Abstract
We sought to investigate temporal trends in telehealth availability among outpatient mental health treatment facilities and differences in the pace of telehealth growth by state urbanicity and rurality. We used the National Mental Health Services Survey (2015–2020) to identify outpatient mental health treatment facilities in the US (N = 28,989 facilities; 2015 n = 5,018; 2020 n = 4,889). We used logistic regression to model telehealth, predicted by time, state rurality (1 to 10% rural, 10 to < 20%, 20 to < 30%, or 30%), and their interaction, and adjusted for relevant covariates. We estimated the predicted probability of telehealth based on our model. We estimated effects with and without data from 2020 to assess whether the rapid and widespread adoption of telehealth during the COVID-19 pandemic changed the rural/urban trajectories of telehealth availability. We found that telehealth grew fastest in more urban states (year*rurality interaction p < 0.0001). Between 2015 and 2020, the predicted probability of telehealth in more urban states increased by 51 percentage points (from 9 to 61%), whereas telehealth in more rural states increased by 38 percentage points (from 23 to 61%). Predicted telehealth also varied widely by state, ranging from more than 75% of facilities (RI, OR) to below 20% (VT, KY). Health systems and new technological innovations must consider the unique challenges faced by urban populations and how best practices may be adapted to meet the growing urban demand. We framed our findings around the need for policies that minimize barriers to telehealth.
Keywords: Behavioral health services, Telehealth, Epidemiology
Background
Mental health service utilization is low overall [1, 2], and particularly low in rural areas [3, 4]. In the first quarter of 2023, nearly two-thirds of all mental health provider shortage areas was in rural communities, resulting in 37 million rural Americans with limited or no access to mental healthcare [5]. Urban populations are not without healthcare challenges, however. While a smaller percentage of mental health provider shortage areas are in urban areas (31%), the sheer size and density of urban populations result in 55 million urban residents living in a mental health provider shortage area [5]. The national narrative around mental health system strengthening has largely been around rural populations, driven in part by changing demographics, deteriorating infrastructure, a shrinking workforce, and multiple individual barriers to utilizing services [3, 4, 6–8]. At the same time, mental healthcare in urban areas faces both similar and unique challenges pertaining to treatment uptake, poor outcomes, and disparities [9]. Mental healthcare innovations that can be adapted to meet the needs of both rural and urban populations may help to expand the reach and use of mental health services.
Telehealth is a promising tool that has increased the use of mental health services in the past decade [10], with a notably sharp increase in use during the COVID-19 pandemic [11]. Mental health treatment utilization is universally low due to a range of historical barriers limiting access [2, 12, 13], some of which may be substantially reduced through digital technologies like telehealth. Furthermore, several mental health outcomes between in-person and telehealth treatment settings have not differed significantly [14, 15], providing additional support for telehealth’s clinical potential. The public health emergency (PHE) prompted many mental health providers to pivot to telehealth services primarily to limit community movement, practice social distancing, and respond to an increase in home-based isolation and stress associated with the pandemic [16]. With the end of the COVID-19 PHE declaration in May 2023, an investigation into telehealth trends before and during the pandemic may offer insight into the post-pandemic telehealth trajectory. Importantly, telehealth modalities vary, and differentiating between types of telehealth services is important to our understanding of how people are receiving and using these services. At the same time, not all reports define specific components of telehealth, like audio-only or audio–video, for example, which results in a valuable but more ambiguous interpretation of health system characteristics. Audio-only telehealth may be more appropriate for individuals with low access to broadband or limited digital literacy, many of whom are disproportionately represented in Medicaid and health disparity populations [17]. While investigating differences in the utilization of different telehealth modalities is beyond the scope of this study, such differences are important to recognize and future research should address emerging questions about audio-only and audio-visual services.
Telehealth, defined broadly, is growing in mental healthcare settings, due in part to recent federal policies that supported the continuation of telehealth growth in behavioral health settings during and after the COVID-19 pandemic, like the Consolidated Appropriations Act of 2021 (2021 CAA), for example [18]. As part of the 2021 CAA, flexibilities were approved that allowed for the evaluation, diagnosis, and treatment of mental health and substance use disorders accessible from a person’s home, eased access to telehealth for Medicare beneficiaries, and updated the Physician Fee Schedule (PFS) for mental health providers. Federally Qualified Health Centers and Rural Health Centers were also newly allowed to act as distant site telehealth providers and able to be reimbursed at an amount comparable to PFS amount. At the same time, there remain barriers to adoption that apply to both rural and urban providers, including reimbursement, access to the internet and digital device, workforce challenges, and licensure regulations [13, 19, 20]. One study found that low interoperability between electronic record systems, difficulties with data integration, and non-user-friendly telehealth software applications were major barriers to telehealth adoption in rural hospitals, while urban hospitals cited many fewer technological challenges [21]. Implementing telehealth services in urban areas is not without challenges, however. Bagchi and colleagues [22] identified high distrust in the security and privacy of digital systems among urban residents, and that access to basic telehealth technology was a particular concern in under-resourced urban communities. While access to broadband internet and digital devices is generally more of a challenge in rural communities, there are relatively small but nontrivial concentrations of low broadband connectivity and low access to digital technology in urban areas, specifically among poor and racial/ethnic minority neighborhoods [23, 24]. In addition, given the magnitude of differences in the population density between rural and urban areas, the raw number of households without an internet connection is almost three times higher in urban areas (13.6 million households without internet) versus rural areas (4.6 million) [24]. The COVID-19 pandemic clearly played a role in telehealth adoption nationally, but little national research has investigated whether the changing pace of telehealth adoption in mental health treatment settings differed by rurality.
We investigated differences in telehealth availability in outpatient mental health treatment settings, focusing on state rurality and changes over time. Given the abrupt and sweeping adoption of telehealth in 2020 across most sectors, including mental health, we designed our study to assess changes with and without 2020 to help illustrate the influence of the pandemic on projected trends. Our study was motivated by the theoretical underpinning of the diffusion of innovation theory (DIT) [25]. DIT was instrumental in our conception of differences in the rate of telehealth adoption across levels of rurality and within states. Specifically, the extant literature has focused much more on telehealth as a solution for rural healthcare problems, but urban populations also have a demonstrated demand for this technology. The process of diffusion may change in some instances when a new technology converges with national attention to a problem [26, 27], like COVID-19, for example. Our study addresses this concern by highlighting differences and similarities in the diffusion of telehealth in mental health settings before and during the pandemic.
Methods
Data source and Sample
We used repeated, cross-sectional administrative data from the National Mental Health Services Survey (N-MHSS; 2015–2020) to identify outpatient mental health treatment facilities in the US (N = 28,989 facilities; 2015 n = 5018; 2020 n = 4889). N-MHSS is planned and directed by the Center for Behavioral Health Statistics and Quality, which is housed within the Substance Abuse and Mental Health Services Administration. In brief, N-MHSS includes data on characteristics of all known public and private facilities in the US that provide specialty mental health treatment, defined by SAMHSA as any facility or entity that provides mental health treatment services to people with mental illness. Representatives from each facility completed an annual survey about services provided. In 2015, 2019, and 2020, the response rates among facilities eligible to participate were 90%, 91%, and 89%, respectively [28]. This study was a secondary analysis of publicly available administrative data describing characteristics of mental health facilities. As such, no human subjects were involved in this study and no individual-level data was available or used.
Variables
Our outcome of interest was a binary indicator of whether a facility offered telehealth (yes/no). Survey respondents were asked to mark all that apply in response to the question, “Which of these mental health treatment modalities are offered at this facility, at this location?” Our indicator of telehealth was derived from the response option, “Telemedicine/telehealth therapy (including internet, web, mobile, and desktop programs).” Examples of the 15 other possible response options include cognitive behavioral therapy, couples/family therapy, and transcranial magnetic stimulation.
Our focal predictors included year and state rurality. Year was a continuous variable, ranging from 2015 to 2020. State rurality data came from the US Census Bureau estimates for the percentage of state residents living in a rural area in 2020 [29]. Residence in a rural location is defined by the Census Bureau as anyone not residing in an urbanized area of 50,000 people or more or in an urban cluster of 2500–50,000 people. We categorized the state percentages into four groups: < 10% of state residents living in a rural area, 10 to < 20%, 20 to < 30%, and 30%. We also included several facility-level covariates in our model based on a priori understanding of factors that may confound the relationship between our outcome and focal predicators. We included the facility owner type (private for-profit, private non-profit, or public agency), whether a facility was licensed by a state department of health, whether the facility was accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF), and whether the facility offered integrated primary care services.
Analysis
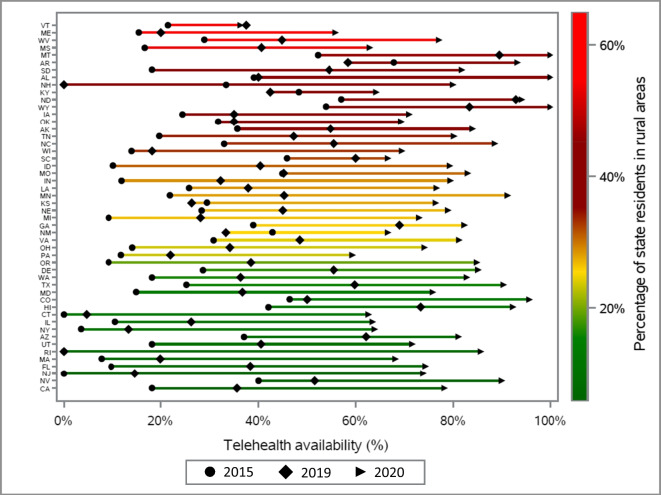
We used SAS v9.4 for all analyses [30]. We described the distribution of each study variable for the total sample as well as stratified by our outcome of telehealth availability. All subsequent analyses were designed to account for a substantial jump in telehealth availability from 2019 (35%) to 2020 (75%), which was very likely due to the rapid and far-reaching adoption of remote healthcare services during the first year of the COVID-19 pandemic. To show changes in telehealth availability by state rurality and over time, we calculated the percentage of facilities that offered telehealth within each level of rurality every year. We calculated the relative percentage change in telehealth availability from 2015 and 2019, as well as from 2019 to 2020. To help visualize these summary statistics by state, we used a barbell graph and plotted the proportion of facilities in every state that offered telehealth in 2015 (circle), 2019 (diamond), and 2020 (arrow). We used a color ramp to visually rank each state based on the percentage of residents living in a rural area (green = less rural, red = more rural). This approach provides valuable information about the pace and direction of telehealth adoption for each state, with wider distances between each year interpreted as a bigger, or faster, change in telehealth. We also provided supplementary information about the number of telehealth facilities and the number of total outpatient facilities in each state in multiple years. This is useful in interpreting the differences in the numerators and denominators used to calculate the state percentages. For example, in 2020, Louisiana had 59 out of 77 total facilities offering telehealth and Kansas had 13 out of 17 total facilities offering telehealth, which translates to 76% of facilities offering telehealth in both states.
We used multiple logistic regression to model telehealth availability. We developed two models to compare effects with and without data from the year 2020 (model 1, 2015–2019; model 2, 2015–2020). The model specifications were identical for both models. We included an interaction between year and rurality to test whether the odds of telehealth availability over time differed depending on state rurality category. We reported the p-value for a joint test of the overall significance of the interaction, which is an indication of a significant difference in the slopes of predicted telehealth values over time and within each rurality category. Interactions in generalized linear models specify that the effect of one variable is conditional on the value of a second variable. As such, there are no main or average effects for year or rurality independent of the interaction term [31]. To ease the interpretation of our interaction findings, we provided adjusted odds ratios, 95% confidence intervals, and p-values for the within-group estimates of each interaction term. The within-rural estimates are interpreted as the increase in the odds of telehealth availability for each additional year within each rurality category. The within-year estimates are interpreted as the odds of telehealth availability at each level of rurality (compared to < 10% rural [reference]) in 2015, 2019, and 2020. Within-year estimates for the years 2016, 2017 and 2018 were not reported. Finally, to visualize the interaction, we used output from both models to plot the adjusted predicted probabilities of telehealth availability within each rurality category over time.
Results
Across all years, the proportion of outpatient mental health treatment facilities offering telehealth increased from 18.6% in 2015 to 74.7% in 2020 (Table 1). The majority of facilities was owned by private non-profit entities (62.8%), was not licensed by a state department of health (55.9%), was not CARF-accredited (78.7%), and did not offer integrated primary care (81.9%). The proportion of facilities offering telehealth was higher in more rural states (30.1% of facilities offered telehealth in states with less than 10% rural populations, 38.3% of facilities offered telehealth in states with 30% or more rural populations).
Table 1.
Facility- and state-level characteristics of specialty outpatient mental health treatment facilities (N-MHSS; 2015–2020)
| Variables | Total N = 28,989 |
Provided telehealth n = 9807 (33.83%) |
Did not provide telehealth n = 19,182 (66.17%) |
|---|---|---|---|
| n (%) | Row % | Row % | |
| Facility-level characteristics | |||
| Year | |||
| 2015 | 5018 (17.31) | 18.59 | 81.41 |
| 2016 | 4747 (16.38) | 21.47 | 78.53 |
| 2017 | 4563 (15.74) | 24.26 | 75.74 |
| 2018 | 4610 (15.90) | 28.44 | 71.56 |
| 2019 | 5162 (17.81) | 34.62 | 65.38 |
| 2020 | 4889 (16.87) | 74.66 | 25.34 |
| Facility owner | |||
| Private for-profit | 6132 (21.15) | 35.26 | 64.74 |
| Private non-profit | 18,203 (62.79) | 30.75 | 69.25 |
| Public agency | 4654 (16.05) | 43.98 | 56.02 |
| Licensed by state department of health | |||
| Yes | 12,760 (44.02) | 37.39 | 62.61 |
| No | 16,229 (55.98) | 31.03 | 68.97 |
| Accredited by CARF | |||
| Yes | 6155 (21.23) | 43.10 | 56.90 |
| No | 22,834 (78.77) | 31.33 | 68.67 |
| Offered integrated primary care | |||
| Yes | 5234 (18.06) | 45.32 | 54.68 |
| No | 23,755 (81.94) | 31.30 | 68.70 |
| State-level characteristic | |||
| Rurality1 | |||
| < 10% | 5672 (19.57) | 30.10 | 69.90 |
| 10 to < 20% | 9138 (31.52) | 31.40 | 68.60 |
| 20 to < 30% | 7139 (24.63) | 35.45 | 64.55 |
| 30% | 7040 (24.29) | 38.35 | 61.65 |
1Percentage of state residents living in rural areas was derived from the US Census Bureau’s 2020 American Community Survey, defined as anyone not residing in an urbanized area of 50,000 people or more, or an urban cluster of at least 2,500 and less than 50,000
The proportion of facilities offering telehealth increased the most in the least rural states (< 10% rural) (Table 2), such that telehealth availability grew by 144.2% from 2015 to 2019 and by 143.9% from 2019 to 2020. In contrast, in the most rural states ( 30% rural), telehealth availability decreased by 3.4% from 2015 to 2019 and increased by 101.2% from 2019 to 2020. Overall, the percentage change became smaller as states became more rural, and this trend was observed comparing 2015 to 2019 as well as comparing 2019 to 2020.
Table 2.
Change in telehealth availability among specialty mental health outpatient treatment facilities, by state rurality and over time
| Telehealth availability | % change | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2015–2019 | 2019–2020 |
| Rurality1 | row % | row % | row % | row % | row % | row % | ||
| < 10% | 12.72 | 16.16 | 19.64 | 24.10 | 31.07 | 75.81 | 144.26 | 143.99 |
| 10 to < 20% | 13.82 | 18.05 | 21.23 | 25.02 | 32.08 | 73.45 | 137.34 | 123.93 |
| 20 to < 30% | 19.38 | 22.76 | 27.21 | 31.33 | 36.86 | 73.86 | 90.19 | 100.38 |
| 30% | 39.23 | 28.34 | 29.14 | 33.48 | 37.88 | 76.24 | − 3.44 | 101.26 |
1Percentage of state residents living in rural areas was derived from the US Census Bureau’s 2020 American Community Survey, defined as anyone not residing in an urbanized area of 50,000 people or more, or an urban cluster of at least 2500 and less than 50,000
The proportion of facilities offering telehealth in 2015, 2019, and 2020 varied by state (Fig. 1). Telehealth availability decreased in five states from 2015 to 2019 (AR, KS, KY, NH, NM), all of which had larger rural populations (KS and NM, 20 to < 30% rural; AR, KY, and NH, 30% rural). Only one state had a decrease in telehealth availability from 2019 to 2020 (VT, 30% rural). The biggest changes from 2015 to 2020 were observed in more urban states, including Rhode Island and New Jersey (1 to < 10% rural) and Oregon (10 to < 20% rural).
Fig. 1.
Telehealth availability among specialty mental health outpatient treatment facilities by state, rurality, and over time
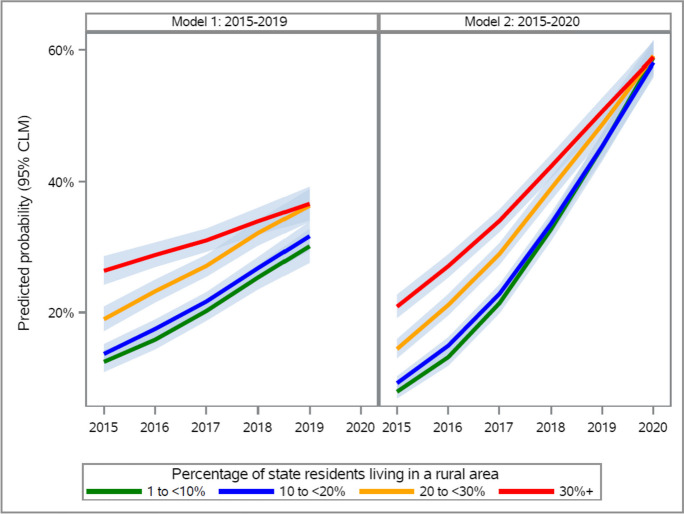
The year*rurality interaction was significant in both model 1 (2015–2019) and model 2 (2015–2020) (p < 0.0001 for both; Table 3). With each additional year, the odds of telehealth availability were smaller for more rural vs. more urban states, and this trend was observed in model 1 (< 10% rural, aORyear = 1.33, 95% CIyear = 1.26–1.40, pyear < 0.0001; 30% rural, aORyear = 1.14, 95% CIyear = 1.09–1.19, pyear < 0.0001) and in model 2 (< 10% rural, aORyear = 1.79, 95% CIyear = 1.72–1.86, pyear < 0.0001; 30% rural, aORyear = 1.43, 95% CIyear = 1.39–1.48, pyear < 0.0001). By 2020 (model 2), compared to the most urban states, there was no observed difference in the odds of telehealth availability in more rural states (10 to < 20% rural, aOR = 0.94, 95% CI = 0.83–1.07, p = 0.36; 20 to < 30% rural, aOR = 0.95, 95% CI = 0.83–1.08, p = 0.46; 30% rural, aOR = 1.05, 95% CI = 0.92–1.20, p = 0.46). Figure 2 helps to visualize the interaction by plotting the predicted probabilities by rurality group over time for both models. In models 1 and 2, the slowest growth in telehealth is seen among the most rural states ( 30% rural, red lines). In model 2, the fastest growth is depicted by the steepest upward slopes as seen among the most urban states (1 to < 10% rural, green line; 10 to < 20% rural, blue line). By 2020, the predicted probabilities of telehealth converge to roughly the same point below 60%.
Table 3.
Multiple logistic regression modeling the association between telehealth availability and year*rurality interaction
| Variables1 | Model 1: 2015–2019 | Model 2: 2015–2020 | ||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | p-value | aOR | 95% CI | p-value | |
| Year*rurality interaction | Joint test p < 0.0001 | Joint test p < 0.0001 | ||||
| Within-rural estimates of year2 | ||||||
| Rurality3 | ||||||
| < 10% rural | 1.33 | 1.26, 1.40 | < 0.0001 | 1.79 | 1.72, 1.86 | < 0.0001 |
| 10 to < 20% | 1.31 | 1.26, 1.37 | < 0.0001 | 1.71 | 1.66, 1.77 | < 0.0001 |
| 20 to < 30% | 1.26 | 1.21, 1.31 | < 0.0001 | 1.56 | 1.51, 1.62 | < 0.0001 |
| 30% | 1.14 | 1.09, 1.19 | < 0.0001 | 1.43 | 1.39, 1.48 | < 0.0001 |
| Within-year estimates of rurality | Within-2015 | Within-2015 | ||||
| Rurality | ||||||
| < 10% rural | Ref | Ref | ||||
| 10 to < 20% | 1.12 | 0.93, 1.34 | 0.22 | 1.19 | 0.99, 1.42 | 0.06 |
| 20 to < 30% | 1.56 | 1.30, 1.86 | < 0.0001 | 1.87 | 1.56, 2.24 | < 0.0001 |
| 30% | 2.69 | 2.26, 3.20 | < 0.0001 | 3.22 | 2.71, 3.82 | < 0.0001 |
| Rurality | Within-2019 | Within-2020 | ||||
| < 10% rural | Ref | Ref | ||||
| 10 to < 20% | 1.07 | 0.93, 1.24 | 0.35 | 0.94 | 0.83, 1.07 | 0.36 |
| 20 to < 30% | 1.25 | 1.08, 1.45 | < 0.01 | 0.95 | 0.83, 1.08 | 0.43 |
| 30% | 1.47 | 1.27, 1.71 | < 0.0001 | 1.05 | 0.92, 1.20 | 0.46 |
1Models adjusted for facility owner type, health department licensure, CARF accreditation, and integrated primary care
2Year is a continuous variable
3Percentage of state residents living in rural areas was derived from the US Census Bureau’s 2020 American Community Survey, defined as anyone not residing in an urbanized area of 50,000 people or more, or an urban cluster of at least 2500 and less than 50,000
Fig. 2.
Predicted probability of offering telehealth, year*rurality interaction. Notes: Models adjusted for facility owner type, health department licensure, CARF accreditation, and integrated primary care; year*rurality interaction difference in slopes p < 0.0001 for both models
Discussion
Telehealth has historically been focused on strengthening health systems in rural areas. We found that growth in telehealth availability was fastest among more urban states, and this trend was observed in the years before and early in the COVID-19 pandemic. By 2020, we observed a convergence in telehealth availability such that there was little discernable difference in telehealth between mental health treatment facilities in more rural versus more urban states. We recommend future research to identify how or whether telehealth continues to make headway in urban states as more annual data becomes available.
The use of telehealth is growing in urban areas as lessons learned from rural experiences are adapted by a wider range of facilities and providers. Strengthening telehealth systems for behavioral healthcare in urban areas should be a public health priority as the nation considers how to sustain pandemic-era programs and funding. Some policies outlined in the COVID-19 public health emergency have been authorized to be extended through 2024 [32]. Medicare flexibilities and changes in Medicaid coverage and reimbursement for telehealth were integral in encouraging providers to adopt telehealth in uncertain times [33, 34]. We point specifically to the importance of the expansion of Medicaid telehealth coverage targeting the most vulnerable and marginalized US populations, with all 50 states now covering primary care and behavioral health services delivered through telehealth [35]. While many behavioral health Medicare policies were made permanent through the Consolidated Appropriations Act of 2021 [18], some aspects of the mid- and long-term sustainability of current telehealth trends remain in question. A more telehealth-dependent future in the USA is likely, and policies are needed to help steer systems towards addressing the needs of high-risk and marginalized populations across geographies [36]. Heeding these calls for equity in telehealth policy is important; we found that telehealth in mental health treatment facilities has grown fastest in more urban states, which have unique health system needs that must be responsive to disproportionate burdens of concentrated poverty, trauma, environmental exposures, and exposure to the criminal justice system [37]. Telehealth policy and changes to behavioral healthcare systems must account for the changing demographics of telehealth utilizers. In addition, telehealth has been a major focus of health system strengthening in rural areas for much longer than it has been in urban areas. This is reflected in our findings, such that telehealth was more prevalent in rural areas, but the pace of growth—or incidence—was faster in urban areas. In this context, telehealth had more room to expand and may have been more of a novel solution to urban healthcare problems in recent years. The intense and prolonged national focus on telehealth during the PHE occurred across geographies, and rural areas may have had less to gain from the rapid scale-up of a new technology. This context of differences in the starting points between rural and urban areas is an important piece of the telehealth narrative in the USA.
We identified wide state variation in telehealth availability in mental health treatment facilities. Some strategies employed by states that demonstrated large increases in telehealth (RI, + 86% points; OR, + 76%; NJ, + 74%) may be useful if adapted and tailored to the needs of states that demonstrated the smallest increases in telehealth (VT, + 15% points; KY, + 16%; SC, + 21%). Although state-level policies were beyond the scope of this study, acknowledging state policy differences can help contextualize our findings and may provide inspiration for future studies. The content of the following anecdote was not incorporated as part of our study design, but through describing one state policy we may highlight the need for more in-depth analyses of specific policies as they relate to mental health and telehealth. For example, minimizing the amount of oversight or co-signing required by physicians for telehealth visits provided by nurse practitioners is one strategy to broaden the clinical telehealth workforce. A report by the Reason Foundation [19] ranked states from best to worst in terms of telehealth practices, including whether they allowed nurse practitioners to practice fully independently without a collaborative practice agreement or supervision from a physician (best, 20 states), allowed nurse practitioners to practice independently after a certain period of time or required limited physician supervision (moderate, 11 states), or never allowed nurse practitioners to practice independently without a collaborative practice agreement or physician supervision (worst, 19 states). In relation to our findings, the three states with the fastest telehealth growth between 2015 and 2020 (RI, OR, NJ) were all ranked as implementing best nurse practitioner telehealth practices. Conversely, the three states identified with the slowest telehealth growth (VT, KY, SC) were ranked as moderate or worst. This post hoc anecdote is useful when considering upstream factors driving telehealth availability in mental health treatment settings and suggests that future policy research is warranted.
Limitations
We used US Census data to define the percentage of state residents living in a rural area. The Census overcounted people in rural areas (as well as some other populations), known as coverage error. However, in the 2020 decennial census, there was not a statistically significant overcount or undercount for the total population [38]. An overcount could potentially bias our results, such that some rural states may have larger urban populations than were reported in the Census data.
The N-MHSS definition of “telemedicine/telehealth therapy (including internet, web, mobile, and desktop programs)” is broad and encompasses a wide range of potential telehealth services. The annual survey is completed by an individual delegated by the facility, and responses to what qualifies as telehealth may vary between respondents. For example, a respondent could conceivably endorse this question when considering self-guided web-based modules about addiction, which is outside of the scope of how we are conceptualizing telehealth in this study to be live interactions with providers addressing issues of behavioral health. While such responses are likely outliers, this would potentially overestimate telehealth availability. There is also no variable in N-MHSS that indicates the frequency or magnitude of telehealth services offered. Telehealth for specialized or intermittent/monthly care is not relevant to the general population seeking mental health services, but may have been included in some respondent’s definitions.
Conclusion
Telehealth availability grew the fastest in more urban states since 2015, and this trend held true in models with and without data from 2020. Telehealth availability also grew at a slower rate in more rural states. The pace of growth varied widely between states, with several states demonstrating all or nearly all mental health treatment facilities offering telehealth by 2020, while several other states demonstrated rates substantially below the national average. Given the notable telehealth growth in urban states, health systems and new interventions must consider the unique challenges faced by urban populations and how best practices may be adapted to meet the growing urban demand. Telehealth as a strategy to strengthen rural mental health systems remains important, however, as populations across all geographies may benefit from increased access to a critical healthcare resource.
Acknowledgements
This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of award U3GRH40001 to the Rural Telehealth Research Center. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS, or the U.S. government. For more information please visit HRSA.gov.
Data Availability
The Nationa Mental Health Services Survey is available online for free for public use through the Substance Abuse and Mental Health Services Administration. A link to the data files and codebooks is below: https://www.datafiles.samhsa.gov/dataset/national-mental-health-services-survey-2020-n-mhss-2020-ds0001.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Edlund M, Unutzer J, Curran G. Perceived need for alcohol, drug, and mental health treatment. Soc Psychiatry Psychiatr Epidemiol. 2006;41:480–487. doi: 10.1007/s00127-006-0047-1. [DOI] [PubMed] [Google Scholar]
- 2.Green J, McLaughlin K, Fillbrunn M, et al. Barriers to mental health service use and predictors of treatment drop out: racial/ethnic variation in a population-based study. Administration and Policy in Mental Health and Mental Health Services Research. 2020;47:606–616. doi: 10.1007/s10488-020-01021-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolin J, Bellamy G, Ferdinand A, et al. Rural Health People 2020: new decade, same challenges. J Rural Health. 2015;31(3):326–333. doi: 10.1111/jrh.12116. [DOI] [PubMed] [Google Scholar]
- 4.Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–1678. doi: 10.2105/AJPH.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Health Resources and Services Administration. Designated Health Professional Shortage Areas statistics. First quarter of fiscal year 2023, designated HPSA quarterly summary. Rockville, MD. HRSA, Bureau of Health Workforce. 2023. https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport. Accessed 30 Aug 2023.
- 6.United States Centers for Disease Control and Prevention. About Rural Health. U.S. Department of Health & Human Services. Updated May 9, 2023. Accessed 30 Aug 2023.
- 7.Morales D, Barksdale C, Beckel-Micthener A. A call to action to address rural mental health disparities. Journal of Clinical and Translational Science. 2020;4(5):463–467. doi: 10.1017/cts.2020.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh G, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969-2009. Am J Preven Med. 2014;46(2):e19–e29. doi: 10.1016/j.amepre.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Cyr M, Etchin A, Guthrie B, Benneyan J. Access to specialty healthcare in urban versus rural US populations: a systematic literature review. BMC Health Serv Res. 2019;19(974):1–17. doi: 10.1186/s12913-019-4815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel S, Huskamp H, Busch A, Megrotra A. Telemental health and US rural-urban differences in specialty mental health use, 2010–2017. Am J Public Health. 2020;110(9):1308–1314. doi: 10.2105/AJPH.2020.305657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cantor J, McBain R, Kofner A, Hanson R, Stein B, Yu H. Telehealth adoption by mental health and substance use disorder treatment facilities in the COVID-19 pandemic. Psychiatr Serv. 2021;73(4):411–417. doi: 10.1176/appi.ps.202100191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bogue-Kawaii B, Williams N, MacNear K. Mental health care access and treatment utilization in African American communities: an integrative care framework. Ingenta Connect. 2017;13(2):11–29. [Google Scholar]
- 13.Myers C. Using telehealth to remediate rural mental health and healthcare disparities. Issues Ment Health Nurs. 2019;40(3):233–239. doi: 10.1080/01612840.2018.1499157. [DOI] [PubMed] [Google Scholar]
- 14.Bulkes N, Davis K, Kay B, Riemann B. Comparing efficacy of telehealth to in-person mental health care in intensive-treatment-seeking adults. J Psychiatr Res. 2022;145:347–352. doi: 10.1016/j.jpsychires.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levinson C, Spoor S, Keshishian A, Pruitt A. Pilot outcomes from a multidisciplinary telehealth versus in-person intensive outpatient program for eating disorders during versus before the COVID-19 pandemic. Int J Eat Disord. 2021;54(9):1672–1679. doi: 10.1002/eat.23579. [DOI] [PubMed] [Google Scholar]
- 16.Whaibeh E, Mahmoud H, Naal H. Telemental health in the context of a pandemic: the COVID-19 experience. Curr Treat Options Psych. 2020;7:198–202. doi: 10.1007/s40501-020-00210-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beschloss A, Van Ramshorst R, Bachireddy C, Chen C, Ostrovsky A. New coding modifier offers opportunity to investigate audio-only telehealth. Health affairs forefront blog. November 18, 2022. https://www.healthaffairsorg/content/forefront/new-coding-modifier-ffers-opportunity-investigate-audio-only-telehealth. Accessed 30 Aug 2023.
- 18.Consolidated Appropriations Act, 2021. H.R. 133. 116th Congress (2019-2020). House foreign relations committee. Senate foreign relations committee. Public Law No. 116-260. Accessed 30 Aug 2023.
- 19.Archambault J, Nastasi V. Rating the states on telehealth best practices: a toolkit for a pro-patient and provider landscape. Expanded February 10, 2022. The Reason Foundation Los Angeles, CA. https://www.reasonorg/wp-content/uploads/rating-states-on-telehealth-best-practicespdf. Accessed 30 Aug 2023.
- 20.Neri A, Whitfield G, Umeakunne E, et al. Telehealth and public health practice in the United States - Before, during, and after the COVID-19 pandemic. Public Health Manag Pract. 2022;28(6):650–656. doi: 10.1097/PHH.0000000000001563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen J, Amaize A, Barath D. Evaluating telehealth adoption and related barriers among hospitals located in rural and urban areas. J Rural Health. 2020;37(4):801–811. doi: 10.1111/jrh.12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bagchi A, Damas K, Salazar de Noguera N, et al. Comfort with telehealth among residents of an underserved urban area. J Prim Care Commun Health. 2022;13:215013192211196. doi: 10.1177/21501319221119692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Auxier B, Anderson M. As schools close due to the coronavirus, some U.S. students face a digital ‘homework gap’. Pew Research Center. Research Topics - Coronavirus (COVID-19). March 16, 2020. Washington, D.C. 2020; Sourced from: https://www.pewresearch.org/fact-tank/2020/03/16/as-schools-close-due-to-the-coronavirus-some-u-s-students-face-a-digital-homework-gap/. Accessed 30 Aug 2023.
- 24.Porter E. A rural-urban broadband divide, but not the one you think of. The New York Times. Business section. Published on June 1, 2021. Sourced from: https://www.nytimes.com/2021/06/01/business/rural-urban-broadband-biden.html. Accessed 30 Aug 2023.
- 25.Rogers E. Diffusion of innovations. 5. New York, NY: Free Press; 2003. [Google Scholar]
- 26.Boushey G. Policy diffusion dynamics in America. New York, NY: Cambridge University Press; 2010. [Google Scholar]
- 27.Dearing J, Cox J. Diffusion of innovations theory, principles, and practice. Health Aff. 2018;37(2):183–190. doi: 10.1377/hlthaff.2017.1104. [DOI] [PubMed] [Google Scholar]
- 28.Substance Abuse and Mental Health Services Administration . National Mental Health Services Survey (N-MHSS): 2020. Data on Mental Health Treatment Facilities Rockville, MD: Substance Abuse and Mental Health Services Administration; 2020. [Google Scholar]
- 29.United States Census Bureau. Urban and Rural. US Census Bureau Geography Program. Guidance for Geography Users. 2023. Sourced from: https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural.html. Accessed 30 Aug 2023.
- 30.SAS/STAT Inc. SAS Version 9.4. Cary, North Carolina, USA.
- 31.University of California at Los Angeles Office of advanced research computing. Analyzing and visualizing interactions in SAS. UCLA OARC statistical methods and data analytics. section 7 - Logistic regression and comparing simple odds ratios and interpreting exponentiated interaction coefficients. 2023. Sourced from https://stats.oarc.ucla.edu/sas/seminars/analyzing-and-visualizing-interactions/ Accessed 30 Aug 2023.
- 32.Health Resources and Services Administration (HRSA). Telehealth policy changes after the COVID-19 public health emergency. Information for providers. Update on the telehealth flexibilities during the COVID-19 public health emergency. 2023. Sourced from: https://telehealth.hhs.gov/providers/policy-changes-during-the-covid-19-public-health-emergency/policy-changes-after-the-covid-19-public-health-emergency. Accessed 30 Aug 2023.
- 33.Schofield M. Regulatory and legislative issues on telehealth. Nutr Clin Pract. 2021;36(4):729–738. doi: 10.1002/ncp.10740. [DOI] [PubMed] [Google Scholar]
- 34.Brotman J, Kotloff R. Providing outpatient telehealth services in the United States: before and during coronavirus disease 2019. Educ Clin Pract: CHEST Rev. 2021;159(4):1548–1558. doi: 10.1016/j.chest.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chu R, Peters C, De Lew N, Sommers B. State Medicaid telehealth policies before and during the COVID-19 public health emergency. US Department of Health and Human Services. Office of Health Policy. Issue Brief, July 2021, No. HP-2021–17. 2021. Sourced from: https://aspe.hhs.gov/sites/default/files/documents/eb9e147935a2663441a9488e36eea6cb/medicaid-telehealth-brief.pdf. Accessed 30 Aug 2023.
- 36.Shaver J. The state of telehealth before and after the COVID-19 pandemic. Prim Care. 2022;49(4):517–530. doi: 10.1016/j.pop.2022.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Academies of Sciences, Engineering and Medicine. Communities in Action: Pathways to health equity. The state of health disparities in the United States. NASEM Board on population health and public health practice, committee on community-based solutions to promote heatlh equity in the United States. National Academies Press. 2017. Sourced from: https://www.ncbi.nlm.nih.gov/books/NBK425844/. Accessed 30 Aug 2023.
- 38.Jensen E, Kennel T. Who was underconted, overcounted in the 2020 census? Detailed coverage estimates for the 2020 census released today. United States Census Bureau. March 10, 2022. Sourced from: https://www.census.gov/library/stories/2022/03/who-was-undercounted-overcounted-in-2020-census.html. Accessed 30 Aug 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The Nationa Mental Health Services Survey is available online for free for public use through the Substance Abuse and Mental Health Services Administration. A link to the data files and codebooks is below: https://www.datafiles.samhsa.gov/dataset/national-mental-health-services-survey-2020-n-mhss-2020-ds0001.