Abstract
Background:
Non-pharmacological treatments, particularly TCM health exercises, have garnered attention for their affordability, ease of access, and potential health advantages. Despite this interest, systematic and direct comparative studies assessing the effectiveness and safety of these therapies in patients with CHD-CHF remain scarce.
Methods:
This study aimed to compare the efficacy and safety of conventional treatment, conventional treatment integrated with aerobic endurance training, and various TCM health exercises in treating patients with CHD-CHF using NMA. The analysis was designed to provide a reference for developing treatment plans. To achieve this, literature databases were searched for RCTs on different TCM health exercises for CHD-CHF patients up to December 6, 2022. Major outcomes analyzed included NT-proBNP, LVEF, 6-minute walk test, MLHFQ, clinical effectiveness, and adverse event occurrence. The Cochrane risk of bias tool was employed to assess the risk of bias in the included RCT studies. Systematic review with NMA was conducted using RevMan 5.4 and Stata for cumulative ranking, and comparative adjustment funnel plot analysis.
Results:
Traditional Chinese medicine gong methods included BaDuanJin (A) and TaiChiQuan (B). The NMA and SUCRA results revealed that: A + D and A + C + D were most likely to be the best interventions to improve NT-proBNP; B + D and A + C + D were most likely to be the best interventions to improve LVEF; A + D and A + C + D were the best interventions to improve 6WMT in CHD-CHF patients; B + C + D had the best effect on shrinking LVESD;A + D and B + C + D was likely the best interventions for contracting LVEDD;B + D and A + D were consistent in their capacity to improve MLHFQ in patients with CHD-CHF, but B + D had better efficacy. Unlike A + C + D, B + C + D was the best intervention to improve MLHFQ. In contrast with interventions, including Dand C + D, B + D was the most clinically effective intervention. Unlike interventions including B + C + D, C + D, and D, A + C + D was the most clinically efficient intervention.
Conclusion:
The findings of this NMA showed that traditional Chinese health exercises integrated with conventional treatment are more effective than conventional treatment (D) alone in patients with CHD-CHF, with A + D, B + D, B + C + D, and A + C + D considered potentially optimal treatment interventions.
Keywords: cardiac function, chronic heart failure, network meta-analysis, quality of survival, traditional health exercises
1. Introduction
Chronic heart failure (CHF) is the final step in the development of various cardiovascular disorders. The disease is characterized by anomalies in the structure or function of the heart, and a decrease in the capacity of the heart to pump blood. As a result, the blood oxygen metabolism of the body becomes disrupted, causing a number of symptoms, including dyspnea, restricted activity, and fluid retention.[1] A latest epidemiological survey reported that 48.3% of chronic heart failure is caused by coronary heart disease (CHD). Moreover, coronary heart disease combined with chronic heart failure (CHD-CHF) is responsible for more than 60 million global deaths annually.[2] In recent years, the prevalence and mortality rates of CHD-CHP have been increasing. Therefore, investigating effective therapies and preventive measures for CHD-CHF patients is a public health issue that should be urgently addressed. The current conventional clinical treatment of CHD-CHF mainly includes western drug therapy, symptomatic supportive therapy, and other interventions, which, however, yield limited therapeutic effects. CHD-CHF has a complex pathogenesis mediated by various specific pathological factors; therefore, these traditional single-treatment methods have multiple clinical limitations and hardly yield desired efficacy. Previous studies indicate that patients with CHD-CHF should avoid physical activity and exercise during the stabilization period to reduce the burden on the heart. With the gradual development and widespread use of modern cardiac rehabilitation theories, increasing clinical evidence confirms that low-intensity exercise can effectively improve the biochemical indices of cardiac function, exercise endurance, and quality of survival in patients with CHD-CHF.[3]
Traditional Chinese healthcare exercises are based on traditional Chinese medicine theory and ancient Chinese simple philosophy. They are designed to maintain coordination of the human body and all internal organs through limb stretching and respiratory adjustment for successful cardiac rehabilitation. Studies have shown that TCM health exercises can significantly lower blood lipids, improve negative emotions including anxiety, stress, or depression, improve quality of life among patients as well as reduce morbidity and mortality.[4] In addition, traditional Chinese health exercises are easy to learn, do not rely on fitness venues or equipment, have moderate intensity, and are relatively safe; thus, they can help improve participation and compliance of CHD-CHF patients to exercise rehabilitation. They are also an important supplement to the modern cardiac rehabilitation system.[5]
Randomized controlled studies of TCM health exercises integrated with conventional treatment of CHD-CHF have been highly reported. Nonetheless, simultaneous comparisons of the efficacy and safety of different TCM health exercises are lacking.[6] Therefore, this study selected common TCM health exercises in clinical settings as study subjects and integrated relevant clinical evidence of direct and indirect comparative relationships using NMA. Further, we performed quantitative and comprehensive statistical analysis of different interventions, ranked the probability based on the superiority of index efficacy, and finally screened the best TCM health exercises.
2. Research methodology
2.1. Registration and reporting of the selected topic
The study was registered with PROSPERO, a prospective systematic evaluation registry created by the National Institute for Health Research Centre for Evaluation and Dissemination in the UK, under the registration number: CRD42022364351. The Preferred Reporting Items for Systematic Evaluation and Meta-Analysis (PRISMA) guidelines were strictly followed.
2.2. Eligibility criteria
This study used PICOS as the eligibility criteria for review, details of which are shown below.
2.2.1. Study design.
Randomized controlled trial of traditional Chinese health exercises integrated with conventional medications in the treatment of patients with coronary heart disease combined with chronic heart failure.
2.2.2. Participants.
All patients included met internationally recognized diagnostic criteria, including the Chinese Heart Failure Diagnosis and Treatment Guidelines 2018, the New York Heart Association (NYHA) Cardiac Function Class II-III, and the Nomenclature and Diagnostic Criteria for Ischemic Heart Disease promulgated by the International Society of Cardiology and the World Health Organization in 1979. Patients were at a stable stage of CHD-CHF without serious underlying diseases and malignancies. There was no restriction on age, gender, race, disease duration, and concomitant symptoms.
2.2.3. Intervention and control.
Control group: Patients only used conventional treatment or conventional treatment combined with aerobic endurance training, among them walking, jogging, brisk walking, and walking (no restriction on the duration of aerobic endurance training). Conventional treatment included symptomatic treatment and medication, including nitrates, aspirin,β-blockers, angiotensin-converting enzyme inhibitors, and other drugs (no restrictions on drug dose, dosing time, and duration of treatment were made).
Intervention group: Patients were treated with conventional therapy combined with traditional Chinese medicine fitness exercises or conventional therapy combined with aerobic endurance training combined with traditional Chinese medicine health care exercises, (traditional Chinese medicine health care exercises: Taijiquan, Five Animal Play, Yi Jin Jing, Baduan Jin).
2.2.4. Outcome indicators.
The included literature had one or more of the following outcome indicators: left ventricular ejection fraction (LVEF); N-terminal brain natriuretic peptidogen (NT-proBNP); left ventricular end-diastolic internal diameter (LVEDD); left ventricular end-systolic internal diameter (LVESD); 6-minute walk test; Minnesota Living with Heart Failure Questionnaire (MLHFQ); Effective rate = (significant patients + effective patients)/total patients X 100%; adverse event occurrence.
2.2.5. Exclusion criteria.
Study type: animal experiments, in vitro cell experiments, and other non-RCT studies; literature type, that is, reading reports, conference papers, famous doctors’ experiences, case reports, reviews, and other literature; incomplete data, that is, inconsistent interventions; unclear study conclusions; literature with incomplete data results.
2.3. Literature data sources and search strategy
We systematically searched Chinese and English databases, including CNKI, WangFang, VIP, PubMed, Embase, The Cochrane Library, and Web of Science by computer. The search was conducted for clinical RCTs related to traditional Chinese medicine health exercises for patients with coronary heart disease combined with chronic heart failure. The search year was from the date of establishment of the databases to November 30, 2022. The search terms comprised free words and subject terms, and the search strategy. “Tai Chi, Yijinjing, Baduanjin, Wuqinxi,” etc. The search was conducted with PubMed as an example, and the detailed search strategy is presented in Table 1.
Table 1.
PubMed search strategy.
| Steps | Strategy |
|---|---|
| #1 | “Coronaryheartdisease”[MeSHTerms] |
| #2 | ((((((((Coronary disease[Title/Abstract])OR(Disease,Coronary[Title/Abstract]))OR(Diseases,Coronary[Title/Abstract]))OR(Coronary Heart Disease[Title/Abstract]))OR(Coronary Heart Diseases[Title/Abstract]))OR(Disease,Coronary Heart[Title/Abstract]))OR(Diseases,Coronary Heart[Title/Abstract]))OR(Heart Disease,Coronary[Title/Abstract]))OR(Heart Diseases,Coronary[Title/Abstract]) |
| #3 | #1OR#2 |
| #4 | “HeartFailure”[MeSHTerms] |
| #5 | ((((((((Cardiac Failure[Title/Abstract])OR(Myocardial Failure[Title/Abstract]))OR(Heart Failure,Left-Sided[Title/Abstract]))OR(Left-Sided Heart Failure[Title/Abstract]))OR(Heart Failure,Right-Sided[Title/Abstract])) OR(Right-Sided Heart Failure[Title/Abstract])) OR(Congestive Heart Failure[Title/Abstract])) OR(Heart Failure,Congestive[Title/Abstract]))OR(Decompensation,Heart[Title/Abstract]) |
| #6 | #4OR#5 |
| #7 | “Tai-ji”[MeSHTerms] |
| #8 | ((((((((Tai Chi[Title/Abstract])OR(Chi,Tai[Title/Abstract]))OR(Tai Ji Quan[Title/Abstract]))OR(Ji Quan,Tai[Title/Abstract])) OR(Quan, Tai Ji[Title/Abstract]))OR(Tai ji[Title/Abstract])) OR(Tai ji quan[Title/Abstract]))OR(T’ai Chi[Title/Abstract])) OR(Tai Chi Chuan[Title/Abstract]) |
| #9 | #7OR#8 |
| #10 | “Baduanjin”[MeSHTerms] |
| #11 | “Wuqinxi”[MeSHTerms] |
| #12 | “Yijinjing”[MeSHTerms] |
| #13 | “Five-animalplay”[MeSHTerms] |
| #14 | “TraditionalChineseMedicineMovemen”[MeSHTerms] |
| #15 | “ChineseMedicineExercise”[MeSHTerms] |
| #16 | #9OR#10OR#11OR#12OR#13OR#14OR#15 |
| #17 | “RandomizedControlledTrial”[PublicationType] |
| #18 | (((controlled clinical trial[Title/Abstract])OR(randomized[Title/Abstract]))OR(placebo[Title/Abstract]))OR(RCT[Title/Abstract]) |
| #19 | #17OR#18 |
| #20 | #3AND#6AND#9AND#16AND#19 |
2.4. Literature screening and data extraction
Two systematically trained researchers (PSW and LYJ) independently read the title, abstract and full text of the literature screened the literature based on the established inclusion and exclusion criteria and created an excel sheet to extract the following contents: basic information on the first author, year of publication, title, and journal of the included literature; subjects in the intervention and control groups of the included literature gender, age, intervention, duration of treatment, outcome indicators and other relevant information; study design and quality evaluation information of the included literature; outcome indicators, including cardiac function indicators, exercise tolerance, Minnesota Quality of Survival Scale for Heart Failure, efficiency, adverse effects.
2.5. Literature quality evaluation
Two systematically trained researchers (QJ and ZYL) independently performed risk evaluation of literature bias using the assessment tools recommended by the Cochrane Centre for Evidence; they evaluated the following: randomization scheme; implementation of allocation concealment scheme; implementation of blinding; completeness of outcome data; selective reporting bias; other sources of bias. Disagreements, if any, were further discussed or evaluated by a third investigator.
2.6. Statistical analysis
Conventional Meta-analysis was performed by “RevMan 5.4.” The ratio (OR), and 95% confidence interval (CI) were selected as effect indicators when the outcome indicators were dichotomous variables. When the outcome indicator was a continuous variable with consistent units, the weighted mean difference (WMD) and 95% confidence interval (CI) were selected as the effect indicators. Meta-analysis was performed using a fixed-effects model when I2 was < 50%, and a random-effects model if I2 was ≥ 50%. A single node in the graph represented an independent intervention, the node size represented the sample size of the intervention, and the lines connecting the different nodes represented the number of studies included in the intervention. If there is a closed loop in the mesh relationship graph, its inconsistency is judged by the inconsistency factor; if the lower limit of 95% CI of the inconsistency factor value is 0 or close to 0, it means that the direct evidence is consistent with the indirect evidence. Eventually, the area under the curve of the cumulative probability plot was compared to obtain a ranking among the interventions, and a larger value of SUCRA indicated a more effective intervention. Additionally, comparison-corrected funnel plots were developed using the “Stata14” software to identify the presence of small sample effects and publication bias between studies.
3. Results
3.1. Literature screening results and basic characteristics
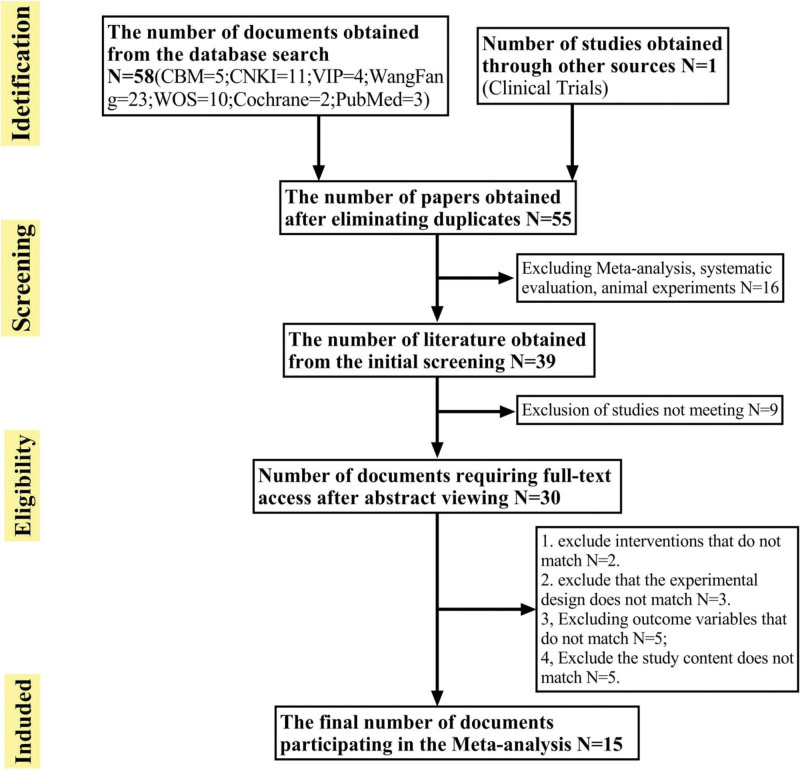
A total of 58 papers were initially obtained; 2 researchers screened these papers based on the inclusion and exclusion criteria out of which 15[7–21] RCT studies were finally included. The details of the literature screening are shown in Figure 1. The 15 RCT studies were all in Chinese, involving 1352 patients, and all patients were randomly divided into intervention and control groups; In the intervention group, 2 different interventions were used: Traditional Chinese Medicine health exercises (Taijiquan, FiveAnimalPlay, BaDuanJin, YiJinJing) single treatment combined with conventional treatment; Traditional Chinese Medicine fitness exercises combined with aerobic endurance training (walking, jogging, walking, brisk walking) single treatment combined with Traditional Chinese Medicine health exercises combined with conventional treatment. The control group used 2 different interventions: aerobic endurance training monotherapy combined with conventional treatment; conventional treatment. The basic characteristics of the included studies are shown in Tables 2 and 3.
Figure 1.
Flowchart.
Table 2.
Basic characteristics of the included literature.
| NO | Author | Year | Male | Female | Age | Disease duration | Cardiac function classification | Walking distance of 6MWT | Interventions | course of treatment | Outcome | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T | C | |||||||||||||||||||
| T | C | T | C | T | C | T | C | II | III | II | III | T | C | T | C | |||||
| 1 | Jiang QH | 2022 | 47 | 44 | 33 | 36 | 67.78 ± 4.10 | 67.23 ± 4.34 | 7.37 ± 3.16 | 7.55 ± 3.22 | 49 | 31 | 52 | 28 | 249.54 ± 34.32 | 250.18 ± 30.56 | O + B + A | O + B | 24W | ①②③ |
| 2 | Gu X | 2022 | 20 | 19 | 14 | 15 | 67.00 ± 8.55 | 67.00 ± 8.50 | 6.38 ± 2.30 | 7.1 ± 4.12 | 19 | 15 | 18 | 16 | 258.91 ± 18.35 | 263.38 ± 16.38 | O + B + S | O + B | 24W | ①②④ |
| 3 | Zhou YX | 2021 | 27 | 23 | 31 | 19 | 57.87 ± 4.61 | 58.41 ± 4.52 | 6.21 ± 1.24 | 5.67 ± 1.74 | 10 | 11 | 9 | 5 | 360.85 ± 21.64 | 354.52 ± 20.7 | O + A | O + C | 12W | ①②③ |
| 4 | Kang ZL | 2021 | 21 | 17 | 23 | 15 | 68.36 ± 5.03 | 69.25 ± 5.33 | 7.12 ± 1.23 | 4.78 ± 2.1 | 21 | 17 | 19 | 19 | 258.98 ± 18.33 | 263.36 ± 16.36 | O + B + A | O + B | 24W | ①②⑤ |
| 5 | Hong XJ | 2020 | 23 | 25 | 10 | 60 | 60.70 ± 7.82 | 60.24 ± 7.26 | 2.32 ± 1.30 | 2.21 ± 1.30 | 29 | 4 | 31 | 3 | 397.88 ± 24.55 | 398.76 ± 26.01 | O + A | O + C | 8W | ①②③ |
| 6 | Chen XP | 2020 | 25 | 21 | 24 | 22 | 68.45 ± 3.89 | 69.23 ± 2.34 | 3.43 ± 1.06 | 3.52 ± .2.1 | 12 | 8 | 12 | 9 | 127.57 ± 27.86 | 129.94 ± 0.48 | O + A | O + C | 2W | ①② |
| 7 | Tang HM | 2020 | 23 | 7 | 22 | 8 | 63.10 ± 8.44 | 64.37 ± 6.00 | 4.32 ± 2.34 | 4.12 ± 2.4 | 14 | 16 | 13 | 17 | 297.39 ± 5.377 | 298.29 ± 5.760 | O + A | O + C | 12W | ①②③ |
| 8 | Deng XF | 2020 | 28 | 31 | 20 | 21 | 66.8 ± 3.04 | 66.6 ± 2.42 | 5.45 ± 2.13 | 3.12 ± 4.3 | 12 | 6 | 12 | 12 | 307.49 ± 25.77 | 302.24 ± 24.01 | O + A | O + C | 24W | ①②③ |
| 9 | YU ML | 2018 | 50 | 47 | 10 | 13 | 60.33 ± 8.78 | 60.68 ± 9.7 | 2.72 ± 3.14 | 2.21 ± 3.14 | 54 | 6 | 55 | 5 | 396.61 ± 23.35 | 392.18 ± 41.55 | O + A | O + C | 24W | ①②③⑥⑦⑧ |
| 10 | Shi ZB | 2018 | 12 | 14 | 17 | 12 | 58.60 ± 4.17 | 58.20 ± 4.42 | 4.02 ± 1.56 | 3.78 ± 1.46 | 49 | 31 | 52 | 28 | 434 ± 23.12 | 556 ± 34.89 | O + A | O + C | 4W | ①③⑥ |
| 11 | Liu HJ | 2017 | 15 | 18 | 16 | 17 | 55.21 ± 1.32 | 54.76 ± 1.31 | 6.19 ± 0.34 | 5.72 ± 0.34 | 19 | 15 | 18 | 16 | 192.71 ± 6.80 | 195.32 ± 23.13 | O + D | O + C | 12W | ①②③⑨ |
| 12 | Xiong XH | 2016 | 20 | 13 | 18 | 12 | 70.3 ± 6.4 | 69.7 ± 7.2 | 6.34 ± 2.12 | 4.6 ± 1.23 | 13 | 12 | 16 | 8 | 316.8 ± 42.3 | 312.1 ± 45.6 | O + A | O + C | 8W | ①②③ |
| 13 | Sang L | 2015 | 28 | 22 | 29 | 21 | 65.3 ± 8.2 | 76.2 ± 7.5 | 2.23 ± 2.13 | 6.78 ± 2.3 | 13 | 8 | 12 | 9 | 312.2 ± 130. 1 | 439. 7 ± 80. 21 | O + D | O + C | 24W | ①②③ |
| 14 | Huang C | 2014 | 21 | 23 | 23 | 21 | 61.59 ± 7.06 | 64.27 ± 6.46 | 9.91 ± 5.97 | 11.6 ± 5.68 | 5 | 7 | 8 | 7 | 348.34 ± 41.15 | 348.34 ± 35.11 | O + D | O + C | 3W | ①②③⑩ |
| 15 | Pang W | 2019 | 22 | 20 | 23 | 19 | 68.28 ± 8.36 | 68.59 ± 8.14 | 3.62 ± 1.19 | 3.50 ± 1.23 | 8 | 4 | 7 | 5 | 347.23 ± 23.2 | 334.6 ± 34.15 | O + D | O + C | 8W | ①② |
6MWT = 6-minute walk test.
A: Baduanjin; B = aerobic exercise; C = no intervention; D = taijiquan; O = conventional drug therapy.
① cardiac function; ② 6min walk test; ③ quality of survival; ④ compliance; ⑤ mood to quality of survival score ratio; ⑥ pulmonary function; ⑦ Chinese medicine main symptoms score; ⑧ ultrasensitive C-reactive protein; ⑨ Lee heart failure score efficacy; ⑩ cardiac ultrasound.
Table 3.
Results of the mesh Meta-analysis between interventions (WMD [95% CI]).
| Interventions | NT-proBNP | LVEF | LVEDD | LVESD | LVESD | MLHFQ | 6WMT | Effective | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Interventions1 | Interventions2 | Effect size | 95%CI | Effect size | 95%CI | Effect size | 95%CI | Effect size | 95%CI | Effect size | 95%CI | Effect size | 95%CI | Effect size | 95%CI | Effect size | 95%CI |
| C + D | A + C + D | −74.97 | −142.08, −7.86 | 22.1 | 10.46, 46.71 | 0.24 | 1.88, 4.31 | 2.21 | −0.36, 4.78 | 22.7 | 16.94, 28.47 | −1.1 | −9.13, 6.93 | 22.71 | 16.94, 28.47 | 18.54 | 32.47.4.61 |
| B + C + D | 17 | −126.93, 126.57 | 5.75 | 0.00, 516.25 | 5.75 | −2.34, 5.84 | - | - | 0.55 | −13.06, 14.16 | 3.32 | −8.88, 15.52 | 0.55 | −13.06, 14.16 | 19.09 | 13.90, 23.12 | |
| D | 15.98 | −109.38, 141.34 | 0.24 | 0.02, 2.62 | 0.1 | −2.44, 5.26 | - | - | −18.53 | −32.47, −4.61 | −2.47 | −11.02, 6.08 | −18.54 | −32.47, −4.61 | 0.45 | 12.65, 23.32 | |
| D | A + D | 90.95 | −51.24, 233.15 | 4.1 | 0.06, 266.59 | - | - | - | - | −26.39 | −80.40, 27.61 | −5.25 | 8.63, −1.86 | 45.49 | 23.59, 67.39 | 12.34 | 34.27, 12.45 |
| B + D | 16.16 | −162.11, 194.43 | 2692.8 | 28.34, 255.86 | - | - | 3.47 | −4.05, 11.00 | −18.55 | −77.02, 39.92 | −7.44 | −13.07, −1.80 | 87.64 | 6.31, 68.97 | 10.10 | 23.29.45.0 | |
| A + C + D | B + C + D | 74.795 | −68.63, 218.21 | 0.26 | 0.02, 3.60 | 2.4 | 0.20, 28.59 | - | - | −22.15 | −36.94, −7.37 | 4.42 | −13.55, 22.39 | −22.16 | −36.94, −7.37 | 12.23 | 22.23, 29.01 |
LVEDD = left ventricular end-diastolic internal diameter, LVESD = left ventricular end-systolic internal diameter, LVEF = left ventricular ejection fraction, MLHFQ = Minnesota Living with Heart Failure Questionnaire, NT-proBNP = N-terminal brain natriuretic peptidogen.
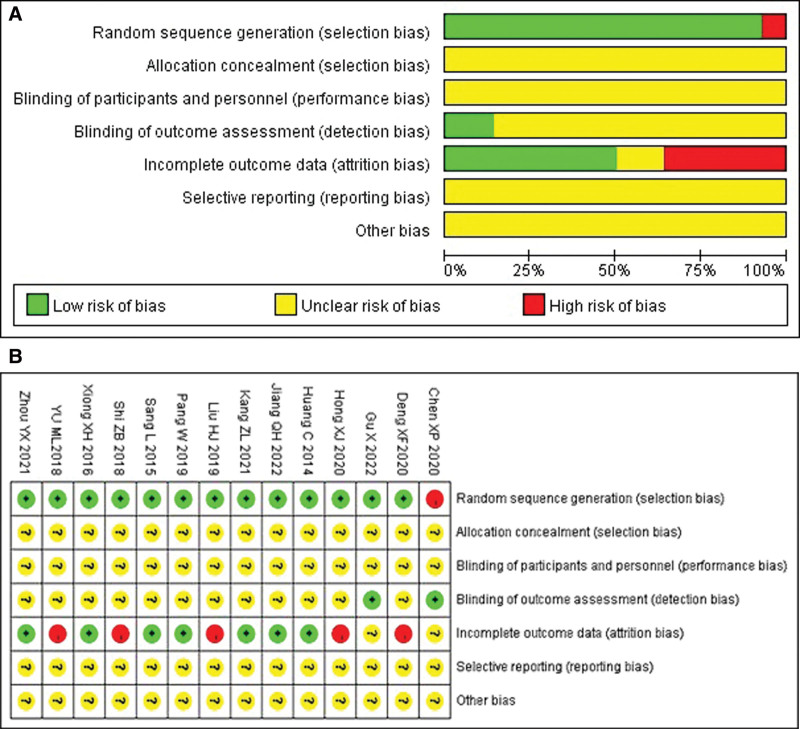
3.2. Evaluation of the quality of included studies
The 15 included RCT studies were assessed for risk of bias; all 15[7–21] studies were RCTs; 14 described specific randomization methods; none of the 15 provided information on whether allocation concealment and blinding were used; 6 of the 15 studies had dislodged subjects. Therefore, data from 6 studies were incomplete; due to insufficient evidence of selective reporting and other biases in the included literature. This was because the original study protocols were not available due to the omission of registration information in the studies. Overall, the risk of bias in the included literature was high as revealed by the literature risk assessment evidence map. The evaluation of the quality of included studies are shown in Figure 2.
Figure 2.
(A) Bias Risk Bar Chart. Figure 2B. Bias risk map.
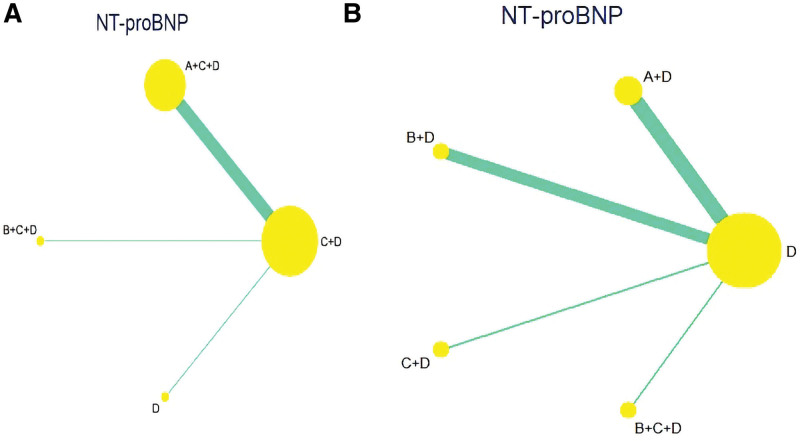
3.3. Effect of Traditional Chinese Medicine Health Exercises on NT-proBNP Intervention in patients with CHD-CHF
A total of 11[7,8,10,12–15,17,18,20,21] RCT studies reported changes in NT-proBNP in patients with CHD-CHF before and after treatment, including 4 different interventions, 2 different traditional Chinese health exercises, and 2 control measures involving 1006 patients. A reticulated meta-analysis was performed on the included data, and no inconsistency test was required since no closed loop was formed between the interventions. Figure 3 and Tables 2–3 show the reticulated relationships and effect sizes between the interventions.
Figure 3.
(A) NT proBNP network evidence graph. Figure 3B. NT proBNP network evidence graph.
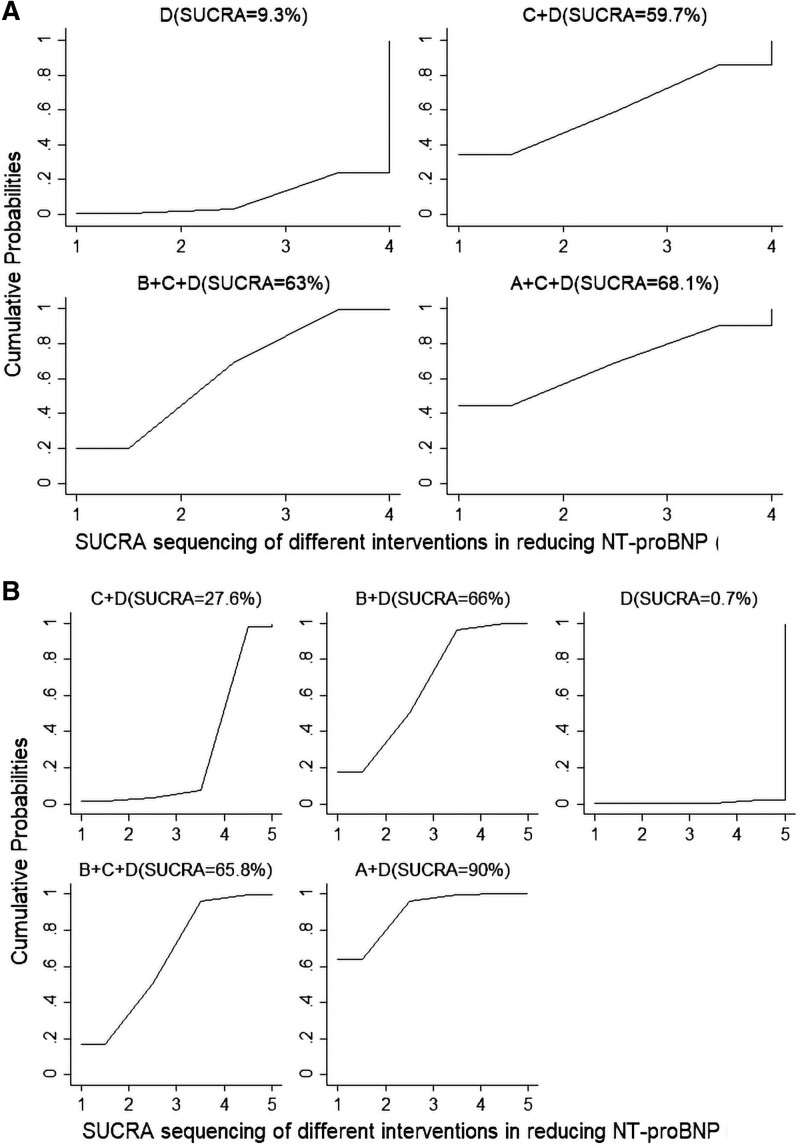
In contrast with D, A + D (WMD = 90.95, 95% CI [−51.24, 233.15], P = .392). B + D (WMD = 16.16, 95% CI [−162.11, 194.43], P < .05). C + D (WMD = −15.98, 95% CI [−162.11, 194.43], P < .05). SUCRA was used to rank the 4 interventions that modulate NT-proBNP and the 2 controls: A + D (SUCRA = 90%) > B + D (SUCRA = 66%) > B + C + D (SUCRA = 65.8%) > C + D (SUCRA = 27.6%) > D (SUCRA = 0.7%). The results shown in Figure 4A indicate the SUCRA ranking of NT-proBNP efficiency of different TCM traditional health exercises on improving CHD-CHF:A + D showed the best improvement on NT-proBNP.
Figure 4.
(A) SUCRA sequencing of NT-proBNP (A). Figure 4B. SUCRA sequencing of NT-proBNP (B).
Unlike C + D, A + C + D (WMD = 74.97, 95% CI [−142.08, −7.86], P = .029), B + C + D (WMD = 17, 95% CI [−126.93, 126.57], P = .998), and D (WMD = 15.98, 95% CI [−109.38, 141.34], P = .803). The ability of A + C + D and B + C + D to improve NT-proBNP in CHD-CHF patients was significantly better than that of C + D, and the difference was statistically significant. An indirect comparison of 2 traditional Chinese medicine health exercises revealed that Ba Duan Jin was superior to Taijiquan (WMD = 74.80, 95% CI [−68.63, 218.21], P < .05), whereas differences between other intercomparisons were not statistically significant. SUCRA was used to rank the 4 interventions for modulating NT-proBNP as well as the 2 controls: A + C + D (SUCRA = 68.1%) > B + C + D (SUCRA = 63%) > C + D (SUCRA = 59.7%) > D (SUCRA = 9.3%) SUCRA ranking plots showed in Figure 4B. A + C + D was most likely the best intervention for improving NT-proBNP.
3.4. Efficacy of Traditional Chinese Medicine Health Exercise Interventions on LVEF in patients with CHD-CHF
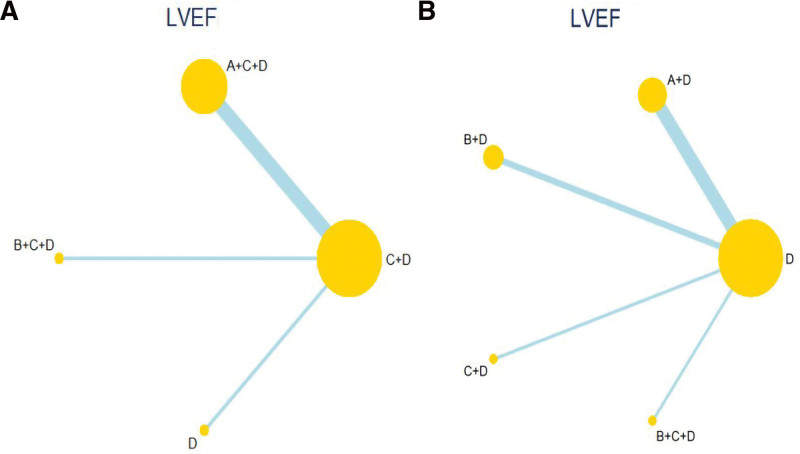
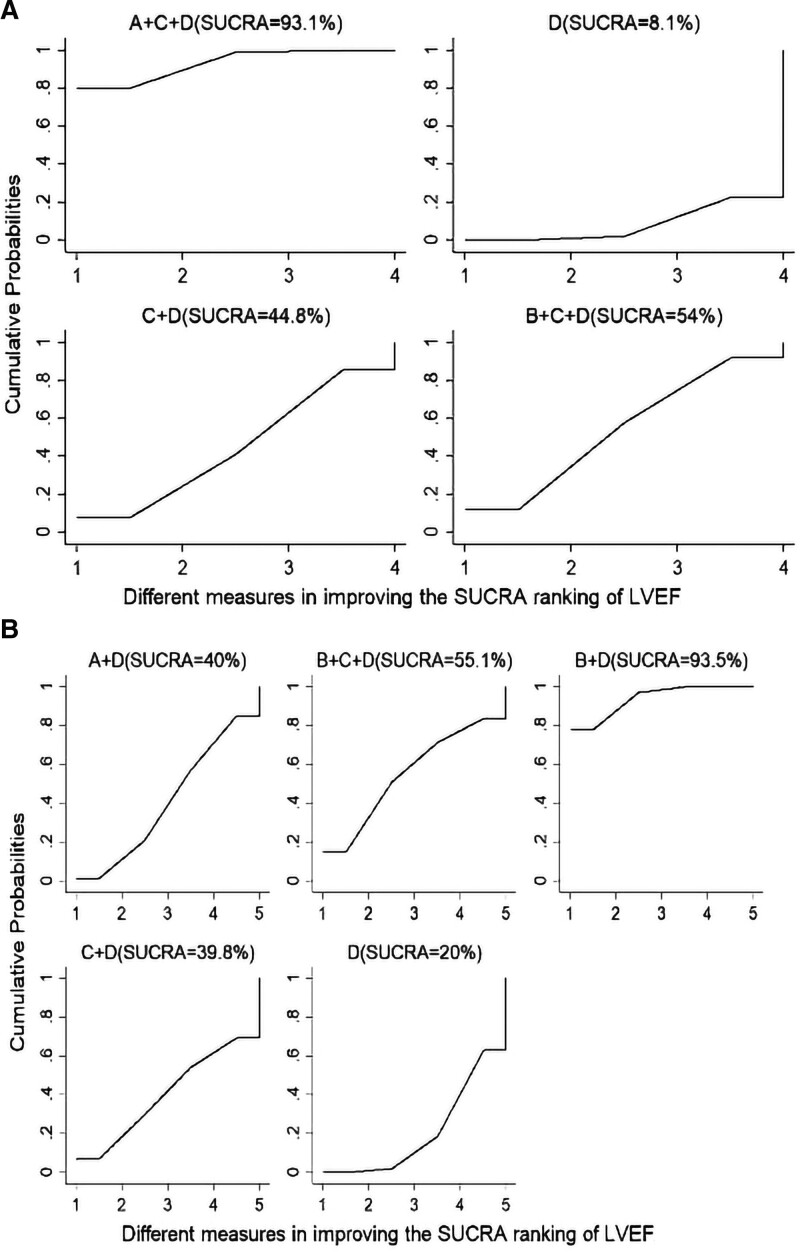
A total of 12[7–10,12,13,15–18,20,21] RCT studies reported changes in LVEF in patients with CHD-CHF before and after treatment, including 4 different interventions, 2 different traditional Chinese health exercises, and 2 control measures involving 1027 patients. NMA was performed on the included data, and no inconsistency test was required since no closed loop was formed between the interventions. The reticulated relationships and effect sizes between interventions are presented in Figure 5 and Table 3.
Figure 5.
(A) LVEF Network Evidence Diagram (A). Figure 5B. LVEF Network Evidence Diagram (B). LVEF = left ventricular ejection fraction.
In comparison with D, A + D (WMD = 2.91, 95% CI [−4.06, 6.88], P = .54). B + D (WMD = 7.90, 95% CI [1.93, 13.87], P = .019). C + D (WMD = 1.41, 95% CI [−9.15, 11.97], P = .745). B + C + D (WMD = 3.16, 95% CI [−7.44, 13.75], P = .478). SUCRA was used to rank the 4 interventions that modulate NT-proBNP and the 2 controls: B + D (SUCRA = 93.5%) > B + C + D (SUCRA = 55.1%) > A + D (SUCRA = 40%) > C + D (SUCRA = 39.8%) > D (SUCRA = 20%). SUCRA ranking plots are shown in Figure 6A. B + D was most likely the best intervention to improve LVEF.
Figure 6.
(A) The SUCRA of LVEF (A). Figure 6B. The SUCRA of LVEF (B). LVEF = left ventricular ejection fraction.
Unlike C + D (WMD = 22.10, 95%CI [10.46, 46.71], P < .05), A + C + D (WMD = 5.75, %CI [0.46, 71.35], P < .05), D (WMD = 0.24, 95% CI [0.02, 2.62], P < .05), A + C + D and B + C + D were significantly better than D and C + D in improving LVEF in patients with CHD-CHF, with statistically significant differences. Indirect comparison of the 2 traditional Chinese health exercises revealed superior Taijiquan to Baduanjin (WMD = 0.26, 95% CI [0.02, 3.60], P < .05), but differences between other intercomparisons were not statistically significant. SUCRA was used to rank the 4 interventions for improving LVEF and the 2 controls: A + C + D (SUCRA = 93.1%) > B + C + D (SUCRA = 54%) > C + D (SUCRA = 44.8%) > D (SUCRA = 8.1%). The SUCRA ranking plot is shown in Figure 6B. A + C + D was most likely the LVEF with the best intervention.
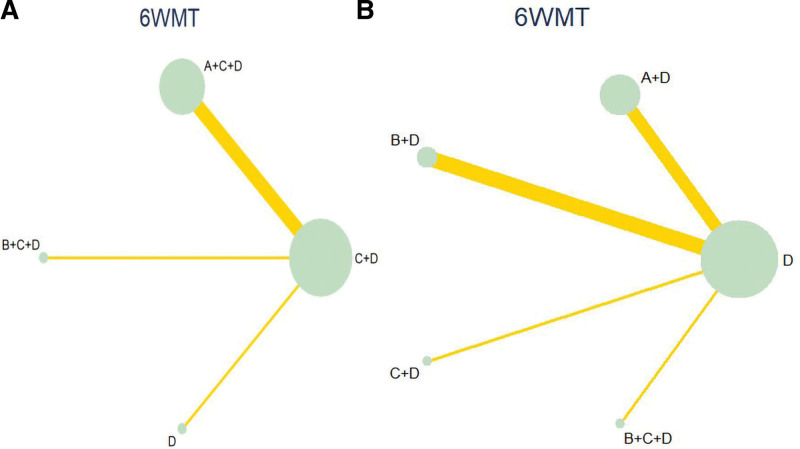
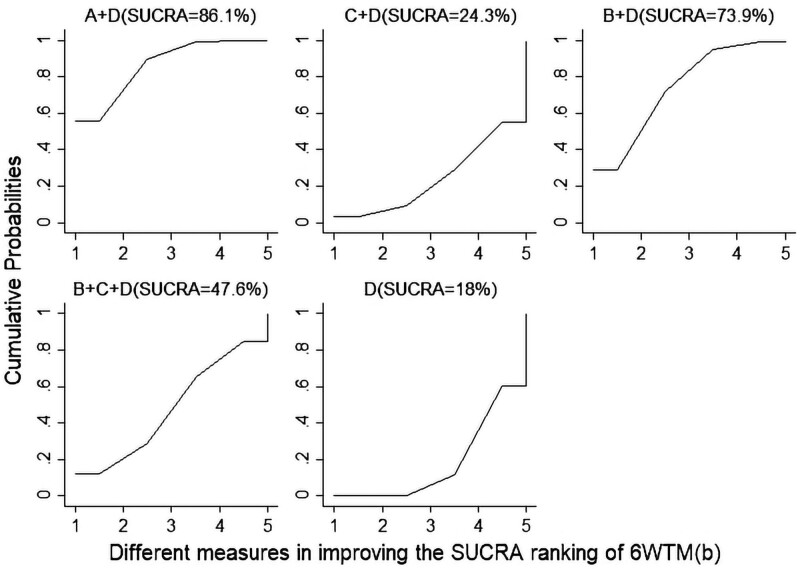
3.5. Effect of Traditional Chinese Medicine Health Exercises on 6WTM in CHD-CHF patients
Further,10[7,8,11,13,15,17–21] RCT studies reporting changes in LVESD in patients with CHD-HF before and after treatment were subjected to conventional Meta-analysis, including 4 different interventions, 2 different traditional Chinese health exercises, and 2 control measures involving 525 patients. A reticulated Meta-analysis was performed on the included data, and no inconsistency test was necessitated since no closed loop was formed between the interventions. The reticulated relationships and effect sizes between the interventions are shown in Figure 7 and Table 3.
Figure 7.
(A) 6WMT network evidence graph (A). Figure 7B. 6WMT network evidence graph (B).
In contrast with D, A + D (WMD = 45.49, 95% CI [23.60, 67.39], P = .000). B + D (WMD = 37.64, 95% CI [6.31, 68.97], P = .019). C + D (WMD = 19.09, 95% CI [−2.10, −1.12], P < .05). B + C + D (WMD = 19.09, 95% CI [−30.28, 68.46], P = .449). SUCRA was used to rank the 4 interventions for improving 6WMT and the 2 controls: A + D (SUCRA = 86.1%) > B + D (SUCRA = 73.9%) > B + C + D (SUCRA = 47.6%) > C + D (SUCRA = 24.3%) > D (SUCRA = 18%). A + D was most likely to be the best intervention for improving the 6WMT measure.
Unlike C + D, A + C + D (WMD = 22.7, 95% CI [16.94, 28.47], P = .000), B + C + D (WMD = 0.55, 95% CI [−13.06, 14.16], P = .937), D (WMD = −18.53, 95% CI [−32.47, −4.61], P = .000). An indirect comparison of the 2 traditional Chinese health exercises revealed that Badaanjin was superior to Taijiquan (WMD = 4.26, 95% CI [0.02, 3.60], P < .05), whereas differences between other intercomparisons were not statistically significant. SUCRA was used to rank the 4 interventions for improving LVEF as well as the 2 controls: A + C + D (SUCRA = 93.1%) > B + C + D (SUCRA = 54%) > C + D (SUCRA = 44.8%) > D (SUCRA = 8.1%). The SUCRA ranking plot is shown in Figure 8B. A + C + D was most likely the best intervention for improving 6 WMT with the best intervention.
Figure 8.
The SUCRA ranking of 6WTM.
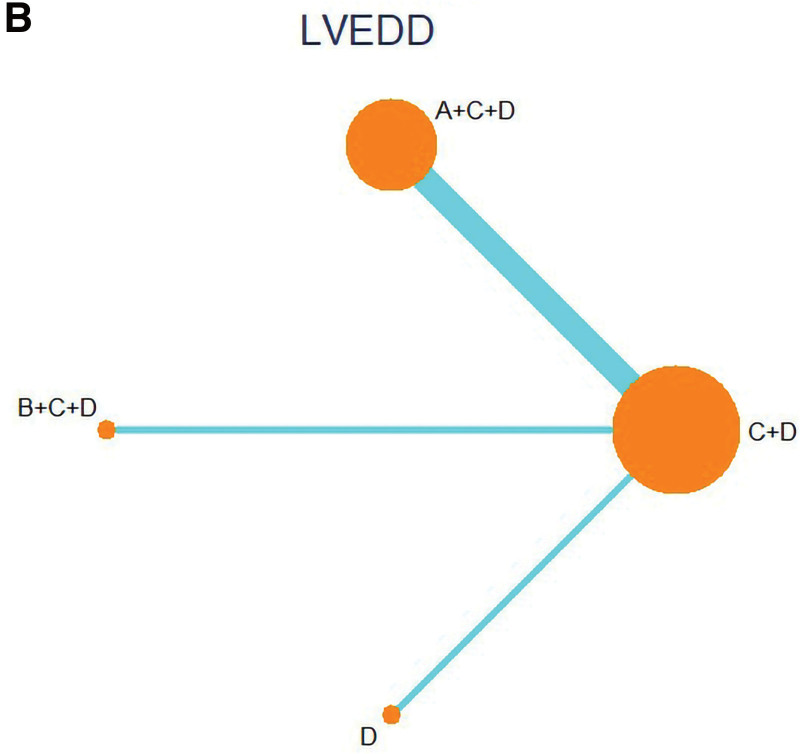
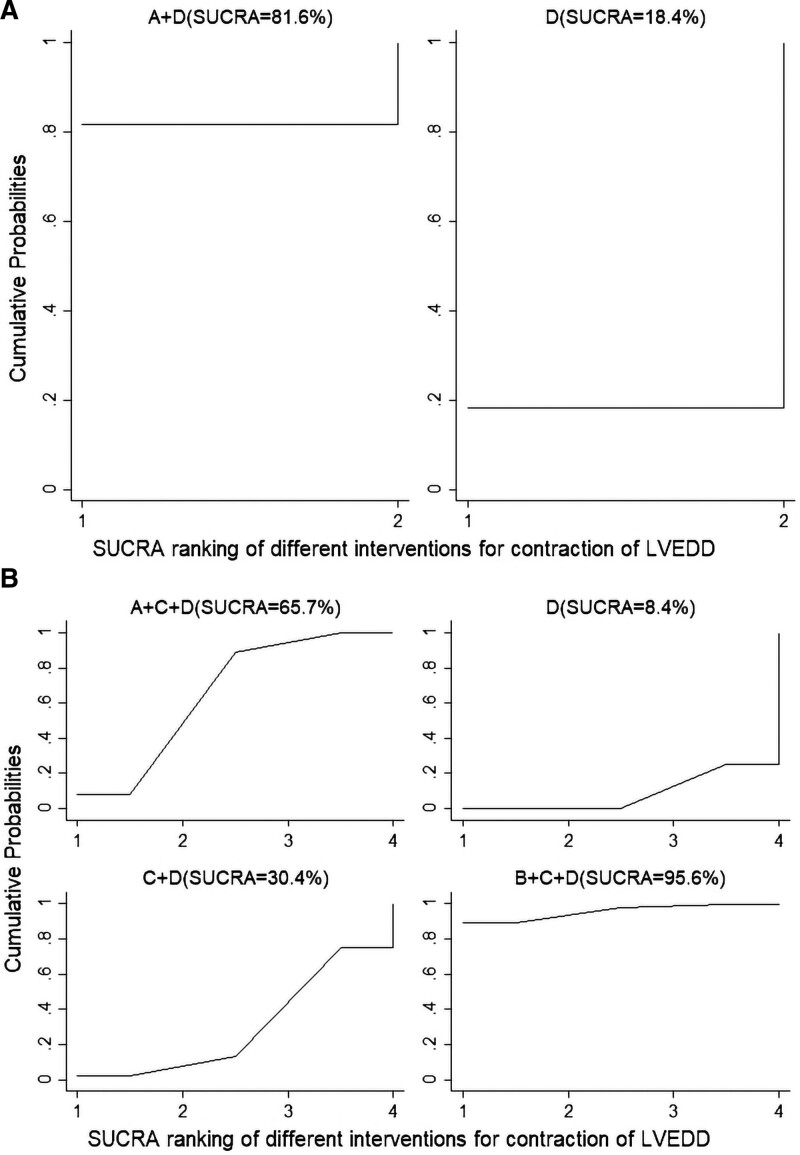
3.6. Effect of Traditional Chinese Medicine Health Exercises on LVEDD in patients with CHD-CHF
Seven[7,9,11,13,14,16,17] RCT studies reporting changes in LVESD in patients with CHD-HF before and after treatment were subjected to traditional Meta-analysis, including 4 different interventions, 2 different traditional Chinese health exercises, and 2 control measures involving 525 patients. NWA was performed on the included data, and no inconsistency test was required since no closed loop was formed between the interventions. The reticulated relationships and effect sizes between interventions are shown in Figure 9 with Table 3.
Figure 9.
LVEDD network evidence diagram (B). LVEDD = left ventricular end-diastolic internal diameter.
In comparison with D, A + D (WMD = 45.49, 95% CI [23.60, 67.39], P = .000). b + c + d (WMD = 37.64, 95% CI [6.31, 68.97], P = .019). c + d (WMD = 19.09, 95% CI [−2.10, −1.12], P < .05). B + C + D (WMD = 19.09, 95% CI [−30.28, 68.46], P = .449). SUCRA was used to rank 4 interventions for improving 6WMT and the 2 controls: A + D (SUCRA = 81.6%) > D (SUCRA = 18.4%). The SUCRA ranking plot is shown in Figure 10A. A + D was most likely the best intervention for shrinking LVEDD.
Figure 10.
(A) The SUCRA ranking of LVEDD (A). Figure10B. The SUCRA ranking of LVEDD (B). LVEDD = left ventricular end-diastolic internal diameter.
Unlike C + D (WMD = 0.24, 95%CI [1.88, 4.31], P < .05), B + C + D (WMD = 5.75, %CI [−2.34, 5.84], P < .05), D (WMD = 0.1, 95% CI [−2.44, 5.26], P < .05), A + C + D Indirect comparison of the 2 traditional Chinese health exercises revealed superior Taijiquan to Baduanjin (WMD = 2.4, 95% CI [0.20, 28.59], P < .05), whereas differences between the other intercomparisons were not statistically significant. SUCRA was used to rank the 4 interventions for improving LVEF and the 2 controls: B + C + D (SUCRA = 95.6%) > A + C + D (SUCRA = 65.7%) > C + D (SUCRA = 30.4%) > D (SUCRA = 8.4%). The SUCRA ranking plot is shown in Figure 10B. B + C + D was most likely the shrinkage the best intervention for LVEDD.
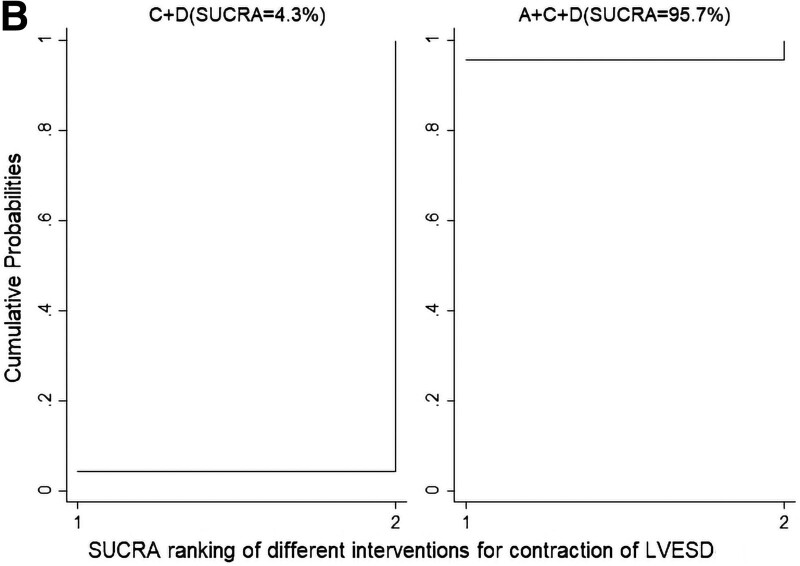
3.7. Effect of Traditional Chinese Medicine Health Exercises on LVESD in patients with CHD-CHF
Five[7–11]RCT studies reporting changes in LVESD in patients with CHD-HF before and after treatment were subjected to traditional Meta-analysis, including 2 different interventions, 2 different TCM traditional health exercises, and one control measure, involving 536 patients. NMA was performed on the included data, and a descriptive analysis was conducted considering that the number of included studies was small and further combined analysis was not more meaningful.
Unlike D, A + D (WMD = 3.47, 95% CI [−4.05, 11.00], P = .37), A + D significantly shrank LVESD in patients with CHD-HP compared with D. In contrast with C + D, A + C + D (WMD = −2.21, 95% CI [−0.36, 4.78], P = .092). A + C + D significantly shrank LVESD in patients with CHD-HP compared with C + D shrinking LVESD in patients with CHD-HP. The 2 interventions for improving LVEF and 1 control group were ranked using SUCRA: A + C + D (SUCRA = 95.7%) > C + D (SUCRA = 4.3%), and the SUCRA ranking plot showed that A + C + D was most likely the best intervention to shrink LVESD (Fig. 11).
Figure 11.
The SUCRA ranking of LVEDD (A). LVEDD = left ventricular end-diastolic internal diameter.
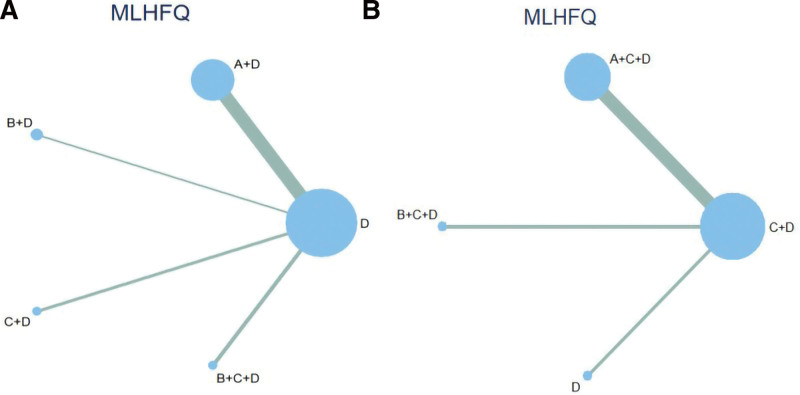
3.8. Effect of Traditional Chinese Medicine Health Exercises on MLHFQ in patients with CHD-CHF
Thirteen[7–12,14–16,18–21] RCT studies reporting changes in MLHFQ in patients with CHD-CHF before and after treatment were netted for Meta-analysis, including 4 different interventions, 2 different traditional Chinese health exercises, and 2 control measures involving 525 patients. NMA was performed on the included data, and an inconsistency test was unnecessary since no closed loop was formed between the interventions. Figure 12 with Table 3 presents the mesh relationships between the interventions with effect sizes.
Figure 12.
(A) MLHFQ Network Evidence Graph (A). Figure 12B. MLHFQ Network Evidence Graph (B). MLHFQ = Minnesota Living with Heart Failure Questionnaire.
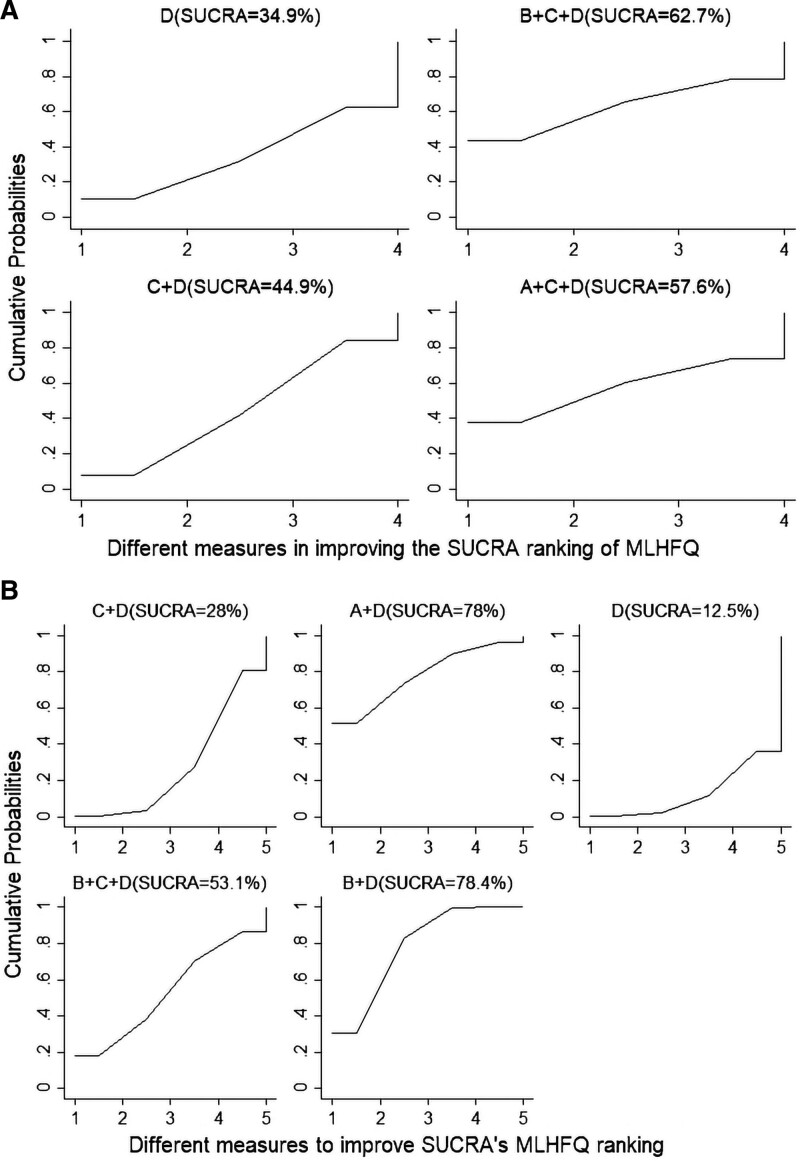
In contrast with D, A + D (WMD = −5.25, 95% CI [−8.63, −1.86], P = .002). B + D (WMD = −7.43, 95% CI [−13.07, −1.80], P = .010). C + D (WMD = −2.47, 95% CI [−2.10, −1.12], P = .57). B + C + D (WMD = 0.84, 95% CI [−7.85, 9.55], P = .848). SUCRA was used to rank the 4 interventions to improve MLHFQ and the 2 controls: B + D (SUCRA = 78.4%) > A + D (SUCRA = 78%) > B + C + D (SUCRA = 53.1%) > C + D (SUCRA = 28%) > D (SUCRA = 12.5%); SUCRA ranking plots are shown in Figure 13B. B + D and A + D are most likely the best interventions to improve MLHFQ.
Figure 13.
(A) The SUCRA ranking of MLHFQ (A). Figure13B. The SUCRA ranking of MLHFQ (B). MLHFQ = Minnesota Living with Heart Failure Questionnaire.
Unlike C + D, A + C + D (WMD = −1.1, 95% CI [−9.13, 6.93], P < .05), B + C + D (WMD = 3.32, 95% CI [−8.88, 15.52], P < .05), D (WMD = −2.47, 95% CI [−11.02, 6.08], P < .05), compared to C + D, A + C + D and B + C + D were significantly better than D and C + D in improving LVEF in patients with CHD-HF, with a statistically significant difference. An indirect comparison of the 2 traditional Chinese health exercises revealed that taijiquan was superior to Baduanjin (WMD = 4.42, 95% CI [−13.55, 22.39], P < .05), and the differences between the other intercomparisons were not statistically significant. SUCRA was used to rank the 4 interventions to improve MLHFQ in patients and the 2 control groups: B + C + D (SUCRA = 62.7%) > A + C + D (SUCRA = 57.6%) > C + D (SUCRA = 44.9%) > D (SUCRA = 34.9%), and the SUCRA ranking plot showed in Figure 13A. B + C + D was most likely the best intervention to improve MLHFQ.
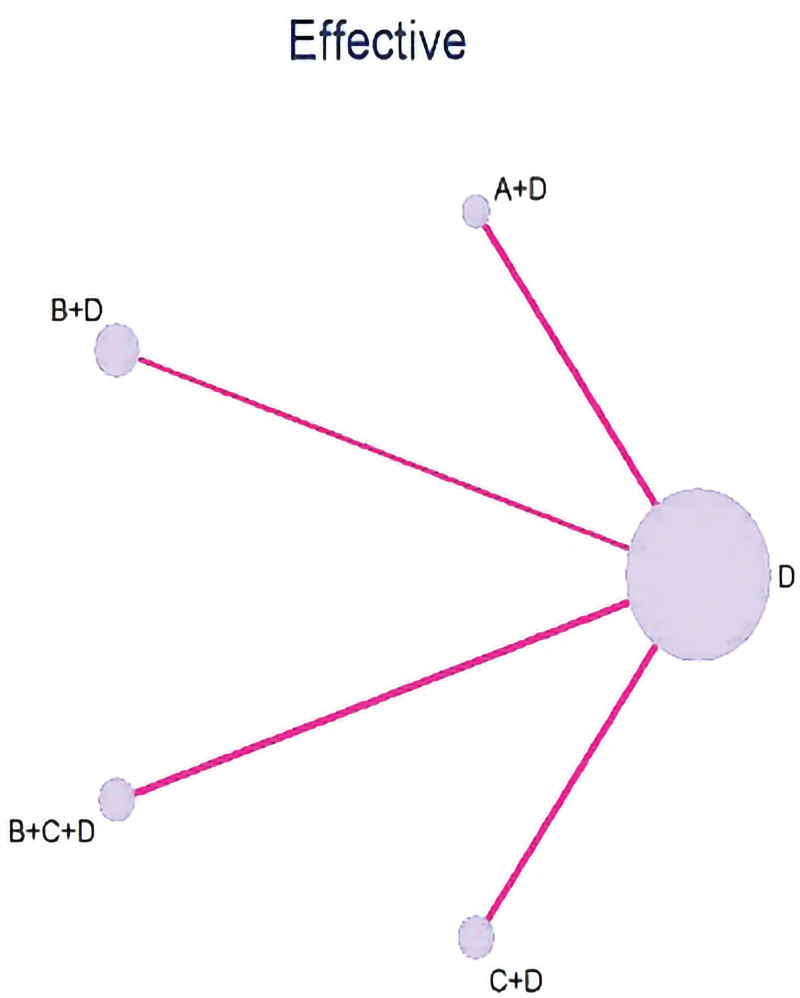
3.9. Efficacy of traditional Chinese health exercises in patients with CHD-CHF
Four[7,15,19,20] RCT studies that reported changes in efficiency rates in patients with CHD-HF before and after treatment included 4 different interventions, 2 different traditional Chinese health exercises, and 2 control measures involving 350 patients. The reticulated relationships between the interventions with effect sizes are shown in Figure 14 with Table 3.
Figure 14.
Effective Network Evidence Graph.
In contrast with D, A + D (OR = 4.84, 95% CI [−8.59, −4.10], P = .02). B + D (OR = 1.56, 95% CI [−5.08, −5.40], P = .01). C + D (OR = 0.21, 95% CI [−8.20, −5.12], P = .05). B + C + D (OR = 0.12, 95% CI [−7.44, 13.75], P = .478). SUCRA was used to rank the 4 interventions to modulate NT-proBNP and the 2 controls: B + D (SUCRA = 93.5%) > A + C + D (SUCRA = 55.1%) > A + D (SUCRA = 40%) > C + D (SUCRA = 39.8%) > D (SUCRA = 20%). B + D is likely clinically B + D is likely the best intervention with the highest clinical efficiency in CHD-CHF patients.
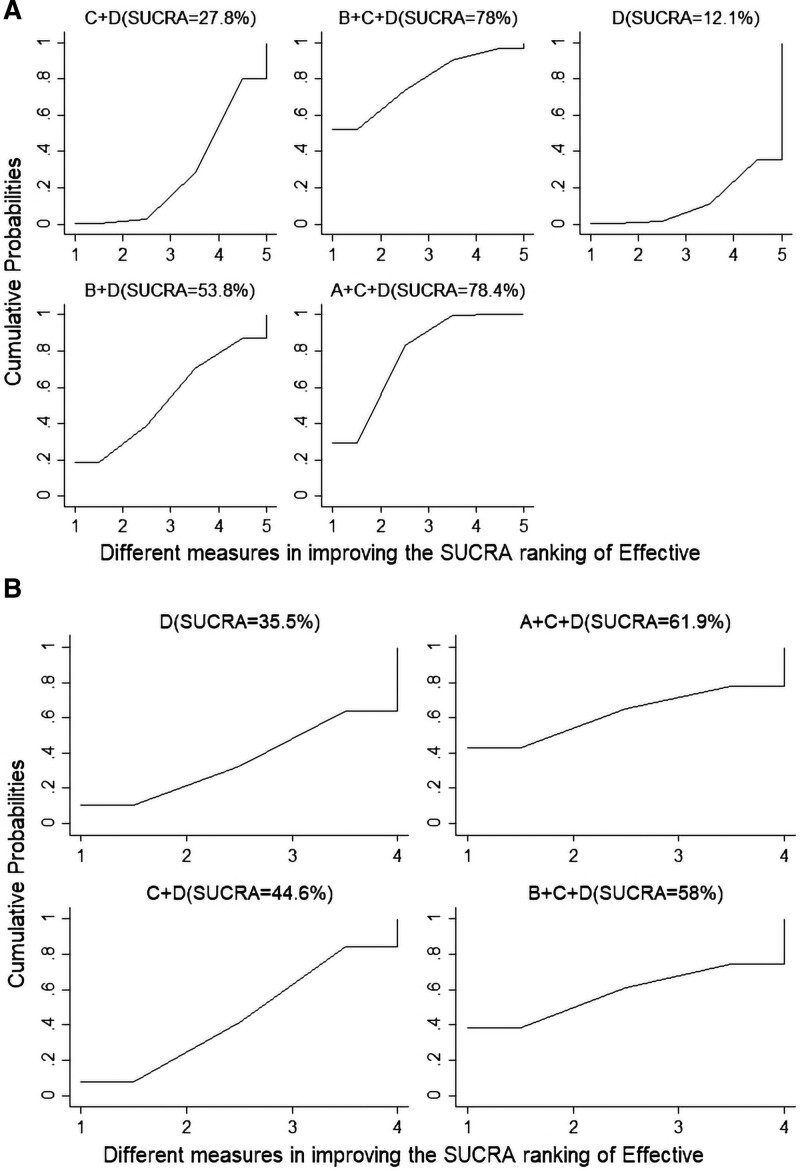
Unlike C + D, B + C + D (OR = 12.10, 95% CI [0.46, 8.71], P < .05), D (WMD = −1.4, 95% CI [0.04, 1.62], P < .05), B + C + D improved the clinical efficiency of CHD-HF patients more than D and C + D with a statistically significant difference. Comparison of the 2 TCM exercises showed that Taijiquan was superior to Baduanjin. (WMD = 4.26, 95% CI [0.02, 3.60], P < .05), and the differences between the other intercomparisons were not statistically significant. SUCRA was used to rank the 4 interventions for improving LVEF and the 2 controls: A + C + D (SUCRA = 93.1%) > B + C + D (SUCRA = 54%) > C + D (SUCRA = 44.8%) > D (SUCRA = 8.1%). A + C + D is likely the best intervention with the highest clinical efficiency in patients with CHD-CHF. The SUCRA probability ranking of the intervention effect of TCM health exercises on Effective in patients with CHD-HF are shown in Figure 15.
Figure 15.
(A) The SUCRA ranking of Effective (A). Figure 15B. The SUCRA ranking of Effective (B).
3.10. Number of adverse events
Furthermore, 2 cases of adverse reactions were included in 15 RCT studies, 1 case with dizziness and weakness symptoms, and 1 case with dizziness and panic symptoms; 2 cases of adverse reactions occurred in A + C + D. This suggests that the use of traditional Chinese medicine health care exercise is safe to a certain extent in patients with coronary heart disease combined with chronic heart failure. However, the development of exercise interventions should be performed based on the actual situation of the patient to avoid severe adverse reactions and aggravating the heart burden of the patient.
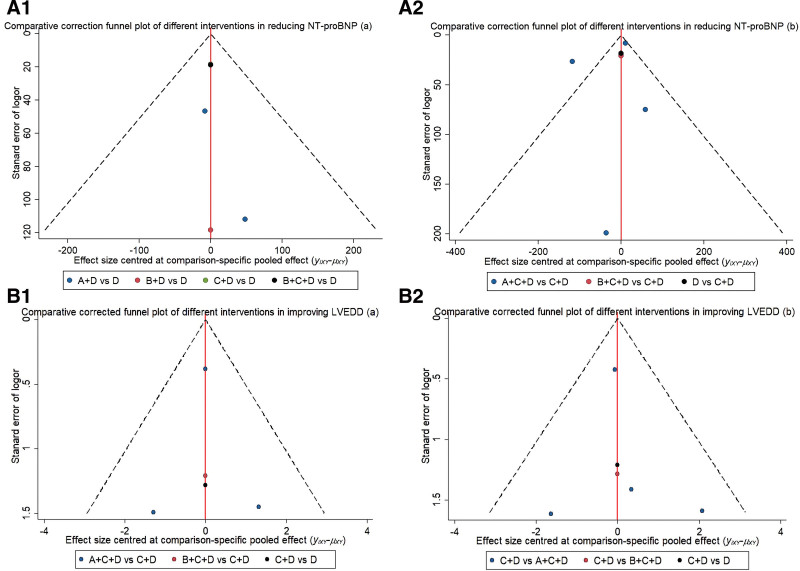
3.11. Publication bias
Correction-comparison funnel plotting of the included studies is shown in Figure 16A–F. All literature was distributed at locations near the central axis of the funnel plot, and the number of papers around the central axis was largely uniform and symmetrically distributed on both sides. This indicates a low likelihood of a small sample effect.
Figure 16.
(A1) Comparative correction funnel plot of NT-proBNP (A1). Figure 16A2. Comparative correction funnel plot of NT-proBNP (A2). Figure 16B1. Comparative corrected funnel plot of LVEDD (B1). Figure 16B2. Comparative corrected funnel plot of LVEDD (B2). Figure 16C. Comparative corrected funnel plot of LVEF (C). Figure 16D. Comparative corrected funnel plot of MLHFQ (D). Figure 16E. Comparative corrected funnel plot of 6WMT (E). Figure 16F. Effect size centered at comparison (F). LVEDD = left ventricular end-diastolic internal diameter, LVEF = left ventricular ejection fraction, MLHFQ = Minnesota Living with Heart Failure Questionnaire, NT-proBNP = N-terminal brain natriuretic peptidogen.
4. Discussion
Modern TCM rehabilitative exercise therapies trace their origins to the ancient art of Daoyin for health preservation. Grounded in the foundational tenets of TCM, such as the Yin-Yang, Five Elements, and the Zang-Fu meridian theories, these practices aspire to a harmonious unity of man and nature, skillfully balancing both strength and flexibility, dynamism and stillness. This holistic approach emphasizes a trinity of wellness: physical conditioning (through body movements), breath regulation, and mental nourishment. Notably, the “Baduanjin” or “Eight Brocades” stands out as a time-honored health regimen in TCM, casting a profound influence over generations. Compared to Tai Chi, the Eight Brocades offers more straightforward and accessible movements, making it a preferred choice for contemporary practitioners. Historical records credit Xu Xun of the Eastern Jin dynasty as the pioneer in integrating physical exercises into cardiac treatments. He devised a method dubbed “Cardiac Daoyin,” detailing movements reminiscent of the Eight Brocades, such as “stretching upwards to regulate the triple burners” and “drawing the bow on both sides as if shooting hawks.” These descriptions underscore that each sequence in the Eight Brocades correlates with specific organs, offering targeted therapeutic benefits. For instance, the “drawing the bow” movement stimulates the hand 6 meridians, particularly the Lung Meridian of Hand-Taiyin, while the “swaying the head and shaking the tail” technique revitalizes the spine and the Governor Vessel, harmonizing the heart energy. A notable emphasis of the Eight Brocades is the rotation of both arms, resonating with the insights from the classic “Ling Shu,” which states, “when the lungs and heart are diseased, the Qi lingers in both elbows.” Flexion and extension of the arms play a pivotal role in energizing the elbows, facilitating smooth energy flow through the heart and lung meridians, thereby promoting health and dispelling maladies. Intrinsically linked, the heart and lungs coexist in the upper burner, orchestrating blood circulation and respiratory functions, respectively, to ensure seamless Qi and blood flow. However, for patients with CHD-CHF, the predominant TCM diagnosis often revolves around Qi deficiency and blood stagnation. Through the rhythmic modulation of Qi and blood, the Eight Brocades can help restore the Yin-Yang balance of the heart and lungs. As a moderate-intensity aerobic exercise, it holds promise for CHD-CHF patients, especially those categorized under NYHA Class II to III.
4.1. Efficacy analysis of different traditional Chinese medicine health exercises on patients with CHD-CHF
In modern medicine, the therapeutic effects of the traditional exercise regimen, Ba Duan Jin, on patients with CHD-CHF are increasingly garnering attention. Numerous clinical studies have ascertained that consistent practice of Ba Duan Jin can significantly enhance the cardiac function, exercise endurance, and oxygen uptake of CHF patients. Yu Mei[21] involving 109 CHF patients demonstrated, over a span of 6 months, that the cohort employing Ba Duan Jin in conjunction with conventional exercises showed a marked superiority in enhancing physical stamina, pulmonary function, alleviating primary symptoms in traditional medicine, and elevating the quality of life compared to the control group that only engaged in standard exercises. Deng Xiangfeng[9] research further attested that, besides conventional western medical treatments, an integrated approach encompassing Ba Duan Jin improved several pivotal metrics, including BNP, METs, VO2 max, 6MWD, NYHA classification, traditional medical symptoms, and life quality. Notably, the composite treatment group exhibited a pronounced improvement in left ventricular ejection fraction compared to the control group. Shi Zibo,[18] albeit conducting a month-long study, yielded equally significant results. The Ba Duan Jin group demonstrated enhancements in key metrics such as anaerobic threshold, VO2 max, and carbon dioxide ventilatory equivalent slope compared to the control group. For CHF patients who cannot endure moderate-intensity exercises, especially those with heart function class IV or those with stable vital signs during acute HF bedridden phases, seated or supine Ba Duan Jin offers commendable rehabilitation benefits. As a venerable exercise regimen, Ba Duan Jin introduces a novel and efficacious alternative in modern medicine for the rehabilitation of CHD-CHF patients.
NMA of 15[7–21] RCT studies was conducted to objectively analyze the efficacy and safety of traditional Chinese medicine health exercises on improving clinical symptoms of CHF patients; we used cardiac function indices, 6WMT, efficiency, quality of survival, and the number of adverse events as observation indices. The results revealed that: A + D, A + C + D, B + C + D significantly improved the NT- proBNP better than D and C + D. According to the SUCRA ranking, A + D and A + C + D were most likely the best interventions for improving NT-proBNP. B + D, A + C + D, and B + C + D were significantly better than D and C + D in improving LVEF in patients with CHD-CHF; B + D, B + D, A + C + D was most likely the best interventions for improving LVEF based on the SUCRA ranking chart. A + D, B + D, A + C + D, B + C + D improved 6WMT in CHD-CHF patients, but A + D, A + C + D were the best interventions to improve 6WMT in CHD-CHF patients. B + C + D had the best effect on shrinking LVESD. Unlike D and C + D interventions, A + D and B + C + D were the most likely the best interventions for contracting LVEDD in patients with CHA-CHA. According to the SUCRA ranking chart, B + D and A + D were consistent in their capacity to improve MLHFQ in CHD-CHF patients compared to D and C + D interventions, but B + D had better efficacy. In contrast with A + C + D, B + C + D was most likely the best intervention for improving MLHFQ. According to the SUCRA ranking chart, B + D was the most clinically effective intervention compared to D and C + D. Unlike B + C + D, C + D, and D interventions, A + C + D was the most clinically effective intervention.
Out of all the RCT studies we included, only half investigated the safety and the majority did not report adverse reactions. The comparison revealed 2 cases of adverse reactions in the intervention group in which BaduanJin was implemented, that is, 1 patient experienced dizziness and weakness symptoms, whereas the other experienced dizziness and panic symptoms during the implementation of Baduanjin.
4.2. Mechanism of action analysis of different traditional Chinese medicine health exercises on CHD-CHF patients
Patients with CHD-CHF have long-term pathological factors that induce changes in cardiac structure, particularly in the left heart chambers, resulting in abnormalities in cardiac function including decreased compliance of the ventricular wall and lower cardiac output. Deng Xiangfeng et al[22] confirmed that regular 8-danjin exercises in patients with stable heart failure can effectively improve muscle aerobic metabolic capacity, promote cardiac function recovery, and increase the left heart ejection fraction of patients. The reasons for this are primarily explained in terms of special characteristics of traditional health exercises: Baduannjin and Taijiquan are traditional Chinese medicine health exercises guided by Chinese medicine theory, which are slower, softer, more coherent, and more varied in their movements than ordinary aerobic exercises. During the exercise process, Baduanjin and Taijiquan focus on a combination of limb trunk and whole-body muscle stretching exercises and breathing, which, stimulates yang energy through limb movement, increases the ability of heart to govern blood and vessels for optimal blood circulation, improves warm Yang and transform water to reduce edema, relieves symptoms of heart failure, and improves cardiopulmonary function, thereby preventing left ventricular remodeling to maintain cardiac function.
Patients with CHD-CHF are usually characterized by a prolonged period of illness, recurrent disease, and numerous complications, which have different degrees of effect on the physical, emotional, and social aspects of patients. The probability ranking of this study revealed that traditional Chinese health exercises improved patient symptoms, quality of life, and exercise endurance[3] revealed that Baduanjin has benefits in improving the quality of life of patients with chronic heart failure and to a certain extent improving negative emotions including anxiety and depression. The reasons for this are mainly explained in terms of the psychological characteristics of traditional health exercises: Unlike ordinary aerobic exercise, traditional health exercises in Chinese medicine focus more on a combination of mind and body and emphasize psychological conditioning. Physical exercise and psychological conditioning during exercise can help patients manage their intestinal flora structure and autonomic function, reduce cardiac load, improve cardiac function indexes, and increase exercise endurance and quality of life. Exercise and psychological treatment can help patients feel comfortable and happy, relieve tension and anxiety, improve interpersonal skills, and play an important role in promoting psychological health.
4.3. Limitations of the present study
A network Meta-analysis was applied to evaluate the improvement of clinical symptoms in patients with CHD-CHF by different traditional Chinese medicine health exercises. However, this work has compelling limitations: There were differences in gender, age, disease duration, cardiac function classification, complications, study design, intervention period, and clinical medication among the subjects; this may cause heterogeneity between studies. The number of literature incorporated for different interventions significantly varied, for instance, only 4 articles for Taijiquan and 9 articles for Baduanjin; this may cause bias. The results of our network meta-analysis must be interpreted with caution due to the variable data quality and limited sample sizes of the included studies. In terms of study methodology, we only used SUCRA curves to rank the efficacy of different interventions, which is limitation that should not be ignored.
5. Conclusion
The incidence and mortality rates of cardiovascular diseases globally remain consistently high.[23] Academician Chen Keji and others have pointed out that while drawing upon and learning from the advanced rehabilitation experiences and techniques of Western countries, it essential to integrate traditional Chinese medicine rehabilitation methods.[24] Combining both Western and traditional Chinese medical approaches to cardiac rehabilitation is a significant advantage for China. Traditional Chinese medical rehabilitation exercises have shown superiority in strengthening skeletal muscles (including respiratory muscles), enhancing exercise endurance, improving respiratory efficiency, increasing tissue oxygen content, and regulating emotions to promote mental health.
In conclusion, the results of the combined reticulated Meta-analysis showed that the 2 types of Ba Duan Jin and Taijiquan can improve LVEF, 6WMT, MLHFQ, LVEDD, and LVESD in patients with CHD-CHF. Moreover, traditional Chinese health exercises combined with conventional treatment are more effective than conventional treatment D alone in patients with CHD-CHF. Therefore, clinicians should consider whether Ba Duan Jin or Taijiquan should be added as an adjunct to cardiac rehabilitation in the clinical treatment plan for patients with CHD-CHF based on the condition and physical status of the patient.
The following aspects should be addressed in follow-up studies: Future RCT-related studies should be performed with strict reference to international norms for study design to significantly avoid methodological heterogeneity; high-quality RCT studies should be continued on different types of traditional Chinese health exercises; additional studies on traditional Chinese health exercises and patients with coronary heart disease combined with chronic heart failure, including exercise frequency and further studies on traditional Chinese health exercises and patients with coronary heart disease combined with chronic heart failure, including exercise frequency and duration; more high-quality clinical trials are required to validate the findings of this work.
Acknowledgments
This study has integrated the research findings of many scholars, for which we are immensely grateful. We also extend our heartfelt thanks to all the authors who collaborated in completing this study, with special gratitude directed towards Dr. Shuwen Pang. Finally, I (Dr. Xiwei Huang) would like to express my deepest appreciation to my wife, Ms. Jiaman Chen, and our adorable little treasure, Huang Muchen, for their unwavering support in my research work.
Author contributions
Conceptualization: Xiwei Huang, Shuwen Pang, Yueli Zhao, Jing Qian, Jiahui Zhong, Shuai Liu.
Data curation: Xiwei Huang, Shuwen Pang, Yueli Zhao, Jing Qian, Shuai Liu.
Formal analysis: Xiwei Huang, Shuwen Pang, Jing Qian, Jiahui Zhong.
Funding acquisition: Shuwen Pang, Jiahui Zhong, Shuai Liu.
Investigation: Shuwen Pang, Jiahui Zhong, Shuai Liu.
Methodology: Xiwei Huang, Shuwen Pang.
Project administration: Xiwei Huang, Shuwen Pang.
Resources: Shuwen Pang.
Software: Xiwei Huang, Shuwen Pang.
Supervision: Shuwen Pang.
Validation: Shuwen Pang.
Visualization: Xiwei Huang, Shuwen Pang.
Writing – original draft: Shuwen Pang.
Writing – review & editing: Xiwei Huang, Shuwen Pang.
Abbreviations:
- CHD
- coronary heart disease
- CHF
- chronic heart failure
- LVEDD
- left ventricular end-diastolic internal diameter
- LVEF
- left ventricular ejection fraction
- LVESD
- left ventricular end-systolic internal diameter
- MLHFQ
- Minnesota Living with Heart Failure Questionnaire
- NMA
- net meta-analysis
- NT-proBNP
- N-terminal brain natriuretic peptidogen
- NYHA
- The New York Heart Association
- RCT
- randomised controlled trials
- TCM
- Traditional Chinese medicine.
XH and SP contributed equally to this work.
The authors have no conflicts of interest to disclose.
This work was funded by Guangzhou Science and Technology Innovation Committee, Guangdong Province, China, and is part of the Guangzhou Science and Technology Innovation Project (No. 202002020036); the project title is Research on AI Models and Key Technologies for Acute Chest Pain Diagnosis and Treatment Using Big Data.
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Systematic evaluation registration: PROSPERO underwent study registration and received registration number: CRD42022364351.
The datasets generated during and/or analyzed during the current study are publicly available.
How to cite this article: Huang X, Pang S, Zhao Y, Qian J, Zhong J, Liu S. Efficacy and safety of different traditional Chinese health exercises in patients with coronary heart disease combined with chronic heart failure: A network meta-analysis. Medicine 2023;102:50(e36522).
Contributor Information
Shuwen Pang, Email: pangshuwen514@163.com.
Yueli Zhao, Email: zhaoyueligz@163.com.
Jing Qian, Email: qianjing0414@163.com.
Jiahui Zhong, Email: dorisinsight@163.com.
Shuai Liu, Email: Liu19866680654@outlook.com.
References
- [1].Chen M, Ou L, Chen Y, et al. Effectiveness and safety of Baduanjin exercise (BDJE) on heart failure with preserved left ventricular ejection fraction (HFpEF): a protocol for systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e22994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Elgendy IY, Mahtta D, Pepine CJ. Medical therapy for heart failure caused by ischemic heart disease. Circ Res. 2019;124:1520–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Park JJ, Choi DJ. Current status of heart failure: global and Korea. Korean J Intern Med. 2020;35:487–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Liao Y, Wen H, Ge S, et al. Effects of traditional Chinese exercise in patients with chronic heart failure: a systematic review and meta-analysis. Eur J Integr Med. 2020;40:101218. [Google Scholar]
- [5].Nichols S, McGregor G, Breckon J, et al. Current insights into exercise-based cardiac rehabilitation in patients with coronary heart disease and chronic heart failure. Int J Sports Med. 2021;42:19–26. [DOI] [PubMed] [Google Scholar]
- [6].Pagliaro BR, Cannata F, Stefanini GG, et al. Myocardial ischemia and coronary disease in heart failure. Heart Fail Rev. 2020;25:53–65. [DOI] [PubMed] [Google Scholar]
- [7].Yang X, Cui C. The function of Taijiquan in the cardiac rehabilitation. Chin Med Mod Distance Educ China. 2017;15:427–37. [Google Scholar]
- [8].Chen X, Yang L. Analysis of the effect of Badaanjin in the cardiac rehabilitation of patients with chronic heart failure. Mod Drug Appl China. 2020;14:2–5. [Google Scholar]
- [9].Deng X. Clinical study of “Eight Duan Jin” on the rehabilitation of patients with chronic heart failure [diss.]. Yunnan University of Traditional Chinese Medicine; 2020. Available at: https://link.cnki.net/doi/10.27460/d.cnki.gyzyc.2019.000004 [access date December 6, 2022]. [Google Scholar]
- [10].Deng X, Zhang J. Effect of Baduanjin with aerobic endurance training on coronary heart disease and heart failure. Knowl Cardiovasc Dis Control Acad Ed. 2022;12:3–9. [Google Scholar]
- [11].Hong X. A clinical study on the use of Ba Duan Jin in patients with coronary heart disease and chronic heart failure[diss.]. Fujian University of Chinese Medicine; 2020. Available at: https://link.cnki.net/doi/10.27021/d.cnki.gfjzc.2020.000121 [access date December 6, 2022]. [Google Scholar]
- [12].Huang C. Study on the rehabilitation of cardiac function in patients with coronary artery disease (NYHA Class III) by Tai Chi ball-holding and cloud hand [diss.]. Fujian University of Chinese Medicine; 2014. Available at: https://kns.cnki.net/kcms2/article/abstract?v=lVku9qtM8H_1JZKEuva5HSEpwXM3FwOE0mchn5Rl8bQI9PjfQyeFvPrPULgIbrl3s2Cw8w9UrOWyBE7XF4IPxy9UsXYuvdQoMihvycQwWsPxdzQX0lk5OvGV366LAsVQoKtFCZJuko=&uniplatform=NZKPT&language=CHS [access date December 6, 2022]. [Google Scholar]
- [13].Jiang Q, You X. Aerobic endurance training with Baduanjin in elderly patients with coronary heart disease with heart failure. Knowl Cardiovasc Dis Control Acad Ed. 2022;12:3–7. [Google Scholar]
- [14].Kang Z, Liu C, Wang Y, et al. Analysis of the effect of Baduanjin combined with aerobic endurance training on elderly patients with stable coronary artery disease combined with chronic heart failure. Chin J Front Med Electron Version. 2021;13:4. [Google Scholar]
- [15].Liu H. Clinical efficacy of Tai Chi exercise in the treatment of chronic heart failure in coronary heart disease[diss.]. Guangzhou University of Chinese Medicine; 2022. Available at: https://kns.cnki.net/kcms2/article/abstract?v=lVku9qtM8H_r7Tlq0wJLLfrfFV7QU2rsAEhl2ka6pZhqxRcPFam5VvAk9JdH843hzs0WLLGUKQrDJ7yYhw9hkpMqjfiFOOUFCz0mhO7xsHFwMVLMBt232dqb58I1tLoJ8_JKrstqIEG4Rco1Nwwgw==uniplatform=NZKPTlanguage=CHS [access date December 6, 2022]. [Google Scholar]
- [16].Pan W, Zhou H, Wang Y, et al. The effect of Ba Duan Jin in the cardiac rehabilitation of patients with chronic heart failure. Guangming Chin Med. 2019;34:3–6. [Google Scholar]
- [17].Sang L, Liu Z, Lang F, et al. Effect of “Tai Chi Rehabilitation Exercise” on cardiac function and quality of life of elderly patients with coronary heart disease and chronic heart failure. Chin J Gerontol. 2015;14:3957–8. [Google Scholar]
- [18].Shi Z. Clinical study of “Eight Duan Jin” on the rehabilitation of patients with chronic heart failure[diss.]. Liaoning University of Traditional Chinese Medicine; 2018. Available at: https://kns.cnki.net/kcms2/article/abstract?v=lVku9qtM8H-fxoHtJPBkXFHKxTJXjOzRjB1oXKRiWQMKgDX2cp0NIEYBY5491pBddWQDFUruVhuta8ryBx_COmvJ45dfcb4AvZ9aAV07doIqXnYEquicN6iv59e7gF7z93907OAEAsOIR5ONwyv-lg==uniplatform=NZKPTlanguage=CHS [access date December 6, 2022]. [Google Scholar]
- [19].Tong H. A clinical study of Baduanjin exercise as an aid in the treatment of chronic heart failure[diss.]. Guangzhou University of Chinese Medicine; 2019. Available at: https://link.cnki.net/doi/10.27044/d.cnki.ggzzu.2019.000511 [access date December 6, 2022]. [Google Scholar]
- [20].Xiong X, Deng X. The efficacy of Ba Duan Jin in patients with coronary heart disease and chronic heart failure. Chin J Mod Med. 2016;5:55–6. [Google Scholar]
- [21].Yu M. A randomized controlled study of Ba Duan Jin applied to phase II rehabilitation of chronic heart failure patients with coronary artery disease[diss.]. Beijing University of Chinese Medicine; 2018. Available at: https://kns.cnki.net/kcms2/article/abstract?v=lVku9qtM8H8PGuxtAe7_x_UPBW6Na8xngrcxcQ4LF-5o969N6l79MZsEc0Syxcvsxuty6SdkmFJykui76N8QE3hNhrjsdxDmkSIigXlaHy-5qHFFFZFLUVwemzBTapoKF6Aud8WN2TCkthetZW-YfQ==uniplatform=NZKPTlanguage=CHS [access date December 6, 2022]. [Google Scholar]
- [22].Deng X, Li S, Zhao C, et al. The application of “Eight Duan Jin” in the rehabilitation of patients with chronic heart failure. Chin Ethn Folk Med. 2019;28:3–7. [Google Scholar]
- [23].Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Zhang J, Li Y, Zhang B, et al. Evidence-based traditional Chinese medicine research: Beijing declaration. J Evid Based Med. 2020;13:91–2. [DOI] [PubMed] [Google Scholar]