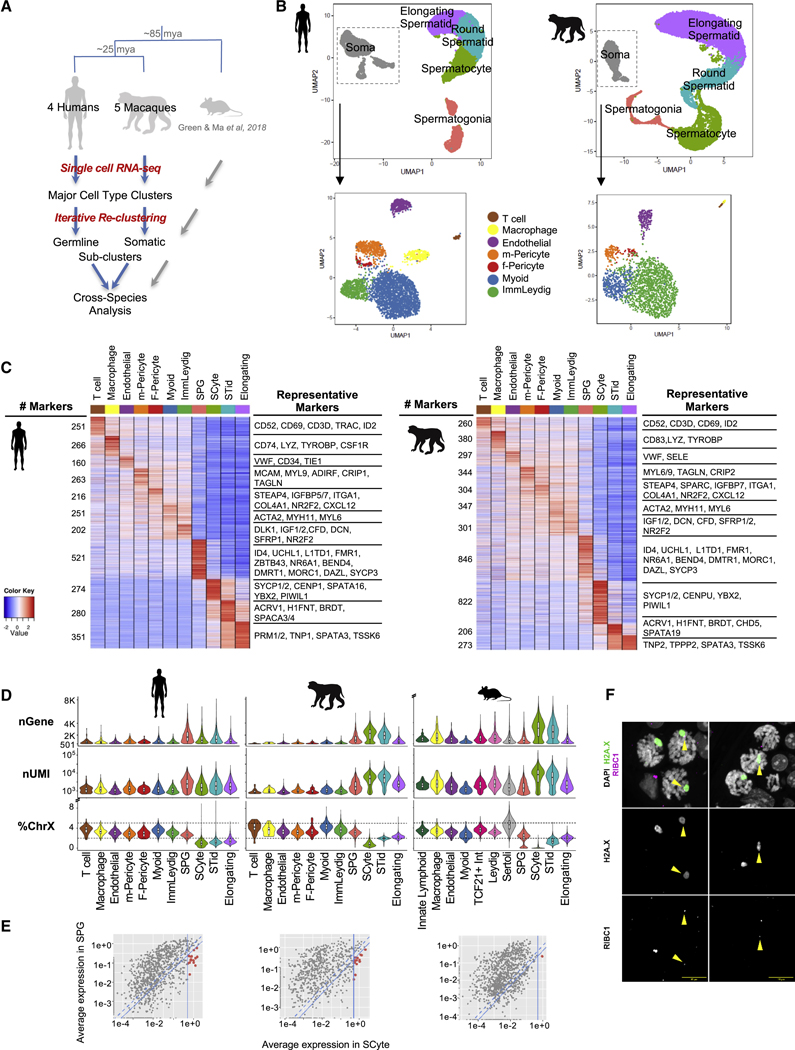
Introduction
A stay in an intensive care unit (ICU) can be a highly stressful life event for both patients and their family caregivers. Family caregivers of ICU patients are at high risk of developing adverse psychological outcomes such as anxiety, depression, and post-traumatic stress disorder (PTSD).1 Post-intensive care syndrome-family (PICS-F) refers to the development of a cluster of common symptoms among family caregivers of ICU patients.2 Family caregivers may experience psychological symptoms during ICU care and/or following the ICU admission, and those symptoms can last for months to years after the ICU discharge.2
Approximately 40% of ICU patients in the United States need mechanical ventilation (MV) to assist or replace spontaneous breathing3 rendering the patient unable to produce vocal speech. Patient communication is further limited by physical weakness and fluctuations in cognition. Communication difficulty is one of the most common burdens reported by mechanically ventilated patients in ICU.4,5 While communication difficulty during MV treatment is associated with negative feelings such as frustration, fear, anxiety, and anger for patients,4,6–9 family caregivers report emotional distress, feelings of loss, and frustration.10–13 These negative feelings may induce or worsen adverse psychological outcomes such as anxiety, depression, and PTSD, yet little is known about the impact of patient-family communication on psychological symptoms in ICU family caregivers.
Augmentative and alternative communication (AAC) methods, such as writing tools, communication boards, or electronic communication devices, may relieve or reduce communication challenges.13 Despite a lack of evidence or support, clinicians report relying on family caregivers to provide interpretation of nonvocal communication when ICU patients are unable to speak.10,14,15 Therefore, there is a need for effective strategies to facilitate communication between nonvocal ICU patients and family caregivers.
The Facilitated Sensemaking Model (FSM), is a middle range theory, providing a basis for how to care for family caregivers of ICU patients.16 The FSM guides nursing interventions to prevent and/or reduce adverse psychological outcomes in family caregivers in the ICUs.16 The purpose of this paper is to extend the FSM to promote an electronic intervention to aid patient-family communication in the ICU. In this paper, we present the scientific evidence and theoretical background for adding interventions to facilitate patient-family communication to prevent and/or alleviate adverse psychological outcomes in family caregivers of nonvocal ICU patients. An electronic tablet communication application is one example of an intervention to facilitate patient-family communication in the ICU.
Literature Review
Post-Intensive Care Syndrome-Family (PICS-F)
Since investigators first recognized that family caregivers of ICU patients could have clinically diagnosable psychological problems in the early 1990s,17 there has been growing interest in the impact of critical illness on family caregivers. There is wide variation in reported prevalence of depression, anxiety, and PTSD-related symptoms among ICU family caregivers, which may be related to differences in study settings, time frames for symptom assessment, sample and measurement tools.18,19 For example, the reported short- and longer-term prevalence of post-ICU depressive symptoms in ICU family caregivers ranged from 12 to 26% at three months and 23–44% at one year.19 The prevalence of anxiety symptoms ranged between 24 – 63% at three months and the prevalence of PTSD-related symptoms was estimated between 32–80% at one year post-ICU.18 Despite the wide variation of estimated prevalence, the findings still indicate that ICU family caregivers experience high levels of psychological symptoms considering that reported lifetime prevalence of depression in the general population ranged between 8–15%20 and lifetime prevalence of PTSD among adult Americans is 6.8%.21
Clinical practice guidelines for support of family-centered care in the ICU22,23 address the need for more structured family support interventions to reduce anxiety, depression, and post-traumatic stress in ICU family caregivers. However, few interventions have been developed and tested to improve adverse psychological outcomes in ICU family caregivers. An ICU diary is one strategy developed and implemented to reduce the psychological distress in ICU survivors and caregivers. ICU diaries are designed to provide a story of the patient’s ICU stay,24,25 and diaries are generally written by nurses, other hospital staff, or family caregivers during the ICU care. As a focus for family empowerment and family-centered care in the ICUs, several studies involving ICU diaries encouraged the participation of the family caregivers, yet the impact of diaries on family caregivers’ adverse psychological outcomes is inconclusive.26–28
The results on adverse psychological outcomes in ICU families were also mixed in other studies of information-related interventions such as educational programs designed to inform family caregivers about care, diagnosis, or prognosis of the patient. Those programs can be delivered during the ICU admission29–31 or after discharge as part of a post-ICU rehabilitation program.32
Communication Difficulty in MV Patients and Family Caregivers
Communication between ICU patients and family caregivers is seriously impaired during treatment with MV due to multiple factors, most prominently, the placement of an oral endotracheal or tracheostomy tube which prevents voice production and impedes communication with vocal speech.33 Communication is essential to understand patients’ needs and detect patients’ symptoms, which may help improve the quality of care and safety. MV patients generally use natural communication methods such as gestures, head nods, mouthing words, and writing with paper and pen to communicate with nurses.34 However, those natural methods are time-consuming and can be unreliable.
Communication impairment due to MV during ICU stay may add psychological distress which can cause a new onset of psychological problems or worsen existing symptoms. A cross-sectional study conducted by Khalaila et al.6 examined the correlation between communication characteristics and psycho-emotional distress in ICU patients. The study demonstrated a strong association between higher psychological distress and negative feelings, such as fear and anger, with perceived communication difficulty and indicated that perceived communication difficulty was the strongest predictor of psychological distress.6 The results suggest possible associations between perceived communication difficulty and psychological symptoms in ICU family caregivers and support that providing effective communication strategies may help family caregivers, alleviate their psychological symptoms.
Augmentative and alternative communication (AAC) refers to all forms of communication used to supplement or replace oral speech including all ways to express messages such as facial expressions or gestures, body language, and aided low- and high- tech tools for those with speech or language impairment.35 Alternative communication methods developed and tested to improve communication for MV patients in the ICUs include low-tech tools such as communication boards and speaking valves for patients with tracheostomy and high-tech tools such as computerized communication tools. Table 1 summarizes several low- and high-tech communication tools available and tested for nonvocal patients in the ICUs.36
Table 1.
Summary of low- and high-tech communication tools for nonvocal patients
| Features | |
|---|---|
| Low-tech Tools | |
| Communication Boards | • Usually consist of an arrangement of the alphabet, words/phrases, icons, or pictures. • Icons and pictures represent common messages in which patients can easily point with fingers |
| Tracheostomy Speaking Valves | • Can be placed in the tracheostomy tube to allow phonation. • Facilitate verbal communication for tracheostomized patients. |
| High-tech Tools | |
| Speech Generating Devices (SGDs) | • Electronic AAC devices that produce pre-recorded voice messages or computer-generated voice when touching specific locations on the device screen or keyboard. • SGDs can be simple such as recorder devices or specialized computer systems. |
| Communication Computer Applications (apps) | • Communication apps may or may not speech-generating. • Several software apps for tablet computers or smartphones are commercially available. • Contain messages/icons like communication boards. • Most apps provide keyboard feature which allows the user to create novel messages |
| Eye Tracking Devices (ETDs) | • Can be used for paralyzed patients or others with restricted use of upper extremities. • Integrate the data by detecting eye-movement and position to create a gaze point for selections on a computer screen. • Allow patients to use their eyes to operate a speech-generating device using eye-gaze control technology. |
Although there is a growing recognition that effective communication is essential to improve the quality of healthcare and multiple AAC tools are available for nonvocal patients in hospital settings, patient-family communication has received little to no attention in critical care research. The involvement of family caregivers in assisted communication strategies with nonvocal ICU patients and the use of AAC tools in patient-family communication in the ICU has not been systematically investigated. The role of family involvement in communication remains unknown. When evaluated through qualitative research family caregivers expressed emotional distress, feelings of loss, and frustration with dysfunctional communication during MV treatment.10–13,37 Families want to help patients and to protect their feelings by calming and encouraging them,38,39 but they often do not know how to accomplish this. In previous research, patients described that a specific family member with exceptional ability to communicate took the time to understand their current condition, helped the patient to communicate, and made sure care providers understood the patient.14,15 Family caregivers often served the role as interpreters for the nonvocal patients and nurses tended to rely on their interpretation to communicate with the patients.10,14,15
A retrospective descriptive study to identify communication methods and the content of communication with non-surviving MV patients in the ICU showed that communication between patients and family caregivers often took the form of emotional expressions.40 In a feasibility study of electronic speech generating devices for MV patients, the primary content of speech generating devices-constructed messages was “I love you” and questions about home/family.41 These findings suggest that communication between family caregivers and patients may be more complex and stressful than simple, standard yes or no questions. Broyles and colleagues13 conducted a qualitative analysis of enrollment notes, intervention logs, and observation records from the Study of Patient-nurse Effectiveness with Assisted Communication Strategies (SPEACS) study42 to identify which AAC tools families used and to describe family caregivers’ and nurses’ perceptions of communication between family caregivers and MV patients. Family caregivers in this study were generally unprepared for the MV patient’s inability to communicate. Family caregivers experienced negative feelings, such as frustration, with unsuccessful communication. Although family caregivers were not familiar with AAC tools and strategies, they expressed interest in learning about AAC strategies and desired the highest level of communication with their critically ill patients.13
Despite evidence of the communication difficulties expressed by family caregivers and their desire to improve communication, to date, families of MV patients typically have only simple and low-tech tools to overcome communication difficulties and these are not consistently available at the ICU bedside.13 Information on the communication challenges between ICU patients and family caregivers is sparse and its impact on psychological outcomes family caregivers has not been addressed in previous studies.
The Facilitated Sensemaking Model
The Facilitated Sensemaking Model (FSM) was developed by Davidson16 to provide a basis for family-centered care in the ICU and guide interventions to prevent adverse psychological outcomes in ICU family caregivers. Table 2 describes the theoretical underpinnings of the FSM. The FSM was also developed inductively through literature review, consultation with content experts and family members during the development of the intervention set, and input from doctoral students, professors, and clinical nurse specialists during the validating process.16 The FSM has been tested for feasibility in the ICU setting.43 A family engagement intervention based on the FSM was associated with decreased levels of anxiety in family caregivers of cardiac surgery patients.44
Table 2.
Theoretical Underpinnings of the FSM
| Central Propositions | Adaptation to the FSM | ||
|---|---|---|---|
| Combination of RAM and WOST by Davidson while developing the FSM | Roy’s Adaptation Model (RAM) | • The goal of nursing is to promote a person’s adaptation whose life is disrupted such as illness. • Illness can cause a disruption in life, and adaptation occurs when people respond to the new environment in a positive way. |
• The FSM follows the adaptation theory premise that family caregivers experience a life disruption which requires a compensatory process to adjust to the disruption and adapt to the new circumstances of a family member’s critical illness and their role as ICU family caregivers. |
| Weick’s Organizational Sensemaking Theory (WOST) | • Leaders help others form a perception of a crisis event and make sense out of the situation. • Leaders can help others in the workplace with cue sorting to shape a positive impression of the situation. |
• Nurses proactively take cues from the environment and help the family caregivers sort those cues appropriately to make sense of what is going on. | |
| Sensemaking in psychology social and cognitive | Self-regulation Theory | • Concrete, clear objective information facilitates coping by affecting the person’s schema formation about stressful events such as illness. • A schema based on concrete objective information can focus a person’s attention away from the emotional dimensions of an impending experience leading to reduced emotional distress during the stressful experience. |
• The FSM follows the self-regulation theory premise that facilitated sensemaking help family caregivers reduce psychological symptoms by making sense out of what happened and their new roles as caregivers in the ICU environment. |
The primary goal of the FSM is to guide nursing interventions to prevent adverse psychological outcomes in family caregivers of ICU patients. The FSM assumes that exposure to critical illness can be a life crisis for family members of critically ill patients. The FSM proposes that nurses can provide a series of interventions to facilitate the sensemaking process with family caregivers. According to the model, family caregivers of an ICU patient experience life disruptions during the critical illness which may challenge their coping. In response to the disruption, family caregivers need a compensation period to overcome the challenges and adapt to the new situation. They need to make sense out of what has happened in the new situation and their new roles as ICU caregivers.16,43 During this compensation period, the nurse can engage in and facilitate the sense-making process with family caregivers through directed interventions.16,44
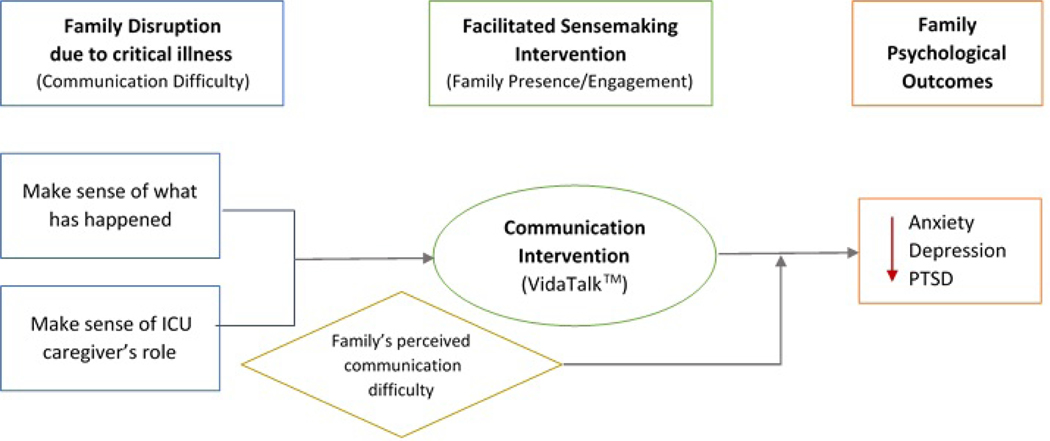
A facilitated sensemaking intervention has two main goals: 1) to help the family understand what is happening in the new situation, and 2) to coach what the family should do as a family caregiver of an ICU patient (Figure 1). Sensemaking interventions include identifying the family caregivers’ needs, providing information about the prognosis or care plan, providing family support, coaching the family on how to meet their own needs, and guiding bedside activities that they can perform while they visit their loved one in the ICUs.44 As a result of nursing interventions, family caregivers may be able to adapt to the new situation in a more positive way through improved coping. The FSM provides suggestions on specific bedside activities in two categories: 1) personal care/healing, and 2) bringing normalcy into the room. Personal care activities may include applying lip balm, giving a massage, assisting in passive range-of-motion exercises, praying, and engaging in cognitive exercises. The other group of activities includes reading aloud, talking about daily events, bringing in cards/pictures from home to bring normalcy into the room which may help the patient feel relieved.16 The sensemaking process will finally lead to adaptation which is described as lower adverse psychological outcomes such as anxiety, depression, and PTSD.
Figure 1.
The Facilitated Sensemaking Model.
From Davidson JE, McDuffie M, Kay M. Family-centered care. In: Goldsworthy S, Kleinpell R, Williams G, editors. International best practices in critical care nursing. 2nd edition. Dayboro, Australia: World Federation of Critical Care Nurses; 2018; with permission.
Application of the Facilitated Sensemaking Model to a Communication Intervention
The communication column in the FSM model (Figure 1) is intended to focus on and guide communication between the clinicians and the family (Davidson, personal communication). The presence column refers to family bedside presence activities. We have, therefore, added patient-family communication interventions to that area of the model (Figure 1). Our application of the FSM to the problem of communication difficulty and impairment is depicted in a research model (see Figure 2).
Figure 2.
Application of the FSM
The original FSM included low-tech communication tools such as paper pad, pencil, and foam grip as one of the components in the family visiting kit to enhance patient-family communication.43 This application of the FSM incorporates advances in technology not available at the time the model was originally constructed. We add an explicit assumption to the theory: Communication difficulty due to MV treatment is an unplanned and sudden event that seriously disrupts patient-family interactions and may cause or amplify psychological distress in family caregivers of nonvocal patients. Family-patient communication is an essential interaction for the family caregivers to interpret the experience of critical illness and understand the emotional reactions and thoughts of the patient. A communication intervention developed to improve communication between nonvocal patients and family caregivers may facilitate the family caregiver’s sensemaking process to compensate for the disruption and adapt to the new situation. An electronic communication intervention in addition to traditional pen and paper techniques may help family caregivers meet their own needs for effective communication with the patient to understand the patient’s situation, feelings/thoughts, and what they are experiencing. This will help family caregivers meet the first sensemaking goal: to make sense of what has happened in the ICU. More effective communication may also facilitate the family caregiver’s bedside activities as they better understand the patient’s expressed needs and allow the family caregivers to bring normalcy into the room by talking about daily events with more effective communication. Through these mechanisms, family caregivers would feel engaged and involved in the patient’s care, instead of remaining as visitors and meet the second sensemaking goal.
The results of previous studies exploring the communication experience between MV patients and their family caregivers support the need for a communication intervention to reduce family caregivers’ psychological distress.14,15 Although family members are usually familiar conversation partners, interpreting what the nonvocal MV patient is trying to say is typically a new role for a family caregiver, particularly in the context of serious and sudden illness or injuries and the ICU environment. The family caregiver needs to figure out how best to communicate with the nonvocal patient in a different way. We posit that more effective communication will help the family caregiver reduce the uncertainty, therefore, alleviate their adverse psychological outcomes and may also decrease frustration and agitation in patients. The FSM has not been tested for the impact of patient-family caregiver communication on psychological outcomes in family caregivers. Communication distress is expected to be relieved in nonvocal ICU patients and family caregivers by providing strategies to allow the patients and their families to communicate with each other.
Clinically applicable Communication Strategy
To illustrate how the FSM can guide practice regarding patient-family communication in the ICU, we provide an example of a newly developed electronic patient communication application (app) as a potential intervention to facilitate making sense of the experience and performing in the role as ICU family caregiver. Newer technology-based communication tools such as communication applications (apps) may be beneficial because apps are easy to use and less expensive than other communication devices such as specialized computer systems. Considering that approximately 50% of U.S. adults possess tablet computers and 80% own smartphones45 and the apps can be easily downloaded, using an electronic communication aid with nonvocal MV patients appears feasible. VidaTalk™ (Vidatak, LLC), an electronic patient communication board, is a tablet app designed to help patients who are unable to speak to communicate their needs to care providers and family caregivers. The communication app contains picture icons with words/phrases pertaining to needs and well-being, emotions, pain scales, pictures of the body to indicate needs in a certain area. Type and finger-drawing features allow the patient to generate novel messages. When a patient touches one of the icons, the message is produced audibly via digital speech and the text of the message is displayed on the screen, which enables two-way communication between the patient and others.
As mentioned previously, there are two sensemaking goals to help family caregivers reduce their psychological symptoms in our theoretical framework (Figure 2): 1) make sense of what is happening in the new situation, and 2) make sense of their new role as a caregiver of ICU patient. Various preset messages that are commonly used by ICU patients and novel messages created by the patient using writing or typing within the VidaTalk™ app will facilitate more complex conversations between MV patient and family caregivers. Therefore, use of a communication app may help family caregivers to meet the first goal by assisting with understanding the patient’s experience in the ICU and improving expressions of feelings/thoughts. The second sensemaking goal incorporates the family’s role as ICU caregiver serving the bedside activities and bringing normalcy into the room.16 More effective communication will help families understand the patient’s expressed needs/requests, as well as the patients, express their wishes clearly.
VidaTalk™ may help family caregivers to have clearer communication with the patient which may promote family caregivers’ bedside activities. For example, a family member may know, through the use of VidaTalk™, that the patient needs repositioning or pain medication, and would be able to provide or facilitate that bedside care assistance. This may further enhance the family caregiver’s role as advocate for the patient in the ICU. Also, the ability to communicate a variety of messages including conversations about everyday events outside of the hospital such as home/family and patient’s feelings/emotions may help families to bring normalcy into the room.
Happ et al. (2007) described communication processes between patients and families that emphasized the importance of normalizing talk to distract patients during weaning from MV and included talking about everyday, non-illness-related events.46 Consistent with these findings, the FSM also suggests normalizing the ICU environment as an important component of the sensemaking process in family caregivers.16 VidaTalk™ may help the families serve in the caregiver role by distracting patients from the stressful ICU environment with normalizing talk.
The keys to family-centered care are a beneficial relationship between family caregivers, patients, and care providers; and family presence, and family involvement in decision making and patient care.47 Communication strategies to enhance patient-family communication in the ICU may increase family involvement and allow families serve more active roles as ICU caregivers, which may help them reduce psychological distress through sensemaking process. We present a clinical case exemplar of family caregiver’s use of VidaTalk™ with the ICU patient to illustrate a family’s communication experience with nonvocal patient, how a communication tool enables patient-family communication, and how families emotionally react to communication with their loved one in the ICU (Box 1).
Box 1. Clinical Case Exemplar of a Communication Intervention in the FSM.
| Family Disruption Due to Critical Illness. | Mr. Stone (pseudonym), a 65-year-old, ICU patient was orally intubated, receiving mechanical ventilation, alert and cognitively intact. His wife, a 62-year-old woman, stayed at the bedside in the ICU room for most of the day. They initially communicated with each other using hand gestures or writing with paper and pen. Due to developing hand and arm weaknesses from the illness and extended hospitalization, hand writing on a paper became difficult for Mr. Stone and his written messages became nearly uninterpretable to his wife. After tracheostomy placement, Mr. Stone was able to mouth words with his lips, however, lip reading was not always clear or successful. Family members, visitors, and staff often failed to understand his wishes or requests leaving them feeling frustrated and disappointed with these communication challenges. When Mr. Stone’s wishes were not understood, he waved off any additional attempts to communicate. |
| Patient-Family Communication Intervention. | We introduced the VidaTalk™ communication app to Mr. and Ms. Stone on a hospital-issued android tablet. We provided a brief, 5-minute demonstration of the communication app including patient return demonstration, instruction on how to operate the tablet and an instruction sheet. The couple started using the app almost immediately. They used the app daily to communicate with each other during the rest of the hospitalization. Using the VidaTalk™ tablet app, Mr. Stone began asking a lot of questions including questions about home or his children (bringing normalcy to the situation). He asked his wife about the treatment plan and insurance (making sense of what is happening) as well as about daily events outside of the hospital (bringing normalcy). Mr. Stone also said ‘I love you’ to his wife almost every day, a normal, profound and meaningful expression between husband and wife. They continued to use hand gestures or mouthing words for simple messages, but used the VidaTalk™ app for conversations more complex than a simple request or when natural communication methods such as gestures or lip reading did not work well. |
| Outcomes. | With the communication app, Ms. Stone was able to clearly understand her husband’s needs, thoughts and feelings (making sense of the patient’s experience). Clear communication with the app reduced the family’s frustration and stress with inability to communicate and Ms. Stone described feeling “relieved” and “appreciated” (psychoemotional outcomes) as a result of communication with the app. |
Clinical Implications
The ICU environment can be unfamiliar to family caregivers. Many families are overwhelmed with the uncertainty associated with their loved one’s serious illness. Families are typically not prepared for the patient’s inability to communicate with MV.13
Critical care nurses have an opportunity to recognize the psychological and social importance of family caregivers’ needs for effective communication with the MV patient. Assessment of family communication needs, perceived communication difficulty, and familiarity with AAC strategies can become standard care in the ICU. Nurses can further positively impact patient-family communication by encouraging MV patients and their family caregivers use AAC tools/strategies that are available in the unit. Nurses’ awareness of and familiarity with available communication tools/devices in the unit will be critical to facilitate utilization of the communication tools.
Discussion
Although previous studies revealed the significance of adverse psychological outcomes in family caregivers,19 the FSM is the only model that guides specific interventions to improve family caregivers’ coping and adjustment to the challenging situation of a loved one’s critical illness. Interventions to improve communication between family caregivers and patients might moderate or alleviate families’ distress, and therefore, prevent or reduce adverse psychological outcomes. By extending the FSM to address patient-family communicative interactions with electronic solutions, we propose that more effective communication will help the family caregivers make sense of what is happening. The VidaTalk™ application is an example of a communication intervention that may serve as a bedside activity and provide a means for bringing normalcy to the bedside.
The FSM provides a framework for understanding how critical care nurses can assist ICU family caregivers to overcome a disruptive situation and reduce adverse psychological outcomes through the sensemaking process. The FSM comprehensively considers a crisis, experience, interventions, and psychological outcomes specifically for the population of ICU family caregivers. The FSM, as a middle range theory, is directly applicable to patient-family communication in the ICU. In our expanded version of the FSM, we added a new family communication intervention to the model to guide a communication intervention for ICU family caregivers. Because of its comprehensiveness, the FSM is useful to guide research on short- and long-term adverse psychological outcomes in family caregivers of ICU patients. The use of an electronic communication tool is one possible solution to reduce families’ psychological distress by facilitating communication with the nonvocal ICU patient.
Key Points.
Family caregivers of nonvocal ICU patients are at high risk of developing psychological symptoms and further distressed with communication difficulty, but patient-family communication in the ICU is understudied.
The Facilitated Sensemaking Model (FSM) is the first model to guide nursing interventions to help ICU family caregivers overcome and prevent the adverse psychological outcomes associated with Post-Intensive Care Syndrome (PICS-F).
Applying and expanding the FSM, communication interventions delivered by critical care nurses may facilitate family caregiver bedside activities and a better understanding of the patient’s feelings, symptoms and needs, thereby, reducing anxiety, depression, and PTSD.
Synopsis.
Family caregivers of intensive care unit (ICU) patients are at high risk for adverse psychological outcomes including anxiety, depression, and post-traumatic stress disorder (PTSD). Communication difficulty due to mechanical ventilation may induce or worsen adverse psychological outcomes. The Facilitated Sensemaking Model (FSM) is the first model to guide nursing interventions to help ICU family caregivers overcome and prevent the adverse psychological outcomes associated with Post-Intensive Care Syndrome (PICS-F). This paper addresses an understudied phenomenon, communication between patients and family caregivers during mechanical ventilation, as a source of anxiety and distress for ICU family caregivers. The FSM serves to guide supportive interventions for critical care nurses to improve patient-family communication in the ICU. We propose the addition of an electronic patient-family communication intervention within the pre-existing FSM.
Footnotes
Disclosure Statement
The authors have nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ji Won Shin, The Ohio State University College of Nursing, Columbus, Ohio, United States.
Judith A. Tate, The Ohio State University College of Nursing, Columbus, Ohio, United States.
Mary Beth Happ, The Ohio State University College of Nursing, Columbus, Ohio, United States.
References
- 1.Davidson JE, Hopkins RO, Louis D, Iwashyna TJ. Post-intensive Care Syndrome. 2013; https://www.sccm.org/MyICUCare/THRIVE/Post-intensive-Care-Syndrome. Accessed 4/29, 2019.
- 2.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Critical care medicine. 2012;40(2):618–624. [DOI] [PubMed] [Google Scholar]
- 3.Wunsch H, Wagner J, Herlim M, Chong DH, Kramer AA, Halpern SD. ICU occupancy and mechanical ventilator use in the United States. Critical care medicine. 2013;41(12):2712–2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotondi AJ, Chelluri L, Sirio C, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Critical care medicine. 2002;30(4):746–752. [DOI] [PubMed] [Google Scholar]
- 5.Nelson JE, Meier DE, Litke A, Natale DA, Siegel RE, Morrison RS. The symptom burden of chronic critical illness. Critical care medicine. 2004;32(7):1527–1534. [DOI] [PubMed] [Google Scholar]
- 6.Khalaila R, Zbidat W, Anwar K, Bayya A, Linton DM, Sviri S. Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation. American Journal of Critical Care. 2011;20(6):470–479. [DOI] [PubMed] [Google Scholar]
- 7.Carroll SM. Nonvocal ventilated patients perceptions of being understood. Western journal of nursing research. 2004;26(1):85–103; discussion 104–112. [DOI] [PubMed] [Google Scholar]
- 8.Patak L, Gawlinski A, Fung NI, Doering L, Berg J. Patients’ reports of health care practitioner interventions that are related to communication during mechanical ventilation. Heart & lung : the journal of critical care. 2004;33(5):308–320. [DOI] [PubMed] [Google Scholar]
- 9.Engström Å, Nyström N, Sundelin G, Rattray J. People’s experiences of being mechanically ventilated in an ICU: a qualitative study. Intensive and critical care nursing. 2013;29(2):88–95. [DOI] [PubMed] [Google Scholar]
- 10.Happ MB. Interpretation of nonvocal behavior and the meaning of voicelessness in critical care. Social science & medicine. 2000;50(9):1247–1255. [DOI] [PubMed] [Google Scholar]
- 11.Engström Å, Söderberg S. The experiences of partners of critically ill persons in an intensive care unit. Intensive and Critical Care Nursing. 2004;20(5):299–308. [DOI] [PubMed] [Google Scholar]
- 12.Dreyer A, Nortvedt P. Sedation of ventilated patients in intensive care units: relatives’ experiences. J Adv Nurs. 2008;61(5):549–556. [DOI] [PubMed] [Google Scholar]
- 13.Broyles LM, Tate JA, Happ MB. Use of augmentative and alternative communication strategies by family members in the intensive care unit. American Journal of Critical Care. 2012;21(2):e21–e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Engström Å, Söderberg S. Receiving power through confirmation: the meaning of close relatives for people who have been critically ill. J Adv Nurs. 2007;59(6):569–576. [DOI] [PubMed] [Google Scholar]
- 15.Magnus VS, Turkington L. Communication interaction in ICU--Patient and staff experiences and perceptions. Intensive Crit Care Nurs. 2006;22(3):167–180. [DOI] [PubMed] [Google Scholar]
- 16.Davidson JE. Facilitated sensemaking: a strategy and new middle-range theory to support families of intensive care unit patients. Critical care nurse. 2010;30(6):28–39. [DOI] [PubMed] [Google Scholar]
- 17.Pérez-San Gregorio MA, Blanco-Picabia A, Murillo-Cabezas F, Domínguez-Roldán JM, Sánchez B, Núñez-Roldán A. Psychological problems in the family members of gravely traumatised patients admitted into an intensive care unit. Intensive care medicine. 1992;18(5):278–281. [DOI] [PubMed] [Google Scholar]
- 18.Petrinec AB, Daly BJ. Post-Traumatic Stress Symptoms in Post-ICU Family Members: Review and Methodological Challenges. Western journal of nursing research. 2016;38(1):57–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Beusekom I, Bakhshi-Raiez F, de Keizer NF, Dongelmans DA, van der Schaaf M. Reported burden on informal caregivers of ICU survivors: a literature review. Critical Care. 2015;20(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richards D Prevalence and clinical course of depression: a review. Clinical psychology review. 2011;31(7):1117–1125. [DOI] [PubMed] [Google Scholar]
- 21.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 22.Davidson JE, Powers K, Hedayat KM, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Critical care medicine. 2007;35(2):605–622. [DOI] [PubMed] [Google Scholar]
- 23.Davidson JE, Aslakson RA, Long AC, et al. Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU. Critical care medicine. 2017;45(1):103–128. [DOI] [PubMed] [Google Scholar]
- 24.Egerod I, Schwartz-Nielsen KH, Hansen GM, Lærkner E. The extent and application of patient diaries in Danish ICUs in 2006. Nurs Crit Care. 2007;12(3):159–167. [DOI] [PubMed] [Google Scholar]
- 25.Aitken LM, Rattray J, Hull A, Kenardy JA, Le Brocque R, Ullman AJ. The use of diaries in psychological recovery from intensive care. Critical Care. 2013;17(6):253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones C, Bäckman C, Griffiths RD. Intensive care diaries and relatives’ symptoms of posttraumatic stress disorder after critical illness: a pilot study. American Journal of Critical Care. 2012;21(3):172–176. [DOI] [PubMed] [Google Scholar]
- 27.Kloos JA, Daly BJ. Effect of a Family-Maintained Progress Journal on anxiety of families of critically ill patients. Critical care nursing quarterly. 2008;31(2):96–107; quiz 108–109. [DOI] [PubMed] [Google Scholar]
- 28.Garrouste-Orgeas M, Coquet I, Périer A, et al. Impact of an intensive care unit diary on psychological distress in patients and relatives. Critical care medicine. 2012;40(7):2033–2040. [DOI] [PubMed] [Google Scholar]
- 29.Garrouste-Orgeas M, Max A, Lerin T, et al. Impact of Proactive Nurse Participation in ICU Family Conferences: A Mixed-Method Study. Critical care medicine. 2016;44(6):1116–1128. [DOI] [PubMed] [Google Scholar]
- 30.Moreau D, Goldgran-Toledano D, Alberti C, et al. Junior versus senior physicians for informing families of intensive care unit patients. American journal of respiratory and critical care medicine. 2004;169(4):512–517. [DOI] [PubMed] [Google Scholar]
- 31.Curtis JR, Treece PD, Nielsen EL, et al. Randomized Trial of Communication Facilitators to Reduce Family Distress and Intensity of End-of-Life Care. American journal of respiratory and critical care medicine. 2016;193(2):154–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones C, Skirrow P, Griffiths RD, et al. Post-traumatic stress disorder-related symptoms in relatives of patients following intensive care. Intensive care medicine. 2004;30(3):456–460. [DOI] [PubMed] [Google Scholar]
- 33.MacAulay F, Judson A, Etchels M, et al. ICU-Talk, a communication aid for intubated intensive care patients. Proceedings of the fifth international ACM conference on Assistive technologies; 2002; Edinburgh, Scotland. [Google Scholar]
- 34.Happ MB, Garrett K, Thomas DD, et al. Nurse-patient communication interactions in the intensive care unit. American Journal of Critical Care. 2011;20(2):e28–e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American Speech Language Hearing Association (ASHA). Augmentative and Alternative Communication 2018; https://www.asha.org/public/speech/disorders/AAC/. Accessed March 18, 2018, 2018.
- 36.Ten Hoorn S, Elbers PW, Girbes AR, Tuinman PR. Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Critical care (London, England). 2016;20(1):333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alasad J, Ahmad M. Communication with critically ill patients. J Adv Nurs. 2005;50(4):356–362. [DOI] [PubMed] [Google Scholar]
- 38.Hupcey JE, Penrod J. Going it alone: The experienes of spouses of critically ill patients. Dimensions of Critical Care Nursing. 2000;19(3):44. [PubMed] [Google Scholar]
- 39.Ågård AS, Harder I. Relatives’ experiences in intensive care—Finding a place in a world of uncertainty. Intensive and Critical Care Nursing. 2007;23(3):170–177. [DOI] [PubMed] [Google Scholar]
- 40.Happ MB, Tuite P, Dobbin K, DiVirgilio-Thomas D, Kitutu J. Communication ability, method, and content among nonspeaking nonsurviving patients treated with mechanical ventilation in the intensive care unit. American Journal of Critical Care. 2004;13(3):210–218. [PubMed] [Google Scholar]
- 41.Happ MB, Roesch TK, Garrett K. Electronic voice-output communication aids for temporarily nonspeaking patients in a medical intensive care unit: a feasibility study. Heart & lung : the journal of critical care. 2004;33(2):92–101. [DOI] [PubMed] [Google Scholar]
- 42.Happ MB, Garrett KL, Tate JA, et al. Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: results of the SPEACS trial. Heart & lung : the journal of critical care. 2014;43(2):89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davidson JE, Daly BJ, Agan D, Brady NR, Higgins PA. Facilitated sensemaking: a feasibility study for the provision of a family support program in the intensive care unit. Critical care nursing quarterly. 2010;33(2):177–189. [DOI] [PubMed] [Google Scholar]
- 44.Skoog M, Milner KA, Gatti-Petito J, Dintyala K. The Impact of Family Engagement on Anxiety Levels in a Cardiothoracic Intensive Care Unit. Critical care nurse. 2016;36(2):84–89. [DOI] [PubMed] [Google Scholar]
- 45.Pew Research Center. Mobile Fact Sheet. 2019; https://www.pewresearch.org/internet/fact-sheet/mobile/. Accessed November 7, 2019.
- 46.Happ MB, Swigart VA, Tate JA, Arnold RM, Sereika SM, Hoffman LA. Family presence and surveillance during weaning from prolonged mechanical ventilation. Heart & lung : the journal of critical care. 2007;36(1):47–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davidson JE, McDuffie M, Kay M. Family-centered care. In: Sandra Goldsworthy P, Kleinpell Ruth, Williams G, eds. International Best Practices in Critical Care Nursing 2nd Edition. World Federation of Critical Care Nurses. 2018. Available at: http://wfccn.org/ebook/. [Google Scholar]