden R, Hersh D, et al. Developing person-centred goal setting resources with and for people with aphasia: a multi-phase qualitative study. Aphasiology 2021; 36(7): 761–780. [Google Scholar]
- 95.Roe D, Brown T, Thyer L. Validity, responsiveness, and perceptions of clinical utility of the Canadian occupational performance measure when used in a sub-acute setting. Disabil Rehabil 2019; 42: 1–18. [DOI] [PubMed] [Google Scholar]
- 96.Olson CM, Strawderman MS, Graham ML. Use of an online diet goal-setting tool: relationships with gestational weight gain. J Nutr Educ Behav 2019; 51: 391–399. [DOI] [PubMed] [Google Scholar]
- 97.Kuipers P, Foster M, Carlson G, et al. Classifying client goals in community-based ABI rehabilitation: a taxonomy for profiling service delivery and conceptualizing outcomes. Disabil Rehabil 2003; 25: 154–162. [DOI] [PubMed] [Google Scholar]
- 98.Dekker J, de Groot V, ter Steeg AM, et al. Setting meaningful goals in rehabilitation: rationale and practical tool. Clin Rehabil 2020; 34: 3–12. [DOI] [PubMed] [Google Scholar]
- 99.Littooij E, Doodeman S, Holla J, et al. Setting meaningful goals in rehabilitation: a qualitative study on the experiences of clients and clinicians in working with a practical tool. Clin Rehabil 2022; 36: 415–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ishikawa T, Tomori K, Nagayama H, et al. The occupational experience helps to express the clients’ occupational needs in goal setting: a retrospective study in subacute care setting. Occup Ther Health Care 2021; 36(4): 408–421. [DOI] [PubMed] [Google Scholar]
- 101.Rose A, Rosewilliam S, Soundy A. Shared decision making within goal setting in rehabilitation settings: a systematic review. Patient Educ Couns 2017; 100: 65–75. [DOI] [PubMed] [Google Scholar]
- 102.Saeidi Borujeni M, Hosseini SA, Akbarfahimi N, et al. Cognitive orientation to daily occupational performance approach in adults with neurological conditions: a scoping review. Med J Islam Repub Iran 2019; 33: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Polatajko HJ, McEwen SE, Ryan JD, et al. Pilot randomized controlled trial investigating cognitive strategy use to improve goal performance after stroke. Am J Occup Ther 2012; 66: 104–109. [DOI] [PubMed] [Google Scholar]
- 104.Šuc L, Švajger A, Bratun U. Goal setting among experienced and novice occupational therapists in a rehabilitation center. Can J Occup Ther 2020; 87: 287–297. [DOI] [PubMed] [Google Scholar]
- 105.Poulsen AA, Ziviani J, Kotaniemi K, et al. ‘I think I can’: measuring confidence in goal pursuit. Br J Occup Ther 2014; 77: 64–66. [Google Scholar]
- 106.Knutti K, Björklund Carlstedt A, Clasen R, et al. Impacts of goal setting on engagement and rehabilitation outcomes following acquired brain injury: a systematic review of reviews. Disabil Rehabil 2020; 44(12): 2581–2590. [DOI] [PubMed] [Google Scholar]
- 107.Richard LF, Knis-Matthews L. Are we really client-centered? Using the Canadian occupational performance measure to see how the client’s goals connect with the goals of the occupational therapist. Occup Ther Ment Health 2010; 26: 51–66. [Google Scholar]
- 108.Clare L, Linden DEJ, Woods RT, et al. Goal-oriented cognitive rehabilitation for people with early-stage Alzheimer disease: a single-blind randomized controlled trial of clinical efficacy. Am J Geriatric Psychiatry: Off J Am Assoc Geriatric Psychiatry 2010; 18: 928–939. [DOI] [PubMed] [Google Scholar]
- 109.Waddell KJ, Birkenmeier RL, Bland MD, et al. An exploratory analysis of the self-reported goals of individuals with chronic upper-extremity paresis following stroke. Disabil Rehabil 2016; 38: 853–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Donnelly C, Eng JJ, Hall J, et al. Client-centred assessment and the identification of meaningful treatment goals for individuals with a spinal cord injury. Spinal Cord 2004; 42: 302–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Harris JE, Eng JJ. Goal priorities identified through client-centred measurement in individuals with chronic stroke. Physiother Can 2004; 56: 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Parsons JGM, Plant SE, Slark J, et al. How active are patients in setting goals during rehabilitation after stroke? A qualitative study of clinician perceptions. Disabil Rehabil 2018; 40: 309–316. [DOI] [PubMed] [Google Scholar]
- 113.Jogie P, Rahja M, Berg M, et al. Goal setting for people with mild cognitive impairment or dementia in rehabilitation: a scoping review. Aust Occup Ther J Epub ahead of print 3 August 2021; 68. 10.1111/1440-1630.12758 [DOI] [PubMed] [Google Scholar]
- 114.Prescott S, Fleming J, Doig E. Goal setting approaches and principles used in rehabilitation for people with acquired brain injury: a systematic scoping review. Brain Inj 2015; 29: 1515–1529. [DOI] [PubMed] [Google Scholar]
- 115.Sathe NA, Polacek C, Christopher R, et al. Evaluation of the functional goal-setting and self-management tool for osteoarthritis, a patient-centred tool to improve osteoarthritis care. Musculoskeletal Care 2021; 20(2): 396–402. [DOI] [PubMed] [Google Scholar]
- 116.Scobbie L, Duncan EAS, Brady MC, et al. Facilitators and ‘deal breakers’: a mixed methods study investigating implementation of the Goal setting and action planning (G-AP) framework in community rehabilitation teams. BMC Health Serv Res Epub ahead of print 25 August 2020; 20. 10.1186/s12913-020-05651-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Scobbie L, Wyke S, Dixon D, et al. Theory-based approach to goal setting. Physikalische Medizin, Rehabilitationsmedizin, Kurortmedizin Epub ahead of print 10 June 2015; 25. 10.1055/s-0035-1554826 [DOI] [Google Scholar]
- 118.Lewis V, Dell L, Matthews L. Evaluating the feasibility of goal attainment scaling as a rehabilitation outcome measure for veterans. J Rehabil Med 2013; 45: 403–409. [DOI] [PubMed] [Google Scholar]
- 119.Payne C, Allee T. Goal achievement provides new insights into interstitial cystitis/painful bladder syndrome symptoms and outcomes. Neurourol Urodyn 2009; 28: 13–17. [DOI] [PubMed] [Google Scholar]
- 120.Ruble L, McGrew JH, Toland MD. Goal attainment scaling as an outcome measure in randomized controlled trials of psychosocial interventions in autism. J Autism Dev Disord 2012; 42: 1974–1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tennant A. Goal attainment scaling: current methodological challenges. Disabil Rehabil 2007; 29: 1583–1588. [DOI] [PubMed] [Google Scholar]
- 122.Mastos M, Miller K, Eliasson AC, et al. Goal-directed training: linking theories of treatment to clinical practice for improved functional activities in daily life. Clin Rehabil 2007; 21: 47–55. [DOI] [PubMed] [Google Scholar]
- 123.Gould KR, Feeney TJ, Hicks AJ, et al. Individualized goal attainment scaling during a trial of positive behaviour support in adults with acquired brain injury. Neuropsychol Rehabil 2021; 32(9): 2392–2410. [DOI] [PubMed] [Google Scholar]
- 124.Krasny-Pacini A, Evans J, Sohlberg MM, et al. Proposed criteria for appraising goal attainment scales used as outcome measures in rehabilitation research. Arch Phys Med Rehabil 2016; 97: 157–170. [DOI] [PubMed] [Google Scholar]
- 125.Behn N, Marshall J, Togher L, et al. Setting and achieving individualized social communication goals for people with acquired brain injury (ABI) within a group treatment. Int J Lang Commun Disord 2019; 54: 828–840. [DOI] [PubMed] [Google Scholar]
- 126.Chester H, Beresford R, Clarkson P, et al. The Dementia Early Stage Cognitive Aids New Trial (DESCANT) intervention: a goal attainment scaling approach to promote self-management. Int J Geriatr Psychiatry 2021; 36: 784–793. [DOI] [PubMed] [Google Scholar]
- 127.Peckham RH. Uses of individualized client goals in the evaluation of drug and alcohol programs. Am J Drug Alcohol Abuse 1977; 4: 555–570. [DOI] [PubMed] [Google Scholar]
- 128.Barclay DA. Family functioning, psychosocial stress, and goal attainment in brain injury rehabilitation. J Soc Work Disabil Rehabil 2013; 12: 159–175. [DOI] [PubMed] [Google Scholar]
- 129.Abu Tariah H, Aljehani AS, Alenazi DY, et al. Occupational therapy goal achievement for people with stroke: a retrospective study. Occup Ther Int 2020; 2020: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Cabrera-Martos I, Ortiz-Rubio A, Torres-Sánchez I, et al. A randomized controlled study of whether setting specific goals improves the effectiveness of therapy in people with Parkinson’s disease. Clin Rehabil 2019; 33: 465–472. [DOI] [PubMed] [Google Scholar]
- 131.Morrow-Howell N, Yip AM, Gorman MC, et al. A standardized menu for goal attainment scaling in the care of frail elders. Gerontologist 1998; 38: 735–742. [DOI] [PubMed] [Google Scholar]
- 132.Clarkson K, Barnett N. Goal attainment scaling to facilitate person-centred, medicines-related consultations. Eur J Hosp Pharm 2020; 28(2): 106–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rockwood K. Goal setting and attainment in Alzheimer’s disease patients treated with donepezil. J Neurol Neurosurg Psychiatry 2002; 73: 500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Stuifbergen AK, Becker H, Timmerman GM, et al. The use of individualized goal setting to facilitate behavior change in women with multiple sclerosis. J Neurosci Nurs 2003; 35: 94–99. [DOI] [PubMed] [Google Scholar]
- 135.Moorhouse P, Theou O, Fay S, et al. Treatment in a Geriatric Day Hospital improve individualized outcome measures using goal attainment scaling. BMC Geriatr Epub ahead of print 7 January 2017; 17. 10.1186/s12877-016-0397-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Rockwood K, Joyce B, Stolee P. Use of goal attainment scaling in measuring clinically important change in cognitive rehabilitation patients. J Clin Epidemiol 1997; 50: 581–588. [DOI] [PubMed] [Google Scholar]
- 137.Rockwood K, Stolee P, FoxP RA. Use of goal attainment scaling in measuring clinically important change in the frail elderly. J Clin Epidemiol 1993; 46: 1113–1118. [DOI] [PubMed] [Google Scholar]
- 138.Stefanac S, Oppenauer C, Zauner M, et al. From individualised treatment goals to personalised rehabilitation in osteoarthritis: a longitudinal prospective mapping study using the WHO international classification for functioning, disability and health. Ann Med 2022; 54: 2804–2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Khullar V, Espuna-Pons M, Marschall-Kehrel D, et al. Clinical value of a patient-reported goal-attainment measure: the global development of self-assessment goal achievement (SAGA) questionnaire for patients with lower urinary tract symptoms. Neurourol Urodyn 2014; 33: 90–94. [DOI] [PubMed] [Google Scholar]
- 140.McCue M, Parikh SV, Mucha L, et al. Adapting the goal attainment approach for major depressive disorder. Neurol Ther 2019; 8: 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Turner-Stokes L, Jacinto J, Fheodoroff K, et al. Assessing the effectiveness of upper-limb spasticity management using a structured approach to goal-setting and outcome measurement: first cycle results from the Upper Limb International Spasticity-III study. J Rehabil Med 2020; 53(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tang Yan HS, Clemson LM, Jarvis F, et al. Goal setting with caregivers of adults in the community: a mixed methods systematic review. Disabil Rehabil 2014; 36: 1943–1963. [DOI] [PubMed] [Google Scholar]
- 143.Stewart V, McMillan SS, Hu J, et al. Goal planning in mental health service delivery: a systematic integrative review. Front Psychiatry Epub ahead of print 19 December 2022; 13. 10.3389/fpsyt.2022.1057915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.McPherson KM, Kayes N, Weatherall M. A pilot study of self-regulation informed goal setting in people with traumatic brain injury. Clin Rehabil 2009; 23: 296–309. [DOI] [PubMed] [Google Scholar]
- 145.Giguère-Rancourt A, Plourde M, Doiron M, et al. Goal management training ® home-based approach for mild cognitive impairment in Parkinson’s disease: a multiple baseline case report. Neurocase 2018; 24: 276–286. [DOI] [PubMed] [Google Scholar]
- 146.Krasny-Pacini A, Chevignard M, Evans J. Goal management training for rehabilitation of executive functions: a systematic review of effectivness in patients with acquired brain injury. Disabil Rehabil 2014; 36: 105–116. [DOI] [PubMed] [Google Scholar]
- 147.Coffey L, Gallagher P, Desmond D. A prospective study of the importance of life goal characteristics and goal adjustment capacities in longer term psychosocial adjustment to lower limb amputation. Clin Rehabil 2014; 28: 196–205. [DOI] [PubMed] [Google Scholar]
- 148.Bakas T, Jones H, Israel J, et al. Designing and evaluating a goal-setting tip sheet for stroke family caregiver health. Rehabil Nurs 2021; 46(5): 279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Scobbie L, Dixon D, Wyke S. Goal setting and action planning in the rehabilitation setting: development of a theoretically informed practice framework. Clin Rehabil 2011; 25: 468–482. [DOI] [PubMed] [Google Scholar]
- 150.Gaffney E, Gaffney K, Bartleson L, et al. Goal attainment scaling made easy with an app. Pediatr Phys Ther 2019; 31: 225–230. [DOI] [PubMed] [Google Scholar]
- 151.Karsdorp PA, Vlaeyen JWS. Goals matter: both achievement and pain-avoidance goals are associated with pain severity and disability in patients with low back and upper extremity pain. Pain 2011; 152: 1382–1390. [DOI] [PubMed] [Google Scholar]
- 152.Peñacoba C, López-Gómez I, Pastor-Mira MA, et al. Contextualizing goal preferences in fear-avoidance models. Looking at fatigue as a disabling symptom in fibromyalgia patients. PLOS One 2021; 16: e0254200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Dutzi I, Schwenk M, Kirchner M, et al. ‘What would you like to achieve?’ Goal-setting in patients with dementia in geriatric rehabilitation. BMC Geriatr Epub ahead of print 22 October 2019; 19. 10.1186/s12877-019-1296-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Worrall L, Sherratt S, Rogers P, et al. What people with aphasia want: their goals according to the ICF. Aphasiology 2011; 25: 309–322. [Google Scholar]
- 155.Rauch A, Cieza A, Stucki G. How to apply the international classification of functioning, disability and health (ICF) for rehabilitation management in clinical practice. Eur J Phys Rehabil Med 2008; 44: 329–342. [PubMed] [Google Scholar]
- 156.Haas B, Playford ED, Ahmad AQ, et al. Rehabilitation goals of people with spinal cord injuries can be classified against the international classification of functioning, disability and health core set for spinal cord injuries. Spinal Cord 2016; 54: 324–328. [DOI] [PubMed] [Google Scholar]
- 157.Harty M, Griesel M, van der Merwe A. The ICF as a common language for rehabilitation goal-setting: comparing client and professional priorities. Health Qual Life Outcomes 2011; 9: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Helm-Estabrooks N, Whiteside J. Use of life interests and values (LIV) cards for self-determination of aphasia rehabilitation goals. Perspect Neurophysiol Neurogenic Speech Lang Disord 2012; 22: 6. [Google Scholar]
- 159.Katz N, Keren N. Effectiveness of occupational goal intervention for clients with schizophrenia. Ame J Occup Ther 2011; 65: 287–296. [DOI] [PubMed] [Google Scholar]
- 160.Vizzotto A, Celestino D, Buchain P, et al. Occupational goal intervention method for the management of executive dysfunction in people with treatment-resistant schizophrenia: a randomized controlled trial. Am J Occup Ther 2021; 75: 7503180050p1. [DOI] [PubMed] [Google Scholar]
- 161.Stevens A, Moser A, Köke A, et al. The patient’s perspective of the feasibility of a patient-specific instrument in physiotherapy goal setting: a qualitative study. Patient Prefer Adherence 2016; 425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Manhas KP, Olson K, Churchill K, et al. Measuring shared decision-making and collaborative goal setting in community rehabilitation: a focused ethnography using cross-sectional surveys in Canada. BMJ Open 2020; 10: e034745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Valentiner LS, Thorsen IK, Kongstad MB, et al. Effect of ecological momentary assessment, goal-setting and personalized phone-calls on adherence to interval walking training using the InterWalk application among patients with type 2 diabetes – a pilot randomized controlled trial. PLOS ONE 2019; 14: e0208181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Alexanders J, Perry J, Douglas C. Goal setting practices used within anterior cruciate ligament rehabilitation: an exploration of physiotherapists understanding, training and experiences. Musculoskeletal Care Epub ahead of print 11 January 2021; 19. 10.1002/msc.1535 [DOI] [PubMed] [Google Scholar]
- 165.Klein LM, Young D, Feng D, et al. Increasing patient mobility through an individualized goal-centered hospital mobility program: a quasi-experimental quality improvement project. Nurs Outlook 2018; 66: 254–262. [DOI] [PubMed] [Google Scholar]
- 166.Whitehead L, Glass C, Coppell K. The effectiveness of goal setting on glycaemic control for people with type 2 diabetes and prediabetes: a systematic review and meta-analysis. J Adv Nurs 2021; 78(5): 1212–1227. [DOI] [PubMed] [Google Scholar]
- 167.Ogbeiwi O. Theoretical frameworks for project goal-setting: a qualitative case study of an organisational practice in Nigeria. Int J Health Plann Manage 2022; 37(4): 2328–2344. [DOI] [PubMed] [Google Scholar]
- 168.Thomson C, Black L. An exploratory study of the differences between unidisciplinary and multidisciplinary goal setting in acute therapy services. Br J Occup Ther 2008; 71: 422–426. [Google Scholar]
- 169.Elzubeir K, Dye S. Can amount and duration of seclusion be reduced in psychiatric intensive care units by agreeing SMART goals with patients? J Psychiatric Intensive Care 2017; 13: 109–116. [Google Scholar]
- 170.Gardner T, Refshauge K, McAuley J, et al. Combined education and patient-led goal setting intervention reduced chronic low back pain disability and intensity at 12 months: a randomised controlled trial. Br J Sports Med 2019; 53(22): 1424–1431. [DOI] [PubMed] [Google Scholar]
- 171.Hartigan I. Goal setting in stroke rehabilitation: part 1. Br J Neurosci Nurs 2012; 8: 65–69. [Google Scholar]
- 172.Wissel J, Ri S. Assessment, goal setting, and botulinum neurotoxin a therapy in the management of post-stroke spastic movement disorder: updated perspectives on best practice. Expert Rev Neurother 2022; 22: 27–42. [DOI] [PubMed] [Google Scholar]
- 173.Crumbaugh JC. The seeking of noetic goals test (SONG): a complementary scale to the purpose in life test (PIL). J Clin Psychol 1977; 33: 900–907. [DOI] [PubMed] [Google Scholar]
- 174.Copley JA, Nelson A, Hill AE, et al. Reflecting on culturally responsive goal achievement with indigenous clients using the Australian Therapy Outcome Measure for Indigenous Clients (ATOMIC). Aust Occup Ther J 2021; 68(5): 384–394. [DOI] [PubMed] [Google Scholar]
- 175.Lenzen SA, Daniëls R, van Bokhoven MA, et al. Disentangling self-management goal setting and action planning: a scoping review. PLOS ONE 2017; 12: e0188822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Prescott S, Fleming J, Doig E. Refining a clinical practice framework to engage clients with brain injury in goal setting. Aust Occup Ther J 2019; 66(3): 313–325. [DOI] [PubMed] [Google Scholar]
- 177.Preminger J, Lind C. Assisting communication partners in the setting of treatment goals: the development of the goal sharing for partners strategy. Semin Hear 2012; 33: 053–064. [Google Scholar]
- 178.Ylvisaker M, Mcpherson K, Kayes N, et al. Metaphoric identity mapping: facilitating goal setting and engagement in rehabilitation after traumatic brain injury. Neuropsychol Rehabil 2008; 18: 713–741. [DOI] [PubMed] [Google Scholar]
- 179.Nicholas M, Jennelle L, Connor LT, et al. Do caregiver proxy reports and congruence of client–proxy activity participation goals relate to quality of life in people with aphasia? Int J Lang Commun Disord 2020; 55(3): 373–386. [DOI] [PubMed] [Google Scholar]
- 180.Byrnes M, Beilby J, Ray P, et al. Patient-focused goal planning process and outcome after spinal cord injury rehabilitation: quantitative and qualitative audit. Clin Rehabil 2012; 26: 1141–1149. [DOI] [PubMed] [Google Scholar]
- 181.Turner-Stokes L, Rose H, Lakra C, et al. Goal-setting and attainment in prolonged disorders of consciousness – development of a structured approach. Brain Inj 2019; 34: 78–88. [DOI] [PubMed] [Google Scholar]
- 182.COPM July 2019 Newsletter, https://mailchi.mp/b210297e28d2/copm-july-2019-newsletter-2302113 (2019, accessed 15 June 2023).
- 183.Leonardi M, Fheodoroff K. Goal setting with ICF (international classification of functioning, disability and health) and multidisciplinary team approach in stroke rehabilitation. Clin Pathways Stroke Rehabil 2021: 35–56. [PubMed] [Google Scholar]
- 184.Rohde A, Townley-O’Neill K, Trendall K, et al. A comparison of client and therapist goals for people with aphasia: a qualitative exploratory study. Aphasiology 2012; 26: 1298–1315. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-cre-10.1177_02692155231197383 for Characteristics of goal-setting tools in adult rehabilitation: A scoping review by Yuho Okita, Yuko Kawaguchi, Yuki Inoue, Kanta Ohno, Tatsunori Sawada, William Levack and Kounosuke Tomori in Clinical Rehabilitation
Supplemental material, sj-docx-2-cre-10.1177_02692155231197383 for Characteristics of goal-setting tools in adult rehabilitation: A scoping review by Yuho Okita, Yuko Kawaguchi, Yuki Inoue, Kanta Ohno, Tatsunori Sawada, William Levack and Kounosuke Tomori in Clinical Rehabilitation
Supplemental material, sj-pdf-3-cre-10.1177_02692155231197383 for Characteristics of goal-setting tools in adult rehabilitation: A scoping review by Yuho Okita, Yuko Kawaguchi, Yuki Inoue, Kanta Ohno, Tatsunori Sawada, William Levack and Kounosuke Tomori in Clinical Rehabilitation