Abstract
Objective
Racial and ethnic disparities in arthroplasty utilization are evident, but the reasons are not known. We aimed to identify concerns that may contribute to barriers to arthroplasty from the patient’s perspective.
Methods
We identified patients’ concerns about arthroplasty by performing a mixed methods study. Themes identified during semi-structured interviews with Black and Hispanic patients with advanced symptomatic hip or knee arthritis were used to develop a questionnaire to quantify and prioritize their concerns. Multiple linear and logistic regression analyses were conducted to determine the association between race/ethnicity and the importance of each theme. Models were adjusted for sex, insurance, education, HOOS, JR/KOOS, JR, and discussion of joint replacement with a doctor.
Results
Interviews with eight participants reached saturation and provided five themes used to develop a survey answered by 738 (24%) participants; 75.5% White, 10.3% Black, 8.7% Hispanic, 3.9% Asian/Other. Responses were significantly different between groups (p < 0.05). Themes identified were “Trust in the surgeon” “Recovery”, “Cost/Insurance”, “Surgical outcome”, and “Personal suitability/timing”. Compared to Whites, Blacks were two-fold, Hispanics four-fold more likely to rate “Trust in the surgeon” as very/extremely important. Blacks were almost three times and Hispanics over six times more likely to rate “Recovery” as very/extremely important.
Conclusion
We identified factors of importance to patients that may contribute to barriers to arthroplasty, with marked differences between Blacks, Hispanics, and Whites.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-023-07096-0.
Keywords: Access to care, Arthroplasty, Mixed methods, Race/ethnicity, Surveys
Background
Racial and ethnic disparities in healthcare include persistent underutilization of total hip (THR) and total knee replacement (TKR) surgery for Blacks and Hispanics compared to Whites, and while Hispanics may have less OA, there is a higher prevalence of symptomatic and severe osteoarthritis (OA) among Blacks [1–5]. Racial disparities in arthroplasty outcomes are also well documented and include increased mortality and more revision surgery, as well as worse pain and function both before and after surgery, which may reflect delays in accessing care [6–12]. Patients have identified concerns about improvements in pain and function and surgical complications as important concerns regarding arthroplasty utilization, but participants in most studies have undergone arthroplasty, while the concerns in patients who have not undergone arthroplasty or even sought specialty care have been harder to assess [13, 14]. The patient’s perspectives and concerns about arthroplasty are not well understood, limiting the possibility of interventions for change. In addition, since Blacks are more likely to live in poverty, results linked to race may be confounded by poverty, and the utilization and outcomes of arthroplasty are similar for those from poor neighborhoods and for those without much education [10, 11, 15, 16]. Blacks, Hispanics, and individuals from low-income communities have worse pain and function at the time they undergo THR and TKR than those from wealthier communities, and since baseline status impacts outcomes, delays in care have long-term consequences [2, 11]. The reasons for delay in care by these populations are unknown, as studies have not identified the concerns from the patient’s perspective. Since THR and TKR are elective procedures, patients’ preferences are a critical component that needs to be included in a patient centered approach, to improve appropriate utilization of arthroplasty [2, 17]. Potentially important factors described include racial or cultural concordance of the provider, patient trust in medical care, as well as insurance and economic factors, but the patient’s perspective about orthopedic care has not been analyzed [7, 18–20].
The purpose of this sequential qualitative-quantitative mixed methods study was to identify concerns about arthroplasty from the patient’s perspective, then quantify and prioritize their concerns. Concerns identified in semi-structured interviews with Black and Hispanic patients with advanced symptomatic hip (HOA) and knee osteoarthritis (KOA) were used to develop a survey that we deployed to a wider population, to quantify and prioritize the concerns that may contribute to barriers to orthopedic care.
Methods
Design
This study employed a sequential 2-stage qualitative-quantitative research design, incorporating first a qualitative approach involving patient interviews and second a quantitative questionnaire administered to a prospective cohort. Study components were approved by the ethics committee of the Weill Cornell Institutional Review Board (WCM-IRB) [Protocol number: 1807019476]. All participants provided written informed consent and the study was undertaken in accordance with the Declaration of Helsinki.
Qualitative component
We developed a project-working group including staff and community patient partners to develop the interview topic guide. Black and Hispanic patients with advanced knee or hip OA patients with were identified by their treating physicians for recruitment. We used purposeful sampling within the federally qualified Long Island City Community Healthcare Network (LICCHN) where 43% of the population lives below the poverty level. We scheduled multiple focus groups but because of the COVID-19 pandemic lockdown after one focus group switched to semi-structured interviews.
The inclusion criteria for the semi-structured interviews and focus group were being ≥18 years of age, Black or Hispanic, an English speaker and have limiting pain and poor function defined by osteoarthritis relevant short forms of the hip disability and osteoarthritis outcome score (HOOS, JR) and knee injury and osteoarthritis outcome score (KOOS, JR) surveys (score > 60 on a 1–100 scale, higher = worse) [21, 22]. We excluded individuals with prior THR or TKR. We collected demographic and clinical information including age, sex, comorbidities, medications, and employment status in a pre-interview questionnaire.
Pre-interview questionnaire
We collected responses to a short questionnaire with participants of the interviews and focus group regarding their demographic information and medical history.
Qualitative topic guide and qualitative data analysis
The interview topic guide was informed by the Socioecological Framework [23] to elicit perspectives of Black and Hispanic individuals with advanced osteoarthritis of the hip or knee and their perceptions of THR and TKR. We pilot tested the topic guide with two individuals with severe osteoarthritis before recruiting participants for the semi-structured interviews. The topic guide was refined following pilot testing, and the data from the two individuals who piloted it were excluded from the final analysis (Supplementary Table S2). A trained investigator (INM) conducted and supervised the focus group and all interviews for the qualitative component. The interviews and focus group were recorded, transcribed verbatim and analyzed thematically by two independent coders (SRY; INM) using NVivo software Version 12. Following the initial two interviews, the independent coders addressed coding discrepancies and proceeded to code the remaining interviews using the same codebook. Semi-structured interviews were conducted and analyzed until no new themes emerged, indicating thematic saturation. The themes and quotes that emerged during the qualitative phase were used to develop the survey questions.
Quantitative component methods
We developed a survey informed by the qualitative data collected. The initial 30-question survey was scored on a five-level Likert scale (1 = Not at all important; 2 = A little important; 3 = Somewhat important; 4 = Very Important; 5 = Extremely important) [24]. The survey was translated to Spanish and deployed in both English and Spanish via email to patients identified at the Cornell Internal Medicine Practice and the rheumatology clinic at Hospital for Special Surgery, The Brooklyn Methodist Hospital, ArthritisPower [25], and the Global Healthy Living Foundation’s (GHLF) Spanish-language support network, CreakyJoints Español [26], between 2/27/2020 and 7/10/2022.
Quantitative survey statistical analysis
Descriptive statistics were employed to characterize the participants and determine the prevalence of the barriers to undergoing THR or TKR by race/ethnicity. Initial analysis profiled all 30 questions by race/ethnicity, and then calculated reliability metrics using Cronbach’s alpha for each theme. We then conducted a factor analysis to identify the dominant concerns about THR or TKR and reduce the number of factors to be listed for further analysis. We chose a final factor solution (where the eigenvalue was > 1) and subsequently rechecked the reliability of the updated factors. Finally, we calculated mean factor scores for each respondent using the variables with the highest factor loadings on an orthogonally rotated factor matrix. Our final questionnaire contained 21 questions across five themes (Table 1), with high reliability metrics (Cronbach’s alpha 0.75–0.97). Across all the 21 questions, less than 5% of respondents had missing data. Hence, all analysis has been performed on those respondents with complete information.
Table 1.
Barriers to Arthroplasty Survey
| The following statements are factors people think about when getting a joint replacement. Please check the box that shows how important these items would be if you were thinking about getting a joint replacement | |||||
|---|---|---|---|---|---|
| Not at all | A little | Somewhat | Very | Extremely | |
| Cost and Insurance | |||||
| Cost of a joint replacement | |||||
| Cost of the co-pay for a joint replacement | |||||
| Cost of a co-pay for physical therapy after joint replacement | |||||
| Insurance status | |||||
| Recovery | |||||
| Availability of someone to help me recover from a joint replacement | |||||
| Availability to take care of my family/friends while I undergo joint replacement | |||||
| Concern of being healthy enough to undergo joint replacement surgery | |||||
| Accessing transportation to get to physical therapy appointments | |||||
| Finding good physical therapy centers in my community | |||||
| Concerns about how hard the recovery after a joint replacement will be | |||||
| Trust in the surgeon | |||||
| Finding a surgeon I trust | |||||
| Figuring out how to find a qualified and experienced surgeon | |||||
| Finding a surgeon who understands what I need | |||||
| Surgical outcome | |||||
| Fear that I will need another joint replacement after the first one because I am young | |||||
| Fear that a joint replacement will not help me walk and function better | |||||
| Fear that the joint replacement will not improve my pain | |||||
| Timing | |||||
| Having a joint replacement is the last resort, and I think I should wait longer | |||||
| Having many medical problems and having a joint replacement is not a priority now | |||||
| Not doing everything I can do (like lose weight) to avoid having a joint replacement | |||||
| Not having bad enough joint pain to have a joint replacement | |||||
| Not having enough information to decide about having a joint replacement | |||||
We dichotomized each concern (factor) with the top two mean responses (4 = very important; 5 = extremely important) coded as 1 (very/extremely important) and the rest coded as 0 (Not as important). Each concern (factor) was categorized by race and ethnicity. We then conducted crude and multivariable analysis with each dichotomized factor used as a dependent variable in the model to determine the association between race/ethnicity and the importance of each factor, after adjusting for sex, insurance status, education level, HOOS, JR/KOOS, JR scores and discussion of joint replacement with a doctor. Logistic regression models were chosen after running linear and modified Poisson models based on the lowest AIC (Akaike Information Criterion) score, a measure that assesses the fit of the model.
Results
Qualitative interviews and focus group
Thematic saturation was achieved through the analysis of interviews conducted with one focus group and six individual semi-structured interviews (n = 8 individuals), held between 12/1/2018 and 9/19/2019 (9.8% of screened). There were six (75%) females (three Black, two Hispanic, one Asian/Other, mean age 58.9) and two (25%) males (one Black, one White, mean age 55 years), and all had severe KOA. We identified seven initial themes that captured the prominent concerns to proceed with THR and/or TKR. Themes included: trust in the surgeon, cost and insurance, surgical outcomes and improvement in pain and function after surgery, timing, trust in medical establishment and doctors, and recovery. Table 2 presents the themes with corresponding quotes and constructs from the socioecological framework.
Table 2.
Interview Themes Mapped to Socio Ecological Framework with Quotes
| Concerns about Arthroplasty | Socioecological Framework Construct | Interview Quotes |
|---|---|---|
| Cost and insurance | Cost of a joint replacement. (Structures and systems) |
“That is (cost) important … Because I’m only getting Social Security money. I don’t have any other income coming in. What’s the cost?” (P6) “I’m reluctant to see a specialist for my knee because I’ll have to see him once or twice a month and that’s a copay that I have to pay.” (P5) |
| Recovery | Availability of someone to help me recover, to take care of my family/friends. (Interpersonal) |
“If I have support that’s all because, to be honest, I don’t have anybody at home to support me right here because my children are grown. They’re all on their own. I would have to fight it all on my own.” (P4) “Well, if I get a knee replacement, I’m definitely going to need assistance, because I’ve got a handicapped daughter in my apartment. She is 50 years old. She’s having the problem walking because she has cerebral palsy.” (P1) |
| Finding good physical therapy centers in my community (Community or Institutions and Organizations) | “In my neighborhood there’s not really any places that are comprehensive in terms of, in terms of physical therapy or anything like that. They’re not really sophisticated or well-well-built places for physical therapy.” (FG1) | |
| Trust in surgeon | Finding a surgeon I trust. (Individual and Interpersonal) | “I would know how good the surgeon is. I would like to know some results of how many patients he had done things for and they’re still walking, how good a job he did with them, and does he still keep in contact with his patients.” (P1) |
| Figuring out how to find a qualified and experienced surgeon (Individual, Interpersonal, Institutional and Organization) | “ I would want an experienced surgeon. I would like to know about how many surgeries he has done, how long he’s been in that field, the hospital that he works at. How many successful rates are there with him?” (P3) | |
| Surgical outcome | Fear that a joint replacement will not help me walk and function better, will not improve my pain. (Individual) |
“ My outcome (from surgery) would have to be very important because I have to be sure that I’m going to be fine. It won’t be taking too long. I won’t be staying home too long.” (P4) “ If my walking will be improved (walking pain-free)”. (P6) |
| Timing | Having many medical problems and having a joint replacement is not a priority now. (Individual) | “I’ve been working on [deciding whether to have the surgery], but because there’s been other health issues that have been coming up with me, we’re trying to do one thing at a time.” (P2) |
| Not doing everything I can (like lose weight) to avoid having a joint replacement. | “ I need to work on my diet even more. I need to work on my little exercise, just my whole lifestyle needs to change. My weight plays a bit part in it, believe it or not. I know it does.” (P3) | |
| Mistrust | Having someone I know have a bad result from a joint replacement. (Interpersonal, Institutions and Organizations, Community) | “ After you see somebody that took the surgery and they’re not happy with it or anything like that, that sort of scare me. I wouldn’t go into the surgery right now. No.” (P6) |
| Not having any trust in doctors or hospitals. (Individual, Interpersonal, Organization) |
“Some of them (doctors) are in it for the money and some of them are in it because they genuinely care about their patients. Some are just not good at being doctors. Sometimes you get those too.” (FG1) “They didn’t really care, as long as I came to the appointment so that they could get paid or whatever the case may be. And you could tell that that’s what their main interest was, you know? But it’s because I’ve seen doctors, I’ve just seen doctors.” (FG1) |
Participant1,2,3,4,5,6- Patient numbers. FG1- Focus Group 1
Survey results
Between February 27, 2020, and July 10, 2022, 738 (24% response) participants returned surveys, primarily from HSS (Table 3). The majority were females and 19% of the participants were either Black or Hispanic. Due to the limited size and heterogeneity of the “Asian/Other” group, we refrain from further discussing this group although they were not excluded from the analysis. Average HOOS, JR score was 58.9 and KOOS, JR score was 51.7, indicating moderate to severe symptoms, with no difference in reported hip or knee pain between groups.
Table 3.
Characteristics of Survey Responders Grouped by Race/Ethnicitya
| Overall | Race Category | Significance Test* | |||
|---|---|---|---|---|---|
| Cohort N = 738 |
Black (B) N = 76 |
White (W) N = 556 |
Hispanic (H) N = 64 |
p-value | |
| Sociodemographic variables | |||||
| Age, years (mean, SD) | 59.3 (10.8) | 59.9 (13.4) | 59.8 (10.2) | 53.7 (9.8) | < 0.01 |
| Female (%) | 88.0 | 90.8 | 87.9 | 87.3 | |
| Education level (%) | |||||
| Some high school | 8.9 | 14.5 | 5.9 | 20.3 | < 0.01 |
| Some college | 37.7 | 51.3 | 35.3 | 34.4 | |
| College graduate | 53.5 | 34.2 | 58.0 | 45.3 | |
| Insurance statusb (%) | |||||
| Medicare | 46.2 | 50.0 | 48.8 | 32.8 | < 0.01 |
| Medicaid | 18.2 | 27.6 | 16.9 | 20.3 | |
| Private | 49.3 | 40.8 | 51.4 | 53.1 | |
| Uninsured | 4.9 | 7.9 | 3.4 | 10.9 | |
| Pain and disability attributed to arthritis (mean, SD) | |||||
| Pain in hip/knee (Y/N) (%) | 96.9 | 93.4 | 97.5 | 93.8 | < 0.1 |
| Pain VAS (0–100) (0–100) | 61.5 (23.0) | 65.7 (28.5) | 60.5 (21.9) | 60.6 (24.7) | < 0.05 |
| HOOS, JR (0–24) | 58.9 (23.9) | 61.3 (28.1) | 59.6 (20.0) | 55.2 (23.9) | < 0.1 |
| KOOS, JR (0–26) | 51.7 (20.3) | 50.3 (25.3) | 52.7 (19.8) | 49.0 (18.8) | < 0.05 |
| Providers seen to evaluate arthritis (%) | |||||
| Primary care physician | 48.0 | 39.5 | 51.8 | 42.2 | < 0.01 |
| Orthopedist | 47.6 | 56.6 | 48.9 | 35.9 | < 0.05 |
| Rheumatologist | 57.7 | 31.6 | 60.6 | 67.2 | < 0.01 |
| No one | 4.6 | 5.3 | 4.7 | 6.3 | |
| Other | 8.3 | 10.5 | 7.9 | 7.8 | |
| Discussed arthroplasty with provider | 51.4 | 65.8 | 52.5 | 29.7 | < 0.01 |
| Treatments tried for arthritis (%) | |||||
| Over the counter medication | 81.8 | 72.4 | 85.6 | 70.3 | < 0.01 |
| Physical therapy | 61.8 | 61.8 | 63.5 | 53.1 | |
| Acupuncture | 15.0 | 10.5 | 15.7 | 14.1 | |
| Braces | 24.5 | 23.7 | 25.5 | 20.3 | |
| Joint injection | 59.8 | 51.3 | 63.5 | 43.75 | < 0.01 |
| Topical creams/salves | 64.9 | 56.6 | 67.3 | 67.2 | |
| Prescription medication | 75.9 | 65.8 | 77.2 | 81.3 | < 0.1 |
| Other | 10.7 | 4.0 | 11.3 | 14.1 | |
| None | 2.6 | 5.3 | 2.3 | 3.1 | |
*Significance tests are Chi-square/Fisher’s exact tests comparing all race categories (Black, White, Hispanic)
aUnless otherwise stated, all values presented represent the percentage of participants per variable
bPatients can be on multiple insurance categories
A greater percentage of Blacks (57%) had visited an orthopedist compared to Hispanics (36%) or Whites (49%). Compared to Blacks and Hispanics, a larger percentage of White participants attempted to alleviate their symptoms through treatments such as over-the-counter pain medications, prescription medications, and joint injections.
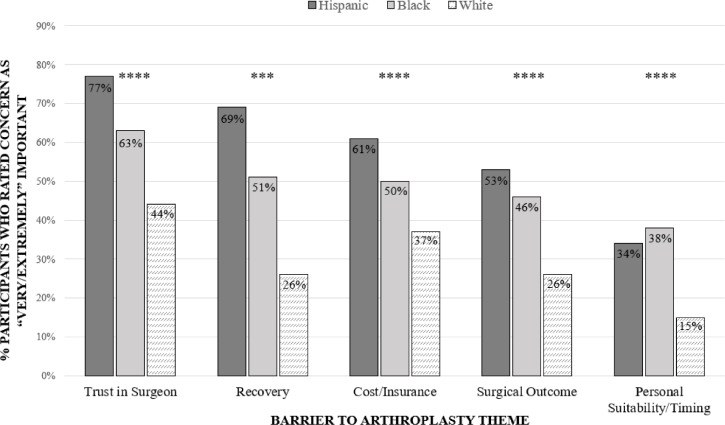
Factor analysis
The factor analysis resulted in five dominant themes identified as concerns for joint replacement: 1. Trust in the surgeon, 2. Recovery, 3. Cost and insurance, 4. Surgical outcome and 5. Timing. (Supplementary Table S1) Dichotomized scores very/extremely important vs. Not as important varied significantly by race and ethnicity, with p-values < 0.01 for all comparisons (Fig. 1). 63.2% of Blacks and 77.8% of Hispanics rated “Trust in the surgeon” as very/extremely important compared to 43.6% of Whites. “Recovery” was very/extremely important for 51.3% of Blacks, 69.8% of Hispanics, and 26.4% of Whites. “Cost and insurance” were very/extremely important for 59.3% of Blacks, 37.7% of Whites, and 61.9% of Hispanics. “Surgical outcome” was very/extremely important to 46.7% of Blacks, 26.6% of Whites, and 54.0% of Hispanics. “Timing” was rated very/extremely important by 36.5% of Blacks compared to 15.6% of White respondents.
Fig. 1.
Racial and Ethnic differences in proportion of Very/Extremely important ratings to the identified concerns to arthroplasty. Statistical significance markers: p < 0.1; * p < 0.05; ** p < 0.01; *** p < 0.001; ****p < 0.0001
After adjusting for sex, insurance status, education level, HOOS, JR/KOOS, JR scores and whether they have discussed the option of joint replacement with a doctor (Table 4), Blacks were two-fold more likely to consider “Trust in the surgeon” as very/extremely important compared to Whites (Adjusted Odds Ratio (aOR) 2.20, 95% CI 1.31, 4.70). Hispanics were more than four-fold more likely to rate “Trust in the surgeon” as very/extremely important compared to Whites (aOR 4.27, 95%CI 2.22,8.20). Blacks (aOR 2.85, 95% CI 1.67,4.86) had almost three-fold higher likelihood than Whites and Hispanics (aOR 6.52, 95% CI 3.49,12.18) had a six-fold greater likelihood than Whites of rating Recovery as very/extremely important. Blacks (aOR 2.27, 95% CI 1.33, 3.85) and Hispanics (aOR 2.73, 95% CI 1.54, 4.85) were twice as likely to rate “Surgical outcome” as very/extremely important compared to Whites. Blacks (aOR 3.92, 95% CI 2.16,7.13) were almost four times and Hispanics (aOR 2.20, 95% CI 1.19, 4.09) more than two-fold more likely to rate the “Timing” of the procedure as very/extremely important compared to Whites. “Cost and insurance” were similar between all racial and ethnic groups (Table 4).
Table 4.
Multivariable Logistic Regression Analysis Associating Race/Ethnicity with Barriers to Arthroplasty
| Barriers for joint replacement theme | Race/Ethnicity | Crude Odds Ratio (95 C.I.) | Adjusted Odds Ratio (95 C.I.)a |
|---|---|---|---|
| Trust in the surgeon | Black | 2.21 (1.35, 3.64) | 2.20 (1.31, 4.70) |
| Hispanic | 4.52 (2.44, 8.38) | 4.27 (2.22, 8.20) | |
| Asian/Other | 2.94 (1.42, 6.09) | 2.52 (1.11, 5.72) | |
| White | Reference | Reference | |
| Recovery | Black | 2.94 (1.80, 4.79) | 2.85 (1.67, 4.86) |
| Hispanic | 6.45 (3.65, 11.42) | 6.52 (3.49, 12.18) | |
| Asian/Other | 2.12 (1.08, 4.18) | 1.77 (0.81, 3.85) | |
| White | Reference | Reference | |
| Cost and insurance | Black | 1.61 (0.99, 2.61) | 1.54 (0.90, 2.65) |
| Hispanic | 2.69 (1.57, 4.60) | 1.73 (0.95, 3.14) | |
| Asian/Other | 1.57 (0.80, 3.05) | 1.10 (0.49, 2.45) | |
| White | Reference | Reference | |
| Surgical outcome | Black | 2.42 (1.48, 3.96) | 2.27 (1.33, 3.85) |
| Hispanic | 3.24 (1.91, 5.41) | 2.73 (1.54, 4.85) | |
| Asian/Other | 1.33 (0.65, 2.71) | 1.10 (0.49, 2.46) | |
| White | Reference | Reference | |
| Timing | Black | 3.12 (1.84, 5.28) | 3.92 (2.16, 7.13) |
| Hispanic | 2.91 (1.65, 5.13) | 2.20 (1.19, 4.09) | |
| Asian/Other | 1.31 (0.56, 3.09) | 1.18 (0.44, 2.74) | |
| White | Reference | Reference |
(a) Models adjusted for sex, education level, HOOS, JR KOOS, JR Score, Insurance Status, and discussion of knee/hip surgery with a doctor
Discussion
Trust in the surgeon, Recovery, Cost and insurance, Surgical outcome, and Timing for having knee replacement were the most important concerns with joint replacement among underrepresented minority groups of Blacks and Hispanics. Whites, Blacks and Hispanics also placed different values on each of these concerns. Hispanics had the highest likelihood of assigning “very/extremely important” to Trust in the surgeon, Recovery, Cost and insurance, and Surgical outcome compared to any other racial and ethnic group. The prevalence of these concerns rated very/extremely important ranged between 15 and 37% among White patients with Trust in the surgeon at 47% compared to 63.2% of Blacks and 77.8% of Hispanics. This emphasizes that the concerns regarding the use of THR or TKR vary greatly among racial and ethnic groups and the importance of addressing the concerns identified in this study to promote the use of THR and TKR among minority patients.
While many studies have benchmarked the persistent racial and ethnic disparities in arthroplasty utilization and outcomes linked to social factors such as social deprivation or race [3, 5, 27], there is little information about the concerns regarding arthroplasty utilization from the patients’ perspective. Furthermore, the duration between orthopedic referral and surgery is similar for White, Black, and Hispanic patients. However, Black and Hispanic patients present for arthroplasty later than White patients, with more severe preoperative pain and functional limitations, suggesting that different concerns between the groups studied may contribute to barriers to arthroplasty arising at multiple points throughout the care process [11, 28].
In this study, we found that a significantly higher proportion of Blacks and Hispanics than Whites rated Trust in the surgeon as a very/extremely important concern. While almost half of the patients in this study have seen an orthopedist, we have no data on physician race concordance. Race concordance improves trust and communication, and patients are more likely to participate in decision making when the physician is the same race [29, 30]. Given that Blacks represent only 6% of physicians overall and < 2% of the orthopedic surgeons, and Hispanics represent 18% of the population and 5% of physicians, it is unlikely that the Black and Hispanic patients were seen by Black or Hispanic orthopedists [31]. In a study of over 130,000 patients in the Kaiser system, only 10% of Blacks and 11% of Hispanics had the same race/ethnicity as their physicians, and only 24% of Spanish-speaking patients were linguistically concordant [32]. Although race and language concordance were not elicited as a concern during our interviews, it is possible that the concerns expressed by Black and Hispanic patients reflects prior experiences with race, language, and ethnicity discordant physicians.
It is also possible that minority groups know only about the resources available to them in their communities, like physical therapy (PT) centers. During the interviews, participants expressed that they had reservations about the quality of the medical facilities available in their community but were unsure where to find better options they could rely on. Blacks and Hispanics were markedly more likely to consider Recovery, a theme that encompasses post-operative physical therapy, including access to PT which is important for optimal arthroplasty outcomes, to be very/extremely important compared to Whites. Prior work using administrative data on almost 24,000 patients has demonstrated that Blacks and Hispanics are less likely to receive PT after TKR than Whites [33]. In a study holding focus groups 3 months after arthroplasty, Black and White participants described differences regarding barriers to PT that included economic factors such as co-pays and time off work, as well as difficulty finding transportation to PT sessions [34]. The basis for the disparity in utilization and access to PT during arthroplasty recovery is not known but may be contributing to the concerns about arthroplasty recovery described in our study. This highlights a less apparent potential barrier to arthroplasty, which is the difficulty in navigating the healthcare system and is reflected in the concerns expressed about surgical recovery.
Blacks and Hispanics endorsed concerns about caring for their family during their recovery as well as concerns about the availability of others to care for them. A study of long term unpaid caregivers who provided substantial help with healthcare found that caretakers are five times less likely to participate in personal activities as well as three times more likely to report a loss in work productivity compared to those not providing help [35]. As our cohort is demographically alike, similar concerns might be applicable.
Black and Hispanic participants were significantly more likely to rate very/extremely high importance to Surgical outcome and improving their pain and function than Whites. These concerns may accurately reflect the frequent use of hospitals with low arthroplasty volume, where many minority groups receive care that are associated with worse scores for pain and function, more frequent postoperative complications including emergency room visits for Blacks and Hispanics, and greater risk of revision surgery reported for Black patients [9, 36–39]. During the interviews, patients expressed concerns about joint replacement procedures, especially after learning about someone who experienced a negative outcome. They expressed uncertainty about identifying a suitable facility for joint replacement, aside from the one where a friend or a person known to them had a negative experience. Moreover, if they were aware of another option, they raised concerns about whether their insurance would cover the cost.
Most participants in all groups considered Timing of surgery related to medical optimization or symptom severity “not as important”, although twice as many Blacks and Hispanics reported “very/extremely important” concerns about medical problems, weight reduction, or “bad enough” pain compared to Whites. This concern may relate to disparities among Blacks and Hispanics regarding diabetes control, hypertension control, and the high prevalence of obesity and smoking which may preclude surgical clearance [40, 41]. Therefore, the barriers for utilization of joint replacement are related but not limited to the procedure for joint replacement but also to the disparities that exist across medical care for chronic conditions. Despite the recommendation of the American College of Rheumatology/American Association of Hip and Knee Surgeon Guideline advising against strict cutpoints for medical conditions [42], poor control of chronic conditions may make surgeons less likely to offer these procedures to these patients until they achieve better glycemic control or better weight [43, 44], while many of them lack the access or best resources to achieve those goals.
While a majority of Hispanics considered Cost and insurance to be a “very/extremely important” factor, only half of Black participants and fewer White participants considered cost and insurance to be “very/extremely important”. The association of higher levels of social deprivation or Medicaid insurance with lower levels of arthroplasty utilization is well described [45, 46] but an experimental hospital reimbursement model aimed to increase access to TKR did not increase TKR utilization among low-income patients [47]. The importance of Cost and insurance from the patient’s perspective includes concerns about co-pays for both the procedure as well as factors during recovery like PT.
One strength of this study is our mixed methods approach. We developed the survey using data obtained through carefully analyzed interviews among underrepresented minority groups living in an impoverished community. The survey was then widely distributed and enabled us to quantify and prioritize the identified barriers in a larger population across multiple sites and multiple states across the USA, improving the generalizability of our results.
A limitation of this study was due to the COVID-19 pandemic, which prevented use of focus groups as originally planned and led to the use of semi-structured phone interviews. Despite this limitation, thematic saturation was achieved. We also faced challenges in obtaining questionnaire responses from Black and Hispanic individuals. To address this, the study reached out to Creaky Joints Español, a Spanish language support group, and Brooklyn Methodist Hospital, a predominantly Black community practice, which increased the non-white response to almost 25% of participants. The consistency of views on the barriers to arthroplasty between the qualitative phase and survey phase in the Black and Hispanic participants, despite representing 25% of responses, indicates that the survey did capture the major concerns about arthroplasty for the Black and Hispanic population. The survey response rate was low overall, as would be expected in our target population. However, since we have no information on non-respondents, it is not possible to determine if there were meaningful differences between groups. Additionally, our Hispanic cohort was largely recruited from the highly engaged Creaky Joints Spanish Language Support Group, which may have influenced our results. As we did not require a validated diagnosis of arthritis in survey participants, we may have included those who would not have a condition treatable by joint replacement. However, we wanted to include those who thought they had symptomatic arthritis of the hip or knee to understand their concerns about arthroplasty, including potential delays in initial consultation for diagnosis.
Conclusion
In summary, we have identified concerns about arthroplasty from the patients’ perspective and report that there are significant differences between Blacks, Hispanics, and Whites in the factors that are most important to them. Solutions to joint replacement utilization disparities will require addressing those concerns that emerged from this study that may contribute to barriers to care, such as access to qualified physicians. Additionally, addressing health disparities related to the treatment of chronic conditions, which were identified as barriers for the utilization of joint replacement in the Black and Hispanic population, is also necessary.
Supplementary Information
Acknowledgements
There are no acknowledgements.
Abbreviations
- GHLF
Global healthy living foundation
- THR
Total hip replacement
- TKR
Total knee replacement
- OA
Osteoarthritis
- HOA
Hip osteoarthritis
- KOA
Knee osteoarthritis
- HOOS, JR
Short form of hip disability and osteoarthritis outcome score
- KOOS, JR
Short form of knee injury and osteoarthritis outcome score
- LICCHN
Long island city community healthcare network
- AIC
Akaike information criterion
- aOR
Adjusted odds ratio
- PT
Physical therapy
- WCM-IRB
Weill cornell institutional review board
Authors’ contributions
S.M.G., I.N.M., L.R., A.B., M.F., M.L.P. and B.M. conceived the research idea and designed the study. I.N.M., C.B., H.T., S.R.Y., A.C., P.L., G.L., W.B.N. and S.V., recruited patients and conducted the semi-structured interviews with patients and analyzed the data. I.N.M., S.R.Y., S.M.G. and M.R. developed and analyzed the questionnaire based on the interview findings. C.B., J.A.B.G., and I.M. collected and compiled the survey responses. M.R. and I.M. conducted statistical analyses on the questionnaire data and prepared Tables 1, 2, 3, 4, Fig. 1, and supplementary tables 1 and 2. S.M.G. and I.M. reviewed the literature and provided background information. S.M.G., I.N.M., S.R.Y., M.R., J.A.B.G. and I.M. prepared the manuscript. All authors have reviewed, provided feedback, and approved the submitted version.
Funding
This work was supported by the Cornell Center for Health Equity Pilot Project [1807019476].
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Study components were approved by the ethics committee of the Weill Cornell Institutional Review Board (WCM-IRB) [Protocol number: 1807019476]. All participants provided written informed consent and the study was undertaken in accordance with the Declaration of Helsinki. Written informed consent to participate was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
I.N.M receives advisory board honoraria from Sobi (Swedish Orphan Biovitrum AB). S.V. is employed by Global Healthy Living Foundation (GHLF), a nonprofit that has received research funding from various pharmaceutical companies including AbbVie, Amgen, BMS, Eli Lilly, and Pfizer. GHLF receives grants and sponsorships from multiple organizations, and a full list of funders is available on their website. S.M.G., I.M., J.A.B.G, M.R., A.B., L.R., B.M., M.F., M.L.P, W.B.N., C.B., G.L., A.C., P.L, H.T., and S.R.Y. declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Allen KD. Racial and ethnic disparities in osteoarthritis phenotypes. Curr Opin Rheumatol. 2010;22(5):528–532. doi: 10.1097/BOR.0b013e32833b1b6f. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez PM, McKeon JF, Spitzer AI, et al. Race, utilization, and outcomes in Total hip and knee arthroplasty: a systematic review on health-care disparities. JBJS Rev. 2022;10(3) 10.2106/JBJS.RVW.21.00161. [DOI] [PubMed]
- 3.Callahan LF, Cleveland RJ, Allen KD, Golightly Y. Racial/ethnic, socioeconomic, and geographic disparities in the epidemiology of knee and hip osteoarthritis. Rheum Dis Clin N Am. 2021;47(1):1–20. doi: 10.1016/j.rdc.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okike K, Chang RN, Royse KE, Paxton EW, Navarro RA, Hinman AD. Association between race/ethnicity and Total joint arthroplasty utilization in a universally insured population. J Am Acad Orthop Surg. 2022;30(20):e1348–e1357. doi: 10.5435/JAAOS-D-22-00146. [DOI] [PubMed] [Google Scholar]
- 5.Zhang W, Lyman S, Boutin-Foster C, et al. Racial and ethnic disparities in utilization rate, hospital volume, and perioperative outcomes after Total knee arthroplasty. J Bone Joint Surg Am. 2016;98(15):1243–1252. doi: 10.2106/JBJS.15.01009. [DOI] [PubMed] [Google Scholar]
- 6.Soares RW, Emara AK, Orr M, et al. When Do we perform elective Total knee arthroplasty? General and demographic-specific trends of preoperative pain and function among 10,327 patients. J Knee Surg. Published online December. 2022;23 10.1055/s-0042-1758774. [DOI] [PubMed]
- 7.Amen TB, Dee EC, Arega MA, et al. Racial and ethnic disparities in access to culturally competent Care in Patients with joint pain in the United States. J Gen Intern Med. 2022;37(3):682–685. doi: 10.1007/s11606-021-06760-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis. 2014;73(12):2107–2115. doi: 10.1136/annrheumdis-2013-203494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bass AR, Do HT, Mehta B, et al. Assessment of racial disparities in the risks of septic and aseptic revision Total knee replacements. JAMA Netw Open. 2021;4(7):e2117581. doi: 10.1001/jamanetworkopen.2021.17581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodman SM, Mehta B, Zhang M, et al. Disparities in Total hip arthroplasty outcomes: census tract data show interactions between race and community deprivation. J Am Acad Orthop Surg. 2018;26(21):e457–e464. doi: 10.5435/JAAOS-D-17-00393. [DOI] [PubMed] [Google Scholar]
- 11.Goodman SM, Mandl LA, Parks ML, et al. Disparities in TKA outcomes: census tract data show interactions between race and poverty. Clin Orthop. 2016;474(9):1986–1995. doi: 10.1007/s11999-016-4919-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen-Levy WB, Lans J, Salimy MS, Melnic CM, Bedair HS. The significance of race/ethnicity and income in predicting preoperative patient-reported outcome measures in primary Total joint arthroplasty. J Arthroplast. 2022;37(7S):S428–S433. doi: 10.1016/j.arth.2022.02.041. [DOI] [PubMed] [Google Scholar]
- 13.Salimy MS, Humphrey TJ, Katakam A, Melnic CM, Heng M, Bedair HS. Which factors are considered by patients when considering Total joint arthroplasty? A Discrete-choice Experiment. Clin Orthop. 2023;481(3):427–437. doi: 10.1097/CORR.0000000000002358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goodman SM, Mehta B, Mirza SZ, et al. Patients’ perspectives of outcomes after total knee and total hip arthroplasty: a nominal group study. BMC Rheumatol. 2020;4:3. doi: 10.1186/s41927-019-0101-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hadad MJ, Rullán-Oliver P, Grits D, et al. Racial disparities in outcomes after THA and TKA are substantially mediated by socioeconomic disadvantage both in black and white patients. Clin Orthop. 2023;481(2):254–264. doi: 10.1097/CORR.0000000000002392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mota REM, Tarricone R, Ciani O, Bridges JFP, Drummond M. Determinants of demand for total hip and knee arthroplasty: a systematic literature review. BMC Health Serv Res. 2012;12:225. doi: 10.1186/1472-6963-12-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ibrahim SA, Blum M, Lee GC, et al. Effect of a decision aid on access to Total knee replacement for black patients with osteoarthritis of the knee: a randomized clinical trial. JAMA Surg. 2017;152(1):e164225. doi: 10.1001/jamasurg.2016.4225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Terlizzi EP, Connor EM, Zelaya CE, Ji AM, Bakos AD. Reported importance and access to health care providers who understand or share cultural characteristics with their patients among adults, by race and ethnicity. Natl Health Stat Rep. 2019;130:1–12. [PubMed] [Google Scholar]
- 19.Riviere P, Kalavacherla S, Banegas MP, et al. Patient perspectives of prostate cancer screening vary by race following 2018 guideline changes. Cancer. 2023;129(1):82–88. doi: 10.1002/cncr.34530. [DOI] [PubMed] [Google Scholar]
- 20.Guzek R, Goodbody CM, Jia L, et al. Implicit racial Bias in pediatric Orthopaedic surgery. J Pediatr Orthop. 2022;42(7):393–399. doi: 10.1097/BPO.0000000000002170. [DOI] [PubMed] [Google Scholar]
- 21.Lyman S, Lee YY, Franklin PD, Li W, Cross MB, Padgett DE. Validation of the KOOS, JR: a short-form knee arthroplasty outcomes survey. Clin Orthop. 2016;474(6):1461–1471. doi: 10.1007/s11999-016-4719-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lyman S, Lee YY, Franklin PD, Li W, Mayman DJ, Padgett DE. Validation of the HOOS, JR: a short-form hip replacement survey. Clin Orthop. 2016;474(6):1472–1482. doi: 10.1007/s11999-016-4718-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark VLP, Ivankova NV. Mixed methods research: a guide to the field. SAGE Publications; 2015. [Google Scholar]
- 24.Likert Scale Definition, Examples and Analysis. Published November 3, 2022. Accessed March 11, 2023. https://simplypsychology.org/likert-scale.html.
- 25.About ArthritisPower – CreakyJoints [Internet]. [cited 2023 Apr 17]. Available from: https://creakyjoints.org/research/arthritispower/.
- 26.Staff G. CreakyJoints® Español Prioritizes Culturally Relevant Rheumatoid Arthritis (RA) Education with New Digital Guide [Internet]. GHLF.org . 2022 [cited 2023 Apr 12]. Available from: https://ghlf.org/ghlf-news/creakyjoints-espanol-prioritizes-culturally-relevant-rheumatoid-arthritis-ra-education-with-new-digital-guide/.
- 27.Rudisill SS, Varady NH, Birir A, Goodman SM, Parks ML, Amen TB. Racial and ethnic disparities in Total joint arthroplasty care: a contemporary systematic review and Meta-analysis. J Arthroplast. 2023;38(1):171–187.e18. doi: 10.1016/j.arth.2022.08.006. [DOI] [PubMed] [Google Scholar]
- 28.Amen TB, Liimakka AP, Jain B, Rudisill SS, Bedair HS, Chen AF. Total joint arthroplasty utilization after Orthopaedic surgery referral: identifying disparities along the care pathway. J Arthroplast. 2023;38(3):424–430. doi: 10.1016/j.arth.2022.09.020. [DOI] [PubMed] [Google Scholar]
- 29.Shen MJ, Peterson EB, Costas-Muñiz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5(1):117–140. doi: 10.1007/s40615-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saha S, Beach MC. Impact of physician race on patient decision-making and ratings of physicians: a randomized experiment using video vignettes. J Gen Intern Med. 2020;35(4):1084–1091. doi: 10.1007/s11606-020-05646-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Census Bureau QuickFacts: United States. Accessed March 11, 2023. https://www.census.gov/quickfacts/fact/table/US/PST045222.
- 32.Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25(11):1172–1177. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ratnasamy PP, Oghenesume OP, Rudisill KE, Grauer JN. Racial/ethnic disparities in physical therapy utilization after Total knee arthroplasty. J Am Acad Orthop Surg. Published online February. 2023;1 10.5435/JAAOS-D-22-00733. [DOI] [PMC free article] [PubMed]
- 34.Bove AM, Dong E, Hausmann LRM, et al. Exploring race differences in satisfaction with rehabilitation following Total knee arthroplasty: a qualitative study. J Gerontol A Biol Sci Med Sci. 2022;77(2):e48–e55. doi: 10.1093/gerona/glab132. [DOI] [PubMed] [Google Scholar]
- 35.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A National Profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016;176(3):372–379. doi: 10.1001/jamainternmed.2015.7664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Losina E, Wright EA, Kessler CL, et al. Neighborhoods matter: use of hospitals with worse outcomes following total knee replacement by patients from vulnerable populations. Arch Intern Med. 2007;167(2):182–187. doi: 10.1001/archinte.167.2.182. [DOI] [PubMed] [Google Scholar]
- 37.Mehta BY, Bass AR, Goto R, et al. Disparities in outcomes for blacks versus whites undergoing Total hip arthroplasty: a systematic literature review. J Rheumatol. 2018;45(5):717–722. doi: 10.3899/jrheum.170855. [DOI] [PubMed] [Google Scholar]
- 38.Hinman AD, Chan PH, Prentice HA, Paxton EW, Okike KM, Navarro RA. The Association of Race/ethnicity and Total knee arthroplasty outcomes in a universally insured population. J Arthroplast. 2020;35(6):1474–1479. doi: 10.1016/j.arth.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Goodman SM, Parks ML, McHugh K, et al. Disparities in outcomes for African Americans and whites undergoing Total knee arthroplasty: a systematic literature review. J Rheumatol. 2016;43(4):765–770. doi: 10.3899/jrheum.150950. [DOI] [PubMed] [Google Scholar]
- 40.Wu M, Belay E, Cochrane N, O'Donnell J, Seyler T. Comorbidity burden contributing to racial disparities in outpatient versus inpatient Total knee arthroplasty. J Am Acad Orthop Surg. 2021;29(12):537–543. doi: 10.5435/JAAOS-D-20-01038. [DOI] [PubMed] [Google Scholar]
- 41.Carender CN, DeMik DE, Elkins JM, Brown TS, Bedard NA. Are body mass index cutoffs creating racial, ethnic, and gender disparities in eligibility for primary Total hip and knee arthroplasty? J Arthroplast. 2022;37(6):1009–16.42. doi: 10.1016/j.arth.2022.02.013. [DOI] [PubMed] [Google Scholar]
- 42.Hannon CP, Goodman SM, Austin MS, et al. 2023 American College of Rheumatology and American Association of hip and knee surgeons clinical practice guideline for the optimal timing of elective hip or knee arthroplasty for patients with symptomatic moderate-to-severe osteoarthritis or advanced symptomatic osteonecrosis with secondary arthritis for whom nonoperative therapy is ineffective. Arthritis Care Res (Hoboken). 2023;75(11):2227–2238. doi: 10.1002/acr.25175. [DOI] [PubMed] [Google Scholar]
- 43.Dlott CC, Metcalfe T, Jain S, Bahel A, Donnelley CA, Wiznia DH. Preoperative risk management programs at the top 50 Orthopaedic institutions frequently enforce strict cutoffs for BMI and hemoglobin A1c which may limit access to Total joint arthroplasty and provide limited resources for smoking cessation and dental care. Clin Orthop Relat Res. 2022;481. [DOI] [PMC free article] [PubMed]
- 44.Wang AY, Wong MS, Humbyrd CJ. Eligibility criteria for lower extremity joint replacement may worsen racial and socioeconomic disparities. Clin Orthop Relat Res. 2018;476(12):2301–2308. doi: 10.1097/CORR.0000000000000511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karimi A, Burkhart RJ, Hecht CJ, Acuña AJ, Kamath AF. Is social deprivation associated with usage, adverse events, and patient-reported outcome measures in Total joint arthroplasty? A Systematic Review. Clin Orthop. 2023;481(2):239–250. doi: 10.1097/CORR.0000000000002394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim CY, Wiznia DH, Hsiang WR, Pelker RR. The effect of insurance type on patient access to knee arthroplasty and revision under the affordable care act. J Arthroplast. 2015;30(9):1498–1501. doi: 10.1016/j.arth.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 47.Wilkie WA, Mohamed NS, Remily EA, et al. Access to Total knee arthroplasty among patients with low incomes has not increased under global budget revenue. Orthopedics. 2022;45(1):e11–e16. doi: 10.3928/01477447-20211124-03. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.