Abstract
Purpose
Healthcare has a large environmental footprint, not least due to the wide use of single-use supplies. Reprocessing of medical devices is a well-established, regulated process, and can reduce its environmental impact. This life cycle assessment (LCA) compares the environmental footprint of a single-use and a reprocessed version of otherwise identical intermittent pneumatic compression (IPC) sleeves.
Materials and Methods
The LCA was performed in accordance with the international standard ISO 14044 using the Environmental Footprint 3.0 (EF) method for the assessment. Data were obtained in cooperation with IPC sleeve manufacturers. Where no primary data were available, ecoinvent database records were used. The functional unit is five hospital treatments applying IPC. The robustness of the results was interrogated in sensitivity analyses of the energy mix, the ethylene oxide emissions during reprocessing, and the transport distances. The impact of waste reduction on hospital disposal costs was calculated.
Results
The environmental footprint of reprocessed IPC sleeves was found to be reduced in all categories compared to single-use devices, leading to a weighted normalized reduction of 43% across all categories. In a breakdown of the LCA results, reprocessed IPC sleeves were found to reduce the carbon footprint by 40%, with the treatment of five patients with single-use IPC sleeves creating 7 kg CO2eq, compared to 4.2 kg CO2eq from reprocessed sleeves. Waste disposal costs were also reduced by 90%.
Conclusion
Reprocessing of IPC sleeves provides an environmental and economic benefit in comparison to single-use devices.
Keywords: circular economy, resource efficiency, equipment reuse, recycling, waste management, environmental footprint
Introduction
Healthcare is resource-intensive and generates large quantities of waste, resulting in a large environmental impact. Between 1% and 5% of the total global environmental footprint is caused by global healthcare.1 Reducing environmental impact is increasingly becoming a focus in healthcare:2 several countries have formally committed to developing the climate resilience and sustainability of their healthcare systems,3 and purchasing policies promoting environmental awareness are becoming more widespread.
A major contributor to the environmental impact of operations are single-use devices, which have been estimated to contribute between 59% and 71% of the carbon footprint of healthcare.4 In comparison, reprocessed devices have repeatedly been found to be more resource efficient, produce less waste, and have a lower environmental impact.5–8 However, confirming the existence and extent of these benefits requires a lifecycle perspective.8–10
Intermittent pneumatic compression (IPC) of the lower limbs provides mechanical prophylaxis for venous thromboembolism after surgery while avoiding the risks associated with anticoagulants used in pharmacological prophylaxis11,12 by increasing the venous blood flow in a cyclical fashion similar to ambulation.13 Kendall SCD™ sleeves for the Kendall SCD™ 700 Smart Compression™ System (Cardinal Health™) are available as either single-use (for example, type 9529) or reprocessed (for example, type 9529R) products. The difference between these products is that the single-use version is disposed of after each patient, and the reprocessed version is reprocessed after patient use and returned to the hospital.
Life cycle assessment (LCA) is a method to determine the environmental footprint and ecological impact of a product throughout its life cycle. This LCA compares a single-use and reprocessed version of a medical device. It considers the resources needed for manufacture and assembly and the environmental impact of reprocessing and distribution, which can be deciding factors in determining sustainability.6,8–10
In this study, we aimed to compare single-use and reprocessed IPC sleeves in an LCA to determine whether reprocessed sleeves offer an environmental advantage. This can be a compelling consideration in the device selection process given the efforts to reduce the environmental impact of healthcare.
Materials and Methods
This LCA is based on four phases in accordance with the international standard ISO 14044: the goal and scope, the life cycle inventory, the impact assessment, and the interpretation.14
Goal and Scope
The aim of this study is to compare the ecological footprint of two IPC sleeves. Type “9529” is a single-use sleeve and “9529R” is its reprocessed counterpart. The product itself is the same for both systems: single-use IPC sleeves are discarded after use whereas reprocessed devices are cleaned, tested, inspected, high-level disinfected, packaged, and then sold back to hospitals.
In this project we consider the entire life cycle of the IPC sleeves. The system operates in North and Central America. Primary data refer to the year 2021. There is no allocation task, as there are no recycling loops, ecological credits, or by-products. We analyze the direct contract distribution system run by the manufacturer. Following the standard, we cut off several inputs that contain less than 1% of the mass of the product system. Additionally, the product components controller and tubing set were not part of this analysis, as they are used multiple times and so their environmental effect is neglectable
Functional Unit
The functional unit of this study is defined as five hospital IPC treatments, corresponding to five pairs of single-use IPC sleeves and one pair of reprocessed IPC sleeves that is reprocessed four times.
Description of the System–Life Cycle Inventory
The life cycle inventory lists and quantifies all in- and outputs of the system in a sufficient quality and accuracy. The setup of the life cycle inventory was an iterative process with the manufacturer that led to a realistic model of the life cycle. The material composition of an IPC sleeve (single-use and reprocessed) is listed in Table 1. The product is the same for the single-use and the reprocessed system.
Table 1.
Material Composition of Single-Use and Reprocessed IPC Sleeves
| Component | Material | Mass [g] |
|---|---|---|
| One top and one bottom sheet | Non-woven polyester | 82 |
| 3 Velcro hook attachments to the bottom sheet | Nylon | 3 |
| 3 Velcro loops attachments to the top sheet | Nylon | 12 |
| 3 ports attached to the top sheet | PVC | 2 |
| One connector plug | ABS | 4 |
| One gasket | PVC | 1 |
| 3 tubes | Soft PVC | 8 |
| Product weight total | Total | 111 |
Abbreviations: ABS, Acrylonitrile Butadiene Styrene; PVC, Polyvinyl chloride.
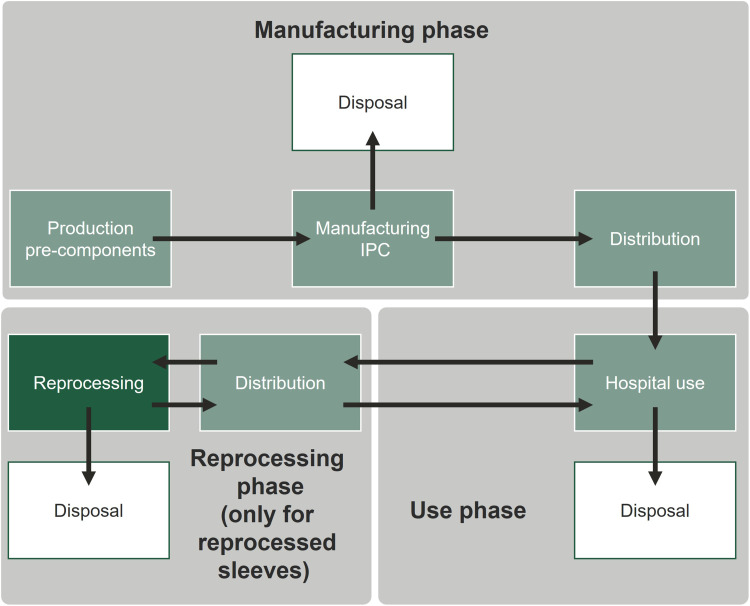
Process Flowchart
The flow chart in Figure 1 shows a simplified model of the life cycle of IPC sleeves (single-use and reprocessed). The pre-components for IPC sleeves are produced in North America, then transported to the manufacturing facility in Costa Rica. The packaged IPC sleeves are distributed via 35 replenishment and/or distribution centers to hospitals across the US (manufacturing phase). After the hospital treatment, the IPC sleeves are either discarded or collected for reprocessing (use phase). The used devices are transported to the reprocessing facility in Florida. After successful reprocessing, the devices are packaged and distributed back to hospitals who opt in to reprocessing (reprocessing phase).
Figure 1.
Overview of the life cycle of IPC sleeves in the three phases: manufacturing, use phase and reprocessing (for the reprocessed IPC sleeve only).
To prepare the inventory for the assessment, a detailed process model including individual process steps for the single-use and reprocessed product systems was elaborated. The model allows linear scale up of the LCA results, based on the functional unit.
Single-Use System Including Production
The IPC sleeves are produced in a manufacturing facility in Costa Rica with an overall energy consumption of 3,527,600 kWh. The state electricity mix of Costa Rica was derived from an ecoinvent dataset.15 Packaging consists of one bag for two products, a cardboard box for five poly bags, and the respective share of transport packaging (wooden pallet, chipboard, corrugated cover, and shrinking foil). Waste at the facility is collected and sent to recycling (paper, cardboard) or landfills.
The manufactured products are transported from Costa Rica to the replenishment center in Georgia, USA. From there, the product is distributed via distribution centers to hospitals across the US. For the transport model, the average distances between the replenishment centers, distribution centers, reprocessing facility, and hospitals was calculated. Finally, the used item is collected at the hospital and disposed of in a landfill or incinerated.
Reprocessing System
The used reprocessed product is collected at the hospitals and transported to the reprocessing facility in Florida. The product is sorted, cleaned, inspected, and tested for functional performance. The packaging of reprocessed IPC sleeves is identical to that of single-use devices.16 The sleeves undergo high-level disinfection using ethylene oxide (ETO).17 The sleeves are then distributed via replenishment and distribution centers to hospitals for reuse. Waste that occurs in Florida is sent to a waste incineration facility. The electricity demand was calculated to be 0.251 kWh per reprocessed sleeve. The primary mix of the electricity source for the reprocessing plant was modeled with ecoinvent datasets15 following the information in the bills of the provider for this facility: 78% natural gas, 13% purchased power, 5% solar power, and 4% coal. The following numbers of necessary products were identified to fulfill the functional unit:
To perform five hospital compression treatments with the single-use IPC sleeves, five primary products are used. Losses occur during the primary production and manufacturing were considered as additional inputs (raw materials, energy).
To perform five hospital treatments within the reprocessed IPC sleeves, 1.22 primary products are used (0.22 primary products arise from losses during reprocessing).
Assumptions Along the Life Cycle
Despite all efforts, some primary data were not available. Thus, assumptions were made based on production data, a site visit, general process descriptions, and scientific literature.
Ecological Footprints of the raw material production and production services (the technologies used) to manufacture the IPC sleeves are modeled using ecoinvent 3.8 datasets.15 Furthermore, we applied datasets for the inventory of transport means, electricity products, and waste treatment technologies. The ecoinvent database supports LCA experts by providing high quality datasets covering a diverse range of sectors at both a global and regional level.18 Its application increases the credibility and acceptance of the LCA results.
Life Cycle Impact Assessment
The core assessment method used for the impact assessment was the Environmental Footprint 3.0 (EF) method as described.19,20 The environmental impact of the product is categorized in 16 different categories (in alphabetical order): Carcinogenic effects (CTUh), Climate change (kg CO2-Eq), Fossils (MJ), Freshwater and terrestrial acidification (mol H+-Eq), Freshwater ecotoxicity (CTUe), Freshwater eutrophication (kg P-Eq), Ionizing radiation (kg U235-Eq), Land use (points), Marine eutrophication (kg N-Eq), Minerals and metals (kg Sb-Eq), Non-carcinogenic effects (CTUh), Ozone layer depletion (kg CFC-11-Eq), Photochemical ozone creation (kg NMVOC-Eq), Respiratory effects, Inorganics (disease incidences), Terrestrial eutrophication (mol N-Eq) and Water scarcity (m3 world-Eq).
Model and data were developed and processed by the software “Umberto” (iPoint-systems GmbH, Germany, 2023), which is linked with database ecoinvent 3.815 to obtain data on the environmental footprint of the material production and resources used in the product lifecycles.
In order to verify the results of the model, assessment methods included the ReCiPe (2008), UBP (2013), and CML (2016) methods. The direction of the results was the same for all methods applied; therefore, the EF 3.0 method was supported and only the results of the EF 3.0 method are reported in this article.
Normalization and weighting of the results allowed us to characterize the relevance of the impact to the categories. We used the global normalization factors set up by the European Joint Research Center.21 Finally, beyond the standard requirements of an LCA, we applied a weighting process that entails multiplying the normalized results of each impact category with a weighting factor representing societal values and expressed as µ-points. The Joint Research Center defined a set of weighting factors for all impact categories.22
Costs of Waste Disposal
We used the waste generated by IPC sleeves (including packaging waste, pre-components and material waste, losses, and reject within the primary production and the reprocessing) to compare hospital waste disposal costs for the single-use versus reprocessed IPC sleeves. The waste associated with the production of the pre-components was not included. We assumed that 90% of the waste is non-hazardous and the remaining 10% is contaminated, hazardous waste (highly contaminated products are not reprocessed). Waste disposal costs were taken from published literature and are presented in 2022 USD. Three studies23–25 report hospital waste disposal costs in the US, with a median cost per ton of $151.07 (range $97.73; $8148.05) for non-hazardous waste and $32,340.72 ($1294.33; $63,387.11) for hazardous waste.
Sensitivity Analysis
A sensitivity analysis was performed to identify the most influential inputs and to evaluate potential uncertainties. Therefore, scenarios were built by changing specific parameters and comparing the results to the initial scenario. The following four parameters were identified as matters of concern: Scenario 1 changed the energy mix of electricity in the reprocessing facility to a 100% renewable energy mix to look at energy related reduction potentials. Scenario 2 scaled up the ETO emissions during high-level disinfection. Scenario 3 extended transport distances by 50% in both product systems to address uncertainties in the assumptions of the transport model. Scenario 4 reduced the transports related to reprocessing by 50%.
Results
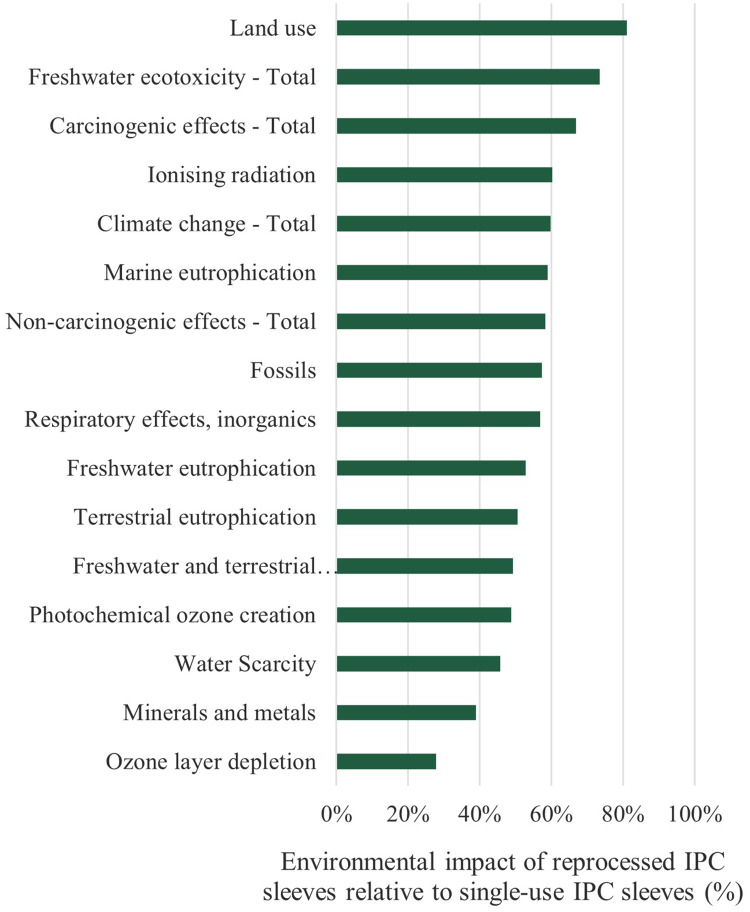
Environmental Impact
In comparison to single-use IPC sleeves, reprocessed IPC sleeves reduce the environmental footprint across all impact categories analyzed in the EF 3.0 methodology (Figure 2). The reduction is largest in the categories “Ozone layer depletion” (−72.1%), ‘Minerals and metals’ (−61.1%), and “Water scarcity” (−54.3%). All impact categories show a reduction of more than −30% except for “Freshwater ecotoxicity” (−26.6%) and “Land use” (−19.0%), where the benefit provided by reprocessed IPC sleeves is smallest.
Figure 2.
Contribution to environmental effects shown in percent of maximum impact in each category for reprocessed compared to single-use IPC sleeves.
The biggest contribution to the environmental footprint of both the single-use and reprocessed IPC sleeves arises from the cardboard box (needed packaging for shipping and storage) and the production of the sheet (main component for the primary production of the IPC sleeves). The third largest contributors are the transports for single-use products and the electricity for reprocessed devices.
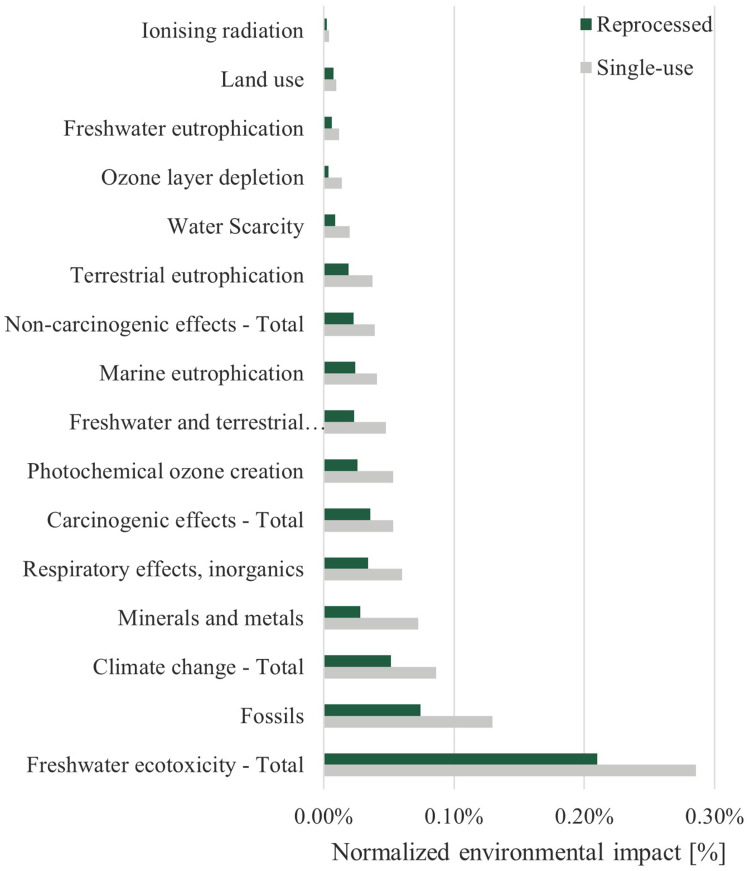
Normalized Environmental Impact
The results of the environmental impact analysis were normalized by multiplying them with global normalization factors to compare the total impact of each category to that of an average person per year. This allows prioritization of the impact categories by relevance. The results are displayed in Figure 3.
Figure 3.
Product contribution to ecological footprint of a person as determined by Environmental Footprint 3.0 method across all impact categories.
The three most relevant impact categories are “Freshwater ecotoxicity”, “Fossils”, and “Climate change”. The main drivers for these three categories are listed in Supplementary Table 1. The cardboard packaging for storage and transport is a major driver in all three categories. Furthermore, the use of deionized water during reprocessing is a major driver of “Freshwater ecotoxicity” for the reprocessed IPC sleeves.
The normalized results were weighted to determine the relative importance of each impact category and allow all results to be added up (Table 2). The three categories “Climate change”, “Fossils”, and “Minerals and metals” were identified as the most important ones. Overall, the weighted normalized results showed that reprocessed IPC sleeves reduce the environmental footprint by 43% compared to single-use devices.
Table 2.
Weighted Normalized Environmental Impacts as Determined by the Environmental Footprint 3.0 Method and Accumulated Across All Impact Categories
| Impact Category | Single-Use | Reprocessed | Difference |
|---|---|---|---|
| Climate change–Total | 182 | 109 | 73 |
| Fossils | 108 | 62 | 46 |
| Minerals and metals | 55 | 21 | 34 |
| Freshwater ecotoxicity–Total | 55 | 40 | 15 |
| Respiratory effects, inorganics | 54 | 31 | 23 |
| Freshwater and terrestrial acidification | 30 | 15 | 15 |
| Photochemical ozone creation | 25 | 12 | 13 |
| Water scarcity | 17 | 8 | 9 |
| Terrestrial eutrophication | 14 | 7 | 7 |
| Marine eutrophication | 12 | 7 | 5 |
| Carcinogenic effects–Total | 11 | 8 | 4 |
| Ozone layer depletion | 9 | 2 | 6 |
| Land use | 8 | 6 | 1 |
| Non-carcinogenic effects–Total | 7 | 4 | 3 |
| Freshwater eutrophication | 3 | 2 | 2 |
| Ionizing radiation | 2 | 1 | 1 |
| Total | 592 | 335 | 257 |
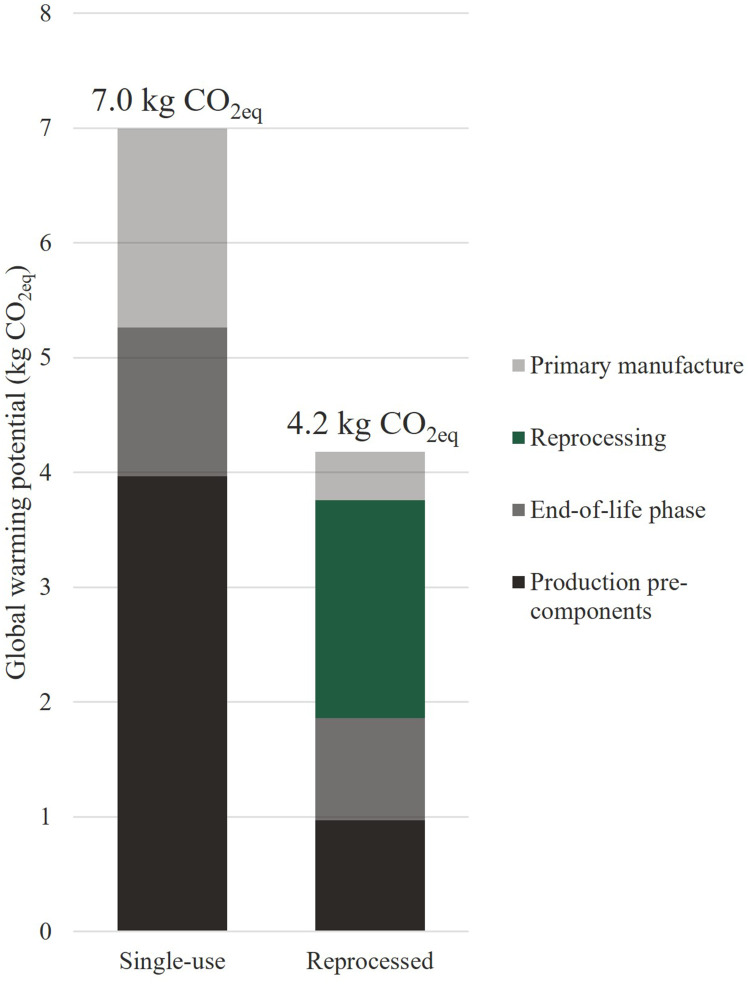
Breakdown of Results
The category “Climate change” has a high relevance, both in the public perception of environmental issues and in this LCA. In order to better understand the contributions of both IPC sleeve products to climate change, a result breakdown with absolute numbers is shown that illustrates the key differences between single-use and reprocessed IPC sleeves (Figure 4). It shows that the treatment of five patients with single-use IPC sleeves creates 7 kg CO2eq, whereas reprocessed IPC sleeves lead to emissions of 4.2 kg CO2eq, effectively reducing the carbon footprint by 40%. The production of pre-components is responsible for the highest share of the carbon footprint of single-use sleeves, whereas reprocessing is the factor contributing most to the carbon footprint of reprocessed IPC sleeves. In the year 2021, an estimated 11 million single-use IPC sleeves were produced, and 3.68 million IPC sleeves were reprocessed, leading to emissions of 77,190 metric tons CO2eq and 15,388 metric tons CO2eq, respectively. If all IPC treatments in 2021 used reprocessed rather than single-use products, the potential reduction of the carbon footprint is estimated to be 6200 metric tons CO2eq.
Figure 4.
Breakdown of accumulated impacts for the impact category “climate change” comparing single-use and reprocessed IPC sleeves.
Costs of Waste Disposal
Reprocessed sleeves save 13.5 kg (50.3%) of total waste compared to single-use ones by reducing the waste generated outside the hospital (during production or reprocessing) by 2.1 kg and preventing 11.4 kg of waste in the hospital. The disposal costs for hospitals were $99.60 for single-use IPC sleeves and $10.45 for reprocessed devices, saving $89.15 (90%). The lower and higher savings estimate were $4.47 and $252.18.
Sensitivity to Assumptions
In order to provide a framework for the interpretation of the results of this LCA, sensitivity analyses were performed for the most relevant scenarios to test the vulnerability of the results with regards to changes in assumptions.
Electricity Mix
All reprocessed IPC sleeves are reprocessed in a dedicated facility located in Florida. In this scenario, it is assumed that the electricity for the reprocessing facility is provided by 100% renewable energy sources. As only the reprocessed IPC sleeves are reprocessed, this scenario only applies to them.
Switching to 100% renewable energy sources decreased the environmental footprint of the reprocessed IPC sleeves in most impact categories (Supplementary Figure 1A). It only increased in the categories “Land use” and “Minerals and metals” due to the rare earth elements required to construct wind and solar power stations and the space requirements to set them up.
Ethylene Oxide Emissions Simulation
Ethylene oxide (ETO) is used for high-level disinfection during IPC sleeve reprocessing. While the facility complies with ISO 10993–7 safety standards and actual emissions are likely much lower, the baseline scenario conservatively assumed that 10% of the ETO used in the process is emitted into the air as a side product of the disinfection process. This scenario increases ETO emission rates to 100%.
This substantially increased the impact category “Carcinogenic effects” (67%) and slightly increased the category “Non-carcinogenic effects” (2%) for reprocessed IPC sleeves (Supplementary Figure 1B). No other impact categories were sensitive with regards to ETO emissions.
Transports (Overall)
Both the single-use and the reprocessed IPC sleeves need to be transported between the manufacturing plant, hospital, and disposal site. The reprocessed IPC sleeve additionally must be transported from the hospital to the reprocessing facility and back. This sensitivity analysis scenario assumes a 50% increase in the number of transports needed for both types of IPC sleeves due to volume constraints.
An increase in the total number of transports increases the values for all impact categories in both single-use and reprocessed IPC sleeves (Supplementary Figure 1C). The increase is larger for reprocessed IPC sleeves, because they require additional transport to and from the reprocessing facility. Despite the larger increase across all impact categories, however, the results of this sensitivity analysis still show an environmental benefit for the reprocessed devices across all impact categories (Supplementary Figure 1A). This shows that the uncertainties in the assumptions regarding transport do not change the overall result of the LCA, despite the negative environmental impact caused by the increase in transport.
Transport (for Reprocessing)
Finally, the fourth scenario focuses on the transport of reprocessed IPC sleeves to and from the reprocessing facility. It assumes that the transport distances are 50% shorter than in the baseline scenario.
This decrease in reprocessing-specific transports caused a reduction in the environmental footprint of reprocessed IPC sleeves across all impact categories (Supplementary Figure 1D). A reduction of transport distances would further reduce the environmental footprint of reprocessed IPC sleeves. This further confirms that the results of this LCA are robust regarding transport variation, as the changes in transport distances and volume constraints do not change the direction of the overall results.
Discussion
What makes this LCA unique in comparison to others is that the initial production process and material composition of single-use and reprocessed IPC sleeves are identical, whereas the devices studied in other LCAs often differ.5,6,26 This means that the differences between the single-use and reprocessed devices in our study are limited to the number of reprocessing circles and the environmental impact of reprocessing as well as associated processes like transports and packaging without affecting any life cycle steps prior to the first use of the device. Reprocessed sleeves also demonstrate a potential for reduction of waste and the resulting disposal costs.
Not all LCAs of single-use versus reusable or reprocessed medical devices and supplies demonstrate an environmental benefit for reprocessing, as some reprocessing efforts can be more resource-intensive and/or environmentally inefficient than the production of the primary product.8,10,26–28
Similar to our observations, other LCAs also found that reprocessing is the largest impact on the environmental footprint of reprocessed devices whereas manufacturing is most prominent for single-use devices.5,6,27
There are several benefits of the LCA method for the health sector. Firstly, this LCA shows that even with rigorous standards around device cleaning and disinfection in reprocessing and long transport distances, reprocessing has an environmental advantage. However, this cannot be said for all medical devices without evaluation as so many parameters have an impact on the overall result.8 Secondly, a comparison of the overall environmental footprint of products is possible with LCAs, providing a holistic view as well as additional key performance indicators for the health sector. These support decision-making in the health sector not just on monetary but also on environmental criteria, which are of increasing relevance.2,4 Finally, the quantification of environmental effects while changing key parameters allows for internal decision-making for production processes in the healthcare sector, leading the way to climate goals by bringing up potential trade-offs with impact categories and help to develop improvements.
When it comes to expanding reprocessing programs, it is important to consider how hospitals can change their processes toward a circular economy. This includes designing practice-oriented collection systems that can be integrated into hospital processes with little effort. More use cases and pilot studies of a circular economy in hospitals are needed to confirm efficiencies.
Limitations of the Study
This study has several limitations. The LCA method comes with intrinsic methodological challenges, as it necessitates assumptions and introduces uncertainties. These uncertainties are related to several factors: (i) the technology processes (such as production of pre-components, waste management or transport) which are generally based on default inventories, (ii) the geographical boundaries (the model describes the USA, so several assumptions were made to develop a transportation model without leaving the geographical boundaries), (iii) the quality of the data available to populate the LCA model, and (iv) the uncertainties inherent in the LCA method. As the regional framework conditions have a great impact on the LCA results, they cannot be generalized across geographic regions without adjusting the inventory accordingly.
In this study, the transportation routes and distances needed to transport the IPC sleeves between the manufacturing site, the hospitals, and the reprocessing plant (for reprocessed devices) include the use of default inventories for the transportation processes where no primary data and/or US-specific data were available, and the assumptions that were made to develop a transport model describing the USA without leaving these geographical boundaries. The most important uncertainties were therefore addressed in the sensitivity analysis, which showed that the results were robust concerning transport distances.
Furthermore, a detailed breakdown of results was not performed for all impact categories. Instead, this study focused on the category “Climate change”, which is considered relevant both in the normalization of the LCA results and in the general understanding of environmental issues.
Finally, it was not possible to calculate the statistical significance of any of the differences.
Conclusion
This life cycle assessment clearly demonstrates that reprocessed IPC sleeves have an environmental benefit compared to single-use IPC sleeves across all considered impact categories, with a reduction of more than 30% in all but two categories. Reprocessing IPC sleeves reduces the overall environmental footprint by 43% (following characterization), and the global warming potential by 40%.
The main influence factors for the environmental impact are material use, transport and storage boxes, and electricity use. The sensitivity analysis showed that the results overall are robust.
Acknowledgments
Professional medical writing and editorial assistance was provided by Juliane Hafermann of Coreva Scientific GmbH & Co. KG (Koenigswinter, Germany).
The authors thank Meg McClanahan, the Global Portfolio Director, and the team of Sustainable Technologies™, a Cardinal Health business, for providing the primary data necessary to develop the LCA.
The LCA was critically reviewed by Dr. Fredy Dinkel of Carbotech AG (Basel, Switzerland). The review states that the requirements of the standard have been met.
Funding Statement
This study was supported by funding from Cardinal Health™. ECOFIDES Consulting GmbH, pulswerk GmbH, Coreva Scientific GmbH & Co. KG and Alex Veloz received consultancy fees from Cardinal Health for work related to this manuscript. Cardinal Health had no role in the design and conduct of the study; management, analysis, and interpretation of the data; preparation, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations
ABS, Acrylonitrile Butadiene Styrene; EF, Environmental Footprint 3.0; ETO, Ethylene Oxide; IPC, Intermittent pneumatic compression; LCA, Life cycle assessment; PEF, Product Environmental Footprint; PVC, Polyvinyl chloride.
Disclosure
Rhodri Saunders is the founding director and owner of Coreva Scientific GmbH & Co. KG, which received consultancy fees from Cardinal Health for performing, analyzing, and communicating the work presented here. Francesca Paolini is an employee of Coreva Scientific GmbH & Co. KG, which received consultancy fees from Cardinal Health for performing, analyzing, and communicating the work presented here. Markus Meissner is an associate member of the Austrian Institute of Ecology and an employee of pulswerk GmbH, the latter of which received consultancy fees from Cardinal Health for performing, analyzing, and communicating the work presented here. Sabrina Lichtnegger is the CEO of ECOFIDES Consulting GmbH, which received consultancy fees from Cardinal Health for performing, analyzing, and communicating the work presented here. Alex Veloz is an independent consultant who received consultancy fees from Cardinal Health for performing, analyzing, and communicating the work presented here. The authors report no other conflicts of interest in this work.
References
- 1.Lenzen M, Malik A, Li M, et al. The environmental footprint of health care: a global assessment. Lancet Planet Health. 2020;4(7):e271–e279. doi: 10.1016/S2542-5196(20)30121-2 [DOI] [PubMed] [Google Scholar]
- 2.Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397(10269):129–170. doi: 10.1016/S0140-6736(20)32290-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Alliance for Transformative Action on Climate and Health (ATACH): country commitments. Available from: https://www.who.int/initiatives/alliance-for-transformative-action-on-climate-and-health/country-commitments. Accessed April 20, 2023.
- 4.Rizan C, Steinbach I, Nicholson R, Lillywhite R, Reed M, Bhutta MF. The Carbon Footprint of Surgical Operations: a Systematic Review. Ann Surg. 2020;272(6):986–995. doi: 10.1097/SLA.0000000000003951 [DOI] [PubMed] [Google Scholar]
- 5.Eckelman M, Mosher M, Gonzalez A, Sherman J. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth Analg. 2012;114(5):1067–1072. doi: 10.1213/ANE.0b013e31824f6959 [DOI] [PubMed] [Google Scholar]
- 6.Sherman JD, Raibley LA, Eckelman MJ. Life Cycle Assessment and Costing Methods for Device Procurement: comparing Reusable and Single-Use Disposable Laryngoscopes. Anesth Analg. 2018;127(2):434–443. doi: 10.1213/ANE.0000000000002683 [DOI] [PubMed] [Google Scholar]
- 7.Meissner M, Lichtnegger S, Gibson S, Saunders R. Evaluating the Waste Prevention Potential of a Multi- versus Single-Use Surgical Stapler. Risk Manag Healthc Policy. 2021;14:3911–3921. doi: 10.2147/RMHP.S325017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perry H, Reeves N, Ansell J, et al. Innovations towards achieving environmentally sustainable operating theatres: a systematic review. Surgeon. 2023;21(3):141–151. doi: 10.1016/j.surge.2022.04.012 [DOI] [PubMed] [Google Scholar]
- 9.Freund J, Gast K, Zuegge K, Hicks A. Environmental considerations in the selection of medical staplers: a comparative life cycle assessment. J Cleaner Prod. 2022;371:133490. doi: 10.1016/j.jclepro.2022.133490 [DOI] [Google Scholar]
- 10.McGain F, McAlister S, McGavin A, Story D. A life cycle assessment of reusable and single-use central venous catheter insertion kits. Anesth Analg. 2012;114(5):1073–1080. doi: 10.1213/ANE.0b013e31824e9b69 [DOI] [PubMed] [Google Scholar]
- 11.Ho KM, Tan JA. Stratified meta-analysis of intermittent pneumatic compression of the lower limbs to prevent venous thromboembolism in hospitalized patients. Circulation. 2013;128(9):1003–1020. doi: 10.1161/CIRCULATIONAHA.113.002690 [DOI] [PubMed] [Google Scholar]
- 12.Sharfman ZT, Campbell JC, Mirocha JM, Spitzer AI. Balancing Thromboprophylaxis and Bleeding in Total Joint Arthroplasty: impact of Eliminating Enoxaparin and Predonation and Implementing Pneumatic Compression and Tranexamic Acid. J Arthroplasty. 2016;31(6):1307–1312. doi: 10.1016/j.arth.2015.11.046 [DOI] [PubMed] [Google Scholar]
- 13.Kakkos SK, Szendro G, Griffin M, Daskalopoulou SS, Nicolaides AN. The efficacy of the new SCD response compression system in the prevention of venous stasis. J Vascular Surgery. 2000;32(5):932–940. doi: 10.1067/mva.2000.110358 [DOI] [PubMed] [Google Scholar]
- 14.International Organization for Standardization. Environmental Management — Life Cycle Assessment — Requirements and Guidelines (ISO 14044:2006 + Amd 1:2017 + Amd 2:2020) (Consolidated Version); 2021 [Google Scholar]
- 15.ecoinvent Centre. Database ecoinvent v3.8 - ecoinvent. Available from: https://ecoinvent.org/the-ecoinvent-database/data-releases/ecoinvent-3-8/#1610466712069-fcebe4bb-f802. Accessed May 4, 2023.
- 16.Cardinal Health Inc. SCD Process (Internal Document); 2020. [Google Scholar]
- 17.Cardinal Health Inc. Reprocessing Single Use Devices (Suds) – Kendall SCD™ Compression Sleeves (Internal Document); 2018. [Google Scholar]
- 18.Weidema BP, Bauer C, Hischier R, et al. Overview and Methodology. Data Quality Guideline for the Ecoinvent Database Version 3. Ecoinvent Report 1(v3). St. Gallen: The ecoinvent Centre; 2013. [Google Scholar]
- 19.Zampori L, Pant R. Suggestions for Updating the Product Environmental Footprint (PEF) Method, EUR 29682 EN. Luxembourg: Publications Office of the European Union; 2019. [Google Scholar]
- 20.European Commission - Joint Research Centre - Institute for Environment and Sustainability. International Reference Life Cycle Data System (ILCD) Handbook - General Guide for Life Cycle Assessment - Detailed Guidance. First Edition March 2010. EUR 24708 EN. Luxembourg: Publications Office of the European Union; 2010. [Google Scholar]
- 21.Sala S, Crenna E, Secchi M, Pant R. Global Normalisation Factors for the Environmental Footprint and Life Cycle Assessment, EUR (28984). Luxembourg: Publications Office of the European Union; 2017. [Google Scholar]
- 22.Sala S, Cerutti AK, Pant R. Development of a Weighting Approach for the Environmental Footprint. Luxembourg: Publications Office of the European Union; 2018. [Google Scholar]
- 23.Babu MA, Dalenberg AK, Goodsell G, Holloway AB, Belau MM, Link MJ. Greening the Operating Room: results of a Scalable Initiative to Reduce Waste and Recover Supply Costs. Neurosurgery. 2019;85(3):432–437. doi: 10.1093/neuros/nyy275 [DOI] [PubMed] [Google Scholar]
- 24.Kagoma YK, Stall N, Rubinstein E, Naudie D. People, planet and profits: the case for greening operating rooms. CMAJ. 2012;184(17):1905–1911. doi: 10.1503/cmaj.112139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riedel LM. Environmental and financial impact of a hospital recycling program. AANA J. 2011;79(4 Suppl):S8–14. [PubMed] [Google Scholar]
- 26.Sørensen BL, Wenzel H. Life cycle assessment of alternative bedpans – a case of comparing disposable and reusable devices. J Cleaner Prod. 2014;83:70–79. doi: 10.1016/j.jclepro.2014.07.022 [DOI] [Google Scholar]
- 27.McGain F, Story D, Lim T, McAlister S. Financial and environmental costs of reusable and single-use anaesthetic equipment. Br J Anaesth. 2017;118(6):862–869. doi: 10.1093/bja/aex098 [DOI] [PubMed] [Google Scholar]
- 28.Schulte A, Maga D, Thonemann N. Combining Life Cycle Assessment and Circularity Assessment to Analyze Environmental Impacts of the Medical Remanufacturing of Electrophysiology Catheters. Sustainability. 2021;13(2):898. doi: 10.3390/su13020898 [DOI] [Google Scholar]