Abstract
Purpose
To provide long-term intraocular pressure (IOP) and ocular hypotensive medication usage outcomes through 36 months for patients treated with canaloplasty and trabeculotomy (OMNI Surgical System) combined with cataract surgery as participants in the GEMINI study.
Setting
Eleven ophthalmology practices in 10 US states.
Design
Non-interventional 36-month extension of the 12-month, prospective, multicenter, GEMINI study.
Methods
GEMINI patients had visually significant cataract, mild-to-moderate glaucoma (ICD-10 guidelines), medicated IOP <33 mmHg, and unmedicated mean diurnal IOP (DIOP) (after washout) 21–36 mmHg. Patients from GEMINI were eligible for inclusion. Outcome measures were reduction in mean unmedicated DIOP, reduction in mean IOP-lowering medications, percent of eyes with ≥20% reduction in unmedicated DIOP, and percent of eyes with unmedicated DIOP ≥6 and ≤18 mmHg.
Results
A total of 66 patients provided consent and were enrolled. Mean (SD) unmedicated DIOP was 23.1 (2.7) mmHg at baseline, 16.7 (4.1), 16.3 (3.3) at 24 and 36 months; mean reductions of 6.2 (4.1) and 6.9 (3.4) mmHg. Twelve-month IOP at the end of GEMINI was 15.6 mmHg. The proportion of eyes with ≥20% reduction in IOP was 77% and 78% (months 24 and 36) compared to 87% at month 12 from GEMINI. About 68% of patients had an IOP between 6 and 18 mmHg at 24 months and 71% at 36 months. Mean IOP-lowering medications was 1.7 at baseline, which was reduced to 0.4 (24 months, −1.3) and 0.3 (36 months, −1.4). About 74% of patients (46 of 62) were medication free at 36 months.
Conclusion
GEMINI demonstrated 12-month effectiveness of canaloplasty and trabeculotomy with OMNI combined with cataract surgery for IOP and medication reduction in mild-to-moderate glaucoma. However, longer-term data is key to the decision making in the selection of a surgical treatment. This GEMINI extension demonstrates that the 12-month outcomes from GEMINI were sustained through 36 months.
Keywords: canaloplasty, trabeculotomy, MIGS, OMNI, glaucoma
Introduction
Minimally invasive glaucoma surgery (MIGS) has become a mainstay treatment choice for many glaucoma surgeons over the past two decades.1 MIGS is attractive because the surgeries, as a group, are relatively atraumatic, sparing conjunctiva and sclera, compared to traditional bleb-forming procedures. There is rapid patient recovery, and, a growing body of data showing that, on average, resultant intraocular pressure can be expected to be in the mid to low teens while also reducing reliance on medication.2,3 Canaloplasty and trabeculotomy (OMNI Surgical System, Sight Sciences, Menlo Park, CA, USA) is a MIGS technology that combines two established procedures with the aim of treating proximal (trabecular meshwork) and distal (Schlemm’s canal and the collector channels) resistance to restore physiological outflow through the conventional outflow pathway.
The GEMINI study was a 12-month prospective, multicenter, interventional clinical study of patients with mild-moderate of (mainly) primary open-angle glaucoma (POAG, 93%, 139 of 149) undergoing 360° canaloplasty and 180° trabeculotomy with OMNI combined with phacoemulsification cataract surgery.4 The study employed a baseline and terminal (12 month) medication washout with results showing meaningful intraocular pressure (IOP) and medication reductions similar to those achieved in randomized controlled trials of trabecular bypass stents.4–6 A limitation of the GEMINI study was the 12-month follow-up period. Longer term follow-up is desirable in order to show durability of the treatment effect as well as identification of any late-term adverse events. The present observational study was designed to evaluate longer term safety and effectiveness of canaloplasty and trabeculotomy combined with cataract surgery through 36 months for patients participating in GEMINI.
Methods
This was an observational, non-interventional follow-up study for patients originally treated as part of the GEMINI prospective, interventional 12-month study (NCT03861169). This follow-up study was reviewed and approved by the WCG IRB (Puyallup, WA, USA) and all patients provided written informed consent. The study was registered on clinicaltrials.gov (NCT05044793) and adhered to the tenets of the Declaration of Helsinki. There were 15 centers in the original GEMINI study; 11 elected to participate in the follow-up study. All surgeries took place between April 2019 and March 2020.
GEMINI was a prospective single-arm study with eligibility criteria closely following those used in pivotal MIGS implant trials.5,6 These included a diagnosis of mild-to-moderate glaucoma according to ICD-10 guidelines with visual field mean deviation no worse than −12 dB, unmedicated washed out IOP of between 21 and 36 mmHg, 0–4 pre-study, pre-washout IOP-lowering medications, Shaffer grade of at least 3 in all quadrants, visually significant cataract, and no history of prior glaucoma surgery.4 Only one eye per patient was enrolled. Additional eligibility requirements for the present extension study included participation and completion of 12 months follow-up in the GEMINI study, and no new ocular pathology which would place the patient at increased risk or contraindicate medication washout at the endpoint visits.
Surgical Technique
The OMNI surgical technique as performed in the original GEMINI study has been previously described.4 All eyes underwent standard phacoemulsification with implantation of a posterior chamber intraocular lens (PCIOL). The OMNI device was then used to perform a 360° canaloplasty followed by 180° trabeculotomy. In brief, the OMNI cannula tip was inserted through the same clear corneal incision used for the phaco procedure, and then across the anterior chamber under intraoperative gonioscopy. A small cut was made in the nasal trabecular meshwork (TM) using the cannula tip, and the flexible microcatheter was advanced 180° through the canal of Schlemm. On retraction, a fixed volume (5.5 µL per 180°) of cohesive viscoelastic was automatically dispensed, dilating the canal and the collector channels. This was repeated for the other 180° using the same TM entry point to complete the canaloplasty. The trabeculotomy was then performed by again advancing the microcatheter to its full extent (180°) into the canal and withdrawing slowly to unroof 180°. A standard regimen of steroid, nonsteroidal anti-inflammatory drug, and antibiotic was prescribed postoperatively.
Follow-up visits were scheduled for 24 and 36 months following the index procedure (canaloplasty and trabeculotomy combined with cataract surgery), with an appropriate medication washout prior to each of these (minimum 28 days for beta-blockers, prostaglandin analogs, or rho kinase inhibitors, 14 days for alpha agonists, and 5 days for carbonic anhydrase inhibitors or muscarinics). At both 24 and 36 months, changes in medical or ocular history, ocular hypotensive medication usage, and any adverse events that may have occurred were recorded. Manifest refraction was performed and monocular best corrected visual acuity was assessed. Diurnal IOP (DIOP) measurements (Goldmann) using an operator/reader technique were taken (9 am, noon, 4 pm), and a thorough slit lamp exam was performed including gonioscopy and dilated fundus. Finally, automated perimetry (Humphrey 24–2 SITA) was performed at both visits.
Effectiveness endpoints were 1) reduction in mean DIOP from the pre-surgical baseline, 2) reduction in the mean number of medications from baseline, 3) the proportion of patients with a ≥ 20% reduction in unmedicated DIOP, and 4) the proportion of patients with unmedicated DIOP between 6 and 18 mmHg inclusive. Any patients requiring a secondary surgical or laser intervention for IOP control (SSI) in the study eye during the follow-up period were considered failures for binary responder endpoints (eg ≥20% IOP reduction). Safety was assessed through collection of adverse events, best corrected visual acuity, and necessity of any SSI.
The sample size for this study was a “convenience” sample based on all available GEMINI patients that provided informed consent at the 11 participating sites. With an assumed standard deviation of 3.5 mmHg for intraocular pressure, a minimum change in IOP of 5.0 mmHg from a pre-operative baseline of mean = 21 mmHg, and alpha = 0.05, a sample size of minimum 50 subjects was required to get at least 90% power to detect statistical significance. This was a descriptive study and was not designed to test pre-planned hypotheses. T-tests (2-sample, 2-sided, equal variance) were used to compare outcomes at 24 and 36 months versus baseline with a significance level set at 0.05. Multiplicity was addressed using a Bonferroni correction.
Results
Demography and Baseline Characteristics
Sixty-six patients were enrolled in this study. The majority were White (59 of 66, 89%), not Hispanic (44 of 66, 66%), averaged 72 years of age (SD 7.5, minimum 51, maximum 95), with males and females approximately equally represented (46% and 54%, respectively), and nearly all with a diagnosis of primary open-angle glaucoma (63 of 66, 96%). There were 3 patients with pseudoexfoliation. Mild glaucoma was predominant with mean (SD) visual field mean deviation (MD) −3.10 (3.08) dB (56 of 66 with mean deviation better than −6.0 dB). Mean (SD) pattern standard deviation (PSD) was 3.18 (2.27) dB. Mean medicated screening IOP was 16.4 (3.0) mmHg on 1.7 (0.9) medications. There were 3 patients on zero medications, 34 on 1, 15 on 2, and 14 on 3 or more.
Intraocular Pressure and Medications
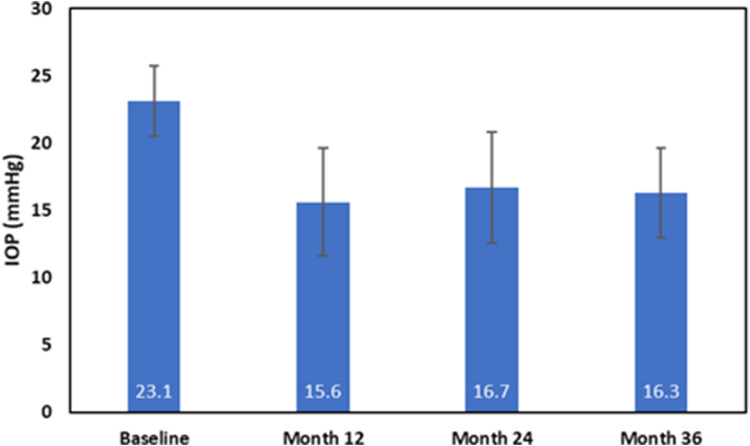
Following the pre-surgical medication washout at the start of the original GEMINI study, mean unmedicated DIOP was 23.1 (2.70) mmHg, similar to that for the full GEMINI (n=120) cohort of 23.9 (3.0) mmHg.4 At 12, 24, and 36 months mean unmedicated DIOP was 15.6 (4.0), 16.7 (4.1), and 16.3 (3.3) mmHg, all P<0.00001 versus baseline (Figure 1) representing mean decreases of 7.4 mmHg (−32%), 6.2 mmHg (−27%), and 6.9 mmHg (−29%), respectively. While the proportion of patients with a 20% or more reduction in mean DIOP from baseline was 84.2% at 12 months in GEMINI,4 it was 77% at 24 and 78% at 36 months. The proportion of patients with unmedicated DIOP between 6 and 18 mmHg was 68% at 24 months and 71% at 36 months.
Figure 1.
Mean IOP (SD) at each visit. Medication washout prior to each visit. All visits P<0.00001 versus Baseline.
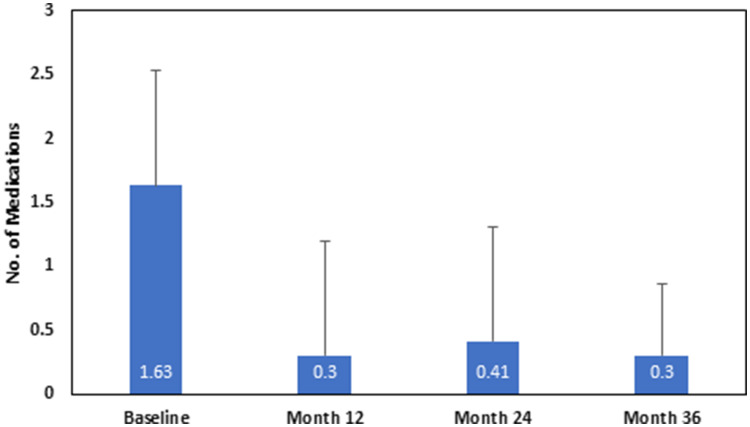
Medication usage was low at the end of the 12-month GEMINI study (0.3 average medications)4 and remained low at 24 and 36 months, 0.4 (0.9) and 0.3 (0.6) (Figure 2). Follow-up medication use was significantly different from baseline at all visits (P<0.00001). At 36 months, only 3 patients required 2 meds and zero patients required 3 or more in contrast to pre-surgery when 15 (23%) were on 2 and 14 (22%) on 3 or more meds. At 36 months, 53 of the 59 patients (90%) on at least 1 medication at baseline had a decrease from baseline of 1 or more medications. Many patients remained medication free entirely through 36 months (Table 1).
Figure 2.
Mean medication (SD) use at each visit (prior to medication washout). All visits P<0.00001 versus Baseline.
Table 1.
Number and Proportion of Medication-Free*Patients at 24 and 36 Months
| Timepoint | Medication Free | Proportion Medication Free |
|---|---|---|
| Pre-Surgical Baseline (n = 66) | 3 | 5% |
| Month 24 (n = 66) | 51 | 77% |
| Month 36 (n = 62) | 46 | 74% |
Note: *Before mandatory medication washout.
Safety
Ocular adverse events (AE) reported in GEMINI over the first 12 months were relatively uncommon (19 for 149 patients) and were all mild and transient. The most common were layered hyphema ≥1 mm (9, 6%), and IOP spikes (3, 2%). All others occurred at an incidence of ~1% or less.4 In this extension study, there were only 4 AE considered related to either the device or procedure; one for complaint of dry eye at about 18 months post-surgery which subsequently resolved, the other 3 for posterior capsular opacification, all reported at 24 months post-surgery. Mean (SD) visual field MD and PSD were unchanged from baseline at months 24 and 36; MD (BL, 24 months, 36 months) was −3.10 dB (3.08), −2.46 dB (3.84), −3.10 dB (3.88); PSD was 3.18 dB (2.27), 3.35 dB (2.69), 3.51 dB (2.77). No SSI were required during the first year of the GEMINI study4 and only one, a tube shunt procedure at approximately 30 months post-surgery, was needed for the patients in this extension study.
Discussion
The GEMINI study was the first prospective multicenter clinical study to assess the safety and effectiveness of the OMNI Surgical System used in combination with cataract surgery in mild-to-moderate POAG patients4,7 GEMINI was designed to have similar eligibility criteria and endpoints to the pivotal MIGS trabecular bypass stent trials for Hydrus and iStent inject following ANSI Z80.27 guidelines.5,6 While GEMINI did not have a parallel cataract surgery only control group, the study was statistically powered to show a minimum 1.0 mmHg greater IOP reduction for OMNI with cataract surgery over cataract surgery alone at 12 months based on an estimated 6.0 mmHg reduction at 12 months for cataract surgery only derived from the results of the two stent studies. In fact, at 12 months, OMNI plus cataract surgery achieved a mean IOP reduction of 8.2 mmHg (−34%), comparable to what was achieved in the HORIZON Hydrus pivotal trial (−8.5 mmHg).4,6 Moreover, a post-hoc analysis of diurnal IOP fluctuations in the GEMINI study showed that 12 months after surgery with OMNI, IOP fluctuations were significantly reduced compared to pre-surgical measurements.8
Longer-term data, beyond 12 months, are important in order to understand the durability of the treatment effect, potential safety issues that may not be apparent in the short term,9,10 and also potential impacts on disease progression that have a longer time horizon.11 In this report, we show that the IOP and medication reductions observed at 12 months in GEMINI persist through 36 months. The IOP reduction at 36 months is similar to that at 12 months with little change in mean medication use or the proportion of patients medication-free. Sustained long-term (>12 months) IOP and medication reductions with OMNI have also been reported in other studies of OMNI. In the retrospective multicenter ROMEO study, standalone patients with baseline IOP >18 mmHg had IOP of 16.3 mmHg on 1.4 medications (month 12) and 14.7 mmHg on 1.6 medications (month 24), while the corresponding group combined with cataract surgery went from 15.0 mmHg on 1.2 medications (month 12) to 15.6 mmHg on 1.4 medications at 2 years.12 In ROMEO, the proportion of medication-free patients also remained stable between 1 and 2 years, 34.7% and 33.3%, respectively.12 Klabe and Kaymak reported 24 month outcomes for a retrospective single-center case series including 38 eyes of 27 patients that had undergone standalone canaloplasty and trabeculotomy with OMNI. These patients had all undergone medication washout prior to surgery, similar to GEMINI. Consistent with our present results, they found that IOP was reduced to the mid-teens at one year and remained there through the endpoint at 24 months (Baseline IOP 24.6 mmHg, month 12 14.7 mmHg, month 24 14.9 mmHg). Medications were also stable going from 1.9 prior to baseline washout to 0.4 and 0.5 at 12 and 24 months.13 Ondrejka et al followed a series of 206 eyes treated with OMNI for canaloplasty only through 36 months of follow-up and also found that the significant IOP and medication reductions observed by 12 months persisted with little change through 36 months.14
The consistency of the IOP reductions that are obtained with OMNI are noteworthy. A recent review of OMNI clinical studies (including the 12-month GEMINI study) found that across 5 studies of OMNI including 159 eyes, 155 (97.5%) had a decrease in IOP at last follow-up and most of these (120 of 159, 75%) had a 20% or greater reduction in IOP.15 In addition, considering only those patients from 6 studies with a baseline IOP > 20 mmHg (219 eyes), IOP reductions were between 8.5 and 10 mmHg.15
While most studies of OMNI are centered on mild-to-moderate glaucoma, Yadgarov et al has recently shown that OMNI is equally effective in IOP-lowering across mild, moderate, and severe glaucoma as categorized using the Center for Medicare and Medicaid Services (CMS) criteria.16 There was an approximately equal number at each severity level in this study including 171 patients. Most patients completed 12 months of follow-up and 71 completed 24 months. Interestingly, the lowest mean IOP at 24 months was achieved by the advanced subgroup, 13.0 mmHg, perhaps because these patients were being treated to a lower target IOP and had greater average medication use (1.48 at 24 months compared to 0.95 moderate and 0.31 mild).16 In another study evaluating the effectiveness of OMNI for eyes that had a previous iStent, 30% of eyes had a diagnosis of moderate glaucoma and 26% advanced. At last follow-up mean IOP was 17.2 mmHg, a reduction of 5.1 mmHg from baseline.17
Follow-up through 36 months did not reveal any worrisome adverse events. There were just 4 related or possibly related AE and 3 of these were for posterior capsular opacification, a commonplace occurrence post-cataract surgery. There was a single SSI required, a rate of just 1.5% over 3 years, which compares favorably to other OMNI studies; Hirsch et al 5% (12 months), Vold et al 10% (12 months), Klabe et al 5% (2 years)13,18,19 and also when compared to other MIGS trials; Hydrus, 2% (2 years),20 5.4% (5 years);11 iStent inject, 5.4% (2 years),5 4.5% (3 years),21 8.4% (3 years),22 1.8% (4 years),23 4% (5 years).24 Yadgarov et al conducted a Kaplan–Meier survival analysis on their cohort of mild, moderate and severe glaucoma patients and found that 95% of mild,96% of moderate, and 89% of severe stage glaucomatous eyes avoided subsequent glaucoma incisional surgery over a 2-year interval. Sequential visual field data was not reported in this study so it is not possible to compare progression rates across these severity groups treated with OMNI. The somewhat higher proportion of severe patients requiring an SSI, despite the substantially greater IOP reduction of the three cohorts, likely reflects the generally lower target IOP set for eyes at higher risk for significant loss of vision from glaucoma.16
The strengths of this study include its multicenter design, medication washout pre-operatively and at the 12, 24, and 36 month endpoints, inclusion and exclusion criteria (for the original GEMINI study) modelled after those used in the large pivotal trabecular bypass trials, diurnal IOP measurements at baseline and the endpoints, and operator/reader methodology for IOP.4–6 In terms of diversity, the majority of patients were White, non-Hispanic; however, the 11% of patients identifying as Black or African American closely mirrors the 13.6% recorded in the 2020 US census, and while 19% of the US population identifies as Hispanic, Hispanic patients comprised one-third of the patients in this study. There are limitations that should be noted. This observational study and the preceding interventional GEMINI study did not have a parallel control group and were not randomized. Nevertheless, the original GEMINI study design was informed by the pivotal trials for MIGS implants in terms of patient population and overall design; the sample size was calculated based on demonstrating superiority to that achieved by the cataract surgery only control arms of these earlier studies. GEMINI 2 did not include all of the patients or all of the study sites from GEMINI. Nevertheless, baseline characteristics and demographics are similar for the entire GEMINI study population and for GEMINI 2 suggesting generalizability of the 24 and 36 month outcomes.
Conclusions
OMNI is unique in the MIGS space in that it encompasses two distinct procedures, canaloplasty and trabeculotomy (colloquially termed TCOR, trabeculocanalicular outflow restoration), with the aim of addressing outflow resistance residing in the trabecular meshwork, Schlemm’s canal, and the distal collector channels. As OMNI was initially FDA cleared in early 2018 longer term data has, until recently, been lacking. In the present study, we report prospective 3-year outcomes which confirm and extend the previously reported 12-month data.4 This data, along with the 2-year results of the retrospective ROMEO study12 demonstrate that the beneficial reductions in IOP and medication use observed in the short term are sustained for two and three years post-surgically. The low rate of SSI observed over the study period suggest that mild-to-moderate glaucoma patients treated with OMNI can very likely avoid (or postpone) more aggressive traditional surgery for a meaningful period of time.
Acknowledgments
GEMINI 2 STUDY GROUP: Brandon Baartman, Anita Campbell, Brian Flowers, Mark Gallardo, Michael Greenwood, Sebastian Heersink, Mark Pyfer, Steven Sarkisian, Inder Paul Singh, Russell Swan, Arkadiy Yadgarov.
Funding Statement
Sight Sciences Inc. provided financial support.
Data Sharing Statement
The authors do not intend to share participant level data. Other queries or requests should be directed to the corresponding author (JD).
Disclosure
MDG has received research support from Sight Sciences. AY is a consultant to Sight Sciences and has received research support from Sight Sciences. SRS is a consultant and speaker for Sight Sciences and has an equity interest in Sight Sciences. BEF has consulted for and received research support from Sight Sciences. He also reports grants, personal fees from Alcon, IStar, Glaukos, Sight science, New world medical, Sanoculis, and Iantrek, outside the submitted work. JED and AON are employees of Sight Sciences.
References
- 1.Yang SA, Mitchell W, Hall N., et al. Trends and usage patterns of minimally invasive glaucoma surgery in the United States: IRIS® registry analysis 2013–2018. Ophthalmol Glaucoma. 2021;4(6):558–568. doi: 10.1016/j.ogla.2021.03.012 [DOI] [PubMed] [Google Scholar]
- 2.Bicket AK, Le JT, Azuara-Blanco A, et al. Minimally invasive glaucoma surgical techniques for open-angle glaucoma: an overview of cochrane systematic reviews and network meta-analysis. JAMA Ophthalmol. 2021;139(9):983–989. doi: 10.1001/jamaophthalmol.2021.2351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birnbaum FA, Neeson C, Solá-Del Valle D. Microinvasive glaucoma surgery: an evidence-based review. Semin Ophthalmol. 2021;36(8):772–786. doi: 10.1080/08820538.2021.1903513 [DOI] [PubMed] [Google Scholar]
- 4.Gallardo MJ, Pyfer MF, Vold SD, et al. Canaloplasty and trabeculotomy combined with phacoemulsification for glaucoma: 12-month results of the GEMINI study. Clin Ophthalmol. 2022;16:1225–1234. doi: 10.2147/OPTH.S362932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Samuelson TW, Sarkisian SR, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811–821. doi: 10.1016/j.ophtha.2019.03.006 [DOI] [PubMed] [Google Scholar]
- 6.Samuelson TW, Chang DF, Marquis R, et al. A schlemm canal microstent for intraocular pressure reduction in primary open-angle glaucoma and cataract: the HORIZON Study. Ophthalmology. 2019;126(1):29–37. doi: 10.1016/j.ophtha.2018.05.012 [DOI] [PubMed] [Google Scholar]
- 7.Gallardo MJ, Sarkisian Jr SR, Vold SD, et al. Canaloplasty and trabeculotomy combined with phacoemulsification in open-angle glaucoma: interim results from the GEMINI study. Clin Ophthalmol. 2021;15:481–489. doi: 10.2147/OPTH.S296740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pyfer MF, Campbell A, Flowers BE, Dickerson JE, Talla A, Dhamdhere K. Suppression of diurnal (9AM–4PM) IOP fluctuations with minimally invasive glaucoma surgery: an analysis of data from the prospective, multicenter, single-arm GEMINI study. Clin Ophthalmol.2021;15:3931–3938. doi: 10.2147/OPTH.S335486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reiss G, Clifford B, Vold S, et al. Safety and effectiveness of CyPass supraciliary micro-stent in primary open-angle glaucoma: 5-year results from the COMPASS XT study. Am J Ophthalmol. 2019;208:219–225. doi: 10.1016/j.ajo.2019.07.015 [DOI] [PubMed] [Google Scholar]
- 10.Lass JH, Benetz BA, He J, et al. Corneal endothelial cell loss and morphometric changes 5 years after phacoemulsification with or without CyPass micro-stent. Am J Ophthalmol. 2019;208:211–218. doi: 10.1016/j.ajo.2019.07.016 [DOI] [PubMed] [Google Scholar]
- 11.Ahmed IIK, De Francesco T, Rhee D, et al. Long-term outcomes from the HORIZON randomized trial for a schlemm’s canal microstent in combination cataract and glaucoma surgery. Ophthalmology. 2022;129(7):742–751. doi: 10.1016/j.ophtha.2022.02.021 [DOI] [PubMed] [Google Scholar]
- 12.Williamson BK, Vold SD, Campbell A, et al. Canaloplasty and trabeculotomy with the OMNI system in patients with open-angle glaucoma: two-year results from the ROMEO Study. Clin Ophthalmol. 2023;17:1057–1066. doi: 10.2147/OPTH.S407918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klabe K, Kaymak H. Standalone trabeculotomy and viscodilation of schlemm’s canal and collector channels in open-angle glaucoma using the OMNI surgical system: 24-month outcomes. Clin Ophthalmol. 2021;15:3121–3129. doi: 10.2147/OPTH.S325394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ondrejka S, Körber N, Dhamdhere K. Long term effect of canaloplasty on IOP and use of IOP-lowering medications in patients with open angle glaucoma: canaloplasty and IOP/Medications in open angle glaucoma. J Cataract Refract Surg. 2022;48(12):1388–1393. doi: 10.1097/j.jcrs.0000000000001000 [DOI] [PubMed] [Google Scholar]
- 15.Dickerson JE, Dhamdhere K. Combined circumferential canaloplasty and trabeculotomy ab interno with the OMNI surgical system. Front Ophthalmol. 2021;1(2):106–114. [Google Scholar]
- 16.Yadgarov A, Dentice K, Aljabi Q. Real-world outcomes of canaloplasty and trabeculotomy combined with cataract surgery in eyes with all stages of open-angle glaucoma. Clin Ophthalmol. 2023;17:2609–2617. doi: 10.2147/OPTH.S422132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Terveen DC, Sarkisian SR, Vold SD, et al. Canaloplasty and trabeculotomy with the OMNI(®) surgical system in OAG with prior trabecular microbypass stenting. Int Ophthalmol. 2022;43(5):1647–1656. doi: 10.1007/s10792-022-02553-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirsch L, Cotliar J, Vold S, et al. Canaloplasty and trabeculotomy ab interno with the OMNI system combined with cataract surgery in open-angle glaucoma: 12-month outcomes from the ROMEO study. J Cataract Refract Surg. 2021;47(7):907–915. doi: 10.1097/j.jcrs.0000000000000552 [DOI] [PubMed] [Google Scholar]
- 19.Vold SD, Williamson BK, Hirsch L, et al. Canaloplasty and trabeculotomy with the OMNI system in pseudophakic patients with open-angle glaucoma: the ROMEO study. Ophthalmol Glaucoma. 2021;4(2):173–181. doi: 10.1016/j.ogla.2020.10.001 [DOI] [PubMed] [Google Scholar]
- 20.Pfeiffer N, Garcia-Feijoo J, Martinez-de-la-Casa JM, et al. A randomized trial of a schlemm’s canal microstent with phacoemulsification for reducing intraocular pressure in open-angle glaucoma. Ophthalmology. 2015;122(7):1283–1293. doi: 10.1016/j.ophtha.2015.03.031 [DOI] [PubMed] [Google Scholar]
- 21.Hengerer FH, Auffarth GU, Riffel C, Conrad-Hengerer I. Second-generation trabecular micro-bypass stents as standalone treatment for glaucoma: a 36-month prospective study. Adv Ther. 2019;36(7):1606–1617. doi: 10.1007/s12325-019-00984-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clement C, Howes F, Ioannidis A, et al. Multicenter effectiveness and disease stability through 3 years after istenttrabecular micro-bypass with phacoemulsification in glaucoma and ocular hypertension. Clin Ophthalmol. 2022;16:2955–2968. doi: 10.2147/OPTH.S373290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindstrom R, Sarkisian SR, Lewis R, Hovanesian J, Voskanyan L. Four-year outcomes of two second-generation trabecular micro-bypass stents in patients with open-angle glaucoma on one medication. Clin Ophthalmol. 2020;14:71–80. doi: 10.2147/OPTH.S235293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hengerer FH, Auffarth GU, Conrad-Hengerer I. iStent inject trabecular micro-bypass with or without cataract surgery yields sustained 5-year glaucoma control. Adv Ther. 2022;39(3):1417–1431. doi: 10.1007/s12325-021-02039-4 [DOI] [PMC free article] [PubMed] [Google Scholar]