Abstract
Background
With ongoing gaps in obesity education delivery for health professions in Canada and around the world, a transformative shift is needed to address and mitigate weight bias and stigma, and foster evidence-based approaches to obesity assessment and care in the clinical setting. Obesity Canada has created evidence-based obesity competencies for medical education that can guide curriculum development, assessment and evaluation and be applied to health professionals' education programs in Canada and across the world.
Methods
The Obesity Canada Education Action Team has seventeen members in health professions education and research along with students and patient experts. Through an iterative group consensus process using four guiding principles, key and enabling obesity competencies were created using the 2015 CanMEDS competency framework as its foundation. These principles included the representation of all CanMEDS Roles throughout the competencies, minimizing duplication with the original CanMEDS competencies, ensuring obesity focused content was informed by the 2020 Adult Obesity Clinical Practice Guidelines and the 2019 US Obesity Medication Education Collaborative Competencies, and emphasizing patient-focused language throughout.
Results
A total of thirteen key competencies and thirty-seven enabling competencies make up the Canadian Obesity Education Competencies (COECs).
Conclusion
The COECs embed evidence-based approaches to obesity care into one of the most widely used competency-based frameworks in the world, CanMEDS. Crucially, these competencies outline how to address and mitigate the damaging effects of weight bias and stigma in educational and clinical settings. Next steps include the creation of milestones and nested Entrustable Professional Activities, a national report card on obesity education for undergraduate medical education in Canada, and Free Open Access Medication Education content, including podcasts and infographics, for easier adoption into curriculum around the world and across the health professions spectrum.
Keywords: Obesity, Education, Medicine, Canada
1. Introduction
In 2010, Lancet's landmark independent commission on health professionals' education outlined how the redesign of health professionals' education programs around the world would need to be transformative to address priority health needs both within and between countries [1]. They defined transformative learning as the highest possible level of learning, with the goal of producing enlightened change makers for healthcare systems around the world [1]. Developed from a global vision and strategy for health professionals' education by representatives from diverse countries and fields, the Commission adopted a comprehensive framework with both instructional and institutional reforms in mind. Instructional reforms included the adoption of competency-driven approaches, promotion of interprofessional education, and development of stronger educational resources for transformative learning to occur [1]. As a chronic disease, obesity healthcare is complex, is fraught with bias, and is limited by simplistic definitions that focus solely on Body Mass Index (BMI) [2]. Addressing this priority health need will require a transformative shift in educational approaches that confront weight bias and stigma at all levels of healthcare and are patient-centered in nature, as reflected in the Canadian Obesity Clinical Practice Guidelines (CPGs) [3]. Regarding obesity training for physicians, there is no currently available roadmap for medical education curricula that not only incorporates the aforementioned transformative learning reforms outlined by the Lancet Commission but also the latest clinical practice guidelines for obesity care. Such a roadmap would rely on a competency-based approach to education, which in medicine is known as Competency Based Medical Education (CBME).
Defined by its orientation to graduate outcome abilities and organized around competencies derived from both societal and patient needs [4], this method of instruction is mainstream in many medical education institutions worldwide [5]. Despite its criticisms [6,7], CBME continues to evolve over time in some important areas, including the introduction of Entrustable Professional Activities (EPA) and milestones [8,9] to help bridge the gap between the theory of CBME and its implementation into clinical practice.
The recent 2019 Obesity Competencies for Medical Education by the Obesity Medicine Education Collaborative (OMEC), based on the Accreditation Council for Graduate Medical Education (ACGME) competency framework [10], provided a crucial stepping stone for obesity education that arose from gaps in medical education training in the US. The ACGME competency framework, however, is limited in its use to US medical education institutions, and when compared to the Royal College of Physicians and Surgeons of Canada CanMEDs framework for physicians, this has limited application to other health professionals' education programs both locally and internationally [11]. The CanMEDS framework is divided into seven roles (Medical Expert, Communicator, Collaborator, Professional, Scholar, Leader, and Health Advocate), with CBME delivery in Canada focusing on key and enabling Competencies as well as milestones.
Key competencies are defined as essential abilities within each of the seven CanMEDS roles, while an enabling competency represents an essential component of its key competency, which, in concert with other enabling competencies, describes the overall key competency in greater detail. Further, CanMEDS milestones are educational statements that illustrate the progression of the clinician's competence from novice to mastery of a particular enabling competency [12]. Key and enabling competencies, along with their associated milestones, are difficult to measure in clinical environments, which is why in recent years, the development of EPAs has helped to bridge the gap between theory and practice by defining specific tasks to be entrusted to learners to perform independently [13]. EPAs translate competencies from multiple CanMEDS roles into clinical practice and are usually training program-specific (i.e. EPAs for a residency program in pediatrics would differ from those seen in an orthopedics program) [12]. Learners are provided an opportunity to complete these tasks during training and are observed by preceptors, allowing for assessment and feedback to occur simultaneously. EPAs are then recorded in a portfolio, in which learners can review the information for future encounters. The Assessment or Competency Committee then uses EPAs to make decisions about the advancement of learners to the next stage of training.
In Canada, foundational undergraduate training EPAs are available through the Association of Faculties of Medicine of Canada (AFMC) and are adapted at most institutions to inform clinical assessments of clerkship students. They are mapped to the existing CanMEDS Roles and incorporate multiple different competencies [14]. EPAs are also present in most Canadian postgraduate medical education training programs through the Competence by Design initiative [15]. One of the benefits of using EPAs in obesity education is that specialty-specific, or “nested”, EPAs can be created based on the CanMEDS framework and evidence-based clinical practice guidelines [16]. In obesity care, the widely adopted CPGs provide an evidence-based summary of obesity care that not only encourage a comprehensive approach to the interprofessional management of patients living with obesity, but also usher in a transformative change to clinical practice through the integration of patient experience. This CPG highlights an important, patient-driven context for any obesity education competency, including the need to recognize and address the damaging effects of obesity bias and stigma, and promote patient-focused obesity care [3]. A truly transformative set of obesity education competencies that not only incorporates a patient-focused approach to obesity care, but also transcends interprofessional boundaries and embraces the evolving benefits of CBME is therefore required. In this paper, we, as members of the Obesity Canada Education Action Team, set out the process by which these new educational competencies in obesity care, titled the Canadian Obesity Education Competencies (COECs), were created. The COECs can act as a standalone set of competencies for educational programs and institutions, although it best serves as a complement to the existing CanMEDS framework for graduating clinicians in health professions. We also present steps on how these competencies can be applied to curriculum development and assessment across Canadian institutions. This will be accomplished using the CanMEDs framework through both nested EPAs and innovative educational resources, specifically addressing how competencies can be translated across the health professionals’ education spectrum globally to address disparities in obesity care.
2. Methods
As Canada's largest registered charity dedicated to improving obesity care, Obesity Canada is working towards the development of a national obesity care framework focused on four pillars: Education, Research, Policy, and Community. As part of the education pillar, the Education Action Team was tasked with the development of an updated set of competencies for obesity education in medical education that could be translated more broadly into other health professions. The objectives of the group were to identify gaps and opportunities while developing recommendations for advancing health professionals' education in obesity in Canada, and work towards collaboratively developing standards of care for obesity to health professionals at national and international levels. Table 1 provides a summary of key terms and acronyms.
Table 1.
Acronyms.
| Body Mass Index | BMI |
|---|---|
| Canadian Obesity Education Competencies | COEC |
| Canadian Obesity Clinical Practice Guidelines | CPGs |
| Competency-Based Medical Education | CBME |
| Entrustable Professional Activities | EPA |
| International Medical Education Collaboration on Climate and Sustainability | IMMCCS |
| Obesity Medicine Education Collaborative | OMEC |
| Accreditation Council for Graduate Medical Education | ACGME |
| Association of Faculties of Medicine of Canada | AFMC |
| Free Open Access Medical education | FOAM |
| Open Education Resources | OERs |
| Quality Improvements | QI |
| Ask, Assess, Advise, Agree, Assist | 5As |
The Obesity Education Action Team was created in November 2021 and is composed of Obesity Canada members from multiple health professions, including medicine, dietetics, nursing, occupational therapy, and psychology, research faculty across the country and patient and community representatives. Members of the committee were selected based on their previous experience in teaching obesity care in health professionals’ education programs, their experience in writing competencies (47 %) and their involvement with the 2020 CPGs (50 %). Representation occurred in 4 Canadian provinces and one U.S. representative with leadership experience in the creation of the OMEC competencies. Seventy-six percent of the team consisted of academic faculty members, with clinical faculty, learners, and patient representatives comprising the remaining members. Team members met regularly via web-based videoconferencing calls from November 2021 to March 2023 and collaborated during these calls and through web-based shared documents.
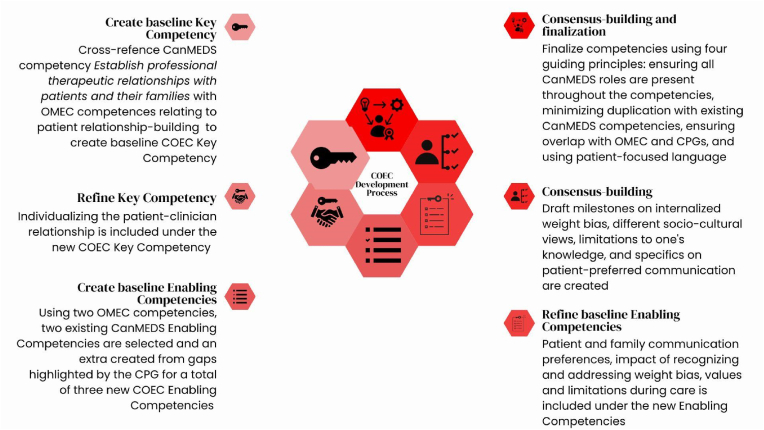
The Canadian Obesity Education Competencies represent obesity-focused key and enabling competencies based on the 2015 CanMEDS Competency Framework [17]. First, the group analyzed the overall 2015 CanMEDS Competency Framework and MD program competencies at two Canadian institutions [18,19] and cross-referenced them with the OMEC competencies to create a baseline set of key competencies that were relevant to obesity care across the medical education spectrum. These baseline key competencies in the COECs were drawn from existing CanMEDS competencies, albeit with changes to their description to reflect obesity-specific care. Next, the focus shifted to tailoring these key competencies to obesity-specific care by filling in gaps with specific elements from the OMEC competencies and CPGs. Enabling competencies were then completed in a similar manner, with the only difference being that if a gap in obesity care was felt to be too large, a new enabling competency would be created. Specific wording of the competencies relied on existing language from the OMEC Competencies, the 2015 CanMEDS framework, and Bloom's Revised Taxonomy [20]. Finally, consensus building occurred in two steps. The first step involved creating draft milestones for each of the enabling competencies to simulate the various benchmarks expected of trainees at different levels of medical training. Although the milestones themselves have yet to be finalized, the process of crafting draft examples facilitated group discussion towards the creation of a comprehensive set of key and enabling competencies. The second step of consensus building occurred simultaneously through iterative refinement of the competencies with group discussion by following four guiding principles: ensuring that all CanMEDS Roles were captured in the competencies, minimizing duplication of existing CanMEDS competencies unless relevant to obesity care, ensuring sufficient overlap in content with both OMEC competencies and the 2020 CPGs, and emphasizing patient-focused language in all competencies. An example of key competency #4 and its associated enabling competencies is shown in Fig. 1. The creation of these competencies did not require ethics board approval.
Fig. 1.
Development of Canadian Obesity Education Competencies (COEC) Key Competency 4 - Establish personalized relationships with patients with obesity and their families.
3. Results
The Canadian Obesity Education Competencies are presented as 13 key competencies and 37 enabling competencies in Table 2.
Table 2.
CanMEDS Roles and associated Obesity-Focused Key and Enabling Competencies.
| Medical Expert Role |
| Key competency #1: Apply medical knowledge and professional values to the provision of patient centered obesity care |
|
|
| Key Competency #2: Perform and document a comprehensive, obesity-focused, patient-centered clinical assessment |
|
|
|
|
| Key competency #3: Co-construct a comprehensive, obesity-focused management plan with the patient and family |
|
|
|
|
|
|
|
| Communicator Role |
| Key competency #4: Establish personalized relationships with patients with obesity and their families |
|
|
|
| Key competency #5: Engage with patients and families to create individualized plans through shared-decision making in obesity care |
|
|
| Collaborator Role |
| Key competency #6: Collaborate effectively with other colleagues and trainees in the health professions to provide care for individuals living with obesity |
|
|
| Leader Role |
| Key competency #7: Contribute to the improvement of obesity care delivery in teams, organizations, and systems |
|
|
| Advocate Role |
| Key competency #8: Respond to the individual needs of a patient with obesity by advocating with the patient within the clinical environment and beyond |
|
|
|
| Key competency #9: Respond to the needs of the patient population living with obesity by advocating collaboratively for system-level change |
|
|
| Scholar Role |
| Key competency #10: Engage in ongoing learning to enhance obesity care delivery to patients |
|
|
|
| Key competency #11: Teach junior and seniors colleagues, and colleagues in the health care professions around obesity care |
|
|
| Key competency #12: Integrate best available evidence on obesity care into clinical practice |
|
|
| Professional Role |
| Key competency #13: Demonstrate a commitment to patients by applying best practices of obesity care to all clinical settings and adhering to high ethical standards |
|
|
|
Denotes an enabling competency not seen in either the OMEC competencies or the 2015 CanMEDS framework.
CanMEDS framework.
As seen in Table 2, the COECs are organized using the seven CanMEDS Roles and represent a comprehensive set of observable abilities that designate competence in all areas of obesity care for a physician or healthcare professional. These competencies span the entire length of training, and will likely be subdivided into three or more stages (e.g. novice, intermediate, and expert) with soon to be released milestones designating the appropriate benchmarks to be obtained at these stages. Table 3 shows an example of three milestones for enabling competency 1.2, and reflects the types of benchmarks for completing this competency in a health professionals' education program. Key Competencies 6, 7, 10, 11, 12, and 13 had small changes made in description to address obesity education in comparison to the original CanMEDS wording, with only two to three associated enabling competencies. All other Key Competencies had larger descriptive changes from the existing CanMEDS competencies and contained anywhere from two to seven associated enabling competencies. Through the COEC development process, all of the OMEC competencies were integrated either in key or enabling competencies, or in draft milestones for future use. Enabling competencies 3.2 (i.e. assessment of mental health) and 4.1 (i.e. recognition of weight bias) were new competencies identified throughout the process that did not have any overlap with either the OMEC competencies or the 2015 CanMEDS Framework.
Table 3.
Example Milestones for Enabling competency 1.2: Demonstrate awareness of one's own personal weight bias and stigma in relation to obesity care.
| Novice | Intermediate | Expert |
|---|---|---|
| Demonstrate an understanding of weight bias, stigma, and discrimination and how they can present in the clinical environment | Recognize when one's own personal weight bias can impact obesity care in different clinical settings (pediatric, surgical, medicine, psychiatry, etc.) | Role-model effective reflection on one's own personal weight bias and its impacts on obesity care |
4. Discussion
The COECs represent a transformative leap in obesity education in that they define a comprehensive set of competencies that are based on the most widely adopted CBME framework in the world, and lay the groundwork for not only medical education but other health professions education programs to deliver evidence-based, patient-centered obesity care curricula that can inspire healthcare system change.
Adherence to an established CBME framework, the CanMEDS framework, was instrumental in creating a set of competencies, and all seven roles were successfully incorporated with key and enabling competencies. Having all CanMEDS Roles represented was the first guiding principle in the group's consensus building process and was important if the COECs were going to be used as a comprehensive set of competencies for any educational program or institution, regardless of their use of the CanMEDS framework. Despite having this broad representation of competencies, however, fewer competencies overall were encouraged as the second guiding principle of consensus building, in order for the COECs to be more easily adopted in institutions that use the CanMEDS framework. Although just under half of the key competencies were similar in wording to their original CanMEDS competencies, the number of associated enabling competencies was usually limited to a maximum of two or three in order to improve training programs' integration into curricula. In contrast, the rest of the key competencies had between two and seven enabling competencies. A smaller number of high quality competencies will ultimately facilitate adoption across multiple health professionals' education programs. The benefits of using OMEC competencies were apparent throughout the COECs development process, as they assisted in creating baseline key competencies, and informing many enabling competencies and draft milestones. All OMEC competencies were embedded into COECs as the third guiding principle for consensus building. Integration of the CPGs was another guiding principle for consensus building in the COECs development process, and this was apparent in several competencies. Recognizing and mitigating the effects of weight bias and stigma in the clinical setting and beyond spanned a wide range of CanMEDS Roles from Medical Expert to Scholar; these particular competencies highlight the importance of defining weight bias and stigma, recognizing and addressing their effects in the clinical setting, partnering with patients and families to recognize and address the effects of weight bias and stigma in all aspects of their care, and finally recognizing the influence of role-modeling has on weight bias and stigma when interacting with colleagues and learners from all professions. Furthermore, framing all the COECs in an updated definition of obesity that moves beyond BMI signifies an important step in reducing weight stigma in evidence based patient-centered obesity care. The negative health impacts of weight stigma are far reaching [21,22], hence the need for transformative changes to health professions education programs [3]. By outlining a comprehensive approach through multiple CanMEDS Roles, the COECs lay the groundwork for meaningful change to health professions curricula around weight bias and stigma, especially in the context of the important focus on health equity, inclusion and disability in current health professions curriculum reform [23]. Collaborating with patients towards patient-centered obesity care is also a hallmark of the CPGs, hence why multiple competencies encompass patient-centered concepts ranging from patient-focused clinical assessments, co-construction of management plans, personalized relationships to enhance communication, individualized discussions with patients and families around shared-decision making, and advocating with patients for local and system-wide changes. Patient-centered care has been shown to decrease healthcare system utilization and improve patient-centered outcomes [24], and therefore is needed more than ever in obesity care [25,26] and obesity education [27]. Similarly, the final guiding principle for consensus building was the use of patient-focused language in all of the competencies. Key competency 3, for instance, which describes management planning in obesity care, is intentional in replacing verbs seen in the CanMEDS framework such as “formulate” and “establish” with “co-construct” and “collaborate” to highlight the importance of patient-centered care and shared-decision making in management planning. Furthermore, a number of key competencies are careful in including both patients and families in their descriptions, to be inclusive of all patients who are seeking obesity care.
For educators and institutions that have already adopted the OMEC competencies for obesity education, we encourage that they view the COECs as complementary in nature. Although all of the obesity education content from the OMEC competencies are embedded within the COECs, there are still distinct areas in the latter worth highlighting for educators. Primarily, the COECs represent a shift towards appreciating and mitigating the broad impact that both weight bias and stigma have on obesity education in multiple different domains. Starting with the Medical Expert Role in the COECs, learners are asked to demonstrate an awareness of their own weight bias and how that can impact their overall care of patients through enabling competency 1.2. Teaching self-awareness through methods such as reflective journaling in undergraduate health professionals' education, for instance, has been shown to not only raise awareness of weight bias in healthcare professionals but also improve clinical competency in the area [28]. Through enabling competency 8.1 in the Advocate Role, learners are then asked to work with patients and families to not only recognize the effects of weight bias and stigma on their own care, but also on how to address them. The importance of mitigating weight bias and stigma in the clinical setting is seen in the OMEC competencies, but an emphasis on addressing patients’ internalized weight bias is also essential in obesity education as it has implications in overall obesity care [29], and would feature prominently in the future milestones for enabling competency 8.1. Finally, the Communicator Role, and specifically enabling competency 4.1, asks the learner to develop personalized relationships with patients and their families in obesity care by recognizing and addressing weight bias and stigma. The 5As approach, which acts as the foundation for the patient-focused obesity assessment in the CPGs, showcases how co-creation of goals and a strengths-based approach can mitigate internalized weight bias and personalize the relationship between the patient and their provider [30]. Highlighting both mental health and psychological health in obesity management planning is the second major difference between the OMEC competencies and the COECs, as seen in enabling competency 3.2. Mental health in obesity management is particularly important to mention in obesity education, as learners must be aware of how mental illness can impact obesity management efforts, how side-effects of medications used in the treatment of mental illness can impact obesity care, and how pharmacological, surgical, and behavioural therapies are influenced by mental illness [3]. Psychological health in obesity management, on the other hand, focuses on psychological factors that mediate obesity and well-being, such as distress over obesity, negative thoughts, low self-esteem, and poorer perceived health [31]. By considering these factors, learners can begin to collaborate with patients in setting achievable and realistic goals [32].
The COECs now look towards adoption into curriculum and assessment as they strive towards transformative change in our institutions. The strengthening of educational resources is especially relevant to that change on a global level [1], and so a portable curriculum of easily accessible content made available through innovative technology is needed. Free Open Access Medical education (FOAM) represents the medical education community's response to the broader trend towards open educational resources (OERs), and generally comprises various types of digital content in the forms of blogs, podcasts and infographics to relay information to learners [31]. In order to break down institutional and interprofessional silos, the dissemination of COEC related curricular content will occur in a similar fashion. Challenges with implementation at different institutions necessitates an approach to overcome common institutional barriers, the most significant being addition of COEC related content to an already full curriculum. A six-step implementation model used for Planetary Health medical curriculum in the US offers up a possible framework to address this barrier. The International Medical Education Collaboration on Climate and Sustainability (IMECCS) Model highlights Identification, Infusion, Implementation, Evaluation, Improvement, and Reinforcement as the important steps to efficiently integrate curriculum [33]. The Identification and Implementation phases mirror the efforts currently underway and/or planned by the Obesity Canada Education Action Team. These include compiling a list of relevant learning outcomes through competencies, auditing a school's existing curriculum based on those outcomes with the development of a report card, identifying gaps in the curriculum related to obesity care, and then infusing COEC related curricular content in the form of OERs to complement or replace existing modules with the assistance of participating instructors and course coordinators. An organization like Obesity Canada is already well equipped for part of this delivery, having provided various open access resources for the CPGs after their release in 2020, and having led the creation of the COECs. Nested EPAs will represent the cornerstone for assessment of the COECs, given the adoption of EPAs in most Canadian postgraduate medical education training programs and many undergraduate health professionals' education programs across the world [34]. Again, the distinction between competencies and EPAs is important, yet often confusing. Whereas a competency represents the ability of a health professional in a particular domain or role, an EPA is an essential task, made up of several different competencies of a particular discipline, that a learner is trusted to perform independently in a specific health care setting and when sufficient competence has been demonstrated [35]. Nested EPAs are tasks that require proficiency in a subset of the knowledge, skills, and attitudes required for the broader EPA [35] and could be tailored to obesity care based on the COECs. In the case of undergraduate medical education in Canada, there are already 12 Core EPAs that exist [14], and therefore COEC-informed nested EPAs would offer easy adoption into assessment delivery across the country around obesity education. Similar adoption could occur in other health professionals' education programs around the world where EPAs are readily used for assessment, with Obesity Canada's experience in adapting the CPGs in South America and Europe [36,37] demonstrating its capability in accomplishing a similar task.
Renewal is essential to the COECs, as the evolving clinical environment for health professionals requires consistent updates to education competencies. CanMEDS is planning for major updates in the next few years with emerging concepts in Planetary Health, Equity, Diversity, and Inclusion, Anti-Racism, Humanism, Virtual Care, Clinical Learning Environment, Adaptive Expertise, Complex Adaptive Systems, Data-Informed Medicine, and Clinical Reasoning for the next iteration, CanMEDS 2025 [23]. Likewise, the CPGs have already undergone renewal in the areas of medical nutrition therapy and pharmacotherapy in 2022 [3]. Update of the COECs based on changes in both of these frameworks will be essential to the longevity of the competencies.
There are a few important limitations to highlight regarding the methodology. In health professionals' education, the Delphi methodology is typically used to secure a finalized set of competencies, allowing for anonymity of the participants and multiple iterations of feedback to reach consensus in a coordinated fashion [38]. In the construction of the COECs, however, it became clear that a sufficient sampling of obesity education experts with the requisite expertise in both CBME and the CanMEDS framework outside of the members of the Obesity Education Action Team was lacking. To encourage anonymity within the group, participants were able to provide feedback anonymously through web-based shared documents and to Obesity Canada administrative staff, and the COEC guiding principles assisted in the iterative consensus building of competencies during the development process. Another important limitation to highlight is the lack of finalized milestones for the COECs at this current time. Although crucial to the full adoption of the competencies into health professionals' education curriculum, the key and enabling competencies on their own can still serve as a foundation for broad curricular change in obesity education, including the development of obesity education evaluation tools for medical education, such as report cards. Nested EPAs can also be created without the completion of milestones, meaning that work can begin in this important area of assessment for schools who are looking towards transformative change in obesity education.
5. Conclusion
The COECs represent a critical step forward in obesity education delivery by adapting the most widely used competency framework for medical education in the world and grounding it both in the OMEC obesity-focused competencies and the Canadian Obesity CPGs. Not only does this lay a path forward for innovative curriculum and assessment delivery through Open Educational Resources (OERs) and Entrustable Professional Activities (EPAs), respectively, but it also represents a shift to an internationally adopted curriculum in obesity care. Obesity Canada's Education Action Team will continue to work towards establishing a comprehensive set of milestones and OERs for various stages of training, nested EPAs for assessment, and consistent renewal based on evolving changes in CBME and obesity care. Additional studies on the use and implementation factors facilitating the integration of the COECs into existing training curricula will be needed to support the widespread adoption of these competencies across health professionals' education.
Authorship statement
In the development of the competencies, JRA and NP initiated the conceptualization. JRA conceptualized the methodology. All authors drafted, edited and finalized the competencies. The development of the paper was initially drafted by JRA. JRA, TSN, NP, KKD, MEH, MF, SH, RH, RFK, DLB, MM, SN, HPV, MV, SW, DW and SS all reviewed, edited and approved the final paper. RFK participated as a representative of the Obesity Medicine Education Collaborative.
Declaration of use of artificial intelligence
During the preparation of this work the authors did not use AI-assisted technologies.
Funding
Funding came from Obesity Canada's Fund for Obesity Collaboration and Unified Strategies (FOCUS) initiative in addition to in-kind support from the scientific and professional volunteers engaged in the process. There was no external funding provided for this research.
Ethical review
Ethical review was not required.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: The authors declare no conflict of interest. Nicole Pearce is an employee of Obesity Canada. Sanjeev Sockalingam is the Scientific Director of Obesity Canada. Mary Forhan is the past Scientific Director of Obesity Canada. All authors are volunteer members of Obesity Canada’s Education Committee.
Acknowledgements
The authors would like to thank Michelle McMillan for providing invaluable contributions to the team and this project with her lived-experience perspective and experience.
Contributor Information
Joseph Abraham Roshan, Email: jrabraha@ualberta.ca.
Taniya S. Nagpal, Email: tnagpal@ualberta.ca.
Nicole Pearce, Email: pearce@obesitynetwork.ca.
Khushmol K. Dhaliwal, Email: khushmol@ualberta.ca.
Mohamed El-Hussein, Email: melhussein@mtroyal.ca.
Mary Forhan, Email: mary.forhan@utoronto.ca.
Stasia Hadjiyanakis, Email: shadjiyannakis@cheo.on.ca.
Raed Hawa, Email: raed.Hawa@uhn.ca.
Robert F. Kushner, Email: rkushner@northwestern.edu.
Dayna Lee-Baggley, Email: dayna.lee-baggley@dal.ca.
Michelle McMillan, Email: mlym@shaw.ca.
Sarah Nutter, Email: snutter@uvic.ca.
Helena Piccinini-Vallis, Email: helena.piccinini@dal.ca.
Michael Vallis, Email: tvallis@dal.ca.
Sean Wharton, Email: sean@whartonmedicalclinic.com.
David Wiljer, Email: David.Wiljer@uhn.ca.
Sanjeev Sockalingam, Email: sanjeev.sockalingam@camh.ca.
References
- 1.Frenk J., Chen L., Bhutta Z.A., Cohen J., Crisp N., Evans T., et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The lancet. 2010;376:1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 2.Sharma A.M., Campbell-Scherer D.L. Redefining obesity: beyond the numbers. Obesity. 2017;25:660. doi: 10.1002/oby.21801. [DOI] [PubMed] [Google Scholar]
- 3.Wharton S., Lau D.C., Vallis M., Sharma A.M., Biertho L., Campbell-Scherer D., et al. Obesity in adults: a clinical practice guideline. CMAJ (Can Med Assoc J) 2020;192:E875–E891. doi: 10.1503/cmaj.191707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frank J.R., Mungroo R., Ahmad Y., Wang M., De Rossi S., Horsley T. Toward a definition of competency-based education in medicine: a systematic review of published definitions. Med Teach. 2010;32:631–637. doi: 10.3109/0142159X.2010.500898. [DOI] [PubMed] [Google Scholar]
- 5.Ten Cate O. Competency-based postgraduate medical education: past, present and future. GMS journal for medical education. 2017;34 doi: 10.3205/zma001146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hodges B. Medical education and the maintenance of incompetence. Med Teach. 2006;28:690–696. doi: 10.1080/01421590601102964. [DOI] [PubMed] [Google Scholar]
- 7.Brightwell A., Grant J. Competency-based training: who benefits? Postgrad Med. 2013;89:107–110. doi: 10.1136/postgradmedj-2012-130881. [DOI] [PubMed] [Google Scholar]
- 8.Ten Cate O., Scheele F. Competency-based postgraduate training: can we bridge the gap between theory and clinical practice? Acad Med. 2007;82:542–547. doi: 10.1097/ACM.0b013e31805559c7. [DOI] [PubMed] [Google Scholar]
- 9.Frank J.R., Snell L.S., Cate O.T., Holmboe E.S., Carraccio C., Swing S.R., et al. Competency-based medical education: theory to practice. Med Teach. 2010;32:638–645. doi: 10.3109/0142159X.2010.501190. [DOI] [PubMed] [Google Scholar]
- 10.Kushner R.F., Horn D.B., Butsch W.S., Brown J.D., Duncan K., Fugate C.S., et al. Development of obesity competencies for medical education: a report from the Obesity Medicine Education Collaborative. Obesity. 2019;27:1063–1067. doi: 10.1002/oby.22471. [DOI] [PubMed] [Google Scholar]
- 11.Frank J., Snell L., Sherbino J.C. Royal College of Physicians and Surgeons of Canada. CanMEDS 2015 Physician Competency Fram Ottawa R Coll Physicians Surg Canada; Ottawa: 2015. Physician competency framework. 2015. [Google Scholar]
- 12.CANMEDS. About. 2023. https://canmeds.royalcollege.ca/en/about#:~:text=Key competencies%3A Within each of,components of a key competency Retrieved from: [Google Scholar]
- 13.Ten Cate O. Nuts and bolts of entrustable professional activities. Journal of graduate medical education. 2013;5:157–158. doi: 10.4300/JGME-D-12-00380.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Association of Faculties of Medicine . 2023. Education.https://www.afmc.ca/resources-data/education/undergraduate-students-electives-md-graduates/ Retrieved from: [Google Scholar]
- 15.Cheung W.J., Wagner N., Frank J.R., Oswald A., Van Melle E., Skutovich A., et al. Implementation of competence committees during the transition to CBME in Canada: a national fidelity-focused evaluation. Med Teach. 2022;44:781–789. doi: 10.1080/0142159X.2022.2041191. [DOI] [PubMed] [Google Scholar]
- 16.Pinilla S., Lenouvel E., Cantisani A., Klöppel S., Strik W., Huwendiek S., et al. Working with entrustable professional activities in clinical education in undergraduate medical education: a scoping review. BMC Med Educ. 2021;21:1–10. doi: 10.1186/s12909-021-02608-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CANMEDS. Guide. 2023. https://canmeds.royalcollege.ca/guide Retrieved from: [Google Scholar]
- 18.University of Toronto . 2023. Education goals and competency framework.https://md.utoronto.ca/education-goals-and-competency-framework Retrieved from: [Google Scholar]
- 19.Western University Canada . 2023. Graduation competencies/program learning outcomes.https://www.schulich.uwo.ca/cbme/undergraduate/graduation_competencies/index.html Retrieved from. [Google Scholar]
- 20.Krathwohl D.R. A revision of Bloom's taxonomy: an overview. Theor Pract. 2002;41:212–218. [Google Scholar]
- 21.Papadopoulos S., Brennan L. Correlates of weight stigma in adults with overweight and obesity: a systematic literature review. Obesity. 2015;23:1743–1760. doi: 10.1002/oby.21187. [DOI] [PubMed] [Google Scholar]
- 22.Wu Y.K., Berry D.C. Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: a systematic review. J Adv Nurs. 2018;74:1030–1042. doi: 10.1111/jan.13511. [DOI] [PubMed] [Google Scholar]
- 23.Thoma B., Karwowska A., Samson L., Labine N., Waters H., Giuliani M., et al. Emerging concepts in the CanMEDS physician competency framework. Canadian Medical Education Journal. 2023;14:4–12. doi: 10.36834/cmej.75591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertakis K.D., Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24:229–239. doi: 10.3122/jabfm.2011.03.100170. [DOI] [PubMed] [Google Scholar]
- 25.Cardel M.I., Newsome F.A., Pearl R.L., Ross K.M., Dillard J.R., Miller D.R., et al. Patient-centered care for obesity: how health care providers can treat obesity while actively addressing weight stigma and eating disorder risk. J Acad Nutr Diet. 2022;122:1089–1098. doi: 10.1016/j.jand.2022.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernstein K.M., Manning D.A., Julian R.M. Multidisciplinary teams and obesity: role of the modern patient-centered medical home. Prim Care Clin Off Pract. 2016;43:53–59. doi: 10.1016/j.pop.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Liebhart J.L., Goodman A.B., Lindros J., Krafft C., Cook S.R., Baker A., et al. Key predictors of primary care providers' self-efficacy in caring for children with overweight or obesity. Academic Pediatrics. 2022;22:1158–1166. doi: 10.1016/j.acap.2022.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oliver T.L., Shenkman R., Diewald L.K., Smeltzer S.C. Reflective journaling of nursing students on weight bias. Nurse Educ Today. 2021;98 doi: 10.1016/j.nedt.2020.104702. [DOI] [PubMed] [Google Scholar]
- 29.Alberga A.S., Russell-Mayhew S., von Ranson K.M., McLaren L. Weight bias: a call to action. Journal of eating disorders. 2016;4:1–6. doi: 10.1186/s40337-016-0112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luig T., Anderson R., Sharma A., Campbell‐Scherer D. Personalizing obesity assessment and care planning in primary care: patient experience and outcomes in everyday life and health. Clinical obesity. 2018;8:411–423. doi: 10.1111/cob.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chan T.M., Stehman C., Gottlieb M., Thoma B. A short history of free open access medical education. the past, present, and future. ATS scholar. 2020;1:87–100. doi: 10.34197/ats-scholar.2020-0014PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vallis M. Quality of life and psychological well‐being in obesity management: improving the odds of success by managing distress. Int J Clin Pract. 2016;70:196–205. doi: 10.1111/ijcp.12765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bevan J.H., Casco K.A., Contento N., Gadre A., Hancock-Cerutti W., Jammes C., Sedlacek V., Sheffield P. Collaborating to overcome the barriers to implementing planetary health education for medical students: the international medical education collaboration on climate and sustainability (IMECCS) Eng Manag J. 2023;8(3):67–75. [Google Scholar]
- 34.Bramley A.L., McKenna L. Entrustable professional activities in entry‐level health professional education: a scoping review. Med Educ. 2021;55:1011–1032. doi: 10.1111/medu.14539. [DOI] [PubMed] [Google Scholar]
- 35.Englander R., Frank J.R., Carraccio C., Sherbino J., Ross S., Snell L., et al. Toward a shared language for competency-based medical education. Med Teach. 2017;39:582–587. doi: 10.1080/0142159X.2017.1315066. [DOI] [PubMed] [Google Scholar]
- 36.Contreras S. Obesity in adults: clinical practice guideline adapted for Chile. Medwave. 2022;22 doi: 10.5867/medwave.2022.10.2649. [DOI] [PubMed] [Google Scholar]
- 37.Breen C., O'Connell J., Geoghegan J., O'Shea D., Birney S., Tully L., et al. Obesity in adults: a 2022 adapted clinical practice guideline for Ireland. Obes Facts. 2022;15:736–752. doi: 10.1159/000527131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Meyrick J. The Delphi method and health research. Health Educ. 2003;103:7–16. [Google Scholar]