Abstract
Background:
Chronic diseases such as type II diabetes place a large burden on the healthcare system and are associated with increased morbidity and mortality. A team-based multidisciplinary approach which organizes care to improve chronic disease management may actually decrease traditional continuity of care metrics. Visit Entropy (VE) provides a novel measure of care organization produced by team-based approaches. Higher VE, reflecting more disorganized care, has been associated with more hospital readmissions. We hypothesized that higher VE was also associated with reduced adherence to the D5 quality criteria.
Methods:
A retrospective study of 6,590 adult diabetic patients in five established medical home practices was conducted. Multivariate logistic regression was used to determine if VE was associated with the dependent variable of D5 control. Separate models for usual provider continuity, continuity of care index, and sequence continuity were also constructed.
Results:
Less organized care with a higher VE was associated with decreased odds of D5 control (OR=0.88, 95%CI 0.80–0.97). The other continuity measures were not significant. Age, education level, and initial HgA1c were significant covariates, but gender, race, endocrine consults, and Charlson comorbidity were not significant. The Number Needed to be Exposed to more organized care to produce one more controlled diabetic was 32.5.
Conclusions:
More organized care reflected by a lower VE is associated with improved odds of D5 diabetic control. VE represents a better measure of care organization in team based medical home environments than traditional continuity of care metrics.
Keywords: Visit Entropy, Continuity, Diabetes, Primary Care
INTRODUCTION
Chronic disease, such as type II diabetes, places a significant burden on the healthcare system within the United States. Diabetes has an estimated prevalence of 12% within the US adult population.[1] A diagnosis of type II diabetes confers greatly increased risk of additional morbidity and mortality due to macrovascular and microvascular disease, as well as increased healthcare costs throughout a patient’s lifetime when compared with patients who have never received a diagnosis of diabetes.[2] Interventions targeted at preventing these complications have been shown to decrease the incidence of developing diabetes-related complications.[2] Thus, the D5 was developed by the Minnesota Community Measurement organization to assess care quality in diabetic patients.[3] It consists of five treatment goals: hemoglobin A1c (HgA1c) controlled (<8.0), blood pressure controlled (<140/90), statin use (unless contraindicated), tobacco free, and aspirin or other anti-platelet therapy (unless contraindicated). Meeting all five treatment goals has been associated with lower mortality, decreased hospitalizations, and fewer emergency department visits.[4]
It is well known that patient level continuity of care, characterized by longitudinal relationships that foster communication, improve outcomes in patients with chronic diseases, including diabetes.[5–7] A majority of published studies use metrics to quantify continuity that either measure provider density (Usual Provider Continuity), sequence (Sequence of Continuity), dispersion (Continuity Of Care), or duration of visits.[7–12] The chronic disease model states that team based care directed by primary care physicians is necessary to improve outcomes.[13] Patient centered, team based care is rapidly being adopted by many primary care practices due in part to financial incentives.[14,15] Such team based care should be more organized than usual care because patients are actively directed by their primary care physician to needed resources and consults. The very nature of care teams, with inherent patient interactions involving multiple care team members, decrease longitudinal continuity as currently measured by conventional metrics.[16]
Visit entropy (VE) may provide a mechanism to characterize the quality of team care environments when conventional continuity metrics fail. VE, based on the concept of Shannon entropy from information science, quantifies the amount of unpredictability or disorganization in a patient’s previous visit pattern to clinicians and is described in detail by Garrison, et.al.[17] Because team based care is organized care, it produces a lower VE. In fact, decreased VE (i.e. more organized care) has been associated with reduced hospital readmissions in a patient-centered medical home.[18] We hypothesize that increased organization of care, measured as decreased VE, is associated with improved odds of meeting all the Minnesota D5 criteria amongst type II diabetics observed over a 3 year period.
METHODS
A retrospective cohort study of all adult diabetic patients cared for in five primary care clinics in Olmsted county, Minnesota was conducted in order to determine if continuity of care over a three year period influenced diabetic control. All five clinics are patient centered medical home practices with well established care teams. Clinicians (physicians and advanced practitioners), registered nurses, pharmacists, social workers, and panel managers work together as a care team utilizing an electronic registry to facilitate care of diabetic patients. When necessary, referrals are made to well defined groups of community specialists.
Inclusion criteria were any adult patient (age > 18 at 1/1/2015) who had at least two instances of an ICD9 or ICD10 code indicating type II diabetes mellitus and was not pregnant at any point during the three year study period of 1/1/2015 to 12/31/2017. A total of 8,107 patients who had given permission for research review of their medical records were identified from an electronic clinical registry as meeting the inclusion criteria. Of these, 228 were excluded because they had fewer than two visits of any type and another 486 were excluded because they had fewer than two HgA1c values obtained during the three year study period. Additionally, 803 subjects were 80 years or older and were excluded because diabetic treatment goals are often highly individualized in elderly patients [19].
The study was reviewed and approved by the Institutional Review Board. Data regarding the remaining 6,590 subjects was electronically abstracted from the medical record including demographics (age, gender, birthdate, race, language preference, education level), diabetic control (HgA1c values, blood pressures, statin use, tobacco use, anti-platelet therapy), Charlson comorbidities, and medical visits (visit date, clinician, specialty). The D5 metric (controlled or uncontrolled) at the conclusion of the study period was defined as our primary endpoint and dependent variable. During the study period the five elements of the D5 were defined as: HgA1c controlled (<8.0), blood pressure controlled (<140/90), statin use (unless contraindicated), tobacco free, and aspirin or other anti-platelet therapy (unless contraindicated).
The scaling constant k used for maximum likelihood estimation in the calculation of VE was chosen to be the maximum number of different clinicians seen by any of the subjects (k=102). For comparison purposes, usual provider continuity (UPC), continuity of care index (COC), and sequence continuity (SECON) were calculated as they represent other accepted measures of continuity of care. The mathematical definition of each measure is shown in Table 1 and was reviewed previously by Garrison et al.[17]
Table 1:
Continuity Metrics
| Measure | Definition |
|---|---|
| Density (UPC) |
|
| Dispersion ( COC) |
|
| Sequence (SECON) |
|
| Entropy/Disorganization (VE) |

|
Statistical analysis was carried out using R version 3.0.2.[20] The highest education level achieved was imputed from demographic data using a missing at random (MAR) assumption for 1,237 subjects who answered unknown or did not provide an answer to their education level in the medical record. Bivariate analysis was carried out using the chi square test (for categorical independent variables), Wilcoxon rank sum (for non-normally distributed continuous independent variables), or t-test (for normally distributed continuous independent variables). P-values less than 0.05 were considered significant. Multivariate logistic regression was carried out to assess the impact of the independent variables (age, gender, race, language preference, education level, Charlson comorbidity score, initial HgA1c, endocrine visits, number of visits, and Visit Entropy) on the dependent variable D5. Odds ratios and 95% confidence limits were calculated with pr(>|z|) < 0.05 considered significant.
RESULTS
A total of 6,590 subjects were analyzed, 3,210 (48.7%) of whom had a D5 that was controlled at the end of the study period. As Table 2 shows, bivariate analysis demonstrated that those with a controlled D5 were slightly older (61.7 vs 58.4 yrs, p<0.001), had more years of formal education (p<0.001), and had a lower initial HgA1c (7.2 vs. 8.0, p<0.001). They were also less likely to have seen an endocrinologist or an endocrine advanced practitioner (20.6% vs. 23.8%, p=0.002). Gender, race, primary language, Charlson comorbidities, and the total number of medical visits were not statistically different. Visit Entropy was slightly lower (3.55 vs. 3.59, p=0.03) in those with a controlled D5. COC was also slightly higher (0.151 vs. 0.145, p=0.008), but UPC and SECON were not different.
Table 2:
Bivariate Comparison Between Controlled and Uncontrolled D5 Patients
| Uncontrolled | Controlled | p-value | |
|---|---|---|---|
| N (%) | 3378 (51.3%) | 3210 (48.7%) | NA |
|
| |||
| Age, yrs mean (SD) | 58.4 (12.6) | 61.7 (11.8) | <0.001 |
|
| |||
| Gender, Female (%) | 1521 (45.0%) | 1409 (43.9%) | 0.359 |
|
| |||
| Race, Non-white (%) | 468 (13.9%) | 419 (13.1%) | 0.348 |
|
| |||
| Language, Non-english (%) | 235 (7.0%) | 190 (5.9%) | 0.088 |
|
| |||
| Education | <0.001 | ||
| Unknown |
712 (21.1%) |
524 (16.3%) |
|
| Some High School |
77 (2.3%) |
75 (2.3%) |
|
| High School or GED |
792 (23.4%) |
734 (22.9%) |
|
| Some College or 2yr degree |
1042 (30.8%) |
901 (28.1%) |
|
| College Graduate |
430 (12.7%) |
497 (15.5%) |
|
| Post-Graduate Studies |
325 (9.6%) |
479 (14.9%) |
|
|
| |||
| Charlson comorbidity, mean (SD) | 1.5 (1.2) | 1.5 (1.2) | 0.266 |
|
| |||
| Initial Hemoglobin a1c, mean (SD) | 8.0 (1.8) | 7.2 (1.4) | <0.001 |
|
| |||
| Endocrine Consult (%) | 805 (23.8%) | 661 (20.6%) | 0.002 |
|
| |||
| Total # Visits, mean (SD) | 21.4 (21.8) | 21.5 (21.6) | 0.168 |
|
| |||
| Continuity Measures | |||
| Entropy, mean, median, (SD) | 3.59, 3.59 (0.69) | 3.55, 3.56 (0.69) | 0.034 |
| UPC, mean (SD) | 0.34, 0.29 (0.20) | 0.34, 0.29 (0.19) | 0.333 |
| COC, mean (SD) | 0.14, 0.08 (0.18) | 0.15, 0.09 (0.18) | 0.008 |
| SECON, mean (SD) | 0.19, 0.13 (0.21) | 0.18, 0.13 (0.20) | 0.848 |
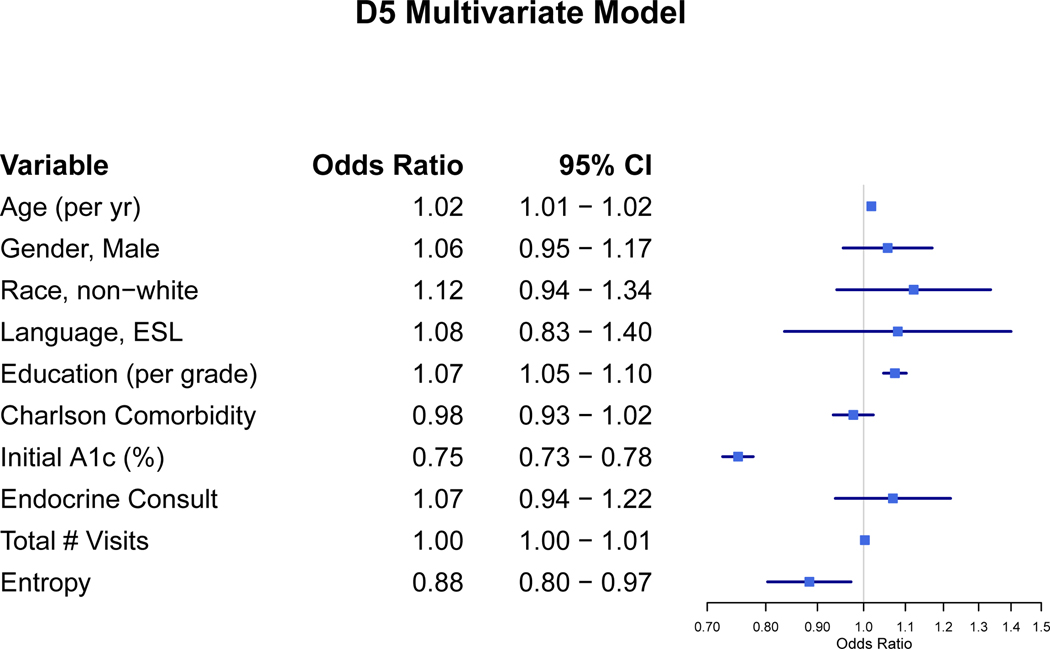
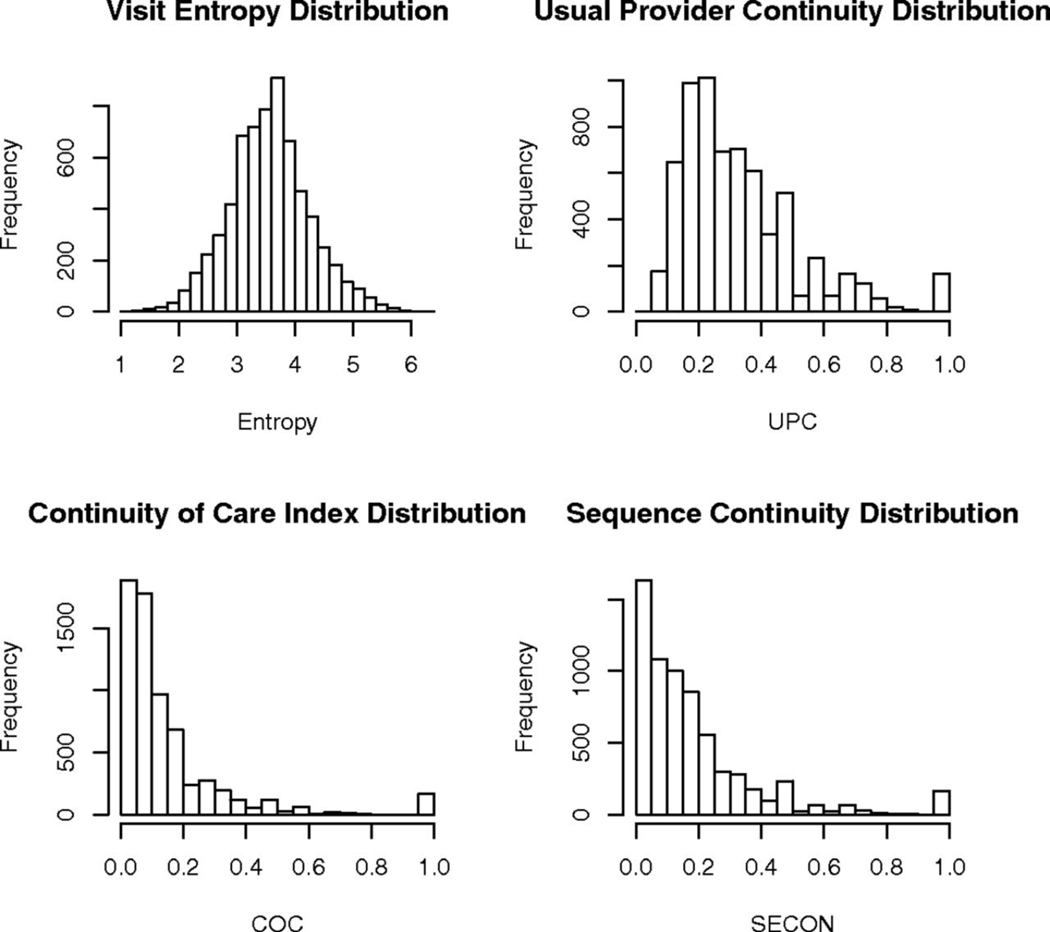
Results of the multivariate analysis are shown in Figure 1. The adjusted odds ratios for age (1.01, 95%CI 1.01–1.02), education level (1.07, 95%CI 1.05–1.10), and initial HgA1C (0.75, 95%CI 0.73–0.78) were significant. Less organized care, represented by a higher VE score, was associated with lower adjusted odds of a controlled D5 (0.88, 95%CI 0.80–0.97). Gender, race, primary language, Charlson comorbidities, presence of endocrine consults, and the total number of medical visits were not statistically significant. Additional models for UPC, COC, and SECON in place of VE as a continuity measure did not reach statistical significance (Pr(<|z|) = 0.46, 0.25, 0.90 respectively). As seen in Figure 2, these other continuity measures have highly skewed distributions when compared to VE. Using the method of Bender and Blettner for multivariate logistic regression adjusted odds, the Number Needed to be Exposed (NNE) to this more organized care to produce one more controlled D5 is 32.5 patients.[21]
Figure 1:
Factors Associated with Diabetic D5 Control
NOTE: The other continuity measures (UPC, COC, and SECON) showed non-significant odds ratios that crossed 1.0 when run in separate models.
Figure 2:
Distribution of Continuity Measures
DISCUSSION
Our results demonstrate that decreased VE is associated with increased odds of a diabetic patient meeting all of the D5 criteria (D5 controlled). This effect was independent of Charlson comorbidity score, age, education, and entry HgA1c, amongst others. VE can be thought of as quantifying the amount of predictability in a patient’s visit pattern using the prior probability distribution of that patient’s visits. A more predictable visit pattern results in a lower VE. Highly functioning care teams should produce more organized and predictable visit patterns reflected by lower VE scores for their patients. Additionally, VE can differentiate between planned referrals and unplanned subspecialty visits because unplanned visits make the visit pattern less predictable.
VE and COC (derived from Rae and Taylor’s measure of political fragmentation [22]) both quantify disorganization of care across multiple providers. However, VE is more robust as seen with the example visit patterns in Table 3. Clearly pattern A has more organization and continuity when compared to pattern B, and this is reflected in both VE and COC. VE correctly differentiates the lower continuity of Pattern D as compared to Pattern C but COC is unable to detect this difference in the number of visits to the primary physician. According to our results, the probability of a controlled D5 would be 47% lower for Pattern B or D when compared to Pattern A or C [0.88/(1+0.88) = 0.47] due to the approximately one unit change in VE.
Table 3:
Example Visit Patterns Contrasting COC and VE
| Pattern | Description | COC | VE |
|---|---|---|---|
| A | Visiting the primary MD 5 times, the care team advanced practitioner 3 times, and an endocrinologist twice. | 0.24 | 2.37 |
| B | Visiting the primary MD twice, and seeing four other clinicians a total of once each for acute visits. | 0.07 | 3.42 |
| C | Visiting only the primary MD 4 times. | 1.00 | 2.04 |
| D | Visiting only the primary MD twice. | 1.00 | 3.11 |
Other measures of continuity (COC, UPC, and SECON) did not demonstrate a similar association with controlled D5 in the multivariate model. As previously noted by Garrison et al. 2017, these measures are all highly skewed relative to VE, which is approximately normally distributed.[7] Furthermore, patients with 0, 1, or 2 visits during the study period have to be removed to prevent undefined division-by-zero errors inherently present in the other metrics. VE does not suffer from this shortcoming and remains defined even with zero visits.
Quality measures are increasingly being collected, published, and used to determine reimbursement, thus identifying office processes and care team structures that improve quality of care must be intentional within patient centered medical homes.[23] A highly functioning cohesive team with physicians, NP/PAs, pharmacists, care coordinators, and social workers should provide more predictable, organized care with a lower VE. Designing such high functioning care teams, as measured by VE, may be an important strategy to maximize quality measures for patients with diabetes.
Limitations
Because retrospective studies can only show associations, it is unclear whether interventions designed to reduce VE will lead to improved diabetic outcomes. The measured change in VE associated with beneficial results in this study was small and its magnitude depends on the choice of the scaling constant k. This study was conducted at five patient centered medical home sites within a single academic medical center, thus results may not be generalizable to community medical practices nationwide. We arbitrarily choose the D5 composite metric as our endpoint. The D5 standard in place during the study period specified statin and aspirin use unless contraindicated for all patients. The recently published ACCORD trial and American Diabetes Association guidelines may alter these recommendations in the future.[24,25] Finally, this study was focused on adults with type II diabetes and results may not be generalizable to other chronic disease states.
Conclusions
Lower VE representing more organized medical care is associated with improved diabetic control as measured by the D5.
ACKNOWLEDGMENTS
We thank Ms. Julie Maxson and Ms. Alicia Meek for coordinating data collection.
This project was supported by grant number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Support: Department of Family Medicine, Mayo Clinic, Rochester, MN This project was supported by grant number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS).
Footnotes
Conflict of Interest: None.
CONFLICT OF INTEREST STATEMENT
Author #1: none
Author #2: none
Author #3: none
Author #4: none
Contributor Information
Benjamin T. Dilger, Department of Family Medicine, Mayo Clinic.
Margaret C. Gill, Department of Family Medicine, Mayo Clinic.
Jill G. Lenhart, Department of Family Medicine, Mayo Clinic Health System.
Gregory M. Garrison, Department of Family Medicine, Mayo Clinic.
REFERENCES
- 1.National Center for Chronic Disease Prevention and Health Promotion CfDC. Estimated Diabetes Statistics Report, 2017. 2017.
- 2.Zhuo X, Zhang P, Barker L, Albright A, Thompson TJ, Gregg E. The lifetime cost of diabetes and its implications for diabetes prevention. Diabetes Care. Sep 2014;37(9):2557–2564. [DOI] [PubMed] [Google Scholar]
- 3.The D5 for Diabetes. 2014; http://mncm.org/reports-and-websites/the-d5/. Accessed May 11, 2016.
- 4.Takahashi PY, St Sauver JL, Finney Rutten LJ, et al. Health outcomes in diabetics measured with Minnesota Community Measurement quality metrics. Diabetes Metab Syndr Obes. 2015;8:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donaldson MS, Yordy KD, Lohr KN, Vanselow NA. Primary Care: America’s Health in a New Era. The National Academies Press; 1996. [PubMed] [Google Scholar]
- 6.Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract. Dec 2004;53(12):974–980. [PubMed] [Google Scholar]
- 7.Hussey PS, Schneider EC, Rudin RS, Fox DS, Lai J, Pollack CE. Continuity and the costs of care for chronic disease. JAMA internal medicine. May 2014;174(5):742–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. Sep-Oct 2003;1(3):134–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salisbury C, Sampson F, Ridd M, Montgomery AA. How should continuity of care in primary health care be assessed? Br J Gen Pract. Apr 2009;59(561):e134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dreiher J, Comaneshter DS, Rosenbluth Y, Battat E, Bitterman H, Cohen AD. The association between continuity of care in the community and health outcomes: a population-based study. Isr J Health Policy Res. May 23 2012;1(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bentler SE, Morgan RO, Virnig BA, Wolinsky FD. Do claims-based continuity of care measures reflect the patient perspective? Med Care Res Rev. Apr 2014;71(2):156–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bazemore A, Petterson S, Peterson LE, Bruno R, Chung Y, Phillips RL Jr., Higher Primary Care Physician Continuity is Associated With Lower Costs and Hospitalizations. Ann Fam Med. Nov 2018;16(6):492–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Jama. Oct 9 2002;288(14):1775–1779. [DOI] [PubMed] [Google Scholar]
- 14.Basu S, Phillips RS, Song Z, Landon BE, Bitton A. Effects of New Funding Models for Patient-Centered Medical Homes on Primary Care Practice Finances and Services: Results of a Microsimulation Model. Ann Fam Med. Sep 2016;14(5):404–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khanna N, Shaya FT, Gaitonde P, Abiamiri A, Steffen B, Sharp D. Evaluation of PCMH Model Adoption on Teamwork and Impact on Patient Access and Safety. J Prim Care Community Health. Apr 2017;8(2):77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schottenfeld L, Petersen D, Peikes D, et al. Creating Patient-Centered Team-Based Primary Care. Rockville, MD: AHRQ; March 2016. [Google Scholar]
- 17.Garrison GM, Bania B. Visit Entropy: Comparing a Novel Measure to Existing Care Measures. European Journal for Person Centered Healthcare. 2015;3:343–351. [Google Scholar]
- 18.Garrison GM, Keuseman R, Bania B, Robelia P, Pecina J. Visit Entropy Associated with Hospital Readmission Rates. J Am Board Fam Med. Jan 2 2017;30(1):63–70. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes A. 11. Older Adults: Standards of Medical Care in Diabetes-2018. Diabetes Care. Jan 2018;41(Suppl 1):S119–S125. [DOI] [PubMed] [Google Scholar]
- 20.R: A Language and Enviroment for Statistical Computing [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 21.Bender R, Blettner M. Calculating the “number needed to be exposed” with adjustment for confounding variables in epidemiological studies. J Clin Epidemiol. May 2002;55(5):525–530. [DOI] [PubMed] [Google Scholar]
- 22.Rae DWT, Michael. The Analysis of Political Cleavages. American Political Science Review. September 1971;65(3):790–792. [Google Scholar]
- 23.Centers for M, Medicaid Services HHS. Medicare program; Medicare Shared Savings Program: Accountable Care Organizations. Final rule. Federal register. Nov 2 2011;76(212):67802–67990. [PubMed] [Google Scholar]
- 24.Group ASC, Bowman L, Mafham M, et al. Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus. N Engl J Med. Oct 18 2018;379(16):1529–1539. [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes A. 10. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2019. Diabetes Care. Jan 2019;42(Suppl 1):S103–S123. [DOI] [PubMed] [Google Scholar]