Abstract
Purpose
We assess whether the sequential mediating effects of self-efficacy and depressive symptoms on the relationship between community efficacy for non-communicable disease management (COEN) and medication adherence and whether these relationships differed by sex and age.
Patients and Methods
Overall, 662 individuals from 12 communities in China were interviewed twice 1 year apart. Serial mediation analysis examined whether the relationship between COEN and medication adherence was mediated by self-efficacy and depressive symptoms. Model invariance across sex and age groups was assessed using multi-group analysis.
Results
Serial mediation analysis indicated that self-efficacy and depressive symptoms sequentially mediated relationship between COEN and medication adherence. Multi-group analysis by sex showed that the path from self-efficacy to medication adherence was significant only for females and from depressive symptoms to medication adherence was significant only for males.
Conclusion
Interventions that enhance individual self-efficacy may be beneficial in decreasing depressive symptoms and improving medication adherence.
Keywords: medication adherence, neighborhood, community, self-efficacy, depressive symptoms, non-communicable chronic diseases, social cognitive theory, China
Introduction
Medication adherence refers to how well a patient follows a prescribed medication regimen.1 It is an important factor in the control of non-communicable chronic diseases (NCDs). Yet, various studies have reported modest levels (as low as 38%) of medication adherence among patients with hypertension and/or diabetes.2,3 Such low levels of medication adherence can lead to an increase in morbidity and mortality associated with these NCDs, which can, in turn, lead to additional disease burdens and unnecessary use of healthcare resources.4 Thus, identification of factors associated with NCD medication non-adherence is important to guide interventions to improve health outcomes.
Neighborhood characteristics are structural social determinants of health behaviors.5 Numerous studies have assessed the connection between neighborhood characteristics (eg, neighborhood environment) and health-related behaviors, including physical activity,6 smoking,7 and alcohol use.8 A recent meta-analysis found that perceived neighborhood disorder was consistently associated with substance abuse.9 Only a few studies have examined the potential effects of neighborhood characteristics (eg, neighborhood socioeconomic status) on medication adherence.10,11 A notable research gap persists in examining the relationship between neighborhood characteristics and medication adherence,5 there is motivation to address this gap in the literature and understand if neighborhood characteristics influence medication adherence, particularly among individuals with NCD.
Social cognitive theory (SCT) suggests that psychological factors play pivotal roles in explaining the impact of sociostructural factors (eg, community characteristics) on health behaviors.12 Sociostructural factors might not exert a direct impact on health behaviors (eg, medication adherence) but rather influence them through various psychological mechanisms, notably self-efficacy.12,13 Self-efficacy reflects an individual’s beliefs about how much control they have over events affecting their lives.14 By integrating insights from collective efficacy—a community-level theory,15 and research on neighborhood effects on self-efficacy,10,16,17 it appears that individuals experiencing favorable conditions in their communities are likely to improve their confidence in achieving both current and future goals. Therefore, it is possible that self-efficacy can serve as a mediator between neighborhood characteristics and medication adherence in patients with NCDs.
A growing body of research has been dedicated to comprehending the influence of neighborhood environments influence mental well-being.18,19 Although the association between neighborhood characteristics (eg, neighborhood social cohesion and social engagement) and depression has been extensively explored, there is limited knowledge about this linkage in China and the fings findings from China are inconclusive. Perceived neighborhood social cohesion was associated with subsequent depression over the 4-year follow-up period.20 However, a recent review underscores that more cohesive relationships can, at times, be linked to unfavorable well-being outcomes (eg, depressive symptoms).21 SCT posits that there is a link between self-efficacy and depressive symptoms.22 Correspondingly, some previous studies have indicated that self-efficacy can predict depressive symptoms.23,24 Thus, a mechanism linking neighborhood characteristics with medication adherence may involve self-efficacy and depressive symptoms.
The effect that sex and age can have on medication adherence has been evaluated extensively, but a clear conclusion has not yet been reached.25,26 A systematic review exploring potential sociodemographic factors influencing medication adherence among adult patients with chronic diseases suggests that the observed impact of sex on medication adherence is not consistent. Furthermore, age seems to exhibit an inverse u-shaped relationship with medication adherence, with the lowest levels observed in both very young and elderly individuals.26 Relatively few investigations into sex and age differences in neighborhood contextual effects have been conducted. Previous research found that sex and age were significant moderators in the relationship between perceptions of neighborhood environment (eg, crime/safety) and health behaviors, with older women showing stronger associations than younger men.27 In general, women tend to have higher levels of self-efficacy and lower levels of depressive symptoms compared to men.28 Therefore, there may be age and sex differences in the mediation pathway between neighborhood characteristics, self-efficacy, depressive symptoms, and medication adherence.
Most of the literature on predictors of medication adherence has focused on personal demographic factors using a cross-sectional study design. The theoretical underpinnings of many studies are weak, particularly as few studies use SCT to investigate how neighborhood characteristics affect medication adherence.29 Perceived measures have also been associated with the physical health of relevant individuals.5,9,30 Some of the study focused on physical factors,9 while others focused on social factors.5,30 Neighborhoods vary in their social and physical characteristics, and these characteristics need to be measured to determine how neighborhood characteristics affect health behaviors. In our previous research, we developed and validated a novel community efficacy for NCD management (COEN) scale for assessing individual perceptions of community-level COEN.31–33 The scale can be used to collect data on individual-level perceptions of the five aspects of neighborhood characteristics associated with NCD management.34
During our literature search, we were unable to identify any longitudinal studies that examined the mediating influence of self-efficacy and depressive symptoms on the relationship between neighborhood characteristics and medication adherence among patients with type 2 diabetes and/or hypertension patients. The aims of this study using longitudinal data, collected twice 1 year apart, were to 1) explore whether self-efficacy and depressive symptoms play serial-mediation roles in the relationship between COEN and medication adherence among type 2 diabetes and/or hypertension patients in China and 2) assess whether the serial mediating role of self-efficacy and depressive symptoms between COEN and medication adherence differed by age and sex. We hypothesize that: 1) self-efficacy mediates the association between COEN and medication adherence; 2) depressive symptoms mediate the association between COEN and medication adherence; 3) self-efficacy and depressive symptoms sequentially mediate the association between COEN and medication adherence; and 4) the sequential mediating roles of self-efficacy and depressive symptoms between COEN and medication adherence differ by sex and age.
Material and Methods
Study Design and Setting
An observational longitudinal survey was conducted at 12 community health service (CHS) centers from June 2019 to October 2020 in three cities (Kunshan, Taicang, and Shanghai) in Shanghai municipality and Jiangsu province, China. We selected 12 CHS centers covering communities of diverse socioeconomic status while considering population size, per capita disposable income (eg, wages, pensions, part-time jobs, etc.), and level of urbanization.
Participants and Procedures
We randomly sampled participants with type 2 diabetes or hypertension from an electronic health record system managed by the community health service centres in the 12 communities. Inclusion criteria were as follows: diagnosed with hypertension or type 2 diabetes by a health professional; aged ≥45 years; lived in the community for at least 6 months in the past year; and expected to continue to live in the community for the next 2 years. Those who had physical or intellectual disabilities or other interfering conditions were excluded. For participants who met our inclusion criteria and agreed to participate in the study, stratified random sampling was conducted based on sex (male: female = 1:1) and disease diagnosis (hypertension: type 2 diabetes = 1:1).
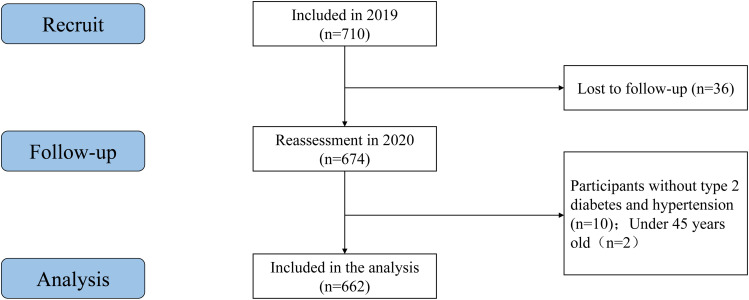
Data were collected at two-time points: baseline (T1; data collected between June and September 2019) and at one-year follow-up (T2; data collected between August and October 2020). The survey items included demographics questionnaire, the Self-Efficacy to Managing Chronic Disease Scale (SEMCD), the 9-item Patient Health Questionnaire (PHQ-9), and the Community efficacy for NCD management (COEN) Scale. For this analysis, baseline values of COEN, follow-up values of self-efficacy and depressive symptoms, baseline and follow-up values of medication adherence, and baseline values of sociodemographic variables were considered. Figure 1 illustrates the process of selecting the study sample.
Figure 1.
Flowchart of the screening process for the selection of eligible participants.
A total of 662 participants who completed the survey on COEN (T1), self-efficacy (T2), depressive symptoms (T2), and other covariates (T1) were included in the present study. A total of 626 participants had complete data for medication adherence (T2). Trained interviewers conducted face-to-face interviews with all enrolled patients in the included communities. All participants signed a consent form after being informed about the study’s goals. The survey lasted on average 20 min. Upon completion of the questionnaires, the participants were encouraged to verify that all items were completed and received small appreciation gifts.
Measure Variables and Tool
Community Efficacy for NCD Management (at Baseline)
COEN, defined as “the ability of a community to provide NCD management for its residents.” Assessments were done using the COEN scale, which measures the ability of a community to provide NCD management as perceived by residents. The COEN scale was developed and validated in a three-step process. First, a thorough literature review and expert interviews were conducted to establish the conceptual framework of COEN and initial scale items, drawing from existing literature.31 Second, two rounds of Delphi panels were organized to select scale items, ensuring good face validity.32 Thirdly, two community-based surveys collected data from 345 and 657 individuals, respectively, and confirmed the scale’s desirable internal consistency (overall Cronbach’s α=0.86), test–retest reliability (Kappa value >0.2 for all items), and structural validity (a five-factor structure representing five dimensions of the scale).33,34
As illustrated in Table S1, the scale has 38 items covering 5 dimensions: community physical environment (9 items), behavioral risk factors (11 items), mental health and social relationships (6 items), community health management (5 items), and community organizations and activities (7 items). All items were measured using a 5-point Likert scale. Positive items beneficial to COEN range from 1 (not positive) to 5 (extremely positive), while negative items unfavourable to COEN range from 1 (not negative) to 5 (extremely negative), with higher summed scores representing a community’s stronger ability to provide NCD management for its residents. In the current study, the mean score of all items was calculated as the COEN score.
Self-Efficacy (at Follow-Up)
Self-efficacy was considered the first mediator. The Self-Efficacy to Managing Chronic Disease Scale (SEMCD) was used to assess the self-efficacy of participants in preventing mental distress, pain, fatigue, physical discomfort, and other symptoms that interfere with their goals.35 The overall score is the sum of the six items’ scores, each of which ranges from 10 (very confident) to 1 (not confident). In this study, the mean score of these six items was calculated as the self-efficacy score. We calculated its internal consistency to be α = 0.82 for our sample.
Depressive Symptoms (at Follow-Up)
Depressive symptoms were considered as the secondary mediator. The 9-item Patient Health Questionnaire (PHQ-9) was used to assess depression.36 The scale has nine items and one dimension. Each item is scored from 3 (nearly every day) to 0 (not at all). The final score ranged from 0 to 27. In this study, the mean score of the nine items was calculated as the depressive symptoms score. We calculated its internal consistency to be α = 0.77 for our sample.
Medication Adherence (Both at Baseline and at Follow-Up)
The Chinese version of the Morisky Green-Levine Scale (MGLS) was used for this study – this scale has been widely used and has been demonstrated to be valid.37 The MGLS scale consists of four questions, each posed in the reverse direction to mitigate social desirability bias.37 MGLS is a 4-item scale that measures medication nonadherence among patients with chronic health conditions. By inquiring about forgetfulness or carelessness, the MGLS assesses unintentional facets of medication non-adherence. Additionally, the two questions relating to cessation of prescribed medications when feeling better or worse target the intentional aspects of medication non-adherence.37 Based on the yes/no response to each question, the items were rated as 1 or 0. Giving a total score of 0–4. In this study, the mean score of all items was calculated as the medication adherence score.
Statistical Analyses
Frequencies and percentages were calculated for categorical variables. Means and standard deviations (SD) were calculated for continuous variables. Pearson correlation analysis was performed to evaluate correlations among all study variables. The proposed serial mediation model (see Figure 2) was step-by-step tested using a structural equation modeling (SEM) framework. Specifically, three regression models were developed, with self-efficacy, depressive symptoms, and medication adherence as outcome variables using multiple linear regressions. To distinguish between variables that changed between follow-up and baseline from those that did not, baseline values were used to adjust the outcome variables during follow-up.38 The adjustment was conducted using the outcome’s baseline values in the path model as a covariate. Additionally, demographic variables, such as age, sex, and education level, were included as covariates in the serial mediation model and regressed on both the outcome and intermediate variables.
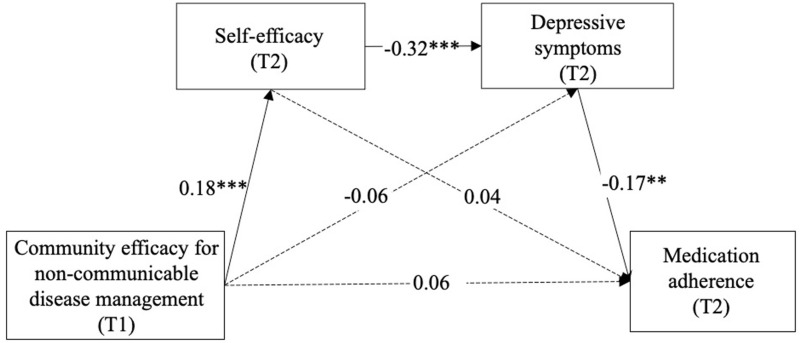
Figure 2.
The serial mediation model (N = 626). Values are standardized coefficients. Model fit statistics: Good fit; χ2/df = 1.33, CFI = 0.997, TLI = 0.973, RMSEA = 0.023, SRMR = 0.014. Paths between each covariate (sex, age, education, and baseline medication adherence) in the model are not displayed. Solid-lined curves represent statistical significance. T1 = Time 1; T2 = Time 2. **p < 0.01, ***p < 0.001.
A bias-corrected nonparametric percentile bootstrap analysis was used to confirm the mediating effect and estimate the 95% confidence interval with 1000 repetitions. The strength of correlations (standardized beta coefficients, β) and their significance level (p value) are reported in path diagrams. The model fit statistics are considered to be good when the comparative fit index (CFI) ≥0.95, Chi-squared ratio (χ2/df) ≤3, the root mean squared error of approximation (RMSEA) ≤0.05, the Tucker-Lewis index (TLI) ≥0.95, and the standardized root mean squared residual (SRMR) ≤0.08.39,40
Multi-group invariance analysis was performed to determine whether the mediation model was invariant across sex or age groups. Analyses were stratified by age into middle-aged (40–64 years) and older adults (65 years and above).41,42 This study compared the two models separately: (1) an unconstrained model (M1) with all regression paths allowed to be unequal across sex and age, and (2) a constrained model (M2) with all regression paths constrained to be identical across sex and age. Multi-group analysis by sex was adjusted for age, and multi-group analysis by age was adjusted for sex. Because the sample size greatly affects χ2, the RMSEA and CFI were used as criteria for model comparisons. We accept the null hypothesis of invariance if ΔRMSEA < 0.015 and ΔCFI < 0.01 between the more and less restrictive models. The equality assumption for all model coefficients across the two groups was considered untenable when the fully constrained model (ie, M2) had a significantly worse fit than the unconstrained model (ie, M1). If this happens, a Wald test statistic is used to examine each regression path. This allowed us to identify which model coefficients differed across the groups.
Descriptive analyses were conducted using SPSS v26.0 (IBM, Armonk, NY, USA). Bootstrap analyses and multi-group modeling analysis were conducted in Mplus version 8.3 (Muthén & Muthén, Los Angeles, CA). All statistical analyses used two-tailed tests of significance and a significance level of 0.05.
Results
Correlation and Descriptive Analyses
Table 1 depicts the sample characteristics at T1 and the descriptive statistics of the variables used at T1 and T2. The study included 319 (48.2%) females and 342 (51.8%) males. The majority of the subjects were aged 40–64 years (52.7%) and had completed secondary school or higher education (51.5%). Table 2 shows the correlation matrix for the variables used in the analyses. Both COEN and self-efficacy were positively correlated with medication adherence at T2 (for COEN, r = 0.09, p < 0.05; for self-efficacy, r = 0.12, p < 0.01). Depressive symptoms were negatively correlated with COEN (r = −0.11, p < 0.01), self-efficacy (r = −0.35, p < 0.001), and medication adherence at T2 (r = −0.19, p< 0.001).
Table 1.
Descriptive Statistics of the Study Participants, 2019 (T1), 2020 (T2), N = 662
| Measures | Mean (SD) or n (%) |
|---|---|
| T1 measures | |
| Sex, n (%) | |
| Male | 342 (51.8%) |
| Female | 319 (48.2%) |
| Age, n (%) | |
| ≤ 65 years | 349 (52.7%) |
| > 65 years | 313 (47.3%) |
| Education, n (%) | |
| Primary school or less | 321 (48.5%) |
| Secondary school or higher | 341 (51.5%) |
| COEN, Mean (SD) | 3.54 (0.38) |
| Medication adherence, Mean (SD) | 1.82 (0.24) |
| T2 measures | |
| Depressive symptoms, Mean (SD) | 8.15 (1.49) |
| Self-efficacy, Mean (SD) | 0.30 (0.36) |
| Medication adherence, Mean (SD) | 1.84 (0.23) |
Abbreviation: COEN, community efficacy for non-communicable disease management.
Table 2.
Correlations Between Study Variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Sex | 1 | |||||||
| 2. Age | −0.04 | 1 | ||||||
| 3. Education | 0.19*** | −0.26*** | 1 | |||||
| 4. COEN (T1) | 0.08 | 0.05 | −0.02 | 1 | ||||
| 5. Depressive symptoms (T2) | 0.24*** | 0.05 | −0.13*** | −0.11** | 1 | |||
| 6. Self-efficacy (T2) | −0.02 | −0.04 | 0.08* | 0.19*** | −0.35*** | 1 | ||
| 7. Medication adherence (T1) | −0.11** | 0.05 | 0.02 | 0.05 | −0.05 | 0.07 | 1 | |
| 8. Medication adherence (T2) | −0.07 | 0.04 | −0.02 | 0.09* | −0.19*** | 0.12** | 0.28*** | 1 |
Notes: *p< 0.05, **p < 0.01, ***p< 0.001.
Abbreviations: SD, standard deviation; COEN, Community efficacy for non-communicable disease management; T1, Time 1; T2, Time 2.
The Relationship Between COEN, Self-Efficacy, Depressive Symptoms, and Medication Adherence
Table 3 shows the results of regression testing approach for mediation. The relationship between COEN and self-efficacy was significant (β = 0.19, p < 0.001). The relationship between self-efficacy and depressive symptoms was significant (β = −0.33, p < 0.001). The relationship between depressive symptoms and medication adherence was significant (β = −0.17, p = 0.002).
Table 3.
Estimated Standardized Coefficients Between COEN, Self-Efficacy, Depressive Symptoms, and Medication Adherence
| Variables | Self-Efficacy (T2) | Depressive Symptoms (T2) | Medication Adherence (T2) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| β (LLCI, ULCI) | t | p value | β (LLCI, ULCI) | t | p value | β (LLCI, ULCI) | t | p value | |
| COEN (T1) | 0.19 (0.11, 0.26) | 4.926 | <0.001 | −0.06 (−0.14, 0.01) | −1.772 | 0.102 | 0.06 (−0.01, 0.14) | 1.551 | 0.118 |
| Self-efficacy (T2) | −0.33 (−0.41, −0.26) | −9.256 | <0.001 | 0.04 (−0.04, 0.11) | 0.895 | 0.367 | |||
| Depressive symptoms (T2) | −0.17 (−0.27, −0.06) | −3.972 | 0.002 | ||||||
| Medication adherence (T1) | 0.27 (0.18, 0.35) | 6.892 | <0.001 | ||||||
| Sex | −0.02 (−0.09, 0.05) | −0.403 | 0.687 | 0.23 (0.16, 0.29) | 6.306 | <0.001 | −0.02 (−0.10, 0.06) | −0.592 | 0.553 |
| Age | −0.03 (−0.11, 0.04) | −0.715 | 0.475 | 0.04 (−0.03, 0.10) | 0.992 | 0.285 | 0.02 (−0.06, 0.09) | 0.414 | 0.668 |
| Education | 0.08 (0.01, 0.15) | 1.878 | 0.061 | −0.05 (−0.12, 0.01) | −1.259 | 0.169 | −0.06 (−0.14, 0.01) | −1.568 | 0.101 |
| R2 | 0.037 | 0.186 | 0.123 | ||||||
| F | 7.315*** | 30.020*** | 12.032*** | ||||||
Note: ***p<0.001.
Abbreviations: COEN, Community efficacy for non-communicable disease management; LLCI, lower limit confidence interval; ULCI, upper limit confidence interval; T1, Time 1; T2, Time 2.
Mediation Analysis
The coefficients of the six paths are shown in Table 4 and Figure 2. The model demonstrated adequate model–data fit: χ2/df = 1.33, CFI = 0.997, TLI = 0.973, RMSEA = 0.023, SRMR = 0.014. We found that COEN had a significant and positive total effect on medication adherence (β = 0.087, p < 0.05). COEN was not directly associated with medication adherence, as indicated by the non-significant direct effect (β= 0.061, p = 0.118, CI = [−0.013, 0.135]). The serial mediating effect of COEN and medication adherence through self-efficacy and depressive symptoms was significant (β = 0.009; 95% CI: 0.003–0.022).
Table 4.
Summary of Indirect Effects, Direct Effects, Total Effects, and 95% Confidence Intervals (CI)
| Effects | Sample | β | 95% CI | p value | |
|---|---|---|---|---|---|
| Indirect effects | |||||
| Total indirect effects | Total sample | 0.027 | 0.008 | 0.057 | 0.029 |
| Males | 0.023 | −0.020 | 0.081 | 0.395 | |
| Females | 0.027 | 0.008 | 0.061 | 0.036 | |
| COEN→SE→MA | Total sample | 0.007 | −0.007 | 0.022 | 0.379 |
| Males | −0.016 | −0.048 | 0.011 | 0.258 | |
| Females | 0.014 | 0.001 | 0.041 | 0.127 | |
| COEN→depressive symptoms→MA | Total sample | 0.011 | −0.001 | 0.030 | 0.143 |
| Males | 0.019 | −0.003 | 0.055 | 0.203 | |
| Females | 0.009 | −0.002 | 0.034 | 0.296 | |
| COEN→SE→depressive symptoms→MA | Total sample | 0.009 | 0.003 | 0.022 | 0.035 |
| Males | 0.020 | 0.005 | 0.051 | 0.066 | |
| Females | 0.004 | 0.000 | 0.017 | 0.247 | |
| Direct effects | |||||
| COEN→MA | Total sample | 0.061 | −0.013 | 0.135 | 0.118 |
| Males | 0.093 | −0.039 | 0.212 | 0.137 | |
| Females | 0.032 | −0.066 | 0.127 | 0.513 | |
| Total effects | |||||
| Direct + indirect effects | Total sample | 0.087 | 0.014 | 0.160 | 0.021 |
| Males | 0.116 | -0.012 | 0.221 | 0.052 | |
| Females | 0.060 | −0.033 | 0.154 | 0.229 | |
Abbreviations: β, standardized coefficient; COEN, community efficacy for non- communicable disease management; SE, self-efficacy; MA, medication adherence. Bold text implies significant effects.
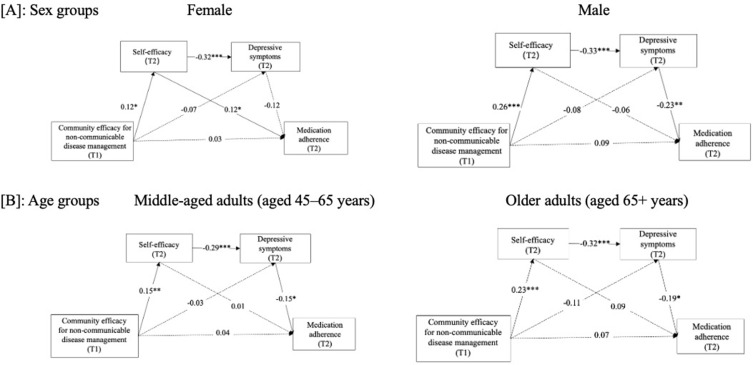
Model Invariance by Sex Group
Multi-group analyses were done to test if the path coefficients were significantly different by sex group. The fit indices for multi-group analysis were adequate (see Table 5, Model A). The results suggested that the unconstrained model was significantly different from the constrained model (ΔCFI = 0.024 > 0.01 and ΔRMSEA = 0.018 > 0.015).
Table 5.
Model Fit and Comparison for Measurement Invariance Across Sex and Age Groups
| Models | Model fit | Model Comparison | |||
|---|---|---|---|---|---|
| χ2 (df) | CFI | RMSEA | ΔCFI | ΔRMSEA | |
| Model A: multiple-group analysis across sex | |||||
| Model 1A | 4.675 (4) | 0.997 | 0.023 | 0.024 | 0.018 |
| Model 2A | 15.280 (10) | 0.973 | 0.041 | ||
| Model B: multiple-group analysis across age | |||||
| Model 1B | 3.319 (4) | 1.000 | 0.000 | 0.001 | 0.010 |
| Model 2B | 10.320 (10) | 0.999 | 0.010 | ||
Abbreviation: CFI, comparative fit index; RMSEA, root mean square error of approximation.
As shown in Figure 3 and Table 4, six paths were freely estimated (ie, not constrained by sex); only one of them was related to the hypothesized model (ie, COEN→SE→MA) in females, while only one of them was related to the hypothesized model (ie, COEN→SE→Depressive symptoms →MA) in males. When we examined these paths for females and males (see Table 6), COEN was positively related to the self-efficacy of males and females (β = 0.26, p < 0.001; β = 0.12, p < 0.05, respectively), and the Wald Chi-squared (χ2) test showed that these two paths had no significant difference (Wald χ2= 2.44, p = 0.12). Self-efficacy was negatively related to depressive symptoms among females and males (β = −0.32, p < 0.001; β =−0.33, p < 0.001, respectively), and the Wald χ2 test showed that these two paths had no significant difference (Wald χ2 = 0.64, p = 0.43). Moreover, a statistically significant association on the path from self-efficacy to medication adherence was only found for females (β = 0.12, p < 0.05). The Wald χ2 test showed that these two paths had a significant difference (Wald χ2 = 5.02, p < 0.05). A statistically significant association on the path from depressive symptoms to medication adherence only found for males (β = −0.23, p < 0.01). The Wald χ2 test showed that these two paths had a significant difference (Wald χ2 = 4.28, P < 0.05).
Figure 3.
Serial mediation diagram between community efficacy for NCD management, self-efficacy, depressive symptoms, and medication adherence by sex (A), female and male) groups and age (B), middle-aged adults and older adults) groups. Solid-lined curves represent statistical significance. T1 = Time 1; T2 = Time 2. *p < 0.05, **p < 0.01, ***p < 0.001.
Table 6.
Standardized Path Coefficients of Sex
| Paths | Male | Female | Wald χ2 | p value |
|---|---|---|---|---|
| COEN→self-efficacy | 0.26*** | 0.12* | 2.44 | 0.12 |
| COEN→depressive symptoms | −0.08 | −0.07 | 0.07 | 0.79 |
| COEN→medication adherence | 0.09 | 0.03 | 0.53 | 0.47 |
| Self-efficacy→depressive symptoms | −0.33*** | −0.32*** | 0.64 | 0.43 |
| Self-efficacy→medication adherence | 0.06 | 0.12* | 5.02 | < 0.05 |
| Depressive symptoms→medication adherence | −0.23** | −0.12 | 4.28 | < 0.05 |
Note: Bold type implies a regression path with significant sex differences. *p < 0.05, **p < 0.01, ***p < 0.001.
Abbreviation: COEN, community efficacy for non-communicable disease management.
Model Invariance by Age Group
We also explored whether the mediation model differed significantly for middle-aged and older adults. The fit indices for the multi-group analysis were adequate (see Table 5, Model B). As shown in Figure 3, six paths were freely estimated (ie, not constrained by age); only one of them was related to the hypothesized model (ie, COEN→SE→Depressive symptoms→MA) among middle-aged and older adults. The multi‐group analysis revealed that the middle-aged and older adults did not significantly differ in the model (ΔCFI = 0.001 < 0.01 and ΔRMSEA = 0.010 < 0.015), thus the model can be considered invariant by sex. Therefore, the Wald χ2 test was not used to examine whether the specific paths differed by age group.
Discussion
This study is the first longitudinal study focusing on self-efficacy, depressive symptoms, COEN, and medication adherence among middle-aged and older adults with type 2 diabetes and/or hypertension in China. Our findings support the sequential mediation of the relationship between COEN and medication adherence by self-efficacy and depressive symptoms. Moreover, the findings also showed a mediation effect from COEN to medication adherence through self-efficacy in females and a serial mediation effect from COEN to medication adherence in males. Importantly, the only relevant difference between sex was observed in the direct path from self-efficacy to medication adherence, which was statistically significant in females but not in males, while the direct path from depressive symptoms to medication adherence, which was statistically significant in males but not in females.
We found that self-efficacy and depressive symptoms have serial mediating effects on the relationship between COEN and medication adherence, and COEN is associated with medication adherence by increasing self-efficacy levels and decreasing depressive symptoms, thus supporting our hypothesis.43,44 However, this result is not entirely consistent with previous findings. For instance, Wen et al examined 238 elderly Chinese patients with coronary heart disease and found that social environment and self-efficacy mediated the relationship between depression and medication adherence.45 These inconsistencies could be explained by SCT, in which self-efficacy can impact human behavior both directly and indirectly via other mediating processes, including outcome expectations and social support.46 SCT also posits that self-efficacy and depressive symptoms are linked.22 It argues that depressive feelings might result from a low level of self-efficacy due to a discrepancy between expectations and perceived abilities.22 Although an earlier study indicated that self-efficacy could predict depressive symptoms, few studies have examined these two constructs together.23 As such, this integrated multiple mediation model provides us with a more comprehensive process accounting for how neighborhood characteristics are related to medication adherence in Chinese culture.
We found that self-efficacy partially mediated the relationship between COEN and medication adherence for females. The study further found a statistically significant association between self-efficacy and medication adherence among females. However, this association was not statistically significant among males. However, the findings of this study were not consistent with the results of the findings of Mahmoodi (2019) et al,47 who found that self-efficacy can predict medication adherence in both females and males. This may be attributable to the different cognitive, motivational, behavioral, and emotional pathways used by males and females regarding medication adherence.47 Specifically, females had a significantly greater belief in their ability to manage their NCDs, and they also reported a greater sense of connectedness and perceived more support when compared to males, which contributes to better medication adherence in females.
We also found that self-efficacy and depressive symptoms sequentially mediated the relationship between COEN and medication adherence for males. The study further found a statistically significant association between depressive symptoms and medication adherence in males, but not in females, which is consistent with previous research.48 Empirical studies in the domains of social support offer insight into sex differences in depression and medication adherence for chronic diseases.48,49 A previous study found that men are socialized to rely on others (eg, spouses) for help in managing their mental health, while women mostly relied on themselves to manage their mental health.49 This possibly explains why males were prone to experiencing depressive symptoms and having lower medication adherence. Another possibility is that men may perceive chronic diseases as more threatening, experience more depressive symptoms, and are less likely to adhere to medication.50
The current study found no age difference in the association between COEN and medication adherence. Our findings imply that, in the community context, these relationships among COEN, self-efficacy, depressive symptoms, and medication adherence are important for middle-aged and older patients with NCDs. Theories of life course, stress processes, and human behavior indicate that psychosocial factors (eg, self-efficacy) within neighborhood characteristics exert age-invariant effects. These effects persist irrespective of an individual’s life stage and subsequently influence psychosocial responses that further impact health behaviors.51 Empirical work has also suggested that there are no age differences in the effects of the neighborhood on health behaviors.52 Nevertheless, it is important to investigate the effects of neighborhood characteristics on health behaviors from a dynamic life-course perspective.
One of the strengths of this study is the use of the COEN scale, a validated and innovative scale based on community residents’ reports of neighborhood characteristics. The present study builds on previous research and complements the theoretical approach by using a multi-dimensional scale that quantifies COEN based on resident perceptions. Second, current study builds upon previous research by demonstrating the serial mediating role of self-efficacy and depressive symptoms in the relationship between COEN and medication adherence in Chinese type 2 diabetes and/or hypertension adults. Third, the present study uses multi-group analysis to test whether the proposed relationships are consistent with sex and age groups. Our study sheds light on the significance of sex in the context of NCD management.
Several limitations should be considered when interpreting the results of this study. First, the analyses were based on data collected through self-reporting. Due to a variety of reporting issues (eg, respondent biases and social desirability bias), self-report measures have been suggested to overestimate medication adherence, which may affect the results of this study.50,53 Electronic drug monitoring is a promising technology allowing patient adherence to be measured more accurately.54 It is often considered the “gold standard” for measuring adherence.55 Therefore, it is suggested that future investigations employ a combination of self-reported and objective methodologies (eg, electronic drug monitoring) to enhance the accuracy in determining the true status of medication adherence. Additionally, as we measured both depressive and self-efficacy at the same time, we were unable to rule out the possibility of a bidirectional relationship between these two variables. Hence, future research needs to use more rigorous longitudinal design and comprehensive analyses to better understand the direction of the associations documented in this study.
Conclusion
This study examined the relationships among COEN, self-efficacy, depressive symptoms, and medication adherence. Our findings indicate that self-efficacy and depressive symptoms sequentially mediate the relationship between COEN and medication adherence. Furthermore, we observed that self-efficacy was statistically associated with medication adherence only in females, while depressive symptoms were statistically associated with medication adherence only in males. The results regarding sex differences justify additional investigation and have the potential to provide sex-tailored strategies for NCD management.
Practice Implications
Our findings are important from a public health perspective because the results show that self-efficacy and depressive symptoms play a vital role in the relationship between COEN and medication adherence. Therefore, healthcare providers and educational programs should focus on helping NCD patients enhance their self-efficacy, reduce their depressive symptoms, and further improve their medication adherence. Moreover, self-efficacy was statistically associated with medication adherence in females but not in males, whereas depressive symptoms were statistically associated with medication adherence in males but not in females. The observed sex differences warrant further research and could potentially inform sex-specific strategies on NCD management. More specifically, for female patients, strategies that address depressive symptoms (eg, through patient-support groups and community care services), may more effectively enhance medication adherence. For male patients, on the other hand, approaches incorporating collaborative care, enhanced patient–physician interaction, and promoting community empowerment may enhance self-efficacy and thus improve medication adherence.
Acknowledgment
We are indebted to Amanda Li for assistance with methodology.
Funding Statement
This study was supported by the National Natural Science Foundation of China (Grant number: 71774075).
Data Sharing Statement
The deidentified data underlying this article will be shared upon written request to and approval by the corresponding author.
Ethics Approval and Informed Consent
All methods were carried out in accordance with relevant guidelines and regulations. This project was approved by the Ethics Committee of Duke Kunshan University (2019YANL013), and Fudan University approved the study. Patients were informed that they could refuse to participate, discontinue their participation at any point, and refuse to answer any questions. Each patient signed a consent form before enrolling in the study. The study complies with the Declaration of Helsinki.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Brawley LR, Culos-Reed SN. Studying adherence to therapeutic regimens: overview, theories, recommendations. Control Clin Trials. 2000;21(5 Suppl):S156–S163. doi: 10.1016/S0197-2456(00)00073-8 [DOI] [PubMed] [Google Scholar]
- 2.DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–209. doi: 10.1097/01.mlr.0000114908.90348.f9 [DOI] [PubMed] [Google Scholar]
- 3.Chew SM, Lee JH, Lim SF, Liew MJ, Xu Y, Towle RM. Prevalence and predictors of medication non-adherence among older community-dwelling people with chronic disease in Singapore. J Adv Nurs. 2021;77(10):4069–4080. doi: 10.1111/jan.14913 [DOI] [PubMed] [Google Scholar]
- 4.Aravindakshan R, Abraham SB, Aiyappan R. Medication adherence to oral hypoglycemic drugs among individuals with type 2 diabetes mellitus - a community study. Indian J Community Med. 2021;46(3):503–507. doi: 10.4103/ijcm.IJCM_985_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bayly JE, Panigrahi A, Rodriquez EJ, et al. Perceived neighborhood factors, health behaviors, and related outcomes in the Hispanic community health study/study of latinos. Prev Med. 2022;164:107267. doi: 10.1016/j.ypmed.2022.107267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlson JA, Sallis JF, Jankowska MM, et al. Neighborhood built environments and Hispanic/Latino adults’ physical activity in the U.S.: the Hispanic community health study/study of Latinos community and surrounding areas study. Prev Med. 2022;160:107073. doi: 10.1016/j.ypmed.2022.107073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vallarta-Robledo JR, Marques-Vidal P, Sandoval JL, et al. The neighborhood environment and its association with the spatio-temporal footprint of tobacco consumption and changes in smoking-related behaviors in a Swiss urban area. Health Place. 2022;76:102845. doi: 10.1016/j.healthplace.2022.102845 [DOI] [PubMed] [Google Scholar]
- 8.Karriker-Jaffe KJ, Li L, Cherpitel CJ, Bensley KMK, Zemore SE. Neighborhood contexts and alcohol use disorder among Mexican Americans living in the US-Mexico border region. Alcohol Alcohol. 2022;57(6):678–686. doi: 10.1093/alcalc/agac020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Brien DT, Farrell C, Welsh BC. Broken (windows) theory: a meta-analysis of the evidence for the pathways from neighborhood disorder to resident health outcomes and behaviors. Soc Sci Med. 2019;228:272–292. doi: 10.1016/j.socscimed.2018.11.015 [DOI] [PubMed] [Google Scholar]
- 10.Jiang Y, Li X, Cho H, Brown MJ, Qiao S, Haider MR. Effects of individual and neighborhood socioeconomic status on antiretroviral therapy adherence: the role of adherence self-efficacy. J Health Psychol. 2021;26(8):1143–1153. doi: 10.1177/1359105319869809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pichardo MS, Pichardo CM, Talavera GA, et al. Change in neighborhood socioeconomic status and adherence to the cancer prevention lifestyle guidelines in Hispanic/Latino adults: results from the HCHS/SOL study. Cancer Res Commun. 2023;3(10):1981–1991. doi: 10.1158/2767-9764.CRC-23-0187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13(4):623–649. doi: 10.1080/08870449808407422 [DOI] [Google Scholar]
- 13.Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Ann Behav Med. 2007;34(3):304–312. doi: 10.1007/BF02874555 [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 1999;2(1):21–41. [DOI] [PubMed] [Google Scholar]
- 15.Gearhart MC. Mutual efficacy, self-efficacy, and collective efficacy theory: an examination of empowerment and activism. Soc Work. 2023;68(3):192–200. doi: 10.1093/sw/swad018 [DOI] [PubMed] [Google Scholar]
- 16.Soller B, Jackson AL. Girls’ self-efficacy in the context of neighborhood gender stratification. Soc Sci Res. 2018;72:100–114. doi: 10.1016/j.ssresearch.2018.01.005 [DOI] [PubMed] [Google Scholar]
- 17.Boardman JD, Robert SA. Neighborhood socioeconomic status and perceptions of self-efficacy. Sociol Perspect. 2000;43(1):117–136. doi: 10.2307/1389785 [DOI] [Google Scholar]
- 18.Anderson JR, Novak JR, Johnson MD, et al. A dyadic multiple mediation model of patient and spouse stressors predicting patient dietary and exercise adherence via depression symptoms and diabetes self-efficacy. J Behav Med. 2016;39(6):1020–1032. doi: 10.1007/s10865-016-9796-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med. 2015;32(6):725–737. doi: 10.1111/dme.12651 [DOI] [PubMed] [Google Scholar]
- 20.Kim ES, Chen Y, Kawachi I, VanderWeele TJ. Perceived neighborhood social cohesion and subsequent health and well-being in older adults: an outcome-wide longitudinal approach. Health Place. 2020;66:102420. doi: 10.1016/j.healthplace.2020.102420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Villalonga-Olives E, Kawachi I. The dark side of social capital: a systematic review of the negative health effects of social capital. Soc Sci Med. 2017;194:105–127. doi: 10.1016/j.socscimed.2017.10.020 [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. On the functional properties of perceived self-efficacy revisited. J Manag. 2012;38(1):9–44. [Google Scholar]
- 23.Scott WD, Dearing E. A longitudinal study of self-efficacy and depressive symptoms in youth of a North American Plains tribe. Dev Psychopathol. 2012;24(2):607–622. doi: 10.1017/S0954579412000193 [DOI] [PubMed] [Google Scholar]
- 24.Bandura A, Caprara GV, Barbaranelli C, Gerbino M, Pastorelli C. Role of affective self-regulatory efficacy in diverse spheres of psychosocial functioning. Child Dev. 2003;74(3):769–782. doi: 10.1111/1467-8624.00567 [DOI] [PubMed] [Google Scholar]
- 25.Burkhart PV, Sabaté E. Adherence to long-term therapies: evidence for action. J Nurs Scholarsh. 2003;35(3):207. doi: 10.1111/j.1547-5069.2003.tb00001.x [DOI] [PubMed] [Google Scholar]
- 26.Gast A, Mathes T. Medication adherence influencing factors-an (updated) overview of systematic reviews. Syst Rev. 2019;8(1):112. doi: 10.1186/s13643-019-1014-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stafford M, Cummins S, Macintyre S, Ellaway A, Marmot M. Gender differences in the associations between health and neighbourhood environment. Soc Sci Med. 2005;60(8):1681–1692. doi: 10.1016/j.socscimed.2004.08.028 [DOI] [PubMed] [Google Scholar]
- 28.Yang ZY, Wang YT, Xia L, Zheng YC, Feng ZZ. The relationships between prospection, self-efficacy, and depression in college students with cross-lagged analysis. Int J Environ Res Public Health. 2022;19(22). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tan JP, Cheng KKF, Siah RC. A systematic review and meta-analysis on the effectiveness of education on medication adherence for patients with hypertension, hyperlipidaemia and diabetes. J Adv Nurs. 2019;75(11):2478–2494. doi: 10.1111/jan.14025 [DOI] [PubMed] [Google Scholar]
- 30.Bowling A, Barber J, Morris R, Ebrahim S. Do perceptions of neighbourhood environment influence health? Baseline findings from a British survey of aging. J Epidemiol Community Health. 2006;60(6):476–483. doi: 10.1136/jech.2005.039032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Z, Gong EY, Peng WX, et al. Community empowerment for the prevention and control of non-communicable diseases. Chin General Pract. 2019;22(10):1153–1160. [Google Scholar]
- 32.Xiong SZ, Zhang SJ, Gong EY, et al. Establishing the evaluation system of community efficacy for non-communicable diseases in Chinese urban area by Delphi method. Chin J Prev Cont Chronic Dis. 2021;29(9):674–678. [Google Scholar]
- 33.Xiong S, Zhu G, Malhotra R. Community efficacy for non-communicable disease management in China: conceptualization, measurement and Validation; 2023. [DOI] [PMC free article] [PubMed]
- 34.Zhu G, Xiong S, Malhotra R. Individual perceptions of community efficacy for non-communicable disease management in twelve communities in china: cross-sectional and longitudinal analyses. Public Health. 2024;226:207–214 doi: 10.1016/j.puhe.2023.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Ritter PL, Lorig K. The English and Spanish self-efficacy to manage chronic disease scale measures were validated using multiple studies. J Clin Epidemiol. 2014;67(11):1265–1273. doi: 10.1016/j.jclinepi.2014.06.009 [DOI] [PubMed] [Google Scholar]
- 36.Na PJ, Yaramala SR, Kim JA, et al. The PHQ-9 Item 9 based screening for suicide risk: a validation study of the patient health questionnaire (PHQ)-9 item 9 with the Columbia suicide severity rating scale (C-SSRS). J Affect Disord. 2018;232:34–40. doi: 10.1016/j.jad.2018.02.045 [DOI] [PubMed] [Google Scholar]
- 37.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007 [DOI] [PubMed] [Google Scholar]
- 38.Stafford MAI, McMunn A, De Vogli R. Neighbourhood social environment and depressive symptoms in mid-life and beyond. Ageing Soc. 2011;31(6):893–910. doi: 10.1017/S0144686X10001236 [DOI] [Google Scholar]
- 39.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. doi: 10.1037/0033-2909.88.3.588 [DOI] [Google Scholar]
- 40.Kline RB. Convergence of structural equation modeling and multilevel modeling. In: Handbook of Methodological Innovation. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- 41.Liao B, EWvdB P, van Wesemael PJV, A Arentze T. How does walkability change behavior? A comparison between different age groups in the Netherlands. Int J Environ Res Public Health. 2020;17(2):540. doi: 10.3390/ijerph17020540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peng PS, Kao TW, Chang PK, Chen WL, Peng PJ, Wu LW. Association between HOMA-IR and Frailty among U.S. Middle-aged and Elderly Population. Sci Rep. 2019;9(1):4238. doi: 10.1038/s41598-019-40902-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Son Y-J, Won MH. Depression and medication adherence among older Korean patients with hypertension: mediating role of self-efficacy. Int J Nurs Pract. 2017;23(3):e12525. doi: 10.1111/ijn.12525 [DOI] [PubMed] [Google Scholar]
- 44.Schoenthaler A, Ogedegbe G, Allegrante JP. Self-efficacy mediates the relationship between depressive symptoms and medication adherence among hypertensive African Americans. Health Educ Behav. 2006;36(1):127–137. doi: 10.1177/1090198107309459 [DOI] [PubMed] [Google Scholar]
- 45.Wen J, Yeh TP, Xie H, Yu X, Tang J, Chen Y. Resilience, self-esteem, self-efficacy, social support, depression and ART adherence among people living with HIV in Sichuan, China. AIDS Care. 2021;33(11):1414–1421. doi: 10.1080/09540121.2020.1828800 [DOI] [PubMed] [Google Scholar]
- 46.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 47.Mahmoodi H, Jalalizad Nahand F, Shaghaghi A, Shooshtari S, Jafarabadi MA, Allahverdipour H. Gender based cognitive determinants of medication adherence in older adults with chronic conditions. Patient Prefer Adherence. 2019;13:1733–1744. doi: 10.2147/PPA.S219193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gentil L, Vasiliadis HM, Préville M, Bossé C, Berbiche D. Association between depressive and anxiety disorders and adherence to antihypertensive medication in community-living elderly adults. J Am Geriatr Soc. 2012;60(12):2297–2301. doi: 10.1111/j.1532-5415.2012.04239.x [DOI] [PubMed] [Google Scholar]
- 49.Nau DP, Aikens JE, Pacholski AM. Effects of gender and depression on oral medication adherence in persons with type 2 diabetes mellitus. Gend Med. 2007;4(3):205–213. doi: 10.1016/S1550-8579(07)80041-6 [DOI] [PubMed] [Google Scholar]
- 50.Callaghan D. Healthy behaviors, self-efficacy, self-care, and basic conditioning factors in older adults. J Community Health Nurs. 2005;22(3):169–178. doi: 10.1207/s15327655jchn2203_4 [DOI] [PubMed] [Google Scholar]
- 51.Lei MK, Berg MT, Simons RL, Beach SRH. Neighborhood structural disadvantage and biological aging in a sample of Black middle age and young adults. Soc Sci Med. 2022;293:114654. doi: 10.1016/j.socscimed.2021.114654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang TC, South SJ. Neighborhood poverty and physical health at midlife: the role of life-course exposure. J Urban Health. 2020;97(4):486–501. doi: 10.1007/s11524-020-00444-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pearson CR, Simoni JM, Hoff P, Kurth AE, Martin DP. Assessing antiretroviral adherence via electronic drug monitoring and self-report: an examination of key methodological issues. AIDS Behav. 2007;11(2):161–173. doi: 10.1007/s10461-006-9133-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kheir N, Greer W, Yousif A, et al. The utility of an electronic adherence assessment device in type 2 diabetes mellitus: a pilot study of single medication. Patient Prefer Adherence. 2010;4:247–254. doi: 10.2147/PPA.S10347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Al-Hassany L, Kloosterboer SM, Dierckx B, Koch BC. Assessing methods of measuring medication adherence in chronically ill children-a narrative review. Patient Prefer Adherence. 2019;13:1175–1189. doi: 10.2147/PPA.S200058 [DOI] [PMC free article] [PubMed] [Google Scholar]