Abstract
Background
Black‐White disparities in heart disease treatment may be attributable to differences in physician referral networks. We mapped physician networks for Medicare patients and examined within‐physician Black‐White differences in patient sharing between primary care physicians and cardiologists.
Methods and Results
Using Medicare fee‐for‐service files for 2016 to 2017, we identified a cohort of Black and White patients with heart disease and the primary care physicians and cardiologists treating them. To ensure the robustness of within‐physician comparisons, we restricted the sample to regional health care markets (ie, hospital referral regions) with at least 10 physicians sharing ≥3 Black and White patients. We used claims to construct 2 race‐specific physician network measures: degree (number of cardiologists with whom a primary care physician shares patients) and transitivity (network tightness). Measures were adjusted for Black‐White differences in physician panel size and calculated for all settings (hospital and office) and for office settings only. Of 306 US hospital referral regions, 226 and 145 met study criteria for all settings and office setting analyses, respectively. Black patients had more cardiology encounters overall (6.9 versus 6.6; P<0.001) and with unique cardiologists (3.0 versus 2.6; P<0.001), but fewer office encounters (31.7% versus 41.1%; P<0.001). Primary care physicians shared Black patients with more cardiologists than White patients (mean differential degree 23.4 for all settings and 3.6 for office analyses; P<0.001 for both). Black patient‐sharing networks were less tightly connected in all but office settings (mean differential transitivity −0.2 for all settings [P<0.001] and near 0 for office analyses [P=0.74]).
Conclusions
Within‐physician Black‐White differences in patient sharing exist and may contribute to disparities in cardiac care.
Keywords: cardiology referrals, Medicare, patient sharing, physician networks, racial disparities
Subject Categories: Disparities, Health Services
Nonstandard Abbreviations and Acronyms
- HRR
hospital referral region
- SNA
social network analysis
Clinical Perspective.
What Is New?
Black patients are shared by the same primary care physician with more cardiologists than White patients irrespective of clinical care setting.
These differences occur after adjusting for physicians' White and Black patient panel size.
What Are the Clinical Implications?
Black‐White differences in patient sharing between primary care physicians and cardiologists may lead to disparities in care coordination and quality of care.
Factors underlying differences in the way primary care physicians share their Black and White patients with cardiologists may include differences in treatment setting, disease complexity, and patient preferences.
Each of these factors have different implications for policy and local interventions and need to be better understood.
Black‐White disparities in heart disease treatment have been widely described and persist despite decades of sustained attention. Compared with White patients, Black patients with heart disease are less likely to receive evidence‐based therapies, 1 , 2 , 3 and they have higher rates of adverse outcomes after treatment. 4 , 5 , 6 , 7 , 8 Disparities may be related in part to differences in the providers treating Black and White patients. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16
The role of physicians in health care disparities is supported by a growing body of evidence. Older studies have shown that the care of Black patients is concentrated among a small number of primary care physicians (PCPs) who may have difficulty obtaining specialty referrals, advanced treatments, and elective hospital admissions for their patients. 17 , 18 , 19 More recent studies using computationally powerful social network analysis (SNA) methods 20 , 21 to map large‐scale physician patient‐sharing networks have shown substantial differences in networks treating White and Black patients. Some SNA studies found that physicians practicing in areas with large Black populations had fewer interactions with other network physicians than those practicing in other areas 22 , 23 ; this relative network isolation may have negative consequences for quality of care. Other SNA work found that the segregation of provider teams performing cardiac surgery on Black and White patients within hospitals is associated with higher postoperative mortality for Black patients. 24 One SNA analysis explicitly measured the segregation of physician networks for Black and White patients, 25 but it stopped short of specifically focusing on PCP to specialist (referral) relationships.
To date, little is known about differences in the way Black and White patients are shared by their PCPs with cardiac care specialists. Only 1 prior study 26 evaluated this key entry point into an increasingly integrated health care system 27 and potential pathway for disparities in quality of care. The study, which examined 6 high‐volume specialties, including cardiology, found that PCPs shared Black patients with fewer and different specialists, raising concerns of racial bias in referrals to specialty care. However, analyses were restricted to 12 markets with large proportions of Black patients, providing an incomplete picture of PCP to specialist patient‐sharing patterns. A comprehensive assessment of these patterns is necessary to better understand the contributions of specialty referrals to disparities.
In this study, we conducted a national examination of differences in the way PCPs share their Black and White patients with heart disease with cardiologists across market‐level physician networks. We used claims data for Medicare beneficiaries and SNA methods to map separate market‐level patient‐sharing physician networks treating Black and White patients with heart disease and assessed differences in patient sharing between PCPs and cardiologists.
METHODS
This study was approved by the RAND Institutional Review Board. Because of the retrospective nature of this study, the requirement for informed consent was waived. The sponsors of this study were not involved in data analysis and article preparation. Because of a strict Data Use Agreement with the Centers for Medicare & Medicaid Services, requests to access the data set from qualified researchers trained in human subject confidentiality protocols may be sent to the Centers for Medicare & Medicaid Services.
Data Sources and Study Sample
We used the 100% Medicare Beneficiary Summary File to identify all Black and White fee‐for‐service Medicare patients with heart disease during 2016 to 2017, based on chronic conditions flags 28 for acute myocardial infarction, ischemic heart disease, heart failure, and atrial fibrillation. To ascertain race, we used the Research Triangle Institute Medicare variable, which uses an algorithm including names, surnames, and geography to improve the accuracy of the original Medicare enrollment variable; the Research Triangle Institute variable has high validity for Black and White race. 29 Because racial disparities are often mediated by social drivers of health, we also analyzed a subset of Medicare‐Medicaid dually eligible (low‐income) Black and White patients. 30
We used Medicare Carrier and Outpatient files to obtain all claims submitted for these patients by PCPs (ie, internal medicine, family medicine, geriatrics, and general practice physicians) and cardiologists. We used Medicare specialty codes present on claims to ascertain physician specialty.
Mapping Physician Networks for Cardiac Care
We mapped physician networks at the US hospital referral region (HRR) level. HRRs are regional markets for tertiary health care with at least 1 hospital performing major cardiac procedures. We assigned Medicare patients to HRRs based on their residential zip code. We then assigned PCPs and cardiac specialists to HRRs as follows: First, we identified all the HRRs where patients treated by each physician resided. Second, we identified each physician's organizational affiliations using a unique data set developed by the RAND Center of Excellence on Health System Performance. 31 , 32 Within this data set, physicians are assigned to physician organizations; in turn, physician organizations are assigned to HRRs. We included physicians in a particular HRR network if (1) the physician treated patients residing in the HRR and (2) the physician's organization had office locations in that HRR. Using this algorithm, we assigned 98% of physicians to HRR networks, with most (92%) assigned to 1 or 2 networks.
We used physician claims and SNA methods to map the HRR networks. 20 In these networks, nodes represent physicians, and ties between nodes represent shared patients (ie, patients for whom both physicians submitted claims). Following prior work, 21 , 26 we ascertained a tie between 2 physicians if they shared ≥3 patients. This ensured that we identified nonspurious relationships between physicians. To focus on specialty referrals, we restricted networks to ties between PCPs and cardiologists.
For each HRR, we mapped 2 physician networks for comparison: one reflecting PCP‐cardiologist connections based on shared White patients, and the other reflecting connections based on shared Black patients. In this approach, 2 physicians may be connected in 1 patient‐sharing network but not in the other within the HRR (Figure). Because the study focused on within‐PCP racial differences in patient sharing, we limited our analyses to physicians sharing at least 3 Black and 3 White patients and HRRs with at least 10 such physicians, to ensure the statistical robustness of comparisons.
Figure 1. Physician participation in Black and White market‐level patient‐sharing networks: an example.
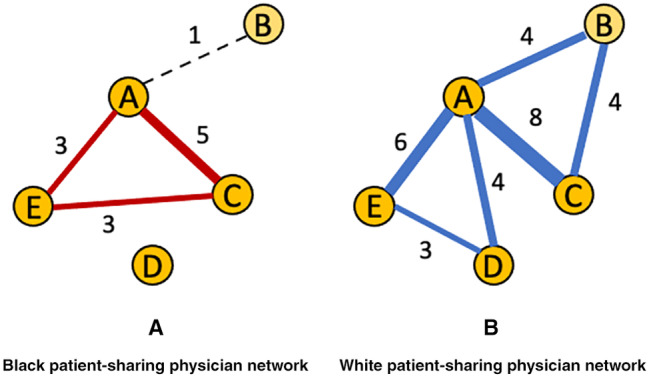
Physicians are represented as nodes, and shared patients are represented as ties. Physicians A, C, and E share ≥3 Black patients and ≥3 White patients and are included in both the Black (A) and White (B) patient‐sharing networks, whereas physicians B and D only share ≥3 White patients and are included only in the White patient‐sharing network.
In addition, because differences in Black and White patient‐sharing networks' characteristics may be attributable to Black and White patients using medical services differently by setting (eg, Black patients use PCPs less often as usual source of care 33 ), we mapped networks from claims submitted in all settings of care (ie, hospital inpatient or outpatient, emergency department, and office type settings), and then only using claims submitted in office type settings. Office settings were identified via Evaluation and Management Healthcare Common Procedure Coding System codes. Analyses of all care settings included 226 HRRs, whereas those restricted to office settings included 145 HRRs. Included HRRs were located in all 4 US Census regions: 14.2% in the Northeast, 49.6% in the South, 24.8% in the Midwest, and 11.5% in the West for all setting analyses; and 13.8% in the Northeast, 55.9% in the South, 22.8% in the Midwest, and 7.6% in the West for office setting analyses. Excluded HRRs had smaller patient populations, fewer physicians, and fewer connections among them (Table S1).
The final study cohort included 88% of all White and 99% of all Black Medicare fee‐for‐service beneficiaries with heart disease during 2016 to 2017 in all setting analyses, and 67% of White and 92% of Black Medicare beneficiaries in office analyses.
Last, to approximate episodes of care, we conducted analyses using network ties observed during the entire study period (2 years) and restricted to encounters occurring within 90 days of each other.
Measuring Network Characteristics
We calculated 2 network measures that are potentially relevant to understanding differences in referral networks: degree and transitivity. 34 Degree is a measure of a physician's connections with other physicians in the network, via shared patients. In this analysis of network relationships between PCPs and cardiologists, the Black and White physician degree measures represent the number of cardiologists with whom each PCP shares his/her Black and White patients, respectively. Higher degree per physician has been associated with increased hospital and emergency department use for network patients. 35 , 36 Transitivity describes the tightness of a network or the propensity of each physician to share patients (ie, form triads) with network physicians who are also connected to each other. Although there are no established absolute cutoffs for high versus low network transitivity, higher values represent higher network tightness and values can be compared across similarly constructed networks, such as the Black and White patient‐sharing networks in this study. In our case, Black and White transitivity values are based on the proportion of an individual physician's peers who also share patients with each other in the Black or White patient‐sharing networks, respectively. Higher network transitivity has been associated with better care coordination and patient satisfaction. 35 , 37
For each physician who shared both Black and White patients, we computed separate Black and White degree and transitivity measures and the Black‐White difference in measures based on their participation in the Black and White patient‐sharing networks. The Black‐White differential degree represents the difference in the number of cardiologists with whom each PCP is sharing his/her Black versus White patients, whereas the Black‐White differential transitivity represents the difference in the probability for a physician to share Black versus White patients with other physicians also connected to each other. These differences are calculated for each physician in comparison to herself/himself, using either their Black or White patients.
More important, the probability that a physician appears in the White patient‐sharing network but not in the Black network (or vice versa) increases with the increase in difference between each physician's Black and White patient panel sizes; therefore, we adjusted the measures for differences in these counts. Most HRRs, and most physicians within them, had more White patients. For these HRRs, we refitted networks by randomly sampling 10 sets of White patients from each physician's own White patient panel using a sample size equal to his/her own number of Black patients. We then calculated the degree and transitivity based on each of the 10 random samples and averaged across to obtain resampled estimates of White patient‐sharing network degree and transitivity measures. Three HRRs had higher Black patient counts; the same correction method was applied, but randomly sampling was used among the Black patients of each physician. This adjustment allowed us to understand whether degree and transitivity differ systematically based on how physicians share their White and Black patients rather than simply reflecting a difference in Black and White patient counts. 36 Finally, for HRR‐level comparisons, we averaged physician‐level measures of degree and transitivity within an HRR.
Statistical Analysis
We used t tests for all study comparisons. For comparisons of Black and White Medicare patients' encounter rates with different provider specialties, we applied the Welch (2‐sample unequal variances) t test with Satterthwaite approximation and applied across all beneficiaries. For within‐physician comparisons of Black versus White patient sharing, we used 1‐sample t tests. All t tests were 2‐tailed. The units of analysis were unique Medicare beneficiaries for Black‐White comparisons of encounters by type of setting and unique physicians for within‐physician Black‐White comparisons of degree and transitivity. All data management steps and statistical tests for patient encounters and type of settings were performed with SAS, version 9.4. All physician network statistical analyses were performed with base R, version 4.1.3.
RESULTS
Table 1 describes the overall specialty composition and structure of physician patient‐sharing HRR networks. The number of PCPs and cardiologists varied widely across study networks from 113 to 5112 PCPs and from 11 to 1032 cardiologists in all setting analyses and from 49 to 3014 PCPs and from 11 to 611 cardiologists in office setting analyses.
Table 1.
Characteristics of HRR‐Level Patient‐Sharing Networks for Black and White Medicare Beneficiaries Treated for Heart Disease During 2016 to 2017
| HRR characteristic | All care settings (N=226)* | Office settings (N=145)* | ||
|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | |
| No. of PCPs | 935.5 (810.0) | 113–5112 | 604.3 (533.3) | 49–3014 |
| No. of cardiologists | 175.7 (150.6) | 11–1032 | 121.1 (118.4) | 11–611 |
| Overall† network degree | 36.9 (16.0) | 11.2–93.5 | 12.8 (4.2) | 4.3–24.9 |
| Overall† network transitivity | 0.8 (0.0) | 0.7–0.8 | 0.6 (0.1) | 0.4–0.8 |
| PCP network degree | 23.9 (10.5) | 6.1–61.0 | 8.0 (2.6) | 2.9–15.5 |
| PCP network transitivity | 0.8 (0.0) | 0.7–0.9 | 0.6 (0.1) | 0.5–0.8 |
| % PCPs included‡ in network comparisons | 46.2 (18.2) | 9.3–86.1 | 30.8 (20.2) | 2.0–79.6 |
| % Cardiologists included‡ in network comparisons | 57.4 (20.9) | 13.2–100 | 52.5 (19.9) | 6.8–95.3 |
HRR indicates hospital referral region; N, number of HRRs; and PCP, primary care physician.
Analyses were restricted to HRRs for which we were able to calculate Black‐White differential degree and transitivity.
Network measures calculated for all PCPs and cardiologists within the HRR who shared at least 3 Medicare patients with heart disease.
Physicians who shared at least 3 Black and 3 White patients within the HRR and were thus included in final analyses of differential degree and transitivity.
The mean overall network degree (ie, including PCPs and cardiologists sharing at least 3 patients irrespective of race) was 36.9 for all care settings and 12.8 for office settings (Table 1), meaning that, on average, physicians shared Medicare patients with heart disease with 37 other physicians in all settings and 13 other physicians in office settings over the entire study period. The mean overall network transitivity was 0.8 and 0.6 in all settings versus office settings only, respectively. The mean degree for PCPs only was somewhat lower (degree, 23.9 versus 8.0), whereas mean transitivity was similar (0.8 versus 0.6) to the overall network measures, in analyses of all settings and office settings, respectively.
Physicians included in the final Black‐White differential degree and transitivity comparisons (ie, those sharing at least 3 Black and 3 White patients with cardiologists within the HRR) represented on average 46.2% of all PCPs and 57.4% of all cardiologists in all setting networks, and 30.8% of all PCPs and 52.5% of all cardiologists in office setting only networks (Table 1).
Table 2 presents the proportion of cardiology encounters occurring in different types of care settings and the numbers of total visits and visits with unique cardiologists for Black and White Medicare patients. Black Medicare patients saw a cardiologist significantly less often in office settings (31.7% versus 41.1%; P<0.001) and more often in nonoffice settings (68.3% versus 58.9%; P<0.001). In analyses of all care settings, Black Medicare patients had more visits with cardiologists overall (mean, 6.9 versus 6.6; P<0.001) and with unique cardiologists (3.0 versus 2.6; P<0.001) than White Medicare patients. This difference stemmed from higher numbers of visits in the nonoffice setting: office‐based visits were similar for Black and White patients (Table 2).
Table 2.
Counts of Cardiology Encounters for Black and White Medicare Patients With Heart Disease During 2016 to 2017, Overall and by Type of Setting
| Variable | Black beneficiaries (N=945 227) | White beneficiaries (N=6 980 486) | P value* |
|---|---|---|---|
| All care settings | |||
| No. of cardiology encounters, mean (SD) | 6.9 (8.4) | 6.8 (7.6) | <0.001 |
| Encounters with unique cardiologists, mean (SD) | 3.0 (2.7) | 2.6 (2.2) | <0.001 |
| Office settings | |||
| % of All visits | 31.7 (34.6) | 41.1 (35.4) | <0.001 |
| No. of cardiology encounters, mean (SD) | 3.8 (3.7) | 3.9 (3.8) | <0.001 |
| Encounters with unique cardiologists, mean (SD) | 1.3 (0.6) | 1.2 (0.6) | <0.001 |
| Nonoffice settings | |||
| % of All visits | 68.3 (34.6) | 58.9 (35.4) | <0.001 |
| No. of cardiology encounters, mean (SD) | 5.2 (7.3) | 4.6 (5.9) | <0.001 |
| Encounters with unique cardiologists, mean (SD) | 2.9 (2.7) | 2.6 (2.2) | <0.001 |
All data are reported as mean (SD). N indicates number of Black and White Medicare beneficiaries.
P values were estimated via 2‐tailed Welch (2‐sample unequal variances) t test with Satterthwaite approximation and applied across all beneficiaries in the study hospital referral regions.
In analyses of all care settings, 21% of Medicare patients were Medicare‐Medicaid dually eligible for at least 1 month during the study, but the percentage varied substantially by race (18% White and 50% Black Medicare patients were dually eligible). In analyses of office settings, percentages were smaller, but the Black‐White difference remained substantial (12% overall, 12% White, and 28% Black Medicare patients were dually eligible).
Table 3 describes the types of heart diseases for which Black and White Medicare patients in the study sample were treated, and the prevalence of 1 versus >1 distinct condition. Black patients were treated more often for heart failure, whereas White patients were more often treated for atrial fibrillation; the prevalence of coronary heart disease was relatively similar. Black patients were also treated for >1 condition slightly more often than White patients.
Table 3.
Types and Counts of Heart Diseases That Study Black and White Medicare Patients Were Treated For
| Variable | All settings | Office settings only | ||
|---|---|---|---|---|
| Black patients (N=1 246 260) | White patients (N=10 279 661) | Black patients (N=993 867) | White patients (N=9 032 347) | |
| Heart failure (yes/no) | 57.9 | 43.0 | 56.4 | 41.3 |
| Atrial fibrillation (yes/no) | 15.5 | 29.7 | 15.9 | 30.5 |
| Ischemic heart disease (yes/no) | 79.2 | 81.4 | 80.4 | 82.2 |
| AMI condition flag (yes/no) | 4.6 | 4.4 | 4.6 | 4.3 |
| No. of heart diseases | ||||
| 1 | 54.8 | 56.8 | 55.4 | 57.3 |
| ≥2 | 45.2 | 43.2 | 44.6 | 42.7 |
Data are given as percentage of each group. AMI indicates acute myocardial infarction; and N, number of Black and White Medicare beneficiaries.
Table 4 and Table S2 present the HRR‐level Black‐White differences in adjusted network degree and transitivity for most HRRs, which had higher numbers of White patients, and for 3 HRRs with higher numbers of Black patients, respectively. A mean difference near 0 for a particular network characteristic indicates that the White and Black patient‐sharing networks are highly similar with respect to that characteristic.
Table 4.
Mean HRR‐Level Black‐White Differential Network Degree and Transitivity for Patient‐Sharing Networks With Higher Numbers of White Medicare Patients
| Network type | HRRs, N | Black‐White differential degree, mean (SD) | P value* | Black‐White differential transitivity, mean (SD) | P value* |
|---|---|---|---|---|---|
| Networks based on patients shared at any point during the entire study period | |||||
| PCP−cardiologist ties, all settings | 222 | 23.4 (10.4) | <0.001 | −0.2 (0.1) | <0.001 |
| PCP−cardiologist ties, office settings | 139 | 3.6 (1.9) | <0.001 | −0.0 (0.1) | 0.74 |
| Networks restricted to Medicare‐Medicaid dually eligible patients† | |||||
| PCP−cardiologist ties, all settings | 202 | 10.3 (5.8) | <0.001 | −0.09 (0.09) | <0.001 |
| Networks restricted to patients shared within 90 d | |||||
| PCP−cardiologist ties, all settings | 223 | 23.8 (10.5) | <0.001 | −0.4 (0.1) | <0.001 |
| PCP‐cardiologist ties, office settings | 135 | 4.1 (2.1) | <0.001 | −0.0 (0.1) | 0.31 |
HRR indicates hospital referral region; N HRR, number of HRRs for which we could calculate differential degree and transitivity; and PCP, primary care physician.
P values were estimated via 1‐sample, 2‐tailed t tests of the differences in each physician's Black and resampled White degree and transitivity.
For this subset of patients, we did not have sufficient power to perform comparisons limited to office settings only.
For most HRRs (Table 4), the mean adjusted degree was significantly higher in the Black patient‐sharing networks than in the White patient‐sharing networks (differential Black‐White degree, 23.4 for all settings and 3.6 for office settings only; P<0.001 for both), meaning that, compared with White patients, PCPs shared their Black patients with heart disease with 23.4 more cardiologists in all settings and 3.6 more cardiologists in office settings during the 2‐year study period. Mean adjusted transitivity (network tightness) was lower for Black patient‐sharing networks in analyses of all settings (−0.2; P<0.001), meaning that physicians were less connected in the Black patient‐sharing networks, but analyses restricted to offices settings yielded similar transitivity for White and Black patient‐sharing networks.
Subanalyses of dual‐eligible patient‐sharing networks were limited to all care settings (only 6 HRRs had physicians sharing ≥3 White and ≥3 Black dual‐eligible patients in office settings, and power was insufficient for calculating differential network measures). These analyses also found robust Black‐White degree and transitivity differences (Table 4). Finally, analyses restricted to networks based on encounters occurring within 90 days yielded similar results in terms of direction, magnitude, and significance (Table 4).
The 3 HRRs with higher numbers of Black patients (Table S2) also showed higher adjusted degree for Black versus White patient‐sharing networks, but, different from the other HRRs, adjusted transitivity was larger (except for New Orleans, LA office settings), meaning that for these 3 markets, Black patient‐sharing networks were more tightly connected.
DISCUSSION
In this study of physician networks for cardiac care, we found significant differences in the way Black and White fee‐for‐service Medicare beneficiaries are shared between PCPs and cardiologists. First, we found that Black beneficiaries were shared by their PCPs with more specialists, on average, compared with White beneficiaries. This finding was consistent in analyses using all claims (ie, including hospital and emergency department settings) and in analyses restricted to office‐based claims, but the magnitude of difference was attenuated when restricted to the office setting. Second, we found that network transitivity (tightness) was lower for Black versus White patient‐sharing networks in all setting analyses, but this difference became nonsignificant in analyses restricted to the office setting. For both network measures, the substantial decrease in the Black‐White difference between all settings and office settings may be attributable to greater use of nonoffice care settings among Black beneficiaries with heart disease, as those types of settings (eg, emergency department or hospital care) likely result in sharing of patients between physicians who do not typically work together (eg, PCPs providing usual care and cardiologists providing emergency care at hospitals that the PCPs are not affiliated with). This type of sharing would both increase degree and reduce transitivity.
Perhaps the single most important finding of the current study is that Black patients are shared by the same PCP with more cardiologists (eg, referred to more cardiologists) than White patients, even in analyses restricted to office settings. In contrast, another recent study 26 found that Black patients may be shared with fewer specialists compared with White patients, a finding explained as possibly attributable to lesser access to specialty care for Black patients. The prior study was limited to 12 select markets with large Black populations, and primary analyses did not account for differences arising from 1 patient group (Black patients) being much smaller than the other patient group (White patients). In secondary analyses that similarly performed a resampling procedure to account for these differences, however, the results became nonsignificant or changed direction.
The patterns we observe in our analyses (ie, Black Medicare patients with heart disease being shared with a higher number of specialists) may be attributable to several reasons. The large Black‐White differential degree observed in analyses of all settings may be related at least in part to Black Medicare patients receiving treatment for heart disease more often in nonoffice settings, attributable to either having less often a usual source or care or higher disease severity. However, in analyses restricted to office settings, we also observed a smaller but significant difference in the number of cardiologists that a PCP shared their Black and White patients with. The relationships captured in these analyses are likely to be mostly referrals, as self‐referral to specialty care is relatively rare in the office setting. 38 , 39 This finding may have several implications that deserve discussion.
First, little is known about physician referral processes in general, 40 and even less about racial differences in referrals and how they may lead to health disparities. Coordination of care has been shown to improve patient outcomes, 41 yet may be difficult to achieve if the specialists with whom PCPs share their patients change often; PCPs rely on communications with and from specialists to provide timely, good quality care. 42 Recent SNA work found that patients in networks with more specialist connections per PCP and less stable ties had higher rates of emergency department visits 35 and hospitalizations. 43 Consequently, fewer PCP to specialist ties (as noted for White patients in our study) may reflect more continuity of care and possibly better care coordination. This explanation is also strengthened by prior work showing that fewer, repeated interactions between PCPs and specialists (ie, PCPs referring patients to fewer distinct specialists) result in lower health care service use while maintaining high quality of care. 44
Second, prior work shows that Black patients are more likely to receive care at large, urban teaching hospitals. 45 , 46 Thus, it is possible that Black patients may be seen more often by different members of cardiology groups at these large academic medical centers, although they may be referred to the same practice consistently. This is particularly true for patients seen by medical trainees who submit claims under the National Provider Identifiers of interchangeable supervising attending physicians, and prior work has shown that Black and low‐income patients are more often treated by trainees than White patients at the same academic medical center. 47
Third, Black patients may present for cardiac care with more complex heart disease, leading to greater use of more and diverse cardiology specialists. In our study, Black patients were more often treated for heart failure and had ≥2 distinct conditions slightly more often. Heart failure is treatment intensive, potentially requiring visits to different subspecialists (eg, interventional cardiologists, electrophysiologists, and advanced heart failure/transplant specialists), which, in addition to other heart diseases, may contribute to our finding of a significant Black‐White differential degree. However, Black‐White differences in encounters with unique cardiologists were small, suggesting that these differences are unlikely to explain the within‐PCP difference in patient sharing observed in all settings. Fourth, subanalyses limited to dually eligible Medicare‐Medicaid patients, who typically have low income and high medical complexity, showed similar findings, suggesting that the differential degree is not mediated by Black patients' being disproportionately enrolled in these programs. Last, prior work showing persistent geographic and health care segregation 33 , 48 and high levels of health care system distrust for Black patients 33 , 49 , 50 , 51 suggests that Black patients may also follow different referral patterns because of unmeasured factors, such as geographic access and patient preferences.
Unlike differences in degree, differences in transitivity were not significant for networks limited to office settings, meaning that overall, physicians have similarly (more or less) tight office‐based connections with their network peers when providing care to Black and White Medicare patients with heart disease. Although this finding may be more difficult to interpret in terms of access to specialty care, prior work has shown that higher transitivity is associated with better coordination of care as well as better patient experience, 37 implying that Black and White patients receive, at least in some respects, similar quality of care. Further work is needed to better understand both the properties of transitivity in physician networks and its implications for processes of care 52 and disparities in quality of care.
Several limitations to the current study should be noted. First, although PCP to cardiologist referrals likely contribute the largest share to the observed patient‐sharing patterns, these patterns may also include other types of shared care (eg, emergent care for all settings or self‐referral for office settings). In addition, to assess within‐physician differences in patient sharing, our study has focused on physicians sharing both White and Black patients with heart disease and HRRs with at least 10 such physicians. Other types of analyses are needed to understand differences between physicians treating only or predominantly Black patients or White patients, or physicians treating lower numbers of patients in smaller, excluded HRRs. Finally, prior work suggests that network structure differs based on the types of claims used. 53 Our findings are based on claims submitted for aged Medicare fee‐for‐service beneficiaries; however, other types of health care disparities could be investigated using different claims and similar methods.
Despite these limitations, the current study offers the most comprehensive analysis to date of physician networks for cardiac care, as well as a starting point for research into the factors underlying the differences in the way PCPs share (eg, refer) their Black and White patients with specialists and consequences for outcome disparities. Each of the potential factors contributing to the observed patterns, as discussed above, may have different implications for local disparities’ policy. For example, differences in PCP degree that are attributable to the care setting (eg, academic center) may need interventions to improve equal access to types of specialists practicing in those settings, whereas differences attributable to patients' comfort level with specialists at some institutions may need interventions to regain community trust. Disentangling these scenarios will require further qualitative and survey research, combined with local in‐depth analyses focused on referral patterns and the relative roles of patients and providers in treatment decision‐making.
Sources of Funding
The study was funded by grants from the National Institutes of Health (National Heart, Lung, and Blood Institute, R01HL148420) and the Agency for Healthcare Research and Quality (1U19HS024067‐01).
Disclosures
None.
Supporting information
Tables S1–S2
This article was sent to Mahasin S. Mujahid, PhD, MS, Associate Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.123.030653
For Sources of Funding and Disclosures, see page 8.
References
- 1. Desai NR, Udell JA, Wang Y, Spatz ES, Dharmarajan K, Ahmad T, Julien HM, Annapureddy A, Goyal A, de Lemos JA, et al. Trends in performance and opportunities for improvement on a composite measure of acute myocardial infarction care. Circ Cardiovasc Qual Outcomes. 2019;12:e004983. doi: 10.1161/CIRCOUTCOMES.118.004983 [DOI] [PubMed] [Google Scholar]
- 2. Singh JA, Lu X, Ibrahim S, Cram P. Trends in and disparities for acute myocardial infarction: an analysis of Medicare claims data from 1992 to 2010. BMC Med. 2014;12:190. doi: 10.1186/s12916-014-0190-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lui C, Fraser CD, Zhou X, Suarez‐Pierre A, Kilic A, Zehr KJ, Higgins RSD. Racial disparities in patients bridged to heart transplantation with left ventricular assist devices. Ann Thorac Surg. 2019;108:1122–1126. doi: 10.1016/j.athoracsur.2019.03.073 [DOI] [PubMed] [Google Scholar]
- 4. Bolorunduro OB, Kiladejo AV, Animashaun IB, Akinboboye OO. Disparities in revascularization after ST elevation myocardial infarction (STEMI) before and after the 2002 IOM report. J Natl Med Assoc. 2016;108:119–123. doi: 10.1016/j.jnma.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 5. Brown TM, Deng LQ, Becker DJ, Bittner V, Levitan EB, Rosenson RS, Safford MM, Muntner P. Trends in mortality and recurrent coronary heart disease events after an acute myocardial infarction among Medicare beneficiaries, 2001‐2009. Am Heart J. 2015;170:249–255. doi: 10.1016/j.ahj.2015.04.027 [DOI] [PubMed] [Google Scholar]
- 6. Chaudhry SI, Khan RF, Chen J, Dharmarajan K, Dodson JA, Masoudi FA, Wang Y, Krumholz HM. National trends in recurrent AMI hospitalizations 1 year after acute myocardial infarction in Medicare beneficiaries: 1999–2010. J Am Heart Assoc. 2014;3:e001197. doi: 10.1161/JAHA.114.001197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Angraal S, Khera R, Wang Y, Lu Y, Jean R, Dreyer RP, Geirsson A, Desai NR, Krumholz HM. Sex and race differences in the utilization and outcomes of coronary artery bypass grafting among Medicare beneficiaries, 1999‐2014. J Am Heart Assoc. 2018;7:e009014. doi: 10.1161/JAHA.118.009014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Becker ER, Rahimi A. Disparities in race/ethnicity and gender in in‐hospital mortality rates for coronary artery bypass surgery patients. J Natl Med Assoc. 2006;98:1729–1739. [PMC free article] [PubMed] [Google Scholar]
- 9. Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–2641. doi: 10.1161/CIRCULATIONAHA.105.543231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jha AK, Orav EJ, Epstein AM. Low‐quality, high‐cost hospitals, mainly in South, care for sharply higher shares of elderly black, Hispanic, and Medicaid patients. Health Affair. 2011;30:1904–1911. doi: 10.1377/hlthaff.2011.0027 [DOI] [PubMed] [Google Scholar]
- 11. Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167:1177–1182. doi: 10.1001/archinte.167.11.1177 [DOI] [PubMed] [Google Scholar]
- 12. Dimick J, Ruhter J, Sarrazin MV, Birkmeyer JD. Black patients more likely than whites to undergo surgery at low‐quality hospitals in segregated regions. Health Affair. 2013;32:1046–1053. doi: 10.1377/hlthaff.2011.1365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Girotti ME, Shih T, Revels S, Dimick JB. Racial disparities in readmissions and site of care for major surgery. J Am Coll Surg. 2014;218:423–430. doi: 10.1016/j.jamcollsurg.2013.12.004 [DOI] [PubMed] [Google Scholar]
- 14. Rangrass G, Ghaferi AA, Dimick JB. Explaining racial disparities in outcomes after cardiac surgery the role of hospital quality. JAMA Surg. 2014;149:223–227. doi: 10.1001/jamasurg.2013.4041 [DOI] [PubMed] [Google Scholar]
- 15. Popescu I, Cram P, Vaughan‐Sarrazin MS. Differences in admitting hospital characteristics for black and white Medicare beneficiaries with acute myocardial infarction. Circulation. 2011;123:2710–2716. doi: 10.1161/CIRCULATIONAHA.110.973628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Popescu I, Nallamothu BK, Vaughan‐Sarrazin MS, Cram P. Racial differences in admissions to high‐quality hospitals for coronary heart disease. Arch Intern Med. 2010;170:1209–1215. doi: 10.1001/archinternmed.2010.227 [DOI] [PubMed] [Google Scholar]
- 17. Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–584. doi: 10.1056/NEJMsa040609 [DOI] [PubMed] [Google Scholar]
- 18. Reschovsky JD, O'Malley AS. Do primary care physicians treating minority patients report problems delivering high‐quality care? Health Aff (Millwood). 2008;27:w222–w231. doi: 10.1377/hlthaff.27.3.w222 [DOI] [PubMed] [Google Scholar]
- 19. Varkey AB, Manwell LB, Williams ES, Ibrahim SA, Brown RL, Bobula JA, Horner‐Ibler BA, Schwartz MD, Konrad TR, Wiltshire JC, et al. Separate and unequal: clinics where minority and nonminority patients receive primary care. Arch Intern Med. 2009;169:243–250. doi: 10.1001/archinternmed.2008.559 [DOI] [PubMed] [Google Scholar]
- 20. Barnett ML, Landon BE, O'Malley AJ, Keating NL, Christakis NA. Mapping physician networks with self‐reported and administrative data. Health Serv Res. 2011;46:1592–1609. doi: 10.1111/j.1475-6773.2011.01262.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Landon BE, Keating NL, Barnett ML, Onnela JP, Paul S, O'Malley AJ, Keegan T, Christakis NA. Variation in patient‐sharing networks of physicians across the United States. JAMA. 2012;308:265–273. doi: 10.1001/jama.2012.7615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ghomrawi HMK, Funk RJ, Parks ML, Owen‐Smith J, Hollingsworth JM. Physician referral patterns and racial disparities in total hip replacement: a network analysis approach. PLoS One. 2018;13:e0193014. doi: 10.1371/journal.pone.0193014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hollingsworth JM, Funk RJ, Garrison SA, Owen‐Smith J, Kaufman SR, Landon BE, Birkmeyer JD. Differences between physician social networks for cardiac surgery serving communities with high versus low proportions of black residents. Medical Care. 2015;53:160–167. doi: 10.1097/MLR.0000000000000291 [DOI] [PubMed] [Google Scholar]
- 24. Hollingsworth JM, Yu XS, Yan PL, Yoo H, Telem DA, Yankah EN, Zhu J, Waljee AK, Nallamothu BK. Provider care team segregation and operative mortality following coronary artery bypass grafting. Circ Cardiovasc Qual Outcomes. 2021;14:e007778. doi: 10.1161/CIRCOUTCOMES.120.007778 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25. Austin AM, Carmichael DQ, Bynum JPW, Skinner JS. Measuring racial segregation in health system networks using the dissimilarity index. Soc Sci Med. 2019;240:112570. doi: 10.1016/j.socscimed.2019.112570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Landon BE, Onnela JP, Meneades L, O'Malley AJ, Keating NL. Assessment of racial disparities in primary care physician specialty referrals. JAMA Netw Open. 2021;4:e2029238. doi: 10.1001/jamanetworkopen.2020.29238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Machta RM, Reschovsky J, Jones DJ, Kimmey L, Furukawa MF, Rich EC. Health system integration with physician specialties varies across markets and system types. Health Serv Res. 2020;55(Suppl 3):1062–1072. doi: 10.1111/1475-6773.13584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chronic conditions data warehouse. Centers for Medicare & Medicaid Services. https://www2.ccwdata.org/web/guest/condition‐categories Accessed December 17, 2020. [Google Scholar]
- 29. Jarrin OF , Nyandege AN, Grafova IB, Dong X, Lin H. Validity of race and ethnicity codes in Medicare administrative data compared with gold‐standard self‐reported race collected during routine home health care visits. Med Care. 2020;58:e1–e8. doi: 10.1097/MLR.0000000000001216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. The Medicare Payment Advisory Commission (MedPAC) . Report to the Congress: New Approaches in Medicare. Washington, DC: MedPAC; 2004. Dual eligible beneficiaries: an overview. Pages 71‐92. https://www.medpac.gov/wp‐content/uploads/import_data/scrape_files/docs/default‐source/reports/June04_ch3.pdf Accessed October 30, 2023. [Google Scholar]
- 31. Kranz AM, DeYoreo M, Eshete‐Roesler B, Damberg CL, Totten M, Escarce JJ, Timbie JW. Health system affiliation of physician organizations and quality of care for Medicare beneficiaries who have high needs. Health Serv Res. 2020;55(Suppl 3):1118–1128. doi: 10.1111/1475-6773.13570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Timbie JW, Kranz AM, DeYoreo M, Eshete‐Roesler B, Elliott MN, Escarce JJ, Totten ME, Damberg CL. Racial and ethnic disparities in care for health system‐affiliated physician organizations and non‐affiliated physician organizations. Health Serv Res. 2020;55(Suppl 3):1107–1117. doi: 10.1111/1475-6773.13581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Arnett MJ, Thorpe RJ Jr, Gaskin DJ, Bowie JV, LaVeist TA. Race, medical mistrust, and segregation in primary care as usual source of care: findings from the Exploring Health Disparities in Integrated Communities study. J Urban Health. 2016;93:456–467. doi: 10.1007/s11524-016-0054-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. O'Malley AJ, Marsden PV. The analysis of social networks. Health Serv Outcomes Res Methodol. 2008;8:222–269. doi: 10.1007/s10742-008-0041-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. DuGoff EH, Cho J, Si Y, Pollack CE. Geographic variations in physician relationships over time: implications for care coordination. Med Care Res Rev. 2018;75:586–611. doi: 10.1177/1077558717697016 [DOI] [PubMed] [Google Scholar]
- 36. Barnett ML, Christakis NA, O'Malley J, Onnela JP, Keating NL, Landon BE. Physician patient‐sharing networks and the cost and intensity of care in US hospitals. Med Care. 2012;50:152–160. doi: 10.1097/MLR.0b013e31822dcef7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Moen EL, Bynum JPW. Evaluation of physician network‐based measures of care coordination using Medicare patient‐reported experience measures. J Gen Intern Med. 2019;34:2482–2489. doi: 10.1007/s11606-019-05313-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Forrest CB, Weiner JP, Fowles J, Vogeli C, Frick KD, Lemke KW, Starfield B. Self‐referral in point‐of‐service health plans. JAMA. 2001;285:2223–2231. doi: 10.1001/jama.285.17.2223 [DOI] [PubMed] [Google Scholar]
- 39. Lantz R, Young S, Lubov J, Ahmed A, Markert R, Sadhu S. Self‐ vs provider‐referral differences for coronary artery calcium testing. Am Heart J Plus. 2022;13:100088. doi: 10.1016/j.ahjo.2022.100088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Katz MH. A new paradigm for primary care‐reply. Arch Intern Med. 2012;172:894. doi: 10.1001/archinternmed.2012.1183 [DOI] [PubMed] [Google Scholar]
- 41. Chen LM, Ayanian JZ. Care continuity and care coordination: what counts? JAMA Intern Med. 2014;174:749–750. doi: 10.1001/jamainternmed.2013.14331 [DOI] [PubMed] [Google Scholar]
- 42. Schiaffino MK, Murphy JD, Nalawade V, Nguyen P, Shakya H. Association of physician referrals with timely cancer care using tumor registry and claims data. Health Equity. 2022;6:106–115. doi: 10.1089/heq.2021.0089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Landon BE, Keating NL, Onnela JP, Zaslavsky AM, Christakis NA, O'Malley AJ. Patient‐sharing networks of physicians and health care utilization and spending among Medicare beneficiaries. JAMA Intern Med. 2018;178:66–73. doi: 10.1001/jamainternmed.2017.5034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Agha L, Ericson KM, Geissler KH, Rebitzer JB. Team relationships and performance: evidence from healthcare referral networks. Manage Sci. 2022;68:3175–3973. doi: 10.1287/mnsc.2021.4091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kahn KL, Pearson ML, Harrison ER, Desmond KA, Rogers WH, Rubenstein LV, Brook RH, Keeler EB. Health care for black and poor hospitalized Medicare patients. JAMA. 1994;271:1169–1174. doi: 10.1001/jama.1994.03510390039027 [DOI] [PubMed] [Google Scholar]
- 46. Iwashyna TJ, Curlin FA, Christakis NA. Racial, ethnic, and affluence differences in elderly patients' use of teaching hospitals. J Gen Intern Med. 2002;17:696–703. doi: 10.1046/j.1525-1497.2002.01155.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Vanjani R, Pitts A, Aurora P. Dismantling structural racism in the academic residency clinic. N Engl J Med. 2022;386:2054–2058. doi: 10.1056/NEJMms2117023 [DOI] [PubMed] [Google Scholar]
- 48. Gaskin DJ, Dinwiddie GY, Chan KS, McCleary R. Residential segregation and disparities in health care services utilization. Med Care Res Rev. 2012;69:158–175. doi: 10.1177/1077558711420263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Armstrong K, McMurphy S, Dean LT, Micco E, Putt M, Halbert CH, Schwartz JS, Sankar P, Pyeritz RE, Bernhardt B, et al. Differences in the patterns of health care system distrust between blacks and whites. J Gen Intern Med. 2008;23:827–833. doi: 10.1007/s11606-008-0561-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Armstrong K, Putt M, Halbert CH, Grande D, Schwartz JS, Liao K, Marcus N, Demeter MB, Shea JA. Prior experiences of racial discrimination and racial differences in health care system distrust. Med Care. 2013;51:144–150. doi: 10.1097/MLR.0b013e31827310a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Grande D, Shea JA, Armstrong K. Perceived community commitment of hospitals: an exploratory analysis of its potential influence on hospital choice and health care system distrust. Inquiry. 2013;50:312–321. doi: 10.1177/0046958013516585 [DOI] [PubMed] [Google Scholar]
- 52. Breslau J, Dana B, Pincus H, Horvitz‐Lennon M, Matthews L. Empirically identified networks of healthcare providers for adults with mental illness. BMC Health Serv Res. 2021;21:777. doi: 10.1186/s12913-021-06798-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Trogdon JG, Weir WH, Shai S, Mucha PJ, Kuo TM, Meyer AM, Stitzenberg KB. Comparing shared patient networks across payers. J Gen Intern Med. 2019;34:2014–2020. doi: 10.1007/s11606-019-04978-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2


